Abstract
Background
Although only a few patients with severe mental disorders (SMD) can commit violent behaviour in the community, violent behaviour aggravates the stigma towards patients with SMD. Understanding the subtypes of violent behaviour may be beneficial for preventing violent behaviour among patients with SMD, but it has rarely been studied.
Methods
This longitudinal study investigated 1914 patients with SMD in the community at baseline, and the follow-up period ranged from February 2021 to August 2021. The Barratt Impulsiveness Scale Version-11, the Buss-Perry Aggression Questionnaire, the Impulsive/Premeditated Aggression Scale, the Personality Diagnostic Questionnaire and the MacArthur Community Violence Instrument were used at baseline. The Modified Overt Aggression Scale was used to assess the occurrence of violent behaviour (outcome) during the follow-up period. Cox regression models were used to calculate hazard ratios (HRs) with 95% confidence intervals (CIs). Latent class analysis was used to characterise the subtypes of patients with SMD who engaged in violent behaviour at follow-up.
Results
We found that 7.2% of patients with SMD presented violent behaviour within six months in the community. Younger age (OR = 0.98, 95% CI = 0.96-1.00, p = 0.016) and no economic source (OR = 1.60, 95% CI = 1.10–2.33, p = 0.014) were risk factors for violent behaviour. Patients with SMD who engaged in violent behaviour could be classified into three subtypes: one class characterised by a history of violence and impulsivity, another class characterised by high levels of aggression and motor impulsivity, and the last class characterised by median cognitive impulsivity.
Conclusions
Socio-demographic factors were risk factors for violent behaviour among patients with SMD, which could eliminate the discrimination toward this group. Impulsivity played a vital role in identifying the three subtypes of patients with SMD who engaged in violent behaviour. These findings may be helpful for the development of a personalised violence risk management plan for patients with SMD who commit violent behaviour in the community.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12888-024-06044-z.
Keywords: Severe mental disorder, Violent behaviour, Aggression, Impulsivity, Latent class analysis
Background
Violence is one of the main negative outcomes of mental disorders, and it has been the focus of psychiatry, public health and policy fields for decades [1]. Although only a few patients with mental disorders engage in violent behaviour, the elevated risk of violence has led this group to experience more stigma [2, 3], which leads to enormous negative effects on society, with a total social cost of £2.5 billion annually [4]. To decrease the risk of violence among patients with mental disorders, violence risk management has always been the key point of community mental health service (CMHS) in China. The CMHS manages severe mental disorders (SMD), including six diagnoses: schizophrenia, schizoaffective disorder, delusional disorder, bipolar disorder, psychotic disorder due to epilepsy, and mental retardation with mental disorders [5]. The “686 Project” and the National Basic Public Health Services were launched in 2004 and 2009, respectively [6, 7]. However, the lack of objective evidence has always been an obstacle to improving the effectiveness of violence risk management in CMHS.
Although the MacArthur Violence Risk Assessment Study revealed that psychiatric symptoms did not increase the risk of violence among patients with mental disorders [8], several meta-analyses have shown that different mental disorders, such as schizophrenia, personality disorder and bipolar disorder, increased the risk of violence to different degrees [9]. These various findings were attributed to the heterogeneity of violent behaviour, which includes many subtypes. According to the objective, violence may be classified into violence to others, violence to oneself, etc., according to the form, violence may be classified into verbal and physical violence, etc., and according to the cause, violence may be classified into impulsive and premeditated violence [10, 11]. However, the first and second classifications are based on the characteristics of violence, which makes it difficult to provide evidence for violence risk management. The last classification, which may provide valuable information for violence risk management still needs a profile to expand the understanding of mental disorders among patients with mental disorders [12]. Therefore, it is necessary to analyse the subtypes of violence among patients with mental disorders.
A retrospective study using latent class analysis (LCA) revealed that schizophrenia may be divided into three subgroups on the basis of the associations of psychotic symptoms, alcohol and drug intoxication with violence, psychopathic traits, and impulsivity [13]. Another study divided offenders with SMD who were released from prisons and forensic psychiatric hospitals into psychotic, repetitive, institutional and less violent subtypes [14]. However, these studies focused on patients receiving compulsory medical treatment or who were released into the community shortly after treatment, and they may not be suitable for the violence risk management of patients with mental disorders in the community. Furthermore, none of these studies were longitudinal studies, and longitudinal studies could provide more robust evidence for the violence risk management of patients with SMD in the community.
Prior studies in Western countries have established that several risk factors, such as younger age, male sex, and substance use, escalate the risk of violent behaviour among patients with mental disorders [12, 15], but the risk factors may vary in China, because China has different legal systems and social national conditions [16]. Furthermore, our previous research revealed that substance use, which is a powerful predictor of violence among patients with schizophrenia in Western countries, rarely occurred in patients with schizophrenia allegedly homicide offenders in China [17], because substance use is an illegal behaviour in China, and the Chinese government has a strict anti-drug policy [18].
In addition, many studies focusing on violence used a cross-sectional study design in China [19–21]. Only a few longitudinal studies focused on the risk factors for violence among patients with SMD in Chinese communities. A three-year follow-up study in Hong Kong revealed that previous violence, male sex and low education significantly increased the risk of violence among young patients presenting with first-episode psychosis [22]. Therefore, performing a longitudinal study to explore the risk factors for violent behaviour among patients with SMD in the community of China is essential.
Given this background, the present study aimed to: (1) identify the risk factors for violent behaviour among patients with SMD and (2) explore the subtypes of SMD patients engaged in violent behaviour during the follow-up period and present the characteristics of different subtypes. These findings may be helpful for developing targeted violence risk management for patients with SMD committing violent behaviour in the community.
Methods
Participants and procedure
The participants included 1914 patients with SMD who were registered in the Chengdu Mental Health Prevention and Management System in the community, and were between 18 and 65 years old (mean = 44.6, SD = 11.0). The following inclusion were used: (1) diagnosed with any of six severe mental disorders, including schizophrenia, schizoaffective disorder, delusional disorder, bipolar disorder, psychotic disorder due to epilepsy, and mental retardation with mental disorders; (2) aged between 18 and 65 years; and (3) registered in the Chengdu Mental Health Prevention and Management System. The following exclusion criteria were used: (1) unwillingness to accept community health management services; (2) failure to visit the management system; (3) unwillingness to participate in the questionnaire survey; and (4) documented substance use disorders.
The baseline survey was performed in February 2021. Social and demographic information, such as gender, age, and source of income, was collected from the Chengdu Mental Health Prevention Management System. Self-report questionnaires were used to assess aggression, impulsivity and antisocial personality disorder (ASPD) characteristics. The self-evaluation scale was completed by the patient using a mobile phone at the community health service centre. The community mental health prevention personnel filled out the other questionnaires by combining the information of the Chengdu Mental Health Prevention Management System and interview information (face to face or telephone interviews). The follow-up survey was performed in August 2021 to assess whether the participants committed violent behaviour during the follow-up period. The violent behaviour (outcome) at follow-up was identified according to the score of the Modified Overt Aggression Scale (MOAS). Participants who scored above 0 according to their behaviour in the follow-up period were identified as positive; otherwise, they were identified as negative.
