Abstract
Study Design
A prospective experimental study.
Purpose
This biomechanical in vitro study aimed to examine the extent to which the use of a rod persuader (RP) leads to additional mechanical stress on the screw–rod system and determine its influence on the bony anchoring of primary pedicle screws.
Overview of Literature
Degenerative spine diseases and deformities are the most common indications for the stabilization and fusion of spinal segments. The pedicle screw–rod system is considered the gold standard for dorsal stabilization, and an RP is also increasingly being considered to fit the spondylodesis material.
Methods
Ten lumbar spines from body donors were examined. Bisegmental dorsal spinal lumbar interbody fusion of the L3–L5 segments was performed using a pedicle screw–rod system (ROCCIA Multi-LIF Cage; Silony Medical, Germany). In group 1, the titanium rod was inserted without tension, whereas in group 2, the rod was attached to the pedicle screws at the L4 and L5 levels, creating a 5-mm gap. To attach the rod, the RP was used to press the rod into the pedicle screw. The rod was left in place for 30 minutes and then removed.
Results
The rod reduction technique significantly increased the mechanical load on the overall construct measured by strain gauges (p<0.05) and resulted in outright implant failure with pedicle screw pullout in 88.9%.
Conclusions
In cases where the spondylodesis material is not fully attached within the pedicle screw, an RP can be used with extreme caution, particularly in osteoporotic bones, to avoid pedicle screw avulsion and screw anchor failure.
Keywords: Rod persuader, Spine surgery, Pedicle screw avulsion, Lumbar spine, Biomechanics
Introduction
Degenerative spine diseases and deformities are the most common indications for the stabilization and fusion of spinal segments. The pedicle screw–rod system is currently considered the gold standard for dorsal stabilization and fusion of the lumbar spine [1].
In particular, when treating multisegmental spinal deformities and segmental instabilities with spondylolisthesis, a mismatch between the rigid pedicle screws and the rod often occurs during surgery. Here, the spinal surgeon uses a special instrument at his/her disposal, the so-called rod persuader (RP, also called rod-insertion forceps), which presses the rod into the head of the pedicle screw by axially pulling it. Through targeted use, this technique enables not only the treatment of deformities but also the repositioning of a sliding vertebra to restore normal spine alignment. In everyday clinical practice, RPs are also increasingly used to fit the rod into the screw head. This technique does not require the removal of the rod again and manual shaping it outside the site, saving surgical time [2].
Pedicle screw loosening is the most common complication after dorsal instrumentation of the spine. A study reported a pedicle screw loosening rate of 15% in nonosteoporotic spines and up to 60% in osteoporotic vertebral bodies [3]. Consequences of pedicle screw loosening include painful nonunion, spinal instability, deformation, material dislocation up to perforation through the skin, and ultimately, the need for revision surgery [3].
In addition to bone quality, the anchoring stability of pedicle screws is also influenced by the screw design, screw thickness, insertion technique, insertion torque, and screw placement [3]. In contrast, increased axial tension, such as that occurring when using an RP, can result in screw loosening and even tearing out of the screw. This effect has been examined biomechanically in the thoracic spine without additive fusion surgery [2,4]. Despite the widespread use of RPs in everyday clinical and surgical practice, no biomechanical studies have examined the biomechanical consequences of using an RP in lumbar fusion surgery.
This biomechanical in vitro study aimed to examine the extent to which the use of RPs leads to additional mechanical stress on the pedicle screw–rod system and its influence on the bony anchoring of the primary pedicle screws. We hypothesized that the use of RPs increases the tension on the rod, thereby reducing the bony anchoring of the pedicle screw. As a secondary outcome, this study examined whether this technique leads to an outright extraction of the pedicle screws.
Materials and Methods
The study analyzed 10 fresh-frozen lumbar spines from body donors at the Medical Faculty of the Anatomical Institute. The lumbar spines were thawed before preparation and immediately sent for biomechanical analysis.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. The study’s protocol was reviewed and approved by the Institutional Review Board (IRB approval no., 23-1417).
