Abstract
Currently, 280 million people worldwide experience depression, ranking it third in the global burden of disease. The incidence of depression has risen due to the COVID-19 pandemic, making it essential to examine evidence-based practices in reducing depressive symptoms during this unprecedented time. This systematic review and meta-analysis aim to analyze randomized controlled trials during the COVID-19 pandemic that evaluated the effect of mindfulness meditation on depressive symptoms in individuals with depression. Four databases (PubMed, Embase, Web of Science, and Scopus) were searched in November 2023 using search terms including meditation, mindfulness, depression, and depressive symptoms. The meta-analysis was conducted using Review Manager 5.4 software (Cochrane Collaboration). A random model and Standard Mean Difference analysis with 95% CIs were used for continuous variables. The systematic review included 26 RCT studies. The meta-analysis showed significant effects of mindfulness meditation interventions (SMD = − 1.14; 95% CI − 1.45 to − 0.83; P < 0.001) in reducing depressive symptoms compared to comparison groups. The findings suggest a positive effect of mindfulness meditation on depressive symptoms in individuals with depression during the COVID-19 pandemic.
Keywords: COVID-19, Depression, Depressive symptoms, Meditation, Mindfulness
Subject terms: Rehabilitation, Psychology
Introduction
Depression, a complex and multifaceted mental illness, affects millions of people worldwide and remains a significant challenge to understand and treat due to its unclear pathogenesis and numerous contributing factors2. About 280 million people in the world are currently suffering from depression2. The symptoms of depression manifest in the cognitive, emotional, and neurological domains, and the resulting functional impairment increases with severity3. The pathogenesis of depression is not yet fully understood, and the prevailing academic view is that depression occurs as a pathological result of the interaction of multiple factors3. Several studies have shown that depression may be associated with levels and activity of serotonin and dopamine levels, changes in hypothalamic–pituitary–adrenal (HPA), hippocampal neuroplasticity, neurogenesis, structural changes in the brain, inflammation, genes and other factor3–8. It is worth noting that the serotonin hypothesis, which is currently controversial, asserts that the behavior and functioning of people with depression are related to their levels of 5-hydroxytryptamine (5HT) in the brain6. A study by Moncrieff et al. shows that there is no compelling evidence for including serotonin levels as a contributing factor to depression. It is because of such a complex multifactorial nature that the treatment of depression is challenging.
The COVID-19 pandemic significantly impacted global mental health, exacerbating depression and anxiety rates, and highlighting the urgent need for effective interventions to mitigate its effects9. The severe respiratory symptoms, high mortality rates, and rapid spread of the virus have contributed to its classification as a serious illness affecting both physical and mental health10,11. The widespread implementation of social distancing regulations, mandatory lockdowns, and other psychosocial factors during the pandemic have further exacerbated depression12. The rise in depression and anxiety during the pandemic has created a significant global burden on health systems and is expected to have long-term economic and social repercussions11. The emergence of new variants has caused heightened concerns about reinfection, leading to increased psychological distress and the need for more mental health support, further exacerbating the risk of depression13. Therefore, it is crucial to identify evidence-based interventions to provide timely and accessible mental health care to those affected, thereby reducing the burden of depression during the pandemic.
Approaches to treat depression
The use of antidepressant medications is the first-line treatment approach for depression, with a variety of classes of medications being used to target different symptoms and severity levels14. Selective serotonin reuptake inhibitors (SSRIs) are the most commonly used antidepressants in clinical practice15. Furthermore, serotonin and norepinephrine reuptake inhibitors (SNRI), monoamine oxidase inhibitors (MAOIs), and tricyclic antidepressants (TCAs) are also widely used in depression treatment16,17. One article compared the efficacy and resistance of several existing antidepressant medications. They found that discontinuation rates were higher in most antidepressant groups than in the placebo group18. Another meta-analysis showed that antidepressant efficacy increased incrementally with the severity of depression, but there was minimal improvement in mild or moderate patients19. The effect size, advantages and disadvantages of antidepressants are shown in Table 1.
Table 1.
Comparative effect sizes of pharmacological and non-pharmacological treatments for depression.
| Treatment | Effect size | Advantages | Disadvantages |
|---|---|---|---|
| Antidepressants | − 0.320 |
Currently available to prevent relapse and recurrence of depression In long-term antidepressant treatment, antidepressants can be administered by non-psychiatric physicians without specialized training 21 |
Adverse effects, higher cost, social stigma 22, gastrointestinal symptoms, sexual disfunction, weight gain, sleep disturbances, require high compliance21, low remission rate, and high recurrence rate23 |
| CBT | − 0.7524 | Cost-effective, superior relapse prevention25 | Time-consuming, costly and not easily accessible in some countries, may not be effective for all individuals25 |
| Exercise |
Walking and jogging22: − 0.62 Yoga22: − 0.55 Tai chi or Qi Gong22: − 0.42 Strength training22: − 0.49 Mixed aerobic exercise22: − 0.43 |
Fewer adverse effects than antidepressant treatment, easy to perform, low cost, no stigma23 | High drop-out rate than antidepressant treatment22 |
Despite their widespread use, antidepressants have significant drawbacks that warrant consideration, including potential side effects, limited treatment options for drug-resistant cases, and high costs associated with long-term management26,27. Antidepressants can cause significant changes in body weight, nausea, and headache symptoms, and even negatively affect sexual function15,16,28,29. In drug-resistant clinical cases, other treatment alternatives are used such as electroconvulsive therapy (ECT)3. However, accessibility to treatment options for drug-resistant cases is limited30. This kind of intervention is not suitable for all patients because electroconvulsive therapy may cause cognitive impairment and loss of autobiographical memory31. Depression is a chronic condition with a high relapse rate and requires expensive long-term counseling and medication32. Hospitalization may be required if somatization symptoms are severe, which will add additional costs. Given the above-mentioned issues, there is an urgent need for novel and effective therapies for depression.
Effective non-pharmacological interventions (Table 1), including psychotherapy, exercise, dietary treatment, and music therapy, have emerged as viable alternatives to antidepressant medications for reducing depressive symptoms, offering a safer and potentially more effective treatment option for individuals with depression33,34. Cognitive behavior therapy (CBT) is the combination of basic behavior and cognitive principles, can help patients understand and check how their thoughts, emotions and behavior interact, leading to or aggravate depression, to teach patients how to use more adaptive thoughts and behavior to replace dysfunctional thoughts and behavior, which can reduce pain and improve mood35. Currently, cognitive behavioral therapy has been a mature and effective psychotherapy for the treatment of depression36. Exercise therapy, especially tai chi, has also been reported to be beneficial in the non-pharmacological treatment of depression4. It emphasizes soothing and fluid movement along with rhythmic deep breathing to help relieve stress and depression37. In terms of dietary therapy, saffron is credited with antidepressant potential. Another article revealed that saffron's antidepressant effect may be comparable to the effects of several antidepressant medications, with fewer side effects38. Music therapy uses music as a means of intervening with depressed patients through both active and receptive approaches39,40. In summary, these treatments can be used in addition to medication or as stand-alone treatment options to help patients reduce their depressive symptoms.
While non-pharmacological interventions for depression have been shown to be effective in reducing symptoms and improving quality of life, they can also have potential side effects that should be considered. Adverse effects reported in CBT include distress, worsening of symptoms, and strains in family relations41. Music therapy may cause anxiety, depression, disorientation, mental fatigue, emotional distress, or physical discomfort due to factors such as maladaptive use, altered states, repetition, negative associations, or uncomfortable sound properties42. The adverse effects commonly reported in exercise interventions, including muscle or joint pain, headache, and fatigue, can be exacerbated if pre-existing orthopedic injuries are present43.
Mindfulness meditation for depression
Mindfulness meditation, a non-pharmacological intervention, has been shown to have a significant impact on depressive symptoms in various populations and has emerged as a promising adjunct therapy for depression. According to the National Institutes of Health, mindfulness meditation focuses on the interactions between the brain, mind, body, and behavior44. Mindfulness meditation can also be a form of mental training to help improve concentration and mood45. Modern mindfulness meditation techniques can be categorized as loving-kindness meditation, focused attention meditation, open-monitoring meditation, mind–body meditation, and transcendental meditation46. Mindfulness meditation is commonly defined clinically as non-judgmental attention to the energies of the present moment45. Mindfulness meditation is often used in everyday life to reduce stress and anxiety47. In recent years, many studies have shown the positive effects of mindfulness meditation on depressive symptoms in several populations48–51. Mindfulness meditation can lead to a calming of attitudes, help people to modulate their attention, and guide them to focus on their feelings in the present moment45. People can increase their self-awareness when practicing mindfulness meditation, which helps them to better comprehend their own emotions and states, thus increasing flexibility of thought and driving positive thoughts45. In addition, mindfulness meditation can help people relieve stress and detach from negative feelings50,52–54. Results of a meta-analysis showed a significant effect of mindfulness meditation on depressive symptoms and recommended the use of meditation-based interventions as evidence-based treatments55. In another study on mindfulness meditation and mental disorders, meditation was shown to be an effective adjunct therapy for depression46. In addition, the simplicity and safety of the procedure are the biggest advantages of mindfulness meditation over other depression treatment methods, such as ECT. It is less restricted by environment and time and can be done anywhere at any time37. Furthermore, mindfulness meditation can help treat depression and alleviate depressive symptoms at a lower cost compared with CBT, usual care, and maintenance antidepressant medication37,56. In the context of social distancing and lock down experienced in the COVID-19 pandemic, mindfulness meditation interventions could be remotely administered57. Another advantage of mindfulness meditation during the pandemic is that it can be delivered to a large number of people at once in group sessions led by trained instructors, making it a more scalable intervention compared to other approaches for depression.
