Abstract
Background
Faecal incontinence is a particularly embarrassing and distressing condition with significant medical, social and economic implications. Anal sphincter exercises (pelvic floor muscle training) and biofeedback therapy have been used to treat the symptoms of people with faecal incontinence. However, standards of treatment are still lacking and the magnitude of alleged benefits has yet to be established.
Objectives
To determine the effects of biofeedback and/or anal sphincter exercises/pelvic floor muscle training for the treatment of faecal incontinence in adults.
Search methods
We searched the Cochrane Incontinence Group Specialised Trials Register (searched 24 January 2012) which contains trials from searching CENTRAL, MEDLINE and handsearching of conference proceedings; and the reference lists of relevant articles.
Selection criteria
All randomised or quasi‐randomised trials evaluating biofeedback and/or anal sphincter exercises in adults with faecal incontinence.
Data collection and analysis
Two review authors assessed the risk of bias of eligible trials and two review authors independently extracted data from the included trials. A wide range of outcome measures were considered.
Main results
Twenty one eligible studies were identified with a total of 1525 participants. About half of the trials had low risk of bias for randomisation and allocation concealment.
One small trial showed that biofeedback plus exercises was better than exercises alone (RR for failing to achieve full continence 0.70, 95% CI 0.52 to 0.94).
One small trial showed that adding biofeedback to electrical stimulation was better than electrical stimulation alone (RR for failing to achieve full continence 0.47, 95% CI 0.33 to 0.65).
The combined data of two trials showed that the number of people failing to achieve full continence was significantly lower when electrical stimulation was added to biofeedback compared against biofeedback alone (RR 0.60, 95% CI 0.46 to 0.78).
Sacral nerve stimulation was better than conservative management which included biofeedback and PFMT (at 12 months the incontinence episodes were significantly fewer with sacral nerve stimulation (MD 6.30, 95% CI 2.26 to 10.34).
There was not enough evidence as to whether there was a difference in outcome between any method of biofeedback or exercises. There are suggestions that rectal volume discrimination training improves continence more than sham training. Further conclusions are not warranted from the available data.
Authors' conclusions
The limited number of identified trials together with methodological weaknesses of many do not allow a definitive assessment of the role of anal sphincter exercises and biofeedback therapy in the management of people with faecal incontinence. We found some evidence that biofeedback and electrical stimulation may enhance the outcome of treatment compared to electrical stimulation alone or exercises alone. Exercises appear to be less effective than an implanted sacral nerve stimulator. While there is a suggestion that some elements of biofeedback therapy and sphincter exercises may have a therapeutic effect, this is not certain. Larger well‐designed trials are needed to enable safe conclusions.
Keywords: Adult; Female; Humans; Male; Anal Canal; Combined Modality Therapy; Combined Modality Therapy/methods; Electric Stimulation Therapy; Electric Stimulation Therapy/methods; Exercise Therapy; Exercise Therapy/methods; Fecal Incontinence; Fecal Incontinence/therapy; Feedback, Sensory; Feedback, Sensory/physiology; Pelvic Floor; Randomized Controlled Trials as Topic; Treatment Outcome
Plain language summary
Exercises of the muscles around the anus with or without biofeedback (aids for knowing when the muscles are contracting) for the treatment of faecal incontinence in adults
Faecal incontinence (inability to control bowel movements or leaking stool) can be a very embarrassing and socially restricting problem. There are many possible causes, including childbirth damage to the muscles which control bowel movements. Exercises to strengthen these muscles and 'biofeedback', where equipment is used to show people how to use the muscles properly, are often recommended. There was some evidence from trials suggesting that these treatments are helpful. If patients who have tried and failed other simpler treatments, such as changing their diet or using medications, are selected then biofeedback using computer equipment or rectal balloon is more beneficial than exercises alone. Exercises and electrical stimulation used in the anus may be more helpful than vaginal exercises for women with faecal incontinence after childbirth. About half of the 21 trials were at low risk of bias. They compared different combinations of treatments and different outcome measures, making comparison between them difficult. However, a small number of the larger recent trials provide better evidence.
Background
Description of the condition
Faecal incontinence has been variously defined. An international consensus meeting has recommended: "Faecal incontinence is the involuntary loss of liquid or solid stool that is a social or hygienic problem" (Norton 2009).
Faecal incontinence is a common healthcare problem, affecting 5% to 10% of community‐dwelling adults (Macmillan 2004; Perry 2002; Whitehead 2009), with 1% to 2% experiencing significant impact on daily activities (Perry 2002). It becomes more common with advancing age and disability (Potter 2002). It is a symptom which is particularly embarrassing and socially unacceptable, and many sufferers do not seek professional help (Johanson 1996). Faecal incontinence has a major negative impact on physical and psychological health and lifestyle (Boreham 2005; Cotterill 2011; Wilson 2007), with severe social restrictions in many instances (Rockwood 1999; Rockwood 2000).
Faecal incontinence has many possible causes, including (among others) obstetric or other trauma, or a congenital abnormality of one or both of the anal sphincters or the pelvic floor muscles; loose stool or intestinal hurry; neurological disease or injury causing sensory or motor impairment to the continence mechanism; local anorectal pathology; rectal loading and subsequent 'overflow' leakage in frail or immobile individuals; and physical or mental disabilities affecting toilet habits. For many people, a combination of structural, physiological and psycho‐social factors (Norton 2004; Rao 2004; Tuteja 2004) combine to cause faecal incontinence.
It is generally recognised that symptoms may be of urgency with urge faecal incontinence, usually consequent upon external striated voluntary sphincter weakness or disruption, or loose stool or intestinal hurry; or of passive soiling in the absence of an urge to defecate, secondary to smooth muscle internal anal sphincter dysfunction, local pathology or incomplete evacuation. Recent advances in investigation techniques (notably ano‐rectal physiology studies and endo‐anal ultrasound) allow more accurate characterisation of the underlying cause for each patient. However, for many conditions the treatment options are limited, relying mainly on surgery and constipating drugs (Madoff 2009; Norton 2009; Whitehead 2001).
Description of the intervention and how it might work
Pelvic floor muscle training (PFMT) is a well‐established therapy for the treatment of urinary incontinence (Dumoulin 2010), but has been less commonly reported for faecal incontinence. The external anal sphincter is continuous with the puborectalis muscle and, as a striated muscle, is theoretically amenable to the same re‐educative and training techniques. The role of the ano‐rectal angle, maintained by the pubo‐rectalis muscle, is controversial but is believed to be important in faecal continence. It is not established whether pelvic floor muscle training can be distinguished from anal sphincter exercises in practice by patients, and the two will be considered together for the purposes of this review, with the use of vaginal or anal palpation, teaching, or biofeedback made explicit. The purpose of the exercises is stated variously as enhancing the strength, speed, or endurance of voluntary anal sphincter contraction. Some have also suggested that there could be an effect on resting closure pressure of the anus. Reported exercise regimens for faecal incontinence vary widely in terms of the type, number and intensity of exercises taught (for example maximal squeeze and how long to attempt to hold it; submaximal endurance squeeze; fast twitch squeezes), how many per day and in what pattern, and in length of time the exercises are suggested to be performed for. Some have reported a single regimen for all patients (for example 10 squeezes of 5 seconds each five times per day); others have individualised the exercise programme, depending on the initial muscle strength and endurance, on the principle of improving muscle performance by 'overload' (aiming to exercise at a level just above current ability). There is no consensus among professionals on the best exercise regimen for faecal incontinence.
Biofeedback uses equipment to record or amplify and then feed back to the patient activities of the body. Originally based on the principles of operant conditioning (Engel 1974), it is a very commonly reported clinical treatment for faecal incontinence in the colorectal and gastroenterology literature. Reviews of large numbers of case series, in the era before randomised controlled trials became the accepted method for evaluating the efficacy of treatment, have concluded that biofeedback is an effective treatment for the majority of people with faecal incontinence (Heymen 2001: Norton 2001). Many different therapies have been used with people with faecal incontinence under the label of 'biofeedback'. Early studies concentrated on operant conditioning to enhance what was presumed to be a reflex contraction of the external anal sphincter in response to the reflex inhibition of the internal anal sphincter when the rectum filled (recto‐anal inhibitory reflex). It has subsequently been suggested that this external sphincter reaction is in fact not a reflex but a voluntary response (Whitehead 1981). Other studies have focused on teaching the patient to discriminate progressively smaller volumes of distension of a rectal balloon, and to respond appropriately (by contracting the external sphincter) and as promptly as possible, abolishing any delay in sensation or reaction to it. Some have disregarded these elements and focused entirely on improving the strength or endurance of external anal sphincter contraction.
Three main modalities have been described
1. Rectal sensitivity training. A rectal balloon is gradually distended with air or water and the patient is asked to report the first sensation of rectal filling. Once this threshold volume is determined, repeated re‐inflations of the balloon are performed with the objective being to teach the patient to feel the distension at progressively lower volumes. The rationale is that some patients are found to have high threshold volumes and if the patient detects stool arriving sooner there is more possibility to either find a toilet or use an anal squeeze, or both. Conversely, the same technique can also be used to teach the patient to tolerate progressively larger volumes, in those with urgency and a hypersensitive rectum.
2. Strength training. Biofeedback techniques have been used to demonstrate to the patient anal sphincter pressures or activity, thereby enabling teaching of anal sphincter exercises and giving feedback on performance and progress. This can be achieved by using electromyography (EMG) skin electrodes, manometric pressures, intra‐anal EMG, or anal ultrasound. The patient is encouraged by seeing or hearing the signal to enhance squeeze strength and endurance. There is no consensus on an optimum exercise regimen for use at home between sessions, nor on the number of squeezes, the frequency of exercises or treatment duration, with different authors describing very different programmes.
3. Co‐ordination training. Some authors have described a three‐balloon system for biofeedback for faecal incontinence. One distension balloon is situated in the rectum, the second and third smaller pressure‐recording balloons are situated in the upper and lower anal canal. Rectal distension triggers the rectal‐anal inhibitory reflex. This momentary anal relaxation is a point of vulnerability for people with faecal incontinence and incontinence can occur at this time. By distending the rectal balloon and showing the patient this consequent pressure drop, the aim is to teach the patient to counteract this by a voluntary anal squeeze that is hard enough and for long enough for resting pressure to return to its baseline level.
The three methods are not mutually exclusive, and many protocols combine two or three elements together. There has been considerable variation in protocols, such as the number or frequency of sessions, intensity and duration of exercises and instructions for practice at home. Some studies have included other elements, such as patient teaching, diet and fluid advice and titration of medication, although many fail to mention these other elements or give details. Some have used additional surface electrode electrical stimulation of the anal sphincter muscles, which is the subject of a separate Cochrane review (Hosker 2007). There is widespread agreement on the crucial role of patient motivation and the patient‐therapist interaction.
Why it is important to do this review
There are numerous case series reporting on biofeedback for faecal incontinence, nearly all of which have reported positive results (Heymen 2001; Norton 2001). Only one published study has reported negative results (van Tets 1996). It would be easy to conclude from case series that biofeedback or exercises are an effective intervention. However, it is known that there is a publication bias in favour of publishing positive results and that there is an effect of intervention per se, especially in many functional gastrointestinal disorders (Thompson 1999). Delivering a programme of biofeedback or anal sphincter exercises, or both, inevitably involves a complex combination of patient‐therapist interaction, patient education and formal or informal advice on a range of related issues. Randomised controlled trials provide the best evidence of the efficacy of health care interventions. More complex interventions are likely to involve more clinic attendances for the patients and more costs. Patients who fail to respond to conservative treatments are often referred for costly surgical treatments such as sacral nerve stimulation. If they have not tried the most effective available conservative interventions, they may undergo surgery unnecessarily or alternatively decide to live with distressing symptoms which might have responded to the best available treatment.
The aim of the present review is to systematically search for and combine evidence from all relevant randomised controlled trials on the effects of biofeedback or sphincter exercises, or both, for the treatment of faecal incontinence in order to provide the best evidence currently available on which to base recommendations for clinical practice and for future research.
Objectives
To determine the effectiveness of anal sphincter exercises/pelvic floor muscle training (PFMT) with or without biofeedback in the treatment of the symptoms of faecal incontinence in adults. The following comparisons were considered:
1. Anal sphincter exercises/PFMT with or without biofeedback versus no treatment
2. Anal sphincter exercises/PFMT with or without biofeedback versus any other treatment alone
3. Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone
4. Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus exercises with or without biofeedback
5. Anal sphincter exercises/PFMT and biofeedback versus anal sphincter exercises/PFMT alone
6. One type of biofeedback versus another type of biofeedback
7. One type of anal sphincter exercises/PFMT versus another type of anal sphincter exercises/ PFMT
Methods
Criteria for considering studies for this review
Types of studies
All randomised or quasi‐randomised controlled trials of patients with faecal incontinence receiving anal sphincter exercises or biofeedback, or both as treatment.
Types of participants
Adults (18 years and older or as defined by the trialists) suffering from faecal incontinence.
Types of interventions
Anal sphincter exercises and/or biofeedback. Under the term 'anal sphincter exercises' we included: anal sphincter exercises, 'Kegel exercises' (Kegel 1948), pelvic floor exercises, or pelvic floor muscle training.
All types of visual, sensory (usually with a rectal balloon) or auditory biofeedback were considered. As the specific techniques used for biofeedback might have differed among studies, a clear description of the modality used was made explicit in each instance (see table 'Characteristics of included studies').
Types of outcome measures
1. Patient symptoms
Incontinence status Frequency of incontinence Number of pads changes Incontinence score. Occurrence of adverse events
Diary
2. Patient satisfaction with outcome
Self‐report
3. Ano‐rectal physiology measurements
Resting anal pressure (pressure or EMG) Pressure rise and squeeze increment on voluntary contraction (pressure or EMG) Duration of pressure rise on voluntary contraction (pressure or EMG) Vector Symmetry Index Rectal sensation assessment (by balloon distention or electrical means, or both)
4. Health status measures
Psychological health measures (e.g. Hospital Anxiety and Depression Scale, HADS) (Zigmond 1983)
Health‐related quality of life measures (e.g. Short Form‐36) (Ware 1993) or condition‐specific measures
Activities of daily living measures (e.g. Barthel activities of daily living (ADL) Index) (Wade 1988)
5. Health economics
Costs of interventions Resource implications Cost effectiveness or cost utility evaluation (e.g. cost per QALY) (Weinstein 1977)
6. Other outcomes
Other outcome measures given by authors and judged to be important when undertaking the review
Search methods for identification of studies
We did not impose any language or other limits on any of the searches.
Electronic searches
This review has drawn on the search strategy developed by the Cochrane Incontinence Group. Relevant trials were identified from the Incontinence Group Specialised Trials Register, which is described under the Incontinence Group's module in The Cochrane Library. The register contains trials identified from MEDLINE, CINAHL, the Cochrane Central Register of Controlled Trials (CENTRAL) and handsearching of journals and conference proceedings. The date of the most recent search of the register was 24 January 2012.
The trials in the Incontinence Group Specialised Trials Register are also contained in CENTRAL. The Incontinence Group Trials Register was searched using the Group's own keyword system. The search terms used were:
({design.rct* or design.cct*}) AND ({TOPIC.FAECAL.INCON* or TOPIC.FAECAL.NEUROGENIC*}) AND ({INTVENT.PHYS.PFMT* or INTVENT.PHYS.BIOFEED* or INTVENT.PHYS.SphincterExercise* or INTVENT.PHYS.exercise*}) (All searches were of the keyword field of Reference Manager 12, ISI ResearchSoft).
Searching other resources
We checked all reference lists of identified trials.
Data collection and analysis
Trials selection
Two review authors (CN, JC) examined all the citations and abstracts derived from the electronic search strategy. Reports of potentially relevant trials were retrieved in full. Both review authors independently applied the selection criteria to trials reports. They were not blind to the names of trials' authors, institutions or journals. Any disagreements were resolved by discussion.
Risk of bias
The risk of bias of identified trials was assessed independently by the two review authors using the Cochrane Collaboration 'Risk of bias' tool (Higgins 2011a). This takes into account the quality of random sequence generation, allocation concealment, the description of dropouts and withdrawals, whether data were analysed on an intention‐to‐treat basis, and whether therapists, participants or outcome assessors were blind to the treatments provided.
Where the method of allocation concealment was not clearly reported the authors were contacted, if possible, for clarification.
Any disagreements were resolved by discussion. Studies were excluded if they not meet the pre‐specified inclusion criteria. The list of excluded studies and the reasons for their exclusion are summarised in the table 'Characteristics of excluded studies'.
