Abstract
Rationale
To provide an overview of the current status of cardiac multimodality imaging practices in Europe and radiologist involvement using data from the European Society of Cardiovascular Radiology (ESCR) MRCT-registry.
Materials and methods
Numbers on cardiac CT and MRI examinations were extracted from the MRCT-registry of the ESCR, entered between January 2011 and October 2023 (n = 432,265). Data collection included the total/annual numbers of examinations, indications, complications, and reporting habits.
Results
Thirty-two countries contributed to the MRCT-registry, including 29 European countries. Between 2011 and 2022, there was a 4.5-fold increase in annually submitted CT examinations, from 3368 to 15,267, and a 3.8-fold increase in MRI examinations, from 3445 to 13,183. The main indications for cardiac CT were suspected coronary artery disease (CAD) (59%) and transcatheter aortic valve replacement planning (21%). The number of patients with intermediate pretest probability who underwent CT for suspected CAD showed an increase from 61% in 2012 to 82% in 2022. The main MRI indications were suspected myocarditis (26%), CAD (21%), and suspected cardiomyopathy (19%). Adverse event rates were very low for CT (0.3%) and MRI (0.7%) examinations. Reporting of CT and MRI examinations was performed mainly by radiologists (respectively 76% and 71%) and, to a lesser degree, in consensus with non-radiologists (19% and 27%, respectively). The remaining examinations (4.9% CT and 1.7% MRI) were reported by non-radiological specialties or in separate readings of radiologists and non-radiologists.
Conclusions
Real-life data on cardiac imaging in Europe using the largest available MRCT-registry demonstrate a considerable increase in examinations over the past years, the vast majority of which are read by radiologists. These findings indicate that radiologists contribute to meeting the increasing demands of competent and effective care in cardiac imaging to a relevant extent.
Clinical relevance statement
The number of cardiac CT and MRI examinations has risen over the past years, and radiologists read the vast majority of these studies as recorded in the MRCT-registry.
Key Points
• The number of cardiac imaging examinations is constantly increasing.
• Radiologists play a central role in providing cardiac CT and MR imaging services to a large volume of patients.
• Cardiac CT and MR imaging examinations performed and read by radiologists show a good safety profile.
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1007/s00330-024-10644-4.
Keywords: Registry data, Cardiac diseases, Magnetic resonance imaging, CT angiography, Cardiac imaging techniques
Introduction
Over the past two decades, the indications for advanced cardiovascular imaging have undergone a significant transformation, reshaping diagnostic paradigms in various clinical scenarios. This evolution aligns with the growing body of scientific evidence regarding the central role of computed tomography (CT) and magnetic resonance imaging (MRI) in the diagnosis, prognostic stratification, and therapeutic guidance of cardiovascular disease [1–6].
Coronary CT angiography is recognized as the primary imaging modality for patients with a low-to-intermediate probability of coronary artery disease (CAD) [7]. Moreover, coronary CT angiography has an important role in pre-procedural imaging, spanning from transcatheter aortic valve replacement (TAVR) planning [8, 9] to newer applications in guiding interventional procedures [10].
Stress MRI has shown the overall highest accuracy in diagnosing ischemia, outperforming stress echocardiography and single-photon emission CT, particularly in patients with intermediate to high probability of CAD [11, 12]. The role of cardiac MRI extends beyond CAD risk stratification and myocardial viability assessment. Major consensus documents and guidelines [13–15] advocate its use for a diverse spectrum of clinical conditions including congenital heart disease, cardiomyopathy, myocarditis and its differentials, and when echocardiography yields suboptimal or inconclusive results [16].
Therefore, the demand for multimodality non-invasive cardiovascular imaging is constantly increasing and requires trained professionals [17, 18]. There are some data (in particular for coronary CT angiography) that the anticipated future workload expansion of cardiovascular imaging could outstrip the existing scanner capacity and trained workforce with regard to radiology technicians and imaging specialists [18]. In response to, and in anticipation of this demand, cardiac CT and MRI are now a formal and integral part of every radiology residency training program in Europe and its individual countries, and fellowship programs assist in the training of radiologists subspecialising in multimodality cardiac imaging [19–22].
In 2011, a registry for cardiac CT and MRI examinations, called the MRCT-registry, was established under the heading of the European Society of Cardiovascular Radiology (ESCR). This registry serves various purposes, such as to map activity of European cardiac radiology practices including trends in protocols, medication, and indications over time, documenting information for accreditation, identification of expert centres, fostering collaboration for multicentre trials, and ensuring consistent, high-quality patient care.
The current study aims to provide an overview of the status of advanced cardiac imaging practices in Europe and radiologist involvement using the structured database of from the MRCT-registry.
Methods
Registry design
The MRCT-registry was established in 2011, the same year that the ESR/ESCR and the German Roentgen Society (DRG) launched cardiovascular imaging certification initiatives, which includes the European Board of Cardiovascular Radiology (EBCR) diploma. The registry was intended to collect anonymized data on the use and indications for cardiac CT and MRI studies in Europe. It remains the only cardiac imaging registry that collects data from both imaging modalities. Complying with the Declaration of Helsinki, a local ethics committee approved the research protocol and waived the need for patient informed consent (Leipzig University; No. 131/17-ek).
Registry composition and available data
The MRCT-registry incorporates a variety of information, including basic patient characteristics like sex and age, but also details regarding the indication, final diagnosis, and imaging protocol characteristics. Documentation of cardiac CT and MRI cases in the MRCT-registry was a prerequisite to apply for Q1-Q3 certificates of the German Roentgen Society (DRG) [22]. Some previous studies reported results from the MRCT-registry on different aspects [22–25].