Recent meta-analyses have explored the efficacy of mindfulness meditation interventions in treating depression across various age groups, yielding valuable insights into the benefits and limitations of this therapeutic approach. One meta-analysis confirmed the effectiveness of mindfulness meditation interventions in the treatment of depression by comparing 45 studies that concluded that mindfulness meditation improved depression to some extent in emerging adults50. Another meta-analysis conducted included depressed adults over the age of 65, and the final results included a total of 19 studies51. They concluded that mindfulness meditation can effectively improve the development of depression in older adults and can be used as an adjunct or alternative therapy to conventional treatment for depression in the elderly51. A meta-analysis analyzed individual differences in meditation interventions. They included and analyzed 51 studies and showed that individuals with higher levels of psychopathology or depression had poorer mental health after the meditation intervention58. However, participant demographics, psychological characteristics, and practice duration did not significantly influence the effects of the meditation intervention58. It is important to note that the COVID-19 pandemic has presented a unique and unprecedented situation, and the effectiveness of mindfulness meditation in addressing depression symptoms during this specific timeframe remains uncertain and may provide valuable information. For instance, the evaluation of efficacy of mindfulness meditation is important because it can guide researchers and clinicians to consider mindfulness meditation as an alternative therapeutic option in times of natural disasters or unprecedented situations such as the COVID-19 pandemic.
As the incidence of depression continues to rise in the wake of the COVID-19 pandemic11, it is essential to investigate the effectiveness of evidence-based practices, such as mindfulness meditation, in this unique and timely context. Although we have already resumed to the new-normal after the COVID-19 pandemic, it is unclear that if mindfulness meditation might still provide benefits in any future possible outbreaks. Previous systematic reviews on mindfulness meditation and depression did not include the follow-up period in the meta-analyses50,51. Therefore, the long-term efficacy of mindfulness meditation deserves to be explored. In terms of the intervention period, one meta analysis50 concluded that a short-term meditation intervention did not affect reducing depression. In contrast, the results of another meta analysis58 contradicted this. Therefore, it is crucial to determine whether the duration of the mindfulness meditation intervention has an impact on the reduction of depressive symptoms. It is uncertain if mindfulness meditation can still alleviate depression during disasters, such as the COVID-19 epidemic. Given the uncertainty of future outbreaks, it is important to assess the efficacy of this evidence-based treatment within this specific timeframe. Therefore, this systematic review and meta-analysis aim to analyze the effectiveness of mindfulness meditation in reducing depressive symptoms in individuals with depression in randomized controlled trials conducted during the COVID-19 pandemic. Specifically, this study aims to compare the effects of different durations of mindfulness meditation interventions, examine how different control group conditions influence the benefits of meditation, assess the differential effects of face-to-face offline versus online and app-based meditation interventions, and evaluate the relative effectiveness of meditation interventions alone versus in combination with other treatments. The research questions guiding this systematic review and meta-analysis are: What is the overall effect of mindfulness meditation on depressive symptoms in individuals with depression, and does the duration of the intervention influence its effectiveness? Do different control group conditions (e.g., waitlist, standard care, or active control) affect the observed benefits of mindfulness meditation? Are face-to-face offline and online/app-based mindfulness meditation interventions equally effective in reducing depressive symptoms, and what are the potential advantages or limitations of each format? Finally, does combining mindfulness meditation with other treatments enhance its benefits for depressive symptoms, and if so, which combinations are most effective?
Method
Search strategy
An electronic search using PubMed, Embase, Web of Science, and Scopus was conducted on November 1st, 2023. The search terms and search strategy are shown in Table 2. Two reviewers were independently involved in the literature search and study selection process. Discrepancies in the study selection were resolved by a third investigator.
Table 2.
Databases and research strategy.
| Databases | Search strategy |
|---|---|
| PubMed |
((Meditation[MeSH Major Topic]) OR (Meditation[Title/Abstract]) OR (Transcendental Meditation[Title/Abstract]) OR (Mindfulness[Title/Abstract]) OR (Mindful[Title/Abstract])) AND ((Depression[MeSH Major Topic]) OR (Emotional Depression[Title/Abstract]) OR (Symptom, Depressive[Title/Abstract]) OR (Depressive Symptom[Title/Abstract]) OR (Depressive Symptoms[Title/Abstract])) AND ((RCT[Title/Abstract]) OR (Randomized controlled trial[Title/Abstract])) Refined by: 2020–2023 |
| Embase | ('meditation'/exp OR meditation OR 'transcendental meditation':ti,ab,kw OR mindfulness:ti,ab,kw OR mindful:ti,ab,kw) AND ('depresison' OR 'depressive symptoms':ti,ab,kw OR 'depressive symptom':ti,ab,kw OR 'symptom, depressive':ti,ab,kw OR 'emotional depression':ti,ab,kw) AND [randomized controlled trial]/lim AND [2020–2023]/py |
| Web of Science |
TS = (meditation OR Transcendental Meditation OR Mindfulness OR Mindful) AND TS = (depression OR Depressive Symptoms OR Depressive Symptom OR Symptom, Depressive OR Emotional Depression) AND TS = (RCT OR randomized control trial) Refined by: Date: 2020–2023 |
| Scopus |
(TITLE-ABS-KEY (transcendental AND meditation) OR TITLE-ABS-KEY (meditation) OR TITLE-ABS-KEY (mindfulness) OR TITLE-ABS-KEY (mindful) AND TITLE-ABS-KEY (depressive AND symptoms) OR TITLE-ABS-KEY (depressive AND symptom) OR TITLE-ABS-KEY (symptom, AND depressive) OR TITLE-ABS-KEY (emotional AND depression) OR TITLE-ABS-KEY (depression) AND TITLE-ABS-KEY (rct) OR TITLE-ABS-KEY (randomized AND control AND trial)) AND PUBYEAR > 2019 AND PUBYEAR < 2024 AND (LIMIT-TO (DOCTYPE, "re")) Refined by: 2020–2023 |
Study selection
The inclusion criteria were (1) randomized controlled trial studies that compared the intervention to a control condition were included, (2) participants were adults above 18 years of age, (3) mindfulness-meditation intervention was used as the main intervention alone or combined with treatment as usual, (4) data collection was conducted during the COVID-19 pandemic, (5) studies that measured depression symptoms using validated tools were included. Studies were excluded if they (1) were reviews, meta-analyses, dissertations, book chapters, or study protocols, (2) did not evaluate mindfulness meditation on depression or depression was the second outcome, (3) were not published in English, (4) did not include results from statistical data analysis of the outcomes of interest.
Risk of bias
Two independent reviewers assessed the methodological quality using the Cochrane Randomized Trials Risk of Bias tool (RoB2). The risk assessment considered the randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome and selection of the reported result to evaluate the overall bias. The outcomes of the assessment were categorized as “High Risk”, “Low Risk” and “Some concerns”. In case of discrepancies, the final decision was made by discussion or consultation with a third author.
Statistical analysis
The meta-analysis was conducted to compare the effect of mindfulness meditation interventions on depression symptoms with the control group. The Review Manager version 5.4 (Cochrane Collaboration) was used to perform the meta-analysis. To analyze the effect of mindfulness meditation on depression, quantitative data of depressive symptoms measured using validated scales were extracted at baseline, post-test and follow-up. Subgroup analyses were conducted to explore the long-term effects of the mindfulness meditation interventions. Considering the variability of the data, standardized mean differences (SMD) were used to generate effect sizes for the forest plot. A random effect model for meta-analysis was used59. For each meta-analysis, hedge's g and the 95% confidence interval (CI) were calculated60. Comprehensive Meta-Analysis (CMA) software version 3.0 was used to conduct univariate meta-regression analysis with depression (baseline depression level), patient’s demographics (age, gender), intervention-related variables (total number of sessions, total duration of the intervention, duration per session), and type of control.
