Abstract
Background
Continuous glucose monitoring (CGM) devices provide detailed information on daily glucose control and glycemic variability. Yet limited population-based studies have explored the association between CGM metrics and fatty liver. We aimed to investigate the associations of CGM metrics with the degree of hepatic steatosis.
Methods
This cross-sectional study included 1180 participants from the Guangzhou Nutrition and Health Study. CGM metrics, covering mean glucose level, glycemic variability, and in-range measures, were separately processed for all-day, nighttime, and daytime periods. Hepatic steatosis degree (healthy: n = 698; mild steatosis: n = 242; moderate/severe steatosis: n = 240) was determined by magnetic resonance imaging proton density fat fraction. Multivariate ordinal logistic regression models were conducted to estimate the associations between CGM metrics and steatosis degree. Machine learning models were employed to evaluate the predictive performance of CGM metrics for steatosis degree.
Results
Mean blood glucose, coefficient of variation (CV) of glucose, mean amplitude of glucose excursions (MAGE), and mean of daily differences (MODD) were positively associated with steatosis degree, with corresponding odds ratios (ORs) and 95% confidence intervals (CIs) of 1.35 (1.17, 1.56), 1.21 (1.06, 1.39), 1.37 (1.19, 1.57), and 1.35 (1.17, 1.56) during all-day period. Notably, lower daytime time in range (TIR) and higher nighttime TIR were associated with higher steatosis degree, with ORs (95% CIs) of 0.83 (0.73, 0.95) and 1.16 (1.00, 1.33), respectively. For moderate/severe steatosis (vs. healthy) prediction, the average area under the receiver operating characteristic curves were higher for the nighttime (0.69) and daytime (0.66) metrics than that of all-day metrics (0.63, P < 0.001 for all comparisons). The model combining both nighttime and daytime metrics achieved the highest predictive capacity (0.73), with nighttime MODD emerging as the most important predictor.
Conclusions
Higher CGM-derived mean glucose and glycemic variability were linked with higher steatosis degree. CGM-derived metrics during nighttime and daytime provided distinct and complementary insights into hepatic steatosis.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12933-024-02409-6.
Keywords: Hepatic steatosis, Continues glucose monitoring, Mean glucose level, Glycemic variability, Time in range
Background
Metabolic dysfunction-associated steatotic liver disease (MASLD), characterized by hepatic lipid accumulation, has become the major cause of chronic hepatic diseases and cardiovascular diseases (CVDs) [1–3]. Given the important role of impaired glucose in the development and progression of MASLD [4], maintaining optimal glycemic control is crucial for its prevention and management. However, traditional blood glucose biomarkers like fasting blood glucose (FBG) and glycated hemoglobin (HbA1c) cannot provide information on daily glucose control and glycemic variability [5].
Continuous glucose monitoring (CGM) could capture dynamic glycemic profiles, addressing the limitations of traditional glucose biomarkers [6]. Clinical practice guidelines have already established specific goals for diabetes management based on CGM-derived measures [7], while their applicability to classify the degree of hepatic steatosis in the general population is still unclear. In addition, given the circadian regulation of glucose and differences in daily activity [8], patterns of glucose characteristics are distinct between the nighttime and daytime periods. The international consensus also recommends reporting CGM glucose data separately for nighttime and daytime periods [9]. So far, there is no study reporting the associations of nighttime and daytime CGM metrics with MASLD progression.
Therefore, in this population-based study of middle-aged and elderly Chinese adults, our primary aim was to examine the cross-sectional associations between CGM-derived metrics and the degree of hepatic steatosis, which was determined with magnetic resonance imaging (MRI)-derived proton density fat fraction (PDFF). Our secondary aim was to evaluate the predictive performance of CGM-derived metrics during different time periods for hepatic steatosis.
Methods
Study design and participants
This study was based on the Guangzhou Nutrition and Health Study (GNHS; ClinicalTrials.gov, ID: NCT03179657), a community-based prospective cohort study in South China. Briefly, 4048 participants aged 40–75 years were enrolled between 2008 and 2013 and followed up every 3 years. Participants with previously confirmed diabetes, CVDs, dyslipidemia, cancers or those using medication known to affect lipid metabolism within the three months prior to enrollment were excluded. Sociodemographic, lifestyle, physical activity, dietary intake, anthropometrics, and blood samples were collected at baseline and each follow-up [10]. The study protocol of the GNHS was approved by the Ethics Committee of the School of Public Health at Sun Yat-sen University, and all participants provided written informed consent.
The present study included GNHS participants who completed the fourth follow-up investigation between 2020 and 2023 (n = 1952). CGM devices were used to monitor continuous glucose for two weeks. MRI was applied to assess liver fat content with PDFF. Participants were excluded with following criteria: without valid CGM recordings (n = 553), without abdominal MRI examination (n = 164), heavy alcohol drinkers (> 70 g/week for women and 140 g/week for men) (n = 5), history of liver cirrhosis (n = 0), or self-reported viral hepatitis (n = 50). Finally, 1180 participants were included in the statistical analyses of the present study (Fig. S1).
Continuous glucose monitoring and glycemic metrics extraction
Participants were equipped with a CGM device (FreeStyle Libre H; Abbott, Abbott Park, IL, USA) for two weeks to continuously monitor interstitial glucose, with readings taken every 15 min. Participants were blinded to their CGM measurements throughout the monitoring period. Valid CGM data were determined after excluding: (1) CGM recordings < 72 h; (2) the first and last two incomplete days; and (3) days with extreme time spent below the target range 3.9 mmol/L (> 99th percentile).
Our present study included nine key CGM-derived measures, which represent different aspects of clinically relevant glycemic characteristics [11, 12]: (1) mean glucose measures, including mean of continuous blood glucose values (MBG), total area under the curve (AUC), and glucose management indicator (GMI); (2) variability measures, including the coefficient of variation (CV) of glucose values, mean amplitude of glucose excursions (MAGE), and mean of daily differences (MODD); and (3) in-range measures, including time in range (TIR), time above range (TAR), and time below range (TBR).
GMI was a linear transformation of the mean glucose value to estimate HbA1C and was calculated using the following formula: 3.31 + 0.02329* (mean glucose in mg/dL) [13]. CV was calculated by dividing the standard deviation (SD) by the mean of the corresponding glucose readings [14]. MAGE was calculated as the average amplitude exceeding one SD from the mean within a day period [15] using the CGMTSA R package [16]. MODD was calculated as the mean difference between glucose values measured at the same time of the day on two consecutive days under standardized conditions [15]. TIR, TBR, and TAR were defined as the percentage of time within the target glucose range of 3.9–10 mmol/L, below 3.9 mmol/L, and above 10 mmol/L, respectively [17].