We obtained data from the MRCT-registry regarding the number of cardiac CT and MRI examinations that were submitted and their main indication, entered from January 2011 until October 1, 2023. We also extracted information about medications administered prior to or during exams, as well as the number and type of complications, and the reporting physician(s) of cardiac CT and MRI examinations. Possible categories for the latter were (i) reporting by radiologists, (ii) consensus reading (radiologist and non-radiologist), (iii) reporting by a non-radiologist, and (iv) separate readings by radiologist and non-radiologist. Pretest probability for patients with suspected CAD was classified as previously suggested [26]. Adverse events categories were predefined by the design of the registry. The Appendix (Supplementary Material, Table S1) contains the complete list of parameters extracted from the registry for this study.
Statistical analysis
The objectives of the registry are descriptive in nature; therefore, absolute numbers and percentages were used to describe the registry data. Linear regression models were fit to plot the trends for the indication and pretest probability of CAD in CT and for the indication of myocarditis in MRI, as main indications for CT and MRI, respectively. From the models, 95% confidence intervals were derived and then plotted with the package ggplot2. Fisher’s exact test was used to compare the frequency of adverse events between stress and non-stress MRI examinations. Analysis was performed in R (version 4.3.1, The R Foundation).
Results
Contributing countries and number of examinations in the MRCT-registry
A total of 32 countries contributed to the MRCT-registry, including 29 European countries (Fig. 1). The three participating non-European countries were Bangladesh, Canada, and Kazakhstan. As of October 1, 2023, the ESCR Registry includes 205,999 entries for CT and 226,266 entries for MRI, totalling 432,265 cardiac cross-sectional imaging examinations. Figure 2 shows the trend in submissions from January 2011 to October 2023. Between 2011 and the end of 2022 (the last complete year included in this study), there was a 4.5-fold increase in annually submitted CT examinations, from 3368 to 15,267, and a 3.8-fold increase in MRI examinations, from 3445 to 13,183. The majority (56.8%) of the 1204 individual examiners in the MRCT-registry submitted both cardiac CT and MRI cases, whereas a minority submitted cases in only cardiac CT (22.3%) or MRI (20.8%). The national situation in Germany as a prime example for the MRCT-registry, certification centres, and accreditation program is provided in Fig. 3.
Fig. 1.

European countries contributing to the MRCT-registry (indicated in red)
Fig. 2.
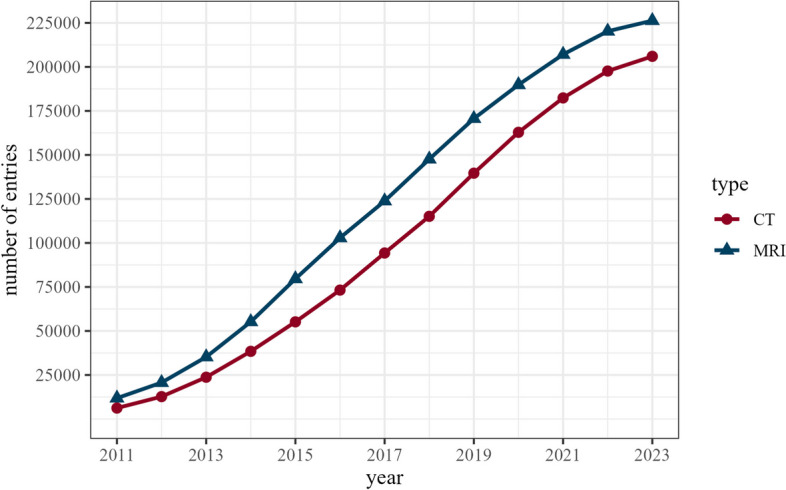
Total number of entries in the ESCR MRCT-registry from January 2011 until October 1, 2023
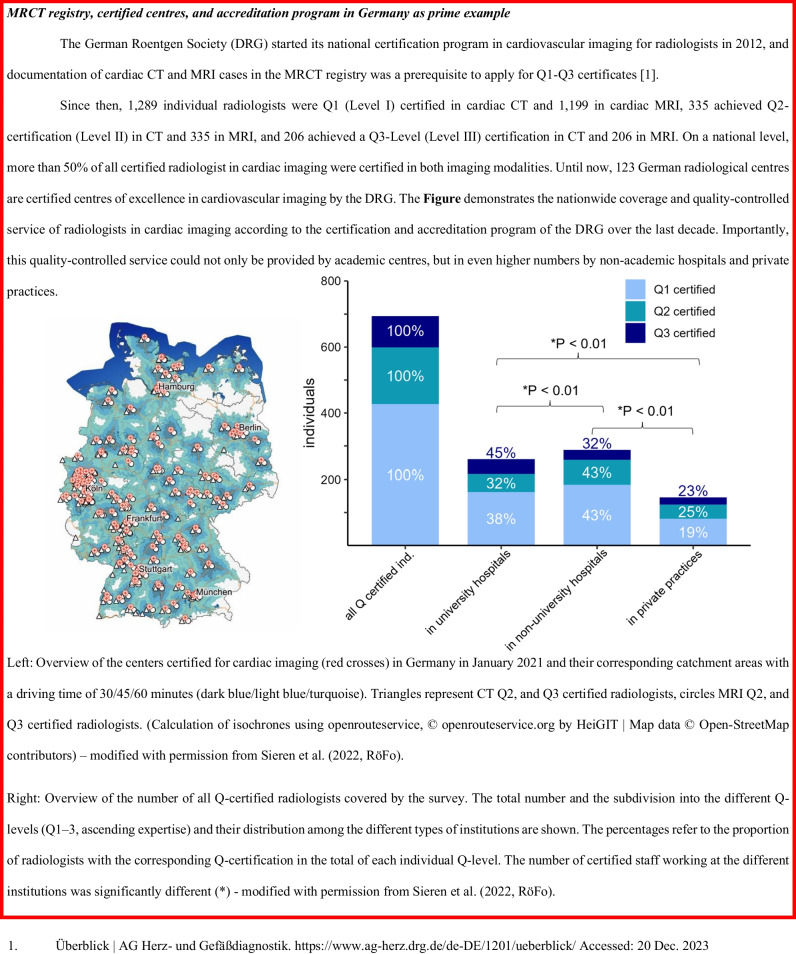
Fig. 3.