Results
Study selection
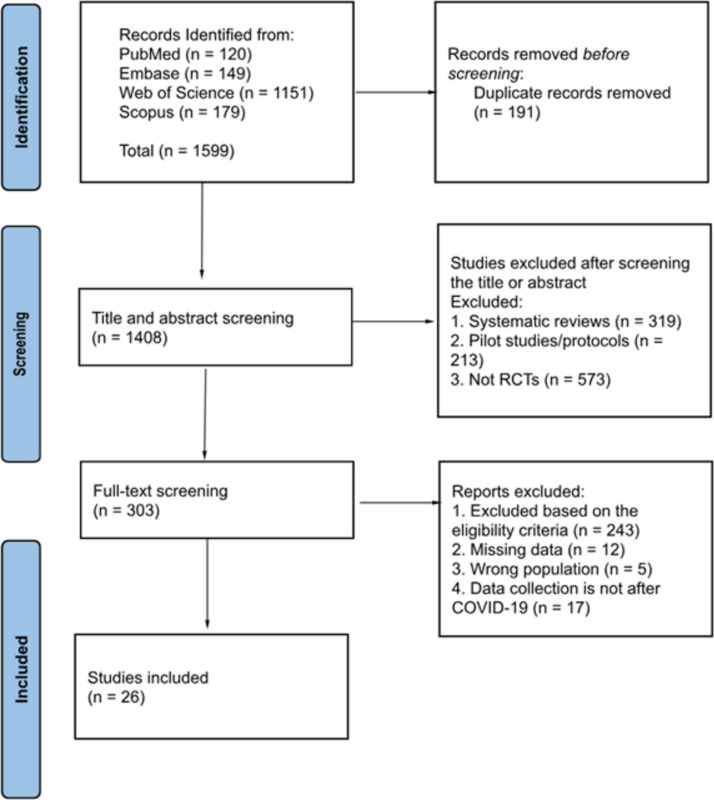
A total of 1599 records were retrieved from PubMed (n = 120), Embase (n = 149), Web of Science (n = 1151) and Scopus (n = 179) (Fig. 1). 191 duplicate records were excluded and the title and abstract of 1408 were screened. 1105 articles were removed after title and abstract screening. Of the remaining 303 studies, 277 papers were excluded because they were not RCTs, missing data, data collection was not during the COVID-19 pandemic or depression was not the primary outcome. Finally, 26 studies were included in both the systematic review and meta-analysis.
Fig. 1.
PRISMA flowchart of study selection.
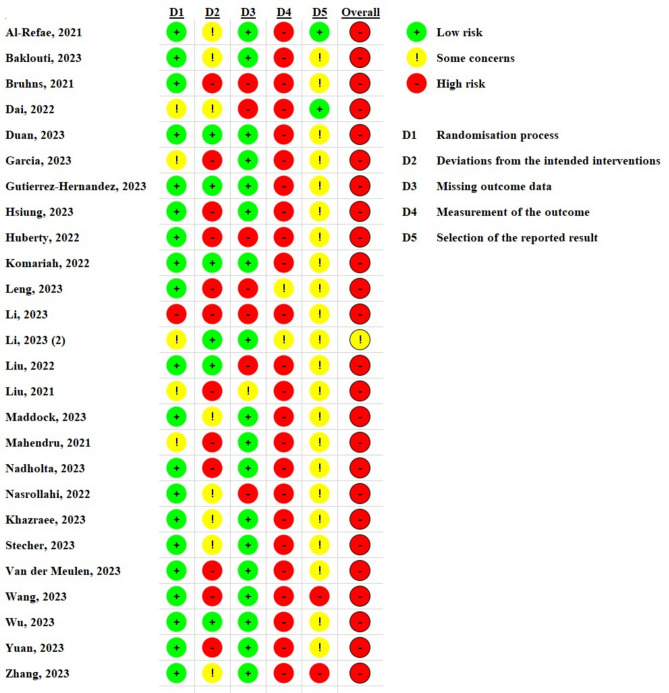
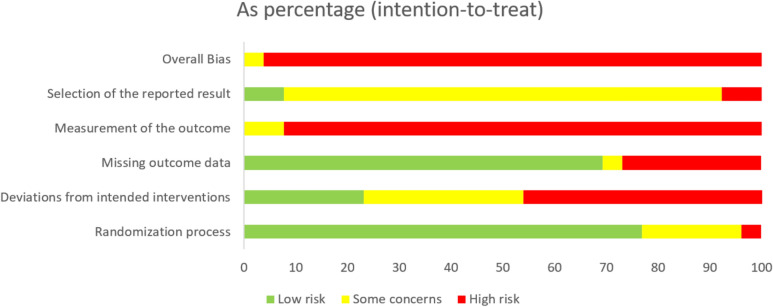
Quality and characteristics of included studies
The results of the quality assessment are shown in Figs. 2 and 3. Most articles have a low risk of bias for random sequence generation. All articles have unclearly and high risk of bias in the measurement of the outcome because it was difficult to blind the participants due to the nature of the intervention.
Fig. 2.
Traffic Light Plots of the Risk of Bias for RCTs.
Fig. 3.
Weighted Bar Plots of the Risk of Bias for RCTs.
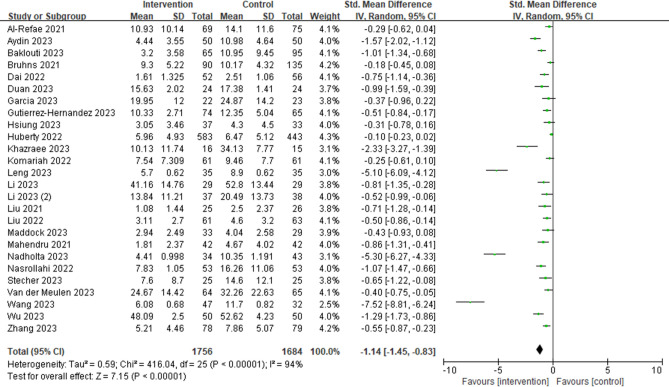
The populations included in the studies were adults. A total of 3440 participants were included in the selected studies with 1756 participants in the intervention group and 1684 participants in the control group. Six studies included women only61–65. Some studies investigated different cohorts of participants with depression-related conditions such as post-stroke depression66 (1.40%), treatment-resistant depression67 (1.31%), major depressive disorder62 (0.90%), emotion-related disorder68 (2.18%) or other health conditions that included measurement of depressive symptoms such as early-stage breast cancer69 (1.48%), autism spectrum disorder70 (1.45%), acute myocardial infarction71 (2.91%) and COVID-19 infection72,73 (6.05%).
In total, 12 studies had longer interventions with more than 8 weeks of mindfulness meditation practice61–64,65,67,69,70,74–77. Ten articles included follow-up measurements62,37–67,69,70,75,77,78. Six studies included meditation combined with other treatments such as Yoga63,69,74 (n = 288), rTMS66 (n = 48), sleep coaching76 (n = 1026) and mindful hypnotherapy72 (n = 31). A total of 635 participants from 8 studies received mindfulness meditation interventions delivered offline61,62,64,65,66,69,71,75 and the other 18 studies received online or app-based mindfulness meditation interventions (n = 2732). There are 3 types of control groups: active control65,68,77,79 (n = 158), passive control or waiting list61,62,70,74,76,78,80–83 (n = 991), and treat as usual group63–37,66–69,71–73,75,84 (n = 535).
The most frequently tools used to assess depressive symptoms were the Beck Depression Inventory (BDI‐II), the Depression Anxiety Stress Scale (DASS) and the Hamilton Depression and Patient Health Questionnaire-9 (PHQ-9) (see Appendix 1).
Results of the statistical analysis
The results of the meta-analysis showed a significant overall effect (standard mean difference (SMD) = − 1.14; 95% CI − 1.45 to − 0.83; P < 0.001, Fig. 4). The statistical analysis showed that subjects effectively reduced depressive symptoms in the mindfulness meditation groups.
Fig. 4.
Forest plot assessing the effectiveness of mindfulness meditation interventions on people with depressive symptoms.
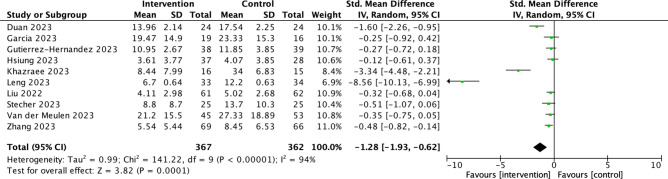
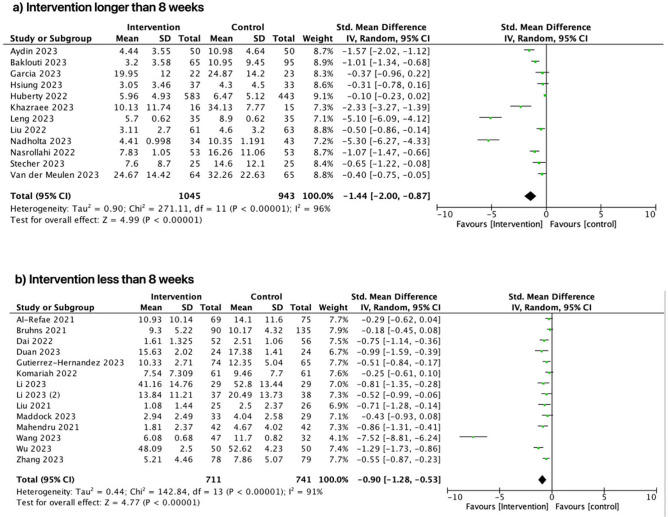
The long-term effects of mindfulness meditation to reduce depression symptoms were investigated at follow-up (see Fig. 5). The SMD was − 1.28 (95% CI − 1.93 to − 0.62) with statistical significance (P < 0.001). In addition, the meta-analysis indicates that mindfulness meditation interventions that lasted more than 8 weeks (see Fig. 6) reduced participants' depressive symptoms slightly better (SMD = − 1.44; 95% CI − 2.00 to − 0.87) than those that lasted less time (see Fig. 6; SMD) = − 0.90; 95% CI − 1.28 to − 0.53).
