Abstract
Objective
Cervical epidural steroid injections (ESIs) can provide effective pain management for patients suffering from chronic neck pain due to various pathological changes of the cervical spine. There are several rare adverse effects reported from interventional pain procedures, including persistent hiccups (“singultus”). Based on a limited number of cases, we propose a modified treatment algorithm for this adverse outcome (Fig. 3).
Case report
Singultus has been documented as an adverse effect of interventional pain procedures, including epidural steroid, facet joint, and sacroiliac joint injections. We describe the case of a general contractor who presented to our clinic with chronic neck pain and central canal stenosis. The patient received an uncomplicated lumbar ESI in the past and was recommended for a cervical interlaminar ESI. After an uneventful C6-C7 interlaminar ESI with dexamethasone, 1% lidocaine, and normal saline the patient developed singultus. Baclofen was sent to his pharmacy, but this was unsuccessful at alleviating his hiccups. The patient was subsequently started on chlorpromazine and found relief from his symptomatology.
Conclusion
Persistent hiccups after ESI or interventional pain procedures can be treated with conservative measures and non-pharmacologic methods, with escalation to therapy with baclofen, gabapentin, pregabalin, metoclopramide, chlorpromazine, other antipsychotic or antidopaminergic agents, and possible dual or triple therapy if further indicated.
Keywords: Singultus, Hiccups, Adverse effect, Interventional pain procedures, Pain management
Background
Hiccups, also known as “singultus,” are a common physiologic occurrence resulting from sudden contraction of the diaphragm and intercostal muscles. This sudden contraction leads to direct closure of the glottis, resulting in the characteristic “hic” sound accompanying the popular term. While most cases of singultus are short lived, others may persist and cause great discomfort in patients. Indeed, the exact pathophysiologic mechanism underlying hiccups is complex and may be due to irritation of a reflex arc along its pathway. The arc itself contains afferents from the phrenic, vagus, and sympathetic nerves (T6 – T12) to the central processing area in the midbrain with efferents in the motor fibers of the phrenic and accessory nerve [1].
Various pharmacologic agents may contribute to the development of singultus, such as corticosteroids, benzodiazepines, and tramadol [2, 3]. However, there is insufficient evidence for any medication to be causative in the etiology of hiccups [2]. Hiccups have even been reported as a postoperative occurrence or with asymptomatic cases of COVID-19 [4, 5]. Furthermore, interventional procedures for the treatment of chronic pain conditions have been instigated in the development of hiccups. The current literature includes cases of singultus after epidural steroid injections (ESIs), facet joint injections, sacroiliac joint injections, and with intrathecal morphine pump use [6]. We present the case of a general contractor who developed singultus after an otherwise uneventful cervical ESI and a previously uncomplicated lumbar ESI. The patient gave written consent for publication of this report.
Case presentation
A 49-year-old general contractor with a past medical history of diabetes, a benign parotid mass, and chronic neck pain presented to our institution’s chronic pain management center for further evaluation and treatment. The patient’s neck pain began a few years prior and gradually worsened. It was associated with radiation to his right elbow and lateral forearm, with positional numbness in the thumb. He had attempted conservative management with over-the-counter analgesics, physical therapy, a home exercise program, and chiropractic adjustments. These treatments were unsuccessful at alleviating his neck pain. He had received an uncomplicated lumbar ESI in the past from an external facility, which alleviated prior back pain complaints.