MRCT registry, certified centres, and accreditation program in Germany as prime example
Main indications
The principal indication for cardiac CT was suspected CAD (n = 121,051, 58.8%). TAVR planning was the indication in 20.9% (n = 43,141). Known valvular heart disease (n = 15,289, 7.4%), visualisation of pulmonary veins pre- or post-ablation (n = 13,354, 6.5%), and imaging of known CAD (n = 12,819, 6.2%) were other common indications. The top 10 indications of cardiac CT are listed in Table 1. The primary indication of suspected CAD showed a considerable proportional increase from 2012 to 2022 from 48.2 to 60.2% of all CT submissions (Fig. 4). Analysis of the pretest probabilities for CAD showed a decrease for the low pretest probability category, from 32.7% (905/2766) in 2012 to 14.1% (1063/7515) in 2022, and a corresponding increase in the intermediate pretest category from 61.1% (1691/2766) in 2012 to 82.4% (6189/7515) in 2022. CT for suspicion of CAD was only limitedly used in patients with a high pretest probability; they comprised 6.1% (170/2766) in 2012 and 3.5% (263/7515) in 2022 of all patients undergoing CT for CAD evaluation (Fig. 5).
Table 1.
Top 10 indications for cardiac CT
| Indication | Number of cases N = 205,999 |
Frequency |
|---|---|---|
| Suspected CAD | 121,051 | 58.8% |
| TAVR planning | 43,141 | 20.9% |
| Rule-out CAD in known heart valve disease | 15,289 | 7.4% |
| Visualisation of pulmonary veins | 13,354 | 6.5% |
| Known CAD | 12,819 | 6.2% |
| Visualisation of coronary veins | 3672 | 1.8% |
| Triple rule-out | 3378 | 1.6% |
| Suspected valve disease | 2043 | 1.0% |
| CABG-patency | 1672 | 0.8% |
| Post-TAVR imaging | 1651 | 0.8% |
CAD coronary artery disease, TAVR transcatheter aortic valve replacement, CABG coronary artery bypass graft. N number of patients with cardiac CT
Categories are not mutually exclusive due to overlapping indications
Fig. 4.
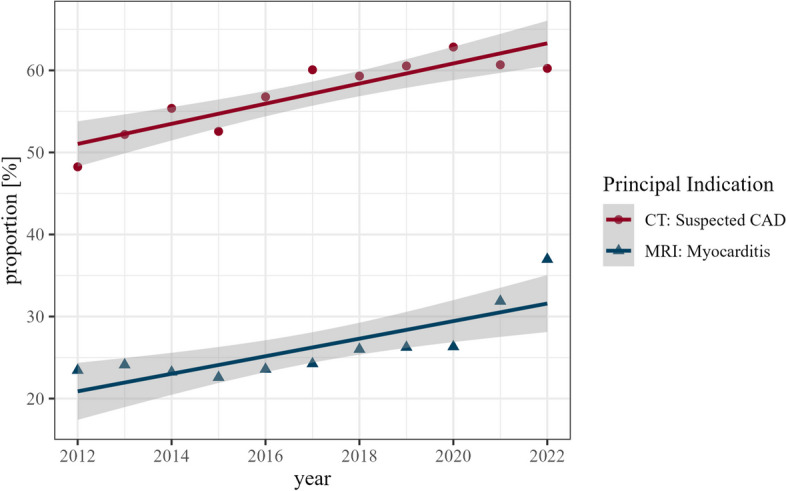
Annual submissions of the principal indication in cardiac CT (red dots) and cardiac MRI (blue triangles). Symbols denote the relative frequency in percentages. Lines represent linear models representing the trend. Grey shading represents the 95% confidence interval derived from the linear models
Fig. 5.
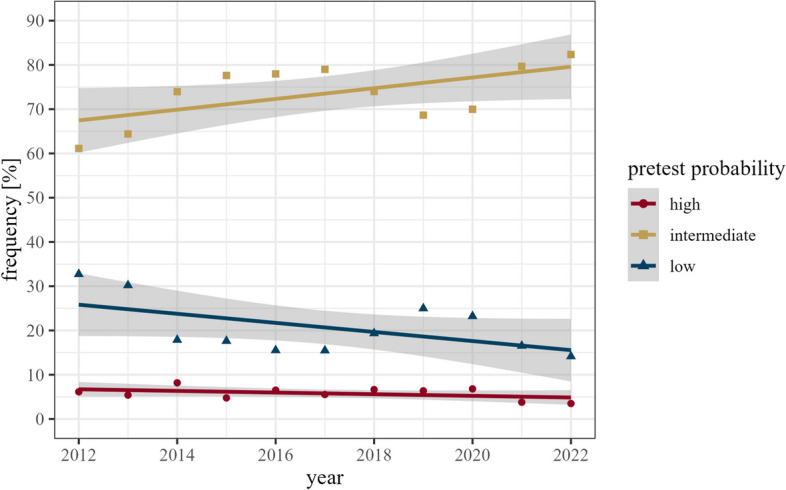
Distribution of pretest probabilities of CAD for annual cardiac CT submissions. Symbols depict data points. Lines represent linear regression models representing trends. Grey shading represents 95% confidence interval derived from the linear models
The main indications for cardiac MRI examinations were suspected myocarditis (25.7%) and suspicion of CAD (21.4%), followed by suspected cardiomyopathy (19.3%), known CAD (16.2%), and myocardial viability (8.9%). The top 10 indications for cardiac MRI are listed in Table 2. The primary indication of suspected myocarditis showed a considerable annual increase from 2012 to 2022 from 23.4 to 36.9% of all MRI indications (Fig. 4).
