Abstract
Background
Distal femur osteotomies are a well known and valuable treatment option to manage valgus malalignment with unicompartmental arthritis. Early postoperative complications are well known, and risk factors, such as pulmonary diseases, smoke, high dependent functional status, and body mass index, have been studied, but no study is available about osteotomies when gait is abnormal because of neurodegenerative conditions or when mineral density is below the normal rate.
Case presentation
We report the case of a 44 year-old female Mediterranean patient who underwent a biplanar distal femur opening wedge osteotomy surgery following a lateral meniscus total removal, which led to the subsequent development of lateral compartment osteoarthritis and pain, despite general comorbidities, such as multiple sclerosis. Additionally, 2 months later a supracondylar femur fracture above the previously applied Tomofix® plate was reported. Fracture was treated by applying a LCP condylar 16 hole (336 mm) plate, a structural fibular graft, and strut fibular graft on the opposite side.
Conclusion
The overall aim of this case report is to provide a lesson to surgeons who want to perform a realignment surgery of the lower limb in patients with abnormal gait. Not only mechanical axes are to be considered, but also bone density, patient’s gait, and load force distribution along the bone stock. Emerging literature on three-dimensional cutting guides fails to account for these factors, thus promoting a standardized approach to surgery across all patients. The present case highlights a patient with low bone density and abnormal force distribution resulting from a pathologic neurodegenerative gait. In such cases, treatment decisions must carefully consider the biomechanical vulnerabilities of the native bone and the distribution of vector forces. These conditions must lead the choice toward a longer plate if an osteotomy is indicated, because surgery is more likely to fail.
Keywords: Distal femoral osteotomy, DFO, Knee fracture, Distal femur fracture, Low density bone, Neurodegenerative gait, Arthrosis, Lateral compartment osteoarthritis, Knee, Trauma, Fibular strut, Allograft, Osteotomy, Lower limb malalignment, Case report, Gait analysis
Introduction
Varus and valgus malalignment with isolated medial or lateral wear of knee compartments can be treated in young and active patients by performing a high tibial osteotomy (HTO) or a distal femoral osteotomy (DFO), shifting the mechanical axis of the lower limb, and thus distributing load equally on knee compartments.
Early postoperative complications include recurrence of deformity, infection, joint contracture, hemartrosis, loss of posterior slope, compartment syndrome, neurovascular injury, hardware failure, delayed union, nonunion, and fractures [4]. The latter ones are among the rarest complications, and usually occur after falls [2].
Preoperative planning of osteotomies should include anterior–posterior weight bearing X-rays of the lower limbs and lateral projections of the knee [1, 2, 4, 6, 7], but no study is available regarding the correlation between gait, distribution of forces, and mechanical axis surgical adjustments.
Case presentation
A 44 year-old Mediterranean woman (weight of 81 kg, height of 178 cm, body mass index of 25,6 kg/m2) affected by a relapsing remitting form of multiple sclerosis in an initial phase, first presented to our outpatient clinic complaining of lateral left knee pain. Nothing relevant was found in the family history. In 2021, the patient underwent an arthroscopic subtotal lateral meniscectomy of the knee owing to a nonspecified lateral meniscal tear; in 2022 she then underwent an arthroscopic meniscal regularization because of residual pain. Physical examination revealed lateral pain during walking and lateral compartment tenderness at palpation and in response to valgus stress; ligaments were stable at stress maneuvers; range of movement (ROM) reported was 0–110°, limited by pain. Radiographs (Fig. 1, left) revealed lateral compartment knee osteoarthritis and valgus femoral deformity. Therefore, an opening wedge DFO with an allograft wedge was scheduled. Initial planning showed lateral distal femoral angle (mLDFA) of 86,71° and medial proximal tibial angle (MPTA) of 87,01°; we therefore estimated a 5 mm medial opening cut to restore a neutral axis (Fig. 2).
Fig. 1.
