Abstract
Background
Although stroke is prevalent among Chinese, individuals with stroke may become more disabling if they have concomitant neck pain (NP) and low back pain (LBP). However, the prevalence and factors associated with post-stroke spinal pain among Chinese remain unknown. The current study used the 2018 cohort data from the China Health and Aged Care Tracking Survey (CHARLS) to determine the prevalence and factors associated with increased post-stroke NP and LBP in China.
Methods
The CHARLS study was conducted on four cohorts of nationally representative samples of individuals aged 45 years and above from 30 provincial-level administrative units in China. We used data from the 2018 cohort of the CHARLS survey to determine the prevalence and factors associated with NP and LBP in the non-stroke and post-stroke populations. Participants aged 45 years or older who reported to have NP, and/or LBP were identified. The study was statistically analyzed using t-test, and ANOVA analysis of variance. A multiple logistic regression model was used to identify factors significantly associated with NP and/or LBP in the non-stroke and post-stroke populations.
Results
A total of 19,816 individuals participated in the 2018 survey. The final inclusion of 17,802 subjects who met the criteria included 16,197 non-stroke and 885 stroke participants. The prevalence of NP and LBP in non-stroke population was 17.80% (95% CI: 17.21–18.39) and 37.22% (95% CI: 36.47–37.96), respectively. The prevalence of NP and LBP in the target stroke population was 26.44% (95% CI: 23.53–29.35) and 45.42% (95% CI: 42.14–48.71), respectively, and the difference was statistically significant (p < 0.05). Factors associated with increased post-stroke NP included female, short sleep duration, long lunch break, physical dysfunction, and depression. Factors associated with increased post-stroke LBP included female, comorbidities of two or more chronic diseases, physical dysfunction, and depression.
Conclusion
The current study highlighted the high prevalence of post-stroke neck pain (26.44%) and LBP (45.42%) in China. While slightly different associated factors were found to be associated with a higher prevalence of post-stroke NP and LBP, female and individuals with more physical dysfunction or depression were more likely to experience post-stroke spinal pain. Clinicians should pay more attention to vulnerable individuals and provide pain management measures.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-19847-2.
Keywords: Stroke, Neck pain, Low back pain, Population-based study, Prevalence
Introduction
Stroke is one of the non-communicable diseases causing massive economic and medical burdens in China. Stroke has been the leading cause of death in China since 2015 [1], and it accounts for almost one-third of all stroke deaths worldwide [2]. As a major cardiovascular disease, stroke poses a major threat to the physical health of Chinese people. With the intensification of population aging in the past 30 years, the overall incidence of stroke in China has been on the rise [3]. The incidence of cerebrovascular disease events in China is projected to increase by approximately 50% by 2030 as compared to the percentage in 2010 [4]. Stroke is known to cause chronic pain and physical dysfunction in these patients, which seriously affects their quality of life, and increases the medical burden on individuals and the society [5–8]. As the course of stroke prolongs and the condition progresses, the risk of complications in patients with stroke greatly increases [9–14].
Pain is a common post-stroke complication that leads to high morbidity, with approximately 10%–45.8% of stroke survivors experiencing some form of pain [15, 16]. The prevalence of pain in the subacute (42.73%) and chronic (31.90%) phases is higher than that in the acute phase (14.06%) [17]. However, pain is often overlooked by clinicians because of patients’ cognitive impairment or suboptimal communication skills. A retrospective study found that more than one-third of stroke patients with pain did not receive pain treatment [18]. Post-stroke pain can hinder the rehabilitation process and reduce the quality of life of stroke survivors [19–22]. Given the high prevalence of post-stroke pain, a growing number of researchers have studied post-stroke shoulder pain and central post-stroke pain [23, 24]. However, post-stroke can also affect other body parts, such as neck and low back, although the prevalence and factors associated with these pain remain uncertain in China. As such, a nationwide population-based study is warranted to investigate the prevalence and factors associated with NP and LBP in the stroke population in China, which may help identify high risk individuals for timely intervention. Using data from the 2018 China Health and Retirement Longitudinal Study (CHARLS), this study aims to: (1) estimate the prevalence of NP and LBP in Chinese stroke populations aged 45 and above; (2) assess the associated factors of NP and LBP in Chinese stroke populations aged 45 and above.
Methods
Study participants
This study used data from the CHARLS Project, which is sponsored by the National School of Development of Peking University and jointly implemented by the China Social Science Survey Center of Peking University and the Communist Youth League Committee of Peking University. CHARLS adopts strict random sampling. The sampling process involved four stages [25]. At the first stage, a random sample of 150 districts and counties was selected using the probability proportional to size (PPS) method and stratified by regions, urban and rural areas, counties nationwide (excluding Tibet), and GDP per capita. At the second stage, three village level units were randomly selected from each county-level unit using the PPS method. At the third stage, a sample of 24 households was randomly selected based on geographic locations and each PSU list. At the fourth stage, one resident at least 45 years old was randomly selected from a family and interviewed together with their spouse. In consideration of the complexity of the CHARLS survey design and the lack of response rate, weighted values were constructed based on sampling and response probabilities, which were provided by the CHARLS database.
The national baseline survey began in 2011, and follow-up surveys were conducted in 2013, 2015, and 2018. As of 2018, the CHARLS sample had a total of 19,816 respondents from 12,400 households. The present study was a secondary analysis of data from CHARLS. The National Institute of Development Studies at Peking University keeps all data collected by CHARLS, and the dataset is available at http://charls.pku.edu.cn/pages/data/111/zh-cn.
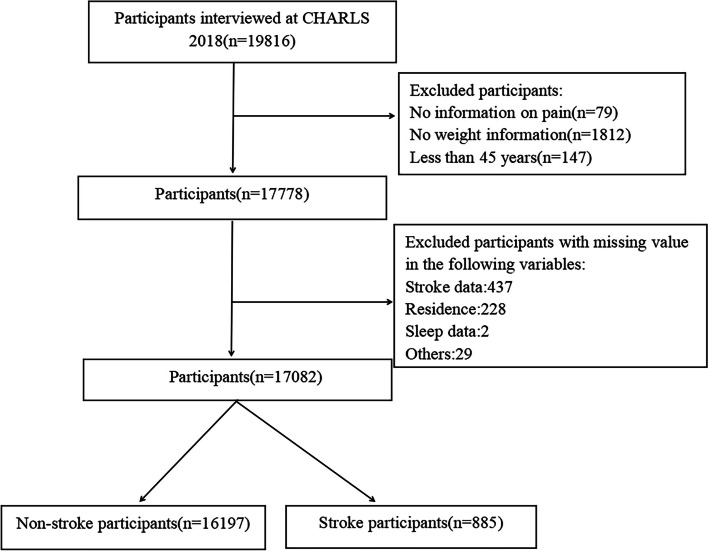
This study analyzed data from 2018 CHARLS cohort. The inclusion criteria were : (1) aged 45 years and above, (2) having information on NP and LBP, and (3) having information on stroke. The exclusion criteria were those with missing other covariates. Of the 19,816 participants included in the 2018 CHARLS cohort, 17,082 (16,197 non-stroke patients and 885 stroke patients) were ultimately included after excluding covariates with missing values. The detailed screening process is shown in Fig. 1.
Fig. 1.
Study flowchart
Measures of demographic characteristics
Trained interviewers used a structured questionnaire to collect participants ’ date of birth, sex, area of residence (rural or urban), and level of education (illiterate, primary school and below, and secondary school and above).
Measures of health status and functioning
The interviewers used a structured questionnaire to collect information on the participants’ sleep duration, nap duration, drinking status (no or yes), physical dysfunction (no or yes), disability (no or yes), impairment in activities of daily living (ADL; no or yes), impairment in instrumental activities of daily living (IADL; no or yes), and physical activity and chronic diseases. In addition, the interviewers asked the participants if they used the following ways to treat or manage post-stroke complications: taking Chinese medicine, taking Western medicine, physical therapy, acupuncture, and rehabilitation therapy.
Measures of cognition and health insurance use
The interviewers collected the participants ’ depression status (no or yes) and health insurance information (no or yes). CHARLS used the Center for Epidemiological Studies Depression Scale (CESD- 10) to measure the psychological status of middle- aged and older people, and those with a total CESD- 10 self-assessment score of 11 and above were classified as having depression [26].
Outcome measures
Stroke event was assessed by the following question: “Have you been diagnosed with stroke by a doctor?”. Participants who reported stroke were defined as having stroke. Pain event was assessed by the following questions: “Are you often troubled with any body pains?” and “What part of your body do you feel pain?”. Participants were defined as having NP and LBP if they answered NP and LBP.