Table 2.
Top 10 indications for cardiac MRI
| Indication | Number of cases N = 226,266 |
Frequency |
|---|---|---|
| Suspected myocarditis | 58,260 | 25.7% |
| Suspected CAD | 48,406 | 21.4% |
| Suspected cardiomyopathy | 43,733 | 19.3% |
| Known CAD | 36,615 | 16.2% |
| Viability assessment | 20,079 | 8.9% |
| Known valve disease | 7324 | 3.2% |
| Known congenital heart disease | 6992 | 3.1% |
| Known cardiomyopathy | 5596 | 2.5% |
| Suspected valve disease | 4278 | 1.9% |
| Visualisation of pulmonary veins | 4254 | 1.9% |
MRI magnetic resonance imaging [examination], CAD coronary artery disease
N number of patients with cardiac MRI. Categories are not mutually exclusive due to overlapping indications
Medication used for cardiac CT and MRI
The most common medication in cardiac CT was negative chronotropic medication for heart rate control such as beta-blockers (n = 49,766/205,999, 24.2%), ivabradine (n = 1097, 0.5%), and in rare cases (n = 19, 0.01%) calcium channel antagonists. The second most commonly used medications in CT were nitrates (n = 49,471, 24.0%) for vasodilation of the coronary arteries. Drugs for sedation (n = 556, 0.3%), premedication for known or suspected contrast media allergy (n = 416, 0.2%), or perchlorates for hyperthyroidism (n = 62, 0.03%) were also utilized, but rarely. In patients undergoing CT for suspected CAD, beta-blockers and nitrates were administered in 37.2% (n = 45,066/121,051) and 37.0% (n = 44,791/121,051) of examinations, respectively. More details on medication used for CT can be found in Table 3.
Table 3.
Medication for cardiac CT
| Medication | Number of cases in total N = 205,999 |
Frequency in total | Number of cases in suspected CAD N = 121,051 |
Frequency of cases in suspected CAD |
|---|---|---|---|---|
| Nitrates | 49,471 | 24.0% | 44,791 | 37.0% |
| Beta-blockers—oral | 25,297 | 12.3% | 23,087 | 19.1% |
| Beta-blockers—intravenous | 24,469 | 11.9% | 21,979 | 18.2% |
| Ivabradine | 1097 | 0.5% | 1066 | 0.9% |
| Sedation | 556 | 0.3% | 479 | 0.4% |
| Premedication for contrast allergy | 416 | 0.2% | 264 | 0.2% |
| Sodium perchlorate | 62 | 0.03% | 24 | 0.02% |
| Calcium channel blocker | 19 | 0.01% | 17 | 0.01% |
| Adenosine for myocardial perfusion study | 15 | 0.01% | 9 | 0.01% |
CAD coronary artery disease. N number of patients in category
Medications are not mutually exclusive due to different indications
In cardiac MRI, pharmacological stress testing was conducted in 57,428 of 226,266 cases (25.4%). Stress imaging was mostly performed using adenosine (n = 50,131, 87.3%) or regadenoson (n = 6384, 11.1%) as stressor agent, whereas dobutamine was used only in 1.6% of cases (n = 913). In MRI for suspected CAD, stress testing was conducted more frequently than on average (n = 35,173/48,406, 72.7%). Other medication was used rarely, including sedating medication (483, 0.2%), nitrates (254, 0.1%), and negative chronotropic agents (n = 201, 0.1%). More details on medication in MRI can be found in Table 4.
Table 4.
Medication for cardiac MRI
| Medication | Number of cases in total N = 226,266 |
Frequency in total | Number of cases in suspected CAD N = 48,406 |
Frequency of cases in suspected CAD |
|---|---|---|---|---|
| Adenosine | 50,131 | 22.2% | 30,470 | 62.9% |
| Regadenoson | 6384 | 2.8% | 4106 | 8.5% |
| Dobutamine | 913 | 0.4% | 597 | 1.2% |
| Sedation | 483 | 0.2% | 107 | 0.2% |
| Nitrates | 254 | 0.1% | 145 | 0.3% |
| Beta-blockers—intravenous | 108 | 0.05% | 56 | 0.1% |
| Beta-blockers—oral | 85 | 0.04% | 23 | 0.05% |
| Premedication for contrast allergy | 46 | 0.02% | 11 | 0.02% |
| Calcium channel blocker | 8 | 0.004% | 4 | 0.01% |
CAD coronary artery disease. N number of patients in category
Medications are not mutually exclusive due to different indications
Safety evaluation
In both MRI and CT, the rate of adverse events was very low. Safety assessment for CT revealed adverse events in 0.3% of cases (n = 547/205,999), of which 0.17% were related to a hypersensitivity reaction to iodinated contrast media (n = 366/205,999). Extravasation of contrast media accounted for another 0.08% of adverse events (n = 172/205,999). Additionally, six cases of contrast-induced nephropathy (0.003%, n = 6/205,999) and two instances of thyrotoxic crisis (0.001%, n = 2/205,999) were reported. The six events of contrast-induced nephropathy occurred in five male patients and one female patient (median age 81.5 years, IQR 4.75 years); indications for these studies were workup for TAVR in two, suspected CAD in two, and triple rule-out in two patients.