Measures
General information questionnaire
The demographic data, including age, gender, educational level, marital status, employment status, and economic source, were obtained from the Chengdu Mental Health Prevention and Management System. No economic source was defined as the absence of all forms of economic income except subsidies from governmental or non-governmental agencies, including work earnings and economic support from families. Child maltreatment was identified by asking “Have you experienced abuse/neglect before the age of 16, or do you have no fixed and continuous caregivers (this only requires stable caregivers, who can be grandparents or someone having no blood relationship with the patient)”. The participants were classified as having experienced child abuse if they answered “Yes”.
The modified overt aggression scale
The Modified Overt Aggression Scale (MOAS) was used to assess the severity of violence (outcome) after six months of follow-up. The MOAS consists of four subscales: verbal aggression (VA), aggression against property (AAP), self-aggression (SA) and physical aggression (PA) [23]. The intraclass correlation coefficients were 0.90, 0.56, 0.49, and 0.90 for VA, AAP, SA and PA, respectively [24]. The score of each item ranges from 0 to 4, with “0” indicating no aggression and higher scores representing more severe levels of aggression. A weighted score was calculated for each subscale, and the weighted sums of each subscale were added together to obtain the total score [25]. If a participant was scored 0, he or she belonged to the non-violent group, and if the participant was scored above 0, he or she belonged to the violent group.
The MacArthur community violence instrument
The MacArthur Community Violence Instrument (MCVI) was used to evaluate whether participants had a history of violent behaviour: (1) battery acts whether or not physical injury was involved, (2) assaultive acts involving the use of a weapon or threats with a weapon, and (3) sexual assault [26, 27]. The act of any of the above behaviours was identified as having a history of violence.
The Buss-Perry aggression questionnaire
The Buss-Perry Aggression Questionnaire (BPAQ), a self-questionnaire was used to evaluate the characteristics of aggression. It is a four-factor structure scale that includes physical aggression, verbal aggression, anger, and hostility [28]. Each item is scored on a 5-point Likert-type scale: 1 (extremely untypical of me) to 5 (extremely typical of me). Higher total scores on the scale indicated more aggressive behaviour. The Cronbach’s α coefficients of the physical aggression, verbal aggression, anger, and hostility subscales were 0.77, 0.72, 0.81 and 0.81, respectively [29].
The barratt impulsiveness scale-11
The Barratt Impulsiveness Scale-11 (BIS-11), a self-report questionnaire, was used to assess the impulsive characteristics of the participants. It contains three subscales, attentional impulsiveness (AI), non-planning impulsiveness (NPI) and motor impulsiveness (MI) and each item is rated on a 5-point Likert scale from 1 (never) to 5 (always) [30]. The BIS-11 has demonstrated high reliability and validity in English and Chinese versions [31, 32]. The Cronbach’s α coefficients were 0.78, 0.83 and 0.81 for the AI, NPI and MI, respectively [33].
The impulsive/premeditated aggression scale
The Impulsive/Premeditated Aggression Scale (IPAS), a self-report questionnaire, was used to assess the subtypes of violent behaviour. It has two subscales, impulsive aggression (IA) and premeditated aggression (PM) and the rating is performed on a 5-point Likert scale (1 = Strongly Disagree to 5 = Strongly Agree) [34, 35]. It was translated into Chinese in 2009 and the Cronbach’s α values of the IA and PM subscales were 0.73 and 0.70, respectively [36].
The personality diagnostic questionnaire
The Personality Diagnostic Questionnaire (PDQ-4+) is a self-report questionnaire that is used to evaluate 12 types of personality disorders on the basis of the DSM-IV criteria [37, 38]. The PDQ-4 + was translated into Chinese in 2002 [39]. This study used the ASPD subscale, which has 8 items (answering “yes” or “no” for each item), and the Cronbach’s α was 0.68 [40]. The participants who had a score equal to or above three points indicated traits of ASPD [41].
Statistical analysis
The participants were divided into non-violent groups and violent groups according to the occurrence of violent behaviour in the follow-up period. Demographic characteristics were initially compared by outcome status using t tests and χ2 tests for continuous and categorical variables, respectively. Next, a univariate Cox model was used to calculate the hazard ratio (HR) and 95% confidence interval (95% CI) to identify risk factors for violent behaviour. These risk factors were further examined via multivariate Cox models. For all analyses, two-sided p values less than 0.05 were considered statistically significant. These analyses were performed using SPSS Statistics 26.0 software.
Latent class analysis (LCA) was performed using the Z-scores of the BPAQ, BIS-11, IAPS and MOAS from participants who committed violent behaviour in the follow-up period. The Z score is a common and useful method for standardising continuous variables [42]. Each variable was classified into two categories according to whether the Z-score was above or below 0, and the Z score was only used for LCA.
The LCA analyses were performed in Mplus version 7.4. We examined models comprised of 2 to 5 classes to determine the best-fitting latent class model. The fit indices, including the Bayesian Information Criterion (BIC), the Akaike’s Information Criterion (AIC), the sample-size–adjusted BIC (aBIC), and entropy, were used to identify the best fitting model. Smaller AIC, BIC, and aBIC values indicated a better fit of the model. An entropy > 0.8 indicated that the classification was reasonable [43, 44]. The Vuong-Lo-Mendell-Rubin likelihood ratio test (LMRT) and the bootstrap likelihood ratio test (BLRT) were used to identify whether the fit of a model with K classes was better than the fit of a model with K-1 classes [45]. Logistic regression was performed in post-hoc analysis to estimate the different factors between subtypes.
Results
Characteristics of the study population
Table 1 presents the socio-demographic and clinical characteristics grouped by the occurrence of violent behaviour during the follow-up period. Among the 1615 patients, 117 (7.2%) engaged in violent behaviour during the follow-up period. Age, no economic source, child maltreatment, violence history, ASPD, BPAQ, motor impulsivity, non-planning impulsivity, BIS-total score, IA and PM differed significantly between the two groups (p < 0.05).
Table 1.