Statistical analysis
Descriptive statistics were used to report the demographic data. Categorical variables were represented by numbers and percentages, and the continuous variables were represented by means and standard deviations. Further, demographics and covariates of the stroke and non-stroke populations with and without NP and LBP were compared. Comparisons between groups were made using independent samples t-tests or analysis of variance (ANOVA). The test level α=0.05, P<0.05 indicates that the difference is statistically significant. Individual factors associated with NP and LBP were determined using one-way logistic regression analysis. Covariates with p-values < 0.2 in the univariate analysis were entered into the multiple logistic regression model with stepwise reverse exclusion. The significance level was set at 0.05 to investigate factors associated with NP and LBP in stroke and non-stroke populations. The odds ratio (OR) and the corresponding 95% confidence interval (CI) was calculated. Sampling weights were applied to the study population to represent the Chinese population without bias. All analyses were conducted using Stata/MP17 software.
Results
The characteristics of participants are shown in Table 1. There were 885 stroke patients, accounting for 5.18% of the total. Their average age was 67.1 (9.1) years. As shown in Table 2, the prevalence of NP and LBP in non-stroke population was 17.80% (95% CI: 17.21–18.39) and 37.22% (95% CI: 36.47–37.96), respectively. The prevalence of NP and LBP in the target stroke population was 26.44% (95% CI: 23.53–29.35) and 45.42% (95% CI: 42.14–48.71), respectively, and the difference was statistically significant (p < 0.05) (See appendix tables S1,S2). In addition, in different age groups, depressed and non-depressed people, the NP and LBP in the stroke population were still higher than those in the non-stroke population. The prevalence of post-stroke NP was higher in females (33.70%, 95% CI: 29.35–38.05) than in males (18.69%, 95% CI: 14.98–22.40). The prevalence of post-stroke LBP was higher in females (57.33%, 95% CI: 52.78–61.88) than in males (32.71%, 95% CI: 28.25–37.17). Significant between-sex differences in prevalence rates of post-stroke NP and LBP existed in all age groups. The rural residents had a lower prevalence of post-stroke NP (26.19%, 95% CI: 22.81–29.57) than the urban counterparts (27.16%, 95% CI: 21.39–32.92), although the rural residents had a higher prevalence of post-stroke LBP (46.40%, 95% CI: 42.57–50.24) as compared to the urban residents (42.67%, 95% CI: 36.26–49.08).
Table 1.
Baseline characteristics of the distribution of all participants by stroke status in Charls 2018
| All study participants (n = 17,082) | No stroke (n = 16,197) | Stroke (n = 885) | |
|---|---|---|---|
| Participants distribution | 100% | 94.82% | 5.18% |
| Mean age, years | 62.57(9.85) | 62.32(9.83) | 67.11(9.11) |
| Age, years | |||
| 45–54 | 4352(25.48%) | 4270(26.36%) | 82(9.27%) |
| 55–64 | 5795(33.92%) | 5535(34.17%) | 260(29.38%) |
| 65–74 | 4683(27.41%) | 4332(26.75%) | 351(39.66%) |
| ≥ 75 | 2252(13.18%) | 2060(12.72%) | 192(21.69%) |
| Gender | |||
| female | 9024(52.83%) | 8567( 52.89%) | 457(51.64%) |
| male | 8058(47.17%) | 7630 (47.11%) | 428(48.36%) |
| Residence | |||
| rural | 13,077(76.55%) | 12,424(76.71%) | 653(73.79%) |
| urban | 4005(23.45%) | 3773(23.29%) | 232(26.21%) |
| Education | |||
| illiterate | 4040 (23.65%) | 3795 (23.43%) | 245 (27.68%) |
| elementary school or below | 7361 (43.09%) | 6982 (23.43%) | 379 (42.82%) |
| secondary school and above | 5681 (33.26%) | 5420 (33.46%) | 261 (29.49%) |
| Disability | |||
| no | 14,984 (87.72%) | 14,356 (88.63%) | 628 (70.96%) |
| yes | 2098 (12.28%) | 1841 (11.37%) | 257 (29.04%) |
| Chronic Disease | |||
| 0 | 9993 (58.5%) | 9643 (59.54%) | 350 (39.55%) |
| 1 | 4637 (27.15%) | 4355 (26.89%) | 282 (31.86%) |
| 2 | 2452 (14.35%) | 2199 (13.58%) | 253 (28.59%) |
| Low back pain | |||
| no | 10,652 (62.36%) | 10,169 (62.78%) | 483 (54.58%) |
| yes | 6430 (37.64%) | 6028 (37.22%) | 402 (45.42%) |
| Neck pain | |||
| no | 13,965(81.75%) | 13,314(82.2%) | 651(73.56%) |
| yes | 3117(18.25%) | 2883(17.8%) | 234(26.44%) |
| Sleep Time | |||
| ≤ 6h | 9347(54.72%) | 8838(54.57%) | 509(57.51%) |
| 6-8h | 6096(35.69%) | 5821(35.94%) | 275(31.07%) |
| ≥ 8h | 1639(9.59%) | 1538(9.5%) | 101(11.41%) |
| Nap Time | |||
| ≤ 30min | 9494(55.58%) | 9039(55.81%) | 455(51.41%) |
| 31-60min | 4287(25.1%) | 4087(25.23%) | 200(22.6%) |
| ≥ 61min | 3301(19.32%) | 3071(18.96%) | 230(25.99%) |
| Dyspraxia | |||
| no | 5090(29.8%) | 4986(30.78%) | 104(11.75%) |
| yes | 11,992(70.2%) | 11,211(69.22%) | 781(88.25%) |
| Depressive | |||
| no | 11,268(65.96%) | 10,762(66.44%) | 506(57.18%) |
| yes | 5814(34.04%) | 5435(33.56%) | 379(42.82%) |
| Drink | |||
| no | 11,366(66.54%) | 10,683(65.96%) | 683(77.18%) |
| yes | 5716(33.46%) | 5514(34.04%) | 202(22.82%) |
| Insurance | |||
| no | 512(3%) | 499(3.08%) | 13(1.47%) |
| yes | 16,570(97%) | 15,698(96.92%) | 872(98.53%) |
| Number of pain | |||
| None | 6669(39.04%) | 6414(39.6%) | 255(28.81%) |
| One | 2062(12.07%) | 1966(12.14%) | 96(10.85%) |
| Two | 1520(8.9%) | 1453(8.97%) | 67(7.57%) |
| Three | 1278(7.48%) | 1210(7.47%) | 68(7.68%) |
| Four or above | 5553(32.51%) | 5514(31.82%) | 399(45.08%) |
| ADL | |||
| no | 13,905(81.4%) | 13,397(82.71%) | 508(57.4%) |
| yes | 3177(18.6%) | 2800(17.29%) | 377(42.6%) |
| ADL_ins | |||
| no | 12,987(76.03%) | 12,561(77.55%) | 426(48.14%) |
| yes | 4095(23.97%) | 3636(22.45%) | 459(51.86%) |
| Activity_intensive | |||
| Less than 10 min | 11,600(67.91%) | 10,895(67.27%) | 705(79.66%) |
| 10 min to 30 min | 168(0.98%) | 157(0.97%) | 11(1.24%) |
| 30 min to 2 h | 1001(5.86%) | 955(5.9%) | 46(5.2%) |
| 2 h to 4 h | 1249(7.31%) | 1219(7.53%) | 30(3.39%) |
| More than 4 h | 3064(17.94%) | 2971(18.34%) | 93(10.51%) |
| Activity_moderate | |||
| Less than 10 min | 8705(50.96%) | 8146(50.29%) | 559(63.16%) |
| 10 min to 30 min | 1025(6%) | 967(5.97%) | 58(6.55%) |
| 30 min to 2 h | 3425(20.05%) | 3276(20.23%) | 149(16.84%) |
| 2 h to 4 h | 1946(11.39%) | 1876(11.58%) | 70(7.91%) |
| More than 4 h | 1981(11.6%) | 1932(11.93%) | 49(5.54%) |
| Activity_light | |||
| Less than 10 min | 2980(17.45%) | 2769(17.1%) | 211(23.84%) |
| 10 min to 30 min | 1650(9.66%) | 1567(9.67%) | 83(9.38%) |
| 30 min to 2 h | 6923(40.53%) | 6574(40.59%) | 349(39.44%) |
| 2 h to 4 h | 3199(18.73%) | 3044(18.79%) | 155(17.51%) |
| More than 4 h | 2330(13.64%) | 2243(13.85%) | 87(9.83%) |
| Taking Chinese traditional medicine | |||
| no | 16,895(98.91%) | 16,197(100%) | 698(78.87%) |
| yes | 187(1.09%) | 0(0%) | 187(21.13%) |
| Taking Western modern medicine | |||
| no | 16,541(96.83%) | 16,197(100%) | 344(38.87%) |
| yes | 541(3.17%) | 0(0%) | 541(61.13%) |
| Physical therapy | |||
| no | 17,042(99.77%) | 16,197(100%) | 845(95.48%) |
| yes | 40(0.23%) | 0(0%) | 40(4.52%) |
| Acupuncture and moxibustion | |||
| no | 17,013(99.6%) | 16,197(100%) | 816(92.2%) |
| yes | 69(0.4%) | 0(0%) | 69(7.8%) |
| Occupational therapy | |||
| no | 17,037(99.74%) | 16,197(100%) | 840(94.92%) |
| yes | 45(0.26%) | 0(0%) | 45(%) |
| Other treatments, please spcify | |||
| no | 16,997(99.5%) | 16,197(100%) | 800(90.4%) |
| yes | 85(0.5%) | 0(0%) | 85(9.6%) |
| None treatment | |||
| no | 16,850(98.64%) | 16,197(100%) | 653(73.79%) |
| yes | 232(1.36%) | 0(0%) | 232(26.21%) |
Table 2.