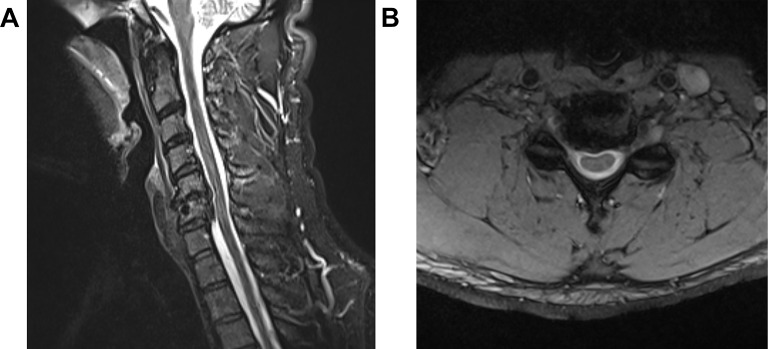
On physical examination, the patient had no associated motor deficits and a magnetic resonance imaging (MRI) scan of his cervical spine demonstrated multilevel spondylosis, facet arthrosis, and right foraminal stenosis, especially at the C6 vertebrae (Fig. 1).
Fig. 1.
(A) MRI of the cervical spine demonstrating multilevel spondylosis and central canal stenosis. (B) MRI of the cervical spine demonstrating foraminal stenosis of the C6 exiting nerve roots
The recommendation was made for a cervical interlaminar ESI under conscious sedation. A C6-C7 interlaminar ESI with 10 milligrams (mg) of dexamethasone, 10 mg of 1% lidocaine, and 3 milliliters of preservative-free normal saline was performed under fluoroscopic-guidance. Appropriate epidural spread was visualized by injection of iohexol 300 (Fig. 2) and there was no evidence of vascular uptake or cerebrospinal fluid leakage. The patient did not experience any paresthesias during or after the procedure.
Fig. 2.

Demonstration of contrast spread into the epidural space via a C6 – C7 interlaminar approach
However, within a few hours after the procedure he developed unrelenting hiccups. This continued while the patient recovered at home, and he ultimately called on postprocedural day five complaining of difficulty eating and dyspnea. The patient was sent to the Emergency Department to rule out urgent or emergent causes (e.g., vertebral artery dissection, meningitis, hematoma formation, spinal cord infarction or stroke), which was done via brain and cervical spine MRI imaging. Physical examination and neurological examination were also unremarkable at this point, and he was diagnosed with persistent singultus. A prescription for baclofen 5 mg up to 10 mg three times daily was sent to his preferred pharmacy. The patient called again on postprocedural day ten with continual hiccups and new complaints of reflux and nausea, which presumably developed because of his reduced food intake. A new prescription for chlorpromazine 25 mg up to three times daily was sent and the patient was instructed to discontinue the baclofen. After two days of therapy and nearly twelve days after his ESI, his hiccups, dyspnea, nausea, and reflux had all resolved.
Discussion
Hiccups are attributable to a diverse array of etiologies, with over 100 documented in the current literature. The foremost culprits include gastrointestinal causes such as gastroesophageal reflux disease [7], while other cases point to cerebrovascular events, intracranial tumors, meningitis or encephalitis, renal dysfunction, metabolic irregularities, and psychosomatic triggers like stress or excitement [8]. Notably, surgical procedures impacting the thorax or upper abdomen, along with endoscopy, have also been implicated in the development of singultus. The estimated incidence of singultus after ESIs stands at 0.5% [9]. Singultus is categorized by duration, with most sources defining it as “persistent” if it lasts beyond 48 h and “intractable” if it persists over a month [8]. While existing literature commonly reports isolated episodes of post-injection singultus, recurring cases following multiple ESIs is limited.
It appears that persistent hiccups result from ESIs with betamethasone, methylprednisolone, triamcinolone, and dexamethasone, regardless of whether local anesthetic was used [6, 10–12]. Notably, hiccups have even been triggered by oral, intravenous, and intra-articular steroid administration [13]. Switching steroids during repeat ESIs has shown potential to prevent reoccurrence of singultus [6]. However, the literature even suggests that some cases of post-epidural injection hiccups may be linked to local anesthetic use without correlation to steroids [14]. Singultus has been associated with ESIs across the cervical, thoracic, and lumbar spine, suggesting no discernible correlation with the level of blockade [15]. Despite uncertainty about the injectate and approach employed during our patient’s prior lumbar ESI, the patient reported no complications from the procedure in the past.
