Abstract
BACKGROUND:
Patients often use manufacturer-sponsored coupons to reduce their out-of-pocket spending. However, little is known whether coupon use is associated with medication-switching behaviors.
OBJECTIVE:
To examine if using a manufacturer-sponsored coupon to initiate a medication is associated with patterns of medication-switching behaviors among patients with type 2 diabetes.
METHODS:
Using IQVIA’s retail pharmacy claims data from October 2017 to September 2019, we analyzed commercially insured patients with type 2 diabetes who had newly started taking the following noninsulin diabetes drugs: generic metformin (nearly no coupon use), Sodium-glucose Cotransporter-2 (SGLT2) Inhibitors (SGLT2, high coupon use), and dipeptidyl peptidase IV inhibitors (DPP-IV inhibitors, moderate coupon use). We assessed if drug-switching behaviors, defined as no switching, switching to a same-class drug, or switching to a drug in a different class, differed among patients who did and did not use coupons to initiate treatments. We performed multinomial logistic regression to estimate the probability of each switching type associated with patients’ initial coupon use.
RESULTS:
Among 9,781 patients in our sample, 83.7% of them initiated treatments with metformin, 8.2% with SGLT2, and 8.1% with DPP-IV inhibitors. The overall switching rate was the lowest for generic metformin (40%) than brand-name drugs (56%-57%). Among the brand-name drug users, patients who used a coupon to initiate these drugs were less likely to switch to any drug compared with patients without coupon use (SGLT2 = −18% [95% CI = −24% to −13%]; DPP-IV inhibitors = −9% [−16% to −2%]). These patients were also less likely to switch to drugs in other competing classes (SGLT2 = −16% [95% CI = −22% to −10%]; DPP-IV inhibitors = −9% [−16% to −2%]).
CONCLUSIONS:
Patients who started their treatment with generic metformin had the lowest rate of drug switching. Using coupons to initiate brand-name drugs in classes with prevalent coupons was associated with reduced medication switching to other class drugs.
Plain language summary
Many patients use coupons when they initiate a brand-name medication. However, little is known if coupon use is associated with patient medication-switching behaviors, which could disrupt chronic condition management. We found that patients with diabetes who started diabetes treatment with a generic oral drug (with or without a coupon) were less likely to switch to other medications compared with brand-name medications. Patients who started either class of brand-name drugs with a coupon were less likely to switch to other classes of drugs than those without coupons.
Implications for managed care pharmacy
Many patients initiate prescription brand-name drugs with manufacturer-sponsored coupons at the point of sale. Once they start using high-cost brand-name drugs with a coupon, they are more likely to use drugs in the same class, which may result in high spending on brand-name drugs. Managed care pharmacies and health plans should consider these switching behaviors and related risks when patients start a brand-name drug with a coupon instead of lower-cost generic options.
Many patients use manufacturer-sponsored coupons to reduce their out-of-pocket spending for brand-name prescription drugs.1 Patients receive direct-to-consumer discounts at the point of sale, commonly at retail pharmacies, by presenting product-specific online coupons or hard copies of copay program vouchers, often available on manufacturers’ websites. Recent research indicates that the availability and use of coupons are associated with the level of market competition for a given product.2,3 Prior research in older populations have found that medication switching could disrupt management of chronic conditions like diabetes.4 This may be one of unintended consequences of coupon use for high-cost medications. It would be particularly concerning for those who initiate drugs relying on coupons but cannot afford the medication when coupons become unavailable. However, little is known regarding how coupon use to initiate a medication could influence patients’ medication-switching patterns.
Type 2 diabetes treatments comprise a competitive market with prevalent coupon usage for brand-name drugs. Prior research suggested that new treatment options, such as Sodium-glucose Cotransporter-2 (SGLT2) Inhibitors, are commonly associated with manufacturer-sponsored coupons, whereas generic options like metformin rarely offer such offsets. This contrast provides an opportunity to investigate medication switching associated with coupon use among patients with type 2 diabetes, which this study examines within and between drug classes. In addition, we compare the difference in patients’ medication-switching behavior by the prevalence of coupon use across different drug classes.