Prevalence of neck and low back pain by gender in the general Chinese population aged 45 years and above
| Non-stroke Neck pain | Non-stroke Low back pain | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Female | Male | Overall | Female | Male | |||||||
| n | Prevalence (95%CI) | n | Prevalence (95%CI) | n | Prevalence (95%CI) | n | Prevalence (95%CI) | n | Prevalence (95%CI) | n | Prevalence (95%CI) | |
| 16,197 | 17.80%(17.21–18.39) | 8567 | 23.43%(22.53–24.32) | 7630 | 11.48%(10.77–12.20) | 16,197 | 37.22%(36.47–37.96) | 8567 | 43.75%(42.70–44.80) | 7630 | 29.88%(28.85–30.91) | |
| Age, years | ||||||||||||
| 45–54 | 4270 | 18.03%(16.88–19.19) | 2401 | 42.40%(40.42–44.38) | 1869 | 29.59%(27.52–31.66) | 4270 | 36.79%(35.34–38.24) | 2401 | 42.40%(40.42–44.38) | 1869 | 29.59%(27.52–31.66) |
| 55–64 | 5535 | 18.68%(17.65–19.71) | 2880 | 42.92%(41.11–44.73) | 2655 | 30.02%(28.27–31.76) | 5535 | 36.73%(35.46–38.00) | 2880 | 42.92%(41.11–44.73) | 2655 | 30.02%(28.27–31.76) |
| 65–74 | 4332 | 17.84%(16.70–18.98) | 2211 | 45.77%(43.69–47.85) | 2121 | 30.08%(28.13–32.03) | 4332 | 38.09%(36.64–39.54) | 2211 | 45.77%(43.69–47.85) | 2121 | 30.08%(28.13–32.03) |
| ≥ 75 | 2060 | 14.85%(13.32–16.39) | 1075 | 44.84%(41.86–47.81) | 985 | 29.64%(26.79–32.50) | 2060 | 37.57%(35.48–39.67) | 1075 | 44.84%(41.86–47.81) | 985 | 29.64%(26.79–32.50) |
| p value | 0.002 | 0.079 | 0.983 | 0.491 | 0.079 | 0.983 | ||||||
| Residence | ||||||||||||
| rural | 12,424 | 17.85%(17.18–18.53) | 6575 | 45.23%(44.03–46.44) | 5849 | 31.49%(30.30–32.68) | 12,424 | 38.76%(37.91–39.62) | 6575 | 45.23%(44.03–46.44) | 5849 | 31.49%(30.30–32.68) |
| urban | 3773 | 17.63%(16.41–18.84) | 1992 | 38.86%(36.71–41.00) | 1781 | 24.59%(22.59–26.59) | 3773 | 32.12%(30.63–33.61) | 1992 | 38.86%(36.71–41.00) | 1781 | 24.59%(22.59–26.59) |
| p value | 0.749 | 0 | 0 | 0 | 0 | 0 | ||||||
| Education | ||||||||||||
| illiterate | 3795 | 20.66%(19.37–21.95) | 3024 | 45.21%(43.43–46.98) | 771 | 33.07%(29.75–36.40) | 3795 | 42.74%(41.17–44.32) | 3024 | 45.21%(43.43–46.98) | 771 | 33.07%(29.75–36.40) |
| elementary school or below | 6982 | 18.30%(17.40–19.21) | 3440 | 45.64%(43.97–47.30) | 3542 | 32.92%(31.37–34.47) | 6982 | 39.19%(38.04–40.33) | 3440 | 45.64%(43.97–47.30) | 3542 | 32.92%(31.37–34.47) |
| secondary school and above | 5420 | 15.15%(14.19–16.10) | 2103 | 38.56%(36.48–40.65) | 3317 | 25.90%(24.41–27.39) | 5420 | 30.81%(29.58–32.04) | 2103 | 38.56%(36.48–40.65) | 3317 | 25.90%(24.41–27.39) |
| p value | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| Disability | ||||||||||||
| no | 14,356 | 16.50%(15.89–17.11) | 7590 | 42.00%(40.89–43.11) | 6766 | 28.26%(27.19–29.33) | 14,356 | 35.53%(34.74–36.31) | 7590 | 42.00%(40.89–43.11) | 6766 | 28.26%(27.19–29.33) |
| yes | 1841 | 27.92%(25.87–29.97) | 977 | 57.32%(54.21–60.43) | 864 | 42.59%(39.29–45.90) | 1841 | 50.41%(48.12–52.69) | 977 | 57.32%(54.21–60.43) | 864 | 42.59%(39.29–45.90) |
| p value | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| Chronic Disease | ||||||||||||
| 0 | 9643 | 14.03%(13.34–14.72) | 5044 | 37.67%(36.33–39.01) | 4599 | 25.20%(23.95–26.46) | 9643 | 31.72%(30.79–32.65) | 5044 | 37.67%(36.33–39.01) | 4599 | 25.20%(23.95–26.46) |
| 1 | 4355 | 20.48%(19.28–21.68) | 2315 | 50.19%(48.16–52.23) | 2040 | 34.02%(31.96–36.08) | 4355 | 42.62%(41.15–44.09) | 2315 | 50.19%(48.16–52.23) | 2040 | 34.02%(31.96–36.08) |
| 2 | 2199 | 29.01%(27.11–30.91) | 1208 | 56.79%(53.99–59.59) | 991 | 43.09%(40.00–46.18) | 2199 | 50.61%(48.52–52.71) | 1208 | 56.79%(53.99–59.59) | 991 | 43.09%(40.00–46.18) |
| p value | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| Sleep Time | ||||||||||||
| ≤ 6 h | 8838 | 22.22%(21.36–23.09) | 4952 | 49.41%(48.02–50.81) | 3886 | 34.82%(33.32–36.32) | 8838 | 43.00%(41.96–44.03) | 4952 | 49.41%(48.02–50.81) | 3886 | 34.82%(33.32–36.32) |
| 6-8 h | 5821 | 12.61%(11.76–13.46) | 2799 | 36.26%(34.48–38.05) | 3022 | 24.95%(23.41–26.49) | 5821 | 30.39%(29.21–31.57) | 2799 | 36.26%(34.48–38.05) | 3022 | 24.95%(23.41–26.49) |
| ≥ 8 h | 1538 | 12.03%(10.40–13.66) | 816 | 35.05%(31.77–38.33) | 722 | 23.96%(20.84–27.08) | 1538 | 29.84%(27.55–32.13) | 816 | 35.05%(31.77–38.33) | 722 | 23.96%(20.84–27.08) |
| p value | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| Nap Time | ||||||||||||
| ≤ 30 min | 9039 | 19.04%(18.23–19.85) | 5185 | 45.36%(44.01–46.72) | 3854 | 31.16%(29.70–32.63) | 9039 | 39.31%(38.30–40.31) | 5185 | 45.36%(44.01–46.72) | 3854 | 31.16%(29.70–32.63) |
| 31-60 min | 4087 | 17.37%(16.21–18.53) | 1995 | 42.16%(39.99–44.32) | 2092 | 28.06%(26.13–29.99) | 4087 | 34.94%(33.48–36.40) | 1995 | 42.16%(39.99–44.32) | 2092 | 28.06%(26.13–29.99) |
| ≥ 61 min | 3071 | 14.72%(13.46–15.97) | 1387 | 40.01%(37.43–42.60) | 1684 | 29.22%(27.04–31.39) | 3071 | 34.09%(32.42–35.77) | 1387 | 40.01%(37.43–42.60) | 1684 | 29.22%(27.04–31.39) |
| p value | 0 | 0.001 | 0.035 | 0 | 0.001 | 0.035 | ||||||
| Dyspraxia | ||||||||||||
| no | 4986 | 7.44%(6.71–8.17) | 1903 | 19.65%(17.87–21.44) | 3083 | 16.67%(15.36–17.99) | 4986 | 17.81%(16.75–18.87) | 1903 | 19.65%(17.87–21.44) | 3083 | 16.67%(15.36–17.99) |
| yes | 11,211 | 22.41%(21.63–23.18) | 6664 | 50.63%(49.43–51.83) | 4547 | 38.84%(37.42–40.26) | 11,211 | 45.85%(44.93–46.77) | 6664 | 50.63%(49.43–51.83) | 4547 | 38.84%(37.42–40.26) |
| p value | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| Depressive | ||||||||||||
| no | 10,762 | 12.70%(12.07–13.33) | 5170 | 35.16%(33.86–36.47) | 5592 | 24.46%(23.34–25.59) | 10,762 | 29.60%(28.74–30.47) | 5170 | 35.16%(33.86–36.47) | 5592 | 24.46%(23.34–25.59) |
| yes | 5435 | 27.89%(26.70–29.09) | 3397 | 56.81%(55.15–58.48) | 2038 | 44.75%(42.59–46.91) | 5435 | 52.29%(50.96–53.62) | 3397 | 56.81%(55.15–58.48) | 2038 | 44.75%(42.59–46.91) |
