Abstract
We aimed to implement strength and balance training for elite adolescent male soccer players with functional ankle instability (FAI) to assess kinesiophobia, ankle instability, ankle function, and performance. This cluster randomized controlled trial comprised 51 elite adolescent male soccer players with FAI recruited from six different teams, divided into strength, balance, and control groups (SG, n = 17; BG, n = 17; and CG, n = 17, respectively). The SG and BG underwent strength and balance training sessions three times per week for 6 weeks. Primary outcomes were the Tampa scale for kinesiophobia-17 (TSK) and Cumberland ankle instability tool (CAIT) scores to assess kinesiophobia and FAI, respectively. Secondary outcomes were ankle strength (four directions), dynamic balance, static balance (ellipse, displacement, velocity), and performance (figure 8 and side-hop tests). A significant interaction effect was observed for both TSK and CAIT post-intervention (both, P < 0.01). In post hoc analyses, the BG had significantly better outcomes in reducing TSK. The SG and BG showed greater improvements in CAIT scores. Regression analysis indicated that CAIT severity correlated significantly with TSK (P = 0.039, R = 0.289). For secondary outcomes, the SG and BG were superior in terms of ankle dorsiflexion/inversion strength, static balance displacement, and figure-8 and side-hop tests (all, P < 0.05). The BG showed significantly better static balance ellipse results (P < 0.05). The 6-week intervention significantly enhanced kinesiophobia management, ankle stability, and performance. Balance training effectively mitigated kinesiophobia and improved balance, compared with strength training alone. Even small variations in CAIT severity can influence kinesiophobia, highlighting the potential benefits of balance training. Integrating balance training into training programs can address both physical and psychological aspects of ankle instability. Research is recommended to explore the longitudinal effects of these interventions and their potential to prevent injury recurrence.
Key points.
The results support the integration of balance training in rehabilitation programs for athletes with FAI. Balance training not only aids in improving physical ankle stability but also contributes to reducing psychological barriers such as kinesiophobia.
The study suggests that consistent and targeted balance and strength training improves FAI and enhances overall athletic performance and readiness, potentially reducing the risk of future ankle injuries.
Through providing evidence-based recommendations for incorporating specific types of training to address both the physical and psychological aspects of FAI in athletes, the findings suggest that such interventions can be immediately applicable in clinical settings.
Key words: Ankle strength, chronic ankle instability, injury prevention
Introduction
Lateral ankle sprain (LAS), the most common injury among athletes (Nelson et al., 2007; Gribble et al., 2016), is associated with high direct and indirect treatment costs (Shah et al., 2016; Feger et al., 2017). Among different sports, soccer has the highest incidence of LAS-related injuries. LAS in young soccer players accounts for approximately 20% of all injuries, resulting in a loss of time during training and competition (Kucera et al., 2005; De Ridder et al., 2017; Donovan et al., 2020). While LAS is generally considered to be easily treatable, it can lead to chronic ankle instability (CAI) (Konradsen et al., 2002; Anandacoomarasamy and Barnsley, 2005). CAI results from repetitive LAS (Hiller et al., 2011), causing mechanical ankle instability, such as ligament laxity. Additionally, it causes functional ankle instability (FAI), marked by proprioceptive deficits, neuromuscular deficits, postural control deficits, and muscle weakness (Hertel, 2002; Sekir et al., 2007; Mitchell et al., 2008; Kobayashi and Gamada, 2014). Moreover, pain and weakness owing to prolonged CAI can lead to decreased joint range of motion (ROM), muscle strength, balance, and performance. These conditions may also progress to articular cartilage defects or post-traumatic ankle osteoarthritis (Hertel, 2000; Valderrabano et al., 2006; 2009).
Several researchers have investigated the efficacy of strength and balance training in improving symptoms associated with FAI (Kidgell et al., 2007; McKeon et al., 2008; Smith et al., 2012; Hall et al., 2015; Linens et al., 2016). While controversial, strength training using elastic bands significantly improved muscular deficits in participants with CAI, providing significant benefits in rehabilitation of this condition (Hall et al., 2015), as well as improving proprioception and balance (Sekir et al., 2007; Smith et al., 2012). Balance training is known to reduce recurrent ankle sprains through improving dynamic balance ability in anterior, anteromedial, and posteromedial directions, the ankle inversion joint position sense, and motor neuron pool excitability (McKeon and Hertel, 2008; Sefton et al., 2011). These types of rehabilitation programs have demonstrated physical improvements in strength, balance, and functional performance (Hall et al., 2018); however, few studies have analyzed the psychological effects of FAI rehabilitation programs in elite adolescent male soccer players.
Psychological variables play a chronic role in physical function (Asiri et al., 2021), and the relationship between FAI and kinesiophobia (fear of movement or activity) has received increasing attention (Fukano et al., 2020; Walankar et al., 2021). Kinesiophobia is an exaggerated fear of movement and the anticipation or sensation of a painful injury (Luque-Suarez et al., 2019), which can affect an athlete's strength or postural control and consequently alter movement patterns, increasing the likelihood of re-injury (Luque-Suarez et al., 2019; Marok and Soundy, 2022). Compared with healthy people, people with FAI have higher levels of kinesiophobia, which negatively affects their muscles and proprioceptors, as well as postural control (Alshahrani and Reddy, 2022; Watanabe et al., 2023).
Investigating the effects of kinesiophobia in ankle rehabilitation could enhance understanding of how to improve this psychological condition and provide valuable data for predicting the success of ankle rehabilitation; however, relevent research is limited.
We aimed to examine the effects of strength and balance training on kinesiophobia, ankle instability, ankle function, and performance in elite adolescent male soccer players with FAI. We hypothesized that incorporating strength and balance exercises into a training program would improve psychological factors, ankle function, and performance compared with those in a control group (CG).
Methods
Study design and blinding
This was a cluster randomized controlled trial, with one elite adolescent male soccer team defined as one cluster to mitigate bias associated with the intervention. Teams expressing a voluntary intention to participate were recruited through phone calls to soccer team coaches. Each recruited team was assigned to either a strength group (SG), a balance group (BG), and a CG by a statistician not involved in the study, using the Research Randomizer program (https://www.randomizer.org/) to conduct randomization by independent lottery.
In this study, double blinding was applied, and all researchers (except JY) and participants remained unaware of each group assignment until the end of the statistical analysis. JY was responsible for training each team on the exercise protocol. JY provided training for the intervention but did not participate in data collection. Statistical analyses were conducted independently by a statistician not involved in the study. The Public Institutional Review Board of the Ministry of Health and Welfare approved this study (P01-202308-01-048), which complied with the tenets of the Declaration of Helsinki. This study was registered with the Clinical Research Information Service under the code (KCT0008854). The Consolidated Standards of Reporting Trials (CONSORT) flow diagram for this study is shown in Figure 1.
Figure 1.