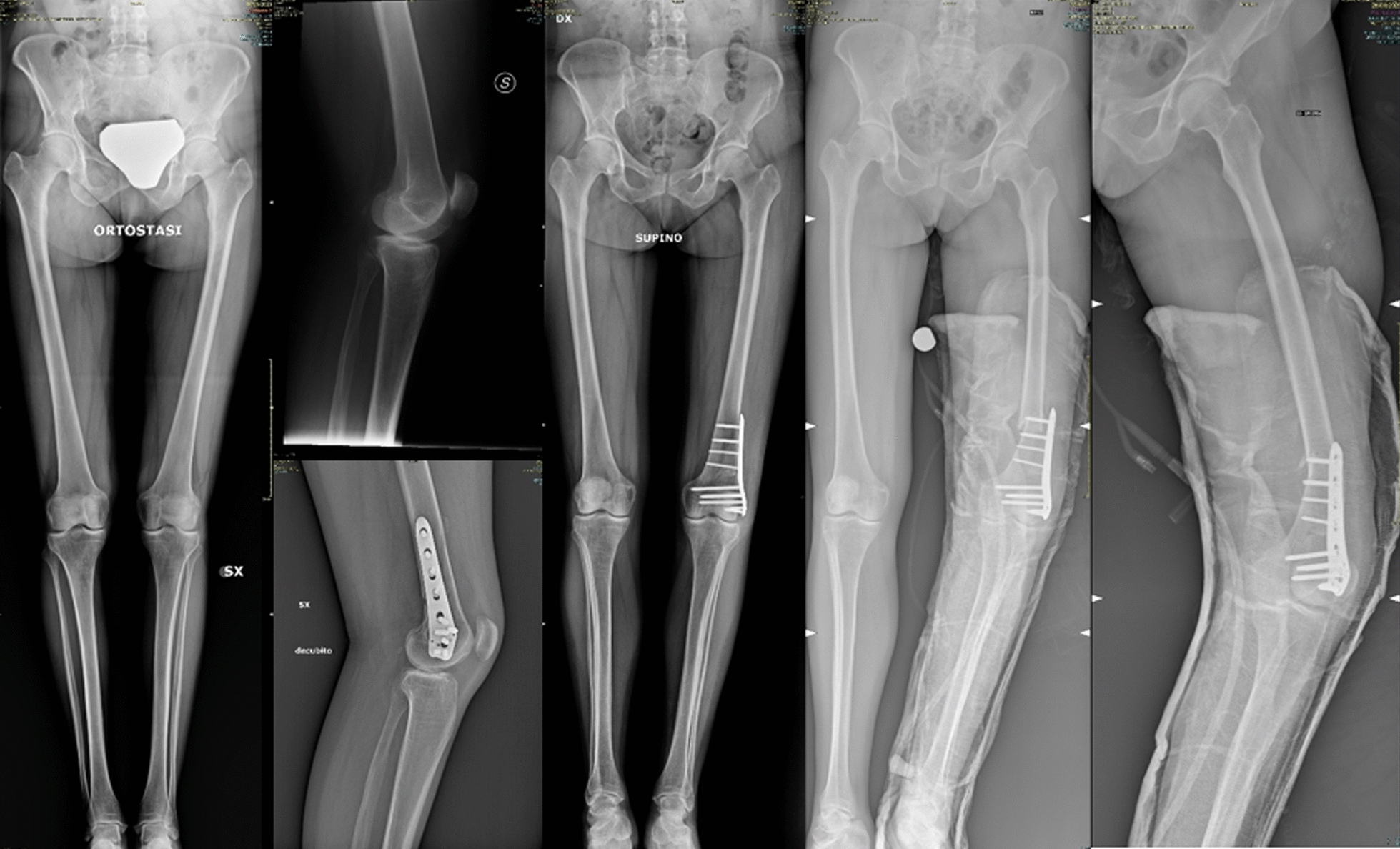
X rays showing preoperative imaging, postoperative imaging, and post fracture imaging
Fig. 2.