The exact mechanism behind singultus that results from epidural injections remains unclear. One theory dictates that the volume of injectate might play a role via dural sac compression or alteration of cerebrospinal fluid volume, composition, and pressure [16]. Other theories propose corticosteroid interaction with receptors in the reflex arc or direct stimulation of nerves like the phrenic or vagus nerve [11, 17]. Steroids may also potentially lower the threshold for synaptic transmission in the midbrain, triggering hiccups [18]. Local anesthetic use could also induce sympathetic blockade and subsequent parasympathetic hyperactivity [10]. Central neurotransmitters involved in the pathophysiology of hiccups include GABA, dopamine, and serotonin, whereas epinephrine, norepinephrine, acetylcholine, and histamine play peripheral roles [19].
Refractory hiccups are typically managed progressively, starting with non-pharmacologic approaches, with escalation to pharmacologic therapy and potentially invasive methods such as vagus nerve stimulation [20], peripheral nerve stimulation, or phrenic nerve blockade [21, 22]. Intriguingly, continuous cervical epidural administration of ropivacaine (via a catheter at the C3–C5 level) demonstrated efficacy in treating hiccups resistant to pharmacologic treatment in 28 patients [23]. This paradoxical finding underscores the multifactorial nature of this rare phenomenon.
Proposed non-pharmacologic therapies and “cures” for singultus encompass various approaches involving nasopharyngeal stimulation (e.g., inhalation of smelling salts, uvular stimulation), glottic stimulation (e.g., drinking multiple sips of water, chewing lemon, inhaling pepper), vagal maneuvers (e.g., fright induction, application of cold compresses), or respiratory techniques (e.g., breath-holding, rebreathing) [8]. Other options involve hypnosis, massage, electrotherapy, and acupuncture (i.e., auricular), although limited bias-free studies exist on acupuncture due to undefined study population characteristics [24].
A lack of high-quality evidence hampers advocating a specific pharmacologic treatment for singultus [1]. Proton-pump inhibitors like omeprazole have been suggested as first-line therapy for persistent hiccups since as many as 80% of cases may be related to gastroesophageal reflux disease [25]. Baclofen, gabapentin, pregabalin, metoclopramide, and chlorpromazine are also considered effective treatments for singultus [8]. Other agents such as antipsychotics or antidopaminergics are recommended based on anecdotal cases [25], and combination therapy can also be considered [26]. Since baclofen, gabapentin, and pregabalin have a lower side effect profile they are typically recommended after proton-pump inhibitors, with metoclopramide, then chlorpromazine following. However, chlorpromazine is the only pharmacologic agent approved by the United States Food and Drug Administration for the treatment of hiccups. Chlorpromazine antagonizes dopamine in the hypothalamus, which may contribute to its role in treating singultus.
In our case, the decision to initiate baclofen followed by chlorpromazine for pharmacologic treatment was based on the available literature. Baclofen monotherapy has been shown to alleviate intractable hiccups [27], even those developed after ESI [28]. Additionally, in one case report chlorpromazine 10 mg every six hours resolved singultus after a cervical ESI by the following day [11]. In the case series by Abbasi et al. one patient experienced complete resolution of hiccups after one dose of chlorpromazine 10 mg, whereas another failed metoclopramide therapy and experienced resolution after starting chlorpromazine. However, in another case, a patient received haloperidol 5 mg, metoclopramide 10 mg, and gabapentin 300 mg every eight hours for singultus following a cervical ESI. Despite treatment by three agents, the patient experienced no relief, and the hiccups gradually resolved thirteen days after the procedure [15]. The literature suggests that this adverse outcome is typically resolved with pharmacologic treatment or self-limited to two weeks. Reassuringly, singultus that develops after an ESI does not appear to necessitate invasive treatments such as vagus nerve stimulation or phrenic nerve blockade.