CGM-derived measures were calculated separately for all-day, nighttime, and daytime intervals. The starting time for night and day period was predefined at 23:00 and 6:30 [18], respectively, aligned with the median bedtime and wake-up time observed within our study population. To consider random errors, the CGM-derived metrics were processed for each day and averaged across all days for further analysis.
Magnetic resonance imaging
Abdominal MRI was performed to measure liver fat content after participants finished the continues glucose monitoring within a few days. The procedure was conducted by experienced technologists according to the protocol of Siemens LiverLab on 3.0 T MAGNETOM Skyra (Siemens Healthineers, Erlangen, Germany), with participants in the supine position. Medical conditions were not considered, except for those that would exclude the participant from being able to undergo an MRI (e.g., if they had an implanted defibrillator or metal implant). Degree of hepatic steatosis was defined by MRI-PDFF [19, 20] as follows: healthy group (PDFF < 5%), mild steatosis (5% ≤ PDFF < 10%), and moderate/severe steatosis (PDFF ≥ 10%).
Statistical analyses
All statistical analyses were performed using R software (version 4.1.2) and Python (version 3.8.5). We presented the characteristics of the study participants according to the degree of hepatic steatosis. Continuous and categorical variables were presented as median (interquartile range 25th and 75th percentiles) and frequencies (%), respectively. Wilcoxon tests were conducted to compare the distributions of CGM-derived metrics between nighttime and daytime.
To normalize the CGM-derived metrics, an arcsine square root transformation was performed for the in-range measures (i.e., TIR, TBR, and TAR), and a log transformation was conducted for the remaining CGM-derived metrics. Normalized CGM-derived metrics were then transformed into sex-specific standardized z-scores for further statistical analyses.
We used multiple ordinal logistic regression models to estimate the cross-sectional associations of CGM-derived metrics (i.e., MBG, AUC, GMI, CV, MAGE, MODD, TIR, TAR, and TBR) during all-day, nighttime and daytime periods with degree of hepatic steatosis (ordered scale), adjusted for age, sex, marital status, education, household income, smoking status, tea drinking, physical activity, total energy intake, dietary carbohydrate, use of glucose-lowering drugs, lipid-lowering drugs, and antihypertensive drugs in model 1, and further adjusted for body mass index (BMI), waist-to-hip ratio (WHR), triglycerides (TG), and high-density lipoprotein (HDL) in model 2. We controlled the false discovery rate (FDR) using the Benjamini–Hochberg method, considering FDR < 0.05 as statistically significant for the above analyses.
To further explore whether the associations between CGM metrics and hepatic steatosis degree could be modified by HbA1c or BMI, we further conducted subgroup analyses stratified by HbA1c (normal glucose tolerance: HbA1c < 5.7%; prediabetes: HbA1c ≥ 5.7% and < 6.5%; and diabetes: HbA1c ≥ 6.5%) and BMI (underweight/normal weight: BMI < 24 kg/m2; and overweight/obese: BMI ≥ 24 kg/m2), adjusting for covariates in model 2. An interaction term was included in the model to test for the interaction effects.
To test the reliability of our primary findings based on above ordinal logistic regression models, we conducted several sensitivity analyses using multiple ordinal logistic regression models, adjusting for covariates in model 2. First, we excluded participants with diabetes (n = 172). Second, we excluded participants with CGM monitoring < ten days (n = 36), as it is recommended to obtain 70% of the CGM data for each participant for statistical analysis [9]. Third, we treated the CGM-derived metrics as sex-specific quantiles. To explore whether different targets of glucose levels may influence the associations between in-range measures and degree of hepatic steatosis, we further processed the in-range measures defined with a target range 3.9–7.8 mmol/L [9] and re-ran the main analyses of model 2.
Then, we employed multinomial logistic regression models to examine the associations between aforementioned CGM-derived metrics and different degrees of hepatic steatosis (unordered scale; healthy group as reference), adjusting for covariates in the model 2. FDR < 0.05 was considered statistically significant.
To evaluate the performance of CGM-derived metrics in the classification of mild and moderate/severe steatosis (healthy group as reference), we built prediction models based on Light Gradient Boosting Machine (lightGBM) [21], which was known for its robust training and low overfitting risk [22]. In the machine learning model, we investigated the performance of different CGM metrics during all day (all-day model), nighttime (nighttime model) and daytime (daytime model), respectively. To explore whether integrating CGM metrics from nighttime and daytime improve the prediction performance for steatosis, we also developed models incorporating CGM metrics from both periods (combined model). We used the average area under the receiver operating characteristic curves (AUROC) derived from 100 iterations of fivefold cross-validation to assess the predictive performance, and performed Wilcoxon tests to compare the performance of different models. Additionally, Youden index was calculated for the developed machine learning models, and the sensitivity and specificity at the maximum Youden index were determined. We used the average Shapley Additive exPlanations (SHAP) [23] values from the combined models to estimate the contribution of CGM-derived metrics for the overall model.
To further explore the associations between CGM metrics and liver fibrosis, we calculated FIB-4 using age and laboratory results from aspartate aminotransferase (AST), alanine aminotransferase (ALT) and platelet count (PLT) as previously described [24]: FIB-4 score = Age [years] × AST [U/L]/(PLT [109/L] × ALT1/2 [U/L]). Participants were categorized into low-risk (FIB-4 < 1.45), indeterminate-risk (FIB-4 1.45–2.67), and high-risk (FIB-4 > 2.67) fibrosis groups. Then, we conducted multiple ordinal logistic regression models to explore the associations between CGM metrics and liver fibrosis degree, adjusting for covariates in model 2. FDR < 0.05 was considered statistically significant.
Results
Population characteristics
A total of 1180 participants were included in the present study (Fig. S1), with a median age of 69.5 years. 698 (59.2%), 242 (20.5%), and 240 (20.3%) participants were categorized as healthy, mild steatosis, and moderate/severe steatosis, respectively. Participant characteristics according to hepatic steatosis degree were summarized in Table 1 and Table S1. Participants with higher degree of hepatic steatosis were more likely to be female, had increased prevalence of diabetes, hypertension and dyslipidemia, higher levels of BMI, waist-to-hip ratio, triglycerides, fasting blood glucose, insulin and HbA1c, and lower levels of high-density lipoprotein cholesterol (Table 1).
Table 1.