Data extraction
Data extraction from the included studies was undertaken independently by the review authors. Only published data have been used for the purposes of this review. Data were processed as described in the Cochrane Collaboration Handbook (Higgins 2011b). Any difference of opinion was resolved by discussion.
Missing information was sought from trialists, if necessary.
Analysis
Data were analysed using Review Manager (RevMan) software.
For each trial, risk ratios and 95% confidence intervals were calculated for dichotomous outcomes using a fixed‐effect model. Continuous variables were processed using mean and standard deviation values. Where the results were reported in terms of the mean and standard error of the mean (SEM), the standard deviation (SD) was calculated using the standard statistical equation: SD = SEM x square root (sample size). Differences between groups were presented as weighted mean differences (WMD) with accompanying 95% confidence intervals.
All outcomes were reported in terms of unfavourable events. This implied that risk ratios less than one or a WMD less than zero indicated a reduction in unfavourable events (that is a beneficial treatment effect). Therefore, the benefits of the experimental treatment were all displayed on the same side of the line of no effect.
Results
Description of studies
Results of the search
Three hundred and ten possible studies were identified by the search of which 21 are included in the review. The flow of literature through the assessment process is shown in the PRISMA flowchart (Figure 1).
1.
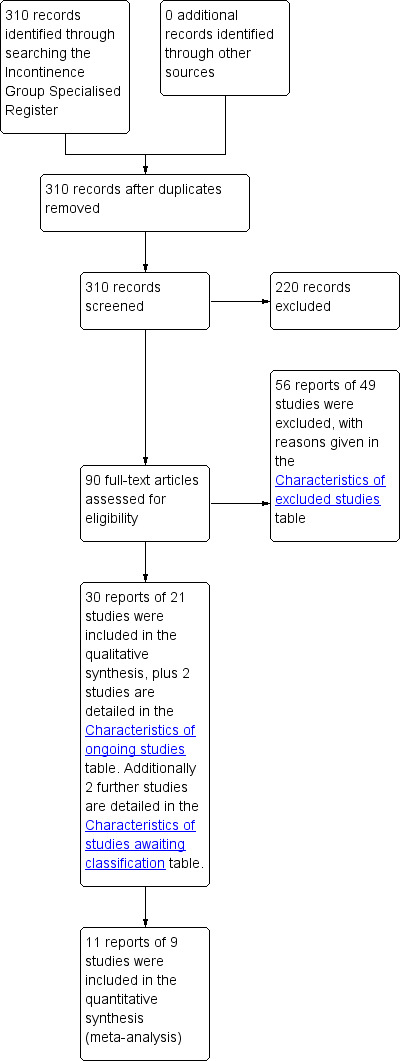
PRISMA study flow diagram.
Included studies
Twenty one studies are included in this review ( Bartlett 2011; Bols 2011; Davis 2004; Fynes 1999; Healy 2006; Heymen 2000; Heymen 2009; Hinninghofen 2003; Ilnyckyj 2005; Latimer 1984; Mahony 2004; Markwell 2006; McHugh 1986; Miner 1990; Naimy 2007; Norton 2003; Schwandner 2010; Schwandner 2011; Solomon 2003; Tjandra 2008; Whitehead 1985). A total of 1525 participants were randomised.
Further details can be found in the Table of Characteristics of included studies.
Design
One study (Whitehead 1985) allocated alternate patients to exercises or a control group.
Seventeen studies prospectively randomised patients to one of two (Bartlett 2011; Bols 2011; Davis 2004; Fynes 1999; Healy 2006; Heymen 2009; Ilnyckyj 2005; Mahony 2004; Markwell 2006; Naimy 2007; Schwandner 2010; Schwandner 2011; Tjandra 2008), three (Hinninghofen 2003; Solomon 2003) or four groups (Heymen 2000; Norton 2003).
Two trials (Latimer 1984; Miner 1990) which attempted to evaluate different components of biofeedback therapy had a complex design. One trial (Latimer 1984) reported the results of single case experiments employed with eight incontinent patients randomly allocated to different components of biofeedback (A, B, C or D). The single case designs were A B A C A D A or A C A B A D A. For each patient, results of the pre‐treatment phase were compared to those of the last follow‐up. Results at the end of each treatment phase were either not reported or provided in a form unsuitable for statistical analyses, rendering the interpretation of trial findings difficult. The other trial (Miner 1990), which investigated some of the factors thought to be responsible for the improvement of patients undergoing biofeedback therapy, was a 'two‐phase randomised trial'. Patients were initially randomised to one of two groups for sensory retraining (phase II); before and after treatment results were reported for both intervention groups. At the end of phase I all patients were again randomly assigned to one of two groups for either strength or coordination training. After a month they were crossed over. Results of the cross‐over phases were not clearly reported. Only results of the final assessment were given for phase II.
One trial randomised patients to two groups using a cross‐over design (McHugh 1986).
Sample sizes
The sample sizes of included trials ranged from eight (Latimer 1984) to 171 (Norton 2003) participants.
Setting
Each of the trials, except two (Schwandner 2010; Schwandner 2011), were carried out in a single hospital centre; these were in a variety of countries. Schwandner 2010 was a multi centre trial which involved eight centres in Germany (Schwandner 2010).
Participants
In all studies where information on gender was reported, the majority of participants were female. Most studies enrolled patients with mixed aetiologies. Four studies included women with obstetric trauma only (Davis 2004; Fynes 1999; Mahony 2004; Naimy 2007). One study included older patients only (Whitehead 1985). One study included only patients undergoing surgical anal sphincter repair (Davis 2004). Some investigators only included patients who had failed previous dietary and medication interventions (Bols 2011; Heymen 2009). In some studies patients with specific diagnoses such as rectal prolapse were excluded, inflammatory bowel disease, and irritable bowel syndrome (see table 'Characteristics of included studies' for details of the inclusion and exclusion criteria in each study).
Interventions
One study used a dual‐balloon system with visual or auditory feedback of anal pressure. Patients were encouraged to contract the anal sphincter in response to rectal distension. Exercises during the session (one hour per week for six weeks, commenced three months following anal sphincter repair surgery) and home practice included maximal, submaximal and fast‐twitch contractions practised at least twice daily. The control group had no therapist contact, biofeedback or exercises (Davis 2004). Another study compared rectal balloon therapy with PFMT against PFMT alone (Bols 2011).
Two other studies included a no biofeedback or exercises group. In one of these studies the control group received one‐to‐one time and advice (Norton 2003); in the other study the control group received no intervention (Whitehead 1985). Three studies included a no‐biofeedback exercise group which involved exercises taught digitally (Norton 2003; Solomon 2003) or verbally (Ilnyckyj 2005).
Heyman 2009 compared manometric biofeedback and pelvic floor exercises against exercises alone.
Bartlett compared a standard clinical protocol (sustained submaximal anal and pelvic floor exercises versus an alternative group (rapid squeeze plus sustained submaximal exercises) with biofeedback in both arms of the study. There were five outpatient sessions over eight weeks. The first four sessions were weekly; participants then practised techniques for four weeks before returning for their final session (Bartlett 2011).
Markwell (Markwell 2006) compared dietary modification, stool bulking agents, specific pelvic floor muscle action using abdominal muscles and defecation training compared with dietary modification, stool bulking agents and conventional pelvic floor exercises.
Tjandra (Tjandra 2008) compared optimum medical therapy, including pelvic floor exercises, bulking agents, dietary management of fluid and fibres, with a team of physiotherapists and dietitians. Attendance varied with need, usually monthly for six months then two‐monthly. This group was compared against two phase sacral nerve stimulation: peripheral nerve evaluation for at least seven days; patients with a 50% reduction or more in incontinence episodes were surgically implanted with a permanent sacral nerve stimulator.
Two studies compared biofeedback and exercises against biofeedback, exercises and electrical stimulation (Fynes 1999; Mahony 2004). The Fynes study (Fynes 1999) randomised women with post‐natal faecal incontinence to either vaginal pressure non‐computer biofeedback (Peritron) with a nurse (weekly 30 minute sessions for 12 weeks) with fast and slow twitch exercises, or to computer‐assisted anal probe EMG biofeedback (fast and slow twitch exercises) with a physiotherapist plus anal electrical stimulation at 20 Hz and 50 Hz. The Mahoney study (Mahony 2004) likewise recruited women with post‐natal incontinence, randomised to have anal EMG biofeedback to perform fast and slow twitch contractions (10 minutes), with or without additional anal electrical stimulation at 35 Hz (20 minutes) at weekly sessions for 12 weeks. The Mahony study randomised women to intra‐anal EMG biofeedback with or without anal electrical stimulation.
Schwandner 2010 (Schwandner 2010) compared "Triple target training" where amplitude‐modulated middle‐frequency electrical stimulation was combined with electromyography biofeedback and compared against electromyography biofeedback carried out at home daily for 20 minutes for a duration of nine months.
Schwandner 2011 (Schwandner 2011) compared "Triple target training" where amplitude‐modulated middle‐frequency electrical stimulation was combined with electromyography biofeedback and compared against low frequency electrostimulation.
Healy (Healy 2006) compared endo‐anal pudendal nerve stimulation daily at home against attending a physiotherapy department for endo‐anal electrical stimulation under supervision. They alternated biofeedback and electrical stimulation using augmented biofeedback.
Hinninghofen (Hinninghofen 2003) included three different groups, sphincter training compared with electrical stimulation, sphincter training with biofeedback and pelvic floor training without support; the intervention lasted three months.
Naimy (Naimy 2007) compared biofeedback with electrical stimulation. Biofeedback consisted of Neuro Trac ETS: using an Anuform anal probe. Quick 3 second squeeze; 10 second squeeze; squeeze for as long as it kept 50% of 3 second amplitude. Each squeeze was repeated five times with equal rest time between. The initial session was for 30 minutes with a 30 minute follow‐up session one week later; then daily 30 minute sessions at home for eight weeks. Electrical stimulation consisted of Neuro Trac ETS: 30 or 40 Hz at alternate sessions; pulse width 200 µsec; upper limit 80 mAmp using Anuform anal probe. Patients turned up the stimulation to the maximum voltage which caused no discomfort: 3 seconds on then 3 seconds rest for 20 minutes twice daily at home. The initial session was 30 minutes with a 30 minute follow‐up session one week later. Both interventions were carried out two times daily for eight weeks.
Four studies compared different methods of delivering biofeedback (Heymen 2000; McHugh 1986; Norton 2003; Solomon 2003). Heymen randomised patients to one of four groups: 1. anal EMG biofeedback plus home exercise; 2. anal EMG biofeedback plus rectal balloon distension sensory training to perceive lower rectal volumes and hold larger rectal volumes; 3. anal EMG biofeedback plus home exercise using a home biofeedback machine; 4. anal EMG biofeedback plus rectal balloon distension sensory training plus home exercise using a home biofeedback machine.
Norton (Norton 2003) randomised patients to one of four groups (all monthly 45 to 60 minute sessions for up to six sessions): 1. education, advice, urge resistance training, medication titration, diet and fluid adjustment (no biofeedback or exercise); 2. as 1, plus anal sphincter exercises taught by digital examination and a leaflet, with instruction to practise maximal, submaximal and fast‐twitch exercises 10 times daily at home; 3. as 2. plus computer‐assisted anal sphincter pressure biofeedback at each session; 4. as 3. plus a home anal EMG biofeedback machine for home practice.
Solomon (Solomon 2003) randomised patients to exercises taught digitally, via anal ultrasound biofeedback or via anal manometry biofeedback (five 30 minute sessions over four months).
One study compared clinic biofeedback with a home biofeedback device (McHugh 1986).
The design of the remaining two trials (Latimer 1984; Miner 1990), which attempted to evaluate different components of biofeedback therapy, have been described above.
Outcomes
Trials included a variety of outcome measures, many of which have not been validated.
Five trials reported patient evaluation of the outcome as a primary outcome measure (Bols 2011; Davis 2004; Naimy 2007; Norton 2003; Solomon 2003).
Eight studies used a patient‐completed diary. One study took no episodes of faecal incontinence in a one week diary at the end of treatment as a 'complete response' (Ilnyckyj 2005).
Nine studies reported results of a variety of continence scores.
Eleven trials reported quality of life evaluation (Bartlett 2011; Bols 2011; Davis 2004; Healy 2006; Heymen 2009; Hinninghofen 2003; Mahony 2004; Naimy 2007; Norton 2003; Schwandner 2010; Tjandra 2008). One study used the SF‐36 tool (Norton 2003).
Eight trials reported changes in manometric data as a proxy for patient outcome.
No attempts were made to include economic data in any trial.
See the Characteristics of included studies table for details of outcome measures used in each study.
Excluded studies
Of the excluded studies, some included children only, others were not randomised controlled trials (RCTs) or did not include the target interventions. Two were abstract reports of subsequently published full papers. See the table 'Characteristics of excluded studies' for details.
Risk of bias in included studies
Allocation
Thirteen trials (Bartlett 2011; Bols 2011; Davis 2004; Fynes 1999; Heymen 2000; Heymen 2009; Mahony 2004; Markwell 2006; Naimy 2007; Norton 2003; Schwandner 2010; Schwandner 2011; Solomon 2003) were judged to be at low risk of bias for random sequence generation, where an independent method such as a computer‐generated list was used to produce the allocation of groups.
The quality of allocation concealment was judged to be adequate in 10 trials (Bartlett 2011; Bols 2011; Heymen 2009; Mahony 2004; Markwell 2006; Norton 2003; Schwandner 2010; Schwandner 2011; Solomon 2003; Tjandra 2008), unclear in 10 trials (Davis 2004; Fynes 1999; Healy 2006; Heymen 2000; Hinninghofen 2003; Ilnyckyj 2005; Latimer 1984; McHugh 1986; Miner 1990; Naimy 2007) and inadequate in one trial (Whitehead 1985). Most of the 'unclear' allocations mentioned computer‐generated random numbers but did not explicitly state that allocation was concealed.
Blinding
In the Bartlett trial (Bartlett 2011) participants were blinded. Markwell (Markwell 2006) was described as 'single blind study' but information on who was actually blinded was not clearly reported.
In four trials (Bols 2011; Fynes 1999; Schwandner 2011; Solomon 2003) the outcome assessor was blind to patients' treatment protocol; in two trials outcome assessors were blinded for some of the outcomes (Norton 2003; Schwandner 2010).
In Heyman 2009 (Heymen 2009) the therapist telephoned to ask if participants had experienced 'adequate relief', which could be considered a violation of the trial protocol.
Incomplete outcome data
Most studies reported overall withdrawals with no indication of which groups patients were originally enrolled. Five trials (Bols 2011; Heymen 2009; Latimer 1984; Norton 2003; Schwandner 2010) that analysed data on an intention‐to‐treat basis and (Fynes 1999) had no or comparable drop outs from each group, were considered to be at low risk of bias.
In two trials (Latimer 1984; Miner 1990) data of the cross‐over phases were not reported separately and it was not possible to analyse them as parallel group data.
Effects of interventions
Twenty one trials with a total of 1525 participants were included in this review.
Only nine trials (Davis 2004; Fynes 1999; Healy 2006; Heymen 2009; Miner 1990; Naimy 2007; Schwandner 2010; Schwandner 2011; Tjandra 2008) provided data in a form suitable for statistical analyses in RevMan.
Follow‐up
Most studies reported results at the end of treatment or within a few weeks of completion only. Two studies reported results nine months after starting biofeedback (Davis 2004; Schwandner 2010) and five studies reported results one year after completing treatment (Bartlett 2011; Markwell 2006; Miner 1990; Norton 2003; Tjandra 2008).
1. Anal sphincter exercises/PFMT with or without biofeedback versus no treatment
One small cross‐over trial with 25 participants was found (Miner 1990). Data suitable to be analysed were presented for the first phase of the trial only. In the experimental group active sensory retraining was employed to teach the patient to discriminate progressively smaller volumes of rectal balloon distension with decreasing delay. Controls received the same procedure but with no feedback on performance. Miner reported that sensory biofeedback produced better results than strength training alone. There was a significant difference between groups in incontinence episodes per week (MD ‐1.40, 95% CI ‐1.51 to ‐1.29) (Analysis 1.3) and rectal sensory threshold (WMD ‐12.90, 95% CI ‐14.10 to ‐11.70) (Analysis 1.8) favouring treatment. However, there was no statistically significant result for people failing to achieve full continence (RR 0.71, 95% CI 0.48 to 1.03) (Analysis 1.1) or no improvement in incontinence status (RR 0.26, 95% CI 0.07 to 1.03) (Analysis 1.2). Controls were said to achieve similar benefits when crossed over to active training but these data were not given.