Fig. 5.
Forest plot comparing follow-up effects.
Fig. 6.
Forest plot for interventions that: (a) lasted longer than 8 weeks; and (b) lasted less than 8 weeks.
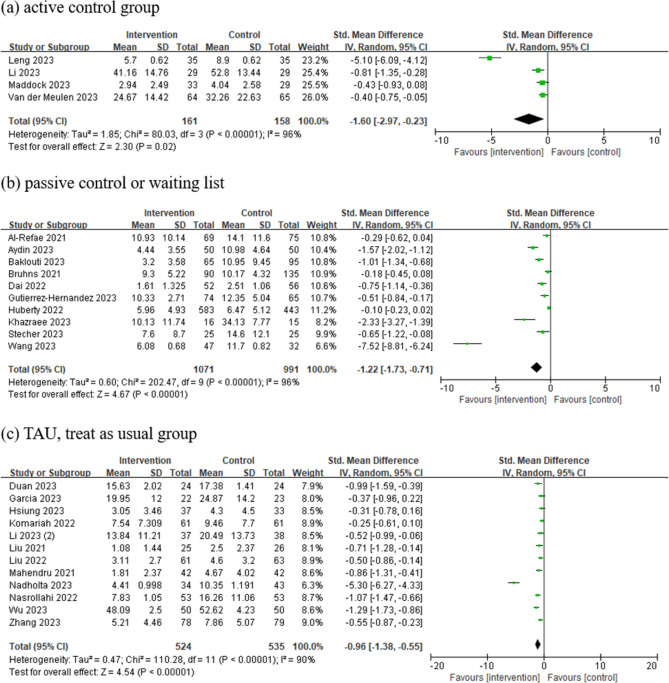
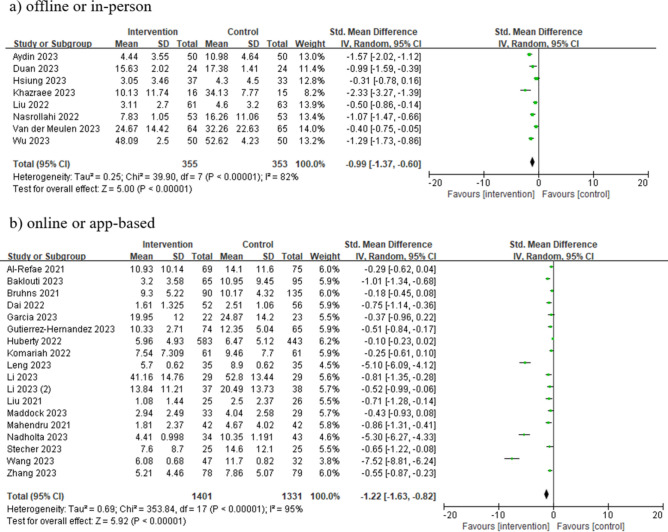
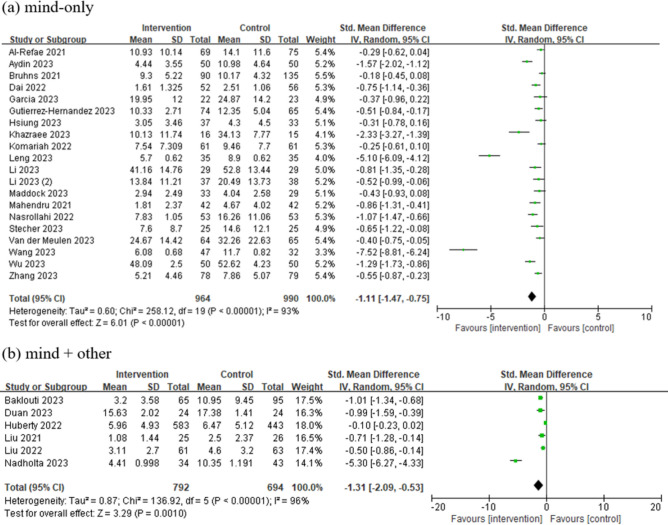
Subgroup analyses conducted based on different types of control groups (Figs. 7, 8, and 9) revealed that mindfulness meditation interventions either delivered online or offline, reduced depressive symptoms regardless of the type of comparison group, including, active or passive control groups. The largest SMD was observed when the comparison was done against active control with an SMD of − 1.60 (95% CI − 2.97 to − 0.23), followed by the passive control group (SMD = − 1.22), and treatment as usual group (SMD = − 0.96). The results also indicate that offline or in-person interventions (SMD = − 0.99; 95% CI − 1.37 to − 0.60) had a similar effect size to online or app-based meditation interventions (Fig. 8; SMD = − 1.22; 95% CI − 1.63 to − 0.82). Mindfulness meditation in combination with other interventions (SMD = − 1.31; 95% CI − 2.09 to − 0.53) were more effective than using mindfulness meditation alone (see Fig. 9; SMD = − 1.11; 95% CI − 1.47 to − 0.75). The univariate meta-regression analysis revealed that the total duration of intervention (p = 0.0015) was significant. This may indicate that the longer the duration, the more efficacious the intervention to reduce depression symptoms (Table 3). The regression scatterplot figures can be found in Appendix 2.
Fig. 7.
Forest plot for studies that used: (a) active control group; (b) passive control or waiting list control; and (c) TAU treat as usual group.
Fig. 8.
Forest plot for interventions that were (a) offline or in-person and delivered (b) online or app-based.
Fig. 9.
Forest plot for interventions, including (a) mindfulness meditation only (mind-only) or (b) mindfulness meditation combined with other interventions (mind + other).
Table 3.
Results of meta-regression of moderators for the effect sizes of depression symptoms.
| Moderators | N | Univariate coefficient | Z-value | p-value |
|---|---|---|---|---|
| Demographics: | ||||
| Mean age (years) | 25 | 0.0053 | 0.56 | 0.5751 |
| Gender (percentage of female patients) | 26 | − 0.0103 | − 1.78 | 0.0748 |
| Baseline: | ||||
| Baseline depression level | 24 | − 0.0028 | − 0.33 | 0.7433 |
| Intervention: | ||||
| Total number of sessions | 22 | − 0.0119 | − 1.22 | 0.2206 |
| Duration per session | 21 | 0.0008 | 0.35 | 0.7248 |
| Total duration of intervention | 21 | − 0.0009 | − 3.17 | 0.0015* |
| Type of control: | ||||
| Passive vs. Active | 26 | 0.5433 | 1.14 | 0.2535 |
| Passive vs. TAU | 0.062 | 0.18 | 0.8593 | |
| TAU vs. Active | − 0.5171 | − 1.02 | 0.3056 | |
TAU Treatment as usual.
*p < 0.05.
Discussion
The COVID-19 pandemic has affected all aspects of human health11. Many individuals and families are experiencing significant COVID-19-related stress and are struggling to find useful coping mechanisms. In response to this, there has been growing interest in the potential of mindfulness meditation as a means of alleviating these symptoms82. However, the evidence regarding the effectiveness of mindfulness meditation in the context of disaster-induced depression, such as that experienced during the COVID-19 outbreak, remains inconclusive. This systematic review and meta-analysis focused on RCTs that evaluated the effects of meditation interventions on depression symptoms after the COVID-19 pandemic. The current evidence indicates that mindfulness and meditation intervention may have certain beneficial effects in reducing depression levels during the COVID-19 period. Once people learn mindfulness meditation strategies, they can practice it anytime, anywhere and incorporate it into their lives82. Mindfulness meditation is a potentially practical life skill that can be used to deal with a variety of health issues55. This systematic review marks an important step in the use of mindfulness meditation as an adjunctive therapy to reduce depression symptoms under pandemic conditions.
Follow-up data were analyzed to examine whether short-term effects were maintained over time. Although our data suggest that mindfulness meditation interventions have long-term efficacy (p < 0.001), 6 of the 10 articles showed that the treatment effect was not statistically significant compared with the control group after follow-up65,67,69,70,75,78. The treatment effect decreased at follow-up. This suggests that mindfulness meditation interventions need to be practiced consistently to maintain the benefits gained and to provide patients with emotion and symptom management skills that are effective in the long term69. In addition, the result in this meta-analysis also suggests that longer-term interventions (lasting more than 8 weeks) were more adequate to reduce depressive symptoms more substantially. This indicates that sustained and consistent practice of mindfulness meditation may be necessary to achieve substantial improvements in depressive symptoms, particularly in the context of disaster-induced depression such as that experienced during the COVID-19 pandemic. The effectiveness of longer-term mindfulness meditation interventions is supported by previous studies on mindfulness meditation that have indicated that the mental health benefits tend to amplify over time85.