Characteristics of the study population according to different degrees of hepatic steatosis in the Guangzhou Nutrition and Health Study
| Healthy | Mild hepatic steatosis | Moderate/Severe hepatic steatosis | P value | |
|---|---|---|---|---|
| n = 698 | n = 242 | n = 240 | ||
| Age, years | 69.1 (66.2, 72.7) | 69.2 (66.2, 72.6) | 69.2 (65.8, 72.4) | 0.369 |
| Female | 483 (69.2) | 160 (66.1) | 192 (80.0) | 0.001 |
| Married | 634 (90.8) | 229 (94.6) | 220 (91.7) | 0.179 |
| Education | 0.280 | |||
| Secondary school or below | 160 (22.9) | 64 (26.4) | 58 (24.2) | |
| High school | 341 (48.9) | 98 (40.5) | 111 (46.2) | |
| College or above | 197 (28.2) | 80 (33.1) | 71 (29.6) | |
| Household income, Yuan/person | 0.279 | |||
| < 1500 | 308 (45.4) | 112 (47.1) | 107 (45.1) | |
| 1500–3000 | 194 (28.6) | 55 (23.1) | 56 (23.6) | |
| > 3000 | 177 (26.1) | 71 (29.8) | 74 (31.2) | |
| Current smoking | 71 (10.2) | 34 (14.0) | 11 (4.6) | 0.002 |
| Current alcohol drinking | 33 (4.7) | 21 (8.7) | 14 (5.8) | 0.076 |
| Current tea drinking | 358 (51.3) | 142 (58.7) | 121 (50.4) | 0.104 |
| Diabetes | 78 (11.2) | 46 (19.0) | 48 (20.0) | < 0.001 |
| Hypertension | 239 (34.3) | 100 (41.3) | 126 (52.5) | < 0.001 |
| Dyslipidemia | 316 (45.3) | 102 (42.1) | 140 (58.3) | < 0.001 |
| Antidiabetic medications | 66 (9.5) | 39 (16.1) | 41 (17.1) | 0.001 |
| Antihypertensive drugs | 215 (30.8) | 95 (39.3) | 115 (47.9) | < 0.001 |
| Lipid-lowering drugs | 202 (29.1) | 74 (30.6) | 66 (27.5) | 0.758 |
| Physical activities, MET-h/d | 36.4 (30.9, 52.6) | 35.9 (31.0, 53.9) | 36.2 (30.7, 47.7) | 0.923 |
| Total energy intake, kcal/d | 1259 (1047, 1549) | 1259 (1023, 1549) | 1202 (977, 1488) | 0.129 |
| Carbohydrate intake, g/d | 170 (149, 192) | 168 (150, 192) | 166 (148, 188) | 0.706 |
| BMI, kg/m2 | 22.4 (20.7, 24.2) | 24.4 (22.6, 26.2) | 25.3 (23.6, 27.4) | < 0.001 |
| Waist-to-hip ratio | 0.92 (0.88, 0.96) | 0.94 (0.91, 0.98) | 0.95 (0.92, 0.98) | < 0.001 |
| Laboratory tests | ||||
| TC, mmol/L | 5.43 (4.68, 6.16) | 5.26 (4.56, 6.00) | 5.38 (4.58, 6.09) | 0.469 |
| TG, mmol/L | 1.16 (0.91, 1.53) | 1.54 (1.13, 2.07) | 1.82 (1.33, 2.56) | < 0.001 |
| HDL, mmol/L | 1.58 (1.35, 1.84) | 1.37 (1.17, 1.55) | 1.29 (1.12, 1.46) | < 0.001 |
| LDL, mmol/L | 3.38 (2.71, 4.04) | 3.28 (2.64, 4.01) | 3.37 (2.54, 3.94) | 0.716 |
| FBG, mmol/L | 5.48 (5.12, 5.93) | 5.78 (5.37, 6.56) | 5.97 (5.48, 6.75) | < 0.001 |
| Insulin, μU/mL | 7.50 (5.40, 10.09) | 10.9 (7.8, 14.0) | 15.2 (10.6, 21.1) | < 0.001 |
| HbA1c, μmol/L | 5.80 (5.50, 6.00) | 5.90 (5.70, 6.30) | 6.00 (5.80, 6.40) | < 0.001 |
| CGM metrics, all day | ||||
| MBG, mmol/L | 5.47 (5.10, 5.91) | 5.70 (5.35, 6.33) | 5.93 (5.51, 6.59) | < 0.001 |
| AUC, mmol/L | 130 (121, 140) | 135 (127, 150) | 141 (131, 157) | < 0.001 |
| GMI, mmol/L | 5.60 (5.45, 5.79) | 5.70 (5.55, 5.96) | 5.80 (5.62, 6.07) | < 0.001 |
| CV, % | 23.7 (20.3, 27.6) | 23.8 (20.1, 28.5) | 24.0 (21.1, 28.3) | 0.604 |
| MAGE, mmol/L | 3.17 (2.61, 4.00) | 3.32 (2.68, 4.31) | 3.61 (2.83, 4.58) | < 0.001 |
| MODD, mmol/L | 0.23 (0.18, 0.30) | 0.25 (0.19, 0.38) | 0.29 (0.21, 0.39) | < 0.001 |
| TAR, % | 0.64 (0.11, 2.46) | 1.00 (0.24, 4.33) | 1.80 (0.39, 6.19) | < 0.001 |
| TBR, % | 3.29 (1.12, 8.81) | 1.92 (0.58, 5.69) | 1.60 (0.40, 4.23) | < 0.001 |
| TIR, % | 93.7 (86.1, 97.4) | 94.4 (87.7, 97.7) | 94.1 (86.3, 97.5) | 0.374 |
Continuous variables were presented as median (interquartile range) and compared by Kruskal–Wallis tests. Categorical variables were presented as n (%) and compared by chi-squared tests. Total number of participants = 1180
MET metabolic equivalent; TC total cholesterol; TG triglycerides; HDL high-density lipoprotein cholesterol; LDL low-density lipoprotein cholesterol; FBG fasting blood glucose; MBG mean blood glucose; AUC total glucose area under the curve; GMI glucose management indicator; CV coefficient of variation; MAGE mean amplitude of glycemic excursions; MODD mean of daily differences; TIR time in range; TAR time above range; TBR time below range
The distributions of the CGM-derived metrics during nighttime and daytime periods are presented in Table S2. Overall, daytime period presented higher glucose levels and variability than nighttime period, including lower TBR and higher MBG, AUC, GMI, CV, MAGE, and TAR (all P < 0.001). However, no significant difference was observed in the distribution of MODD and TIR between daytime and nighttime (P > 0.05).