Preparation of the test phase
Bisegmental spinal fusion of the L3–L5 segments was performed using a pedicle screw–rod system (ROCCIA Multi-LIF Cage; Silony Medical, Leinfelden-Echterdingen, Germany). The pedicle screws (Medtronic Inc., Minneapolis, MN, USA) measured 6.5×50 mm and were implanted into the pedicles of L3–L5 vertebral bodies using an image converter. Before inserting the titanium rod, the sides were randomized into two groups (right and left). On side 1, the titanium rod was inserted without bending (straight). This means that rod-insertion and all-caps serial tightening were performed without using an RP for rod reduction to the proximal screw. On side 2, the rod was attached to the pedicle screws of the L5 and L4, creating a 5-mm gap between the rod and the pedicle screw in L3 caused by the prebending of the rod. To attach the rod to the pedicle screw despite the protrusion, an RP was used to press the rod into the pedicle screw (Fig. 1). The rod was left in place for 30 minutes and was then removed.
Fig. 1.
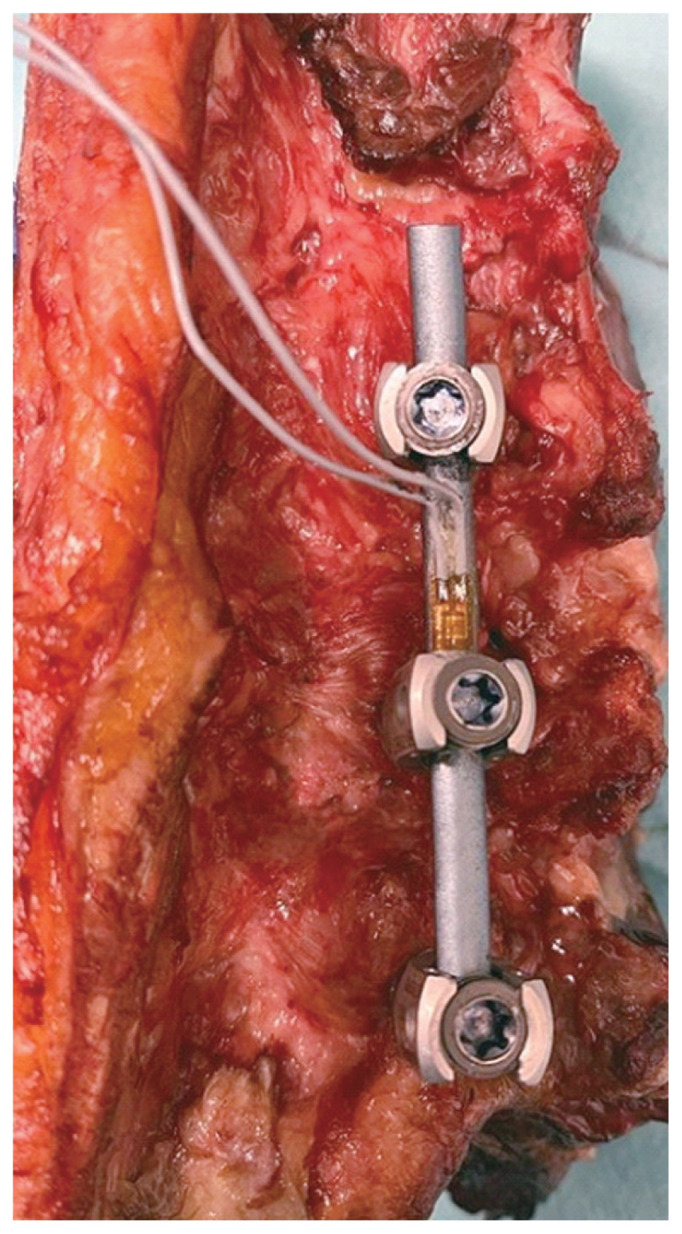
Bi-segmental spinal fusion of the L3–L5 segments using a pedicle screw rod system (ROCCIA Multi-LIF Cage; Silony Medical, Germany). Pedicle screws measure implanted are 6.5×50 mm.
Mechanical load measurement
Rod elongation served as a measure of the mechanical load on the system after attachment to the pedicle screws. For this purpose, a strain gauge (strain gauges, 4-wire strain at 350 Omega; Vishay Measurements Group GmbH, Heilbronn, Germany) was attached to each rod before insertion so that it lay between the pedicle screw of the third and fourth lumbar vertebral bodies. Rod tension was measured before the rod was attached to L3–L5, immediately after attachment, after 1, 5, 10, 15, 20, 25, and 30 minutes, and after the rod was removed (Fig. 2).
Fig. 2.