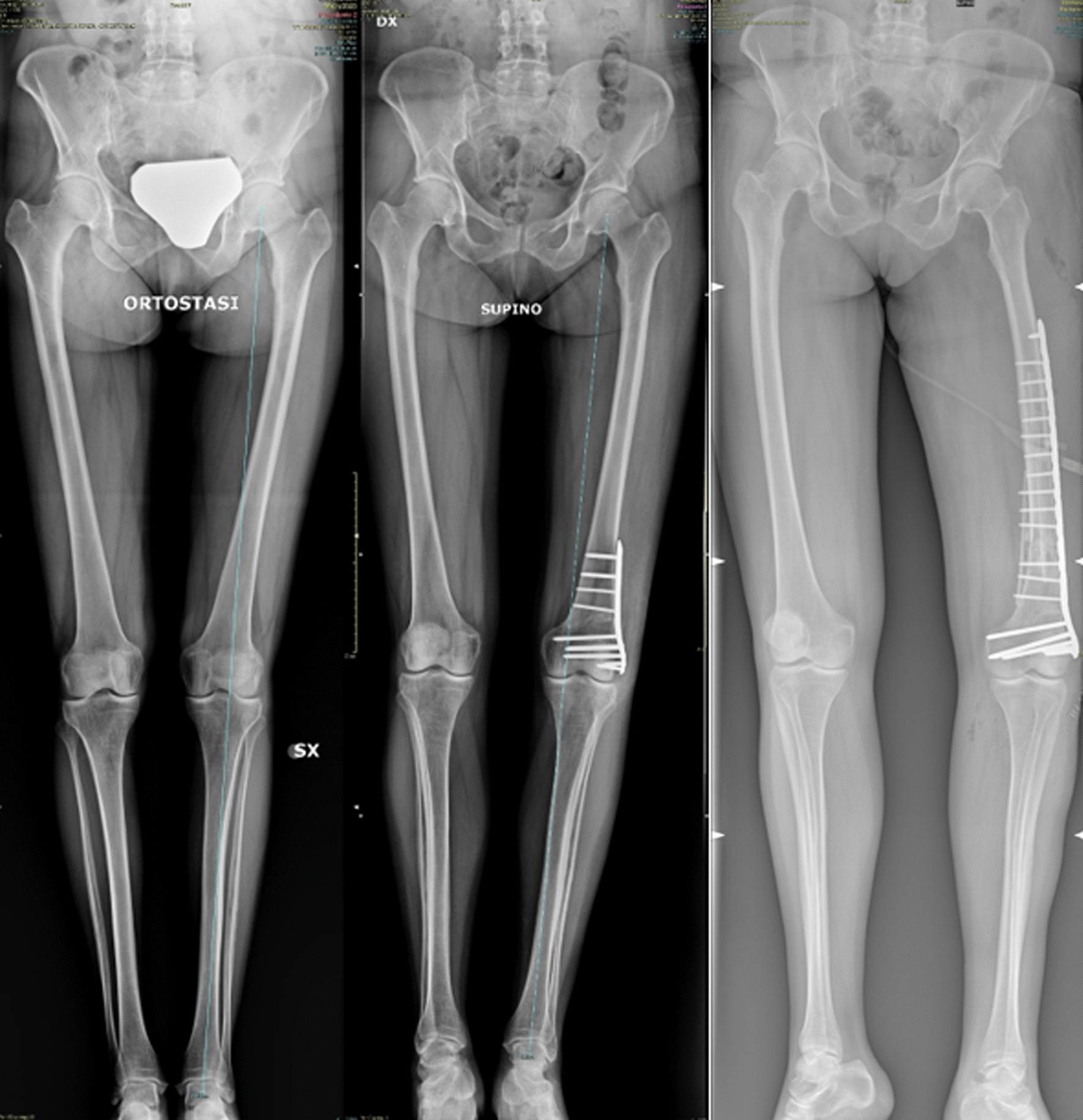
From left to right: preoperative standing X-ray imaging, post distal femoral osteotomy standing X-ray imaging, and posttraumatic fracture fixation non-weight bearing panoramic X ray of the lower limb
Surgery was performed without any intraoperative complications. The patient developed postoperative anemia requiring a transfusion. No other complications were reported. The patient was discharged after 4 days. The rehabilitation program consisted in a knee brace blocked in extension for 30 days, which was removable to perform mobilization exercises; isometry exercises were allowed after 10 days, along with passive leg mobilization with kinetec device (starting with 0–35°). Flexion over 90° was not permitted in the first month. Finally, no weight bearing walking was allowed on the operated limb, and the blocked brace had to always remain on.