1.3. Analysis.
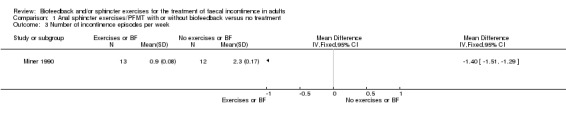
Comparison 1 Anal sphincter exercises/PFMT with or without biofeedback versus no treatment, Outcome 3 Number of incontinence episodes per week.
1.8. Analysis.
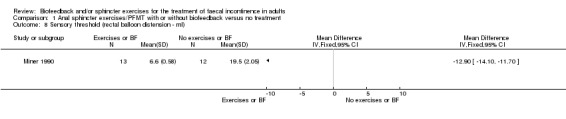
Comparison 1 Anal sphincter exercises/PFMT with or without biofeedback versus no treatment, Outcome 8 Sensory threshold (rectal balloon distension ‐ ml).
1.1. Analysis.
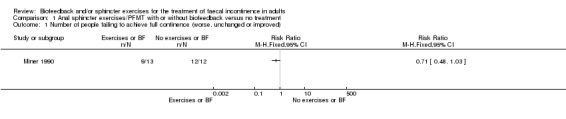
Comparison 1 Anal sphincter exercises/PFMT with or without biofeedback versus no treatment, Outcome 1 Number of people failing to achieve full continence (worse, unchanged or improved).
1.2. Analysis.
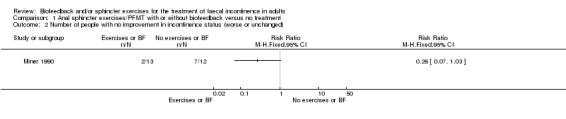
Comparison 1 Anal sphincter exercises/PFMT with or without biofeedback versus no treatment, Outcome 2 Number of people with no improvement in incontinence status (worse or unchanged).
2. Anal sphincter exercises/PFMT with or without biofeedback versus any other treatment alone
Biofeedback versus electrical stimulation
One trial (Naimy 2007) compared biofeedback with electrical stimulation alone, with no mention of exercises between treatments in either group. There was no statistically significant difference for numbers of people dissatisfied with treatment although the confidence interval was wide (Analysis 2.7).
2.7. Analysis.

Comparison 2 Anal sphincter exercises/PFMT with or without biofeedback versus any other treatment alone, Outcome 7 Number of people dissatisfied with the treatment.
3. Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone
Seven trials were found (Davis 2004; Healy 2006; Ilnyckyj 2005; Norton 2003; Schwandner 2011; Tjandra 2008; Whitehead 1985).
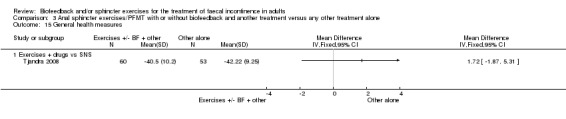
Exercises plus medical therapy versus sacral nerve stimulation
Tjandra compared optimal medical therapy, which consisted of pelvic floor exercises (biofeedback provided with digital guidance), bulking agents, dietary management of fluid and fibres versus two phase sacral nerve stimulation (peripheral nerve evaluation for at least 7 days; patients with a 50% reduction or more in incontinence episodes were implanted with a permanent sacral nerve stimulator). At 12 months the number of incontinence episodes per week was significantly lower in the sacral nerve stimulation group (MD 6.30, 95% CI 2.26 to 10.34) (Analysis 3.4). However the difference in the number of pad changes per week was not statistically significant (Analysis 3.5). Both the Incontinence score and condition‐specific quality of life (fecal incontinence quality of life index, FIQL) showed a statistically significant result favouring sacral nerve stimulation (MD 12.90, 95% CI 12.22 to 13.58, Analysis 3.6; MD 1.00, 95% CI 0.70 to 1.30, Analysis 3.16, respectively).
3.4. Analysis.

Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 4 Number of incontinence episodes per week.
3.5. Analysis.
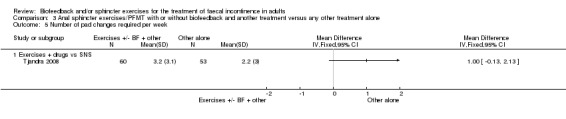
Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 5 Number of pad changes required per week.
3.6. Analysis.
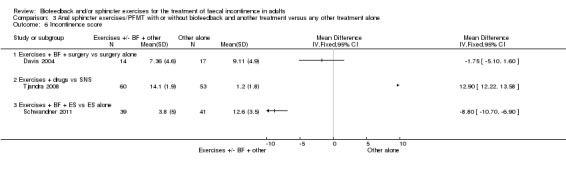
Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 6 Incontinence score.
3.16. Analysis.
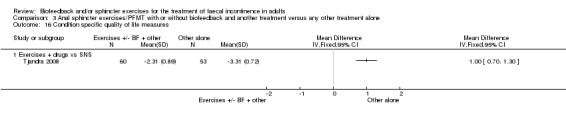
Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 16 Condition specific quality of life measures.
Exercises plus biofeedback plus surgery versus surgery alone
Davis (Davis 2004) compared anal sphincter repair with or without subsequent biofeedback commenced three months post‐operatively in 38 women with obstetric‐related anal sphincter injuries. There was no difference between the groups as regards continence score at nine months (Analysis 3.6) or patient satisfaction measured by visual analogue score (Analysis 3.19). Davis (Davis 2004) used a validated faecal incontinence quality of life questionnaire at nine months and there were no statistically significant differences between the groups in mean score changes for lifestyle, depression and embarrassment measurements.
3.19. Analysis.
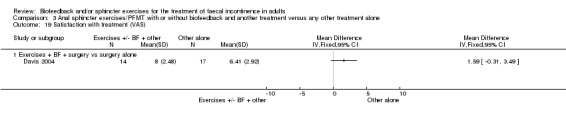
Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 19 Satisfaction with treatment (VAS).
Exercises plus biofeedback plus electrical stimulation versus electrical stimulation alone
Schwandner (Schwandner 2011) compared medium frequency electrical stimulation and electromyographic (EMG) biofeedback (known as triple target treatment) versus low frequency electrostimulation. electrostimulation. The number of people who failed to achieve full continence was significantly lower in the triple target group (RR 0.47, 95% CI 0.33 to 0.65, Analysis 3.1). The Wexner incontinence score was statistically significant favouring triple target training (MD ‐8.80, 95% CI ‐10.70 to ‐6.90) (Analysis 3.6).
3.1. Analysis.
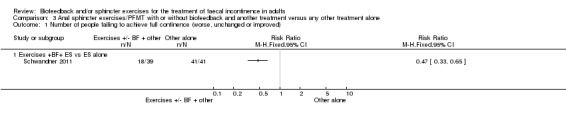
Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 1 Number of people failing to achieve full continence (worse, unchanged or improved).
Healy (Healy 2006) compared endo‐anal pudendal nerve electrical stimulation daily at home versus endo‐anal electrical stimulation plus augmented biofeedback under supervision and reported that low frequency endo‐anal electrical stimulation significantly improves continence scores and quality of life. The data could not be analysed in RevMan.
Exercises plus biofeedback plus education versus exercises plus education
Ilnyckyj (Ilnyckyj 2005) compared anal sphincter exercises plus biofeedback plus education versus exercises and education in 23 women, the data were not suitable for further analyses in RevMan as no measures of variance were reported. Ilnyckyj reported that resting and squeeze manometric pressures were not significantly different between the groups, but there was a trend in favour of biofeedback. Squeeze duration was better in the biofeedback group (P = 0.019). On the outcome measure of no incontinence in a one week diary, 86% (six out of seven) of biofeedback patients and 45% (five of 11) of education without biofeedback participants were "complete responders" (Analysis 3.20).
3.20. Analysis.
Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 20 Manometric pressures (medians).
| Manometric pressures (medians) | |||||
|---|---|---|---|---|---|
| Study | Resting pressure | Squeeze pressure | Fatigue time | ||
| Exercises + BF + education vs exercises + education | |||||
| Ilnyckyj 2005 | Education plus = 51.6 (mm [H2O]) Control (education) = 34.1 (mm [H2O]) | Education plus BF = 91.7 (mm [H2O]) Control = 81.3 (mm [H2O]) | Treatment = 19.4 Control = 14.0 | ||
Norton (Norton 2003) compared education and advice, with or without exercises, with or without biofeedback (clinic and home or clinic alone) in 171 patients. No significant differences between the groups were reported on manometric parameters, continence scores, quality of life, anxiety and depression, diary data and self‐rating.This study consisted of four groups and consequently fits with comparison 3 and 6 below. No data were given in a format suitable for statistical analysis in RevMan.
Group 1: education (advice and information on bowel re‐training).
Group 2: education and sphincter exercises.
Group 3: education, sphincter exercises and clinic biofeedback.
Group 4: education, sphincter exercises, clinic biofeedback and home biofeedback daily.
Education plus exercises versus education alone
In the groups comparing education plus sphincter exercises (43 patients) with education alone (37 patients) there were no reported difference between the groups for any of multiple outcomes on an intention‐to‐treat analysis immediately after and at one year follow‐up.
Education, sphincter exercises and clinic biofeedback versus education alone
In the groups comparing education plus sphincter exercises versus sphincter exercises plus clinic biofeedback versus sphincter exercises plus clinic and home biofeedback there were no statistically significant differences reported between the groups in the outcomes of manometry, scores, quality of life, diary, visual analogue scale, or anxiety and depression at the end of treatment nor at one year follow‐up.
Education, sphincter exercises, clinic biofeedback and home biofeedback daily versus education alone
In the groups comparing education plus sphincter exercises versus sphincter exercises plus clinic biofeedback versus sphincter exercises plus clinic and home biofeedback there were no statistically significant differences reported between the groups in the outcomes of manometry, scores, quality of life, diary, visual analogue scale, or anxiety and depression at the end of treatment nor at one year follow‐up.
Exercises plus habit re‐training versus habit re‐training alone
Whitehead included 18 participants. The data were not suitable for analysis in RevMan. After four weeks of exercises the median number of incontinent episodes per week was 0.70 for the exercise group and 0.54 for the no‐exercise group. Measures of variation were not reported and it was not possible to perform any statistical analyses on these data. All patients underwent habit training. Alternate patients were initially assigned to sphincter exercises or no exercises. The main focus of the trial was, however, biofeedback therapy. All patients who failed to respond to the exercise phase were treated subsequently with biofeedback. Most of the results presented in the paper referred to this non‐randomised phase and consequently were not analysed. No further data were available from the authors (Whitehead 1985).
4. Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus exercises with or without biofeedback
Four trials were included in this comparison (Fynes 1999; Hinninghofen 2003; Mahony 2004; Schwandner 2010).
Exercises plus biofeedback plus electrical stimulation versus exercises plus biofeedback
The combined result of Fynes and Schwandner showed a statistically significant result favouring the addition of electrical stimulation to biofeedback over biofeedback alone for numbers failing to achieve full continence (RR 0.60, 95% CI 0.46 to 0.78) (Analysis 4.1). Participants were on average 40% more likely to achieve full continence in the electrical stimulation group compared with control.
4.1. Analysis.
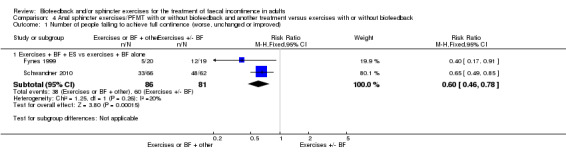
Comparison 4 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus exercises with or without biofeedback, Outcome 1 Number of people failing to achieve full continence (worse, unchanged or improved).
Schwandner (Schwandner 2010) compared 'Triple target training' where amplitude‐modulated middle‐frequency electrical stimulation was combined with electromyography (EMG) biofeedback versus EMG biofeedback carried out at home daily for 20 minutes for a duration of nine months. Schwandner also showed a statistically significant result for the incontinence score favouring the addition of electrical stimulation (Analysis 4.6).
4.6. Analysis.
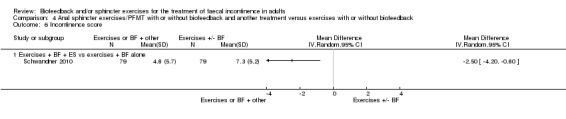
Comparison 4 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus exercises with or without biofeedback, Outcome 6 Incontinence score.
Fynes (Fynes 1999) compared vaginal pelvic floor manometric pressure biofeedback and home exercises taught by a continence nurse versus anal EMG biofeedback and home exercises in combination with anal electrical stimulation taught by a physiotherapist. The number of people with no improvement in their faecal incontinence symptoms was significantly lower in the electrical stimulation group (RR 0.06, 95% CI 0.00 to 0.91) (Analysis 4.2). Other outcomes were presented as median values and range (continence score) or as mean values and range (resting pressure, squeeze pressure, squeeze increment and vector symmetry). The estimation of the standard deviation could not be computed from the range since this would result in an over‐estimation of the standard deviation.
4.2. Analysis.
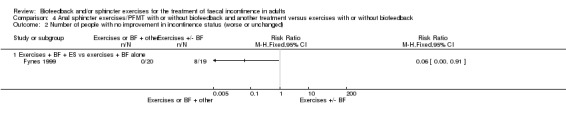
Comparison 4 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus exercises with or without biofeedback, Outcome 2 Number of people with no improvement in incontinence status (worse or unchanged).
Mahony (Mahony 2004) compared exercises plus biofeedback plus anal electrical stimulation versus exercises and biofeedback in 54 women with obstetric‐related faecal incontinence. However, most results given were intra‐group rather than inter‐group comparisons. The authors stated that there were no differences between the groups in continence scores, resting or squeeze pressures or quality of life.
Hinninghofen (Hinninghofen 2003) compared sphincter training with electrostimulation versus sphincter training with biofeedback. The data could not be analysed in RevMan.
5. Anal sphincter exercises/PFMT and biofeedback versus anal sphincter exercises/PFMT alone
Three trials were included in this comparison (Bols 2011; Heymen 2009; Hinninghofen 2003).
Bols (Bols 2011) evaluated rectal balloon therapy in addition to PFMT versus PFMT alone and reported that adding rectal balloon therapy was equally effective as PFMT alone in modifying the continence score of 5 points or more, and that added rectal balloon therapy was better than exercises alone on quality of life, manometric and global perceived effect measurements. The data were not suitable for statistical analyses in RevMan.
Heyman (Heymen 2009) compared manometric biofeedback and pelvic floor exercises with exercises alone. The number of people who failed to achieve full continence was significantly lower in the biofeedback and PFMT group (RR 0.70, 95% CI 0.52 to 0.94, Analysis 5.1). The number of people satisfied with the treatment (Analysis 5.3) was not significantly different between intervention groups.
5.1. Analysis.
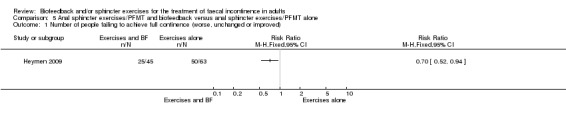
Comparison 5 Anal sphincter exercises/PFMT and biofeedback versus anal sphincter exercises/PFMT alone, Outcome 1 Number of people failing to achieve full continence (worse, unchanged or improved).
5.3. Analysis.
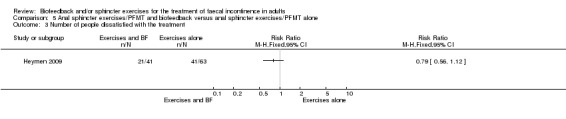
Comparison 5 Anal sphincter exercises/PFMT and biofeedback versus anal sphincter exercises/PFMT alone, Outcome 3 Number of people dissatisfied with the treatment.
Hinninghofen (Hinninghofen 2003) compared sphincter training with biofeedback versus pelvic floor training without support. The data could not be analysed in RevMan, only a brief abstract in German was available.
6. One type of biofeedback versus another type of biofeedback
Three trials were included in this comparison (Heymen 2000; Norton 2003; Solomon 2003).
Heyman (Heymen 2000) compared four different types of biofeedback: clinic EMG; clinic EMG plus rectal distension; clinic EMG plus home biofeedback; or clinic EMG plus rectal distension and home biofeedback. This trial reported no differences between the groups allocated to the different interventions. The data could not be analysed in RevMan.
Solomon (Solomon 2003) compared anal sphincter exercises (taught verbally and on digital examination) alone versus sphincter exercises plus ultrasound or EMG biofeedback in 120 patients. The data could not be analysed in RevMan. Solomon reported that there were no differences between the three groups in manometric measurements, continence scores, incontinence symptoms or quality of life at the end of treatment. The data for continence scores and manometric parameters are presented in 'Other data' tables (Analysis 6.7; Analysis 6.13).