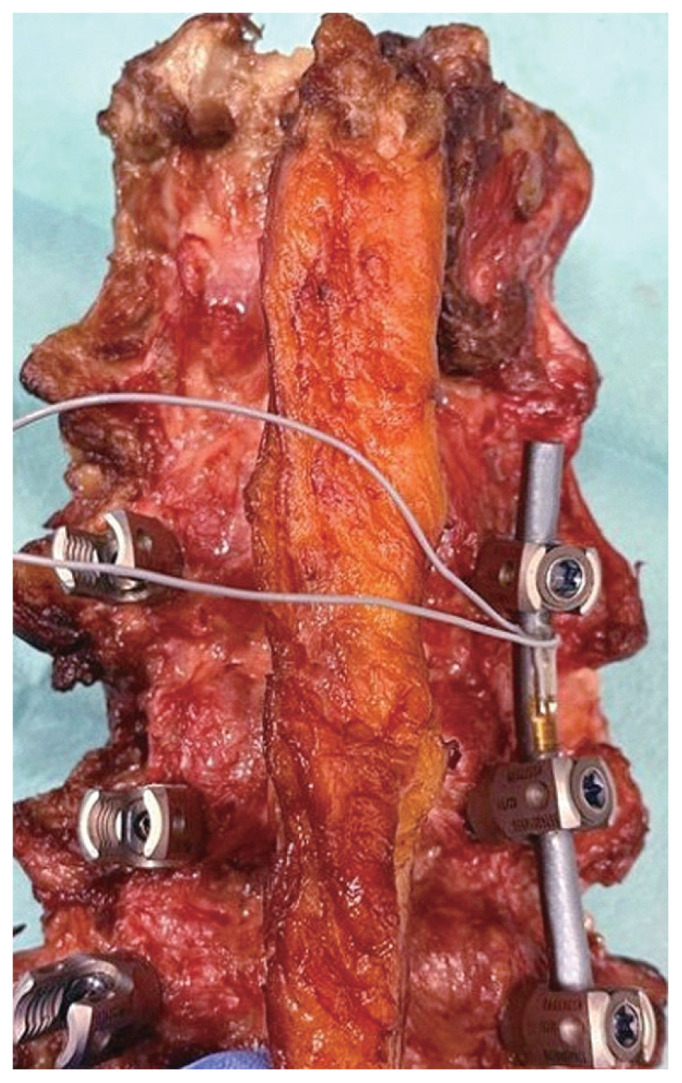
Rod elongation on the system after attachment to pedicle screws attached to a strain gauge (strain gauges, 4-wire strain at 350 Omega; Vishay Measurements Group GmbH, Germany) to each rod so that it lies between the pedicle screw of the third and fourth lumbar vertebral bodies. The rod tension is measured before the rod is attached to L3–5, immediately after attachment, and after 1, 5, 10, 15, 20, 25, and 30 minutes.
Imaging/bone mineral density measurement
A high-resolution computed tomography system was used (Siemens, Munich, Germany). During the evaluation, bone mineral density (BMD) was determined using Hounsfield units (HU).
Statistical analysis
JMP ver. 15.0 (JMP Statistical Discovery LLC, Cary, NC, USA) was used in the analysis of descriptive statistics, providing values of central tendency and dispersion, such as the means and standard deviations of all variables. Bartlett’s test for homoscedasticity was automatically performed using JMP ver. 15.0 [5]. For the comparative analysis, Student t-test was used for normally distributed continuous variables or the Wilcoxon/Kruskal-Wallis test for non-normally distributed continuous variables. For categorical variables, the chi-square test was applied, and for tables with cells <5, Fisher’s exact test was utilized. Statistical significance was defined as p<0.05.