| p value | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| Drink | ||||||||||||
| no | 10,683 | 19.67%(18.91–20.42) | 7362 | 43.10%(41.97–44.23) | 3321 | 30.08%(28.52–31.64) | 10,683 | 39.05%(38.13–39.98) | 7362 | 43.10%(41.97–44.23) | 3321 | 30.08%(28.52–31.64) |
| yes | 5514 | 14.18%(13.26–15.10) | 1205 | 47.72%(44.89–50.54) | 4309 | 29.73%(28.36–31.09) | 5514 | 33.66%(32.41–34.91) | 1205 | 47.72%(44.89–50.54) | 4309 | 29.73%(28.36–31.09) |
| p value | 0 | 0.003 | 0.739 | 0 | 0.003 | 0.739 | ||||||
| ADL | ||||||||||||
| no | 13,397 | 14.50%(13.90–15.09) | 6780 | 38.19%(37.03–39.34) | 6617 | 26.82%(25.76–27.89) | 13,397 | 32.57%(31.78–33.37) | 6780 | 38.19%(37.03–39.34) | 6617 | 26.82%(25.76–27.89) |
| yes | 2800 | 33.61%(31.86–35.36) | 1787 | 64.86%(62.64–67.07) | 1013 | 49.85%(46.77–52.94) | 2800 | 59.43%(57.61–61.25) | 1787 | 64.86%(62.64–67.07) | 1013 | 49.85%(46.77–52.94) |
| p value | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| ADL_ins | ||||||||||||
| no | 12,561 | 14.44%(13.83–15.06) | 6205 | 37.60%(36.39–38.80) | 6356 | 26.83%(25.74–27.91) | 12,561 | 32.15%(31.33–32.96) | 6205 | 37.60%(36.39–38.80) | 6356 | 26.83%(25.74–27.91) |
| yes | 3636 | 29.40%(27.92–30.88) | 2362 | 59.91%(57.93–61.88) | 1274 | 45.13%(42.40–47.87) | 3636 | 54.73%(53.11–56.35) | 2362 | 59.91%(57.93–61.88) | 1274 | 45.13%(42.40–47.87) |
| p value | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| Activity_intensive | ||||||||||||
| less than 10 min | 10,895 | 17.66%(16.94–18.38) | 6223 | 41.68%(40.46–42.91) | 4672 | 26.84%(25.57–28.11) | 10,895 | 35.32%(34.42–36.22) | 6223 | 41.68%(40.46–42.91) | 4672 | 26.84%(25.57–28.11) |
| More than 10 min | 5302 | 18.09%(17.05–19.12) | 2344 | 49.23%(47.21–51.26) | 2958 | 34.69%(32.97–36.40) | 5302 | 41.12%(39.79–42.44) | 2344 | 49.23%(47.21–51.26) | 2958 | 34.69%(32.97–36.40) |
| p value | 0.504 | 0 | 0 | 0 | 0 | 0 | ||||||
| Activity_moderate | ||||||||||||
| less than 10 min | 8146 | 15.39%(14.61–16.18) | 3882 | 41.19%(39.64–42.74) | 4264 | 28.68%(27.32–30.04) | 8146 | 34.64%(33.61–35.68) | 3882 | 41.19%(39.64–42.74) | 4264 | 28.68%(27.32–30.04) |
| More than 10 min | 8051 | 20.23%(19.36–21.11) | 4685 | 45.87%(44.44–47.30) | 3366 | 31.40%(29.83–32.97) | 8051 | 39.82%(38.75–40.89) | 4685 | 45.87%(44.44–47.30) | 3366 | 31.40%(29.83–32.97) |
| p value | 0 | 0 | 0.001 | 0 | 0 | 0.01 | ||||||
| Activity_light | ||||||||||||
| less than 10 min | 2769 | 16.90%(15.50–18.30) | 1479 | 44.62%(42.09–47.16) | 1290 | 27.83%(25.38–30.28) | 2769 | 36.80%(35.00–38.60) | 1479 | 44.62%(42.09–47.16) | 1290 | 27.83%(25.38–30.28) |
| More than 10 min | 13,428 | 17.98%(17.34–18.63) | 7088 | 43.57%(42.41–44.72) | 6340 | 30.30%(29.17–31.43) | 13,428 | 37.30%(36.48–38.12) | 7088 | 43.57%(42.41–44.72) | 6340 | 30.30%(29.17–31.43) |
| p value | 0.175 | 0.456 | 0.077 | 0.619 | 0.456 | 0.077 | ||||||
| Treatments for Stroke | ||||||||||||
| no | 16,197 | 8567 | 7630 | 16,197 | 8567 | 7630 | ||||||
| yes | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| p value | ||||||||||||
| Stroke Neck pain | Stroke Low back pain | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Female | Male | Overall | Female | Male | |||||||
| n | Prevalence (95%CI) | n | Prevalence (95%CI) | n | Prevalence (95%CI) | n | Prevalence (95%CI) | n | Prevalence (95%CI) | n | Prevalence (95%CI) | |
| 885 | 26.44% (23.53–29.35) | 457 | 33.70%(29.35–38.05) | 428 | 18.69%(14.98–22.40) | 885 | 45.42% (42.14–48.71) | 457 | 57.33%(52.78–61.88) | 428 | 32.71%(28.25–37.17) | |
| Age, years | ||||||||||||
| 45–54 | 82 | 29.27%(19.21–39.33) | 40 | 40%(24.13–55.87) | 42 | 19.05%(6.66–31.43) | 82 | 47.56%(36.52–58.60) | 40 | 55%(38.89–71.13) | 42 | 40.48%(24.99–55.96) |
| 55–64 | 260 | 25%(19.70–30.30) | 126 | 30.95%(22.77–39.14) | 134 | 19.40%(12.62–26.19) | 260 | 46.15%(40.05–52.25) | 126 | 61.11%(52.48–69.74) | 134 | 32.09%(24.08–40.10) |
| 65–74 | 351 | 28.77%(24.02–33.53) | 196 | 35.71%(28.95–42.48) | 155 | 20%(13.63–26.37) | 351 | 45.58%(40.35–50.82) | 196 | 57.65%(50.67–64.63) | 155 | 30.32%(23.01–37.64) |
| ≥ 75 | 192 | 22.92%(16.92–28.92) | 95 | 30.53%(21.10–39.96) | 97 | 15.46%(8.14–22.79) | 192 | 43.23%(36.16–50.30) | 95 | 52.63%(42.41–62.86) | 97 | 34.02%(24.42–43.62) |
| p value | 0.421 | 0.591 | 0.83 | 0.901 | 0.641 | 0.65 | ||||||
| Residence | ||||||||||||
| rural | 653 | 26.19%(22.81–29.57) | 338 | 32.84%(27.81–37.87) | 315 | 19.05%(14.69–23.41) | 653 | 46.40%(42.57–50.24) | 338 | 57.69%(52.40–62.99) | 315 | 34.29%(29.02–39.56) |
| urban | 232 | 27.16%(21.39–32.92) | 119 | 36.13%(27.38–44.89) | 113 | 17.70%(10.55–24.84) | 232 | 42.67%(36.26–49.08) | 119 | 56.30%(47.26–65.34) | 113 | 28.32%(19.88–36.75) |
| p value | 0.774 | 0.514 | 0.753 | 0.328 | 0.793 | 0.247 | ||||||
| Education | ||||||||||||
| illiterate | 245 | 28.98%(23.26–34.70) | 185 | 29.73%(23.08–36.38) | 60 | 26.67%(15.15–38.19) | 245 | 53.47%(47.18–59.76) | 185 | 58.38%(51.21–65.55) | 60 | 38.33%(25.67–51.00) |
| elementary school or below | 379 | 31.40%(26.70–36.09) | 190 | 40%(32.97–47.03) | 189 | 22.75%(16.72–28.78) | 379 | 49.34%(44.28–54.40) | 190 | 61.05%(54.06–68.05) | 189 | 37.57%(30.60–44.53) |
| secondary school and above | 261 | 16.86%(12.29–21.43) | 82 | 28.05%(18.12–37.98) | 179 | 11.73(6.97–16.49) | 261 | 32.18%(26.48–37.89) | 82 | 46.34%(35.32–57.37) | 179 | 25.70%(19.24–32.16) |
| p value | 0 | 0.054 | 0.006 | 0 | 0.074 | 0.032 | ||||||
| Disability | ||||||||||||
| no | 628 | 24.84%(21.45–28.23) | 325 | 31.69%(26.61–36.78) | 303 | 17.49%(13.19–21.79) | 628 | 44.11%(40.21–48.00) | 325 | 55.08%(49.64–60.51) | 303 | 32.34%(27.05–37.64) |