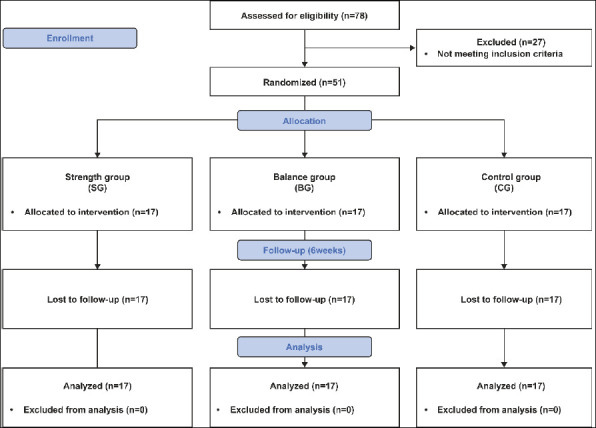
CONSORT flow diagram.
Participants
The study participants were adolescent elite male soccer players, aged 13-18 years, who had experienced an ankle sprain, accompanied with inflammation. This injury had led to an interruption of training for >1 day within 6 months prior to study participation. The participants reported a sensation of instability or ‘giving way’ in the ankle and had experienced at least two previous ankle sprains. Volunteers were required to have a Cumberland ankle instability tool (CAIT) score of ≤25 points. In cases of bilateral ankle FAI, the foot with the lower score was designated as the dominant leg. Individuals who had sustained a fracture or an acute lower extremity injury requiring surgery within 3 months prior to study initiation were excluded.
Additionally, participants who had received any form of treatment, including informal or formal ankle rehabilitation programs for previous sprains within 6 months before the study, were also excluded to minimize confounding variables (Hall et al., 2018). Mechanical instability was assessed using anterior drawer and talar tilt tests, and participants with grade III instability were excluded. The required number of participants was calculated using G*power 3.1 (University of Dusseldorf, Dusseldorf, Germany), with a power set at 0.80, effect size at 0.25, and α at 0.05. Considering a dropout rate of 20%, a total of 51 participants were recruited, with 17 participants allocated to each group.
Prior to study participation, the study purpose, methods, and risks were explained to the participants, and written consent was obtained from the participants and their parents.
Intervention protocol
In this study, an intervention program was implemented three times a week for 6 weeks in all groups. The participants in the SG and BG engaged in strength and balance training, respectively, and only the affected leg was involved. Each week, the first intervention program was implemented with education under the supervision of a physical trainer (JY) with 3 years of experience, and the subsequent sessions were supervised by each team coach. At the end of each week, the intervention program was checked by each team coach to ensure that the intervention program was being implemented appropriately. All participants performed the exercises without the use of ankle braces or bandages to ensure consistency of the intervention and to accurately assess the effects of the training programs on FAI.
Strength training was performed on the basis of an ankle rehabilitation program, as verified in previous studies (Hall et al., 2015; 2018). While seated, the study participants wrapped an elastic band (Theraband®, Akron, OH, USA) around the metatarsal heads of the involved foot, and performed three-directional isotonic ankle strength exercises: dorsiflexion (DF), eversion (EV), and inversion (IV) (Figure 2A). Each trial aimed to maintain a speed of approximately 3-5 s per repetition throughout the full ROM, with approximately 60 s of rest between sets. For ankle plantarflexion (PF), the participants performed a single-leg heel raise over the full ROM (Figure 2B). PF strengthening was performed using single-leg heel raises rather than a resistance band, on the basis of a recommendation by Hall et al. (2015), indicating that heel raises are necessary to provide adequate resistance for the larger muscle groups involved in PF. The strength training protocol is shown in Table 1.
Figure 2.
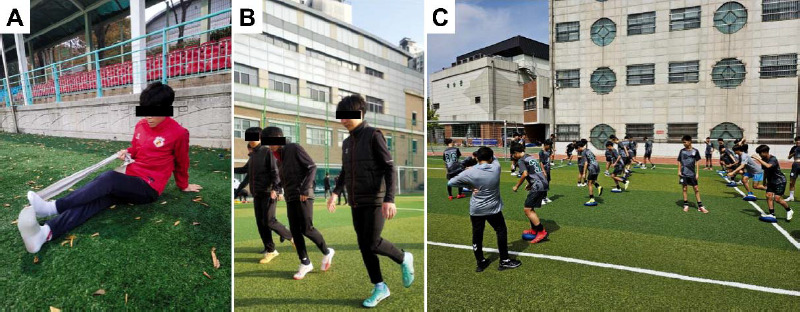
Intervention program. (A) three-direction ankle strength, (B) single-leg heel raise, and (C) balance training.
Table 1.
Strength training protocol.
| Weeks | Exercise | Intensity | Set × repetition |
|---|---|---|---|
| 1 | Three-direction ankle strength | Green band (Level 3) | 3 × 10 |
| Single-leg heel raise | - | 3 × 10 | |
| 2 | Three-direction ankle strength | Green band (Level 3) | 4 × 10 |
| Single-leg heel raise | - | 3 × 10 | |
| 3 | Three-direction ankle strength | Blue band (Level 4) | 3 × 10 |
| Single-leg heel raise | - | 3 × 20 | |
| 4 | Three-direction ankle strength | Blue band (Level 4) | 4 × 10 |
| Single-leg heel raise | - | 3 × 20 | |
| 5 | Three-direction ankle strength | Black band (Level 5) | 3 × 10 |
| Single-leg heel raise | - | 4 × 20 | |
| 6 | Three-direction ankle strength | Black band (Level 5) | 4 × 10 |
| Single-leg heel raise | - | 4 × 20 |
Balance training was performed through modifying the protocol described by McGuine and Keene (2006). The protocol involved performing each exercise twice for 30 s, with a 30-s rest between each exercise. This routine was performed before the main exercise, lasting a total of 8 min. The protocol consisted of a single-leg stance, a single-leg stance while swinging the raised leg, a single-leg squat (30-40°), and a single-leg stance while performing functional activity (catching or kicking). Progression during the 6- week period of balance training was managed as follows. In week 1, participants performed the exercises on the floor with their eyes open. In week 2, the exercises were performed on the floor with the eyes closed. In week 3, the exercises were performed on a balance board with the eyes open. In weeks 4-6, all exercises were performed on the balance board, with single-leg stances conducted with the eyes closed and other movements performed with the eyes open (Figure 2C).
The CG did not implement any additional programs related to ankle rehabilitation beyond the team's own program and was instructed to avoid any additional strength training or rehabilitation of the ankle.
Outcome measurements
Outcome measurements were performed at two different time points (pre- and post-intervention). As primary outcomes, psychological and clinical factors, such as kinesiophobia and ankle instability, were assessed using the Tampa scale for kinesiophobia-17 (TSK) and the CAIT. The TSK, comprising 17 items, assigns a grade on a scale of 1-4 points, where 1 represents strong disagreement; 2, disagreement; 3, agreement; and 4, strong agreement (Luque-Suarez et al., 2019). The TSK score ranges from 17 to 68 points, with a TSK score of ≥37 points indicating kinesiophobia. The TSK questionnaire has high internal consistency (Cronbach’s alpha, 0.79) and excellent test-retest reliability (intraclass correlation coefficient [ICC], 0.90) (Huang et al., 2019). The CAIT questionnaire measures the severity of FAI, and comprises nine items, with scores ranging from 0 to 30 points (Hiller et al., 2006). The CAIT cut-off score is ≤25 points, with scores closer to 0 indicating a greater severity of instability (Wright et al., 2014). The test-retest reliability of the CAIT (ICC) is 0.96 (Hiller et al., 2006).