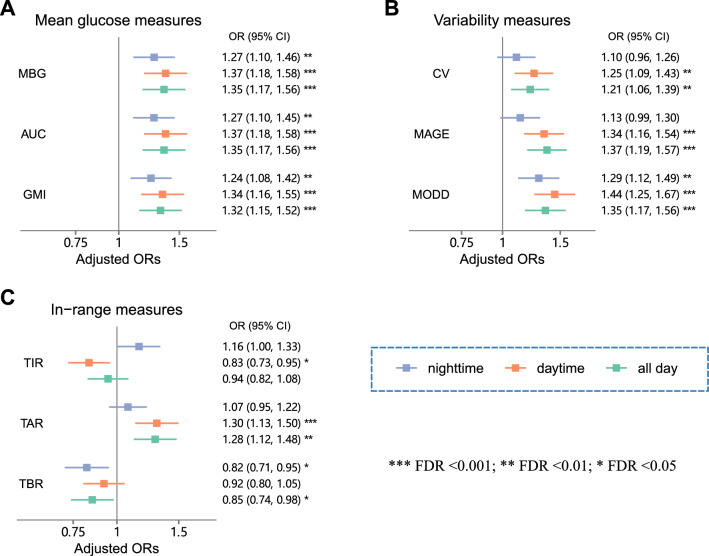
CGM-derived mean glucose and glycemic variability and hepatic steatosis degree
In our analyses with ordinal logistic regression models, after adjusting for potential confounders and multiple testing correction in model 2, higher CGM-derived mean glucose and variability measures were associated with higher degree of hepatic steatosis (Fig. 1A; B). The adjusted ORs (95% CI) of all-day metrics (log-transformed and standardized) for higher steatosis degree were 1.35 (1.17, 1.56) for MBG, 1.35 (1.17, 1.56) for AUC, 1.32 (1.15, 1.52) for GMI, 1.21 (1.06, 1.39) for CV, 1.37 (1.19, 1.57) for MAGE, and 1.35 (1.17, 1.56) for MODD (all FDR < 0.05). Similar results were observed for mean glucose and variability metrics during both nighttime and daytime, with association patterns more pronounced for daytime metrics. The ORs (95% CI) of nighttime and daytime metrics (log-transformed and standardized) for higher steatosis degree were as follows: 1.27 (1.10, 1.46) and 1.37 (1.18, 1.58) for MBG, 1.27 (1.10, 1.45) and 1.37 (1.18, 1.58) for AUC, 1.24 (1.08, 1.42) and 1.34 (1.16, 1.55) for GMI, 1.10 (0.96, 1.26) and 1.25 (1.09, 1.43) for CV, 1.13 (0.99, 1.30) and 1.34 (1.16, 1.54) for MAGE, and 1.29 (1.12, 1.49) and 1.44 (1.25, 1.67) for MODD, respectively (all FDR < 0.05, except for nighttime CV and nighttime MAGE). Consistent results were observed across model 1 (Fig. S2) and model 2. In the subgroup analyses adjusting for covariates in model 2, the association patterns between CGM metrics and hepatic steatosis among subgroups of HbA1c (NGT and prediabetes) (Table S3) and BMI (BMI < 24 kg/m2 and BMI ≥ 24 kg/m2) (Table S4) were consistent with those observed in the main analysis among all participants. No significant interactions were observed (all P for interaction > 0.05).
Fig. 1.
Associations of CGM-derived metrics with higher degree of hepatic steatosis. Forest plots present the ORs (95% CI) of mean glucose measures (A), variability measures (B), and in-range measures (C) for higher degree of hepatic steatosis. Multiple ordinal logistic regression models were performed to examine the associations of CGM-derived measures (normalized and standardized) with higher degree of hepatic steatosis, adjusting for covariates in model 2. False discovery rate (FDR) was applied to correct for multiple comparisons using the Benjamini–Hochberg method. ***FDR < 0.001; **FDR < 0.01; *FDR < 0.05. MBG mean blood glucose; AUC glucose area under the curve; GMI glucose management indicator; CV coefficient of variation; MAGE mean amplitude of glycemic excursions; MODD mean of daily differences; TIR time in range; TAR time above range; TBR time below range
In the sensitivity analyses with multiple ordinal regression models after adjusting for covariates in model 2, similar results were observed for the associations of CGM-derived mean glucose and variability metrics with steatosis degree after excluding participants with diabetes (Fig. S3), excluding participants with CGM data of less than ten days (Fig. S4), or treating the CGM-derived metrics as sex-specific quantiles (Fig. S5).
CGM-derived in-range measures and hepatic steatosis degree
For in-range measures (arcsine square root transformed and standardized) with the target glucose of range 3.9–10.0 mmol/L, TBR exhibited a negative association (OR: 0.85, 95% CI: 0.74–0.98), TAR showed a positive association (OR: 1.28, 95% CI: 1.12–1.48), and TIR exhibited a null association (OR: 0.94, 95% CI: 0.82–1.08) with steatosis degree during all-day period. Notably, the negative association between nighttime TBR and steatosis degree was observed (OR: 0.82, 95% CI: 0.71–0.95), while the positive association between daytime TAR and steatosis degree was observed (OR: 1.30, 95% CI: 1.13–1.50).
Interestingly, TIR demonstrated a negative association with steatosis degree during daytime (OR: 0.83, 95% CI: 0.73–0.95), while a positive association during nighttime (OR: 1.16, 95% CI: 1.00–1.33) (Fig. 1C). To assess whether the associations between TIR and steatosis degree are independent of TAR and TBR, we included TAR and TBR separately into model 2. The positive association between nighttime TIR and steatosis degree remained significant after further adjustment for nighttime TAR, and the negative association between daytime TIR and steatosis degree remained significant after further adjustment for daytime TBR (P < 0.05; Table S5). We obtained similar results with in-range measures when utilizing a target glucose of range 3.9–7.8 mmol/L (Fig. S6; Table S5).
CGM-derived metrics and different degrees of hepatic steatosis
In our subsequent analyses with the multinomial logistic regression models, we obtained consistent results for the associations between CGM-derived metrics and hepatic steatosis, after adjusting for covariates in model 2 (Table 2). Notably, among all nighttime glucose level (i.e., MBG, AUC, and GMI) and variability (i.e., CV, MAGE, and MODD) metrics, only nighttime MODD (OR: 1.32; 95% CI: 1.10, 1.59) was associated with mild steatosis (FDR < 0.05). In addition, a negative association was observed between daytime TIR and moderate/severe steatosis (OR: 0.76; 95% CI: 0.63, 0.92), while a positive association was observed between nighttime TIR and mild steatosis (OR: 1.21; 95% CI: 1.01, 1.45; FDR = 0.054).
Table 2.