6.7. Analysis.
Comparison 6 One type of biofeedback versus another type of biofeedback, Outcome 7 Incontinence score (median).
| Incontinence score (median) | |||
|---|---|---|---|
| Study | St Marks Vaizey 0‐13 | Pescatori (0‐6) | Self‐rating (0‐10) |
| Solomon 2003 | Ultrasound BFB = 7 Manometric = 6 Exercises only = 8 | Ultrasound BFB = 4 Manometric BFB = 4 Exericses alone = 4 | Ultrasound BFB = 3.6 Manometric BFB = 4.0 Exericses alone = 3.5 |
6.13. Analysis.
Comparison 6 One type of biofeedback versus another type of biofeedback, Outcome 13 Manometric pressures (medians).
| Manometric pressures (medians) | |||
|---|---|---|---|
| Study | Resting pressure | Squeeze pressure | Fatigue time |
| Solomon 2003 | Ultrasound BFB = 44 (mm Hg) Manometric BFB = 45 (mm Hg) Exericses alone = 48 | Ultrasound BFB = 95 (mm Hg) Manometric BFB = 78 (mm Hg) Exericses alone = 90 | Ultrasound BFB = 27 (sec) Manometric BFB = 21 (sec) Exericses alone = 15 |
Norton (Norton 2003) compared education, sphincter exercises and clinic biofeedback versus education, sphincter exercises, clinic biofeedback and home biofeedback. The data could not be analysed in RevMan. Norton stated that the addition of home biofeedback did not result in any statistically significant difference in incontinence scores, manometric measurements, quality of life, diary, or anxiety and depression measurements both at the end of treatment and at one year follow‐up.
7. One type of anal sphincter exercises/PFMT versus another type of anal sphincter exercises/ PFMT
Two trials were included in this comparison (Bartlett 2011; Markwell 2006).
Bartlett compared a standard clinical protocol (sustained submaximal anal and pelvic floor exercises versus an alternative group (rapid squeeze plus sustained submaximal exercises) with biofeedback in both arms of the study (Bartlett 2011) and reported no difference in objective manometric measurements, Cleveland Clinic (Wexner) Fecal Incontinence score or the Fecal Incontinence Quality of Life Scale survey tool.
Markwell (Markwell 2006) compared one type of exercise versus another type of exercise, however there were no useable data for this review. One group (Group A) were taught a specific pelvic floor muscle action, abdominal muscle action, toilet dynamics and dietary advice; the other group (Group B) were taught a standard pelvic floor muscle exercise and were provided with the same dietary advice. Markwell (Markwell 2006) reported that those in Group A were significantly more happy with their symptoms than those in Group B, at three months.
One trial with a complex cross‐over design with only eight patients did not report data in sufficient details to be analysed in RevMan (Latimer 1984).
Discussion
Summary of main results
Some studies have suggested that there is no difference between different conservative interventions and that adding exercises or biofeedback, or both, does not enhance the outcomes of conservative management (Norton 2003). However, subsequent studies have used a step‐wise protocol, trying the simpler interventions first and then only recruiting those who fail to respond to simpler measures such as diet and education (Bols 2011: Heymen 2009). These later studies have found a difference between exercise alone and exercise with the addition of rectal balloon (Bols 2011) or EMG biofeedback (Heymen 2009) in favour of adding biofeedback.
There was not enough evidence to say whether different methods of providing feedback made a difference (Heymen 2000; Norton 2003; Solomon 2003) because the trials were small.
Addition of electrical stimulation to biofeedback and exercises may also enhance results (RR 0.60, 95% CI 0.46 to 0.78) (Fynes 1999; Schwandner 2010). A single trial in this review suggests that anal biofeedback is superior to vaginal, and that electrical stimulation might enhance the results of exercises (Fynes 1999). However, the trial focused on the use of electrical stimulation as an adjunct to biofeedback and compared two very different types of interventions (vaginal pelvic floor manometric pressure biofeedback and home exercise with anal EMG biofeedback and home exercises in combination with anal electrical stimulation) and did not single out just the effects of electrical stimulation or biofeedback. Moreover, it is difficult to know how much of this improvement is a consequence of the natural history of faecal incontinence following childbirth as a no‐treatment group was not included.
In one small trial (Tjandra 2008) showed that sacral nerve stimulation was better than conservative management which consisted of biofeedback and PFMT.
One small trial (Schwandner 2011) showed that adding biofeedback to electrical stimulation was better than electrical stimulation alone (RR for failing to achieve full continence 0.47, 95% CI 0.33 to 0.65).
One small trial (Heymen 2009) comparing manometric biofeedback and pelvic floor exercises with exercises alone showed a statistically significant result for number of people failing to achieve full continence favouring biofeedback (RR 0.70, 95% CI 0.52 to 0.94).
It appears also that training to enhance rectal discrimination of sensation may be helpful in reducing faecal incontinence (Bols 2011; Miner 1990). It may be that adding this technique to the more commonly available pelvic floor muscle training (PFMT) would enhance results, but this cannot be a strong recommendation in view of the small numbers and lack of follow‐up data (Bols 2011).
Further conclusions are not warranted from the available data.
Overall completeness and applicability of evidence
There was a wide variation among trial reports in terms of characteristics of participants, characteristics of interventions, choice of outcome measures, duration of treatment and length of follow‐up. Most of the trials were small and probably of insufficient power to detect any differences between intervention groups. The outcome measures used were often insufficiently reported to enable further statistical analyses. Length of follow‐up was not clearly reported or was inadequate in many of the trials. The way in which data were reported in many of the trials (by not reporting measures of variance) made a quantitative synthesis of results (meta‐analysis) impossible.
Quality of the evidence
Randomised controlled trials are thought to provide sound evidence on the effects of healthcare interventions mainly because they can eliminate selection bias. Methodological weaknesses in some studies included in this review are likely to have compromised this assumption. About half of the trials had low risk of bias for randomisation and allocation concealment.
Potential biases in the review process
It should be noted that pressure and EMG measurements may not be comparable between different studies because of equipment and technique variations. Within‐study changes should be more reliable. There are no direct 'objective' measures of faecal incontinence. Changes in anorectal physiology measurements are proxy outcome measures and need not mean changes in the patient's symptoms, which should be seen as the primary end‐point.
Agreements and disagreements with other studies or reviews
There are over 60 uncontrolled trial reports in the literature on the use of biofeedback for the management of faecal incontinence in adults (Norton 2009). Some authors maintain that biofeedback is the treatment of choice for faecal incontinence on the basis of the findings of these observational studies. The results of this review show that there is some evidence from randomised controlled trials to support the effectiveness of biofeedback therapy for the management of people with faecal incontinence. All studies reviewed showed improved symptoms in all groups, and some difference between groups are reported in the latest studies in favour of adding biofeedback or electrical stimulation.
Authors' conclusions
Implications for practice.
We found no evidence that one method of biofeedback or exercises gives any benefit over any other method, but biofeedback or electrical stimulation may offer an advantage over exercises alone if patients have previously failed to respond to other conservative managements. Addition of biofeedback to surgical sphincter repair does not appear to improve the outcome (Davis 2004). On the whole, it is not possible to draw strong conclusions for practice from the data analysed in this review. In particular, there is not enough evidence on which to select patients suitable for anal sphincter exercises or biofeedback, or both; nor to know which modality of biofeedback or exercises is optimal. Reducing the threshold of discrimination of rectal sensation does seem to be clinically useful (Miner 1990). Electrical stimulation or anal biofeedback, or both, may be superior to vaginal biofeedback in women with symptoms after childbirth (Fynes 1999). One trial (Tjandra 2008) included in this review found sacral nerve stimulation to be superior to exercises. However, based on the available evidence these conclusions can only be tentative. No study reported any adverse events or deterioration in symptoms, and it seems unlikely that these treatments may cause any harm.
Treatment options for faecal incontinence have not yet been investigated by means of well‐designed trials. A Cochrane review of surgery for faecal incontinence (Brown 2010) failed to draw conclusions about the effectiveness of different surgical interventions mainly because of the dearth of controlled clinical trials concerning the most common operations (for example anterior overlapping anal sphincter repair). Another Cochrane review on drug treatments failed to draw firm conclusions on the efficacy of current pharmacological interventions (Cheetham 2002).
Implications for research.
There is a need for well‐designed randomised controlled trials with adequate sample sizes, validated outcome measures and long‐term follow‐up. In particular, studies should assess the effectiveness of different components of the package of care often called 'biofeedback', including exercises, feedback on sphincter function, rectal sensitivity training and co‐ordination training, as well as lifestyle advice that is often given to patients during the course of consultation (e.g. dietary advice, use of medication, bowel habit information). Comparisons of intensive versus less intensive exercise regimens would be useful, as would measurement of compliance with exercises and advice. Little attention seems to have been given to the patient's perspective on outcome in the published studies, and there is no information on what patients view as a good or satisfactory outcome of treatment for faecal incontinence. Economic analyses should also be incorporated into future trials.
There is a need for trials comparing exercises or biofeedback, or both, to other treatments such as medication, dietary manipulation or surgery. In all future studies there is a need to characterise the participants in detail so that judgements can be made on which treatments are of benefit to which diagnostic categories.
What's new
| Date | Event | Description |
|---|---|---|
| 23 April 2012 | New search has been performed | Substantive amendment: updated with nine new studies and conclusions changed. |
| 23 April 2012 | New citation required and conclusions have changed | updated with nine new studies. |
History
Protocol first published: Issue 4, 1998 Review first published: Issue 2, 2000
| Date | Event | Description |
|---|---|---|
| 16 September 2008 | Amended | Converted to new review format. |
| 24 May 2006 | New search has been performed | For this update six published studies were added to the previous review (Davis 2004; Heymen 2000; Ilnyckyj 2005; Mahony 2004; Norton 2003; Solomon 2003). |
| 23 May 2006 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We would like to thank Adrian Grant and Charis Glazener for their helpful comments, Sheila Wallace for help and advice with the electronic search strategy and the trialists we were able to contact for their collaboration.
Data and analyses
Comparison 1. Anal sphincter exercises/PFMT with or without biofeedback versus no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Number of incontinence episodes per week | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Number of pad changes required per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Incontinence score | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number of people dissatisfied with the treatment | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Sensory threshold (rectal balloon distension ‐ ml) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9 Manometric resting pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Manometric squeeze pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 General health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Condition specific quality of life measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Psychological health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. Anal sphincter exercises/PFMT with or without biofeedback versus any other treatment alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number of incontinence episodes per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number of pad changes required per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Incontinence score | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number of people dissatisfied with the treatment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 Biofeedback vs electrical stimulation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Sensory threshold (rectal balloon distension ‐ ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Manometric resting pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Manometric squeeze pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 General health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Condition specific quality of life measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Psychological health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 3. Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Exercises +BF+ ES vs ES alone | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Satisfaction with the treatment | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number of incontinence episodes per week | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Exercises + drugs vs SNS | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Number of pad changes required per week | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Exercises + drugs vs SNS | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Incontinence score | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Exercises + BF + surgery vs surgery alone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Exercises + drugs vs SNS | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Exercises + BF + ES vs ES alone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Sensory threshold (rectal balloon distension ‐ ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Manometric resting pressure | 0 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 Exercises + BF + ES vs ES alone | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Manometric squeeze pressure (cm of water) | 0 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Exercises + BF + ES vs ES alone | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Vector symmetry index | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Saline retention test (ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 General health measures | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.1 Exercises + drugs vs SNS | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Condition specific quality of life measures | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Exercises + drugs vs SNS | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
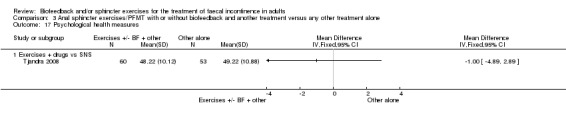
| 17 Psychological health measures | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 17.1 Exercises + drugs vs SNS | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Satisfaction with treatment (VAS) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 19.1 Exercises + BF + surgery vs surgery alone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Manometric pressures (medians) | Other data | No numeric data | ||
| 20.1 Exercises + BF + education vs exercises + education | Other data | No numeric data |
3.15. Analysis.
Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 15 General health measures.
3.17. Analysis.
Comparison 3 Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus any other treatment alone, Outcome 17 Psychological health measures.
Comparison 4. Anal sphincter exercises/PFMT with or without biofeedback and another treatment versus exercises with or without biofeedback.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Exercises + BF + ES vs exercises + BF alone | 2 | 167 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.46, 0.78] |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Exercises + BF + ES vs exercises + BF alone | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number of people dissatisfied with the treatment | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number of incontinence episodes per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number of pad changes required per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Incontinence score | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Exercises + BF + ES vs exercises + BF alone | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Sensory threshold (rectal balloon distension ‐ ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Manometric resting pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Manometric squeeze pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Vector symmetry index | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Saline retention test (ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 General health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Condition specific quality of life measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Psychological health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 5. Anal sphincter exercises/PFMT and biofeedback versus anal sphincter exercises/PFMT alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number of people dissatisfied with the treatment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Number of incontinence episodes per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number of pad changes required per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Incontinence score | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Sensory threshold (rectal balloon distension ‐ ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Manometric resting pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Manometric squeeze pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Vector symmetry index | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Saline retention test (ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 General health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Condition specific quality of life measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Psychological health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 6. One type of biofeedback versus another type of biofeedback.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number of people dissatisfied with the treatment | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number of incontinence episodes per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number of pad changes required per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Incontinence score | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Incontinence score (median) | Other data | No numeric data | ||
| 8 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Sensory threshold (rectal balloon distension ‐ ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Manometric resting pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Manometric squeeze pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Manometric pressures (medians) | Other data | No numeric data | ||
| 14 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Vector symmetry index | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Saline retention test (ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 General health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Condition specific quality of life measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Psychological health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 7. One type of anal sphincter exercises/PFMT versus another type of anal sphincter exercises/ PFMT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of people failing to achieve full continence (worse, unchanged or improved) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number of people with no improvement in incontinence status (worse or unchanged) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number of incontinence episodes per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number of pad changes required per week | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Incontinence score | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number of people with adverse effects | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number of people dissatisfied with the treatment | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Sensory threshold (rectal balloon distension ‐ ml) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Manometric resting pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Manometric squeeze pressure (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Manometric squeeze increment (cm of water) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Duration of squeeze (seconds) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 General health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Condition specific quality of life measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Psychological health measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Activities of daily living measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bartlett 2011.
| Methods | Randomised clinical study. Analysis not intention to treat. |
|
| Participants | Setting and country: single hospital anorectal physiology clinic, Australia. Inclusion criteria: faecal incontinence had failed to respond to conservative treatment prescribed by general practitioners over a 6 to 12 month period. Exclusion criteria: none stated Number of participants:101 approached (26 had moved, 2 excluded, one refused) 72 recruited; 69 completed treatment; 53 completed follow‐up Age: mean age 62.1 years (range 32‐82) Sex: 53 women, 19 men Other characteristics of participants: |
|
| Interventions | Standard clinical protocol (37 participants: sustained submaximal anal and pelvic floor exercises. Alternative group (35 participants: rapid squeeze plus sustained submaximal exercises) with biofeedback in both arms of the study 5 outpatient sessions over 8 weeks. First 4 sessions were weekly; participants then practised techniques for 4 weeks before returning for their final session. |
|
| Outcomes | Cleveland Clinic (Wexner) Fecal Incontinence score Fecal Incontinence Quality of Life Scale survey tool Anorectal function ‐ manometric measurements Follow‐up period: 2 years (n = 53) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Independent unrestricted randomization was performed before study commencement using a computer‐generated sequence' |
| Allocation concealment (selection bias) | Unclear risk | Study arm placed in a sealed opaque envelope with the participant identification number on the front and given to the therapist immediately before session 3 |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants were blinded. Researcher received the randomisation sequence immediately before analysis |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 69/72 completed. 53/72 available at 2 years. Patients who did not complete the programme were treated as missing. Quality of life assessment ‐ 35 out of 37 available for sustained exercise group and 34 out of 35 available in rapid and sustained exercise |
Bols 2011.