Differences of characteristics grouped by the occurrence of violent behaviour in follow-up period (6 months) among patients with SMD
| Variable | Total (n = 1615) |
non-violence (n = 1498) |
violence (n = 117) |
t/χ2 |
|---|---|---|---|---|
| Age (year) | 44.62 ± 10.98 | 44.83 ± 10.91 | 41.94 ± 11.56 | 2.75** |
| Male | 899(55.67) | 838(55.94) | 61(52.14) | 0.64 |
| Education(year) | 7.98 ± 4.30 | 7.97 ± 4.34 | 8.02 ± 3.68 | -0.10 |
| Marital status | 3.63 | |||
| Unmarried | 651(40.31) | 596(39.79) | 55(47.01) | |
| Married | 693(42.91) | 645(43.06) | 48(41.03) | |
| Divorced | 238(14.74) | 225(15.02) | 13(11.11) | |
| widowed | 26(1.61) | 25(1.67) | 1(0.85) | |
| Missingdata | 7(0.43) | 7(0.46) | 0(0.00) | |
| Unemployment | 769(47.62) | 709(47.33) | 60(51.28) | 0.68 |
| No economic source | 514(31.83) | 459(30.64) | 55(47.01) | 13.40*** |
| Child maltreatment | 60(3.72) | 49(3.27) | 11(9.40) | 11.40** |
| Violence history | 460(28.48) | 414(27.64) | 46(39.32) | 7.27** |
| ASPD | 163(10.09) | 144(9.61) | 19(16.24) | 5.25* |
| Schizophrenia | 1223(75.73) | 1135(75.77) | 88(75.21) | 0.02 |
| BPAQ | ||||
| PA | 22.37 ± 6.57 | 22.18 ± 6.58 | 24.83 ± 5.93 | -4.62*** |
| VA | 13.36 ± 3.67 | 13.29 ± 3.68 | 14.28 ± 3.33 | -3.08** |
| Anger | 18.20 ± 4.71 | 18.10 ± 4.69 | 19.51 ± 4.69 | -3.14** |
| Hostility | 22.53 ± 6.85 | 22.36 ± 6.87 | 24.68 ± 6.21 | -3.86*** |
| BPAQ Total Score | 76.46 ± 20.38 | 75.93 ± 20.45 | 83.31 ± 18.25 | -4.17*** |
| BIS-11 | ||||
| AI | 34.34 ± 7.83 | 34.25 ± 7.84 | 35.50 ± 7.59 | -1.66 |
| MI | 23.71 ± 6.45 | 23.60 ± 6.48 | 25.23 ± 5.88 | -2.87** |
| NPI | 34.09 ± 8.77 | 33.96 ± 8.81 | 35.76 ± 8.06 | -2.14* |
| BIS-11 Total Score | 92.14 ± 16.89 | 91.81 ± 16.90 | 96.49 ± 16.20 | -2.89** |
| IA | 19.35 ± 5.22 | 19.19 ± 5.24 | 21.39 ± 4.48 | -5.05*** |
| PM | 24.64 ± 7.07 | 24.43 ± 7.07 | 27.29 ± 6.54 | -4.53*** |
| MOAS | ||||
| VA | 0.08 ± 0.37 | 0.00 ± 0.00 | 1.13 ± 0.83 | -14.78*** |
| AAP | 0.04 ± 0.28 | 0.00 ± 0.00 | 0.57 ± 0.90 | -6.86*** |
| SA | 0.02 ± 0.17 | 0.00 ± 0.00 | 0.25 ± 0.59 | -4.58*** |
| PA | 0.03 ± 0.25 | 0.00 ± 0.00 | 0.36 ± 0.85 | -4.59*** |
| Total MOAS score | 0.32 ± 1.77 | 0.00 ± 0.00 | 4.45 ± 4.99 | -9.65*** |
ASPD Antisocial Personality Disorder, BPAQ Buss Perry Aggression Questionnaire, BIS Barrett Impulsiveness Scale, PA Physical Aggression, VA Verbal Aggression, AI Attentional Impulsiveness, MI Motor Impulsiveness, NPI Non-planning Impulsiveness, IA Impulsive Aggression, PM Premeditated Aggression, AAP Aggression against property, SA Self aggression;
*p < 0.05
*p < 0.01
***p < 0.001
Risk factors for violent behaviour
The risk factors for violent behaviour are presented in Table 2. In the univariate Cox model, age (HR = 0.98, 95% CI = 0.96-1.00, p = 0.009), child maltreatment (HR = 2.43, 95% CI = 1.31–4.53, p = 0.005), no economic source (HR = 1.81, 95% CI = 1.26–2.61, p = 0.004), BPAQ-physical aggression (HR = 1.06, 95% CI = 1.03–1.09, p < 0.001), BPAQ-verbal aggression (HR = 1.06, 95% CI = 1.01–1.12, p = 0.023), BPAQ-anger (HR = 1.05, 95% CI = 1.01–1.09, p = 0.016), BPAQ-hostility (HR = 1.04, 95% CI = 1.01–1.07, p = 0.003), BIS-motor impulsiveness (HR = 1.04, 95% CI = 1.01–1.06, p = 0.012), IA (HR = 1.07, 95% CI = 1.04–1.11, p < 0.001), IA (HR = 1.07, 95% CI = 1.04–1.11, p < 0.001) and PM (HR = 1.06, 95% CI = 1.03–1.09, p < 0.001) were risk factors for violent behaviour in the follow-up period (6 months) (Table 2). According to the multivariate Cox regression analysis, younger age (HR = 0.98, 95% CI = 0.96-1.00, p = 0.016) and no economic source (HR = 1.60, 95% CI = 1.10–2.33, p = 0.014) were statistically significant risk factors for violent behaviour during the follow-up period.
Table 2.
Cox-proportional hazards models for the violent behaviour in follow-up period (6 months)
| Variables | Univariate model | Multivariate model | ||
|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | |
| Age(year) | 0.98(0.96-1.00) | 0.009 | 0.98(0.96-1.00) | 0.016 |
| Child maltreatment | 2.43(1.31–4.53) | 0.005 | 1.55(0.80-3.00) | 0.193 |
| No economic source | 1.81(1.26–2.61) | 0.004 | 1.60(1.10–2.33) | 0.014 |
| BPAQ | ||||
| Physical Aggression | 1.06(1.03–1.09) | < 0.001 | 1.05(1.00-1.11) | 0.061 |
| Verbal Aggression | 1.06(1.01–1.12) | 0.023 | 1.01(0.92–1.11) | 0.865 |
| Anger | 1.05(1.01–1.09) | 0.016 | 0.97(0.90–1.04) | 0.366 |
| Hostility | 1.04(1.01–1.07) | 0.003 | 0.97(0.91–1.04) | 0.405 |
| Motor impulsivity (BIS-11) | 1.04(1.01–1.06) | 0.012 | 1.01(0.97–1.04) | 0.676 |
| IA | 1.07(1.04–1.11) | < 0.001 | 1.02(0.97–1.08) | 0.396 |
| PM | 1.06(1.03–1.09) | < 0.001 | 1.04(1.00-1.08) | 0.067 |
HR hazard ratio, CI confidence interval, BPAQ Buss Perry Aggression Questionnaire, BIS Barrett Impulsiveness Scale, IA Impulsive Aggression, PM Premeditated Aggression
Latent class analysis
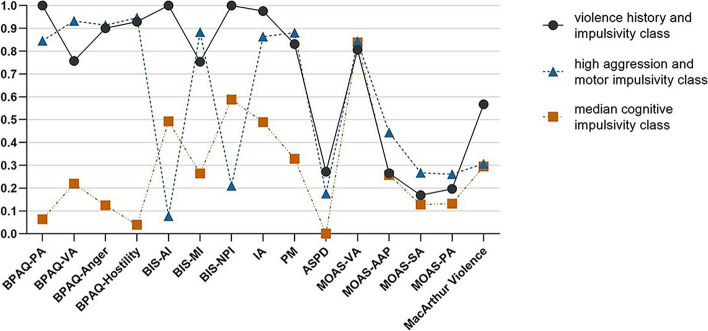
LCA analysis was performed on the basis of the Z score, and the details of the Z score are presented in Table S1 (Supplemental Materials). Model fit indices for various models with different latent classes are listed in Table 3. Although the AIC and aBIC decreased with increasing classification number, the difference in the LMR test was not significant between the 3-class and 4-class models. Moreover, the AIC and aBIC of the 3-class model were smaller than the 2-class model, whereas the entropy of the 3-class model was greater than the 2-class model. Taken together, the 3-class model was the best-fitting model. Figure 1 shows the profiles of the subtypes for the 3-class model.
Table 3.