In MRI, adverse events were reported in 0.7% of cases (n = 1649/226,266) and occurred more often in stress (0.8%, n = 458/57,428) as compared to non-stress (0.7%, n = 1191/168,838) examinations (p = 0.027). The most frequently reported adverse events were dyspnoea (n = 501/226,266, 0.2%) followed by hypersensitivity reactions to contrast media (n = 267/226,266, 0.12%). Very rare occurrences included the accidental discovery of an implanted pacemaker or ICD device (n = 12/226,266, 0.005%) and contrast-induced nephropathy (n = 3/226,266, 0.001%).
Reporting approaches
Most submitted cases were reported by radiologists alone (76.1% for CT, 71.4% for MRI), followed by joint consensus readings of radiologists with non-radiologists (19.0% and 26.9%, respectively). The remaining 4.9% (CT) and 1.7% (MRI) examinations were reported by non-radiological specialties, or in separate readings of radiologists and non-radiologists. A graphical representation of the reporting statistics is shown in Fig. 6.
Fig. 6.
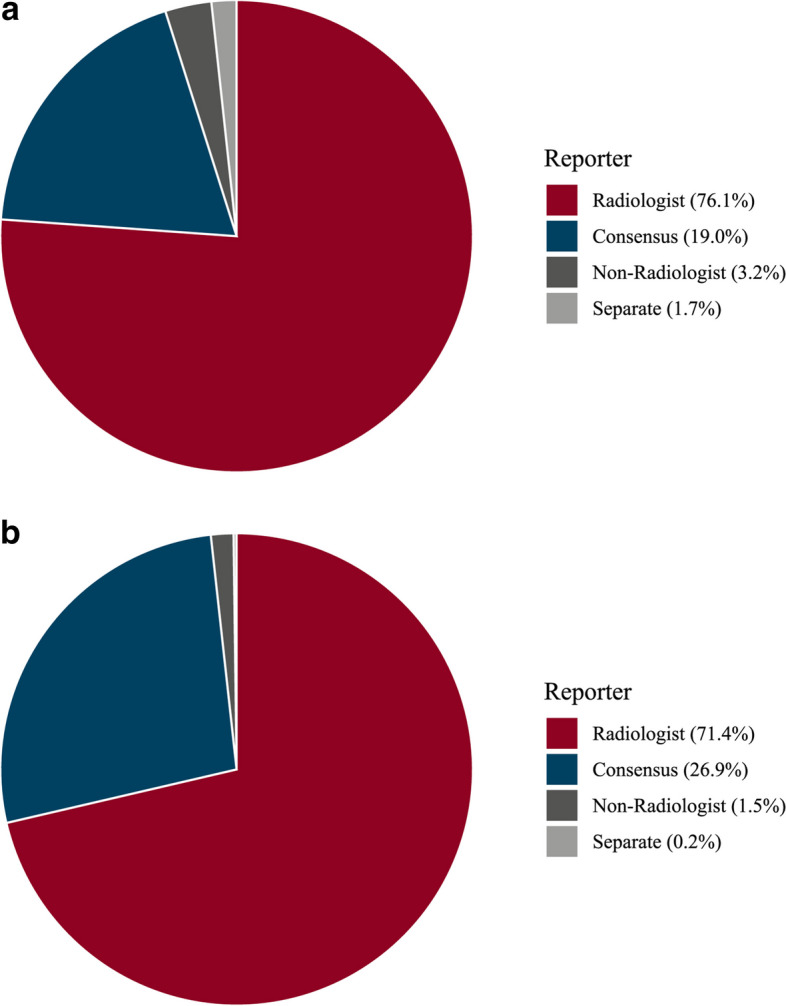
Reporting practices based on MRCT-registry data for CT (a) and MRI (b). Consensus: Examination read by radiologist and cardiologist in consensus
Discussion
The use of cardiac CT and MRI is poised for further growth, based on several scientific publications, guidelines, and recommendation papers by medical societies in Europe and elsewhere [7, 15–18, 27–29]. Therefore, more radiologists trained in multimodal cardiac imaging are required to help cover this demand. In this regard, the current study confirms and expands on the previous literature as follows: (i) the MRCT-registry is the largest available radiological database including more than 400,000 entries on CT and MRI examinations; (ii) The MRCT-registry is fed by the majority of European countries (total 29) and a few non-European countries; (iii) the MRCT-registry demonstrates a continuous increase in the number of performed cardiac CT and MRI examinations across Europe; (iv) the growth in the number of examinations was most pronounced for the evaluation of CAD with CT and for the evaluation of myocarditis with MRI, in line with current guidelines and recommendations; (v) both cardiac CT and MRI examinations, although many require the application of medication, are safe imaging procedures with very low rates for adverse events; and (vi) most submitted cardiac CT (76%) and MRI (71%) examinations were read exclusively by radiologists.
The growing demand for multimodality cardiac imaging expertise [30–32] not only poses significant challenges regarding the expected increasing workload, scanner capacity, and required trained personnel. It also implies the necessity for a centralized, well-defined pathway of access to cardiac CT and MR imaging services, managed by an independent, objective, and well-trained imaging professional, hereby balancing clinical question with available equipment and economic resources in an increasingly challenging healthcare landscape. The MRCT-registry, the largest of its kind, stands now as a testament to the prominent role that radiologists have assumed, not only in providing these necessary imaging services, but also in guiding their correct implementation in the patient’s best interest.