Results
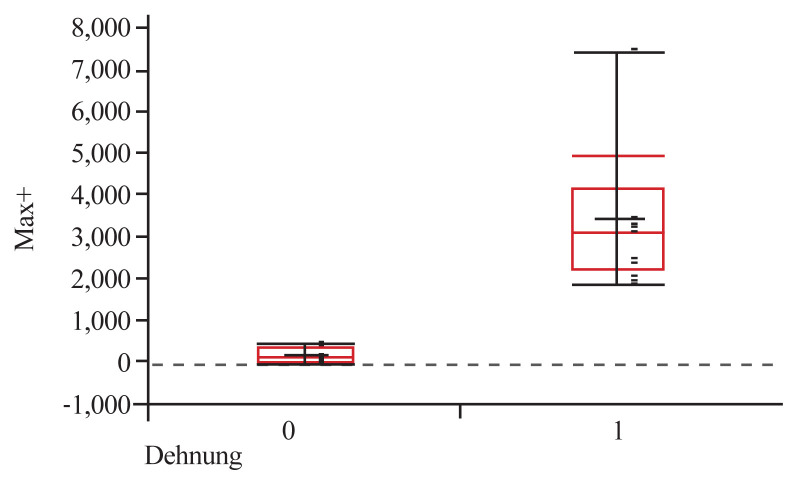
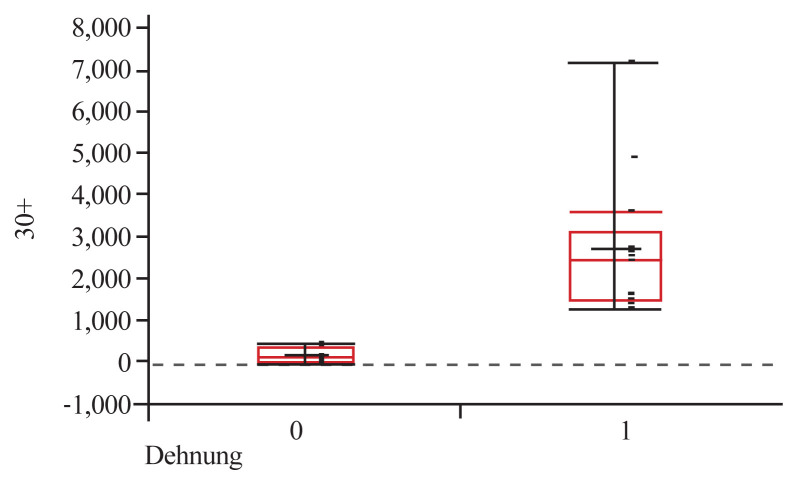
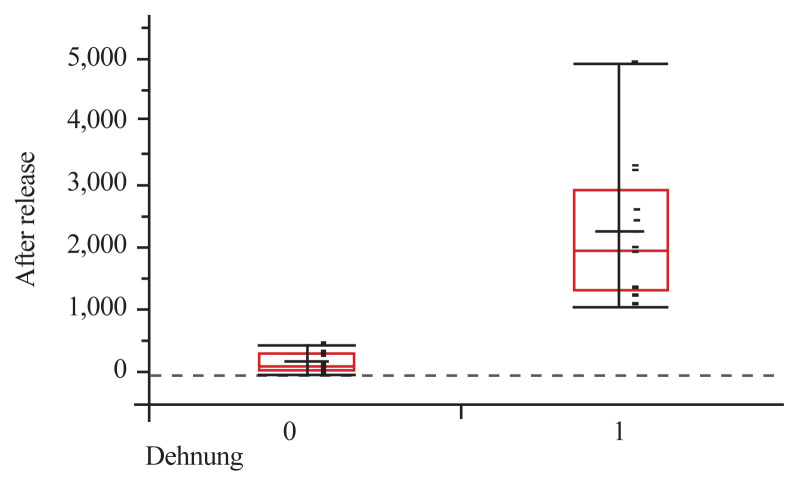
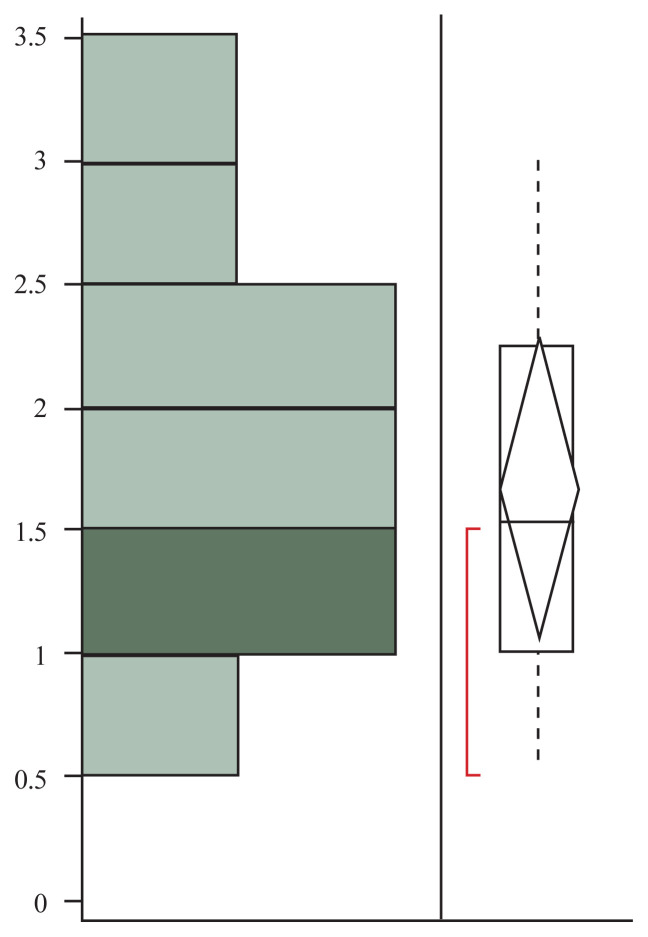
Ten vertebral bodies were prepared for the experiment, and one of them was not used because of a vertebral body fracture and pedicle fracture before preparation. Thus, only nine vertebral bodies were suitable for use in the experiment. They were divided into group 1 (n=9; persuader group) and group 2 (n=9; nonpersuader group). The mean patient age was 87±6.5 years, and there were more women (55.5%) than men. The average BMD in HU the studied vertebrae was 104±80.3 HU. The rod bending values at the beginning of the experiment (0 minutes) were 3,219±1,769 μm/m and 167±173 μm/m in groups 1 and 2, respectively (p<0.001) (Fig. 3). At the end of the experiment (30 minutes), the rod bending values reduced to 2,511±1,854 μm/m and 140±172 μm/m in groups 1 and 2, respectively (p<0.001) (Fig. 4). Furthermore, after the system release, rod bending persisted at 2,009±1,227 μm/m and 129±163 μm/m in groups 1 and 2, respectively (p<0.001) (Fig. 5). Significant differences were found between the control and test specimens at all measurement points (Table 1). The same general trends were observed with no apparent differences noted within those groups when further stratified based on BMD. After rod reduction, screw pullout with an average of 1.5±0.79 mm of dislocation was observed in group 1 (88.9%) compared with 0 mm of dislocation in group 2 (0%) after system release (Fig. 6).
Fig. 3.
Boxplot of rod bending at minute 0.
Fig. 4.
Boxplot of rod bending at minute 30.
Fig. 5.
Boxplot of rod bending after system release.
Table 1.
Biomechanic parameters in group 1 and group 2 as well as macroscopic screw avulsion after persuader
| Variable | Group 1: persuader (n=9) | Group 2: non-persuader (n=9) | p-value |
|---|---|---|---|
| Adjusted rod bending (μm/m) | |||
| 0 min | 3,219±1,769 | 167±173 | <0.001 |
| 1 min | 2,960±1,850 | 149±181 | <0.001 |
| 5 min | 2,719±1,867 | 143±161 | <0.001 |
| 10 min | 2,672±1,867 | 142±158 | <0.001 |
| 15 min | 2,613±1,870 | 142±175 | <0.001 |
| 20 min | 2,558±1,873 | 141±173 | <0.001 |