An intriguing consideration is whether singultus is more commonly associated with cervical, thoracic, or lumbar ESIs and whether the approach matters (i.e., interlaminar versus transforaminal). In our case, the patient had an uncomplicated lumbar ESI, but developed persistent singultus after a cervical interlaminar ESI. The case series by Abbasi et al. reported persistent hiccups after two cervical and five lumbar ESIs, with the cervical ESIs using an interlaminar approach and four of the five lumbar ESIs using a transforaminal approach. Abubaker et al. reported a case after a cervical ESI and purported that there is no association between the level of injection and the development of singultus. Given that singultus can even occur after a sacral transforaminal ESI [28], sacroiliac joint injection [6], and caudal ESI [29] this statement likely holds true. It is interesting to note, however, that of the reported cases there is a slightly higher predominance of singultus following ESIs in individuals 65 years or younger [6, 10–12]. Recently, singultus has been reported after ESIs in patients greater than 65 years of age [28, 30]. While there could be many reasons to explain this finding, there is no conclusive evidence as to why this association exists. Furthermore, persistent hiccups occur more frequently in men than women [31]. This gender predisposition may be due to easier excitability of afferent or efferent nerves in the hiccup reflex arc, but further epidemiologic studies are warranted.
Given that hiccups can emerge after diverse interventional pain procedures and can be distressing to patients, a modified management algorithm was devised for patients experiencing singultus (Fig. 3).
Fig. 3.
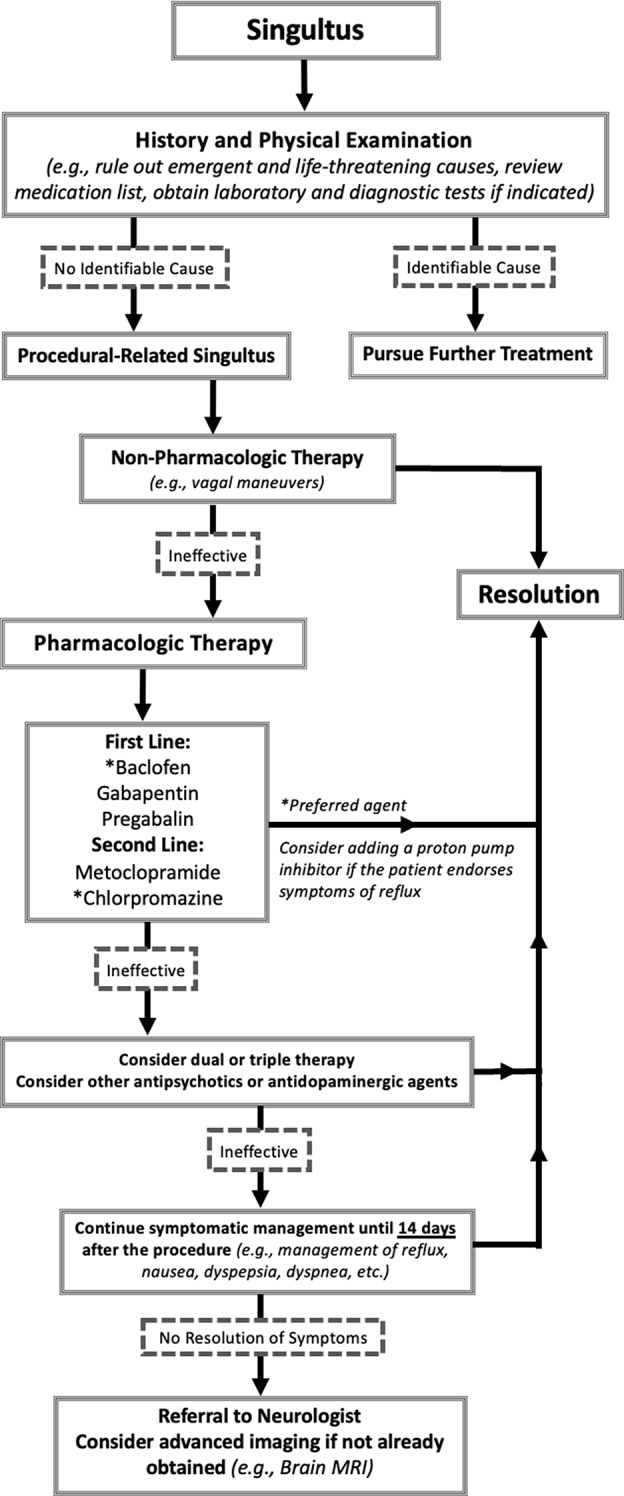
Modified management algorithm for singultus after interventional pain procedures
Although there is limited supporting data to advocate for a specific pharmacologic treatment [1], historically baclofen, gabapentin, pregabalin, metoclopramide, and chlorpromazine have been recommended for singultus. However, given that many pain management patients are already on gabapentin and pregabalin, baclofen may be a better first-line agent unless there is concern over its potential side effects. Baclofen has been shown to lead to full cessation of persistent hiccups within the first six days of treatment in 34 of 35 cases, whereas Gabapentin led to cessation