Fit indices for latent class analysis models with 2–5 classes
| Number of classed | Log Likelihood | Number of parameters | AIC | BIC | aBIC | LMRT P-value |
Entropy | BLRT P-value |
|---|---|---|---|---|---|---|---|---|
| 2 | -897.32 | 31 | 1856.64 | 1942.27 | 1844.27 | < 0.001 | 0.95 | < 0.001 |
| 3 | -855.31 | 47 | 1804.63 | 1934.45 | 1785.88 | 0.002 | 0.95 | < 0.001 |
| 4 | -828.22 | 63 | 1782.43 | 1956.45 | 1757.30 | 0.059 | 0.98 | < 0.001 |
| 5 | -804.42 | 79 | 1766.84 | 1985.05 | 1735.33 | 0.598 | 0.97 | < 0.001 |
AIC The Akaike’s Information Criterion, BIC The Bayesian Information Criterion, aBIC The sample-size–adjusted BIC, LMRT The Vuong-Lo-Mendell-Rubin Likelihood Ratio Test, BLRT The Bootstrap Likelihood Ratio Test
Fig. 1.
Probability distribution of classes for 3-class model among patients with violent behaviour recurrence in follow-up. ASPD, Antisocial Personality Disorder; BPAQ, Buss Perry Aggression Questionnaire; BIS, Barrett Impulsiveness Scale; PA, Physical Aggression; VA, Verbal Aggression; AI, Attentional Impulsiveness; MI, Motor Impulsiveness; NPI, Non-planning Impulsiveness; IA, Impulsive Aggression; PM, Premeditated Aggression; MOAS, Modified Overt Aggression Scale; AAP, Aggression against property; SA, Self aggression
The first class (N = 41, 35.0%), which was labelled as the “violence history and impulsivity” subtype, featured a high probability of aggression and impulsiveness (greater than 70%). The second class (N = 45, 38.5%), which was labelled the “high aggression and motor impulsivity” subtype, consisted of patients who had a high probability of aggression and motor impulsivity (greater than 70%). The third class (N = 31, 26.5%), which was labelled the “median cognitive impulsivity” subtype, consisted of patients featuring a low probability of aggression (less than 30%) and a median probability of attentional impulsivity and non-planning impulsivity (greater than 50%).
The class response percentages within variables and differences in characteristics between classes are presented in Table 4. Class 1, named “violence history and impulsivity”, outperformed the other two subtypes in terms of physical aggression, attentional impulsivity, non-planning impulsivity, and impulsive aggression but these patients were more likely to have a violent history. In contrast, class 2, named “high aggression and motor impulsivity”, was more likely to have higher scores for physical aggression, verbal aggression, anger, hostility and motor impulsivity. In contrast, class3, named “median cognitive impulsivity”, presented greater attentional and no-planning impulsivity compared to class 2 (Table 4). The class response percentages within classes are presented in Table S2 (Supplemental Materials).
Table 4.
Class response percentages within variable and differences of characteristics between classes among participants commetted violent behaviour in 6-month follow-up period (n = 117)
| Class1 (n = 41, 35.04%) |
Class2 (n = 45, 38.46%) |
Class3 (n = 31, 26.50%) |
Class1 vs. Class3 OR (95%CI) |
Class2 vs. Class3 OR (95%CI) |
Class2 vs. Class1 OR (95%CI) |
|
|---|---|---|---|---|---|---|
| Age | 43.59 ± 11.93 | 41.69 ± 11.41 | 40.13 ± 11.34 | 1.03(0.99–1.07) | 1.01(0.97–1.05) | 0.99 (0.95–1.02) |
| Gender | ||||||
| Male | 28(68.29) | 23(51.11) | 10(32.26) | 4.52(1.66–12.29)** | 2.20(0.85–5.70) | 0.49(0.20–1.17) |
| Female | 13(31.71) | 22(48.89) | 21(67.74) | ref | ref | ref |
| Education | 7.51 ± 3.82 | 8.11 ± 3.46 | 8.55 ± 3.85 | 0.93(0.81–1.05) | 0.97(0.85–1.10) | 1.05(0.93–1.18) |
| Marital status | ||||||
| Unmarried | 20(48.78) | 20(44.44) | 15(48.39) | ref | ref | ref |
| Married | 19(46.34) | 16(35.56) | 13(41.94) | 1.10(0.41–2.90) | 0.92(0.34–2.49) | 0.84(0.34–2.09) |
| Divorced | 2(4.88) | 8(17.78) | 3(9.68) | 0.50(0.07–3.38) | 2.00(0.45–8.84) | 4.00(0.75–21.22) |
| widowed | 0(0.00) | 1(2.22) | 0(0.00) | 0.99(0.99–0.99) | - | - |
| Unemployed | 20(48.78) | 22(48.89) | 18(58.06) | 0.69(0.27–1.76) | 0.69(0.28–1.74) | 1.00(0.43–2.34) |
| No economic source | 11(26.83) | 8(17.78) | 0(0.00) | 1.09(0.43–2.76) | 0.57(0.23–1.44) | 0.52(0.22–1.24) |
| Child maltreatment | 6(14.63) | 4(8.89) | 1(3.23) | 5.14(0.59–45.15) | 2.93(0.31–27.53) | 0.57(0.15–2.18) |
| Violence history | 23(56.10) | 14(31.11) | 9(29.03) | 3.12(1.16–8.41)* | 1.10(0.41-3.00) | 0.35(0.15–0.85)* |
| Schizophrenia | 32(78.05) | 35(77.78) | 21(67.74) | 1.69(0.59–4.87) | 1.67(0.60–4.67) | 0.98(0.36–2.73) |
| ASPD | 11(26.83) | 8(17.78) | 0(0.00) | - | - | 0.59(0.21–1.65) |
| BPAQ | ||||||
| PA | 28.80 ± 3.74 | 26.49 ± 3.05 | 17.16 ± 4.12 | 4.16(2.08–8.34)*** | 3.35(1.70–6.62)*** | 0.81(0.69–0.94)** |
| VA | 15.15 ± 2.86 | 15.67 ± 2.20 | 11.13 ± 3.27 | 1.77(1.36–2.30)*** | 1.93(1.46–2.54)*** | 1.09(0.92–1.30) |
| Anger | 21.76 ± 3.64 | 21.29 ± 2.35 | 13.97 ± 4.00 | 1.84(1.46–2.31)*** | 1.74(1.40–2.16)*** | 0.95(0.82–1.10) |
| Hostility | 28.17 ± 4.25 | 27.29 ± 2.44 | 16.29 ± 4.11 | 2.37(1.62–3.46)*** | 2.18(1.51–3.15)*** | 0.92(0.81–1.05) |
| BPAQ Total Score | 93.88 ± 11.16 | 90.73 ± 6.67 | 58.55 ± 13.68 | 3.10(0.87–11.12) | 2.98(0.83–10.68) | 0.96(0.91–1.01) |
| BIS-11 | ||||||
| AI | 41.88 ± 5.46 | 30.42 ± 2.61 | 34.42 ± 8.79 | 1.22(1.11–1.34)*** | 0.87(0.79–0.96)** | 0.71(0.63–0.80)*** |
| MI | 26.41 ± 6.23 | 27.82 ± 3.75 | 19.90 ± 4.48 | 1.27(1.13–1.41)*** | 1.35(1.20–1.52)*** | 1.07(0.97–1.17) |
| NPI | 42.20 ± 4.81 | 30.69 ± 4.89 | 34.61 ± 9.41 | 1.24(1.12–1.36)*** | 0.92(0.85–0.99)** | 0.74(0.67–0.82)*** |
| BIS-11 Total Score | 110.49 ± 9.76 | 88.93 ± 8.35 | 88.94 ± 19.32 | 1.23(1.13–1.33)*** | 1.00(0.97–1.04) | 0.82(0.75–0.88)*** |
| IA | 23.78 ± 2.64 | 21.56 ± 2.57 | 18.00 ± 6.23 | 1.53(1.28–1.84)*** | 1.22(1.07–1.38)** | 0.79(0.68–0.93)** |
| PM | 29.27 ± 4.47 | 28.20 ± 3.98 | 23.35 ± 9.63 | 1.16(1.07–1.27)** | 1.13(1.04–1.22)** | 0.97(0.90–1.04) |
| MOAS | ||||||
| VA | 1.02 ± 0.72 | 1.31 ± 1.00 | 1.00 ± 0.63 | 1.05(0.56–1.95) | 1.59(0.88–2.87) | 1.53(0.90–2.60) |
| AAP | 0.44 ± 0.78 | 0.76 ± 1.00 | 0.48 ± 0.89 | 0.93(0.53–1.66) | 1.38(0.82–2.32) | 1.48(0.91–2.41) |
| SA | 0.24 ± 0.58 | 0.33 ± 0.71 | 0.13 ± 0.34 | 1.72(0.57–5.16) | 2.16(0.75–6.25) | 1.26(0.63–2.52) |
| PA | 0.32 ± 0.72 | 0.40 ± 0.81 | 0.35 ± 1.05 | 0.94(0.53–1.68) | 1.06(0.62–1.81) | 1.13(0.68–1.88) |
| Total MOAS score | 3.90 ± 3.47 | 5.42 ± 6.41 | 3.77 ± 4.23 | 1.01(0.89–1.14) | 1.08(0.96–1.20) | 1.07(0.97–1.18) |
Class 1, violence history and impulsivity; Class 2, high aggression and motor impulsivity; Class 3,median cognitive impulsivity
OR Odds Ratio, CI confidence interval, ASPD Antisocial Personality Disorder, BPAQ Buss Perry Aggression Questionnaire, BIS Barrett Impulsiveness Scale, PA Physical Aggression, VA Verbal Aggression, AI Attentional Impulsiveness, MI Motor Impulsiveness, NPI Non-planning Impulsiveness, IA Impulsive Aggression, PM Premeditated Aggression, MOAS Modified Overt Aggression Scale, AAP Aggression against property, SA Self-aggression
*p < 0.05
**p < 0.01
***p < 0.001
Discussion