| 25 min | 2,538±1,872 | 140±173 | <0.001 |
| 30 min | 2,511±1,854 | 140±172 | <0.001 |
| After system release | 2,009±1,227 | 129±163 | <0.001 |
| Macroscopic screw avulsion after Persuader (mm) | 1.5±0.79 | 0 | NA |
Values are presented as mean±standard deviation. Significant differences between the groups were determined by chi-square test or Fisher’s exact test for dichotomized or categorical data. Continuous data were obtained using the independent sampling Student t-test or Mann-Whitney U test.
NA, not applicable.
Fig. 6.
Distribution boxplot of macroscopic screw avulsion after persuader in millimeters.
Discussion
Despite the routine use of a pedicle screw system for the treatment of spinal instability, complications reported are severe, including screw breakage, loosening, or pullout [6,7]. In this study, the results suggest that the use of an RP has devastating biomechanical consequences by significantly increasing pedicle screw loosening and pedicle detachment. Our results, obtained through continuous measurement of rod bending using strain gauges, demonstrated that RPs not only exert axial tension to the pedicle screw but also bend the rod toward the pedicle screw. Interestingly, rod bending decreased within the first 10 minutes after connection to the screw–rod system and then changed only imperceptibly thereafter until the system was released. This indicates that an elastic restoring force continues to exert an axial pull on the screw even after using an RP. In a closed bow system, as observed in this study, approximately 10% of rod bending was “lost” in the system. Furthermore, according to the law of conservation of matter, as postulated by Lomonosov [8], in a closed system, “matter is neither created nor destroyed, it only transforms”. In the present study, this implies that further repositioning of the vertebral body (with good screw hold) or a slow axial pullout of the screw (with poor screw hold, such as in osteoporotic bones) has occurred. Similar phenomena might be observed when using a rod pusher. However, if deformity correction is not necessary, a rod pusher can still be advantageous because the initial axial stress on the pedicle screw would be less.