in 81 of 83 cases with a duration of therapy ranging up to six months [32]. Furthermore, if patients fail treatment with any first-line agent chlorpromazine should be elected since it is the only medication approved for this indication and has shown efficacy in previous reported cases [6, 11]. Patients treated with chlorpromazine should be monitored due to a higher risk for side effects such as sedation, palpitations, syncope, extrapyramidal symptoms, and dermatologic reactions [33]. If a patient complains of reflux there should be a strong consideration for a proton-pump inhibitor such as omeprazole [1, 25].
Providers should counsel patients that singultus is a rare adverse effect of ESIs and should be ready to treat the outcome should it occur. Given that singultus typically resolves with pharmacologic therapy or within a couple weeks after the ESI, providers should refer patients to other specialists, including a Neurologist, if symptoms continue beyond this timeframe. Advanced imaging should be considered in any patient with refractory singultus after an image-guided pain procedure.
Conclusions
Persistent hiccups after ESI or interventional pain procedures can be treated with conservative measures and non-pharmacologic methods, with escalation to therapy with baclofen, gabapentin, pregabalin, metoclopramide, chlorpromazine, other antipsychotic or antidopaminergic agents and possible dual or triple therapy if further indicated. Hiccups are a rare occurrence after ESIs at any level, and patients should be advised that they are benign and have been reported to resolve after conservative and pharmacologic therapy. Patients should also be counseled that hiccups can occur even if prior epidural steroid injections were tolerated without adverse effects.
Acknowledgements
The authors would like to thank the staff employed at the Stony Brook Center for Pain Management and the patients who continue to pursue care at the center.
Author contributions
SM constructed the initial manuscript and compiled the figures. SM and AR participated in further editing of the manuscript. AK and WC provided guidance during the process and were the supervising physicians. All authors had a final review of the manuscript.
Funding
The authors have no sources of funding to declare for this manuscript.
Data availability
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable for this case report.