| Methods | Randomised controlled trial. Analysis intention to treat: missing values used multiple imputation procedure. |
|
| Participants | Setting and country: Single University Hospital Medical Centre, Netherlands. Inclusion criteria: Adults with faecal incontinence. Vaizey score of at least 12, faecal incontinence lasting at least six months, failure of dietary measures and medication. Exclusion criteria: not stated. Number: 80 participants Age: mean 59.3 (sd ± 11.9) Sex: not stated Other characteristics of participants: groups comparable on demographics at baseline. |
|
| Interventions | 40 patients rectal balloon therapy re‐training sensory threshold and coordination, with PFMT. 40 patients PFMT (strength, duration, timing and co‐ordination of contraction) alone. 12 sessions with a physiotherapist using a standardised protocol, within nine weeks. |
|
| Outcomes | Patients evaluated at mean of 6.8 weeks (SD = 5.3). Primary outcome (subjective) based on Vaizey score ranging from 0 (complete continence) to 24 (complete incontinence) Fecal Incontinence Quality of Life (FIQL) Nine point global perceived effect (GPE) score PERFECT pelvic floor assessment Objective measures were anorectal manometry, rectal capacity measurement, anorectal sensation, anal endosonography and defecography Follow‐up period: mean 6. 8 weeks (SD 5.3) after end of treatment |
|
| Notes | Recruited from August 2006 to May 2009. Abstracts and protocol only available at time of this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomised by means of a computer generated list |
| Allocation concealment (selection bias) | Unclear risk | Researchers were blinded to treatment assignment |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Researchers were blinded to treatment assignment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Ten patients (12.5%) dropped out during or after treatment. Completion rates did not differ between groups (P = 0.31) |
Davis 2004.
| Methods | Randomised controlled trial. Analysis not intention to treat. | |
| Participants | Setting and country: single hospital centre UK. Inclusion criteria: 43 female patients underwent sphincter repair for obstetric external sphincter defect: 38 consented to randomisation: 31 available for follow up. Exclusion criteria: congenital abnormalities, IBS, rectal prolapse, rectocoele, non‐obstetric trauma "anorectal conditions" (number not stated). Number of participants: 38 randomised; 31 completed Age: mean 60.48 years (SD 11.92). Sex: all 38 were women. Other characteristics of participants: 30/31 completing were parous. Groups comparable for age, parity and duration of symptoms. |
|
| Interventions | All patients had an anal sphincter repair. Intervention: anal sphincter repair plus biofeedback which commenced three months after surgery (written and verbal information, one therapist, sessions 1 hour per week for 6 weeks, individualised exercise programme, home exercises: biofeedback: 2 balloon manometry for amplitude and duration of squeeze, isolate from abdominal effort: auditory or visual feedback; sensory training Control: anal sphincter repair only. |
|
| Outcomes | Visual analogue scale for subjective outcome; quality of life; continence score; manometry Follow‐up period: 12 months after surgery (9 months after start of biofeedback). |
|
| Notes | Most data presented as before‐after analysis rather than between group analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated list of random numbers |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 38 randomised: 7 withdrew or lost to follow‐up |
Fynes 1999.
| Methods | Randomised controlled trial. Analysis: not intention to treat. |
|
| Participants | Setting and country: single centre, Dublin, Ireland. Inclusion criteria: consecutive women with faecal incontinence caused by obstetric trauma presenting to a dedicated perineal clinic. Exclusion criteria: none stated. Number of participants: 40, one withdrawal Age: mean 32 years (range 18‐48 years) Sex: 40 women Other characteristics of participants: mean duration of symptoms 4 months (range 3‐28 months). 37 women were symptomatic after primary repair of recognised anal sphincter disruption, and 3 after traumatic instrumental delivery with no attempt at repair. 24 were primiparous, and 16 were multiparous. No significant differences between the two groups in age, parity or duration of symptoms. |
|
| Interventions | Group 1: Sensory biofeedback: by continence nurse using Peritron perineometer vaginal probe. Weekly 30‐minute sessions for 12 weeks. Fast twitch: aim for 20 short maximum contractions of 6‐8 seconds, 10 seconds relaxation between. Slow twitch: aim for 30 seconds duration. Patients treated supine.
Group 2: Augmented biofeedback: weekly sessions with a specialist physiotherapist using Incare PRS 9300 computer with anal probe to give audiovisual EMG feedback and electrical stimulation. Patient in left lateral position. 13‐second cycles: 5 seconds activity, 8 seconds rest, for 15 minutes. Slow twitch: hold for 5 seconds, fast twitch: 3 fast contraction in 5 seconds, alternating. Then electrical stimulation, 20% ramp: 20Hz for 10 minutes (5 seconds stimulation, 8 seconds rest); then 50Hz, time unspecified, 8 seconds stimulation with 30 seconds rest. Both groups advised to practice "standard Kegel pelvic floor exercises" at home (instructions not reported). |
|
| Outcomes | Anorectal manometric parameters (resting, squeeze and squeeze increment pressures and a vector symmetry index), symptom questionnaire and continence scores Follow‐up period: 12 weeks treatment only. |
|
| Notes | Compared two completely different treatments, with different therapists. The authors claim that the difference in outcome is attributable to electrical stimulation is questionable. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated using Ran List |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Therapist blind to obstetric history and previous test findings. Outcome assessor blind to treatment group. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 40 randomised, one dropout |
Healy 2006.
| Methods | Randomised trial. Analysis: not intention to treat. |
|
| Participants | Setting and country:single hospital centre in Ireland. Inclusion criteria: not stated. Exclusion criteria: significant anal sphincter disruption. Number of participants: 58 randomised; 48 completed Age: mean age 55 years (range 40‐78) Sex: 58 women Other characteristics of participants: |
|
| Interventions | Previously excluded stool softening foods for 1 month. 1. Endo‐anal pudendal nerve stimulation daily at home using Anuform anal probe for 1 hour. 2. Attended physiotherapy department for endo‐anal electrical stimulation under supervision. Alternating EMG biofeedback and electrical stimulation using augmented biofeedback. Stimulation alternating 15 minute cycles at 10Hz and 40Hz. 3 months intervention. |
|
| Outcomes | Manometry PNTML Cleveland Clinic (Wexner) faecal incontinence score Generic quality of life (SF‐36) Follow‐up period: end of treatment. |
|
| Notes | Trial lasted 3 years | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 10 of 58 dropped out with no reporting of outcomes |
Heymen 2000.
| Methods | Randomised controlled trial. Analysis: not intention to treat. |
|
| Participants | Setting and country: single centre USA. Inclusion criteria: non‐surgical candidates based on clinical, manometric and electrophysiological parameters. Exclusion criteria: eligible for surgical management. Number of participants: 40 randomised: 6 withdrew after one session: 34 analysed Age: mean 74 years (range 36‐88) Sex: 23 female, 11 male Other characteristics of participants: mean Wexner score 12 (range 7‐14). |
|
| Interventions | Group 1: Feedback display of EMG activity of intra‐anal EMG plus education as to pelvic floor physiology and operant conditioning techniques to retrain function. Group 2: Outpatient EMG biofeedback plus balloon distension sensory training. Group 3: Outpatient BF plus HT EMG biofeedback for home practice. Group 4: Outpatient biofeedback training plus in session balloon distension sensory training plus HT unit for practising exercises. | |
| Outcomes | Diary: Days per week with incontinence episodes Follow‐up period: immediately after treatment only. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation method |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 40 randomised: 6 withdrew: 34 analysed |
Heymen 2009.
| Methods | Randomised controlled trial. Analysis: intention to treat. |
|
| Participants | Setting and country: single centre. Tertiary referral hospital in USA. Inclusion criteria: consecutive series of "chronically incontinent patients referred to University of North Carolina Hospitals". At least 1 teaspoon of faeces at least weekly; anatomic defects on anal ultrasound permissible. Exclusion criteria: flatus incontinence and staining only; psychotic disorder and severe cognitive impairment Number of participants: 168 randomised. After run‐in period of conservative management, 108 started intervention as randomised. Age: average 59.6 years Sex: 83 female, 25 male Other characteristics of participants: |
|
| Interventions | PFMT alone 63 participants. PFMT plus manometric biofeedback 45 participants. Both groups taught behavioural strategies to avoid incontinence. |
|
| Outcomes | Primary: Faecal Incontinence Severity Index (FISI) Secondary: Days per week incontinent; complete continence (no staining); squeeze pressure and abdominal tension; Faecal incontinence quality of life score (FI‐QoL); telephone report to therapist of "adequate relief" |
|
| Notes | Randomised patients prior to run‐in period which resulted in unbalanced group sizes: 35 patients reported adequate relief from run‐in and 24 withdrew, resulting in 109 patients only entering treatment phase. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Co‐investigator produced the randomisation table using random number generator |
| Allocation concealment (selection bias) | Unclear risk | Group membership was reported to the therapist after patient arrived for initial visit. Patients randomised prior to unblinded run‐in phase |
| Blinding (performance bias and detection bias) All outcomes | High risk | Therapist telephoned participant to ask if they had experienced "adequate relief" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis reported: authors replaced missing values with zero |
Hinninghofen 2003.
| Methods | Randomised controlled trial. Analysis: unclear if intention to treat. |
|
| Participants | Setting and country: Germany Inclusion criteria: patients of incontinence clinic Exclusion criteria: none stated Number of participants: 65 randomised Age: 65 ± 12.4 Sex: not stated Other characteristics of participants: none stated |
|
| Interventions | 1.Sphincter training with biofeedback machine (26 participants) 2. Sphincter training with electrostimulation (18 participants) 3. Pelvic floor training without support (21 participants) 3 months intervention |
|
| Outcomes | Rockwood faecal incontinence quality of life score; general quality of life score Dupey et al 1994; Wexner incontinence score. | |
| Notes | Brief abstract in German only. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Ilnyckyj 2005.
| Methods | Randomised controlled trial. Analysis: not intention to treat. |
|
| Participants | Setting and country: single centre, Canada. Inclusion criteria: women with regular and frequent "idiopathic" FI; bowel imaging within past 2 years. Exclusion criteria: diabetes with neuropathy, neurological disease, less than 6 months since childbirth, IBS, sphincter injury amenable to surgery. Number of participants: 23 of 54 screened met study criteria. Withdrawals: 5, groups not specified Age: mean 59 years (range 26‐75) Sex: 23 women, 0 men Other characteristics of participants: mean parity 3 |
|
| Interventions | Group 1 education and anal sphincter exercises. Group 2 education and manometric BF therapy. | |
| Outcomes | Success defined as no incontinence episode during last week of study
Manometry Follow‐up: end of study. |
|
| Notes | Probably under powered to detect a difference. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No mention |
| Allocation concealment (selection bias) | Unclear risk | No mention |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No mention |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 23 randomised 5 drop outs. Of 18 completers, 7 in biofeedback, 11 in education group |
Latimer 1984.
| Methods | Single case experiments to examine three components of biofeedback. Cross‐over design. Analysis: intention to treat. Allocation: patients randomly assigned to treatment B or C after A (see interventions). Design ABACADA or ACABADA. |
|
| Participants | Setting and country: single centre, Canada. Inclusion criteria: recruited from colleagues. Exclusion criteria: none stated. Number of participants: 8 subjects (4 adults and 4 children) Age: mean age: 49 years for adults and 11 years for children (range 8‐72) Sex: 4 males, 4 females Other characteristics of participants: heterogeneous pathologies. |
|
| Interventions | 4 phases to study: A ‐ one month self‐monitoring diary. B ‐ sphincter strengthening exercise training (squeeze anus in response to rectal balloon inflation: 50 trials over 2 hours, verbal feedback only). C ‐ rectal sensory discrimination training (2‐3 second balloon inflations, decreased in 5‐10ml steps, verbal reinforcement, 50 trials over 2 hours). D ‐ biofeedback (B+C + biofeedback using 3‐balloon system to demonstrate recto‐anal inhibitory reflex and teach appropriate external anal sphincter contraction in response to reflex internal anal sphincter relaxation, visual feedback of performance. Two hour session weekly for 4 weeks using manometric anal probe. Same number of learning trials and same time with therapist at each session. Weekly contact by phone. Also allowed to use laxatives or enemas. | |
| Outcomes | Daily diary of accidents, stains and changes of underwear throughout, returned weekly by post when not attending. Manometry before, after and at 6 months follow‐up Follow‐up period: each phase 4 weeks duration (28 weeks total). |
|
| Notes | Participants randomised to order of components only; insufficient data at the end of each phase to enable analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No mention |
| Allocation concealment (selection bias) | Unclear risk | Patients randomly assigned to treatment B or C after A (see interventions). Design ABACADA or ACABADA |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No mention of blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdrawals |
Mahony 2004.
| Methods | Randomised controlled trial. Analysis: not intention to treat. |
|
| Participants | Setting and country: single centre, Ireland. Inclusion criteria: consecutive women with FI after obstetric injury attending a perineal clinic. Exclusion criteria: Diabetes, IBS, IBD, previous ano rectal surgery, malignancy. Number of participants: 60 Age: range 22 to 42 Sex: 60 women Other characteristics of participants: median parity one |
|
| Interventions | Group 1: Intra‐anal EMG BF weekly for 12 weeks. Group 2: Intra‐anal EMG BF plus 20 mins with 5 second stimulation and 8 seconds relaxation between contractions. Intra‐anal EMG BF plus electrostimulation at 35 Hz with a 20% ramp modulation time. Stimulation. |
|
| Outcomes | Questionnaire and faecal incontinence quality of life scale, continence score and manometry Follow‐up period: end of treatment. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated allocation |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No mention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 60 randomised 6 withdrawals: 4 from biofeedback, 2 from electrostimulation |
Markwell 2006.
| Methods | Randomised trial. Analysis not intention to treat. First stage ( 3 months) parallel group design then participants were asked if they wanted to cross‐over to the treatment arm. |
|
| Participants | Setting and country: single centre, Australia. Inclusion criteria: self reported inability to perceive loss on more than one occasion. Exclusion criteria: dementia unable to understand written and spoken English, lack of abdominal muscle innervation, previous pelvic floor treatment. Number of participants: 111 Age: mean 62 years (SD 12) Sex: 87 women, 24 men Other characteristics of participants: mean length of incontinence 7.85 years. |
|
| Interventions | A. dietary modification, stool bulking agents, specific pelvic floor muscle action using abdominal muscles, defecation training, 54 participants. B. dietary modification, stool bulking agents, conventional pelvic floor exercise, 57 participants. |
|
| Outcomes | visual analogue scale for happiness with symptoms and happiness with physiotherapy programme, bowel diary, rectal sensation, descending perineum syndrome Follow‐up period: immediate (70/111) and one year (63%). |
|
| Notes | Unpublished study only reported in lengthy and unclear report. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated, stratified by gender and structural sphincter damage |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Single blind mentioned but who was blinded is unclear |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 45 completed in Group A out of 54 49 completed in Group B out of 57 36 in Group A went on to Group B protocol after Stage 1 |
McHugh 1986.
| Methods | Randomised controlled trial. Analysis: unclear if intention to treat. Allocation: randomised to biofeedback or exercises, cross‐over design. |
|
| Participants | Setting and country: single centre, Canada. Inclusion criteria: regular and frequent (more than 8 of 28 days) "idiopathic" FI. Exclusion criteria: 93 patients who responded to initial dietary manipulation excluded. Number of participants: 18. 5 of 18 dropped out (all from exercise group) Age: mean 55.2 ± 11.4 years |
|
| Interventions | Biofeedback ‐ standardised protocol ‐ 3 sessions over 2 months. No details given. Exercises: Daily voluntary sphincter exercise programme using a home manometer. | |
| Outcomes | Daily diaries of stains, accidents and stools Follow‐up period: 8 months study duration. |
|
| Notes | Abstract only. Insufficient data to allow statistical analyses. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No mention |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No mention of blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 5 of 18 dropped out (all from exercise group) |
Miner 1990.
| Methods | Two phase randomised controlled trial. Analysis: unclear if intention to treat. |
|
| Participants | Setting and country: single centre, UK. Inclusion criteria: incontinence on one month diary. Exclusion criteria: not incontinent on one month diary Number of participants: 28 consecutive patients, 3 excluded as not incontinent on one month diary, 25 entered study Age: 17‐76 years Sex: 8 men 17 women Other characteristics of participants: heterogeneous diagnoses. 5 had previous post‐anal repair, 2 inflammatory bowel disease; many also irritable bowel symptoms. Mean parity of women 4.2. |
|
| Interventions | One month diary, then phase 1 for 4 weeks (controls 8 weeks); then random allocation in phase 2 : strength or co‐ordination training, all crossed‐over.