Because these differences were not observed when the rod was inserted without tension using an RP, the authors emphasized the importance of fitting the rod appropriately outside the surgical site using a rod bending device whenever possible. In deformity surgery, if screw pullout occurred after repositioning, implanting a pedicle screw with a larger screw diameter must be considered. Alternatively, for osteoporotic bones, cement augmentation of the pedicle screws before the repositioning maneuver can be performed to prevent material failure caused by poor bone quality. Recent research reveals a significant number of biomechanical studies evaluating the multiple variables affecting rod–pedicle screw system strength [5]. These factors include osteoporosis [9–13], pedicle morphology [10,14], pedicle screw size [15–18], screw insertion [19,20], pilot-hole tapping [21,22], insertional torque [21,23–26], and pedicle screw augmentation with cement or bone graft substitute [27].
Although the clinical consequences of decreased pedicle screw pullout strength reported in biomechanical studies need further elucidation, the significance of the apparent biomechanical effects of the rod reduction device on pedicle screw fixation, which are nearly universally used particularly during longitudinal construct assembly for posterior instrumentation, cannot be understated. Thus, our results suggest that the rod reduction maneuver causes weakening of the screw–bone interface with consequent rupture by forcing the pedicle screw to be pulled out from the osseous canal, causing fractures in the lumbar spine [5]. A threshold mismatch distance may have existed between the rod and pedicle screw construct that precludes catastrophic failure of the screw. Furthermore, depending on the complexity of the spine pathology, an RP could be used in situations with an important ventral–dorsal mismatch such as spondylolisthesis.
A limitation of this study is the evaluation of an isolated pedicle screw system. Although a comparison of all available commercial pedicle screw systems is untenable, the findings of this study could not be generalized to other screw systems. This issue could depict the failure rate between one screw type and another, requiring improvements in spondylodesis material and further investigations. In addition, cemented pedicle screws in osteoporotic specimens should be compared with pedicle screws with a larger diameter. Furthermore, as with mostly cadaveric biomechanical studies, the whole experiment under controlled conditions is limited by a small sample size and is dependent on the availability of specimens in the laboratory. Although each spine level was compared by pair, variations in the bone matrix quality and pedicle morphology may bias the results. Our laboratory setting enables the use of an X-ray device (fluoroscope) with direct visualization of the vertebral composition, allowing for optimal trajectories of pedicle screws and avoiding accidental fractures of the vertebral body along the axis of the pedicle screw during experiments.
Overall, our results may have significant application in the clinical setting. Although many spine surgeons promoted the rod reduction technique to be safe and effective, they may unknowingly compromise the biomechanical fixation strength of the manipulated pedicle screw. Therefore, close observation of the bone–screw interface during any reduction technique is necessary. Based on the results of our in vitro experience, many intraoperative screw pullout events may be unnoticed when using an RP. Despite the ease and convenience of rod reduction, our results point out that this technique biomechanically results in a poor pedicle screw pullout strength, increased failure of the screw–rod system, and subsequent instability in the operated spine segments. Nevertheless, the exact biomechanical mismatch of the RP through rod reduction on the overall system is poorly understood and was not assessed in this study. A detailed literature search did not yield clinical studies evaluating the abovementioned question. Pedicle screw loosening after using an RP may not be necessary after unilateral reduction in the middle part of a long screw–rod construct. However, screw loosening could be catastrophic with the use of an RP at the cranial or caudal portion of a long screw–rod construct or bilateral at the same level. Techniques to reduce the use of an RP should include rod contouring, using polyaxial screw heads, adjusting the screw depth, or redirecting the trajectory of the pedicle screws [2,20–26].
Conclusions
RP reduction increases pedicle screw pullout in the lumbar spine and typically results in failure of the spondylodesis material. Therefore, in cases where a rod does not fully fit within the pedicle screw head, the use of an RP should proceed with caution, particularly in the osteoporotic spine. Techniques for reducing the need for rod reduction to the pedicle screw heads may include further rod contouring, using polyaxial screw heads, adjusting the screw depth, or redirecting the pedicle screw trajectory. Ultimately, surgeons must be patient, and a detailed preoperative in intraoperative surgical planning is necessary.