The present study provides primary findings that distinctive impulsivity features three subtypes of violent behaviour among patients with SMD on the basis of longitudinal community samples in China. To our knowledge, this report is the first study to use the LCA model to investigate potential subtypes of SMD patients engaged in violent behaviour in the community. We found that younger age and no economic source were risk factors for violent behaviour among patients with SMD in the community. There were three subtypes of patients with SMD who engaged in violent behaviour and various profiles of impulsivity and violence history were presented in these subtypes. These results should be helpful for setting targeted violence and risk management of violence according to the subtype feature in the community and provide useful information on the mechanism of violence, which has shown inconsistent findings because of the heterogeneity of violent behaviour.
Our results revealed that during the 6-month follow-up period, 7.2% of patients exhibited violent behaviour. The incidence of violence was relatively low compared to that reported in Huang’s study 40.3%, which was based on 491 participants with schizophrenia in a rural area of southern China [46]. We believe that the various follow-up periods, the 6-month follow-up period in the present study and the 2-year follow-up period in Huang’s study, may account for the difference. Compared to the rural areas, the treatment compliance of urban community-dwelling patients was relatively good, and the community management system provided basic guarantees for antipsychotic treatment for patients with SMD, which may be another reason for the low rate of violent behaviour in this study. This finding suggests that the Chengdu Mental Health Prevention and Management System was effective in managing the violent risk of patients with SMD. Although an uneven distribution of mental health resources still exists in China [47], these findings suggest that increasing the investment intensity of these projects, especially in rural areas, may be useful for preventing violent behaviour among SMD.
Our study revealed that younger age and no economic source were risk factors for violent behaviours in patients with SMD, which is consistent with the findings of previous studies. There is ample evidence that young people with mental disorders are more likely to be engaged in violent behaviour [2, 48]. Patients without financial resources were also more prone to violent behaviour, which was confirmed in previous studies [48, 49]. Moreover, our results showed that the violent behaviour of patients with SMD was not associated with unemployment but with a lack of financial resources. This result is possibly because patients have no job and no financial support from their family, which indirectly reflects a lack of supervision. Patients without supervision have low medication adherence [50], which is related to the occurrence of violent behaviour [51]. Therefore, more attention should be focused on monitoring the risk of violent behaviour among young and economically disadvantaged patients with SMD.
Moreover, our study revealed that schizophrenia was not a risk factor for violence among patients with SMD. This finding was different from a meta-analysis that identified schizophrenia as a risk factor for violence [15]. We believe that the various study designs used may explain this difference because this study was performed among patients diagnosed with schizophrenia, schizoaffective disorder, delusional disorder, bipolar disorder, psychotic disorder due to epilepsy, or mental retardation with mental disorders, whereas the meta-analysis was performed with a general population sample. Furthermore, many studies have identified substance use as a strongly predictive factor of violence [1, 15], which was not the finding of our study. This difference is because substance use disorders were not included in this study, which included participants from the Chengdu Mental Health Prevention Management System. Substance use is illegal in China [18], so people with substance use disorders are not included in the Chengdu Mental Health Prevention Management System. In addition, as stated in other studies, SMD does not independently predict future violent behaviour [52] and risk factors affecting non-psychotic persons could similarly increase the risk among those with psychosis [53]. Further mechanistic studies revealed that anger due to delusional beliefs was a key intermediate variable in the pathway from persecutory/threat delusions to serious violence among psychiatric patients [54, 55]. These results may partially eliminate the stigma of patients with SMD.
Our results revealed that patients with SMD who engaged in violent behaviours were classified into three subtypes. The “violence history and impulsivity” subtype was more likely to have a violent history. A violent history has been consistently reported as a risk factor for violence among patients with mental disorders or among the general population [56, 57]. Moreover, this class presented the highest percentage of antisocial traits among the three subtypes, which was similar to Hodgin’s first phenotype of schizophrenia patients with violence described as displaying violent and antisocial behaviours regardless of the onset of schizophrenia [12]. Hodgin classified violent schizophrenia patients through clinical observation, and our results of an LCA model based on violent patients with SMD also supported this observation. In addition, the “violence history and impulsivity” subtype was similar to Joyal’s cluster II labelled “repetitive violent offenders”, which reported significantly more lifetime violent acts and higher scores for impulsivity [14]. Although the study design, sample source and variables included in the LCA varied between these studies, they all reported similar subtypes, which strongly demonstrated the robustness of this subtype. Therefore, the “violence history and impulsivity” subtype may be a target of the risk management of violence in the mental health services of communities. These findings may aid mental health professionals in recognising appropriate indicators to prevent violent behaviour among community patients with SMD to facilitate more tailored treatment programs.
Different profiles of impulsivity were the main factors that distinguished the three subtypes of violent behaviour among SMD patients. Impulsivity has been consistently associated with different types of violent behaviour, such as careless driving, starting fights, and implementing domestic violence [58–61]. Our previous study revealed that impulsivity was a key factor in the relationship between child maltreatment and negative behaviour [62]. Furthermore, the three components of impulsivity, including motor, non-planning and attentional impulsivity, could play different roles in violent behaviour [31, 63]. Previous studies found that non-planning impulsivity was an independent crucial indicator of homicidal patients with schizophrenia [64], whereas a higher level of motor impulsivity in patients with externally directed violence as well as self-directed violent behaviour played a vital role in the occurrence of violence [65]. The potential route by which impulsivity causes violent behaviour may result from impaired executive function and control function of the brain [66, 67]. These results provide new evidence for the heterogeneity of violent behaviour, which suggests that different profiles of impulsivity in these subtypes have different underlying mechanisms of violent behaviour.