Allocation: random allocation to sensory training or sham. Phase 1: Rectal discrimination versus sham training: random allocation to 3 x 20 minute sessions (within 3 days) of rectal discrimination training ‐ taught to recognise small volumes in rectal balloon and abolish any sensory delay (controls sham training with no feedback), controls cross‐over to active after 1 month). Phase 2: All then randomised to strength or co‐ordination training, crossed over after 1 month. Strength training: 3 20‐minute sessions within 3 days, encouraged to hold a maximal contraction for at least 20 seconds, then 4 exercise periods per day of 4 x 20second squeezes, resting for 20 seconds between, for 1 month. Co‐ordination training: 3 sessions within 3 days: aim for maximal voluntary contraction within 0.5 seconds of balloon inflation and not allow pressure to fall below pre‐inflation level (oppose recto‐anal inhibitory reflex). |
|
| Outcomes | Diary ‐ frequency of defecation, urgency and incontinence, manometry (resting and squeeze pressures and sensory threshold of rectal balloon distension) and questionnaire Follow‐up period: outcomes at end of each treatment phase and at 12 month follow‐up. |
|
| Notes | Sufficient data for analysis only from Phase 1. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No mention |
| Allocation concealment (selection bias) | Unclear risk | No mention |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No mention of blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No withdrawals |
Naimy 2007.
| Methods | Randomised trial. Analysis not intention to treat. |
|
| Participants | Setting and country: single centre, Norway Inclusion criteria: women after 3rd or 4th degree perineal rupture during childbirth. Any grade of anal incontinence Exclusion criteria: major anal sphincter defect requiring surgical repair (only those with major symptoms were scanned by anal ultrasound); primary or secondary anal sphincter repair less than 12 months ago; pregnancy; inflammatory bowel disease or diarrhoea for other reasons. Number of participants: 49 Age: mean age 36 years (range 22‐44) Sex: 49 women Other characteristics of participants: mean parity 2.1 (range 1‐4). |
|
| Interventions | 1. Biofeedback: Neuro Trac ETS:using Anuform anal probe. Quick 3 second squeeze; 10 second squeeze; squeeze for as long as it kept 50% of 3 second amplitude. Each squeeze repeated 5 times with equal rest time between. Initial session 30 minutes with 30 minute follow‐up session 1 week later. Then daily 30 minute session at home for 8 weeks. 2. Electrical stimulation: Neuro Trac ETS: 30 or 40Hz at alternate sessions; pulse width 200 µsec; upper limit 80 mAmp using Anuform anal probe. Patient turned up to maximum voltage which caused no discomfort. 3 seconds on 3 seconds rest for 20 minutes twice daily at home. Initial session 30 minutes with 30 minute follow‐up session 1 week later. Both 2 times daily for 8 weeks. |
|
| Outcomes | Cleveland Clinic (Wexner) FI score (primary outcome); Faecal incontinence quality of life score (FIQLS); visual analogue for quality of life; patient self‐rating of treatment effect (visual analogue score). Compliance monitor incorporated into equipment Follow‐up period: end of treatment. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation list |
| Allocation concealment (selection bias) | Unclear risk | No mention |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 40/49 completed: 19 in biofeedback and 21 in electrical stimulation |
Norton 2003.
| Methods | Randomised controlled trial. Analysis: intention to treat. |
|
| Participants | Setting and country: Single centre, UK Inclusion criteria: 18+ years, referred for symptoms of incontinence regardless of frequency or severity. Exclusion criteria: major structural sphincter disruption; previous BFB or exercises, neurologic disease, cognitive impairment, IBD, need urgent medical referral, insufficient written English. Number of participants: 171 randomised, 140 completed Age: Mean age 56 (range 26 to 85) Sex:12 men, 159 women Other characteristics of participants: 93% of women parous, median 2 vaginal deliveries. |
|
| Interventions | Median of 5 sessions with the same therapist. Group 1: up to 6 one hour sessions of advice and information plus bowel re‐training. Group 2: as group 1plus 50 anal sphincter contractions per day (taught on digital examination). Group 3: as group1 plus computer BFB to teach anal sphincter exercises. Group 4: As group 3 plus 20 mins home EMG BFB daily. |
|
| Outcomes | Patient rating, manometry, questionnaire, diary, score, SF36, HADS Follow‐up period: 1 year after finishing treatment. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated numbers |
| Allocation concealment (selection bias) | Low risk | Opaque brown envelopes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessor for repeat manometry |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 171 randomised, 140 completed. No difference between groups in completion rates |
Schwandner 2010.
| Methods | Randomised controlled trial. Analysis intention to treat. |
|
| Participants | Setting and country: multicentre (8 sites) in Germany. Inclusion criteria: patients with anal incontinence deemed capable of independent training; over 18 years. Exclusion criteria: retention/overflow incontinence; complete rectal prolapse; chronic inflammatory bowel disease; definite or possible pregnancy. Number of participants: 158: 7 withdrew consent before commencing therapy Age: mean 64 in group 1, 62 in group 2 Sex: 138 female, 13 male Other characteristics of participants: |
|
| Interventions | 1. "Triple target training": amplitude‐modulated middle‐frequency stimulation with current amplitude high enough to achieve perineal contraction; EMG‐triggered and EMG‐controlled exercises. 2. Biofeedback: training at home for 20 minutes twice daily while standing. 3‐8 second squeeze with pause of 10‐15 seconds. Need to activate puborectalis. Both interventions daily for 20 minutes at home for 9 months. |
|
| Outcomes | Primary: Cleveland Clinic incontinence score at 9 months (Wexner score); Vaizey score at 9 months Secondary: change from baseline in Cleveland Clinic incontinence score (Wexner score) and Vaizey score at 3 and 6 months; Faecal Incontinence Quality of life Score; acceptance and compliance; changes from baseline in stool‐modifying drug use. Follow‐up period: 9 months. |
|
| Notes | Note large and differential dropout rate (see below). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Generated by a clinical trials centre: self‐adjusting design of Nordle and Brandtmark was used with centre and incontinence grade as column variables and gender as row variable |
| Allocation concealment (selection bias) | Low risk | Telephone communication after registration form available |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Open label with blinded observers for secondary outcome measures. Person handing out patient self‐completion questionnaire was blinded to allocated group |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Report an intention‐to‐treat analysis: patients who dropped out assumed to have no change. However, there was a large and differential dropout rate between the groups which jeopardises the randomisation and the validity of the intention‐to‐treat analysis. Biofeedback: 19 of 79 completed; Triple therapy: 43/79 completed |
Schwandner 2011.
| Methods | Multicentre randomised trial, open parallel group design. | |
| Participants | Anal incontinence of Grade 1 or higher, 18% had endosonographically diagnosed sphincter damage | |
| Interventions | 80 participants. 1. "Triple target training": amplitude‐modulated middle‐frequency electrical stimulation with current amplitude high enough to achieve perineal contraction plus electromyographic (EMG) biofeedback and EMG‐controlled exercises 39 participants. 2. Standard treatment low frequency electrical stimulation 41 participants. |
|
| Outcomes | Cleveland clinic score, proportion of patients regaining continence, quality of life | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation performed centrally by telephone |
| Allocation concealment (selection bias) | Low risk | Randomisation performed centrally by telephone |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinded observer |
Solomon 2003.
| Methods | Randomised controlled trial. Analysis: not intention to treat. |
|
| Participants | Setting and country: single centre, Australia. Inclusion criteria: failed dietary and medical treatment. Exclusion criteria: No anatomic defect in external sphincter, IBD, peri‐anal inflammation, diarrhoea, rectal prolapse. Number of participants: 120 randomised, 102 completed Age: mean age 62 years Sex:107 women, 13 men Other characteristics of participants: |
|
| Interventions | Five thirty minute sessions over four months. Group 1: Anal sphincter exercises taught on digital examination. Group 2: Anal sphincter exercises taught with transanal ultrasound feedback. Group 3: Anal sphincter exercises taught with manometric feedback. | |
| Outcomes | Scores, VAS, investigators assessment, quality of life, manometry, fatigue rate Follow‐up period: end of treatment. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Opaque envelopes organised centrally |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes organised centrally |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessor blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 120 randomised, 102 completed (groups not stated) |
Tjandra 2008.
| Methods | Randomised study over 12 months. Analysis not intention to treat. |
|
| Participants | Setting and country: Single centre in Australia. Inclusion criteria: severe faecal incontinence. Exclusion criteria: rectal prolapse; inflammatory bowel disease; congenital ano‐rectal malformation; neurological disorders; stoma in situ; pregnancy; external anal sphincter defect of more that 120 degrees; bleeding diathesis; mental or physical disability precluding adherence to study protocol. Number of participants: 120 Age: 39‐86 years Sex: Mostly women, figures not given Other characteristics of participants: most had previous sphincter repair. |
|
| Interventions | 1. Optimum medical therapy, including pelvic floor exercises, bulking agents, dietary management of fluid and fibres with team of physiotherapists and dietitians. Attended varied with need, usually monthly for 6 months then 2 monthly. 2. two phase sacral nerve stimulation: peripheral nerve evaluation for at least 7 days. Patients with a 50% reduction or more in incontinence episodes were implanted with a permanent sacral nerve stimulator. |
|
| Outcomes | No primary outcome specified. Wexner incontinence score; Faecal Incontinence Quality of Life score; SF‐12; bowel diary; manometric resting and squeeze pressure Follow‐ up period: 12 months. |
|
| Notes | Main focus of the paper was sacral nerve stimulation: exercise group was the control. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Low risk | Performed from central registry using sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 7 patients in the SNS group did not proceed beyond the peripheral nerve evaluation stage |
Whitehead 1985.
| Methods | Allocation: Alternate patients allocated to exercises or control, all underwent simultaneous habit training. Analysis: unclear if intention to treat. |
|
| Participants | Setting and country: single centre, USA. Inclusion criteria: recruited by physicians or newspaper advertisement. Exclusion criteria: none stated. Number of participants: 18 Age: 65‐92 (mean 73.3 years) Sex: 3 men, 15 women Other characteristics of participants: 6 doubly incontinent. 2 demented and 3 depressed. |
|
| Interventions | Initial habit training (attempted defecation after breakfast and use of enema if no bowel action for two days), bulk agents for 11 patients; alternate patients also instructed to perform 50 sphincter exercises per day for 10 seconds each, with no such instruction in controls. If still incontinent after 4 weeks of habit training plus exercises or control, all received biofeedback. |
|
| Outcomes | Incontinent episodes per week; manometric sphincter strength, rectal sensation. Follow‐up period: 4 weeks. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Allocation by alternate patients |
| Allocation concealment (selection bias) | High risk | Alternate patients allocated to exercises or control, all underwent simultaneous habit training. If still incontinent after 4 weeks of habit training plus exercises or control, all received biofeedback |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No mention of blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
BFB: Biofeedback
EMG: Electromyography FI: Faecal incontinence
HADS: Hospital Anxiety and Depression Scale
HT: Home trainer IBD: Inflammatory bowel disease IBS: Irritable bowel syndrome SF36: Short Form‐36 VAS: Visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bates‐Jensen 2003 | Study of effect of general exercise on skin health |
| Byrne 2002 | Quality of life study, not RCT |
| Chase 2004 | Urinary incontinence only |
| Christensen 2009 | intervention trans‐anal irrigation not biofeedback |
| Cox 1996 | Participants were children |
| Cox 2003 | Participants were children |
| Croffie 2005 | Participants were children |
| Dannecker 2004 | Pre‐natal exercises, participants did not have faecal incontinence |
| Enck 1994 | Non‐randomised trial |
| Fang 2003 | Physiotherapy after stroke |
| Gaier 2010 | Prevention study, women were randomised to supervised PFMT or usual care. Women were not fecally incontinent at start of study |
| Glazener 2005 | Effect of post‐natal exercises on urinary incontinence. Most participants did not have faecal incontinence at baseline |
| Gouldthorpe | Abdominal muscle training during pregnancy |
| Harari 2004 | Effect of nursing advice on bowel function after stroke. Most participants did not have faecal incontinence at baseline |
| Heymen 2003 | Only one group of patients |
| Heymen 2004 | Pre‐treatment prior to randomisation |
| Heymen 2004a | Pre‐treatment prior to randomisation |
| Heymen 2005 | Constipation not faecal incontinence |
| Jorge 1994 | Intervention used for patients undergoing an ileo‐anal pouch operation as a preventive measure, not as a treatment for current faecal incontinence. |
| Klijn 2003 | Urinary incontinence |
| Leroi 2005 | Surgical study of sacral nerve stimulation |
| Levy‐Storms 2007 | Participants included on basis of urinary incontinence. No data on faecal incontinence |
| Loening‐Baucke 1988 | Non‐randomised trial in which participants were children |
| Loening‐Baucke 1990a | Non‐randomised trial |
| Loening‐Baucke 1990b | Participants were children |
| Loening‐Baucke 1995 | Non‐randomised trial in which participants were children |
| Markland 2009 | Epidemiology study. No intervention |
| Mathew 2004 | Wrote to authors to clarify contents and methodology. No reply received |
| Norton 2006 | Electrical stimulation with no exercises or biofeedback |
| O'Brien 2005 | Surgery (artificial bowel sphincter) |
| Oresland 1988 | Intervention used for patients undergoing an ileo‐anal pouch operation as a preventive measure, not as a treatment for current faecal incontinence |
| Osterberg 2004 | RCT comparing surgery with electrical stimulation. No exercises or biofeedback |
| Pager 2002 | Not an RCT |
| Pourmomeny 2011 | Study covers constipation |
| Powell 2003 | Abstract with no data |
| Richter 2011 | Cohort study, inclusion all women who underwent a sphincter repair at time of singleton delivery. Investigation of faecal incontinence |
| Ritterband 2003 | Participants were children |
| Roth 1999 | Electrical stimulation only |
| Schnelle 2002 | Effect of general mobility exercises in nursing home |
| Schnelle 2003 | Effect of general mobility exercises in nursing home |
| Simmons 2005 | Mobility and toileting intervention |
| Solomon 2000 | Not an RCT |
| Surh 1998 | Translation obtained, no mention of how patients were allocated. Written to authors |
| Tekeoglu 1998 | TENS intervention for activities of daily living in stroke patients, no faecal incontinence |
| van der Plas 1996a | Participants were children |
| van der Plas 1996b | Participants were children |
| Wald 1984 | Non‐randomised trial. Rectal sensation of diabetic patients compared to non‐incontinent diabetics and non‐diabetic incontinent people. All incontinent diabetics received biofeedback |
| Wald 1987 | Participants were children |
| Whitehead 1986 | Participants were children |
Characteristics of studies awaiting assessment [ordered by study ID]
Marshall 1995.
| Methods | Not clear how participants were allocated to treatment |
| Participants | 44 women with fecal incontinence after first delivery |
| Interventions | Transcutaneous electrical stimulation versus pelvic floor exercises |
| Outcomes | ICS draft questionnaire, visual analogue scales, resting and squeeze pressure, diary |
| Notes |
Pages 2003.
| Methods | Participants alternately assigned (used Google translate) this needs to be confirmed |
| Participants | Patients with fecal incontinence |
| Interventions | Biofeedback daily for 4 weeks Biofeedback daily for 4 weeks followed by a 2 month home exercise programme Electrostimulation for 3 months |
| Outcomes | Faecal frequency, subjective improvement, incontinence score |
| Notes | German paper, only English abstract, alternately assigned? need formal translation |
Characteristics of ongoing studies [ordered by study ID]
Dehli 2009.
| Trial name or title | A randomized, controlled, clinical trial of biofeedback and anal injections as first treatment of fecal incontinence. ControlledTrials.com (www.controlled‐trials.com) [accessed 2 February 2009] 2009. |
| Methods | Randomised study, blinded outcome assessor |
| Participants | Faecal incontinence lasting more than 6 months St Marks score of 4 or more No known local or general neurological disease 18 years or older No constipation |
| Interventions | Biofeedback versus anal injections |
| Outcomes | St Mark's incontinence score, quality of life, physiological parameters |
| Starting date | April 2006 |
| Contact information | Trond Dehli, Department of gastroenterological surgery, University hospital North Norway, Breivika, 9038 Tromsø trond.dehli@unn.no tlf: +47 776 26 000 |
| Notes |
Stott 2000.
| Trial name or title | A study to determine the effects of neuro‐stimulation on anal sphincter function when used in conjunction with biofeedback and pelvic floor exercises in the treatment of faecal incontinence. |
| Methods | Randomised controlled trial |
| Participants | Patients with faecal incontinence |
| Interventions | PFMT plus biofeedback versus PFMT plus biofeedback plus electrical stimulation |
| Outcomes | Continence score, quality of life, anal manometry, endoanal ultrasound |
| Starting date | January 2000 |
| Contact information | Sonia Stott |
| Notes |
Contributions of authors
One review author (C Norton) wrote the initial protocol of the review. Both review authors independently assessed the pertinence and quality of eligible studies and selected which to include in the review. Two review authors independently extracted data from trial reports of identified studies and both interpreted the results and contributed to the writing of the final version of the review.