Although many confounding factors are likely involved in patient outcomes after spinal surgery, most surgeons use rod reduction devices in the clinical setting. Clinical examinations of the effects of rod reduction on construct failure or pseudarthrosis rates are necessary.
Key Points.
This study involved the use of 10 lumbar spines from body donors. A bi-segmental dorsal spinal lumbar interbody fusion of the L3–L5 segments was performed using a pedicle screw rod system (ROCCIA Multi-LIF Cage, Silony Medical, Germany).
It was demonstrated through continuous measurement of rod bending using strain gauges, that the use of a rod-persuader not only applies axial tension to the pedicle screw but also bends the rod towards the pedicle screw. Interestingly, rod bending decreased within the first 10 minutes after connection to the screw-rod system and then changed only imperceptibly thereafter until the system was released. This indicates that an elastic restoring force continues to exert axial pull on the screw even after the use of the rod-persuader has ceased.
The study highlights the importance that rod persuader reduction increases pedicle screw pull-out in the lumbar spine and typically results in failure of the spondylodesis material.
Footnotes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conceptualization: NK. Methodology: NK, VJH, NO, JMVR. Data curation: VJH, JMVR. Investigation: NK, VJH. Formal analysis: JMVR. Validation: JMVR. Resources: NO, AP. Supervision: PE. Writing–original draft: NK, VJH, JMVR. Writing–review & editing: NK, VJH, NO, AP, JMVR. Final approval of the manuscript: all authors.
References
- 1.Reid PC, Morr S, Kaiser MG. State of the union: a review of lumbar fusion indications and techniques for degenerative spine disease. J Neurosurg Spine. 2019;31:1–14. doi: 10.3171/2019.4.SPINE18915. [DOI] [PubMed] [Google Scholar]
- 2.Paik H, Kang DG, Lehman RA, Jr, Gaume RE, Ambati DV, Dmitriev AE. The biomechanical consequences of rod reduction on pedicle screws: should it be avoided? Spine J. 2013;13:1617–26. doi: 10.1016/j.spinee.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 3.Galbusera F, Volkheimer D, Reitmaier S, Berger-Roscher N, Kienle A, Wilke HJ. Pedicle screw loosening: a clinically relevant complication? Eur Spine J. 2015;24:1005–16. doi: 10.1007/s00586-015-3768-6. [DOI] [PubMed] [Google Scholar]
- 4.Kang DG, Lehman RA, Jr, Wagner SC, et al. Effects of rod reduction on pedicle screw fixation strength in the setting of Ponte osteotomies. Spine J. 2015;15:146–52. doi: 10.1016/j.spinee.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 5.Cho W, Cho SK, Wu C. The biomechanics of pedicle screw-based instrumentation. J Bone Joint Surg Br. 2010;92:1061–5. doi: 10.1302/0301-620X.92B8.24237. [DOI] [PubMed] [Google Scholar]
- 6.Grevenstein D, Scheyerer MJ, Meyer C, et al. Impact of lumbar pedicle screw positioning on screw stability: a biomechanical investigation. Clin Biomech (Bristol, Avon) 2020;74:66–72. doi: 10.1016/j.clinbiomech.2020.02.013. [DOI] [PubMed] [Google Scholar]
- 7.Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Joint Surg Am. 1999;81:1519–28. doi: 10.2106/00004623-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Lomonosov MV. Introduction. In: Lomonosov MV, editor; Leicester HM, editor. Mikhail Vasil'evich Lomonosov on the corpuscular theory. Cambridge (MA): Harvard University Press; 1970. p. 25. [Google Scholar]
- 9.Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS, 3rd, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976) 1994;19:2415–20. doi: 10.1097/00007632-199411000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Coe JD, Warden KE, Herzig MA, McAfee PC. Influence of bone mineral density on the fixation of thoracolumbar implants: a comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine (Phila Pa 1976) 1990;15:902–7. doi: 10.1097/00007632-199009000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Cook SD, Salkeld SL, Stanley T, Faciane A, Miller SD. Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J. 2004;4:402–8. doi: 10.1016/j.spinee.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 12.Paxinos O, Tsitsopoulos PP, Zindrick MR, et al. Evaluation of pullout strength and failure mechanism of posterior instrumentation in normal and osteopenic thoracic vertebrae. J Neurosurg Spine. 2010;13:469–76. doi: 10.3171/2010.4.SPINE09764. [DOI] [PubMed] [Google Scholar]