Limitations
This study also has several limitations. First, this study had a relatively short (6 months) follow-up period. Although this duration may be derived from the impact of the COVID-2019 epidemic to some degree, the limited observation period may reduce the rate of violent behaviour. Second, because the assessors were community psychiatric management physicians rather than psychiatrists, we did not assess the severity of psychotic symptoms in patients with mental disorders. However, we used a diagnosis made by a clinical psychiatrist to compensate for this limitation to some degree. Third, certain instruments, such as the BPAQ, were self-administered, which may result in some bias, particularly among patients with SMD whose consecutive altered perceptions of themselves and their environment may be distorted. Fourth, this study included patients with SMD containing six diagnoses, which may be associated with diagnostic heterogeneity, because of the different aetiologic and symptomatologic aspects of the different diagnoses. Finally, we only assessed whether violence occurred within the given 6 months and did not count the length of time the violence occurred from the baseline survey, but the latter data could provide more information.
Conclusions
Only a few patients with SMD engaged in violent behaviour within six months in the community, and sociodemographic factors, rather than diagnosis, were risk factors for violent behaviour among patients with SMD in the community of China, which could eliminate the discrimination towards patients with mental disorders. Patients with SMD who engaged in violent behaviour may be classified into three subtypes, namely, violence history and impulsivity, high aggression and motor impulsivity, and median cognitive impulsivity subtypes, which provides novel evidence for the heterogeneity of violent behaviour. Future studies investigating violent behaviour in patients with psychiatric disorders should consider the violent history and the impact of impulsivity. It is necessary to perform longitudinal studies among a general population sample to identify the influence of diagnostic heterogeneity in China. These findings may be helpful for identifying the target of violence risk management for patients with SMD in the community and provide useful information on the mechanism of violence in mental disorders.
Supplementary Information
Abbreviations
- SMD
Severe mental disorders
- CMHS
Community mental health service
- IA
Impulsive aggression
- ASPD
Antisocial personality disorder
- PM
Premeditated aggression
- COVID-2019
Coronavirus disease 2019
- LCA
Latent class analysis
- BPAQ
Buss-Perry Aggression Questionnaire
- PDQ-4+
Personality Diagnostic Questionnaire
- PA
Physical aggression
- SA
Self aggression
- VA
Verbal aggression
- AAP
Aggression against property
- BIS-11
Barratt Impulsiveness Scale-11
- MOAS
Modified Overt Aggression Scale
- AI
Attentional impulsiveness
- HR
Hazard ratio
- NPI
Non-planning impulsiveness
- CI
Confidence interval
- MI
Motor impulsiveness
- OR
Odds ratio
- IPAS
Impulsive/Premeditated aggression scale
- MCVI
MacArthur Community Violence Instrument
- BIC
Bayesian Information Criterion
- AIC
: Akaike's Information Criterion
- aBIC
Sample-size–adjusted BIC
- LMRT
Vuong-Lo-Mendell-Rubin Likelihood Ratio Test
- BLRT
Bootstrap Likelihood Ratio Test
Authors’ contributions
CXC and YQ designed this study. YQ completed the data collection. WQK and CXC analyzed the data and drafted the manuscript. ZQT, LCX, YQ, QYF, YXT and HJM provided critical revision of the manuscript. All authors contributed to revising the manuscript and approving the final manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (no. 82302119), the China Postdoctoral Science Foundation (no. 2020TQ0219), the Sichuan Science and Technology Program (no. 2023YFS0291) and the Open Project of Shanghai Key Lab of Forensic Medicine, Key Lab of Forensic Science, Ministry of Justice, China (Academy of Forensic Science) (no. KF202313).
Availability of data and materials
All data and materials are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of Sichuan University (No: K2021010). Informed consent was obtained from all participants before data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Qi-Kai Wang and Qin Yang contributed equally to this work.
Contributor Information
Qin-Ting Zhang, Email: zhangqinting@126.com.
Xia-Can Chen, Email: xiacanchen17@scu.edu.cn.
References
- 1.Whiting D, Lichtenstein P, Fazel S. Violence and mental disorders: a structured review of associations by individual diagnoses, risk factors, and risk assessment. Lancet Psychiatry. 2021;8:150–61. 10.1016/S2215-0366(20)30262-5 [DOI] [PubMed] [Google Scholar]
- 2.Large MM, Nielssen O. Violence in first-episode psychosis: a systematic review and meta-analysis. Schizophr Res. 2011;125:209–20. 10.1016/j.schres.2010.11.026 [DOI] [PubMed] [Google Scholar]
- 3.Van Dorn R, Volavka J, Johnson N. Mental Disorder and violence: is there a relationship beyond substance use? Soc Psychiatry Psychiatr Epidemiol. 2012;47:487–503. 10.1007/s00127-011-0356-x [DOI] [PubMed] [Google Scholar]
- 4.Senior M, Fazel S, Tsiachristas A. The economic impact of violence perpetration in severe mental illness: a retrospective, prevalence-based analysis in England and Wales. Lancet Public Health. 2020;5:e99–106. 10.1016/S2468-2667(19)30245-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ministry of China. Chinese managerial and treatment regulations for severely mentally disordered patients (in Chinese). 2012.