It is worth noting that the control group settings were not uniform across the reviewed articles. When compared with active control groups (SMD of -1.60), mindfulness meditation interventions were more effective than when compared with passive control groups (SMD = − 1.22). However, only a few studies used active control groups with a small sample size in the comparison group. The larger effect observed when comparing mindfulness interventions and active control groups as opposed to passive control groups may be explained by the nature of the conditions of the active controls. It has been previously suggested that active controls used in mindfulness should be structurally equivalent to the intervention1. For instance, conditions such as the number and duration of sessions, therapist training and qualification, format (i.e., individual or group-based), and group discussion (if applicable) of the active control should match the conditions of the mindfulness-based intervention group1. The structural differences between the active control and the intervention group of the studies included in the subgroup analysis may be responsible for the larger effect observed when compared with passive controls. In one study65, the intervention group used a group-based format, whereas the active control involved individual consultation sessions. This difference in format may have contributed to a more significant disparity between the two groups, as the group-based intervention could lead to enhanced participant engagement and support. Therefore, it is crucial for future studies to ensure structural equivalence when selecting an appropriate active control, thereby verifying that the structural conditions are comparable to those of the intervention.
It is important to consider the comparison groups used in RCT studies of mindfulness interventions (Davidson & Kaszniak 2015), and most published mindfulness intervention RCTs use TAU or wait-list controlled comparison groups. These studies provide a valuable initial evaluation of whether mindfulness interventions have an impact on outcomes above and beyond standard care or no treatment. Researchers have made impressive efforts to develop active treatment comparison programs that control for non-mindfulness-specific treatment factors (e.g., group support, home practice exercises, relaxation, placebo expectancies). These programs provide opportunities to evaluate whether mindfulness interventions have unique treatment effects above and beyond non-mindfulness-specific factors and whether mindfulness interventions can outperform gold-standard active pharmacological or behavioral treatments.
Mindfulness meditation interventions reduced depressive symptoms when compared with TAU. Therefore, standardizing the treatment provided to the control group is a challenge that should be addressed in future research as the intensity of treatment received by the control group can directly impact the effectiveness of the intervention measures undertaken by the experimental group.
There are a variety of interventions on mindfulness meditation to reduce symptoms associated with depression, which include mindfulness-based stress reduction (MBSR), Mindfulness-Based Cognitive Therapy (MBCT), yoga, combined with rTMS and online programs48,55,86. Our result is similar to previous research that meditation can be combined with other interventions to reduce depression symptoms87–89. MBSR and MBCT are the most frequently used interventions in mindfulness meditation for alleviating depression symptoms, as indicated by their utilization in many research articles61,64,65–69,71,75,78–80,82–84,86. Some studies believe that mindfulness meditation can help individuals cope with depression during the COVID-19 pandemic by reducing over-identification with one's own negative emotions through self-compassion62,77–80,83. Self-compassion is the ability to treat oneself with kindness (with care and understanding rather than self-judgment)78. Improved self-compassion increases a person's openness and heightened ability to adapt to stressful situations90,91. Another article highlighted "decentering" as a clinically meaningful mechanism linked to reducing depression relapse/recurrence79. Furthermore, potential mechanisms contributing to the effectiveness of MBCT in reducing depression symptoms include increasing mindfulness and decreasing experiential avoidance, reductions in cognitive reactivity, improvements in autobiographical memory specificity, and reductions in rumination79. In the future, a more comprehensive exploration of these mechanisms may aid in refining mindfulness meditation, enhancing its effectiveness, and potentially eliminating aspects of the treatment that do not yield positive outcomes while incorporating components that do.
Three articles within the reviewed literature incorporate yoga as part of their intervention strategies63,69,74. Mindfulness-based yoga intervention, also included elements like body scanning and sitting meditation, designed to teach individuals how to observe the present moment in a non-reactive and non-judgmental manner69. MBSR participants acquired the ability to approach even intense negative emotions with this non-reactive and non-judgmental mindset. In the context of the COVID-19 pandemic, 18 articles have been implemented online or smartphone-used meditation and they have similar effects in reducing depression symptoms compared with in-person intervention. It is lower in cost and broader in coverage compared to traditional face-to-face intervention and is more in line with the development of the times. The benefits of Internet-based interventions lie mainly in the high degree of autonomy and privacy. They can be used from any location and are usually offered for free or at a low cost. They are not intended to replace traditional psychotherapy, but rather to expand the scope of traditional therapy92. One article found that expected treatment outcomes and attitudes toward Internet and cell phone interventions were correlated with frequency of use81. The more positive the attitude and the more positive the expected outcome, the more frequently the self-help smartphone application was used. Participants with higher expectations and greater hope for treatment outcomes also experienced greater reductions in depressive symptoms. In addition, digital interventions are more effective when they include customized therapist support that provides feedback, questions, and clarifying answers93. These variables can have an impact on determining the effectiveness of methods to improve efficacy, which needs further investigation.
In one of the studies, Repetitive Transcranial Magnetic Stimulation (rTMS) was combined with Mindfulness-Based Stress Reduction (MBSR) as an intervention, and it proved effective in reducing depression symptoms66. Patients who underwent this combination therapy demonstrated significant improvements in various aspects, including their depressed mood, cognitive functioning, daily living activities, and sleep quality. An article66 proposed that depressive symptoms are closely linked to cognitive deficits. The use of rTMS, which incorporates positive thinking meditation and MBSR, appears to enhance the ability of depressed patients to suppress negative stimuli. This improvement is achieved by elevating the Dorsolateral Prefrontal Cortex (DLPFC) activation level and enhancing cognitive functioning. This observation is in line with previous research findings45,94,95. These findings align with the Mindfulness-to-Meaning Theory, which posits that interventions focused on promoting positive thinking effectively enhance cognitive functioning and reduce negative cognitive biases associated with cognitive deficits in individuals with depression96. Moreover, the synergistic effect of MBSR enables the state of depression among patients receiving rTMS to remain stable and valid over the 8-week follow-up period66.
The studies included did not report any adverse events arising from the mindfulness meditation interventions evaluated. However, it is important to consider safety and potential adverse effects associated with mindfulness meditation practices. In recent years, as mindfulness meditation has become more widely used, concerns about its potential adverse effects have also grown. Several adverse effects associated with mindfulness meditation such as pain, anxiety, and even more serious issues like episodes of psychosis or mania, have been reported97–99. While some studies have attempted to standardize the reporting of meditation-related adverse reactions (MRAEs), definitions have remained inconsistent100. Studies specifically focused on contraindications and adverse events experienced by individuals who learn how to meditate in mindfulness-based practices (MBP) have found that serious adverse events are relatively rare, typically occurring during intensive meditation practice101. These reported adverse events are not shown to have more serious consequences or require hospitalization2,3. Mindfulness meditation is still considered a safe intervention due to the rare occurrence of adverse events97,102. Nevertheless, it should be noteworthy that mindfulness meditation may not be suitable for everyone. Therefore, mindfulness meditation teachers and mindfulness researchers should be cautious and carefully screen participants to identify severe symptoms of anxiety, psychosis, trauma, or any physical condition such as asthma or breathing difficulties before the implementation of mindfulness meditation interventions103. Furthermore, mindfulness meditation teachers and researcher must receive the relevant training to screen for potential risks regarding mindfulness meditation practices and to identify adverse events, without causing panic, trauma memory or other discomfort to help patients practice mindfulness meditation safely98.
Limitations
Despite the use of rigorous search criteria and comprehensive reporting of the reviews, there are limitations to the reviews that need to be considered. Firstly, the selected articles were limited to English, which may have resulted in a lack of high-quality articles not written in English. Secondly, the methodological differences between the studies evaluated limits the generalizability of the results. For example, there was a lack of consistency in the outcome measures, with depression assessed using five different scales, each of which may have defined each outcome in a slightly different way. Finally, some characteristics of the participants varied from study to study, such as age, medication taken, and daily activities varied between studies and this variability in the study populations needs to be considered to interpret the overall findings.
Conclusions
Considering the unpredictability of future outbreaks, it is crucial to evaluate the effectiveness of mindfulness medication based on data within this particular timeframe. The systematic review and meta-analysis incorporated data from 26 studies, and the findings suggest that mindfulness meditation interventions alleviate depressive symptoms during the COVID-19 epidemic outbreak, thus improving people's overall physical and mental health. The findings of suggest that prolonged intervention (more than 8 weeks) may be more effective in reducing depressive symptoms. Mindfulness meditation may have long-term benefits, but continuous practice is needed. Online meditation has similar effects compared with offline interventions. Meditation can be combined with other interventions to reduce depressive symptoms. Furthermore, upcoming studies investigating meditation interventions for individuals with depressive symptoms should carefully consider factors such as the dosage of the intervention and the standardization of control groups.