| yes | 257 | 30.35%(24.69–36.01) | 132 | 38.64%(30.22–47.05) | 125 | 21.60%(14.29–28.91) | 257 | 48.64%(42.49–54.79) | 132 | 62.88%(54.53–71.22) | 125 | 33.60%(25.20–42.00) |
| p value | 0.092 | 0.155 | 0.323 | 0.22 | 0.127 | 0.802 | ||||||
| Chronic Disease | ||||||||||||
| 0 | 350 | 21.43%(17.11–25.75) | 177 | 29.38%(22.60–36.15) | 173 | 13.29%(8.18–18.40) | 350 | 38.57%(33.45–43.70) | 177 | 53.11%(45.68–60.53) | 173 | 23.70%(17.30–30.10) |
| 1 | 282 | 26.60%(21.41–31.78) | 146 | 34.93%(27.11–42.76) | 136 | 17.65%(11.16–24.14) | 282 | 43.97%(38.14–49.80) | 146 | 54.11%(45.93–62.29) | 136 | 33.09%(25.08–41.10) |
| 2 | 253 | 33.20%(27.36–39.04) | 134 | 38.06%(29.73–46.39) | 119 | 27.73%(19.57–35.89) | 253 | 56.52%(50.37–62.67) | 134 | 66.42%(58.32–74.52) | 119 | 45.38%(36.30–54.45) |
| p value | 0.005 | 0.258 | 0.007 | 0 | 0.04 | 0.001 | ||||||
| Sleep Time | ||||||||||||
| ≤ 6 h | 509 | 33.99%(29.86–38.12) | 289 | 41.87%(36.15–47.59) | 220 | 23.64%(17.98–29.29) | 509 | 50.29%(45.93–54.65) | 289 | 59.86%(54.18–65.55) | 220 | 37.73%(31.27–44.18) |
| 6-8 h | 275 | 16.36%(11.96–20.76) | 126 | 20.63%(13.47–27.80) | 149 | 12.75%(7.33–18.17) | 275 | 38.18%(32.40–43.96) | 126 | 52.38%(43.54–61.22) | 149 | 26.17%(19.03–33.31) |
| ≥ 8 h | 101 | 15.84%(8.60–23.09) | 42 | 16.67%(4.91–28.42) | 59 | 15.25%(5.80–24.70) | 101 | 40.59%(30.85–50.33) | 42 | 54.76%(39.06–70.46) | 59 | 30.51%(18.41–42.61) |
| p value | 0 | 0 | 0.024 | 0.003 | 0.346 | 0.063 | ||||||
| Nap Time | ||||||||||||
| ≤ 30 min | 455 | 30.11%(25.88–34.34) | 258 | 36.82%(30.90–42.75) | 197 | 21.32%(15.55–27.09) | 455 | 49.67%(45.06–54.28) | 258 | 58.53%(52.48–64.58) | 197 | 38.07%(31.23–44.91) |
| 31-60 min | 200 | 19.50%(13.96–25.04) | 102 | 26.47%(17.76–35.18) | 98 | 12.24%(5.64–18.85) | 200 | 44.00%(37.06–50.94) | 102 | 62.75%(53.20–72.29) | 98 | 24.49%(15.82–33.16) |
| ≥ 61 min | 230 | 25.22%(19.56–30.87) | 97 | 32.99%(23.46–42.52) | 133 | 19.55%(12.72–26.38) | 230 | 38.26%(31.93–44.59) | 97 | 48.45%(38.33–58.58) | 133 | 30.83%(22.88–38.78) |
| p value | 0.016 | 0.172 | 0.163 | 0.016 | 0.106 | 0.055 | ||||||
| Dyspraxia | ||||||||||||
| no | 104 | 10.58%(4.57–16.59) | 26 | 11.54%(-1.62–24.70) | 78 | 10.26%(3.37–17.14) | 104 | 18.27%(10.72–25.82) | 26 | 26.92%(8.65–45.19) | 78 | 15.38%(7.20–23.57) |
| yes | 781 | 28.55%(25.38–31.73) | 431 | 35.03%(30.51–39.56) | 350 | 20.57%(16.32–24.83) | 781 | 49.04%(45.53–52.55) | 431 | 59.16%(54.51–63.82) | 350 | 36.57%(31.50–41.64) |
| p value | 0 | 0.014 | 0.035 | 0 | 0.001 | 0 | ||||||
| Depressive | ||||||||||||
| no | 506 | 19.76%(16.28–23.24) | 231 | 24.68%(19.07–30.28) | 275 | 15.64%(11.32–19.96) | 506 | 35.57%(31.39–39.76) | 231 | 45.89%(39.41–52.36) | 275 | 26.91%(21.63–32.18) |
| yes | 379 | 35.36%(30.52–40.19) | 226 | 42..92%(36.42–49.42) | 153 | 24.18%(17.32–31.04) | 379 | 58.58%(53.59–63.56) | 226 | 69.03%(62.95–75.10) | 153 | 43.14%(35.20–51.07) |
| p value | 0 | 0 | 0.03 | 0 | 0 | 0.001 | ||||||
| Drink | ||||||||||||
| no | 683 | 28.26%(24.87–31.64) | 417 | 32.85%(28.33–37.38) | 266 | 21.05%(16.12–25.98) | 683 | 46.71%(42.95–50.46) | 417 | 55.88%(51.09–60.67) | 266 | 32.33%(26.67–37.99) |
| yes | 202 | 20.30%(14.70–25.89) | 40 | 42.50%(26.49–58.51) | 162 | 14.81%(9.29–20.34) | 202 | 41.09%(34.25–47.93) | 40 | 72.50%(58.04–86.96) | 162 | 33.33%(26.00–40.67) |
| p value | 0.024 | 0.219 | 0.109 | 0.159 | 0.042 | 0.831 | ||||||
| ADL | ||||||||||||
| no | 508 | 21.85%(18.24–25.46) | 229 | 30.57%(24.56–36.58) | 279 | 14.70%(10.52–18.88) | 508 | 39.57%(35.30–43.83) | 229 | 55.46%(48.97–61.94) | 279 | 26.52%(21.31–31.74) |
| yes | 377 | 32.63%(27.87–37.38) | 228 | 36.84%(30.53–43.15) | 149 | 26.17%(19.03–33.31) | 377 | 53.32%(48.26–58.37) | 228 | 59.21%(52.78–65.64) | 149 | 44.30%(36.23–52.36) |
| p value | 0 | 0.157 | 0.004 | 0 | 0.419 | 0 | ||||||
| ADL_ins | ||||||||||||
| no | 426 | 22.07%(18.11–26.02) | 183 | 28.96%(22.33–35.60) | 243 | 16.87%(12.13–21.61) | 426 | 38.03%(33.40–42.66) | 183 | 48.63%(41.32–55.94) | 243 | 30.04%(24.24–35.85) |
| yes | 459 | 30.50%(26.27–34.73) | 274 | 36.86%(31.11–42.61) | 185 | 21.08%(15.15–27.01) | 459 | 52.29%(47.70–56.87) | 274 | 63.14%(57.39–68.89) | 185 | 36.22%(29.23–43.21) |
| p value | 0.004 | 0.08 | 0.27 | 0 | 0.002 | 0.178 | ||||||
| Activity_intensive | ||||||||||||
| less than 10 min | 705 | 25.11%(21.90–28.32) | 376 | 31.91%(27.18–36.65) | 329 | 17.33%(13.21–21.44) | 705 | 43.55%(39.88–47.21) | 376 | 55.32%(50.27–60.37) | 329 | 30.09%(25.11–35.07) |
| More than 10 min | 180 | 31.67%(24.81–38.53) | 81 | 41.98%(30.99–52.96) | 99 | 23.23%(14.77–31.70) | 180 | 52.78%(45.41–60.14) | 81 | 66.67%(56.18–77.16) | 99 | 41.41%(31.54–51.29) |
| p value | 0.075 | 0.083 | 0.187 | 0.15 | 0.061 | 0.035 | ||||||
| Activity_moderate | ||||||||||||
| less than 10 min | 559 | 24.87%(21.27–28.46) | 267 | 31.84%(26.21–37.46) | 292 | 18.49%(14.01–22.97) | 559 | 42.75%(38.64–46.87) | 267 | 55.81%(49.81–61.80) | 292 | 30.82%(25.49–36.15) |
| More than 10 min | 326 | 29.14%(24.18–34.10) | 190 | 36.32%(29.42–43.22) | 136 | 19.12%(12.42–25.81) | 326 | 50%(44.54–55.46) | 190 | 59.47%(52.43–66.52) | 136 | 36.76%(28.56–44.97) |
| p value | 0.165 | 0.319 | 0.878 | 0.037 | 0.436 | 0.223 | ||||||
| Activity_light | ||||||||||||
| less than 10 min | 211 | 24.17%(18.35–29.99) | 132 | 28.03%(20.27–35.79) | 79 | 17.72%(9.11–26.33) | 211 | 47.39%(40.60–54.19) | 132 | 54.55%(45.94–63.15) | 79 | 35.44%(24.66–46.23) |
| More than 10 min | 674 | 27.15%(23.79–30.52) | 325 | 36%(30.75–41.25) | 349 | 18.91%(14.78–23.04) | 674 | 44.81%(41.04–48.57) | 325 | 58.46%(53.08–63.85) | 349 | 32.09%(27.17–37.01) |
| p value | 0.392 | 0.103 | 0.807 | 0.511 | 0.444 | 0.568 | ||||||
| Treatments for Stroke | ||||||||||||
| no | 232 | 22.41%(17.01–27.82) | 124 | 29.84%(21.67–38.01) | 108 | 13.89%(7.26–20.52) | 232 | 43.10%(36.68–49.52) | 124 | 52.42%(43.51–61.33) | 108 | 32.41%(23.44–41.38) |