Associations of CGM-derived metrics with different degrees of hepatic steatosis
| Nighttime | Daytime | All day | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | FDR | OR (95% CI) | FDR | OR (95% CI) | FDR | |
| MBG | ||||||
| Mild | 1.18 (0.99, 1.42) | 0.090 | 1.24 (1.02, 1.50) | 0.047 | 1.23 (1.02, 1.49) | 0.046 |
| M/S | 1.41 (1.17, 1.72) | 0.001 | 1.55 (1.26, 1.90) | < 0.001 | 1.53 (1.25, 1.87) | < 0.001 |
| AUC | ||||||
| Mild | 1.18 (0.99, 1.42) | 0.092 | 1.23 (1.02, 1.50) | 0.047 | 1.23 (1.02, 1.49) | 0.046 |
| M/S | 1.41 (1.16, 1.72) | 0.001 | 1.55 (1.26, 1.90) | < 0.001 | 1.53 (1.25, 1.87) | < 0.001 |
| GMI | ||||||
| Mild | 1.17 (0.97, 1.40) | 0.118 | 1.22 (1.00, 1.48) | 0.064 | 1.21 (1.00, 1.47) | 0.066 |
| M/S | 1.38 (1.14, 1.67) | 0.002 | 1.51 (1.24, 1.84) | < 0.001 | 1.49 (1.22, 1.81) | < 0.001 |
| CV | ||||||
| Mild | 1.01 (0.85, 1.20) | 0.944 | 1.24 (1.05, 1.47) | 0.023 | 1.17 (0.98, 1.39) | 0.097 |
| M/S | 1.17 (0.97, 1.42) | 0.118 | 1.27 (1.05, 1.54) | 0.023 | 1.26 (1.04, 1.53) | 0.030 |
| MAGE | ||||||
| Mild | 1.00 (0.84, 1.20) | 0.998 | 1.26 (1.06, 1.51) | 0.018 | 1.26 (1.06, 1.51) | 0.019 |
| M/S | 1.26 (1.04, 1.54) | 0.034 | 1.44 (1.18, 1.75) | < 0.001 | 1.50 (1.23, 1.83) | < 0.001 |
| MODD | ||||||
| Mild | 1.32 (1.10, 1.59) | 0.006 | 1.34 (1.11, 1.61) | 0.005 | 1.21 (1.00, 1.46) | 0.063 |
| M/S | 1.45 (1.18, 1.78) | < 0.001 | 1.66 (1.34, 2.04) | < 0.001 | 1.55 (1.26, 1.91) | < 0.001 |
| TIR | ||||||
| Mild | 1.21 (1.01, 1.45) | 0.054 | 0.92 (0.76, 1.11) | 0.419 | 1.05 (0.88, 1.25) | 0.640 |
| M/S | 1.12 (0.92, 1.37) | 0.285 | 0.76 (0.63, 0.92) | 0.009 | 0.88 (0.73, 1.06) | 0.200 |
| TAR | ||||||
| Mild | 1.03 (0.87, 1.23) | 0.771 | 1.19 (0.98, 1.44) | 0.103 | 1.19 (0.98, 1.44) | 0.099 |
| M/S | 1.14 (0.97, 1.35) | 0.143 | 1.45 (1.19, 1.76) | < 0.001 | 1.43 (1.18, 1.74) | < 0.001 |
| TBR | ||||||
| Mild | 0.81 (0.68, 0.97) | 0.038 | 0.93 (0.79, 1.10) | 0.422 | 0.85 (0.71, 1.01) | 0.080 |
| M/S | 0.81 (0.66, 1.00) | 0.067 | 0.90 (0.74, 1.09) | 0.321 | 0.83 (0.68, 1.02) | 0.097 |
Multinomial logistic regression models were performed to examine the associations of CGM-derived measures (normalized and standardized) with mild hepatic steatosis and moderate/severe hepatic steatosis (healthy group as reference), adjusting for covariates in model 2
CGM continuous glucose monitoring; M/S moderate/severe; MBG mean blood glucose; AUC total glucose area under the curve; GMI glucose management indicator; CV coefficient of variation; MAGE mean amplitude of glycemic excursions; MODD mean of daily differences; TIR time in range; TAR time above range; TBR time below range
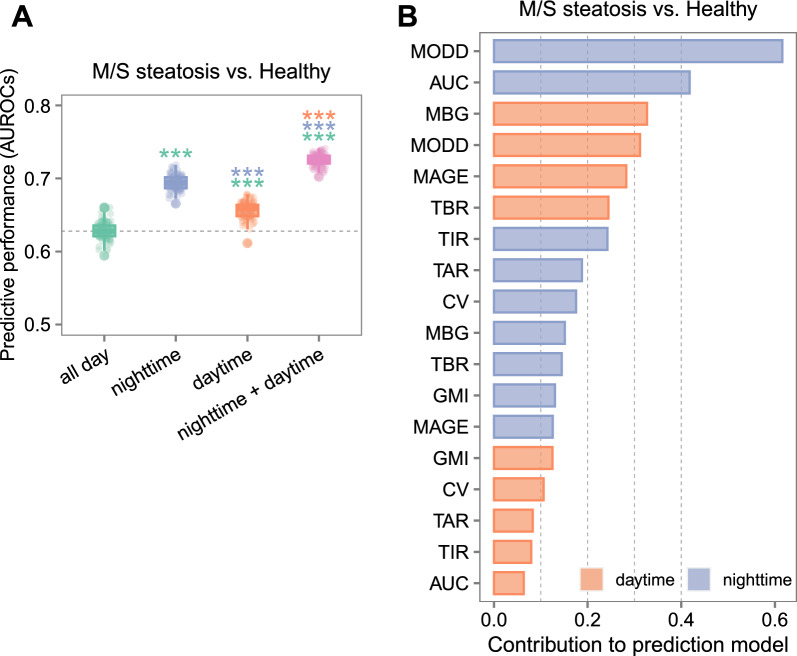
Predictive performance of CGM-derived metrics during different time periods for hepatic steatosis
In the prediction of moderate/severe steatosis (healthy group as reference), nighttime and daytime models both demonstrated higher AUROCs compared to the all-day model (P < 0.001 for both comparisons). The combined model incorporating both nighttime and daytime metrics achieved the greatest performance, with higher AUROC compared to the all-day, nighttime and daytime models (all P < 0.001). The average AUROCs (95% CI) were 0.63 (0.61, 0.65) for the all-day model, 0.69 (0.68, 0.71) for the nighttime model, 0.66 (0.63, 0.68) for the daytime model, and 0.73 (0.71, 0.74) for the combined model, respectively (Fig. 2A). The average sensitivity and specificity (95% CI) were 0.67 (0.50, 0.84) and 0.54 (0.38, 0.71) for the all-day model, 0.70 (0.57, 0.83) and 0.60 (0.47, 0.74) for the nighttime model, 0.65 (0.50, 0.81) and 0.60 (0.44, 0.76) for the daytime model, and 0.73 (0.63, 0.83) and 0.64 (0.54, 0.74) for the combined model (Fig. S7). As ranked by the average SHAP values from the combined model, nighttime MODD showed the strongest predictive power for the prediction of moderate/severe steatosis (Fig. 2B). Similar results were observed for mild steatosis (Fig. S8).
Fig. 2.