Supplementary Information
Author contributions
Conceptualization, and Supervision: DGHT, SPCN, WKWL and BWML; Conceptualization, Methodology, Data curation, and Formal analysis: YF, YS, YL, DISV, JJZ; Writing—original draft: YF, YS, YL, DISV; Writing—review & editing: JJZ, WKWL.
Data availability
All data generated or analyzed during this study are available from the corresponding author on request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Yumiao Fu, Yifan Song, Yining Li and Dalinda Isabel Sanchez-Vidana.
Contributor Information
Way Kwok‑Wai Lau, Email: wkwlau@hkmu.edu.hk.
Davynn Gim Hoon Tan, Email: davynn.gh.tan@polyu.edu.hk.
Benson Wui-Man Lau, Email: benson.lau@polyu.edu.hk.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-71213-9.
References
- 1.MacCoon, D. G. et al. The validation of an active control intervention for mindfulness based stress reduction (MBSR). Behav. Res. Ther.50, 3–12 (2012). 10.1016/j.brat.2011.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Depressive disorder (depression). https://www.who.int/news-room/fact-sheets/detail/depression (2023).
- 3.Malhi, G. S. & Mann, J. J. Depression. Lancet392, 2299–2312 (2018). 10.1016/S0140-6736(18)31948-2 [DOI] [PubMed] [Google Scholar]
- 4.Wang, H.-Q., Wang, Z.-Z. & Chen, N.-H. The receptor hypothesis and the pathogenesis of depression: Genetic bases and biological correlates. Pharmacol. Res.167, 105542 (2021). 10.1016/j.phrs.2021.105542 [DOI] [PubMed] [Google Scholar]
- 5.Moncrieff, J. et al. The serotonin theory of depression: A systematic umbrella review of the evidence. Mol. Psychiatry28, 3243–3256 (2023). 10.1038/s41380-022-01661-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jesulola, E., Micalos, P. & Baguley, I. J. Understanding the pathophysiology of depression: From monoamines to the neurogenesis hypothesis model—Are we there yet?. Behav. Brain Res.341, 79–90 (2018). 10.1016/j.bbr.2017.12.025 [DOI] [PubMed] [Google Scholar]
- 7.Tartt, A. N., Mariani, M. B., Hen, R., Mann, J. J. & Boldrini, M. Dysregulation of adult hippocampal neuroplasticity in major depression: Pathogenesis and therapeutic implications. Mol. Psychiatry27, 2689–2699 (2022). 10.1038/s41380-022-01520-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gałecki, P. & Talarowska, M. Inflammatory theory of depression. Psychiatr. Pol.52, 437–447 (2018). 10.12740/PP/76863 [DOI] [PubMed] [Google Scholar]
- 9.Torales, J., O’Higgins, M., Castaldelli-Maia, J. M. & Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry66, 317–320 (2020). 10.1177/0020764020915212 [DOI] [PubMed] [Google Scholar]
- 10.Shereen, M. A., Khan, S., Kazmi, A., Bashir, N. & Siddique, R. COVID-19 infection: Emergence, transmission, and characteristics of human coronaviruses. J. Adv. Res.24, 91–98 (2020). 10.1016/j.jare.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santomauro, D. F. et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet398, 1700–1712 (2021). 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhu, S. et al. Effects of virtual reality intervention on cognition and motor function in older adults with mild cognitive impairment or dementia: A systematic review and meta-analysis. Front. Aging Neurosci.10.3389/fnagi.2021.586999 (2021). 10.3389/fnagi.2021.586999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Araf, Y. et al. Omicron variant of SARS-CoV-2: Genomics, transmissibility, and responses to current COVID-19 vaccines. J. Med. Virol.94, 1825–1832 (2022). 10.1002/jmv.27588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ruberto, V. L., Jha, M. K. & Murrough, J. W. Pharmacological treatments for patients with treatment-resistant depression. Pharmaceuticals13, 116 (2020). 10.3390/ph13060116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moret, C., Isaac, M. & Briley, M. Review: Problems associated with long-term treatment with selective serotonin reuptake inhibitors. J. Psychopharmacol.23, 967–974 (2009). 10.1177/0269881108093582 [DOI] [PubMed] [Google Scholar]
- 16.Gill, H. et al. Antidepressant medications and weight change: A narrative review. Obesity28, 2064–2072 (2020). 10.1002/oby.22969 [DOI] [PubMed] [Google Scholar]
- 17.Peng, G., Tian, J., Gao, X., Zhou, Y. & Qin, X. Research on the pathological mechanism and drug treatment mechanism of depression. Curr. Neuropharmacol.13, 514–523 (2015). 10.2174/1570159X1304150831120428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cipriani, A. et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. Lancet391, 1357–1366 (2018). 10.1016/S0140-6736(17)32802-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fournier, J. C. et al. Antidepressant drug effects and depression severity: A patient-level meta-analysis. JAMA303, 47 (2010). 10.1001/jama.2009.1943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hengartner, M. P. & Plöderl, M. Statistically significant antidepressant-placebo differences on subjective symptom-rating scales do not prove that the drugs work: Effect size and method bias matter!. Front. Psychiatry9, 517 (2018). 10.3389/fpsyt.2018.00517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cosci, F., Mansueto, G. & Fava, G. A. Relapse prevention in recurrent major depressive disorder. A comparison of different treatment options based on clinical experience and a critical review of the literature. Int. J. Psychiatry Clin. Pract.24, 341–348 (2020). 10.1080/13651501.2020.1779308 [DOI] [PubMed] [Google Scholar]
- 22.Recchia, F. et al. Comparative effectiveness of exercise, antidepressants and their combination in treating non-severe depression: A systematic review and network meta-analysis of randomised controlled trials. Br. J. Sports Med.56, 1375–1380 (2022). 10.1136/bjsports-2022-105964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xie, Y. et al. The effects and mechanisms of exercise on the treatment of depression. Front. Psychiatry12, 1904 (2021). 10.3389/fpsyt.2021.705559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lopez, M. A. & Basco, M. A. Effectiveness of cognitive behavioral therapy in public mental health: Comparison to treatment as usual for treatment -resistant depression. Adm. Policy Ment. Health42, 87–98 (2015). 10.1007/s10488-014-0546-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Myhr, G. & Payne, K. Cost-effectiveness of cognitive-behavioural therapy for mental disorders: Implications for public health care funding policy in Canada. Can. J. Psychiatry51, 662–670 (2006). 10.1177/070674370605101006 [DOI] [PubMed] [Google Scholar]
- 26.Strawn, J. R., Mills, J. A., Poweleit, E. A., Ramsey, L. B. & Croarkin, P. E. Adverse effects of antidepressant medications and their management in children and adolescents. Pharmacotherapy43, 675–690 (2023). 10.1002/phar.2767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhou, Q., Li, X., Yang, D., Xiong, C. & Xiong, Z. A comprehensive review and meta-analysis of neurological side effects related to second-generation antidepressants in individuals with major depressive disorder. Behav. Brain Res.447, 114431 (2023). 10.1016/j.bbr.2023.114431 [DOI] [PubMed] [Google Scholar]
- 28.Lorenz, T., Rullo, J. & Faubion, S. Antidepressant-induced female sexual dysfunction. Mayo Clin. Proc.91, 1280–1286 (2016). 10.1016/j.mayocp.2016.04.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rothmore, J. Antidepressant-induced sexual dysfunction. Med. J. Aust.212, 329–334 (2020). 10.5694/mja2.50522 [DOI] [PubMed] [Google Scholar]
- 30.Voineskos, D., Daskalakis, Z. J. & Blumberger, D. M. Management of treatment-resistant depression: Challenges and strategies. Neuropsychiatr. Dis. Treat.16, 221–234 (2020). 10.2147/NDT.S198774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Porter, R. J. et al. Cognitive side-effects of electroconvulsive therapy: What are they, how to monitor them and what to tell patients. BJPsych Open6, e40 (2020). 10.1192/bjo.2020.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moriarty, A. S. et al. Predicting relapse or recurrence of depression: Systematic review of prognostic models. Br. J. Psychiatry221, 448–458 (2022). 10.1192/bjp.2021.218 [DOI] [PubMed] [Google Scholar]
- 33.Sukhato, K. et al. Efficacy of home-based non-pharmacological interventions for treating depression: A systematic review and network meta-analysis of randomised controlled trials. BMJ Open7, e014499 (2017). 10.1136/bmjopen-2016-014499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Farah, W. H. et al. Non-pharmacological treatment of depression: A systematic review and evidence map. Evid.-Based Med.21, 214–221 (2016). 10.1136/ebmed-2016-110522 [DOI] [PubMed] [Google Scholar]
- 35.Batinic, B. Cognitive models of positive and negative symptoms of schizophrenia and implications for treatment. Psychiatria Danubina31, 181–4 (2019). [PubMed] [Google Scholar]