The patient came to visit as scheduled 30 days later in our outpatient clinic: knee ROM was 0–90°, X-rays were taken (Fig. 1 center), and she was prescribed progressive weight bearing for 30 days, physiotherapy (muscular reinforcement) two times a week, and maximum permitted-kinetec-assisted passive flexion for 45 days.
Then, 20 days later the patient presented to our emergency room (ER) referring a sudden failure of the knee while walking, followed by pain, swelling, and functional impotence. X-rays (Fig. 1, right) revealed a displaced distal femur fracture. The patient was therefore hospitalized, and surgery was scheduled. The patient also brought to our attention a recent preoperative dual-energy X-ray absorptiometry (DEXA) scan showing a −2,5 T score, which was not considered before, because of her young age.
At 6 days after admission, surgery was performed. By laterally accessing the femur, after retracting fascia lata, muscular fascia, and lateral vastus, a multifragmentary displaced fracture, proximal to the previously applied plate was reported. By protecting the previous osteotomy site with k-wires, we removed the plate and its screws. A structural fibular graft was then placed inside the femoral canal. A LCP condylar 16 hole (336 mm) plate was placed after anatomical reduction of the stumps. We placed both locking and nonlocking screws, using a second contralateral fibular graft. Surgery was performed without any complications.
During hospitalization venous bleeding led to multiple transfusions. No other complications were reported. Physiotherapy started 3 days later: no weight bearing on the affected limb and knee brace blocked in extension.
The patient was dismissed 5 days after surgery.
The patient came to visit in our outpatient clinic after 21 days. Stitches were removed and the surgical wound had healed properly. She was given indication to start rehabilitation: progressive weight bearing with crutches. Postoperative X-rays at 1 month showed good progression in bone healing and good positioning of the plate (Fig. 3). The patient was very satisfied with the result. After 6 months from the first surgery, the patient would like to correct the other limb alignment too.
Fig. 3.

X-ray imaging showing plate fixation at 1 month follow up
Discussion and conclusion
No superiority between opening and closing wedge DFO has been found in literature; however, Rosso et al. [7] reported higher intraoperative precision regarding correction and less postoperative plate intolerance with open wedge techniques. Literature reports high variability in complications after opening wedge DFO procedures, ranging from 0% to 30%, the main consisting of hardware related issues [2]. This one is included among early postoperative complications and can compromise surgery, because, as Chahla et al. [2] reported in his systematic review, bone healing time can range from 3 to 6 months. Berk et al. (2023) reported higher rates of early complications in DFO when compared with HTO (11.6% versus 21.5%), suggesting that this procedure may need a strict follow up, especially in the first months. This may be because DFO are performed closer to diaphyseal bone when compared with HTO, and growth potential differs between these areas [6]. We presented the case of a distal femoral fracture after an opening wedge DFO, which occurred only 2 months after the procedure. Despite that, alignment, and healing of the bone in the site of osteotomy were not compromised; still, this complication must be defined as early and hardware related, because the length of the plate caused anomalous distribution of force vectors along the bone stock, defining a locus minoris resistantiae just above the plate itself. According to a 2013 systematic review of Vena et al. analyzing complications after osteotomies, fractures usually happen around the site of wedge opening or just below, with the fracture line directed toward the articular portion and are seen intraoperatively or as late complications. To our knowledge, there are no other cases describing an early fracture above the opening wedge in a low-density bone patient. No studies considered the link between osteoporosis and osteotomies owing to the relatively young age of patients undergoing this procedure (better outcomes in patients < 60 years) [9]. This study could suggest that bone density should be considered in patients who are at risk of osteoporosis. Our case lacked the recognition of preoperative preexisting osteoporosis, which is well known to be linked to multiple sclerosis, such as some fracture patterns, as Yazdan Panah et al. [11] highlighted. Moreover, we must consider that the population is growing progressively older in first world countries and patients might refuse a knee replacement asking for an axis correction (as in osteotomies) if their functional requests are high.