Methods
We used the IQVIA Formulary Impact Analyzer retail pharmacy claims data from October 2017 to September 2019.5 This is a nationally representative claims database with patient-level, transactional information sourced from 95% of the US retail pharmacies, which has been used in previous studies on drug coupons.2,3 In each recorded claim, coupon use was identified if a manufacturer-sponsored copayment offset was documented as the secondary payment method for that claim.3 We included commercially insured patients with type 2 diabetes who newly started noninsulin oral diabetes medications and did not use any insulin products during this 2-year study period.3 We applied a 3-month washout period and included only patients who did not fill diabetes drug during October 2017 to December 2017, the first 90 days in our data sample.
Patients included in our sample initiated their oral diabetes medications in one of the following 3 drug classes: brand-name SGLT2, brand-name dipeptidyl peptidase IV inhibitors (DPP-IV), and generic metformin (Biguanides). We split the patients into cohorts by drug class in order to control for drug class differences in switching because of other, noncoupon factors that may affect drug use. Across these 3 classes, previous evidence had shown that coupon use was highest among SGLT2 drugs because of greater brand-to-brand competition in this market, followed by DPP-IV, and lowest for metformin. We excluded patients with only 1 prescription fill and examined their switching behaviors across different fills for up to 12 months. We defined that a patient had switched drug if at least 1 of the subsequent drug fills differed from the patient’s initial drug fill, under the assumption that different medications should not be used at the same time. Specifically, we categorized switching behaviors as no switching, intraclass switching (ie, using another drug in the same drug class), or interclass switching (ie, using drugs in different drug classes). Within each of the 3 drug groups, we assessed if drug-switching behaviors differed among patients who did not use coupons to initiate their drug fills (proxy for no influence from the coupon) and patients who used coupon for their first fills (proxy for initiating this drug because of the coupon), using chi-square tests (P < 0.05 was significant). For each group, we further estimated multinomial logistic regression models to assess the association between patients’ coupon use at their initial drug fill and the relative risk ratio of intraclass switching and interclass switching relative to no switching, adjusting for patients’ age, sex, and the total number of noninsulin oral drug fills during the 12-month period as potential confounders. We then used marginal effect prediction to calculate the probability of no switching, intraclass switching, and interclass switching, associated with initial coupon use. Institutional review board approval was not sought because this study did not constitute human participants research, in accordance with 45 CFR §46. STATA version 17 (StataCorp LLC) was used for data analysis.
Results
Among 9,781 patients in our sample, 798 (8%), 790 (8%), and 8,193 (84%) patients initiated a SGLT2 drug, a DPP-IV drug, or metformin, respectively. Initial coupon use was highest among the SGLT2 users (50%), followed by DPP-IV users (24%), and metformin users (1%). Patients who started their diabetes treatment with metformin were least likely to switch to other drugs (40%), whereas 56% of SGLT2 and 57% of DPP-IV patients switched to other drugs. We found that, among patients initiating SGLT2 with coupons, 44%, 6%, and 50% had no switching, intraclass switching, and interclass switching, respectively, compared with 24% of no switchers, 8% of intraclass switchers, and 68% of interclass switchers among patients initiating SGLT2 without using coupons (P < 0.001) (Figure 1). Similarly, 43%, 4%, and 53% of patients initiating DPP-IV inhibitors with coupons had no switching, intraclass switching, or interclass switching, respectively, compared with 30%, 4%, and 66% of DPP-IV inhibitor users who initiated their treatments without coupons (P < 0.01). Although SGLT2 and DPP-IV patients who initiated the drugs with a coupon had less frequent switching (especially interclass switching) than those initiating without coupons, the switching patterns among metformin patients did not differ by their initial coupon use. Across the 3 drug groups, patients who started with metformin always had a higher rate of no switching and lower rate of interclass switching than patients initiating with SGLT2 or DPP-IV, regardless of initial coupon use status.
FIGURE 1.
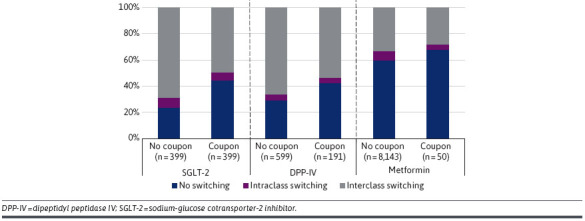
Prevalence of No Switching, Intraclass Switching, and Interclass Switching by Drug Groups and Coupon Use During Patients’ Initial Drug Fill
Multinomial logistic regression estimated similar results. For SGLT2 patients, compared with those initiating the treatment without coupons, those using coupons were associated with 18% (95% CI = 13%-24%; P < 0.001) higher probability of no switching and 16% (95% CI = 10%-22%; P < 0.001) lower probability of interclass switching. For DPP-IV patients, those initiating the treatment with coupons were associated with 9% (95% CI = 2%-16%; P < 0.01) higher probability of no switching and 9% (95% CI = 2%-16%; P < 0.05) lower probability of interclass switching, compared with those starting the treatment without coupons. For patients starting with generic metformin drugs in which coupon use was very rare, we did not observe differences in switching status associated with initial coupon use (Figure 2).