The secondary outcomes were ankle functions such as strength, dynamic/static balance, and performance. Strength was measured in isometric plantar/dorsiflexion, inversion, and eversion of the ankle using a handheld dynamometer (HHD) (K-Push®, KINVENT, Montpellier, France). The reliability of the HDD used for strength measurement has previously been established, with high intra-rater and inter-rater reliability (Olds et al., 2023). Measurements were taken with participants' ankles positioned in subtalar neutral while seated on an examination table in full leg extension, which was secured to prevent movement. The HHD was placed on the plantar surface of the foot from the first to the fifth metatarsal heads (PF), on the dorsal surface from the first to the fifth metatarsal heads (DF), on the lateral aspect of the fifth metatarsal head (EV), and on the medial aspect of the first metatarsal head (IV). Measurements were taken three times, with a 10-s rest between trials. The measured value was the highest peak torque value during the measurement. Dynamic balance was assessed using the star excursion balance test (SEBT) in the anterior, posterolateral, and posteromedial directions after four practice trials. Three measurements were taken in each direction to ensure the accuracy and consistency of the assessment (Hubbard et al., 2007; Robinson and Gribble, 2008). The participants positioned the hallux of the affected leg at the center of the SEBT grid, placed their hands on the hips, and extended the opposite leg as far as possible in each direction. Failure was defined as any instance where the hand was lifted, the foot of the stance leg shifted, or the foot did not return to its original position. To derive a composite score for the statistical analysis, we calculated the sum of the maximum measured value in each direction, divided this sum by the limb length, and subsequently divided this value by 3 and then multiplied it by 100. Limb length was measured from the anterior superior iliac spine to the medial malleolus using a standard tape, with the participants lying down (Gribble and Hertel, 2003).
Static balance was measured during a 10-s single-leg stance, with the eyes closed, on a force plate (K-Force plate®, KINVENT) (Meras Serrano, et al., 2023). The analysis included evaluating the ellipse, displacement, and velocity of the center of pressure, which are key indicators of balance stability. The measurement was performed with each participant standing on the force plate, hands folded across the chest, opposite leg held at 30° hip flexion and 45° knee flexion, eyes closed, and remaining still for 10 s. When a participant’s opposite leg touched the ground or they were unable to maintain a standing position, the trial was terminated, and the measurement was repeated (Hertel and Olmsted-Kramer, 2007).
Performance was measured using figure-8 and side-hop tests. In the figure-8 test, a cone was placed at 5 m, and the participant quickly completed two laps in a figure-8 pattern using the involved ankle, with the fastest of two laps recorded. The side-hop test involved lateral jumps over a 30-cm distance, with the average of three trials recorded. Incomplete jumps, considered as fouls, were reattempted.
Statistical analysis
All data analysis was performed using SPSS software (version 23.0; IBM Corp., Armonk, NY, USA). All data were verified for normality using a Shapiro–Wilk test, homogeneity at baseline was confirmed through one-way analysis of variance (ANOVA) for continuous data, and Fisher’s exact test was used for nominal data. Differences in all dependent variables during baseline and post-intervention were analyzed using two-way repeated measures ANOVA (group × time). Post hoc analysis results were assessed using the Bonferroni correction. In addition, simple linear regression analysis was used to evaluate how kinesiophobia was related to CAIT and other parameters, e.g., ankle strength (PF, DF, EV, and IV), dynamic balance (SEBT), static balance (ellipse, displacement, and velocity), and performance (figure-8 and side-hop tests). The regression analysis provided insights into the psychological effects of ankle instability, function, and performance. Effect size calculations for all statistically significant differences were performed using partial eta squared (η2) measurements. The following cut-off scores were used to interpret η2: small effects, 0.01 - <0.06; medium effects, 0.06 - <0.14; large effects, ≥0.14. The effect size for within-group differences was calculated using Cohen's d formula and interpreted as follows: small, 0.02; medium, 0.5; and large, 0.08 (Cohen, 1992). Statistical significance was set at α <0.05.
Results
All data were collected within 2 weeks (average 1.5 weeks) of the 6-week intervention. The analysis involved 51 participants with FAI from six teams (assigning two teams for each group), with 17 participants in each intervention group. There were no dropouts during the study. The allocation of the six teams was as follows. In the SG, 22 of 88 team members were evaluated for FAI and five were excluded, resulting in 17 participants (22.72%). In the BG, 29 of 75 team members were evaluated for FAI and 12 were excluded, resulting in 17 participants (22.67%). In the CG, 27 of 92 team members were evaluated for FAI and 10 were excluded, resulting in 17 participants (18.48%). No significant differences in characteristics were observed between the groups pre-intervention (P > 0.05). Table 2 presents the study participants’ baseline characteristics.
Table 2.
Baseline characteristics (n = 51). Data are expressed as means ± standard deviations.
| SG (n = 17) |
BG (n = 17) |
CG (n = 17) |
P-value | |
|---|---|---|---|---|
| Age (years) | 14.1 ± 0.7 | 14.2 ± 0.8 | 14.4 ± 0.7 | 0.478* |
| Height (cm) | 167.6 ± 8.7 | 169.9 ± 7.2 | 170.2 ± 9.3 | 0.639* |
| Weight (kg) | 53.9 ± 7.8 | 55.4 ± 7.3 | 57.6 ± 9.6 | 0.429* |
| BMI (kg/m2) | 19.1 ± 1.6 | 19.1 ± 1.4 | 19.8 ± 1.9 | 0.417* |
| Right ankle (n) | 9 (52.9%) | 11 (64.7%) | 12 (70.6%) | 0.671† |
| Left ankle (n) | 8 (47.1%) | 6 (35.3%) | 5 (29.4%) |
BG, balance group; BMI, body mass index; CG, control group; SG, strength group
* One-way analysis of variance
† Fisher’s exact test.
Primary outcomes
Differences in primary and secondary outcomes among the groups are presented in Table 3. There was a significant interaction effect among the groups for the TSK post-intervention (P = 0.006), indicating that changes in TSK scores over time differed between the groups. Post hoc analysis revealed that the BG showed superior improvements in the TSK compared with the SC and the CG. There was also a significant interaction effect among the groups in terms of CAIT scores (P = 0.005), suggesting that changes in the CAIT over time differed between the groups. Both the SG and BG demonstrated better outcomes compared with the CG in the post hoc analysis. Within-group analysis indicated significant improvements in both TSK and CAIT (P < 0.001 for all). The within-group changes in primary outcomes are shown in Table 4. Additionally, a regression analysis revealed that CAIT significantly correlated with TSK scores (P = 0.039, R = -0.289), indicating a moderate negative correlation (Figure 3). However, no significant associations were found between TSK scores and other parameters, e.g., ankle strength, dynamic balance, static balance, and performance (all, P > 0.05). Detailed regression coefficients, standard errors, and P-values for all tested parameters are provided in Supplementary Data 1.