Consent for publication
The patient in this case report provided informed consent. Prior to the inclusion of their medical history, case details, and treatment outcomes, the patient was informed about the purpose and scope of the manuscript. They were made aware that their identity would remain confidential, and any personally identifiable information would be appropriately anonymized to protect privacy. The patient was given the opportunity to ask questions and seek clarification on any aspect of the publication process. Their consent was obtained without coercion and with a clear understanding of the case’s contribution to medical knowledge and research. This informed consent process adhered to all ethical and legal standards for patient confidentiality and research publication.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rouse S, Wodziak M. Intractable hiccups. Curr Neurol Neurosci Rep. 2018;18(8):51. 10.1007/s11910-018-0856-0 [DOI] [PubMed] [Google Scholar]
- 2.Thompson DF, Landry JP. Drug-induced hiccups. Ann Pharmacother. 1997;31(3):367–9. 10.1177/106002809703100318 [DOI] [PubMed] [Google Scholar]
- 3.Panchal R, Bhutt V, Anovadiya A, Purohit B, Dekhaiya F, Goswami N. Tramadol-Induced hiccups: a report of two cases. Drug Saf Case Rep. 2018;5(1):3. 10.1007/s40800-017-0066-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bryer E, Bryer J. Persistent postoperative hiccups. Case Rep Anesthesiol. 2020;2020:8867431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atiyat R, Veeraballi S, Al-Atiyat N, Chan KH, Slim J. A rare case report of persistent hiccups as an atypical presentation of COVID-19. Cureus. 2021;13(3):e13625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abbasi A, Roque-Dang CM, Malhotra G. Persistent hiccups after interventional pain procedures: a case series and review. Pm r. 2012;4(2):144–51. 10.1016/j.pmrj.2011.09.005 [DOI] [PubMed] [Google Scholar]
- 7.de Hoyos A, Esparza EA, Cervantes-Sodi M. Non-erosive reflux disease manifested exclusively by protracted hiccups. J Neurogastroenterol Motil. 2010;16(4):424–7. 10.5056/jnm.2010.16.4.424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steger M, Schneemann M, Fox M. Systemic review: the pathogenesis and pharmacological treatment of hiccups. Aliment Pharmacol Ther. 2015;42(9):1037–50. 10.1111/apt.13374 [DOI] [PubMed] [Google Scholar]
- 9.Lee GY, Lee JW, Yeom JS, Kim KJ, Shin HI, Kang HS. The incidence of various types of systemic reactions related to Epidural Steroid injections: a prospective observational study. Korean J Radiol. 2018;19(2):301–10. 10.3348/kjr.2018.19.2.301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Slipman CW, Shin CH, Patel RK, Braverman DL, Lenrow DA, Ellen MI, et al. Persistent hiccup associated with thoracic epidural injection. Am J Phys Med Rehabil. 2001;80(8):618–21. 10.1097/00002060-200108000-00014 [DOI] [PubMed] [Google Scholar]
- 11.Ritz ML, Bailey C, Overstreet K, Gorlin A. Persistent hiccups following cervical epidural steroid injection with betamethasone. Int Med Case Rep J. 2018;11:263–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beyaz SG. Persistent hiccup after lumbar epidural steroid injection. J Anaesthesiol Clin Pharmacol. 2012;28(3):418–9. 10.4103/0970-9185.98383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sugandhavesa N, Sawaddiruk P, Bunmaprasert T, Pattanakuhar S, Chattipakorn SC, Chattipakorn N. Persistent severe hiccups after Dexamethasone Intravenous Administration. Am J Case Rep. 2019;20:628–30. 10.12659/AJCR.915282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McAllister RK, McDavid AJ, Meyer TA, Bittenbinder TM. Recurrent persistent hiccups after epidural steroid injection and analgesia with bupivacaine. Anesth Analg. 2005;100(6):1834–6. 10.1213/01.ANE.0000153016.82444.20 [DOI] [PubMed] [Google Scholar]
- 15.Abubaker AK, Rabadi DK, Kassab M, Al-Qudah MA. Persistent hiccups after cervical epidural steroid injection. Am J Case Rep. 2018;19:397–9. 10.12659/AJCR.908536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higuchi H, Adachi Y, Kazama T. Effects of epidural saline injection on cerebrospinal fluid volume and velocity waveform: a magnetic resonance imaging study. Anesthesiology. 2005;102(2):285–92. 10.1097/00000542-200502000-00008 [DOI] [PubMed] [Google Scholar]