Well known associated risk factors are age > 45 years, diabetes mellitus, chronic obstructive pulmonary disease, and smoking [4] and are related to failure of the procedure, mainly influencing soft tissue healing but also favoring infection. Moreover, high body mass index, hypertension, and dependent functional status were found to be risk factors [3]. Our patient did not present any of these risk factors, apart from dependent functional status. This evidence could suggest that we should improve our knowledge in this field to avoid complications such as in this case.
According to Berk et al. The most common complications after DFO are anemia requiring transfusion (14%) and readmission (4%). Our patient developed both.
Existing literature already evaluated outcomes of DFO in patients affected by monocompartimental osteoarthritis. Gait analysis is a valuable tool in this field. Regarding valgus correction, it is known that it can cause an increase in the abduction moment and a lateral shift in the dynamic knee joint loading. Varus osteotomies have less literature regarding these aspects, but recent studies seem to suggest that knee adduction moment can increase similarly. It is also well known that the peak knee flexion moment is strongly related to walking speed [10]. No literature exists regarding abnormal distribution of forces on the bone stock after surgeries in patients affected by neurodegenerative diseases. More specifically, no studies evaluated the link between abnormal gait and complications after DFO. Current literature suggests that coronal forces could prevail on other plane vectors during normal gait, above all when a slow gait or an intra-external rotated lower limb axis is considered. In our case, we had both a slow and wide gait, which could have led coronal forces to strongly overcome bone elastic module. Moreover, out patient’s bone was osteoporotic. We chose a Tomofix® plate, because, as Rosso et al. [7] reported that, despite no clinical superiority being found, biomechanically it has greater axial and torsional stability. Positioning a too short plate, such as Tomofix® ones commonly used for osteotomies, on an osteoporotic bone, can elicit peri-implant fractures. Abnormal gait, including poor coordination and balance issues, eventual spasticity, and widening of the docking station typical of neurodegenerative condition affected patients, may add a further risk factor. In these cases, we suggest applying a longer plate and eventually, if other risk factors are highlighted, a contralateral fibular strut on the other side primarily favoring bone regrowth.
Custom guides for osteotomies are becoming more and more popular among orthopedic surgeons, focusing above all on axis realignment, leaving aside how force vectors will distribute after our cuts. New vectors could destabilize previous bone deficiencies leading to surgical failures.
Increasing literature is emerging about distal femur fractures treated with fibular grafts and plating, showing promising results. Wen Chin Su [8] and Ibrahim [5] show that this application may have lower bone healing time and postoperative nonunion or femur collapse in varus rates, particularly when patients are older than 50 years, with a lower bone density (not necessarily pathological). Our patient resembled these risk factors; therefore, we applied the same type of cautions.
The overall aim of this case report is to provide a lesson to surgeons who want to perform a realignment surgery of the lower limb in patients with abnormal gait. Not only mechanical axes are to be considered, but also bone density, patient’s gait and load force distribution along the bone stock. Emerging literature on three-dimensional cutting guides fail to account for these factors, thus promoting a standardized approach to surgery across all patients. The present case highlights a patient with low bone density and abnormal force distribution resulting from a pathologic neurodegenerative gait. In such cases, treatment decisions must carefully consider the biomechanical vulnerabilities of the native bone and the distribution of vector forces. These conditions must guide the choice toward a longer plate if an osteotomy is indicated, because surgery is more likely to fail.
This case report has some limitations. First, follow up time is limited: a long-term follow could provide better clinical and radiographical data. Moreover, we expect this patient to experience a progressive neurological decay, which will affect our outcome in a nonpredictable and measurable way. We also did not report clinical scores prior to surgery.
Acknowledgements
Not applicable.