Table 3.
Comparison between groups from baseline to post-intervention (6 weeks). The data are mean ± standard deviation.
| Outcome | Baseline | 6-Weeks Baseline | P-value* | η2 | Post hoc † | ||||
|---|---|---|---|---|---|---|---|---|---|
| SG (n = 17) | BG (n = 17) | CG (n = 17) | SG (n = 17) | BG (n = 17) | CG (n = 17) | ||||
| TSK | 43.3 ± 3.5 | 43.7 ± 3.7 | 42.5 ± 5.1 | 39.9 ± 4.0 | 36.8 ± 3.0 | 40.0 ± 4.5 | 0.006 | 0.125 | b>a, c |
| CAIT | 20.2 ± 4.1 | 21.3 ± 3.7 | 22.2 ± 2.8 | 25.3 ± 4.1 | 25.5 ± 2.2 | 22.8 ± 3.3 | 0.005 | 0.133 | a, b>c |
| Ankle strength | |||||||||
| PF | 308.8 ± 86.9 | 295.6 ± 70.6 | 292.2 ± 75.0c | 370.8 ± 81.3 | 335.8 ± 51.5 | 308.6 ± 58.5 | 0.095 | 0.140 | |
| DF | 195.2 ± 34.8 | 210.7 ± 62.1 | 192.7 ± 37.7 | 251.8 ± 39.5 | 247.3 ± 27.7 | 212.0 ± 38.8 | 0.025 | 0.208 | a, b>c |
| EV | 105.2 ± 20.3 | 102.3 ± 26.0 | 88.6 ± 21.3 | 122.6 ± 30.0 | 120.4 ± 28.5 | 110.7 ± 37.2 | 0.887 | 0.027 | |
| IV | 127.7 ± 30.1 | 140.2 ± 30.3 | 131.9 ± 45.8 | 190.6 ± 35.5 | 195.7 ± 34.2 | 150 ± 48.1 | <0.001 | 0.219 | a, b>c |
| SEBT | 93.4 ± 6.3 | 98.3 ± 6.0 | 96.5 ± 10.0 | 104.2 ± 4.3 | 102.6 ± 6.2 | 100.3 ± 6.4 | 0.005 | 0.080 | |
| Static balance | |||||||||
| Ellipse | 2215 ± 580.6 | 1948.2 ± 7025 | 2109.9 ± 669 | 1833.2 ± 4689 | 1377.8 ± 429.5 | 2201.7± 647.9 | 0.039 | 0.305 | b>a>c |
| Displacement | 891.5 ± 150.5 | 913 ± 196.1 | 984.1 ± 163.4 | 776.2 ± 160.6 | 745.3 ± 182.1 | 947.3 ± 168.6 | 0.041 | 0.224 | a, b>c |
| Velocity | 88.6 ± 14.9 | 90.7 ± 19.5 | 97.7 ± 16.4 | 77.1 ± 16.0 | 74 ± 18.1 | 85.3 ± 21.1 | 0.634 | 0.066 | |
| Performance | |||||||||
| Figure-8 | 9.8 ± 0.9 | 9.7 ± 0.4 | 9.6 ± 0.6 | 8.8 ± 0.8 | 8.9 ± 0.5 | 9.4 ± 0.5 | <0.001 | 0.184 | a, b>c |
| Side hop | 6.9 ± 1.0 | 7.2 ± 0.7 | 7.2 ± 0.6 | 5.6 ± 0.6 | 6 ± 0.5 | 7.4 ± 0.6 | <0.001 | 0.644 | a, b>c |
BG, balance group; CAIT, Cumberland ankle instability tool; CG, control group; DF, dorsiflexion; EV, eversion; IV, inversion; PF, plantar flexion; SEBT, star excursion balance test; SG, strength group; TSK, Tempa scale of kinesiophobia; a, SG; b, BG; c, CG; the level of statistical significance is indicated in bold.
* Interaction effect (group × time) through two-way repeated measures analysis of variance.
† Post hoc Duncan’s test.
Table 4.
Mean change from baseline to post-intervention (6 weeks) (95% CI).
| Outcome | SG (n = 17) | BG (n = 17) | CG (n = 17) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Δ# | 95% CI | d † | Δ# | 95% CI | d † | Δ# | 95% CI | d † | |
| TSK | 3.4** | 1.5-5.4 | 0.9 | 6.9*** | 4.9-8.8 | 2.0 | 2.5* | 0.5-4.4 | 0.5 |
| CAIT | 5.1*** | 3.2-7.1 | 1.2 | 4.2*** | 2.2-6.1 | 1.4 | 0.6 | -1.3-2.6 | 0.2 |
| Ankle strength | |||||||||
| PF | 62.1*** | 32.9-91.3 | 0.7 | 40.2** | 11.0-69.4 | 0.7 | 16.4 | -12.8-45.6 | 0.2 |
| DF | 56.6*** | 37.9-75.4 | 1.5 | 36.6*** | 17.8-55.3 | 0.8 | 19.3* | 0.5-38.1 | 0.5 |
| EV | 17.4* | 2.6-32.2 | 0.7 | 18.1* | 3.3-32.9 | 0.7 | 22.1** | 7.3-37.0 | 0.7 |
| IV | 62.9*** | 48.5-77.3 | 1.9 | 55.5*** | 41.2-69.9 | 1.7 | 18.1* | 3.7-32.5 | 0.4 |
| SEBT | 10.9*** | 7.6-14.2 | 2.0 | 4.3* | 1.0-7.6 | 0.7 | 3.7* | 0.4-7.0 | 0.4 |
| Static balance | |||||||||
| Ellipse | 381.8* | 13.5-750.1 | 0.7 | 570.4** | 202.2-938.7 | 1.0 | -91.8 | -460.1-276.5 | 0.1 |
| Displacement | 115.3** | 43.7-186.8 | 0.7 | 167.7*** | 96.2-239.3 | 0.9 | 36.9 | -34.7-108.4 | 0.2 |
| Velocity | 11.5** | 3.2-19.8 | 0.7 | 16.7*** | 8.4-25.1 | 0.9 | 12.4** | 4.0-20.7 | 0.7 |
| Performance | |||||||||
| Figure-8 | 1.0*** | 0.7-1.3 | 1.2 | 0.9*** | 0.6-1.1 | 1.9 | 0.2 | <0.1-0.5 | 0.4 |
| Side-hop | 1.3*** | 0.9-1.7 | 1.6 | 1.2*** | 0.8-1.6 | 2.0 | -0.2 | -0.6-0.2 | 0.4 |
BG, balance group; CAIT, Cumberland ankle instability tool; CG, control group; CI, confidence interval; DF, dorsiflexion; EV, eversion; IV, inversion; PF, plantar flexion; SEBT, star excursion balance test; SG, strength group; TSK, Tampa scale of kinesiophobia;
# Mean change from baseline to post-intervention (6 weeks)
† Cohen’s d effect size
***P < 0.001
**P < 0.01
*P < 0.05
Figure 3.