A crucial point to further note, as also shown in a previous sub-analysis of the MRCT-registry data, is that cardiac CT and MRI examinations have disseminated beyond academic centres to additionally include non-academic hospitals and private practices, increasing their accessibility to broader patient cohorts (for illustration, see Fig. 3) [21–23].
The observed rise in examinations most probably indicates appropriate referral, as indications for both CT and MR are firmly aligned with the most recent guidelines [7, 15, 16, 27–29]. CT angiography for patients with suspected CAD is primarily used in low and intermediate pretest scenarios [7]. Adherence to these recommendations is evident in the MRCT-registry analysing the data on CT-based assessment of CAD showing a continuous increase in patients at intermediate pretest probability. The rise in MRI-based assessment of suspected or known myocarditis is also well supported by current literature [33].
Finally, the MRCT data confirms that cardiac CT and MRI procedures, despite frequently necessitating cardiac medication, are safe examinations with only a minimal probability of adverse events. The reported very low adverse rates (0.3% for CT and 0.7% for MRI) are in line with previous literature [24] and randomized trials [34].
The presented data unequivocally reinforces the fundamental premise that radiologists, through their multimodality-based training with a profound understanding of indications, state-of-the-art technology, and imaging findings in and around the organ of interest, are in an ideal position to face future challenges and ensure the correct application and expansion of cardiac CT/MRI services. The European Society of Radiology (ESR) has, being fully aware of this responsibility, established a multilevel, standardized educational framework for imaging, as detailed in the European Training Curriculum (https://www.myesr.org/education/training-curricula/). This curriculum formally includes cardiac multimodality imaging as a core component of every radiology residency, ensuring that at the end of their training, all residents are equally competent to perform and interpret cardiac CT and MR examinations. It also ensures that radiologist not only adeptly manage modern and evolving imaging technologies, but, through their broad imaging training, also accurately diagnose incidental or concomitant diseases beyond cardiac pathology [35], providing as such a complete assessment of all available image data across different organ systems. This competency becomes increasingly important as the need for, e.g., cardiovascular CT imaging expands to emergency departments where the availability of around-the-clock services is essential to assess the various cardiac and non-cardiac differential diagnoses of acute chest pain [36]. Moreover, given that newer imaging technology with fast volume coverage further improves the depiction of the heart even in non-gated chest examinations hereby potentially improving risk stratification and diagnosis [37], it can be assumed that knowledge about cardiac imaging findings will become increasingly relevant for every radiologist in the near future.
While the general growth in medical imaging over the past decades yields unarguable benefits to patients in terms of longer and higher quality of life [38], part of the growth in imaging utilization could also be attributed to overutilization. Inadequate use of imaging resources is a well-known and multifactorial problem. Prior research has explored various factors contributing to overutilization, notably including payment structures, financial incentives, and self-referral, with the latter being particularly significant [39]. Self-referral is the act of a physician referring a patient to him- or herself for additional diagnostic or therapeutic procedures, which can result in financial profit. This poses a concern not just economically, but also in terms of increased exposure to ionizing radiation for both individuals and the general population [40]. Radiology, by definition, is a profession that works on referral from other medical disciplines and, as such, is not susceptible to self-referral. This eliminates conflicts of interests, allowing radiologists to collaboratively determine the most suitable imaging method with the referring physician, based on the patient’s specific clinical needs. This approach also underscores the role of radiologists as a gatekeeper for a correct value-based use of healthcare resources.
This study has the following limitations. First, the results of this study are based on registry data and may be susceptible to reporting bias. Second, no follow-up data regarding patient outcome or late-onset adverse events was available. Third, detailed information about the individual contributing centres in the MRCT-registry is missing. Thus, in-depth analyses on the reasons of increasing case submissions to the registry are not possible. Finally, some parameters which could be used to further analyse the use of cardiac CT and MRI are not recorded in the registry, such as the setting of the scan (outpatient, inpatient, emergency department).
In conclusion, real-life data on cardiac imaging in Europe using the MRCT-registry demonstrates a considerable increase in examinations over the past years, the vast majority of which are read by radiologists. Our results suggest that radiologists have an increasingly important role to provide cardiac CT and MR imaging services, contributing to expanding availability and expertise in both academic and non-academic centres. Radiology acts as a crucial barrier against the overutilization of medical imaging, ensuring correct application of different modalities according to current recommendations and guidelines.
Supplementary Information
Below is the link to the electronic supplementary material.
Abbreviations
- CAD
Coronary artery disease
- DRG
German Roentgen Society
- EBCR
European Board of Cardiovascular Radiology
- ESCR
European Society of Cardiovascular Radiology
- ESR
European Society of Radiology
- TAVR
Transcatheter aortic valve replacement
Funding
Open access funding provided by University of Zurich.
Declarations
Guarantor
The scientific guarantor of this publication is H. Alkadhi.
Conflict of interest
MF is the section editor for the scientific editorial board (cardiac) of European Radiology. LN is a member of the advisory editor board of European Radiology. HA is a deputy editor for European Radiology. They have not taken part in the review or selection process of this article. The remaining authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has statistical expertise.
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent requirement was waived.
Ethical approval
A local ethics committee approved the research protocol and waived the need for patient informed consent (Leipzig University; No. 131/17-ek).
Study subjects or cohorts overlap
Several earlier papers have been published using data from the MRCT-registry, such as Foldyna B et al (2022) Quality and safety of coronary computed tomography angiography at academic and non-academic sites: insights from a large European registry (ESCR MR/CT Registry). Eur Radiol 32:5246–5255, but with other patient populations from the registry and with other purposes.