- 17.Dickerman RD, Overby C, Eisenberg M, Hollis P, Levine M. The steroid-responsive hiccup reflex arc: competitive binding to the corticosteroid-receptor? Neuro Endocrinol Lett. 2003;24(3–4):167–9. [PubMed] [Google Scholar]
- 18.Lee GW, Oh SY, Kang MH, Kang JH, Park SH, Hwang IG, et al. Treatment of dexamethasone-induced hiccup in chemotherapy patients by methylprednisolone rotation. Oncologist. 2013;18(11):1229–34. 10.1634/theoncologist.2013-0224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nausheen F, Mohsin H, Lakhan SE. Neurotransmitters in hiccups. Springerplus. 2016;5(1):1357. 10.1186/s40064-016-3034-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Petroianu GA. Treatment of hiccup by vagal maneuvers. J Hist Neurosci. 2015;24(2):123–36. 10.1080/0964704X.2014.897133 [DOI] [PubMed] [Google Scholar]
- 21.Tariq K, Das JM, Monaghan S, Miserocchi A, McEvoy A. A case report of Vagus nerve stimulation for intractable hiccups. Int J Surg Case Rep. 2021;78:219–22. 10.1016/j.ijscr.2020.12.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arsanious D, Khoury S, Martinez E, Nawras A, Filatoff G, Ajabnoor H, et al. Ultrasound-guided phrenic nerve block for intractable hiccups following Placement of Esophageal Stent for esophageal squamous cell carcinoma. Pain Physician. 2016;19(4):E653–6. 10.36076/ppj/2019.19.E653 [DOI] [PubMed] [Google Scholar]
- 23.Kim JE, Lee MK, Lee DK, Choi SS, Park JS. Continuous cervical epidural block: treatment for intractable hiccups. Med (Baltim). 2018;97(6):e9444. 10.1097/MD.0000000000009444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moretto EN, Wee B, Wiffen PJ, Murchison AG. Interventions for treating persistent and intractable hiccups in adults. Cochrane Database Syst Rev. 2013;2013(1):Cd008768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Polito NB, Fellows SE. Pharmacologic interventions for intractable and persistent hiccups: a systematic review. J Emerg Med. 2017;53(4):540–9. 10.1016/j.jemermed.2017.05.033 [DOI] [PubMed] [Google Scholar]
- 26.Petroianu G, Hein G, Petroianu A, Bergler W, Rüfer R. Idiopathic chronic hiccup: combination therapy with cisapride, omeprazole, and baclofen. Clin Ther. 1997;19(5):1031–8. 10.1016/S0149-2918(97)80055-0 [DOI] [PubMed] [Google Scholar]
- 27.Lee JH, Kim TY, Lee HW, Choi YS, Moon SY, Cheong YK. Treatment of intractable hiccups with an oral agent monotherapy of baclofen -a case report. Korean J Pain. 2010;23(1):42–5. 10.3344/kjp.2010.23.1.42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Colorado B, Decker G. Persistent hiccups after an epidural steroid injection successfully treated with Baclofen: a Case Report. Pm r. 2017;9(12):1290–3. 10.1016/j.pmrj.2017.04.013 [DOI] [PubMed] [Google Scholar]
- 29.Kaydu A, Kılıç ET, Gökçek E, Akdemir MS. Unexpected complication after Caudal Epidural Steroid Injection: hiccup. Anesth Essays Res. 2017;11(3):776–7. 10.4103/aer.AER_90_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Odonkor CA, Smith B, Rivera K, Chhatre A. Persistent Singultus Associated with lumbar epidural steroid injections in a septuagenarian: a Case Report and Review. Am J Phys Med Rehabil. 2017;96(1):e1–4. 10.1097/PHM.0000000000000526 [DOI] [PubMed] [Google Scholar]
- 31.Lee GW, Kim RB, Go SI, Cho HS, Lee SJ, Hui D, et al. Gender differences in hiccup patients: analysis of published case reports and case-control studies. J Pain Symptom Manage. 2016;51(2):278–83. 10.1016/j.jpainsymman.2015.09.013 [DOI] [PubMed] [Google Scholar]
- 32.Kohse EK, Hollmann MW, Bardenheuer HJ, Kessler J. Chronic hiccups: an underestimated problem. Anesth Analg. 2017;125(4):1169–83. 10.1213/ANE.0000000000002289 [DOI] [PubMed] [Google Scholar]
- 33.Friedgood CE, Ripstein CB. Chlorpromazine (thorazine) in the treatment of intractable hiccups. JAMA. 1955;157(4):309–10. 10.1001/jama.1955.02950210005002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.