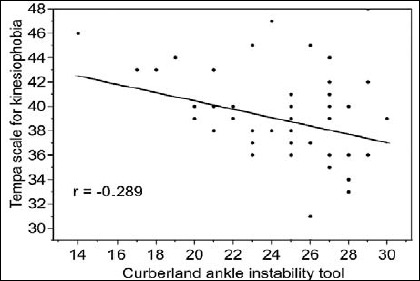
Association between the Cumberland ankle instability tool (CAIT) and the Tampa scale for kinesiophobia (TSK-17).
Supplementary Data 1.
Relationship between kinesiophobia and other factors.
| Factor | B | SE | R | t-value | P-value |
|---|---|---|---|---|---|
| CAIT | -0.342 | 0.162 | -0.289 | -2.116 | 0.039 |
| Ankle strength | |||||
| PF | -0.007 | 0.008 | -0.117 | -0.828 | 0.412 |
| DF | -0.019 | 0.015 | -0.179 | -1.270 | 0.210 |
| EV | -0.018 | 0.018 | -0.140 | -0.993 | 0.326 |
| IV | -0.011 | 0.013 | -0.119 | -0.841 | 0.405 |
| SEBT | -0.007 | 0.100 | -0.010 | -0.068 | 0.946 |
| Static balance | |||||
| Ellipse | 0.001 | 0.001 | 0.107 | 0.755 | 0.454 |
| Displacement | 0.003 | 0.003 | 0.143 | 1.009 | 0.318 |
| Velocity | 0.016 | 0.031 | 0.074 | 0.518 | 0.607 |
| Performance | |||||
| Figure-8 | -0.333 | 0.904 | -0.053 | -0.368 | 0.714 |
| Side hop | 0.208 | 0.588 | 0.050 | 0.354 | 0.725 |
B, partial regression coefficient; CAIT, Cumberland ankle instability tool; DF, dorsiflexion; EV, eversion; IV, inversion; PF, plantar flexion; SEBT, star excursion balance test; SE, standard error; R: standardized partial regression coefficient; TSK, Tampa scale of kinesiophobia; The level of statistical significance is indicated in bold.
Secondary outcomes
There was a significant interaction effect among the groups for ankle strength in DF and IV post-intervention (P = 0.025 and P < 0.001, respectively) (Table 3). Post hoc analysis indicated that the SG and the BG showed superior results compared with the CG. Significant within-group improvements were observed across all four directions of ankle strength (all, P < 0.001) (Table 4). There was a significant interaction effect among the groups for dynamic balance following the intervention (P = 0.005), as well as significant within-group changes (P < 0.001) (Table 3); however, the post hoc analysis did not indicate significant differences between the groups.
There was a significant interaction effect among the groups for static balance of ellipse and displacement following the intervention (P = 0.039 and P = 0.009, respectively) (Table 3). Post hoc analysis showed that the BG demonstrated superior results for ellipse area, while both the SG and BG showed superiority for displacement. Significant within-group improvements were noted for ellipse area, displacement, and velocity (P = 0.009, P < 0.001, and P < 0.001, respectively) (Table 4). There was a significant interaction effect among the groups for performance in both the figure-8 and side-hop tests post-intervention (both, P < 0.001) (Table 3), as well as significant within-group changes (all, P < 0.001) (Table 4). Post hoc comparisons revealed that the SG and the BG exhibited superior results compared with the CG in terms of these performance measures.
Discussion
FAI has emerged as a prevalent concern among elite adolescent soccer players, potentially impeding both physical and psychological performance. Despite the acknowledged significance of FAI, research focusing on rehabilitative strategies for adolescent athletes primarily centers on physical and functional aspects and has often neglected psychological components such as kinesiophobia (Hertel, 2000; Luque-Suarez et al., 2019; Walankar et al., 2021). We aimed to evaluate the effects of targeted ankle rehabilitation exercises, specifically strength and balance training, on psychological, clinical, and functional outcomes in this population. Through systematically comparing improvements in kinesiophobia, ankle instability, and various ankle functions, including strength, static and dynamic balance, and overall performance, we sought to assess the effectiveness of these well-documented rehabilitation approaches in the context of elite adolescent soccer players. Our findings indicated that the SG and the BG exhibited significant enhancements in reducing kinesiophobia and improving ankle stability compared with the CG, with notable differences in specific ankle functions. These results emphasize the importance of tailored rehabilitation exercises in the comprehensive management of FAI among elite adolescent male soccer players.
Kinesiophobia, characterized as a fear of movement and re-injury, has a profound effect on individuals with FAI. This condition hampers joint position sense and postural control and impairs ankle function, which are key factors in maintaining stability and preventing further injury. Studies focusing on CAI, which shares characteristics with FAI, have shown that individuals with ankle instability exhibit significantly higher levels of kinesiophobia compared with their healthy counterparts, highlighting a critical barrier to optimal performance and movement (Hertel and Corbett, 2019; Alshahrani and Reddy, 2022; Watanabe et al., 2023). Kinesiophobia leads to decreased proprioceptive accuracy and impaired postural control in the ankle, which are essential for effective ankle function and stability (Alshahrani and Reddy, 2022; Watanabe et al., 2023). This fear-driven avoidance of movement initiates a detrimental cycle: it contributes to muscle atrophy and dysfunction, leading to altered ankle movement patterns that further exacerbate the risk of injury and the persistence of FAI (Adams et al., 2006; Claeys, 2013; Alshahrani and Reddy, 2022). Our primary outcome was to assess the effects of our interventions on kinesiophobia, to observe any changes post-intervention. The SG and the BG demonstrated significant within-group improvements in reducing kinesiophobia with large effect sizes post-intervention, whereas the CG showed only slight improvements. Post hoc analysis of between-group differences indicated that the BG was most effective in reducing kinesiophobia, while there was no significant difference between the SG and the CG. This suggests that balance training, in particular, plays an essential role in mitigating the fear of movement associated with FAI. Our analysis suggested that enhanced postural control, particularly through improvements in static balance, might play a significant role in reducing kinesiophobia. The SG and the BG showed significant within-group improvements in static balance and muscle strength post-intervention, but the BG exhibited the largest effect sizes for static balance improvements, particularly in the ellipse area values, suggesting that targeted balance training could be particularly effective in mitigating kinesiophobia. In the ellipse area values, the BG group had the best performance, followed by the SG, while the CG showed the least improvement. In terms of displacement, the SG and the BG showed superior results compared with the CG, but no significant difference between the SG and the BG was observed. These results emphasize the potential importance of balance training in effective rehabilitation. This finding suggests that strength and balance training contribute to better control and efficiency in movement, further supporting the role of proprioceptive enhancement in improving joint position sense. These outcomes support the findings of Han et al., who reported that individuals with FAI and higher levels of kinesiophobia relied more on visual cues for maintaining static balance, underscoring the importance of proprioceptive training in reducing reliance on visual input for balance control (Han et al., 2024).