Sources of support
Internal sources
Chief Scientist Office, Scottish Executive Health Department, UK.
External sources
National Health Service R&D Programme for People with Physical and Complex Disabilities, UK.
Declarations of interest
The lead review author is an author of a study included in the review.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Bartlett 2011 {published data only}
- Bartlett L, Sloots K, Nowak M, Ho YH. Biofeedback for fecal incontinence: a randomized study comparing exercise regimens. Diseases of the Colon & Rectum 2011;54(7):846‐56. [DOI] [PubMed] [Google Scholar]
- Bartlett LM, Sloots K, Nowak M, Ho YH. Biofeedback therapy for faecal incontinence: a rural and regional perspective. Rural Remote Health 2011;11(2):1630. [PubMed] [Google Scholar]
Bols 2011 {published data only}
- Bols E, Berghmans B, Hendriks E, Bie RA, Baeten C. Rectal balloon training as add‐on therapy to pelvic floor muscle training in adults with faecal incontinence: a randomized controlled trial (Abstract number RR‐PO‐311‐21‐Wed). Physiotherapy. 2011; Vol. 97 Suppl S1, issue Suppl S1. [DOI] [PubMed]
- Bols E, Berghmans B, Bie R, Govaert B, Wunnik B, Heymans M, et al. Rectal balloon training as add‐on therapy to pelvic floor muscle training in adults with faecal incontinence: a randomised controlled trial (Abstract number 211). Neurourology and Urodynamics 2011;30(6):1093‐4. [DOI] [PubMed] [Google Scholar]
- Bols E, Hendriks E, Bie R, Baeten C, Berghmans B. Predictors of a favourable outcome of physiotherapy in faecal incontinence: secondary analysis of a randomised trial (Abstract number 212). Neurourology and Urodynamics 2011;30(6):1095‐6. [DOI] [PubMed] [Google Scholar]
Davis 2004 {published data only}
- Davis KJ, Kumar D, Poloniecki J. Adjuvant biofeedback following anal sphincter repair: a randomized study. Alimentary Pharmacology & Therapeutics 2004;20(5):539‐49. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Fynes 1999 {published data only}
- Fynes M, Marshall K, Cassidy M, O'Connell R, O'Herlihy C. A prospective randomised study comparing the effect of augmented biofeedback with sensory biofeedback alone on faecal incontinence following obstetric trauma. Proceedings of the International Continence Society (ICS), 28th Annual Meeting, 1998 Sep 14‐17, Jerusalem, Israel 1998:151.
- Fynes MM, Marshall K, Cassidy M, Behan M, Walsh D, O'Connell PR, et al. A prospective, randomized study comparing the effect of augmented biofeedback with sensory biofeedback alone on fecal incontinence after obstetric trauma. Diseases of the Colon & Rectum 1999;42(6):753‐61. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Healy 2006 {published data only}
- Healy CF, Brannigan AE, Connolly EM, Eng M, O'sullivan MJ, McNamara DA, et al. The effects of low‐frequency endo‐anal electrical stimulation on faecal incontinence: a prospective study. International Journal of Colorectal Disease 2006;21(8):802‐6. [DOI] [PubMed] [Google Scholar]
Heymen 2000 {published data only}
- Heymen S, Pikarsky AJ, Weiss EG, Vickers D, Nogueras JJ, Wexner SD. A prospective randomized trial comparing four biofeedback techniques for patients with faecal incontinence. Colorectal Disease 2000;2(2):88‐92. [DOI] [PubMed] [Google Scholar]
Heymen 2009 {published data only}
- Heymen S, Scarlett Y, Jones K, Ringel Y, Drossman D, Whitehead WE. Randomized controlled trial shows biofeedback to be superior to pelvic floor exercises for fecal incontinence. Diseases of the Colon & Rectum 2009;52(10):1730‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hinninghofen 2003 {published data only}
- Hinninghofen H, Wietek B, Jehle EC, Enck P. [Quality of life in patients with incontinence of faeces: Bio‐feedback training versus surgical measures] (Abstract number P103). Zeitschrift fur Gastroenterologie 2003;41(8):783. [Google Scholar]
Ilnyckyj 2005 {published data only}
- Ilnyckyj A, Fachnie E, Tougas G. A randomized‐controlled trial comparing an educational intervention alone vs education and biofeedback in the management of faecal incontinence in women. Neurogastroenterology and Motility 2005;17(1):58‐63. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Latimer 1984 {published data only}
- Latimer PR, Campbell D, Kasperski J. A components analysis of biofeedback in the treatment of fecal incontinence. Biofeedback and Self‐Regulation 1984;9(3):311‐24. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mahony 2004 {published data only}
- Mahony R, Malone P, Nalty J, Cassidy M, O'Connell PR, O'Herlihy C. Prospective randomized comparison of intra‐anal electromyographic biofeedback and intra‐anal electromyographic biofeedback augmented with electrical stimulation of the anal sphincter. [Miscellaneous]. American Journal of Obstetrics and Gynecology 2003;189(6):S71. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Mahony RT, Malone PA, Nalty J, Behan M, O'Connell PR, O'Herlihy C. Randomized clinical trial of intra‐anal electromyographic biofeedback physiotherapy with intra‐anal electromyographic biofeedback augmented with electrical stimulation of the anal sphincter in the early treatment of postpartum fecal incontinence. American Journal of Obstetrics and Gynecology 2004;191(3):885‐90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Markwell 2006 {published data only}
- Markwell S, Unkles E, Hitchman K, Lincoln D, Chumbley J, Theile G, et al. A randomised controlled clinical trial to evaluate the efficacy of specific muscle rehabilitation in people with faecal incontinence (report amended Jun 2007). Canberra, Australia: Department of Health and Ageing, Australian Government, 2006. Available from: http://www.bladderbowel.gov.au/ncp/ncms/projects/phases/intervention/musclerehabilitation.htm (last accessed 9 May 2012). [Google Scholar]
McHugh 1986 {published data only}
- Diamant NE. personal communication 1999.
- McHugh S, Walma K, Diamant NE. Faecal incontinence: a controlled trial of biofeedback. Gastroenterology 1986;90:1545. [Google Scholar]
Miner 1990 {published data only}
- Miner PB, Donnelly TC, Read NW. Investigation of mode of action of biofeedback in treatment of fecal incontinence. Digestive Diseases and Sciences 1990;35(10):1291‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Naimy 2007 {published data only}
- Naimy N, Lindam AT, Bakka A, Faerden AE, Wiik P, Carlsen E, et al. Biofeedback vs. electrostimulation in the treatment of postdelivery anal incontinence: a randomized, clinical trial. Diseases of the Colon & Rectum 2007;50(12):2040‐6. [DOI] [PubMed] [Google Scholar]
Norton 2003 {published data only}
- Norton C, Chelvanayagam S, Kamm M. Randomised controlled trial of biofeedback for faecal incontinence (Abstract). Neurourology and Urodynamics 2002;21(4):295‐6. [MEDLINE: ] [Google Scholar]
- Norton C, Chelvanayagam S, Wilson‐Barnett J, Redfern S, Kamm MA. Randomized controlled trial of biofeedback for fecal incontinence.[see comment]. Gastroenterology 2003;125(5):1320‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schwandner 2010 {published data only}
- Schwandner T, Konig IR, Heimerl T, Kierer W, Roblick M, Bouchard R, et al. Triple target treatment (3T) is more effective than biofeedback alone for anal incontinence: the 3T‐AI study. Diseases of the Colon & Rectum 2010;53(7):1007‐16. [DOI] [PubMed] [Google Scholar]
Schwandner 2011 {published data only}
- Schwandner T, Hemmelmann C, Heimerl T, Kierer W, Kolbert G, Vonthein R, et al. Triple‐target treatment versus low‐frequency electrostimulation for anal incontinence: a randomized, controlled trial. Deutsches Arzteblatt International 2011;108(39):653‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Solomon 2003 {published data only}
- Solomon MJ, Pager CK, Rex J, Roberts R, Manning J. Randomized, controlled trial of biofeedback with anal manometry, transanal ultrasound, or pelvic floor retraining with digital guidance alone in the treatment of mild to moderate fecal incontinence. Diseases of the Colon & Rectum 2003;46(6):703‐10. [DOI] [PubMed] [Google Scholar]
Tjandra 2008 {published data only}
- Tjandra J, Lim J, Green C, Carey M. Sacral neuromodulation in patients with faecal incontinence: a randomized controlled study on efficacy and quality of life. Colorectal Disease 2005;7 Suppl 1:31. [Google Scholar]
- Tjandra JJ, Chan MK, Yeh CH, Murray‐Green C. Sacral nerve stimulation is more effective than optimal medical therapy for severe fecal incontinence: a randomized, controlled study. Diseases of the Colon & Rectum 2008;51(5):494‐502. [DOI] [PubMed] [Google Scholar]
Whitehead 1985 {published data only}
- Whitehead WE. personal communication 1999.
- Whitehead WE, Burgio KL, Engel BT. Biofeedback treatment of fecal incontinence in geriatric patients. Journal of the American Geriatrics Society 1985;33(5):320‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bates‐Jensen 2003 {published data only}
- Bates‐Jensen BM, Alessi CA, Al Samarrai NR, Schnelle JF. The effects of an exercise and incontinence intervention on skin health outcomes in nursing home residents. Journal of the American Geriatrics Society 2003;51(3):348‐55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Byrne 2002 {published data only}
- Byrne CM, Pager CK, Rex J, Roberts R, Solomon MJ. Assessment of quality of life in the treatment of patients with neuropathic fecal incontinence. Diseases of the Colon & Rectum 2002;45(11):1431‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Chase 2004 {published data only}
- Chase J, Sherburn M, Button B. Development of intervention and education program for incontinence in adult women with chronic obstructive pulmonary disease (COPD) and cystic fibrosis. Project 34. Canberra, Australia: Department of Health and Ageing, Australian Government, 2004. Available from: http://www.bladderbowel.gov.au/ncp/ncms/projects/phases/intervention/incontcopdcf.htm (last accessed 9 May 2012). [Google Scholar]
Christensen 2009 {published data only}
- Christensen P, Andreasen J, Ehlers L. Cost‐effectiveness of transanal irrigation versus conservative bowel management for spinal cord injury patients. Spinal Cord 2009;47(2):138‐43. [DOI] [PubMed] [Google Scholar]
Cox 1996 {published data only}
- Cox DJ, Sutphen J, Ling W, Quillian W, Borowitz S. Additive benefits of laxative, toilet training, and biofeedback therapies in the treatment of childhood encopresis. Journal of Pediatric Psychology 1996;21(5):659‐70. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Cox 2003 {published data only}
- Cox DJ, Lucas V, Ritterband LM, Borowitz S, Sutphen J, Kovatchev B, et al. Internet‐based treatment of early childhood fecal incontinence. metaRegister of Controlled Trials 2003.
Croffie 2005 {published data only}
- Croffie JM, Ammar MS, Pfefferkorn MD, Horn D, Klipsch A, Fitzgerald JF, et al. Assessment of the effectiveness of biofeedback in children with dyssynergic defecation and recalcitrant constipation/encopresis: does home biofeedback improve long‐term outcomes. Clinical Pediatrics 2005;44(1):63‐71. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Dannecker 2004 {published data only}
- Dannecker C. [The effect of the pelvic floor training device Epi‐No on the maternal pelvic floor function six months after childbirth ‐ follow‐up study of a randomised controlled trial]. Geburtshilfe und Frauenheilkunde 2004;64(11):1192‐8. [MEDLINE: ] [Google Scholar]
Enck 1994 {published data only}
- Enck P, Daublin G, Lubke HJ, Strohmeyer G. Long‐term efficacy of biofeedback training for faecal incontinence. Diseases of the Colon & Rectum 1994;37(10):997‐1001. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Fang 2003 {published data only}
- Fang Y, Chen X, Li H, Lin J, Huang R, Zeng J. A study on additional early physiotherapy after stroke and factors affecting functional recovery. Clinical Rehabilitation 2003;17(6):608‐17. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Gaier 2010 {published data only}
- Gaier L, Lamberti G, Giraudo D. Pelvic floor muscle training during pregnancy to prevent urinary pelvic floor dysfunctions (Abstract). Neurourology and Urodynamics 2010;29(2S):64‐5. [Google Scholar]
Glazener 2005 {published data only}
- Glazener CM, Herbison GP, MacArthur C, Grant A, Wilson PD. Randomised controlled trial of conservative management of postnatal urinary and faecal incontinence: six year follow up. BMJ 12‐2‐2005;330(7487):337‐40. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glazener CM, Herbison GP, Wilson PD, MacArthur C, Lang GD, Gee H, et al. Conservative management of persistent postnatal urinary and faecal incontinence: randomised controlled trial. BMJ 2001;323(7313):593‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glazener CM, Herbison GP, Wilson PD, MacArthur C, Lang GD, Gee H, et al. Conservative management of persistent postnatal urinary and faecal incontinence: randomised controlled trial [Extended electronic version]. eBMJ 2001;323:1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson PD, Glazener C, McGee M, Herbison P, MacArthur C, Grant A. Randomised controlled trial of conservative management of postnatal urinary and faecal incontinence: long term follow‐up study (Abstract). Neurourology and Urodynamics 2002;21(4):370. [Google Scholar]
Gouldthorpe {published data only}
- Gouldthorpe H. QA physiotherapy abdominal muscle assessment during and after pregnancy: Part 4 (Abstract). Australian and New Zealand Continence Journal YR:2003. 9 Vol. 9, issue 4:92. [MEDLINE: ]
Harari 2004 {published data only}
- Harari D, Norton C, Lockwood L, Swift C. Treatment of constipation and fecal incontinence in stroke patients: randomized controlled trial. Stroke 2004;35(11):2549‐55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Heymen 2003 {published data only}
- Heymen S, Whitehead WE, Scarlett Y. Elevated Beck Depression Inventory (BDI) scores predict biofeedback treatment failure for fecal incontinence and constipation (Abstract number W1511). Gastroenterology 2003;124(4 (Suppl 1)):A685. [Google Scholar]
Heymen 2004 {published data only}
- Heymen S, Scarlett Y, Whitehead WE. Anorectal physiology predicts response to conservative medical management of fecal incontinence (Abstract). Gastroenterology 2004;126(4 (Suppl 2)):A363. [DOI] [PubMed] [Google Scholar]
Heymen 2004a {published data only}
- Heymen S, Scarlett Y, Whitehead WE. Education and medical management resolve fecal incontinence in 35%, but depression and greater symptom severity predict a poor response (Abstract). Gastroenterology 2004;126(4 (Suppl 2)):A480. [Google Scholar]
Heymen 2005 {published data only}
- Heymen S, Scarlett Y, Jones K, Drossman D, Ringel Y, Whitehead WE. Randomized controlled trial shows biofeedback to be superior to alternative treatments for patients with pelvic floor dyssenergia‐type constipation (Abstract number S1838). Gastroenterology 2005;128 Suppl 2:A266. [DOI] [PubMed] [Google Scholar]
Jorge 1994 {published data only}
- Jorge JM, Wexner SD, Morgado PJ, James K, Nogueras JJ, Jagelman DG. Optimization of sphincter function after the ileoanal reservoir procedure. Diseases of the Colon & Rectum 1994;37(5):419‐23. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Klijn 2003 {published data only}
- Klijn AJ, Winkler‐Seinstra PL, Vijverberg MA, Uiterwaal CS, Jong TP. Results of behavioral therapy combined with homeflow biofeedback for non‐neuropathic bladder sphincter dysfunction, a prospective randomized study in 143 patients (Abstract). Proceedings of the International Continence Society (ICS), 33rd Annual Meeting, 5‐9 Oct, Florence. 2003:176‐7.