Methodology
• retrospective
• registry data
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Federica Catapano and Lukas Jakob Moser are equal contributors.
References
- 1.Douglas PS, Hoffmann U, Patel MR et al (2015) Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med 372:1291–1300 10.1056/NEJMoa1415516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Group DT, Maurovich-Horvat P, Bosserdt M et al (2022) CT or invasive coronary angiography in stable chest pain. N Engl J Med 386:1591–1602 10.1056/NEJMoa2200963 [DOI] [PubMed] [Google Scholar]
- 3.Investigators S-H, Newby DE, Adamson PD et al (2018) Coronary CT angiography and 5-year risk of myocardial infarction. N Engl J Med 379:924–933 10.1056/NEJMoa1805971 [DOI] [PubMed] [Google Scholar]
- 4.Nagel E, Greenwood JP, McCann GP et al (2019) Magnetic resonance perfusion or fractional flow reserve in coronary disease. N Engl J Med 380:2418–2428 10.1056/NEJMoa1716734 [DOI] [PubMed] [Google Scholar]
- 5.Greenwood JP, Maredia N, Younger JF et al (2012) Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet 379:453–460 10.1016/S0140-6736(11)61335-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mezquita AJV, Biavati F, Falk V et al (2023) Clinical quantitative coronary artery stenosis and coronary atherosclerosis imaging: a Consensus Statement from the Quantitative Cardiovascular Imaging Study Group. Nat Rev Cardiol 20:696–714 10.1038/s41569-023-00880-4 [DOI] [PubMed] [Google Scholar]
- 7.Knuuti J, Wijns W, Saraste A et al (2020) 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 41:407–477 10.1093/eurheartj/ehz425 [DOI] [PubMed] [Google Scholar]
- 8.Francone M, Budde RPJ, Bremerich J et al (2020) CT and MR imaging prior to transcatheter aortic valve implantation: standardisation of scanning protocols, measurements and reporting-a consensus document by the European Society of Cardiovascular Radiology (ESCR). Eur Radiol 30:2627–2650 10.1007/s00330-019-06357-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ge Y, Gupta S, Fentanes E et al (2021) Role of cardiac CT in pre-procedure planning for transcatheter mitral valve replacement. JACC Cardiovasc Imaging 14:1571–1580 10.1016/j.jcmg.2020.12.018 [DOI] [PubMed] [Google Scholar]
- 10.Andreini D, Collet C, Leipsic J et al (2022) Pre-procedural planning of coronary revascularization by cardiac computed tomography: an expert consensus document of the Society of Cardiovascular Computed Tomography. EuroIntervention 18:e872–e887 10.4244/EIJ-E-22-00036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schwitter J, Wacker CM, Wilke N et al (2013) MR-IMPACT II: Magnetic Resonance Imaging for Myocardial Perfusion Assessment in Coronary artery disease Trial: perfusion-cardiac magnetic resonance vs. single-photon emission computed tomography for the detection of coronary artery disease: a comparative multicentre, multivendor trial. Eur Heart J 34:775–781 10.1093/eurheartj/ehs022 [DOI] [PubMed] [Google Scholar]
- 12.Arai AE, Schulz-Menger J, Shah DJ et al (2023) Stress perfusion cardiac magnetic resonance vs SPECT imaging for detection of coronary artery disease. J Am Coll Cardiol 82:1828–1838 10.1016/j.jacc.2023.08.046 [DOI] [PubMed] [Google Scholar]
- 13.McDonagh TA, Metra M, Adamo M et al (2021) 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 42:3599–3726 10.1093/eurheartj/ehab368 [DOI] [PubMed] [Google Scholar]
- 14.Baumgartner H, De Backer J, Babu-Narayan SV et al (2021) 2020 ESC Guidelines for the management of adult congenital heart disease. Eur Heart J 42:563–645 10.1093/eurheartj/ehaa554 [DOI] [PubMed] [Google Scholar]
- 15.Arbelo E, Protonotarios A, Gimeno JR et al (2023) 2023 ESC Guidelines for the management of cardiomyopathies. Eur Heart J 44:3503–3626 10.1093/eurheartj/ehad194 [DOI] [PubMed] [Google Scholar]
- 16.Esposito A, Gallone G, Palmisano A, Marchitelli L, Catapano F, Francone M (2020) The current landscape of imaging recommendations in cardiovascular clinical guidelines: toward an imaging-guided precision medicine. Radiol Med 125:1013–1023 10.1007/s11547-020-01286-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dreisbach JG, Nicol ED, Roobottom CA, Padley S, Roditi G (2018) Challenges in delivering computed tomography coronary angiography as the first-line test for stable chest pain. Heart (British Cardiac Society) 104:921–927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van den Boogert TPW, Claessen B, Boekholdt SM et al (2021) The impact and challenges of implementing CTCA according to the 2019 ESC guidelines on chronic coronary syndromes: a survey and projection of CTCA services in the Netherlands. Insights Imaging 12:186 10.1186/s13244-021-01122-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Natale L, Vliegenthart R, Salgado R et al (2023) Cardiac radiology in Europe: status and vision by the European Society of Cardiovascular Radiology (ESCR) and the European Society of Radiology (ESR). Eur Radiol 33:5489–5497 10.1007/s00330-023-09533-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gatti M, Liguori C, Muscogiuri G et al (2021) Challenges and opportunities to delivering cardiac imaging training: a national survey by the Italian college of cardiac radiology. Insights Imaging 12:136 10.1186/s13244-021-01076-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Langenbach MC, Sandstede J, Sieren MM et al (2023) German Radiological Society and the Professional Association of German Radiologists Position Paper on coronary computed tomography: clinical evidence and quality of patient care in chronic coronary syndrome. Rofo 195:115–134 10.1055/a-1973-9687 [DOI] [PubMed] [Google Scholar]