- 36.Weersing, V. R., Jeffreys, M., Do, M.-C.T., Schwartz, K. T. G. & Bolano, C. Evidence base update of psychosocial treatments for child and adolescent depression. J. Clin. Child Adolesc. Psychol.46, 11–43 (2017). 10.1080/15374416.2016.1220310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang, X. et al. Effectiveness of digital guided self-help mindfulness training during pregnancy on maternal psychological distress and infant neuropsychological development: Randomized controlled trial. J. Med. Internet Res.25, e41298 (2023). 10.2196/41298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shafiee, M., Arekhi, S., Omranzadeh, A. & Sahebkar, A. Saffron in the treatment of depression, anxiety and other mental disorders: Current evidence and potential mechanisms of action. J. Affect. Disord.227, 330–337 (2018). 10.1016/j.jad.2017.11.020 [DOI] [PubMed] [Google Scholar]
- 39.Aalbers, S. et al. Music therapy for depression. Cochrane Database Syst. Rev.11, CD004517 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hartmann, M. et al. Musical interaction in music therapy for depression treatment. Psychol. Music51, 33–50 (2023). 10.1177/03057356221084368 [DOI] [Google Scholar]
- 41.Schermuly-Haupt, M.-L., Linden, M. & Rush, A. J. Unwanted events and side effects in cognitive behavior therapy. Cogn. Ther. Res.42, 219–229 (2018). 10.1007/s10608-018-9904-y [DOI] [Google Scholar]
- 42.Murakami, B. The music therapy and harm model (MTHM): Conceptualizing harm within music therapy practice. ECOS Revista Científica de Musicoterapia y Disciplinas Afines6, 003–003 (2021). 10.24215/27186199e003 [DOI] [Google Scholar]
- 43.Heissel, A. et al. Exercise as medicine for depressive symptoms? A systematic review and meta-analysis with meta-regression. Br. J. Sports Med.57, 1049–1057 (2023). 10.1136/bjsports-2022-106282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Simkin, D. R. & Black, N. B. Meditation and mindfulness in clinical practice. Child Adolesc. Psychiatr. Clin. N. Am.23, 487–534 (2014). 10.1016/j.chc.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 45.Tang, Y.-Y., Hölzel, B. K. & Posner, M. I. The neuroscience of mindfulness meditation. Nat. Rev. Neurosci.16, 213–225 (2015). 10.1038/nrn3916 [DOI] [PubMed] [Google Scholar]
- 46.Shen, H., Chen, M. & Cui, D. Biological mechanism study of meditation and its application in mental disorders. Gen. Psych.33, e100214 (2020). 10.1136/gpsych-2020-100214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maric, V., Ramanathan, D. & Mishra, J. Respiratory regulation & interactions with neuro-cognitive circuitry. Neurosci. Biobehav. Rev.112, 95–106 (2020). 10.1016/j.neubiorev.2020.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.González-Valero, G., Zurita-Ortega, F., Ubago-Jiménez, J. L. & Puertas-Molero, P. Use of meditation and cognitive behavioral therapies for the treatment of stress, depression and anxiety in students. A systematic review and meta-analysis. IJERPH16, 4394 (2019). 10.3390/ijerph16224394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li, Y., Zhang, J., Meng, Y. & Hofmann, S. G. Effect of mindfulness meditation on depression during pregnancy: A meta-analysis. Mindfulness10.3389/fpsyg.2022.963133 (2023). 10.3389/fpsyg.2022.963133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reangsing, C., Lauderman, C. & Schneider, J. K. Effects of mindfulness meditation intervention on depressive symptoms in emerging adults: A systematic review and meta-analysis. J. Integr. Complement. Med.28, 6–24 (2022). 10.1089/jicm.2021.0036 [DOI] [PubMed] [Google Scholar]
- 51.Reangsing, C., Rittiwong, T. & Schneider, J. K. Effects of mindfulness meditation interventions on depression in older adults: A meta-analysis. Aging Mental Health25, 1181–1190 (2021). 10.1080/13607863.2020.1793901 [DOI] [PubMed] [Google Scholar]
- 52.Pascoe, M. C., Thompson, D. R., Jenkins, Z. M. & Ski, C. F. Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. J. Psychiatr. Res.95, 156–178 (2017). 10.1016/j.jpsychires.2017.08.004 [DOI] [PubMed] [Google Scholar]
- 53.Xunlin, N., Lau, Y. & Klainin-Yobas, P. The effectiveness of mindfulness-based interventions among cancer patients and survivors: A systematic review and meta-analysis. Support Care Cancer28, 1563–1578 (2020). 10.1007/s00520-019-05219-9 [DOI] [PubMed] [Google Scholar]
- 54.Chayadi, E., Baes, N. & Kiropoulos, L. The effects of mindfulness-based interventions on symptoms of depression, anxiety, and cancer-related fatigue in oncology patients: A systematic review and meta-analysis. PLoS ONE17, e0269519 (2022). 10.1371/journal.pone.0269519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Goldberg, S. B. et al. Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clin. Psychol. Review59, 52–60 (2018). 10.1016/j.cpr.2017.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang, L. et al. Economic evaluations of mindfulness-based interventions: A systematic review. Mindfulness (N. Y.)13, 2359–2378 (2022). 10.1007/s12671-022-01960-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Borghi, S. et al. Beneficial effects of a program of Mindfulness by remote during COVID-19 lockdown. Eur. Rev. Med. Pharmacol. Sci.26, 5562–5567 (2022). [DOI] [PubMed] [Google Scholar]
- 58.Buric, I., Farias, M., Driessen, J. M. A. & Brazil, I. A. Individual differences in meditation interventions: A meta-analytic study. Br. J. Health Psychol.27, 1043–1076 (2022). 10.1111/bjhp.12589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med.6, e1000100 (2009). 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Higgins, J. P. T. Measuring inconsistency in meta-analyses. BMJ327, 557–560 (2003). 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Aydin, Ş & Budak, F. K. Effect of mindfulness-based stress reduction training on anxiety, depression, and hopelessness in menopausal women: An experimental study. Psychiatric Ann.53, 83–94 (2023). 10.3928/00485713-20230207-06 [DOI] [Google Scholar]
- 62.Khazraee, H., Bakhtiari, M., Kianimoghadam, A. S. & Ghorbanikhah, E. The effectiveness of mindful hypnotherapy on depression, self-compassion, and psychological inflexibility in females with major depressive disorder: A single-blind, randomized clinical trial. Int. J. Clin. Exp. Hypnosis71, 63–78 (2023). 10.1080/00207144.2022.2160257 [DOI] [PubMed] [Google Scholar]
- 63.Nadholta, P. et al. Mind-body practice as a primer to maintain psychological health among pregnant women–YOGESTA–a randomized controlled trial. Front. Public Health11, 1201371 (2023). 10.3389/fpubh.2023.1201371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nasrollahi, M., Ghazanfar Pour, M., Ahmadi, A., Mirzaee, M. & Alidousti, K. Effectiveness of mindfulness-based stress reduction on depression, anxiety, and stress of women with the early loss of pregnancy in southeast Iran: A randomized control trial. Reprod. Health19, 233 (2022). 10.1186/s12978-022-01543-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Van Der Meulen, R. T., Veringa-Skiba, I. K., Van Steensel, F. J. A., Bögels, S. M. & De Bruin, E. I. Mindfulness-based childbirth and parenting for pregnant women with high fear of childbirth and their partners: Outcomes of a randomized controlled trial assessing short- and longer-term effects on psychological well-being, birth and pregnancy experience. Midwifery116, 103545 (2023). 10.1016/j.midw.2022.103545 [DOI] [PubMed] [Google Scholar]
- 66.Duan, H. et al. Effectiveness evaluation of repetitive transcranial magnetic stimulation therapy combined with mindfulness-based stress reduction for people with post-stroke depression: A randomized controlled trial. Int. J. Environ. Res. Public Health20, 930 (2023). 10.3390/ijerph20020930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Garcia, A. et al. Efficacy of an adjuvant non-face-to-face multimodal lifestyle modification program for patients with treatment-resistant major depression: A randomized controlled trial. Psychiatry Res.319, 114975 (2023). 10.1016/j.psychres.2022.114975 [DOI] [PubMed] [Google Scholar]
- 68.Li, Y. et al. A randomized controlled trial of an online self-help mindfulness intervention for emotional distress: Serial mediating effects of mindfulness and experiential avoidance. Mindfulness14, 1–14 (2023). 10.1007/s12671-023-02083-x [DOI] [Google Scholar]
- 69.Liu, W., Liu, J., Ma, L. & Chen, J. Effect of mindfulness yoga on anxiety and depression in early breast cancer patients received adjuvant chemotherapy: A randomized clinical trial. J. Cancer Res. Clin. Oncol.148, 2549–2560 (2022). 10.1007/s00432-022-04167-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Stecher, C. et al. App-based meditation habits maintain reductions in depression symptoms among autistic adults. Autism28, 1487–502 (2024). 10.1177/13623613231200679 [DOI] [PubMed] [Google Scholar]