- 6.Ma H. Integration of hospital and community services-the ’686 project’-is a crucial component in the reform of China’s mental health services. Shanghai Arch Psychiatry. 2012;24:172–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yip W, Hsiao W. Harnessing the privatisation of China’s fragmented health-care delivery. Lancet. 2014;384:805–18. 10.1016/S0140-6736(14)61120-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Appelbaum PS, Robbins PC, Monahan J. Violence and delusions: data from the MacArthur Violence Risk Assessment Study. Am J Psychiatry. 2000;157:566–72. 10.1176/appi.ajp.157.4.566 [DOI] [PubMed] [Google Scholar]
- 9.Whiting D, Gulati G, Geddes JR, Fazel S. Association of Schizophrenia Spectrum Disorders and violence perpetration in adults and adolescents from 15 countries: a systematic review and Meta-analysis. JAMA Psychiatry. 2022;79:120–32. 10.1001/jamapsychiatry.2021.3721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramírez JM. The usefulness of distinguishing types of aggression by function. Int Soc Sci J. 2010;61:263–72. 10.1111/j.1468-2451.2011.01762.x [DOI] [PubMed] [Google Scholar]
- 11.Weinshenker NJ, Siegel A. Bimodal classification of aggression: affective defense and predatory attack. Aggress Violent Beh. 2002;7:237–50. 10.1016/S1359-1789(01)00042-8 [DOI] [Google Scholar]
- 12.Hodgins S, Schiffer B, Müller-Isberner R. Violence among people with Schizophrenia: phenotypes and neurobiology. Curr Top Behav Neurosci. 2014;17:329–68. 10.1007/7854_2013_259 [DOI] [PubMed] [Google Scholar]
- 13.Lau S, Günther MP, Kling S, Kirchebner J. Latent class analysis identified phenotypes in individuals with schizophrenia spectrum disorder who engage in aggressive behaviour towards others. Eur Psychiatr. 2019;60:86–96. 10.1016/j.eurpsy.2019.05.005 [DOI] [PubMed] [Google Scholar]
- 14.Joyal CC, Côté G, Meloche J, Hodgins S. Severe Mental illness and aggressive behavior: on the importance of considering subgroups. Int J Forensic Mental Health. 2011;10:107–17. 10.1080/14999013.2011.577136 [DOI] [Google Scholar]
- 15.Fazel S, Smith EN, Chang Z, Geddes JR. Risk factors for interpersonal violence: an umbrella review of meta-analyses. Br J Psychiatry. 2018;213:609–14. 10.1192/bjp.2018.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guo W, Gu Y, Zhou J, Wang X, Sun Q. Characteristics and associated factors of violence in male patients with schizophrenia in China. Front Psychiatry. 2023;14:1106950. 10.3389/fpsyt.2023.1106950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen X, Zhang X, Wong SCP, Yang M, Kong D, Hu J. Characteristics of alleged homicide offenders with and without schizophrenia in Sichuan, China. Criminal Behav Ment Health. 2018;28:202–15. 10.1002/cbm.2054 [DOI] [PubMed] [Google Scholar]
- 18.Degenhardt L, Bharat C, Glantz MD, Sampson NA, Scott K, Lim CCW, et al. The epidemiology of drug use disorders cross-nationally: findings from the WHO’s World Mental Health surveys. Int J Drug Policy. 2019;71:103–12. 10.1016/j.drugpo.2019.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou J, Zhong B, Xiang Y, Chen Q, Cao X, Correll CU, et al. Prevalence of aggression in hospitalized patients with schizophrenia in China: a meta-analysis. Asia-Pacific Psychiatry. 2016;8:60–9. 10.1111/appy.12209 [DOI] [PubMed] [Google Scholar]
- 20.Huang Y, Yu S, Liu Z. A correlated analysis of aggressive behavior in patients with schizophrenia. J Clin Psychol Med. 2007;05:303–4. [Google Scholar]
- 21.Li G, Zhou H. The related factors of aggressive behavior in male patients with schizophrenia. J Psychiatry. 2007;03:174–5. [Google Scholar]
- 22.Chang WC, Chan SSI, Hui CLM, Chan SKW, Lee EHM, Chen EYH. Prevalence and risk factors for violent behavior in young people presenting with first-episode psychosis in Hong Kong: a 3-year follow-up study. Aust N Z J Psychiatry. 2015;49:914–22. 10.1177/0004867415603130 [DOI] [PubMed] [Google Scholar]
- 23.Yudofsky SC, Silver JM, Jackson W, Endicott J, Williams D. The overt aggression scale for the objective rating of verbal and physical aggression. Am J Psychiatry. 1986;143:35–9. 10.1176/ajp.143.1.35 [DOI] [PubMed] [Google Scholar]
- 24.Oliver PC, Crawford MJ, Rao B, Reece B, Tyrer P. Modified overt aggression scale (MOAS) for people with intellectual disability and aggressive challenging Behaviour: a reliability study. Res Intellect Disabil. 2007;20:368–72. 10.1111/j.1468-3148.2006.00346.x [DOI] [Google Scholar]
- 25.Xie B, Zheng Z. The modified overt aggression scale(MOAS). Chin J Behav Med Sci. 2001;10:195–6.
- 26.Chen X, Xu J, Wang H, Luo J, Wang Z, Chen G, et al. Profiling the differences of gut microbial structure between schizophrenia patients with and without violent behaviors based on 16S rRNA gene sequencing. Int J Legal Med. 2021;135:131–41. 10.1007/s00414-020-02439-1 [DOI] [PubMed] [Google Scholar]
- 27.Monahan J, Steadman H, Silver E, Appelbaum P, Clark Robbins P, Mulvey E, et al. Rethinking risk assessment. The MacArthur study of mental disorder and violence. New York, USA: Oxford University Press; 2001. [Google Scholar]
- 28.Buss AH, Perry M. The Aggression Questionnaire. J Personal Soc Psychol. 1992;63:452–9. 10.1037/0022-3514.63.3.452 [DOI] [PubMed] [Google Scholar]
- 29.Xia X, Zhang J, Wang X, Wang X. The Approach Behavior to angry words in Athletes—A pilot study. Front Behav Neurosci. 2019;13:117. 10.3389/fnbeh.2019.00117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lu CF, Jia CX, Xu AQ, Dai AY, Qin P. Psychometric characteristics of Chinese Version of Barratt Impulsiveness Scale-11 in suicides and living controls of Rural China. Omega (Westport). 2013;66:215–29. 10.2190/OM.66.3.b [DOI] [PubMed] [Google Scholar]
- 31.Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–74. [DOI] [PubMed] [Google Scholar]
- 32.Yao S, Yang H, Zhu X, Auerbach RP, Abela JRZ, Pulleyblank RW, et al. An examination of the Psychometric properties of the Chinese Version of the Barratt Impulsiveness Scale, 11th Version in a sample of Chinese adolescents. Percept Mot Skills. 2007;104:1169–82. 10.2466/pms.104.4.1169-1182 [DOI] [PubMed] [Google Scholar]
- 33.Qian Z, Liu S, Zhu X, Kong L, Liu N, Wang D, et al. Higher trait impulsivity and altered Frontostriatal Connectivity in Betel-Quid Dependent individuals. Front Hum Neurosci. 2020;14:578913. 10.3389/fnhum.2020.578913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gong M, Yao L, Ge X, Liu Z, Zhang C, Yang Y, et al. Empathy deficit in male patients with schizophrenia and its relationships with impulsivity and premeditated violence. Front Psychiatry. 2023;14:1160357. 10.3389/fpsyt.2023.1160357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stanford MS, Houston RJ, Mathias CW, Villemarette-Pittman NR, Helfritz LE, Conklin SM. Characterizing Aggressive Behav Assess. 2003;10:183–90. [DOI] [PubMed] [Google Scholar]
- 36.Qiao Y, Xie B, Zhang M-D. The Chinese version of impulsive-premeditated aggression scale in adolescents with aggression: its reliability and validity. Chin J Behav Med Brain Sci. 2009;18:366–8. [Google Scholar]
- 37.Hyler SE, Skodol AE, Oldham JM, David Kellman H, Doidge N. Validity of the personality diagnostic Questionnaire-Revised: a replication in an outpatient sample. Compr Psychiatr. 1992;33:73–7. 10.1016/0010-440X(92)90001-7 [DOI] [PubMed] [Google Scholar]
- 38.Zhang T, Wang L, Good M-JD, Good BJ, Chow A, Dai Y, et al. Prevalence of personality disorders using two diagnostic systems in psychiatric outpatients in Shanghai, China: a comparison of uni-axial and multi-axial formulation. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1409–17. 10.1007/s00127-011-0445-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang Y, Shen D, Wang J, Yang J. The reliability and validity of PDQ-4 + in China. Chin J Clin Psychol. 2002;10:165–8. [Google Scholar]
- 40.Yang J, McCrae RR, Costa PT, Yao S, Dai X, Cai T, et al. The cross-cultural generalizability of Axis-II constructs: an evaluation of two personality disorder Assessment instruments in the people’s Republic of China. J Personal Disord. 2000;14:249–63. 10.1521/pedi.2000.14.3.249 [DOI] [PubMed] [Google Scholar]
- 41.He H, Xu M, Fei Z, Xie Y, Gu X, Zhu H, et al. Sex differences in personality disorders in a Chinese clinical population. Front Psychiatry. 2022;13:1006740. 10.3389/fpsyt.2022.1006740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Andrade CZ, Scores. Standard scores, and Composite Test scores explained. Indian J Psychol Med. 2021;43:555–7. 10.1177/02537176211046525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Asparouhov T, Muthén B. Using Mplus TECH11 and TECH14 to test the number of latent classes. Mplus Web Notes. 2012. https://www.statmodel.com/examples/webnote.shtml. Accessed 25 Dec 2023.