| yes | 653 | 27.87%(24.42–31.32) | 333 | 35.14%(29.98–40.29) | 320 | 20.31%(15.88–24.74) | 653 | 46.25%(42.41–50.08) | 333 | 59.16%(53.85–64.47) | 320 | 32.81%(27.64–37.98) |
| p value | 0.106 | 0.288 | 0.139 | 0.409 | 0.196 | 0.938 | ||||||
One-way ANOVA was used to compare the differences in prevalence rates between different groups, with the test level α = 0.05, and p < 0.05 indicating that the differences were statistically significant
In addition, the prevalence of NP (35.36%, 95% CI: 30.52–40.19) and LBP (58.58%, 95% CI: 53.59–63.56) in the stroke population with depression was significantly higher than that in the non-depressed population (for NP: 19.76%, 95% CI 16.28–23.24; for LBP: 35.57%, 95% CI 31.39–39.76). The prevalence of NP and LBP was also significantly higher in the females with depression. Those with physical disability (30.35%, 95% CI: 24.69–36.01), comorbidities with other chronic diseases (33.20%, 95% CI: 27.36–39.04), short sleep duration (33.99%, 95% CI: 29.86–38.12), physical dysfunction (28.55%, 95% CI: 25.38–31.73), ADL impairment (32.63%, 95% CI: 27.87–37.38), and IADL impairment (30.50%, 95% CI: 26.27–34.73) had a high prevalence of post-stroke neck pain. Similar results were found in the post-stroke LBP population. The prevalence of neck pain (16.86%, 95% CI 12.29–21.43) and low back pain (32.18%, 95% CI 26.48–37.89) was significantly lower in the stroke population with higher education (secondary school and above; Table 2). The relationship between stroke participants’ different levels of education, different residential areas, and depression status and their NP or LBP status is detailed in Tables S3, S4, and S5 in the Appendix.
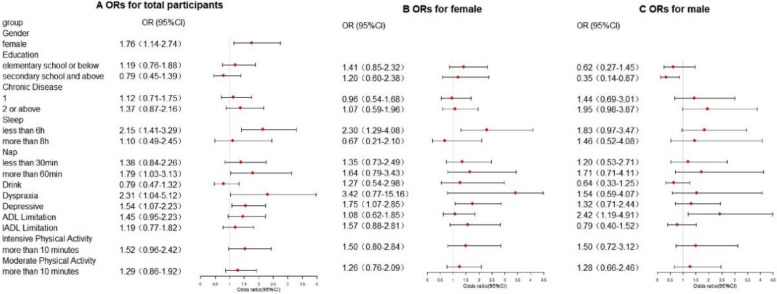
The significant factors associated with NP in the stroke participants identified by logistic regression modeling are shown in Fig. 2. Female (OR = 1.76, 95% CI: 1.14–2.74), sleep duration of less than 6 h (OR = 2.15, 95% CI: 1.41–3.29), lunch breaks for more than 60 min (OR = 1.79, 95% CI: 1.03–3.13), physical dysfunction (OR = 2.31, 95% CI: 1.04–5.12), and depression (OR = 1.54, 95% CI: 1.07–2.23) were factors associated with the presence of NP in the stroke population. Sleeping less than 6 h (OR = 2.30, 95% CI: 1.29–4.08) and depression (OR = 1.75, 95% CI: 1.07–2.85) were factors associated with NP in the female stroke population. ADL disorder (OR = 2.42, 95% CI: 1.19–4.91) was an independent factor associated with NP in males with stroke, whereas high education level (junior high school and above; OR = 0.35, 95% CI: 0.14–0.87) was associated with less likelihood of having NP. The detailed results of subgroup multifactorial regression analyses based on the area of residence, number of comorbidities, depressive symptoms, and education level are presented in the Appendix (Figures S1–S4).
Fig. 2.
Forest plot of risk factors for neck pain in the general Chinese population aged 45 years and above with stroke in China, 2018
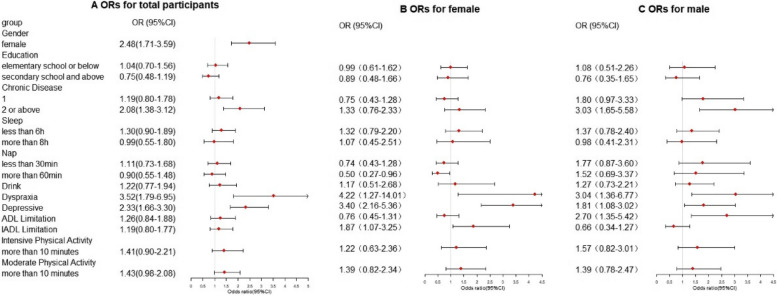
The significant factors associated with LBP in participants with stroke identified by the logistic regression model are shown in Fig. 3. Female (OR = 2.48, 95% CI: 1.71–3.59), comorbidities of two or more chronic diseases (OR = 2.08, 95% CI: 1.38–3.12), physical dysfunction (OR = 3.52, 95% CI: 1.79–6.95), and depression (OR = 2.33, 95% CI: 1.66–3.30) were factors associated with the presence of LBP in the stroke population. The subgroup of sex showed that physical dysfunction (OR = 4.22, 95% CI: 1.27– 14.01), depression (OR = 3.40, 95% CI: 2.16–5.36), and IADL disorder (OR = 1.87, 95% CI: 1.07–3.25) were factors associated with LBP in female participants with stroke. Comorbidities with two or more chronic diseases (OR = 3.03, 95% CI: 1.65–5.58), physical dysfunction (OR = 3.04, 95% CI: 1.36–6.77), depression (OR = 1.81, 95% CI: 1.08–3.02), and ADL disorder (OR = 2.70, 95% CI: 1.35–5.42) were factors associated with the presence of LBP in the male stroke population. The results of the subgroup multifactorial regression analyses based on the area of residence, number of comorbid chronic diseases, depressive symptoms, and education level are displayed in Figures S5–S8 in the Appendix.
Fig. 3.
Forest plot of risk factors for low back pain in the general Chinese population aged 45 years and above with stroke in China, 2018
The factors associated with NP and LBP in the non-stroke population are detailed in Appendix Figures S9–S18.
Discussion
To our knowledge, this is the first and the largest survey on the prevalence of NP and LBP in Chinese stroke populations aged 45 years and above. Our results showed that 26.44% and 45.42% of middle-aged and older individuals with stroke in China experienced NP and LBP, reaching the epidemic level. Our findings revealed that female with stroke had significantly higher prevalence of NP and LBP than the male counterparts, which highlights the importance of paying more attention to post-stroke pain in females. Further, chronic diseases, sleep problem and depression are the major modifiable factors for NP and LBP among Chinese stroke survivors.
The current study found no significant association between medical insurance and NP or LBP in the stroke population. The lack of association may be related to the unique Chinese basic medical insurance system that covers the entire population in 2009. Statistical data indicated that the Chinese basic medical insurance coverage rate exceeded 95% in 2018, and it has remained unchanged till now [27]. This situation is consistent with the situation in the current study where nearly 98% of the participants with stroke had health insurance.