FIGURE 2.
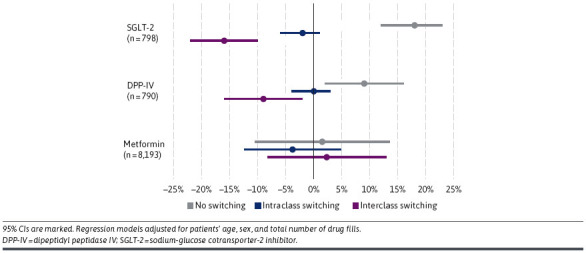
Probability of No Switching, Intraclass Switching, and Interclass Switching Associated with Coupon Use (Compare With No Coupon Use) During Patients’ Initial Drug Fill, by Drug Groups
Discussion
Among patients taking oral medications for their diabetes management, those who started with generic metformin drugs had less frequent drug switching compared with those initiating the brand-name SGLT2 or DPP-IV products. Among patients initiating brand-name SGLT2 or DPP-IV drugs (classes in which coupons were frequently used), using a coupon to initiate the treatment was associated with reduced switching to drugs in other classes. This suggests that coupons may have helped patients afford a clinically beneficial drug that they might not have been able to afford without the coupon (which would have prompted a switch), or, alternatively, that coupon use may have precluded the patient from switching to another drug that might have been clinically more beneficial (which would have prompted a switch). In the first scenario, coupon use would be mainly adding value to patients through increased drug affordability; in the second scenario, coupon use would mainly add value to the drug manufacturer through increased market share.
Our study’s finding extends the literature on the role of patients’ liability for prescription drugs in medication switching among patients with chronic conditions such as type 2 diabetes, which is an important but understudied topic. Although there is a large volume of research on clinical outcomes of switching from one treatment regimen to another, the literature on patient-level cost-related adherence and switching is scarce. Prior research showed that switching to a high deductible health plan increased the discontinuation of brand-name medications among patients with type 2 diabetes.6,7 However, these studies did not take into account the presence of patient-level strategies to reduce their out-of-pocket spending.6,7 To our knowledge, this is the first study documenting medication switching associated with direct-to-consumer copay offset programs among patients with type 2 diabetes.
Although drug coupons reduce patients’ out-of-pocket spending for high-cost brand-name drugs and enhance adherence to the treatment initiation, the availability and eligibility of manufacturer-sponsored coupons is dependent upon manufacturers’ marketing strategy and budgetary situation.8 If a patient starts a high-cost treatment option relying on a coupon, but the coupon value is exhausted, the patient may face challenges in affording the treatment option.
Because of the uncertain and business-dependent nature of coupons, recently, there has been growing policy debates regarding drug coupons at federal and state level.9-11 Some states, such as California and Massachusetts, prohibit the use of drug coupons for multisource brand-name drugs. To address the drug coupons’ effect on high-cost drug use, health plans introduced various copay adjustment programs to steer patients toward lower-cost options. However, with a concern on the impact of payer initiatives on patients’ out-of-pocket spending, 20 states banned health plans from using such programs for their state-sponsored health plans. Similarly, there was legal debates around the federal regulation from implementing copay accumulator programs.12 These contrasts in policy actions taken by different states illustrate that there is limited evidence to inform policy regarding the use and impact of coupons on patients’ and social welfare.
This study’s findings shed light on the issue by empirically documenting both the higher frequency of drug switching among patients with diabetes taking brand-name noninsulin drugs than those taking generic products. Further research is necessary to investigate whether coupon usage impacts patients’ medication adherence and treatment outcomes.
LIMITATIONS
Our study has several limitations. The results should be interpreted as association, not causation, and might not be generalizable to commercially insured patients with other chronic conditions.