- 44.Lubke G, Muthén B. Performance of factor mixture models as a function of model size, Covariate effects, and class-specific parameters. Struct Equation Modeling: Multidisciplinary J. 2007;14:26–47. 10.1080/10705510709336735 [DOI] [Google Scholar]
- 45.Pignon B, Peyre H, Noblins E, Rolland B, Thomas P, Vaiva G, et al. A latent class analysis of Manic and psychotic symptoms. J Nerv Ment Dis. 2020;208:721–8. 10.1097/NMD.0000000000001193 [DOI] [PubMed] [Google Scholar]
- 46.Huang ZH, Wang F, Chen ZL, Xiao YN, Wang QW, Wang SB, et al. Risk factors for violent behaviors in patients with schizophrenia: 2-year follow-up study in primary mental health care in China. Front Psychiatry. 2022;13:947987. 10.3389/fpsyt.2022.947987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu Y, Liu X, Wen H, Wang D, Yang X, Tang W, et al. Risk behavior in patients with severe mental disorders: a prospective study of 121,830 patients managed in rural households of western China. BMC Psychiatry. 2018;18:134. 10.1186/s12888-018-1709-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang L, Qi X, Wen L, Hu X, Mao H, Pan X, et al. Identifying risk factors to predict violent behaviour in community patients with severe mental disorders: a retrospective study of 5277 patients in China. Asian J Psychiatr. 2023;83:103507. 10.1016/j.ajp.2023.103507 [DOI] [PubMed] [Google Scholar]
- 49.Bo S, Abu-Akel A, Kongerslev M, Haahr UH, Simonsen E. Risk factors for violence among patients with schizophrenia. Clin Psychol Rev. 2011;31:711–26. 10.1016/j.cpr.2011.03.002 [DOI] [PubMed] [Google Scholar]
- 50.Wang H, Yao F, Wang H, Wang C, Guo Z. Medication adherence and influencing factors among patients with severe Mental disorders in low-income families during COVID-19 outbreak. Front Psychiatry. 2022;12:799270. 10.3389/fpsyt.2021.799270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li Y, Wen H, Xiong C, Lin C, Yang X, Wang D, et al. Medication nonadherence and risk of violence to others among patients with Schizophrenia in Western China. JAMA Netw Open. 2023;6:e235891. 10.1001/jamanetworkopen.2023.5891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Elbogen EB, Johnson SC. The Intricate Link between Violence and Mental Disorder: results from the national epidemiologic survey on Alcohol and related conditions. Arch Gen Psychiatry. 2009;66:152. 10.1001/archgenpsychiatry.2008.537 [DOI] [PubMed] [Google Scholar]
- 53.Bonta J, Law M, Hanson K. The prediction of criminal and violent recidivism among mentally disordered offenders: a meta-analysis. Psychol Bull. 1998;123:123–42. 10.1037/0033-2909.123.2.123 [DOI] [PubMed] [Google Scholar]
- 54.Ullrich S, Keers R, Coid JW. Delusions, anger, and serious violence: new findings from the MacArthur Violence Risk Assessment Study. Schizophr Bull. 2014;40:1174–81. 10.1093/schbul/sbt126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ullrich S, Keers R, Shaw J, Doyle M, Coid JW. Acting on delusions: the role of negative affect in the pathway towards serious violence. J Forensic Psychiatr Psychol. 2018;29:691–704. 10.1080/14789949.2018.1434227 [DOI] [Google Scholar]
- 56.Barlati S, Stefana A, Bartoli F, Bianconi G, Bulgari V, Candini V, et al. Violence risk and mental disorders (VIORMED-2): a prospective multicenter study in Italy. PLoS ONE. 2019;14:e0214924. 10.1371/journal.pone.0214924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Witt K, van Dorn R, Fazel S. Risk factors for violence in psychosis: systematic review and meta-regression analysis of 110 studies. PLoS ONE. 2013;8:e55942. 10.1371/journal.pone.0055942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bjørkly S. A systematic review of the relationship between impulsivity and violence in persons with psychosis: evidence or spin cycle? Aggress Violent Beh. 2013;18:753–60. 10.1016/j.avb.2013.08.001 [DOI] [Google Scholar]
- 59.Chamorro J, Bernardi S, Potenza MN, Grant JE, Marsh R, Wang S, et al. Impulsivity in the general population: a national study. J Psychiatr Res. 2012;46:994–1001. 10.1016/j.jpsychires.2012.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gvion Y, Apter A. Aggression, Impulsivity, and suicide behavior: a review of the literature. Archives Suicide Res. 2011;15:93–112. 10.1080/13811118.2011.565265 [DOI] [PubMed] [Google Scholar]
- 61.McHugh CM, Chun Lee RS, Hermens DF, Corderoy A, Large M, Hickie IB. Impulsivity in the self-harm and suicidal behavior of young people: a systematic review and meta-analysis. J Psychiatr Res. 2019;116:51–60. 10.1016/j.jpsychires.2019.05.012 [DOI] [PubMed] [Google Scholar]
- 62.Chen XC, Xu JJ, Yin XT, Qiu Y-F, Yang R, Wang ZY et al. Mediating role of anxiety and impulsivity in the association between child maltreatment and lifetime non-suicidal self-injury with and without suicidal self-injury. J Affect Disord. 2023;S0165-0327(23)01448-9. [DOI] [PubMed]
- 63.Ramírez JM, Andreu JM. Aggression, and some related psychological constructs (anger, hostility, and impulsivity); some comments from a research project. Neurosci Biobehav Rev. 2006;30:276–91. 10.1016/j.neubiorev.2005.04.015 [DOI] [PubMed] [Google Scholar]
- 64.Balcioglu YH, Kirlioglu Balcioglu SS, Oncu F, Turkcan A, Yorulmaz AC. Impulsive and aggressive traits and increased peripheral inflammatory status as psychobiological substrates of homicide behavior in schizophrenia. Eur J Psychiatry. 2022;36:207–14. 10.1016/j.ejpsy.2022.01.004 [DOI] [Google Scholar]
- 65.Scocco P, Macis A, Ferrari C, Bava M, Bianconi G, Bulgari V, et al. Self-harm behaviour and externally-directed aggression in psychiatric outpatients: a multicentre, prospective study (viormed-2 study). Sci Rep. 2019;9:17857. 10.1038/s41598-019-53993-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sani SRH, Tabibi Z, Fadardi JS, Stavrinos D. Aggression, emotional self-regulation, attentional bias, and cognitive inhibition predict risky driving behavior. Accid Anal Prev. 2017;109:78–88. 10.1016/j.aap.2017.10.006 [DOI] [PubMed] [Google Scholar]
- 67.Yang Y, Raine A, Han C-B, Schug RA, Toga AW, Narr KL. Reduced hippocampal and parahippocampal volumes in murderers with schizophrenia. Psychiatry Res. 2010;182:9–13. 10.1016/j.pscychresns.2009.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data and materials are available from the corresponding author on reasonable request.