Females with stroke display a higher prevalence of NP and LBP than male counterparts, which concurred with previous studies [28–30]. This finding may be attributed to the fact that females have a higher pain sensitivity than males [31]. Our study also found that depression was associated with NP and LBP in the stroke population. This finding is consistent with prior studies [32, 33]. Two previous Japanese studies revealed that poor mental health is associated with severe pain [34, 35]. Although the current study cannot confirm the causal relationship, it underscores the importance of proper assessment and management psychological well-being in individuals with stroke, especially for those with pain, so that timely psychological counselling and advice can be provided. In addition, women with comorbid depression were more likely to experience NP and LBP. This result suggests that clinicians and relevant health authority should pay more attention to the psychological construction of the female stroke population. The high prevalence of depression (42.82%) in the stroke population found in the current study could be ascribed to the retrospective nature of the survey and the diagnosis of depression based on a self-reported questionnaire rather than the clinical diagnosis of depression by physicians. The connection between depression and pain is still unclear and requires further investigation.
Stroke participants with activity limitations resulting from physical dysfunction were two times more likely to experience frequent NP and almost three times more likely to experience frequent LBP as compared to those without activity limitations (Appendix). Limitations in movement caused by physical dysfunction are common clinical symptoms of stroke. Approximately 80% of patients with stroke experience motor dysfunction [36], while motor dysfunction is highly associated with post-stroke pain [37]. Suboptimal physical activity may be one of the possible causes of post-stroke pain, as shown in this study. Further, the presence of NP and LBP secondary to activity limitation or physical dysfunction was significantly higher in the stroke population in rural areas than in the stroke population in urban areas. A possible explanation is that people in rural areas have a low economic base and lack of systematic rehabilitation training, leading to increased physical dysfunction. Regular exercise has been proven to decrease pain intensity, improve independence from daily activities, and alleviate depression symptoms [38–40]. The current study showed that participation in physical activity of different intensity were related to the presence of NP and LBP in some stroke populations. Therefore, personalized physical activity programs are important in the pain management of individuals with stroke. Our study has also found that the presence of two or more chronic diseases are associated with the presence of LBP in the stroke populations, which may affect allostatic load and cause pain through the dysregulation of physiological mechanisms; however, these mechanisms remain to be confirmed [41]. The stroke populations with other chronic condition were likely to experience frequent NP or LBP due to the limited ability to perform ADL. This finding is consistent with the finding that activity limitation due to physical dysfunction is an explanatory factor for pain because the ADL scale represents mobility capacity. This finding emphasizes the importance of considering other chronic conditions in the pain management in individuals with stroke.
In the stroke population with higher education, the prevalence of NP was associated with female and sleep problem. These findings are similar to previous studies [42, 43]. In the current study, more educated participants were more likely to engage in sedentary lifestyles with concomitant psychological problems and sleep problem as compared to less educated participants. Further, females with a high level of education had a high prevalence of NP. This observation may be due to the sedentary lifestyle and poor posture contribute to the occurrence of NP [44]. Sleep problems are known to be linked to or increase musculoskeletal pain [45]. A cohort study in Northern Finland found that sleep deprivation is an independent risk factor for NP and LBP in women [46]. Both NP and LBP may increase due to increased pain sensitivity and pain-related biomarkers following sleep deprivation [47]. Interestingly, prolonged napping after lunch was associated with NP in our stroke population. Although speculative, it is possible that prolonged napping leads to delayed nighttime sleep, which impairs circadian rhythms and leads to sleep problem. Our study also reported a high prevalence of LBP in stroke populations with low education levels. Female, depression, and comorbidities with other chronic diseases may be important factors in the development of LBP in stroke populations with low levels of education. However, due to the limitations of cross-sectional studies, although an association exists among sleep duration, the female gender, and neck pain, the causal relationship remains unclear.
Strengths and limitations
This study has multiple strengths. First, it used the national CHARLS database, which contains big data. The strict sampling design and data screening process ensure the reliability and validity of our research results. Second, this study comprehensively analyzed the prevalence and factors associated with NP and LBP in the Chinese stroke population. Third, this study has laid the foundation for developing prevention and intervention strategies for NP and LBP in the Chinese stroke population.
However, our study had some limitations. First, the current cross-sectional study could not determine the causal relationships between post-stroke NP or LBP and their associated factors. Second, this work was based on retrospective reports from the participants, and the information might have been subject to recall bias. Third, the database did not distinguish between populations with different types and severity of stroke. Therefore, our findings study should be interpreted with caution and may not be generalized to the whole Chinese stroke population. In addition, the baseline survey of the database did not include residents of nursing homes. However, this is unlikely to cause a major problem because the proportion of nursing home residents is very small in China.
Conclusions
This is the first population-based study to investigate the prevalence of NP and LBP in the Chinese stroke population. Short sleep duration, prolonged napping after lunch, physical dysfunction, and depression were associated with the presence of NP in the stroke population. Comorbidities of two or more chronic diseases, physical dysfunction, and depression were associated with LBP in the stroke population. Additionally, clinicians should pay more attention to female stroke survivors because they are more vulnearable to experience NP and LBP. Our findings provide policy makers and clinicians with empirical data to formulate more effective prevention and management strategies of spinal pain in stroke survivors.
Supplementary Information
Acknowledgements
This study was conducted using data from the China Longitudinal Study of Health and Retirement (CHARLS).We thank all the volunteers and staff who participated in this research.
Authors’ contributions
"XQ W, SQ R, and X J had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. SQ R and X J contributed equally to this study. XQ W, SQ R, X J, AYLW, and X B contributed to the conception and design of the study. Statistical analysis: SQ R , X J , SY W and AY LW. Draft the original manuscript: SQ R and X J. All authors contributed to the edit of the manuscript."
Funding
This study was supported by grants from the National Natural Science Foundation of China (82372578).
Availability of data and materials
The data that support the findings of this study are available from the China Longitudinal Study of Health and Retirement (CHARLS), subject to registration and application process. Further details can be found at http://charls.pku.edu.cn/pages/data/111/zh-cn.
Declarations
Ethics approval and consent to participate
Ethical approval for all the CHARLS waves was granted from the Institutional Review Board at Peking University(IRB00001052-11015). All participants signed informed consent forms before participating in the CHARLS study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Siqiang Ren and Xue Jiang contributed equally to this work.
References
- 1.Wang Y, Li Z, Zhao X, Wang D, Li H, Xian Y, et al. Stroke care quality in China: Substantial improvement, and a huge challenge and opportunity. Int J Stroke : official journal of the International Stroke Society. 2017;12(3):229–35. 10.1177/1747493017694392 [DOI] [PubMed] [Google Scholar]
- 2.Ma Q, Li R, Wang L, Yin P, Wang Y, Yan C, et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: an analysis for the global burden of disease study 2019. Lancet Public health. 2021;6(12):e897–906. 10.1016/S2468-2667(21)00228-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation. 2017;135(8):759–71. 10.1161/CIRCULATIONAHA.116.025250 [DOI] [PubMed] [Google Scholar]
- 4.Wang LDWJ, Peng B, Xu YM. Brief report on stroke prevention and treatment in China, 2019. Chin J Cerebrovasc Dis. 2020;17(5):272–81. [Google Scholar]
- 5.GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795–820. [DOI] [PMC free article] [PubMed]
- 6.Li Z, Jiang Y, Li H, Xian Y, Wang Y. China’s response to the rising stroke burden. BMJ (Clinical research ed). 2019;364:l879. 10.1136/bmj.l879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu S, Wu B, Liu M, Chen Z, Wang W, Anderson CS, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019;18(4):394–405. 10.1016/S1474-4422(18)30500-3 [DOI] [PubMed] [Google Scholar]