Leroi 2005 {published data only}
- Leroi AM, Parc Y, Lehur PA, Mion F, Barth X, Rullier E, et al. Efficacy of sacral nerve stimulation for fecal incontinence: results of a multicenter double‐blind crossover study. Annals of Surgery 2005;242(5):662‐9. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Levy‐Storms 2007 {published data only}
- Levy‐Storms L, Schnelle JF, Simmons SF. What do family members notice following an intervention to improve mobility and incontinence care for nursing home residents? An analysis of open‐ended comments. Gerontologist 2007;47(1):14‐20. [DOI] [PubMed] [Google Scholar]
Loening‐Baucke 1988 {published data only}
- Loening‐Baucke V, Desch L, Wolraich M. Biofeedback training for patients with myelomeningocele and faecal incontinence. Developmental Medicine and Child Neurology 1988;30(6):781‐90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Loening‐Baucke 1990a {published data only}
- Loening‐Baucke V. Biofeedback therapy for faecal incontinence. Digestive Diseases 1990;8(2):112‐24. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Loening‐Baucke 1990b {published data only}
- Loening‐Baucke V. Efficacy of biofeedback training in improving faecal incontinence and anorectal physiologic function. Gut 1990;31(12):1395‐402. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Loening‐Baucke 1995 {published data only}
- Loening‐Baucke V. Biofeedback treatment for chronic constipation and encopresis in childhood: long‐term outcome. Pediatrics 1995;96(1):105‐10. [MEDLINE: ] [PubMed] [Google Scholar]
Markland 2009 {published data only}
- Markland AD, Richter HE, Burgio KL, Bragg C, Hernandez AL, Subak LL. Fecal incontinence in obese women with urinary incontinence: prevalence and role of dietary fiber intake. American Journal of Obstetrics and Gynecology. 2009;200(5):566.e1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mathew 2004 {published data only}
- Mathew R. A phase III, multicentre, single blind, randomised controlled trial in the use of hyperbaric oxygen therapy versus biofeedback therapy in patients with chronic faecal incontinence associated with pudendal neuropathy. metaRegister of Controlled Trials 2004.
Norton 2006 {published data only}
- Norton C, Gibbs A, Kamm M. A randomised controlled trial of anal electrical stimulation for faecal incontinence (Abstract number 474). Proceedings of the 35th Annual International Continence Society (ICS), 28 Aug ‐ 2 Sept, Montreal. 2005. [MEDLINE: ]
- Norton C, Gibbs A, Kamm MA. Randomized, controlled trial of anal electrical stimulation for fecal incontinence. Diseases of the Colon & Rectum 2006;49(2):190‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
O'Brien 2005 {published data only}
- O'Brien PE, Dixon JB, Skinner S, Laurie C, Khera A, Fonda D. A prospective randomised controlled clinical trial of placement of the artificial bowel sphincter (Acticon). Australia: National Continence Management Strategy, Department of Health and Ageing, Australian Government, 2005. [Google Scholar]
- O'Brien PE, Dixon JB, Skinner S, Laurie C, Khera A, Fonda D. A prospective, randomized, controlled clinical trial of placement of the artificial bowel sphincter (Acticon Neosphincter) for the control of fecal incontinence. Diseases of the Colon & Rectum 2004;47(11):1852‐60. [DOI] [PubMed] [Google Scholar]
Oresland 1988 {published data only}
- Oresland T, Fasth S, Hulten L, Nordgren S, Swenson L, Akervall S. Does balloon dilatation and anal sphincter training improve ileo‐ anal pouch function?. International Journal of Colorectal Disease 1988;3(3):153‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Osterberg 2004 {published data only}
- Osterberg A, Edebol Eeg‐Olofsson K, Hallden M, Graf W. Randomized clinical trial comparing conservative and surgical treatment of neurogenic faecal incontinence. British Journal of Surgery 2004;91(9):1131‐7. [DOI] [PubMed] [Google Scholar]
Pager 2002 {published data only}
- Pager CK, Solomon MJ, Rex J, Roberts RA. Long‐term outcomes of pelvic floor exercise and biofeedback treatment for patients with fecal incontinence. Diseases of the Colon & Rectum 2002;45(8):997‐1003. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Pourmomeny 2011 {published data only}
- Pourmomeny AA, Emami MH, Amooshahi M, Adibi P. Comparing the efficacy of biofeedback and balloon‐assisted training in the treatment of dyssynergic defecation. Canadian Journal of Gastroenterology 2011;25(2):89‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Powell 2003 {published data only}
- Powell M. Augmented biofeedback and sensory biofeedback in faecal incontinence: a pilot study (Abstract). Australian and New Zealand Continence Journal 2003;9(4):77‐8. [Google Scholar]
Richter 2011 {published data only}
- Richter HE. Behavioral therapy versus usual care in primiparous women with anal sphincter tears and fecal incontinence: a randomized trial. www.ClinicalTrials.gov [accessed 16 September 2011] 2011.
Ritterband 2003 {published data only}
- Ritterband LM, Cox DJ, Walker LS, Kovatchev B, McKnight L, Patel K, Borowitz S, Sutphen J. An Internet intervention as adjunctive therapy for pediatric encopresis. Journal of Consulting & Clinical Psychology 2003;71(5):910‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Roth 1999 {published data only}
- Roth I, Hasse C, Bohrer T, Stinner B, Rothmund M. Dynamic threshold current therapy ‐ a new method for tonizing the striated musculature of the pelvic floor for anorectal incontinence [abstract number O7]. Langenbeck's Archiv fur Chirurgie/Deutsche Gesellschaft fur Chirurgie 1999;384(5):496. [Google Scholar]
Schnelle 2002 {published data only}
- Schnelle JF, Alessi CA, Simmons SF, Al Samarrai NR, Beck JC, Ouslander JG. Translating clinical research into practice: a randomized controlled trial of exercise and incontinence care with nursing home residents.[comment]. Journal of the American Geriatrics Society 2002;50(9):1476‐83. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schnelle 2003 {published data only}
- Schnelle JF, Kapur K, Alessi C, Osterweil D, Beck JG, Al Samarrai NR, et al. Does an exercise and incontinence intervention save healthcare costs in a nursing home population?[comment]. Journal of the American Geriatrics Society 2003;51(2):161‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Simmons 2005 {published data only}
- Simmons SF, Ouslander JG. Resident and family satisfaction with incontinence and mobility care: sensitivity to intervention effects?. Gerontologist 2005;45(3):318‐26. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Simmons SF, Schnelle JF. Effects of an exercise and scheduled‐toileting intervention on appetite and constipation in nursing home residents. Journal of Nutrition, Health & Aging 2004;8(2):116‐21. [MEDLINE: ] [PubMed] [Google Scholar]
Solomon 2000 {published data only}
- Solomon M, Rex J, Manning J, Eyers A, Stewart P, Roberts R. Randomised controlled trial of biofeedback (manometry vs transanal US) compared with pelvic floor exercises for faecal incontinence (Abstract). Australian and New Zealand Journal of Surgery 2000;70(Suppl May):A56. [MEDLINE: ] [Google Scholar]
- Solomon MJ, Rex J, Eyers AA, Stewart P, Roberts R. Biofeedback for fecal incontinence using transanal ultrasonography: novel approach. Diseases of the Colon & Rectum 2000;43(6):788‐92. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Surh 1998 {published data only}
- Surh S, Kienle P, Stern J, Herfarth C. [Passive electrostimulation therapy of the anal sphincter is inferior to active biofeedback training]. [German] [Die passive Elektrostimulationstherapie des Analsphinkters ist dem aktiven Biofeedbacktraining unterlegen]. Langenbecks Archiv fur Chirurgie ‐ Supplement ‐ Kongressband 1998;115:976‐8. [MEDLINE: ] [PubMed] [Google Scholar]
Tekeoglu 1998 {published data only}
- Tekeoglu Y, Adak B, Goksoy T. Effect of transcutaneous electrical nerve stimulation (TENS) on Barthel Activities of Daily Living (ADL) index score following stroke. Clinical Rehabilitation 1998;12(4):277‐80. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
van der Plas 1996a {published data only}
- Plas RN, Benninga MA, Buller HA, Bossuyt PM, Akkermans LM, Redekop WK, et al. Biofeedback training in treatment of childhood constipation: a randomised controlled study. Lancet 1996;348(9030):776‐80. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
van der Plas 1996b {published data only}
- Plas RN, Benninga MA, Redekop WK, Taminiau JA, Buller HA. Randomised trial of biofeedback training for encopresis. Archives of Disease in Childhood 1996;75(5):367‐74. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wald 1984 {published data only}
- Wald A, Tunuguntla AK. Anorectal sensorimotor dysfunction in faecal incontinence in diabetes mellitus. New England Journal of Medicine 1984;310(20):1282‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wald 1987 {published data only}
- Wald A, Chandra R, Gabel S, Chiponis D. Evaluation of biofeedback in childhood encopresis. Journal of Pediatric Gastroenterology and Nutrition 1987;6(4):554‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Whitehead 1986 {published data only}
- Whitehead WE, Parker L, Bosmajian L, Morrill‐Corbin ED, Middaugh S, Garwood M, et al. Treatment of fecal incontinence in children with spina bifida: comparison of biofeedback and behavior modification. Archives of Physical Medicine and Rehabilitation 1986;67:218‐24. [MEDLINE: ] [PubMed] [Google Scholar]
References to studies awaiting assessment
Marshall 1995 {published data only}
- Marshall K, Donnelly VS, O'Herlihy C, Walsh DM. Effectiveness of physiotherapy in the management of post‐partum faecal incontinence (Abstract number 195). Proceedings of the International Continence Society (ICS), 25th Annual Meeting, 1995 Oct 17‐20, Sydney, Australia 1995:193‐4.
Pages 2003 {published data only}
- Pages I‐H, Lemke J, Grundel K. Comparison of biofeedback and electrostimulation for treatment of fecal incontinence [German]. Physikalische Medizin Rehabilitationsmedizin Kurortmedizin 2003;13(6):325‐9. [Google Scholar]
References to ongoing studies
Dehli 2009 {published data only}
- Dehli T, Vonen B, Stordahl A, Jacobsen A, Lindsetmo RO, Mevik K. A randomized, controlled, clinical trial of biofeedback and anal injections as first treatment of fecal incontinence. ControlledTrials.com (www.controlled‐trials.com) [accessed 2 February 2009] 2009.
Stott 2000 {published data only}
- Stott S. A study to determine the effects of neuro‐stimulation on anal sphincter function when used in conjunction with biofeedback and pelvic floor exercises in the treatment of faecal incontinence. [personal communication] 2000.
Additional references
Boreham 2005
- Boreham MK, Richter HE, Kenton KS, Nager CW, Gregory WT, Aronson MP, et al. Anal incontinence in women presenting for gynecologic care: prevalence, risk factors, and impact upon quality of life. American Journal of Obstetrics and Gynecology 2005;192(5):1637‐42. [DOI] [PubMed] [Google Scholar]
Brown 2010
- Brown SR, Wadhawan H, Nelson RL. Surgery for faecal incontinence in adults. Cochrane Database of Systematic Reviews 2010, Issue 9. [DOI: 10.1002/14651858.CD001757.pub3] [DOI] [PubMed] [Google Scholar]
Cheetham 2002
- Cheetham MJ, Brazzelli M, Norton CC, Glazener CMA. Drug treatment for faecal incontinence in adults. Cochrane Database of Systematic Reviews 2002, Issue 3. [DOI: 10.1002/14651858.CD002116] [DOI] [PubMed] [Google Scholar]
Cotterill 2011
- Cotterill N, Norton C, Avery KN, Abrams P, Donovan JL. Psychometric evaluation of a new patient‐completed questionnaire for evaluating anal incontinence symptoms and impact on quality of life: the ICIQ‐B. Diseases of the Colon & Rectum 2011;54(10):1235‐50. [DOI] [PubMed] [Google Scholar]
Dumoulin 2010
- Dumoulin C, Hay‐Smith J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD005654.pub2] [DOI] [PubMed] [Google Scholar]
Engel 1974
- Engel BT, Nikoomanesh P, Schuster MM. Operant conditioning of rectosphincteric responses in the treatment of faecal incontinence. New England Journal of Medicine 1974;290(12):646‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Heymen 2001
- Heymen S, Jones KR, Ringel Y, Scarlett Y, Whitehead WE. Biofeedback treatment of fecal incontinence: a critical review. Diseases of the Colon & Rectum 2001;44(5):728‐36. [DOI] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011b
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hosker 2007
- Hosker G, Cody JD, Norton CC. Electrical stimulation for faecal incontinence in adults. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD001310.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Johanson 1996
- Johanson JF, Lafferty J. Epidemiology of faecal incontinence: the silent affliction. American Journal of Gastroenterology 1996;91(1):33‐6. [MEDLINE: ] [PubMed] [Google Scholar]
Kegel 1948
- Kegel A. Progressive resistance exercise in the functional restoration of the perineal muscles. American Journal of Obstetrics and Gynecology 1948;56:242‐5. [DOI] [PubMed] [Google Scholar]
Madoff 2009
- Madoff RD, Laurberg S, Matzel KE, Mellgren AF, Mimura T, O'Connell PR, et al. Surgery for faecal incontinence. In: Abrams P, Cardozo L, Khoury S, Wein A editor(s). Incontinence: 4th International Consultation on Incontinence, Paris July 5‐8, 2008. Plymouth, UK: Health Publication Ltd, 2009:1387‐418. [Google Scholar]
Norton 2001
- Norton C, Kamm MA. Anal sphincter biofeedback and pelvic floor exercises for faecal incontinence in adults ‐ a systematic review. Alimentary Pharmacology & Therapeutics 2001;15:1147‐54. [DOI] [PubMed] [Google Scholar]
Norton 2004
- Norton C, Chelvanayagam S. Bowel Continence Nursing. Beaconsfield: Beaconsfield Publishers, 2004. [Google Scholar]
Norton 2009
- Norton C, Whitehead W, Bliss DZ, Harari D, Lang J. Conservative and pharmacological management of faecal incontinence in adults. In: Abrams P, Cardozo L, Khoury S, Wein A editor(s). Incontinence: 4th International Consultation on Incontinence, Paris July 5‐8, 2008. Plymouth, UK: Health Publication Ltd, 2009:1321‐86. [Google Scholar]
Perry 2002
- Perry S, Shaw C, McGrother C, Flynn RJ, Assassa RP, Dallosso H, et al. The prevalence of faecal incontinence in adults aged 40 years or more living in the community. Gut 2002;50:480‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Potter 2002
- Potter J, Norton C, Cottenden A. Bowel care in older people. London: Royal College of Physicians, 2002. [Google Scholar]
Rao 2004
- Rao SS. Pathophysiology of adult fecal incontinence. Gastroenterology 2004;126(1 Suppl 1):S14‐S22. [DOI] [PubMed] [Google Scholar]
Rockwood 1999
- Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG, et al. Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the fecal incontinence severity index. Disease of the Colon & Rectum 1999;42:1525‐32. [DOI] [PubMed] [Google Scholar]
Rockwood 2000
- Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG, et al. Fecal incontinence quality of life scale. Diseases of the Colon & Rectum 2000;43:9‐17. [DOI] [PubMed] [Google Scholar]
Thompson 1999
- Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Muller‐Lissner SA. Functional bowel disorders and functional abdominal pain. Gut 1999;45 Suppl 11:1143‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tuteja 2004
- Tuteja AK, Rao SS. Review article: recent trends in diagnosis and treatment of faecal incontinence. Alimentary Pharmacology & Therapeutics 2004;19(8):829‐40. [DOI] [PubMed] [Google Scholar]
van Tets 1996
- Tets WF, Kuijpers JH, Bleijenberg G. Biofeedback treatment is ineffective in neurogenic fecal incontinence. Disease of the Colon & Rectum 1996;39(9):992‐4. [DOI] [PubMed] [Google Scholar]
Wade 1988
- Wade DT, Collin C. The Barthel ADL Index: a standard measure of physical disability?. International Disability Studies 1988;10(2):64‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ware 1993
- Ware JE, Snow KK, Kosinski M, Gaudek B. SF‐36 Health Survey Manual and Interpretation Guide. Boston: New England Medical Centre, 1993. [Google Scholar]
Weinstein 1977
- Weinstein MC, Statson WB. Foundations of cost‐effectiveness analysis for health and medical practices. New England Journal of Medicine 1977;296(13):716‐21. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Whitehead 1981
- Whitehead WE, Orr WC, Engel BT, Schuster MM. External anal sphincter response to rectal distension: learned response or reflex. Psychophysiology 1981;19(1):57‐62. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Whitehead 2001
- Whitehead WE, Wald A, Norton N. Treatment options for fecal incontinence: consensus conference report. Diseases of the Colon & Rectum 2001;44:131‐44. [DOI] [PubMed] [Google Scholar]
Whitehead 2009
- Whitehead WE, Borrud L, Goode PS, Meikle S, Mueller ER, Tuteja A, et al. Fecal incontinence in US adults: epidemiology and risk factors. Gastroenterology 2009;137(2):512‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2007
- Wilson M. The impact of faecal incontinence on the quality of life. British Journal of Nursing 2007;16(4):204‐7. [DOI] [PubMed] [Google Scholar]
Zigmond 1983
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica 1983;67(6):361‐70. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]