Comparison in the predictive performance of CGM-derive metrics during different time periods for moderate/severe hepatic steatosis. A Area under the receiver operating characteristic curves (AUROCs) of CGM-derived metrics for the prediction of moderate/severe steatosis. Models were constructed with CGM-derived metrics during all-day, nighttime and daytime periods separately, as well as nighttime and daytime metrics together. AUROCs were measured by 100 iterations of fivefold cross-validation. Wilcoxon tests were conducted to compare AUROCs of different models. Horizontal dash lines indicate the median AUROCs of the all-day model. Asterisks denote significant differences in AUROCs compared with the model in the same color as the asterisks. ***P < 0.001; **P < 0.01; *P < 0.05. B Contribution of CGM-derived metrics during nighttime and daytime to the prediction of moderate/severe steatosis. Mean SHAP values from the combined model of nighttime and daytime metrics were used to estimate the contribution of CGM-derived metrics to the overall prediction of hepatic steatosis. AUROC area under the receiver operating characteristic curves; M/S moderate/severe
CGM-derived metrics and liver fibrosis
Among 1115 participants with FIB-4 score, 538 (48.3%), 523 (46.9%) and 54 (4.8%) participants were categorized into low-risk, indeterminate-risk and high-risk fibrosis groups, respectively. After adjusting for covariates in model 2 and applying multiple testing correction, lower mean glucose (i.e., MBG, AUC, and GMI) and glycemic variability (i.e., MAGE) were associated with higher FIB-4 (Fig. S9) (FDR < 0.05). As liver fibrosis is progressed from steatosis, we then performed subgroup analyses among participants with and without hepatic steatosis and examined potential interactions. Notably, the negative associations of mean glucose measures and glycemic variability with liver fibrosis degree were observed among participants without hepatic steatosis, but not among those with hepatic steatosis (FDR interaction < 0.05) (Table S6).
Discussion
In this study, we investigated the associations of CGM-derived metrics with MRI-diagnosed steatosis degree among 1180 middle-aged and elderly Chinese adults. We demonstrated positive associations of CGM-derived mean glucose and variability measures with hepatic steatosis degree, especially for the daytime measures. We observed opposite associations between TIR and hepatic steatosis degree during the nighttime and daytime periods. In addition, we found that CGM metrics during nighttime and daytime alone had superior performance than that of all-day metrics, and together improved the predictive performance for hepatic steatosis. Notably, nighttime MODD was the most important CGM metric in predicting hepatic steatosis.
Our results confirm and extend prior studies demonstrating positive associations between blood glucose levels and fatty liver disease [25–27]. Previous studies have showed positive associations between visit-to-visit fasting plasma glucose variability, an indicator of long-term glycemic variability, and MASLD [28, 29]. In contrast, CGM-derived variability metrics indicated short-term glycemic variability [30], and were reported to be associated with adverse clinical outcomes such as diabetic macrovascular and microvascular complications [31]. Moreover, a recent population-based study of non-diabetic individuals has found positive correlations between CGM-derived variability metrics and liver-related clinical measures [11]. However, some studies have reported null associations between CGM-derived variability measures (e.g., SD, MAGE, and MODD) and liver enzymes [32], liver fat content [33], or liver fibrosis [34]. The inconsistency may arise from variations in sample size and study population.
In addition, as a parameter of inter-day glycemic variability reflecting irregular habits and lifestyle [35], MODD demonstrated the strongest predictive power for hepatic steatosis in the current study. The potential mechanism underlying the impact of glycemic variability on hepatic steatosis may involve oxidative stress [30, 36]. It has been suggested that increased glycemic variability led to the production of more reactive oxygen species compared to hyperglycemia alone [30], and oxidative stress was known to be involved in the pathogenesis of MASLD [37].
As an essential metric for diabetic management in clinical practice, TIR has been shown to be inversely associated with HbA1c and the risk of diabetic complications in diabetic patients [38]. However, in our population-based study of middle-age and elderly adults, we did not observe a significant association between daily TIR and hepatic steatosis. Interestingly, when assessed separately during nighttime and daytime periods, TIR exhibited a negative association with hepatic steatosis during daytime, while a positive association during nighttime. This finding was also supported by Keshet et al. that TIR was positive correlated with liver-related clinical measures during sleep time but not wake time in a large non-diabetic population [11]. The discrepancy may stem from the differences in glucose distributions during different periods, as a wide range of glucose exists for a given TIR level. Our findings supported the recommendation from an international consensus statement to assess and appropriately define time in range measures during sleep periods and active periods [9].
Our study is novel to reveal different associations patterns between CGM-derived metrics and hepatic steatosis during nighttime and daytime periods. Blood glucose levels during sleep at night are mainly regulated by insulin secretion to maintain basic metabolism, while during the day are largely influenced by behavioral factors such as diet, activity, and medication intake [39]. In the current study, associations of mean glucose level and glycemic variability metrics with hepatic steatosis were more prominent during daytime, highlighting the importance of glycemic control through regulating behavioral factors for the management of hepatic steatosis. In addition, our observation of improved predictive capacity with CGM metrics during both nighttime and daytime indicated that impairment of both physiological and behavior-responsive glucose contributed to the development of hepatic steatosis, providing insights into the role of glycemic dysfunction in the pathophysiology of hepatic steatosis.
Interestingly, the association patterns of CGM metrics with FIB-4 score among participants without hepatic steatosis were opposite to those of CGM metrics with hepatic steatosis. In contrast, previous studies have demonstrated positive associations between postprandial glucose and liver fibrosis risk in NAFLD patients [40]. However, studies indicated that FIB-4 index is not suitable for primary screening for liver fibrosis in the general population without liver disease [41]. Therefore, the findings we observed between CGM metrics and FIB-4 among participants without hepatic steatosis still need validation in future studies.
The present study has several strengths. First, unlike previous population-based studies that relied on ultrasound or biomarkers for the diagnosis of hepatic steatosis, our utilization of MRI in a large sample size allows the classification of different degree of hepatic steatosis and helps minimize the misclassification bias. Second, CGM-derived metrics were processed separately for nighttime and daytime periods, going beyond the conventional analyses largely focused on metrics of all day. Our study also has several limitations. First, the nature of cross-sectional study restricts the establishment of temporal and causal relationships between the CGM-derived metrics and hepatic steatosis. Second, all participants included in the current study are middle-aged and elderly Chinese individuals, limiting the generalizability of our findings to other age groups or ethnicities. Third, we cannot exclude the potential for selection biases due to the non-probability sampling, although the initial subject selection is unlikely to be differentially related to CGM metrics between participants with and without hepatic steatosis. Lastly, although MRI is recognized as the most accurate non-invasive method to quantify liver fat content, liver biopsy remains the gold standard for assessing histological features of liver diseases.