Significant improvements in static balance were observed in both the SG and the BG, with the BG showing a larger effect size. This finding aligns with Hall et al. (2018), who reported greater improvements in static balance in their balance training group compared with strength training. While strength training also enhances static balance (Coughlan et al., 2012; Fullam et al., 2014), our results emphasize the critical importance of balance training for improving static balance and ankle joint position sense. These findings are supported by Lazarou et al. (2018) and Ha et al. (2018), whose findings highlight significant improvements in joint position sense following balance training. Improvements in static balance are essential for reducing kinesiophobia (Alshahrani and Reddy, 2022). Therefore, prioritizing static balance in management strategies could be beneficial for effectively addressing kinesiophobia in athletes with FAI.
FAI, assessed using the CAIT, showed significant improvements in the SG and the BG when compared with the CG. This suggests that both interventions effectively addressed the underlying causes of FAI, such as proprioception deficits and ankle muscle weakness (Willems et al., 2002). No significant between-group difference was observed in terms of eversion muscle strength, but significant within-group improvements were observed in all four directions of ankle strength, including eversion, indicating that the interventions were effective in enhancing overall ankle strength. While improvements in evertor muscle strength are important for stabilizing the ankle (Wisthoff et al., 2019; Khalaj et al., 2020), our findings suggest that enhancements in balance and performance played a substantial role in improving CAIT scores. Enhanced static and dynamic balance directly contribute to better postural control and proprioceptive feedback, which are essential for ankle stability. Studies have shown that balance training improves proprioception and reduces the risk of re-injury through enhancing neuromuscular control (McKeon et al., 2008; Sefton et al., 2011). Our regression analysis revealed that CAIT severity scores significantly correlated with TSK scores, indicating a statistically significant but low correlation. This suggests that while the correlation strength was moderate, the improvements in the CAIT scores were meaningful and associated with reductions in kinesiophobia. Furthermore, performance enhancements, as evidenced by better results in the figure-8 and side-hop tests, indicated improved functional capabilities and confidence in movement, contributing to the reduction in perceived instability and fear of movement. Therefore, while muscle strength is important, the improvements in balance and performance we observed were likely to have been more influential in enhancing the CAIT scores and overall ankle stability.
Performance, as evaluated using figure-8 and side-hop tests, significantly increased in both the SG and BG compared with the CG, with a notable large effect size observed. These improvements emphasize the effectiveness of integrating strength and balance training in rehabilitation protocols. The interaction between increased strength and enhanced balance was a key driver of the observed performance gains. This finding accords with prior studies conducted by McKeon et al. (2008) and Hall et al. (2018), which also identified strength and balance training as pivotal in enhancing athletic performance, reinforcing the synergy between these two types of training. A holistic approach is needed when designing training programs for elite adolescent male soccer players with FAI. Specifically, incorporating both strength and balance exercises is important to alleviate clinical and psychological symptoms associated with FAI and to achieve substantial performance improvements. This integrated training approach presents a promising strategy for optimizing rehabilitation outcomes and enhancing overall athletic readiness.
Strength and balance training programs effectively improved kinesiophobia, ankle instability, function, and performance in the study participants. Balance training demonstrated superior efficacy in reducing kinesiophobia and enhancing static balance. This finding highlights the important role of balance training in bolstering physical capabilities and addressing psychological barriers associated with FAI. Notably, while strength training contributed significantly to rehabilitation outcomes, balance training emerged as a key factor for optimal improvements in both kinesiophobia and static balance.
FAI significantly influences physical performance and psychological factors, making comprehensive treatment approaches essential. This study has demonstrated the effect of strength and balance training in reducing kinesiophobia, suggesting that physical training can also alleviate psychological barriers. However, the inherent challenges posed by kinesiophobia may limit some participants' ability to fully engage in rehabilitation exercises. It was observed that despite improvements, a subset of participants continued to exhibit hesitation and fear, particularly with regard to exercises requiring dynamic balance and proprioception. This highlights the need for tailored approaches that consider the psychological readiness of the athletes, ensuring that rehabilitation programs are not only physically, but also psychologically accessible.
Furthermore, while our interventions focused on physical training components, the persisting levels of kinesiophobia in some participants underscore the potential benefit of integrating psychological interventions. Future studies should explore targeted psychological strategies, e.g., cognitive behavioral therapy or mindfulness-based stress reduction, alongside physical rehabilitation to address the multifaceted nature of kinesiophobia. Such integrative approaches could enhance rehabilitation efficacy and athlete compliance, ultimately improving long-term outcomes in FAI management.
This study had several limitations. Controlling for training other than intervention training for each team was not possible. Physical and tactical training varied among teams, and the effect of these differences on the results remains unknown. However, as all teams participated in the training, we assumed that the difference was not significant. The CG showed improvements in several variables despite not receiving any additional training other than team training; however, the reasons for these improvements remain unknown. The most reasonable inference is familiarity with the tests. Given the intervention period was short (6 weeks), medium- and long-term follow-up results could not be predicted. Future research should be undertaken involving teams with similar training levels, and the results need to be confirmed through long-term follow-up studies.
Conclusion
This pioneering study demonstrated the efficacy of integrating strength and balance training into the routines of elite adolescent male soccer players for addressing FAI-related physical and psychological challenges. Notably, our findings revealed that balance training was more beneficial than strength training in improving kinesiophobia and enhancing balance, underlining its key role in comprehensive rehabilitation programs. Given the association found between the CAIT scores and kinesiophobia, our research highlights the need for targeted strategies to mitigate FAI in this demographic. Balance training needs to be included as a fundamental component of training regimens to effectively address kinesiophobia, enhance ankle stability, and improve overall athletic performance. Future research is recommended to determine the effects of kinesiophobia on performance during actual soccer matches, thereby broadening understanding of FAI in competitive sports.
Acknowledgements
We thank the staff of the Sports Medicine Laboratory of Korea National Sport University for their assistance in evaluating the study and collecting data. The experiments complied with the current laws of the country in which they were performed. The datasets generated and analyzed during the current study are not publicly available, but are available from the corresponding author who was an organizer of the study. The authors have no conflicts of interest to declare.
Biographies

Han Soo PARK
Employment
PhD researcher in Department of Sports Medicine, Korea National Sport University
Degree
PhD
Research interests
Athlete Injury Prevention, osteoarthritis, and athlete Performance
E-mail: 302673@knsu.ac.kr

Jae Keun OH
Employment
Professor in the Department of Sports Medicine, Korea National Sport University
Degree
PhD
Research interests
Athlete injury prevention, Athlete performance, sports medicine, and Sarcopenia
E-mail: sportsomd@knsu.ac.kr

Jun Young KIM
Employment
PhD student in the Sports medicine in Korea National Sport University
Degree
MSc
Research interests
The training in soccer players, injury prevention and sports rehabilitation.