- 13.Okuyama K, Sato K, Abe E, Inaba H, Shimada Y, Murai H. Stability of transpedicle screwing for the osteoporotic spine: an in vitro study of the mechanical stability. Spine (Phila Pa 1976) 1993;18:2240–5. doi: 10.1097/00007632-199311000-00016. [DOI] [PubMed] [Google Scholar]
- 14.Hirano T, Hasegawa K, Takahashi HE, et al. Structural characteristics of the pedicle and its role in screw stability. Spine (Phila Pa 1976) 1997;22:2504–10. doi: 10.1097/00007632-199711010-00007. [DOI] [PubMed] [Google Scholar]
- 15.Abshire BB, McLain RF, Valdevit A, Kambic HE. Characteristics of pullout failure in conical and cylindrical pedicle screws after full insertion and back-out. Spine J. 2001;1:408–14. doi: 10.1016/s1529-9430(01)00119-x. [DOI] [PubMed] [Google Scholar]
- 16.Lill CA, Schlegel U, Wahl D, Schneider E. Comparison of the in vitro holding strengths of conical and cylindrical pedicle screws in a fully inserted setting and backed out 180 degrees. J Spinal Disord. 2000;13:259–66. doi: 10.1097/00002517-200006000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Pfeiffer FM, Abernathie DL, Smith DE. A comparison of pullout strength for pedicle screws of different designs: a study using tapped and untapped pilot holes. Spine (Phila Pa 1976) 2006;31:E867–70. doi: 10.1097/01.brs.0000244658.35865.59. [DOI] [PubMed] [Google Scholar]
- 18.Polly DW, Jr, Orchowski JR, Ellenbogen RG. Revision pedicle screws: bigger, longer shims: what is best? Spine (Phila Pa 1976) 1998;23:1374–9. doi: 10.1097/00007632-199806150-00015. [DOI] [PubMed] [Google Scholar]
- 19.Chatzistergos PE, Sapkas G, Kourkoulis SK. The influence of the insertion technique on the pullout force of pedicle screws: an experimental study. Spine (Phila Pa 1976) 2010;35:E332–7. doi: 10.1097/BRS.0b013e3181ba0b0c. [DOI] [PubMed] [Google Scholar]
- 20.Suzuki T, Abe E, Okuyama K, Sato K. Improving the pullout strength of pedicle screws by screw coupling. J Spinal Disord. 2001;14:399–403. doi: 10.1097/00002517-200110000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Defino HL, Rosa RC, Silva P, et al. The effect of repetitive pilot-hole use on the insertion torque and pullout strength of vertebral system screws. Spine (Phila Pa 1976) 2009;34:871–6. doi: 10.1097/BRS.0b013e31819e3556. [DOI] [PubMed] [Google Scholar]
- 22.Erkan S, Hsu B, Wu C, Mehbod AA, Perl J, Transfeldt EE. Alignment of pedicle screws with pilot holes: can tapping improve screw trajectory in thoracic spines? Eur Spine J. 2010;19:71–7. doi: 10.1007/s00586-009-1063-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daftari TK, Horton WC, Hutton WC. Correlations between screw hole preparation, torque of insertion, and pullout strength for spinal screws. J Spinal Disord. 1994;7:139–45. doi: 10.1097/00002517-199407020-00007. [DOI] [PubMed] [Google Scholar]
- 24.Inceoglu S, Ferrara L, McLain RF. Pedicle screw fixation strength: pullout versus insertional torque. Spine J. 2004;4:513–8. doi: 10.1016/j.spinee.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 25.Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Can insertional torque predict screw loosening and related failures?: an in vivo study of pedicle screw fixation augmenting posterior lumbar interbody fusion. Spine (Phila Pa 1976) 2000;25:858–64. doi: 10.1097/00007632-200004010-00015. [DOI] [PubMed] [Google Scholar]
- 26.Zdeblick TA, Kunz DN, Cooke ME, McCabe R. Pedicle screw pullout strength: correlation with insertional torque. Spine (Phila Pa 1976) 1993;18:1673–6. doi: 10.1097/00007632-199309000-00016. [DOI] [PubMed] [Google Scholar]
- 27.Taniwaki Y, Takemasa R, Tani T, Mizobuchi H, Yamamoto H. Enhancement of pedicle screw stability using calcium phosphate cement in osteoporotic vertebrae: in vivo biomechanical study. J Orthop Sci. 2003;8:408–14. doi: 10.1007/s10776-003-0639-6. [DOI] [PubMed] [Google Scholar]