Conclusions
In summary, we found that higher CGM-derived mean glucose and variability metrics were associated with higher degree of hepatic steatosis, and CGM-derived metrics during the nighttime and daytime periods offered unique and complementary information for hepatic steatosis. Our findings provide novel insights into the preventive strategy of hepatic steatosis via precision glycemic management.
Supplementary Information
Acknowledgements
We thank all participants of the Guangzhou Nutrition and Health Study project and all team members involved in the cohort study and data analyses. We thank the High-Performance Computing Center and the High-Throughput Core Facility at Westlake University.
Abbreviations
- ALT
Alanine aminotransferase
- AST
Aspartate aminotransferase
- AUC
Area under the curve
- AUROC
Area under the receiver operating characteristic curves
- BMI
Body mass index
- CGM
Continuous glucose monitoring
- CI
Confidence interval
- CV
Coefficient of variation
- FBG
Fasting blood glucose
- FDR
False discovery rate
- GMI
Glucose management indicator
- GNHS
Guangzhou Nutrition and Health Study
- HbA1c
Glycated hemoglobin
- HDL
High-density lipoprotein
- lightGBM
Light Gradient Boosting Machine
- MAGE
Mean amplitude of glucose excursions
- MBG
Mean of continuous blood glucose values
- MODD
Mean of daily differences
- MRI
Magnetic resonance imaging
- MASLD
Metabolic dysfunction-associated steatotic liver disease
- OR
Odds ratio
- PDFF
Proton density fat fraction
- PLT
Platelet count
- SD
Standard deviation
- SHAP
Shapley Additive exPlanations
- TAR
Time above range
- TBR
Time below range
- TG
Triglycerides
- TIR
Time in range
- WHR
Waist-to-hip ratio
Author contributions
Y.-m.C. and J.-S.Z. designed and supervised the research; H.Z., K.Z., and X.L. contributed to the development of methodology; H.Z., L.L., Y.Y., and H.C. contributed to data collection; H.Z., K.Z., X.L. L.S, J.C., and Z.M. contributed to data curation; H.Z. performed the data analysis and visualization; H.Z., K.Z., and Z.M. drafted the manuscript. Y.-m.C. and J.-S.Z. critically revised the manuscript. Y.-m.C. and J.-S.Z. contributed to the funding acquisition. All authors have read, revised, and approved the final version of the manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (No. 82073546, 82073529, and 81773416), the Key Research and Development Program of Guangzhou, China (202007040003), “Pioneer” and “Leading goose” R&D Program of Zhejiang (2024SSYS0032, 2022C03102), the 5010 Program for Clinical Researches (No. 2007032) of the Sun Yat-sen University (Guangzhou, China), and the Research Program of Westlake Laboratory of Life Sciences and Biomedicine (202208012). The funders were not involved in the study design, collection, analyses, or the interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
Data availability
The datasets supporting the conclusions of this article are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study protocol of the GNHS was approved by the Ethics Committee of the School of Public Health at Sun Yat-sen University, and all participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Haili Zhong and Ke Zhang have contributed equally to this work and share first authorship.
Contributor Information
Ju-Sheng Zheng, Email: zhengjusheng@westlake.edu.cn.
Yu-ming Chen, Email: chenyum@mail.sysu.edu.cn.
References
- 1.Younossi ZM. Non-alcoholic fatty liver disease—a global public health perspective. J Hepatol. 2019;70(3):531–44. 10.1016/j.jhep.2018.10.033 [DOI] [PubMed] [Google Scholar]
- 2.Chen H, Zhan Y, Zhang J, et al. The global, regional, and national burden and trends of NAFLD in 204 countries and territories: an analysis from global burden of disease 2019. JMIR Public Health Surveill. 2022;8(12): e34809. 10.2196/34809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mantovani A, Csermely A, Petracca G, et al. Non-alcoholic fatty liver disease and risk of fatal and non-fatal cardiovascular events: an updated systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6(11):903–13. 10.1016/S2468-1253(21)00308-3 [DOI] [PubMed] [Google Scholar]
- 4.Bhat N, Mani A. Dysregulation of Lipid and Glucose Metabolism in Nonalcoholic Fatty Liver Disease. Nutrients. 2023;15(10):2323. 10.3390/nu15102323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glycemic Goals and Hypoglycemia. Standards of care in diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S111–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodbard D. Continuous glucose monitoring: a review of successes, challenges, and opportunities. Diabetes Technol Ther. 2016;18(Suppl 2):S3–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ElSayed NA, Aleppo G, Bannuru RR, et al. Glycemic goals and hypoglycemia: standards of care in diabetes—2024. Diabetes Care. 2024;47(Supplement_1):S111–25. 10.2337/dc23-S007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poggiogalle E, Jamshed H, Peterson CM. Circadian regulation of glucose, lipid, and energy metabolism in humans. Metabolism. 2018;84:11–27. 10.1016/j.metabol.2017.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Battelino T, Alexander CM, Amiel SA, et al. Continuous glucose monitoring and metrics for clinical trials: an international consensus statement. Lancet Diabetes Endocrinol. 2023;11(1):42–57. 10.1016/S2213-8587(22)00319-9 [DOI] [PubMed] [Google Scholar]
- 10.Ling C, Zhong H, Zeng F, et al. Cohort Profile: Guangzhou Nutrition and Health Study (GNHS): A Population-Based Multi-Omics Study. J Epidemiol. 2023. 10.2188/jea.JE20230108. 10.2188/jea.JE20230108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keshet A, Shilo S, Godneva A, et al. CGMap: characterizing continuous glucose monitor data in thousands of non-diabetic individuals. Cell Metab. 2023;35(5):758–69. 10.1016/j.cmet.2023.04.002 [DOI] [PubMed] [Google Scholar]
- 12.Rodbard D. Interpretation of continuous glucose monitoring data: glycemic variability and quality of glycemic control. Diabetes Technol Ther. 2009;11(Suppl 1):S55–67. 10.1089/dia.2008.0132 [DOI] [PubMed] [Google Scholar]
- 13.Bergenstal RM, Beck RW, Close KL, et al. Glucose management indicator (GMI): a new term for estimating A1C from continuous glucose monitoring. Diabetes Care. 2018;41(11):2275–80. 10.2337/dc18-1581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Umpierrez GE, Kovatchev BP. Glycemic variability: how to measure and its clinical implication for type 2 diabetes. Am J Med Sci. 2018;356(6):518–27. 10.1016/j.amjms.2018.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Service F J, Molnar GD, Rosevear JW, et al. Mean amplitude of glycemic excursions, a measure of diabetic instability. Diabetes. 1970;19(9):644–55. 10.2337/diab.19.9.644 [DOI] [PubMed] [Google Scholar]
- 16.Shao J, Liu Z, Li S, et al. Continuous Glucose Monitoring Time Series Data Analysis: A Time Series Analysis Package for Continuous Glucose Monitoring Data. J Comput Biol. 2023;30(1):112–6. 10.1089/cmb.2022.0100 [DOI] [PubMed] [Google Scholar]
- 17.Battelino T, Danne T, Bergenstal RM, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. 2019;42(8):1593–603. 10.2337/dci19-0028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Millard LAC, Patel N, Tilling K, et al. GLU: a software package for analysing continuously measured glucose levels in epidemiology. Int J Epidemiol. 2020;49(3):744–57. 10.1093/ije/dyaa004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Caussy C, Alquiraish MH, Nguyen P, et al. Optimal threshold of controlled attenuation parameter with MRI-PDFF as the gold standard for the detection of hepatic steatosis. Hepatology (Baltimore, MD). 2018;67(4):1348–59. 10.1002/hep.29639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ye J, Hu X, Wu T, et al. Insulin resistance exhibits varied metabolic abnormalities in nonalcoholic fatty liver disease, chronic hepatitis B and the combination of the two: a cross-sectional study. Diabetol Metab Syndr. 2019;11:45. 10.1186/s13098-019-0440-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ke G, Qi M, Finley T, et al. LightGBM: a highly efficient gradient boosting decision tree. NIPS. 2017;30:3149–57. [Google Scholar]
- 22.Fu X, Mao X, Wu H, et al. Development and validation of LightGBM algorithm for optimizing of Helicobacter pylori antibody during the minimum living guarantee crowd based gastric cancer screening program in Taizhou, China. Prev Med. 2023;174: 107605. 10.1016/j.ypmed.2023.107605 [DOI] [PubMed] [Google Scholar]
- 23.Lundberg SM, Lee S. A unified approach to interpreting model predictions. NIPS, 2017:4768–4777.