E-mail: gkdlfpsem@naver.com

Jin Ho YOON
Employment
Professor in the Department of Sports Medicine, Korea National Sport University
Degree
PhD
Research interests
The Athletic Training, Rehabilitation and Cardiovascular Disease in Athletes
E-mail: tkd97@knsu.ac.kr
References
- Adams N., Poole H., Richardson C. (2006) Psychological approaches to chronic pain management: part 1. Journal of Clinical Nursing 15, 290-300. https://doi.org/10.1111/j.1365-2702.2006.01304.x 10.1111/j.1365-2702.2006.01304.x [DOI] [PubMed] [Google Scholar]
- Alshahrani M.S., Reddy R.S. (2022) Relationship between kinesiophobia and ankle joint position sense and postural control in individuals with chronic ankle instability-a cross-sectional study. International Journal of Environmental Research and Public Health 19, 2792. https://doi.org/10.3390/ijerph19052792 10.3390/ijerph19052792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anandacoomarasamy A., Barnsley L. (2005) Long term outcomes of inversion ankle injuries. British Journal of Sports Medicine 39, 14. https://doi.org/10.1136/bjsm.2004.011676 10.1136/bjsm.2004.011676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asiri F., Reddy R.S., Tedla J.S., ALMohiza M.A., Alshahrani M.S., Govindappa S.C., Sangadala D.R. (2021) Kinesiophobia and its correlations with pain, proprioception, and functional performance among individuals with chronic neck pain. Plos One 16, e0254262. https://doi.org/10.1371/journal.pone.0254262 10.1371/journal.pone.0254262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claeys K. (2013) The role of proprioceptive postural control in the development and maintenance of low back pain: A cross-sectional and a prospective study. Doctoral dissertation, KU Leuven. [Google Scholar]
- Cohen J. (1992) Statistical power analysis. Current Directions in Psychological Science 1, 98-101. https://doi.org/10.1111/1467-8721.ep10768783 10.1111/1467-8721.ep10768783 [DOI] [Google Scholar]
- Coughlan G.F., Fullam K., Delahunt E., Gissane C., Caulfield B.M. (2012) A comparison between performance on selected directions of the star excursion balance test and the Y balance test. Journal of Athletic Training 47, 366-371. https://doi.org/10.4085/1062-6050-47.4.03 10.4085/1062-6050-47.4.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Ridder R., Witvrouw E., Dolphens M., Roosen P., Van Ginckel A. (2017) Hip strength as an intrinsic risk factor for lateral ankle sprains in youth soccer players: A 3-season prospective study. The American Journal of Sports Medicine 45, 410-416. https://doi.org/10.1177/0363546516672650 10.1177/0363546516672650 [DOI] [PubMed] [Google Scholar]
- Donovan L., Hetzel S., Laufenberg C.R., McGuine T.A. (2020) Prevalence and impact of chronic ankle instability in adolescent athletes. Orthopaedic Journal of Sports Medicine 8, 2325967119900962. https://doi.org/10.1177/2325967119900962 10.1177/2325967119900962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feger M.A., Glaviano N.R., Donovan L., Hart J.M., Saliba S.A., Park J.S., Hertel J. (2017) Current trends in the management of lateral ankle sprain in the United States. Clinical Journal of Sport Medicine 27, 145-152. https://doi.org/10.1097/JSM.0000000000000321 10.1097/JSM.0000000000000321 [DOI] [PubMed] [Google Scholar]
- Fukano M., Mineta S., Hirose N. (2020) Fear Avoidance Beliefs in College Athletes with a History of Ankle Sprain. International Journal of Sports Medicine 41, 128-133. https://doi.org/10.1055/a-1065-1940 10.1055/a-1065-1940 [DOI] [PubMed] [Google Scholar]
- Fullam K., Caulfield B., Coughlan G.F., Delahunt E. (2014) Kinematic analysis of selected reach directions of the Star Excursion Balance Test compared with the Y-Balance Test. Journal of Sport Rehabilitation 23, 27-35. https://doi.org/10.1123/JSR.2012-0114 10.1123/JSR.2012-0114 [DOI] [PubMed] [Google Scholar]
- Gribble P.A., Bleakley C.M., Caulfield B.M., Docherty C.L., Fourchet F., Fong D.T., Hertel J., Hiller C.E., Kaminski T.W., McKeon P.O., Refshauge K.M., Verhagen E.A., Vicenzino B.T., Wikstrom E.A., Delahunt E. (2016) Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. British Journal of Sports Medicine 50, 1496-1505. https://doi.org/10.1136/bjsports-2016-096189 10.1136/bjsports-2016-096189 [DOI] [PubMed] [Google Scholar]
- Gribble P.A., Hertel J. (2003) Considerations for normalizing measures of the Star Excursion Balance Test. Measurement in Physical Education and Exercise Science 7, 89-100. https://doi.org/10.1207/S15327841MPEE0702_3 10.1207/S15327841MPEE0702_3 [DOI] [Google Scholar]
- Ha S.Y., Han J.H., Sung Y.H. (2018) Effects of ankle strengthening exercise program on an unstable supporting surface on proprioception and balance in adults with functional ankle instability. Journal of Exercise Rehabilitation 14, 301-305. https://doi.org/10.12965/jer.1836082.041 10.12965/jer.1836082.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall E.A., Chomistek A.K., Kingma J.J., Docherty C.L. (2018) Balance- and strength-training protocols to improve chronic ankle instability deficits, part i: assessing clinical outcome measures. Journal of Athletic Training 53, 568-577. https://doi.org/10.4085/1062-6050-385-16 10.4085/1062-6050-385-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall E.A., Docherty C.L., Simon J., Kingma J.J., Klossner J.C. (2015) Strength-training protocols to improve deficits in participants with chronic ankle instability: a randomized controlled trial. Journal of Athletic Training 50, 36-44. https://doi.org/10.4085/1062-6050-49.3.71 10.4085/1062-6050-49.3.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han S., Oh M., Lee H., Hopkins J.T. (2024) The effects of kinesiophobia on postural control with chronic ankle instability. Gait & Posture 107, 269-274. https://doi.org/10.1016/j.gaitpost.2023.10.014 10.1016/j.gaitpost.2023.10.014 [DOI] [PubMed] [Google Scholar]
- Hertel J. (2000) Functional instability following lateral ankle sprain. Sports Medicine (Auckland, N.Z.) 29, 361-371. https://doi.org/10.2165/00007256-200029050-00005 10.2165/00007256-200029050-00005 [DOI] [PubMed] [Google Scholar]
- Hertel J. (2002) Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. Journal of Athletic Training 37, 364-375. [PMC free article] [PubMed] [Google Scholar]