Author contributions
Each author contributed to the article: GMMM performed the surgery, conceived and designed the paper, and revised the paper; AF contributed data and wrote the paper; SZ conceived and designed the paper and revised the paper.
Funding
Not applicable.
Availability of data and materials
All the data discussed in the manuscript are in the databases of Istituto Ortopedico Rizzoli.
Declarations
Ethical approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Brouwer RW, Huizinga MR, Duivenvoorden T, van Raaij TM, Verhagen AP, Bierma-Zeinstra MA. Osteotomy for treating knee osteoarthritis. Cochrane Database Syst Rev. 2014. 10.1002/14651858.CD004019.pub4. 10.1002/14651858.CD004019.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chahla J, Mitchell JJ, Liechti DJ, Moatshe G, Menge TJ, Dean CS. Opening- and closing-wedge distal femoral osteotomy. Orthopaedic J Sports Med. 2016. 10.1177/2325967116649901. 10.1177/2325967116649901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cotter EJ, Gowd AK, Bohl DD, Getgood A, Cole BJ, Frank RM. Medical comorbidities and functional dependent living are independent risk factors for short-term complications following osteotomy procedures about the knee. Cartilage. 2020. 10.1177/1947603518798889. 10.1177/1947603518798889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Early Postoperative Complications and Associated Variables After High Tibial Osteotomy and Distal Femoral Osteotomy—Cerca con Google. Consultato 5 ottobre 2023. https://www.google.com/search?q=Early+Postoperative+Complications+and+Associated+Variables+After+High+Tibial+Osteotomy+and+Distal+Femoral+Osteotomy&oq=Early+Postoperative+Complications+and+Associated+Variables+After+High+Tibial+Osteotomy+and+Distal+Femoral+Osteotomy&gs_lcrp=EgZjaHJvbWUyBggAEEUYOTIGCAEQRRg80gEHMjgyajBqN6gCALACAA&sourceid=chrome&ie=UTF-8. [DOI] [PubMed]
- 5.Ibrahim FM, El Ghazawy AK, Hussien MA. Primary fibular grafting combined with double plating in distal femur fractures in elderly patients. Int Orthopaedic. 2022. 10.1007/s00264-022-05441-x. 10.1007/s00264-022-05441-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jacobi M, Wahl P, Bouaicha S, Jakob RP, Gautier E. Distal femoral varus osteotomy: problems associated with the lateral open-wedge technique. Archiv Orthopaedic Trauma Surg. 2011. 10.1007/s00402-010-1193-1. 10.1007/s00402-010-1193-1 [DOI] [PubMed] [Google Scholar]
- 7.Rosso F, Margheritini F. Distal femoral osteotomy. Current Rev Musculoskeletal Med. 2014. 10.1007/s12178-014-9233-z. 10.1007/s12178-014-9233-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Su WC, Tzai-Chiu Y, Peng CH, Liu KL, Wen-Tien W, Chen IH, Wang JH, Yeh KT. Use of an intramedullary allogenic fibular strut bone and lateral locking plate for distal femoral fracture with supracondylar comminution in patients over 50 years of age. Medicina. 2022. 10.3390/medicina59010009. 10.3390/medicina59010009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vena G, D’Adamio S, Amendola A. Complications of osteotomies about the knee. Sports Med Arthrosc Rev. 2013. 10.1097/JSA.0b013e3182900720. 10.1097/JSA.0b013e3182900720 [DOI] [PubMed] [Google Scholar]
- 10.van Egmond N, et al. Gait analysis before and after corrective osteotomy in patients with knee osteoarthritis and a valgus deformity. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2017. 10.1007/s00167-016-4045-x. 10.1007/s00167-016-4045-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Panah MY, Vaheb S, Ghaffary EM, Shaygannejad V, Zabeti A, Mirmosayyeb O. Bone loss and fracture in people with multiple sclerosis a systematic review and meta analysis. Multiple Sclerosis Related Disorders. 2024. 10.1016/j.msard.2024.105773. 10.1016/j.msard.2024.105773 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data discussed in the manuscript are in the databases of Istituto Ortopedico Rizzoli.