- 24.Sterling RK, Lissen E, Clumeck N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology (Baltimore, MD). 2006;43(6):1317–25. 10.1002/hep.21178 [DOI] [PubMed] [Google Scholar]
- 25.Zou Y, Yu M, Sheng G. Association between fasting plasma glucose and nonalcoholic fatty liver disease in a nonobese Chinese population with normal blood lipid levels: a prospective cohort study. Lipids Health Dis. 2020;19(1):145. 10.1186/s12944-020-01326-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Deng J, Han Z, Tang H, et al. Elevated fasting glucose level increases the risk of fatty liver disease: a 10-year study of 31,154 individuals. BMC Gastroenterol. 2022;22(1):521. 10.1186/s12876-022-02615-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hsu C, Wu F, Lin K, et al. Role of Fatty Liver Index and Metabolic Factors in the Prediction of Nonalcoholic Fatty Liver Disease in a Lean Population Receiving Health Checkup. Clin Transl Gastroenterol. 2019;10(5):1–8. 10.14309/ctg.0000000000000042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hong S, Lee JS, Kim JA, et al. Glycemic variability and the risk of nonalcoholic fatty liver disease: a nationwide population-based cohort study. Diabetes Res Clin Pract. 2021;177: 108922. 10.1016/j.diabres.2021.108922 [DOI] [PubMed] [Google Scholar]
- 29.Zhou H, Zeng X, Xue Y, et al. Visit-to-visit fasting glucose variability in young adulthood and nonalcoholic fatty liver disease in middle age. J Clin Endocrinol Metab. 2022;107(6):e2301–8. 10.1210/clinem/dgac122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ravi R, Balasubramaniam V, Kuppusamy G, et al. Current concepts and clinical importance of glycemic variability. Diabetes Metab Syndr. 2021;15(2):627–36. 10.1016/j.dsx.2021.03.004 [DOI] [PubMed] [Google Scholar]
- 31.Zhou Z, Sun B, Huang S, et al. Glycemic variability: adverse clinical outcomes and how to improve it? Cardiovasc Diabetol. 2020;19(1):102. 10.1186/s12933-020-01085-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Noordam R, Vermond D, Drenth H, et al. High liver enzyme concentrations are associated with higher glycemia, but not with glycemic variability, in individuals without diabetes mellitus. Front Endocrinol. 2017;8:236. 10.3389/fendo.2017.00236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bian H, Yan H, Zeng M, et al. Increased liver fat content and unfavorable glucose profiles in subjects without diabetes. Diabetes Technol Ther. 2011;13(2):149–55. 10.1089/dia.2010.0101 [DOI] [PubMed] [Google Scholar]
- 34.Schiaffini R, Liccardo D, Alisi A, et al. Early glucose derangement detected by continuous glucose monitoring and progression of liver fibrosis in nonalcoholic fatty liver disease: an independent predictive factor? Horm Res Paediatr. 2016;85(1):29–34. 10.1159/000441842 [DOI] [PubMed] [Google Scholar]
- 35.Bowler AM, Burke LM, Coffey VG, et al. Day-to-day glycemic variability using continuous glucose monitors in endurance athletes. J Diabetes Sci Technol. 2024. 10.1177/19322968241250355. 10.1177/19322968241250355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hjort A, Iggman D, Rosqvist F. Glycemic variability assessed using continuous glucose monitoring in individuals without diabetes and associations with cardiometabolic risk markers: a systematic review and meta-analysis. Clin Nutr (Edinburgh, Scotland). 2024;43(4):915–25. 10.1016/j.clnu.2024.02.014 [DOI] [PubMed] [Google Scholar]
- 37.Guo X, Yin X, Liu Z, et al. Non-alcoholic fatty liver disease (NAFLD) pathogenesis and natural products for prevention and treatment. Int J Mol Sci. 2022;23(24):15489. 10.3390/ijms232415489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yoo JH, Kim JH. Time in range from continuous glucose monitoring: a novel metric for glycemic control. Diabetes Metab J. 2020;44(6):828–39. 10.4093/dmj.2020.0257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dimitriadis GD, Maratou E, Kountouri A, et al. Regulation of postabsorptive and postprandial glucose metabolism by insulin-dependent and insulin-independent mechanisms: an integrative approach. Nutrients. 2021;13(1):159. 10.3390/nu13010159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chang X, Bian H, Xia M, et al. Postprandial glucose is correlated with an increasing risk of liver fibrosis in Chinese patients with nonalcoholic fatty liver disease. Diabetes Metab. 2022;48(6): 101377. 10.1016/j.diabet.2022.101377 [DOI] [PubMed] [Google Scholar]
- 41.Sugiyama A, Kurisu A, Bunthen E, et al. Distribution of FIB-4 index in the general population: analysis of 75,666 residents who underwent health checkups. BMC Gastroenterol. 2022;22(1):241. 10.1186/s12876-022-02290-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets supporting the conclusions of this article are available from the corresponding author on reasonable request.