- 22.Sieren MM, Maintz D, Gutberlet M et al (2022) Current status of cardiovascular imaging in Germany: structured data from the National Certification Program, ESCR Registry, and Survey among Radiologists. Rofo 194:181–191 10.1055/a-1554-9236 [DOI] [PubMed] [Google Scholar]
- 23.Foldyna B, Uhlig J, Gohmann R et al (2022) Quality and safety of coronary computed tomography angiography at academic and non-academic sites: insights from a large European registry (ESCR MR/CT Registry). Eur Radiol 32:5246–5255 10.1007/s00330-022-08639-0 [DOI] [PubMed] [Google Scholar]
- 24.Uhlig J, Lucke C, Vliegenthart R et al (2019) Acute adverse events in cardiac MR imaging with gadolinium-based contrast agents: results from the European Society of Cardiovascular Radiology (ESCR) MRCT Registry in 72,839 patients. Eur Radiol 29:3686–3695 10.1007/s00330-019-06171-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Uhlig J, Al-Bourini O, Salgado R et al (2020) Gadolinium-based contrast agents for cardiac MRI: use of linear and macrocyclic agents with associated safety profile from 154 779 European patients. Radiol Cardiothorac Imaging 2:e200102 10.1148/ryct.2020200102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Taylor AJ, Cerqueira M, Hodgson JM et al (2010) ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol 56:1864–1894 10.1016/j.jacc.2010.07.005 [DOI] [PubMed] [Google Scholar]
- 27.Albus C, Barkhausen J, Fleck E, Haasenritter J, Lindner O, Silber S (2017) The diagnosis of chronic coronary heart disease. Dtsch Arztebl Int 114:712–719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cury RC, Leipsic J, Abbara S et al (2022) CAD-RADS 2.0 - 2022 Coronary Artery Disease-Reporting and Data System: an expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Cardiology (ACC), the American College of Radiology (ACR), and the North America Society of Cardiovascular Imaging (NASCI). JACC Cardiovasc Imaging 15:1974–2001 10.1016/j.jcmg.2022.07.002 [DOI] [PubMed] [Google Scholar]
- 29.Pontone G, Di Cesare E, Castelletti S et al (2021) Appropriate use criteria for cardiovascular magnetic resonance imaging (CMR): SIC-SIRM position paper part 1 (ischemic and congenital heart diseases, cardio-oncology, cardiac masses and heart transplant). Radiol Med 126:365–379 10.1007/s11547-020-01332-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weir-McCall JR, Williams MC, Shah ASV et al (2023) National trends in coronary artery disease imaging: associations with health care outcomes and costs. JACC Cardiovasc Imaging 16:659–671 10.1016/j.jcmg.2022.10.022 [DOI] [PubMed] [Google Scholar]
- 31.Reeves RA, Halpern EJ, Rao VM (2021) Cardiac imaging trends from 2010 to 2019 in the Medicare population. Radiol Cardiothorac Imaging 3:e210156 10.1148/ryct.2021210156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goldfarb JW, Weber J (2021) Trends in cardiovascular MRI and CT in the U.S. Medicare population from 2012 to 2017. Radiol Cardiothorac Imaging 3:e200112 10.1148/ryct.2021200112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Caobelli F, Cabrero JB, Galea N et al (2023) Cardiovascular magnetic resonance (CMR) and positron emission tomography (PET) imaging in the diagnosis and follow-up of patients with acute myocarditis and chronic inflammatory cardiomyopathy: a review paper with practical recommendations on behalf of the European Society of Cardiovascular Radiology (ESCR). Int J Cardiovasc Imaging 39:2221–2235 10.1007/s10554-023-02927-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schonenberger E, Martus P, Bosserdt M et al (2019) Kidney injury after intravenous versus intra-arterial contrast agent in patients suspected of having coronary artery disease: a randomized trial. Radiology 292:664–672 10.1148/radiol.2019182220 [DOI] [PubMed] [Google Scholar]
- 35.Williams MC, Hunter A, Shah ASV et al (2018) Impact of noncardiac findings in patients undergoing CT coronary angiography: a substudy of the Scottish computed tomography of the heart (SCOT-HEART) trial. Eur Radiol 28:2639–2646 10.1007/s00330-017-5181-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Loewe C, Beitzke D, Francone M (2023) How to set up a 24/7 cardiac computed tomography service in an emergency department. Eur Radiol 33:8177–8179 10.1007/s00330-023-09721-x [DOI] [PubMed] [Google Scholar]
- 37.Xia C, Vonder M, Sidorenkov G et al (2021) Cardiovascular risk factors and coronary calcification in a middle-aged Dutch population: the ImaLife study. J Thorac Imaging 36:174–180 10.1097/RTI.0000000000000566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hendrix W, Rutten M, Hendrix N et al (2023) Trends in the incidence of pulmonary nodules in chest computed tomography: 10-year results from two Dutch hospitals. Eur Radiol 33:8279–8288 10.1007/s00330-023-09826-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hendee WR, Becker GJ, Borgstede JP et al (2010) Addressing overutilization in medical imaging. Radiology 257:240–245 10.1148/radiol.10100063 [DOI] [PubMed] [Google Scholar]
- 40.Thrall JH (2012) Radiation exposure in CT scanning and risk: where are we? Radiology 264:325–328 10.1148/radiol.12121137 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.