- 8.Wang YJ, Li ZX, Gu HQ, Zhai Y, Zhou Q, Jiang Y, et al. China stroke statistics: an update on the 2019 report from the National Center for Healthcare Quality Management in Neurological Diseases, China National Clinical Research Center for Neurological Diseases, the Chinese Stroke Association, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention and Institute for Global Neuroscience and Stroke Collaborations. Stroke Vasc Neurol. 2022;7(5):415–50. 10.1136/svn-2021-001374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lanctôt KL, Lindsay MP, Smith EE, Sahlas DJ, Foley N, Gubitz G, et al. Canadian stroke best practice recommendations: mood, cognition and fatigue following stroke, 6th edition update 2019. Int J Stroke : official journal of the International Stroke Society. 2020;15(6):668–88. 10.1177/1747493019847334 [DOI] [PubMed] [Google Scholar]
- 10.Baylan S, Griffiths S, Grant N, Broomfield NM, Evans JJ, Gardani M. Incidence and prevalence of post-stroke insomnia: a systematic review and meta-analysis. Sleep Med Rev. 2020;49:101222. 10.1016/j.smrv.2019.101222 [DOI] [PubMed] [Google Scholar]
- 11.Carnes-Vendrell A, Deus J, Molina-Seguin J, Pifarré J, Purroy F. Depression and apathy after transient ischemic attack or minor stroke: prevalence, evolution and predictors. Sci Rep. 2019;9(1):16248. 10.1038/s41598-019-52721-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Banda KJ, Chu H, Kang XL, Liu D, Pien LC, Jen HJ, et al. Prevalence of dysphagia and risk of pneumonia and mortality in acute stroke patients: a meta-analysis. BMC Geriatr. 2022;22(1):420. 10.1186/s12877-022-02960-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harriott AM, Karakaya F, Ayata C. Headache after ischemic stroke: a systematic review and meta-analysis. Neurology. 2020;94(1):e75–86. 10.1212/WNL.0000000000008591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ali M, Tibble H, Brady MC, Quinn TJ, Sunnerhagen KS, Venketasubramanian N, et al. Prevalence, trajectory, and predictors of poststroke pain: retrospective analysis of pooled clinical trial data set. Stroke. 2023;54(12):3107–16. [DOI] [PubMed]
- 15.Zhang Q, Chen D, Shen Y, Bian M, Wang P, Li J. Incidence and prevalence of poststroke shoulder pain among different regions of the world: a systematic review and meta-analysis. Front Neurol. 2021;12:724281. 10.3389/fneur.2021.724281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang S, Chang MC. Poststroke pain. Semin Neurol. 2021;41(1):67–74. 10.1055/s-0040-1722641 [DOI] [PubMed] [Google Scholar]
- 17.Paolucci S, Iosa M, Toni D, Barbanti P, Bovi P, Cavallini A, et al. Prevalence and time course of post-stroke pain: a multicenter prospective hospital-based study. Pain Med (Malden, Mass). 2016;17(5):924–30. [DOI] [PubMed] [Google Scholar]
- 18.Widar M, Samuelsson L, Karlsson-Tivenius S, Ahlström G. Long-term pain conditions after a stroke. J Rehabil Med. 2002;34(4):165–70. 10.1080/16501970213237 [DOI] [PubMed] [Google Scholar]
- 19.Payton H, Soundy A. The experience of post-stroke pain and the impact on quality of life: an integrative review. Behav Sci (Basel, Switzerland). 2020;10(8):128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang YH, Wang YC, Hu GW, Ding XQ, Shen XH, Yang H, et al. The Effects of gender, functional condition, and ADL on pressure pain threshold in stroke patients. Front Neurosci. 2021;15:705516. 10.3389/fnins.2021.705516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang K, Liu H. Association between widespread pain and dementia, Alzheimer’s disease and stroke: a cohort study from the Framingham Heart Study. Reg Anesth Pain Med. 2021;46(10):879–85. 10.1136/rapm-2021-102733 [DOI] [PubMed] [Google Scholar]
- 22.Tang SC, Lee LJ, Jeng JS, Hsieh ST, Chiang MC, Yeh SJ, et al. Pathophysiology of central poststroke pain: motor cortex disinhibition and its clinical and sensory correlates. Stroke. 2019;50(10):2851–7. 10.1161/STROKEAHA.119.025692 [DOI] [PubMed] [Google Scholar]
- 23.Li C, Shu X, Liu X. Research hotspots and frontiers in post stroke pain: a bibliometric analysis study. Front Mol Neurosci. 2022;15:905679. 10.3389/fnmol.2022.905679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xiong F, Shen P, Li Z, Huang Z, Liang Y, Chen X, et al. Bibliometric analysis of post-stroke pain research published from 2012 to 2021. J Pain Res. 2023;16:1–20. 10.2147/JPR.S375063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43(1):61–8. 10.1093/ije/dys203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen H. Mui ACJIP. Factorial validity of the center for epidemiologic studies depression scale short form in older population in China. 2014;26(1):1–9. [DOI] [PubMed] [Google Scholar]
- 27.Administration NHS. Statistical bulletin on healthcare security 2018. 2019. [Google Scholar]
- 28.Qiu Y, Li H, Yang Z, Liu Q, Wang K, Li R, et al. The prevalence and economic burden of pain on middle-aged and elderly Chinese people: results from the China health and retirement longitudinal study. BMC Health Serv Res. 2020;20(1):600. 10.1186/s12913-020-05461-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Husky MM, Ferdous Farin F, Compagnone P, Fermanian C, Kovess-Masfety V. Chronic back pain and its association with quality of life in a large French population survey. Health Qual Life Outcomes. 2018;16(1):195. 10.1186/s12955-018-1018-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang L, Peng W. Prevalence and factors associated with body pain: results of a nationally representative survey of 9,586 Chinese adults aged 60 and over. Front Public Health. 2021;9:634123. 10.3389/fpubh.2021.634123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yu T, Ma J, Jiang Y, Li J, Gen Y, Wen Y, et al. Assessing pain among Chinese Elderly-Chinese health and retirement longitudinal study. Iran J Public Health. 2018;47(4):553–60. [PMC free article] [PubMed] [Google Scholar]
- 32.Klit H, Finnerup NB, Overvad K, Andersen G, Jensen TS. Pain following stroke: a population-based follow-up study. PLoS ONE. 2011;6(11):e27607. 10.1371/journal.pone.0027607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hansen AP, Marcussen NS, Klit H, Kasch H, Jensen TS, Finnerup NB. Development of persistent headache following stroke: a 3-year follow-up. Cephalalgia : an international journal of headache. 2015;35(5):399–409. 10.1177/0333102414545894 [DOI] [PubMed] [Google Scholar]
- 34.Montgomery W, Vietri J, Shi J, Ogawa K, Kariyasu S, Alev L, et al. The relationship between pain severity and patient-reported outcomes among patients with chronic low back pain in Japan. J Pain Res. 2016;9:337–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsuji T, Matsudaira K, Sato H, Vietri J. The impact of depression among chronic low back pain patients in Japan. BMC Musculoskelet Disord. 2016;17(1):447. 10.1186/s12891-016-1304-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. Lancet Neurol. 2009;8(8):741–54. 10.1016/S1474-4422(09)70150-4 [DOI] [PubMed] [Google Scholar]
- 37.Atalan P, Bērziņa G, Sunnerhagen KS. Influence of mobility restrictions on post-stroke pain. Brain Behav. 2021;11(5):e02092. 10.1002/brb3.2092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tse MM, Tang SK, Wan VT, Vong SK. The effectiveness of physical exercise training in pain, mobility, and psychological well-being of older persons living in nursing homes. Pain Manag Nurs : official journal of the American Society of Pain Management Nurses. 2014;15(4):778–88. 10.1016/j.pmn.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 39.Ma Y, Luo J, Wang XQ. The effect and mechanism of exercise for post-stroke pain. Front Mol Neurosci. 2022;15:1074205. 10.3389/fnmol.2022.1074205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang W, Liu Y, Yu J, Zhang Q, Wang X, Zhang Y, et al. Exercise interventions for post-stroke depression: a protocol for systematic review and meta-analysis. Medicine. 2021;100(8):e24945. 10.1097/MD.0000000000024945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.de Luca KE, Parkinson L, Haldeman S, Byles JE, Blyth F. The relationship between spinal pain and comorbidity: a cross-sectional analysis of 579 community-dwelling, older Australian women. J Manipulative Physiol Ther. 2017;40(7):459–66. 10.1016/j.jmpt.2017.06.004 [DOI] [PubMed] [Google Scholar]
- 42.Lee MK, Oh J. The relationship between sleep quality, neck pain, shoulder pain and disability, physical activity, and health perception among middle-aged women: a cross-sectional study. BMC Womens Health. 2022;22(1):186. 10.1186/s12905-022-01773-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hey HWD, Lim JXY, Ong JZ, Luo N. Epidemiology of neck pain and its impact on quality-of-life-a population-based, cross sectional study in Singapore. Spine. 2021;46(22):1572–80. 10.1097/BRS.0000000000004071 [DOI] [PubMed] [Google Scholar]
- 44.Adams MA, Freeman BJ, Morrison HP, Nelson IW, Dolan P. Mechanical initiation of intervertebral disc degeneration. Spine. 2000;25(13):1625–36. 10.1097/00007632-200007010-00005 [DOI] [PubMed] [Google Scholar]
- 45.Andreucci MA, Campbell P, Dunn KM. Are sleep problems a risk factor for the onset of musculoskeletal pain in children and adolescents? A Systematic Review. Sleep. 2017;40(7). 10.1093/sleep/zsx093. [DOI] [PubMed]
- 46.Auvinen JP, Tammelin TH, Taimela SP, Zitting PJ, Järvelin MR, Taanila AM, et al. Is insufficient quantity and quality of sleep a risk factor for neck, shoulder and low back pain? A longitudinal study among adolescents. Eur Spine J : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2010;19(4):641–9. 10.1007/s00586-009-1215-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Afolalu EF, Ramlee F, Tang NKY. Effects of sleep changes on pain-related health outcomes in the general population: a systematic review of longitudinal studies with exploratory meta-analysis. Sleep Med Rev. 2018;39:82–97. 10.1016/j.smrv.2017.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the China Longitudinal Study of Health and Retirement (CHARLS), subject to registration and application process. Further details can be found at http://charls.pku.edu.cn/pages/data/111/zh-cn.