- 71.Wu, K. et al. Mindfulness-based stress reduction combined with early cardiac rehabilitation improves negative mood states and cardiac function in patients with acute myocardial infarction assisted with an intra-aortic balloon pump: A randomized controlled trial. Front. Cardiovasc. Med.10, 1166157 (2023). 10.3389/fcvm.2023.1166157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Liu, Y. et al. Using mindfulness to reduce anxiety and depression of patients with fever undergoing screening in an isolation ward during the COVID-19 outbreak. Front. Psychol.12, 664964 (2021). 10.3389/fpsyg.2021.664964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mahendru, K. et al. Effect of meditation and breathing exercises on the well-being of patients with SARS-CoV-2 infection under institutional isolation: A randomized control trial. Indian J. Palliat. Care27, 490–494 (2021). 10.25259/IJPC_40_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Baklouti, S. et al. The effect of web-based Hatha yoga on psychological distress and sleep quality in older adults: A randomized controlled trial. Complement. Ther. Clin. Pract.50, 101715 (2023). 10.1016/j.ctcp.2022.101715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hsiung, Y., Chen, Y.-H., Lin, L.-C. & Wang, Y.-H. Effects of Mindfulness-Based Elder Care (MBEC) on symptoms of depression and anxiety and spiritual well-being of institutionalized seniors with disabilities: A randomized controlled trial. BMC Geriatr.23, 497 (2023). 10.1186/s12877-023-04220-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Huberty, J. L., Espel-Huynh, H. M., Neher, T. L. & Puzia, M. E. Testing the pragmatic effectiveness of a consumer-based mindfulness mobile app in the workplace: Randomized controlled trial. JMIR mHealth uHealth10, e38903 (2022). 10.2196/38903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Leng, L. L., Yin, X. C., Chan, C. L. W. & Ng, S. M. Antenatal mobile-delivered mindfulness-based intervention to reduce perinatal depression risk and improve obstetric and neonatal outcomes: A randomized controlled trial. J. Affect. Disord.335, 216–227 (2023). 10.1016/j.jad.2023.04.133 [DOI] [PubMed] [Google Scholar]
- 78.Gutiérrez-Hernández, M. E., Fanjul Rodríguez, L. F., Díaz Megolla, A., Oyanadel, C. & Peñate Castro, W. The effect of daily meditative practices based on mindfulness and self-compassion on emotional distress under stressful conditions: A randomized controlled trial. Eur. J. Investig. Health Psychol. Educ.13, 762–775 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Maddock, A., McGuigan, K. & McCusker, P. A randomised trial of mindfulness-based social work and self-care with social workers. Curr. Psychol.42, 9170–9183 (2023). 10.1007/s12144-023-04410-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Al-Refae, M., Al-Refae, A., Munroe, M., Sardella, N. A. & Ferrari, M. A self-compassion and mindfulness-based cognitive mobile intervention (serene) for depression, anxiety, and stress: Promoting adaptive emotional regulation and wisdom. Front. Psychol.12, 648087 (2021). 10.3389/fpsyg.2021.648087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bruhns, A., Lüdtke, T., Moritz, S. & Bücker, L. A mobile-based intervention to increase self-esteem in students with depressive symptoms: Randomized controlled trial. JMIR mHealth uHealth9, e26498 (2021). 10.2196/26498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dai, Z. et al. Mindfulness-based online intervention on mental health among undergraduate nursing students during coronavirus disease 2019 pandemic in Beijing, China: A randomized controlled trial. Front. Psychiatry13, 949477 (2022). 10.3389/fpsyt.2022.949477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wang, M. et al. Effects of a online brief modified mindfulness-based stress reduction therapy for anxiety among Chinese adults: A randomized clinical trial. J. Psychiatr. Res.161, 27–33 (2023). 10.1016/j.jpsychires.2023.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Komariah, M., Ibrahim, K., Pahria, T., Rahayuwati, L. & Somantri, I. Effect of mindfulness breathing meditation on depression, anxiety, and stress: A randomized controlled trial among university students. Healthcare11, 26 (2022). 10.3390/healthcare11010026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sedlmeier, P., Loße, C. & Quasten, L. C. Psychological effects of meditation for healthy practitioners: An update. Mindfulness9, 371–387 (2018). 10.1007/s12671-017-0780-4 [DOI] [Google Scholar]
- 86.Li, H. et al. Effect of the online mindfulness-based stress reduction on anxiety and depression status of COVID-19 patients treated in fangcang hospitals: A randomized controlled trial. Psychol. Res. Behav. Manag.16, 2735–2745 (2023). 10.2147/PRBM.S414553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yang, Y., Cao, D., Lyu, T. & Gao, W. Meta-analysis of a mindfulness yoga exercise intervention on depression—Based on intervention studies in China. Front. Psychol.14, 1283172 (2023). 10.3389/fpsyg.2023.1283172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fjorback, L. O., Arendt, M., Ørnbøl, E., Fink, P. & Walach, H. Mindfulness-based stress reduction and mindfulness-based cognitive therapy—A systematic review of randomized controlled trials. Acta Psychiatr Scand124, 102–119 (2011). 10.1111/j.1600-0447.2011.01704.x [DOI] [PubMed] [Google Scholar]
- 89.Hofmann, S. G., Sawyer, A. T., Witt, A. A. & Oh, D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J. Consult. Clin. Psychol.78, 169–183 (2010). 10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Luo, Y. et al. Self-compassion may reduce anxiety and depression in nursing students: A pathway through perceived stress. Public Health174, 1–10 (2019). 10.1016/j.puhe.2019.05.015 [DOI] [PubMed] [Google Scholar]
- 91.Neff, K. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self Identity2, 85–101 (2003). 10.1080/15298860309032 [DOI] [Google Scholar]
- 92.Moessner, M. & Bauer, S. E-Mental-Health und internetbasierte Psychotherapie: Auf dem Weg in die Versorgung. Psychotherapeut62, 251–266 (2017). 10.1007/s00278-017-0198-4 [DOI] [Google Scholar]
- 93.Lau, Y., Cheng, J.-Y., Wong, S.-H., Yen, K.-Y. & Cheng, L.-J. Effectiveness of digital psychotherapeutic intervention among perinatal women: A systematic review and meta-analysis of randomized controlled trials. WJP11, 133–152 (2021). 10.5498/wjp.v11.i4.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Allen, M. et al. Cognitive-affective neural plasticity following active-controlled mindfulness intervention. J. Neurosci.32, 15601–15610 (2012). 10.1523/JNEUROSCI.2957-12.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Liu, C., Wang, M., Liang, X., Xue, J. & Zhang, G. Efficacy and safety of high-frequency repetitive transcranial magnetic stimulation for poststroke depression: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil.100, 1964–1975 (2019). 10.1016/j.apmr.2019.03.012 [DOI] [PubMed] [Google Scholar]
- 96.Garland, E. L., Hanley, A. W., Goldin, P. R. & Gross, J. J. Testing the mindfulness-to-meaning theory: Evidence for mindful positive emotion regulation from a reanalysis of longitudinal data. PLoS ONE12, e0187727 (2017). 10.1371/journal.pone.0187727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Binda, D. D., Greco, C. M. & Morone, N. E. What are adverse events in mindfulness meditation?. Glob. Adv. Health Med.11, 2164957X2210966 (2022). 10.1177/2164957X221096640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kabat-Zinn, J. Foreword: Seeds of a necessary global renaissance in the making: the refining of psychology’s understanding of the nature of mind, self, and embodiment through the lens of mindfulness and its origins at a key inflection point for the species. Curr. Opin. Psychol.28, xi–xvii (2019). 10.1016/j.copsyc.2019.02.005 [DOI] [PubMed] [Google Scholar]
- 99.López-Navarro, E. & Al-Halabí, S. Mindfulness on daily life coping in people experiencing psychosis: A randomized controlled trial. Int. J. Clin. Health Psychol.22, 100298 (2022). 10.1016/j.ijchp.2022.100298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Britton, W. B., Lindahl, J. R., Cooper, D. J., Canby, N. K. & Palitsky, R. Defining and measuring meditation-related adverse effects in mindfulness-based programs. Clin. Psychol. Sci.9, 1185–1204 (2021). 10.1177/2167702621996340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chadwick, P. Mindfulness for psychosis: A humanising therapeutic process. Curr. Opin. Psychol.28, 317–320 (2019). 10.1016/j.copsyc.2019.07.022 [DOI] [PubMed] [Google Scholar]
- 102.Amick, H. R. et al. Comparative benefits and harms of second generation antidepressants and cognitive behavioral therapies in initial treatment of major depressive disorder: Systematic review and meta-analysis. BMJ10.1136/bmj.h6019 (2015). 10.1136/bmj.h6019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Dobkin, P. L., Irving, J. A. & Amar, S. For whom may participation in a mindfulness-based stress reduction program be contraindicated?. Mindfulness3, 44–50 (2012). 10.1007/s12671-011-0079-9 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are available from the corresponding author on request.