Among metformin users, drug-switching behaviors did not differ by initial coupon use. This may have been because of the low coupon use for metformin overall, or to other factors, such as a more favorable benefit-safety profile of this drug or a more favorable affordability profile, given its lower price as compared with the other drug classes examined in this study. Considering that metformin is a generic drug, coupon use observed for this drug may represent different manufacturer strategies or discount mechanisms as compared with the other 2 drug classes that we studied (both of which have brand-name products only). Information on coupon use associated with metformin, therefore, should be interpreted with caution. By focusing on coupon use status at patients’ initial drug fill, out results might not fully account for the influence of coupon use at subsequent fills. This study was unable to account for patient-level covariates, including health status and other comorbidities, insurance plan design, drug formulary and coverage (eg, cost-sharing), or use of other drug discount programs, such as GoodRx, because of the limitation of the retail pharmacy claims data. Similarly, despite our grouping approach to control for drug-level factors, there might be other patient-level clinical reasons (eg, safety and effectiveness of the drugs) that could have influenced medication switching. In addition, we are unable to examine switching behaviors associated with discontinuation of coupons or discount programs nor issues related to dollar limits on coupon use when plans implement copayment accumulators or copayment maximizers.
Conclusions
Patients who started their type 2 diabetes treatment with generic metformin drugs had the lowest rate of drug switching. Patients who initiated treatment with brand-name noninsulin oral drugs such as SGLT2 and DPP-IV inhibitors using manufacturer-sponsored coupons were less likely to switch to drugs in other classes compared with those not using coupons at treatment initiation.
Funding Statement
This research was funded in part by the Arnold Ventures.
REFERENCES
- 1.Sen AP, Kang SY, Rashidi E, Ganguli D, Anderson G, Alexander GC. Characteristics of copayment offsets for prescription drugs in the United States. JAMA Intern Med. 2021;181(6):758-64. doi:10.1001/jamainternmed.2021.0733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kang SY, Sen AP, Levy JF, Long J, Alexander GC, Anderson GF. Factors associated with manufacturer drug coupon use at US pharmacies. JAMA Health Forum. 2021;2(8):e212123. doi:10.1001/jamahealthforum.2021.2123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kang SY, Liu A, Anderson G, Alexander GC. Patterns of manufacturer coupon use for prescription drugs in the US, 2017-2019. JAMA Netw Open. 2023;6(5):e2313578. doi:10.1001/jamanetworkopen.2023.13578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coleman C, Salam T, Duhig A, et al. Impact of non-medical switching of prescription medications on health outcomes: An e-survey of high-volume Medicare and Medicaid physician providers. J Mark Access Health Policy. 2020;8(1):1829883. doi:10.1080/20016689.2020.1829883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.IQVIA. Available IQVIA data. Accessed August 25, 2023. https://www.iqvia.com/insights/the-iqvia-institute/available-iqvia-data
- 6.Fendrick AM, Buxbaum JD, Tang Y, et al. Association between switching to a high-deductible health plan and discontinuation of type 2 diabetes treatment. JAMA Netw Open. 2019;2(11):e1914372. doi:10.1001/jamanetworkopen.2019.14372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lucarelli C, Frean M, Gordon AS, Hua LM, Pauly M. How does cost-sharing impact spending growth and cost-effective treatments? Evidence from deductibles. National Bureau of Economic Research; 2020. Nov 30. Accessed April 21, 2024. http://www.nber.org/papers/w28155
- 8.Fraker JH, Socal MP. Manufacturer-sponsored cost-sharing programs for insulin: Are patients getting the help they need? J Gen Intern Med. 2022;37(6):1561-4. doi:10.1007/s11606-021-06892-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Commonwealth of Massachusetts. Mass. General Laws c.175H § 3: Using prescription drug coupons. Accessed April 5, 2023. https://www.mass.gov/info-details/mass-general-laws-c175h-ss-3
- 10.California Legislative Information. AB-265 Prescription drugs: Prohibition on price discount. 2017. Accessed April 21, 2024. https://leginfo.legislature.ca.gov/faces/billTextClient.xhtml?bill_id=201720180AB265
- 11.Congressional Research Service. Prescription drug discount coupons and patient assistance programs (PAPs): R44264. September 12, 2022. Accessed November 6, 2023. https://crsreports.congress.gov/product/pdf/R/R44264
- 12.National Conference of State Legislatures. Copayment adjustment programs. February 29, 2024. Accessed April 21, 2024. https://www.ncsl.org/health/copayment-adjustment-programs