- Hertel J., Corbett R.O. (2019) An updated model of chronic ankle instability. Journal of Athletic Training 54, 572-588. https://doi.org/10.4085/1062-6050-344-18 10.4085/1062-6050-344-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertel J., Olmsted-Kramer L.C. (2007) Deficits in time-to-boundary measures of postural control with chronic ankle instability. Gait & Posture 25, 33-39. https://doi.org/10.1016/j.gaitpost.2005.12.009 10.1016/j.gaitpost.2005.12.009 [DOI] [PubMed] [Google Scholar]
- Hiller C.E., Kilbreath S.L., Refshauge K.M. (2011) Chronic ankle instability: evolution of the model. Journal of Athletic Training 46, 133-141. https://doi.org/10.4085/1062-6050-46.2.133 10.4085/1062-6050-46.2.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiller C.E., Refshauge K.M., Bundy A.C., Herbert R.D., Kilbreath S.L. (2006) The Cumberland ankle instability tool: a report of validity and reliability testing. Archives of Physical Medicine and Rehabilitation 87, 1235-1241. https://doi.org/10.1016/j.apmr.2006.05.022 10.1016/j.apmr.2006.05.022 [DOI] [PubMed] [Google Scholar]
- Huang H., Nagao M., Arita H., Shiozawa J., Nishio H., Kobayashi Y., Kaneko H., Nagayama M., Saita Y., Ishijima M., Takazawa Y., Ikeda H., Kaneko K. (2019) Reproducibility, responsiveness and validation of the Tampa Scale for Kinesiophobia in patients with ACL injuries. Health and Quality of Life Outcomes 17, 150. https://doi.org/10.1186/s12955-019-1217-7 10.1186/s12955-019-1217-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard T.J., Kramer L.C., Denegar C.R., Hertel J. (2007) Contributing factors to chronic ankle instability. Foot & Ankle International 28, 343-354. https://doi.org/10.3113/FAI.2007.0343 10.3113/FAI.2007.0343 [DOI] [PubMed] [Google Scholar]
- Khalaj N., Vicenzino B., Heales L.J., Smith M.D. (2020) Is chronic ankle instability associated with impaired muscle strength? Ankle, knee and hip muscle strength in individuals with chronic ankle instability: a systematic review with meta-analysis. British Journal of Sports Medicine 54, 839-847. https://doi.org/10.1136/bjsports-2018-100070 10.1136/bjsports-2018-100070 [DOI] [PubMed] [Google Scholar]
- Kidgell D.J., Horvath D.M., Jackson B.M., Seymour P.J. (2007) Effect of six weeks of dura disc and mini-trampoline balance training on postural sway in athletes with functional ankle instability. Journal of Strength and Conditioning Research 21, 466-469. https://doi.org/10.1519/R-18945.1 10.1519/R-18945.1 [DOI] [PubMed] [Google Scholar]
- Kobayashi T., Gamada K. (2014) Lateral ankle sprain and chronic ankle instability: a critical review. Foot & Ankle Specialist 7, 298-326. https://doi.org/10.1177/1938640014539813 10.1177/1938640014539813 [DOI] [PubMed] [Google Scholar]
- Konradsen L., Bech L., Ehrenbjerg M., Nickelsen T. (2002) Seven years follow-up after ankle inversion trauma. Scandinavian Journal of Medicine & Science in Sports 12, 129-135. https://doi.org/10.1034/j.1600-0838.2002.02104.x 10.1034/j.1600-0838.2002.02104.x [DOI] [PubMed] [Google Scholar]
- Kucera K.L., Marshall S.W., Kirkendall D.T., Marchak P.M., Garrett W.E. (2005) Injury history as a risk factor for incident injury in youth soccer. British Journal of Sports Medicine 39, 462. https://doi.org/10.1136/bjsm.2004.013672 10.1136/bjsm.2004.013672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarou L., Kofotolis N., Pafis G., Kellis E. (2018) Effects of two proprioceptive training programs on ankle range of motion, pain, functional and balance performance in individuals with ankle sprain. Journal of Back and Musculoskeletal Rehabilitation 31, 437-446. https://doi.org/10.3233/BMR-170836 10.3233/BMR-170836 [DOI] [PubMed] [Google Scholar]
- Linens S.W., Ross S.E., Arnold B.L. (2016) Wobble board rehabilitation for improving balance in ankles with chronic instability. Clinical Journal of Sport Medicine 26, 76-82. https://doi.org/10.1097/JSM.0000000000000191 10.1097/JSM.0000000000000191 [DOI] [PubMed] [Google Scholar]
- Luque-Suarez A., Martinez-Calderon J., Falla D. (2019) Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: a systematic review. British Journal of Sports Medicine 53, 554-559. https://doi.org/10.1136/bjsports-2017-098673 10.1136/bjsports-2017-098673 [DOI] [PubMed] [Google Scholar]
- Marok E., Soundy A. (2022) The effect of kinesiophobia on functional outcomes following anterior cruciate ligament reconstruction surgery: an integrated literature review. Disability and Rehabilitation 44, 7378-7389. https://doi.org/10.1080/09638288.2021.1998665 10.1080/09638288.2021.1998665 [DOI] [PubMed] [Google Scholar]
- McGuine T.A., Keene J.S. (2006) The effect of a balance training program on the risk of ankle sprains in high school athletes. The American Journal of Sports Medicine 34, 1103-1111. https://doi.org/10.1177/0363546505284191 10.1177/0363546505284191 [DOI] [PubMed] [Google Scholar]
- McKeon P.O., Hertel J. (2008) Systematic review of postural control and lateral ankle instability, part II: is balance training clinically effective. Journal of Athletic Training 43, 305-315. https://doi.org/10.4085/1062-6050-43.3.293 10.4085/1062-6050-43.3.293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKeon P.O., Ingersoll C.D., Kerrigan D.C., Saliba E., Bennett B.C., Hertel J. (2008) Balance training improves function and postural control in those with chronic ankle instability. Medicine and Science in Sports and Exercise 40, 1810-1819. https://doi.org/10.1249/MSS.0b013e31817e0f92 10.1249/MSS.0b013e31817e0f92 [DOI] [PubMed] [Google Scholar]
- Meras Serrano H., Mottet D., Caillaud K. (2023) Validity and reliability of kinvent plates for assessing single leg static and dynamic balance in the field. Sensors (Basel, Switzerland) 23, 2354. https://doi.org/10.3390/s23042354 10.3390/s23042354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell A., Dyson R., Hale T., Abraham C. (2008) Biomechanics of ankle instability. Part 1: Reaction time to simulated ankle sprain. Medicine and Science in Sports and Exercise 40, 1515-1521. https://doi.org/10.1249/MSS.0b013e31817356d6 10.1249/MSS.0b013e31817356d6 [DOI] [PubMed] [Google Scholar]
- Moritani T., deVries H.A. (1979) Neural factors versus hypertrophy in the time course of muscle strength gain. American Journal of Physical Medicine 58, 115-130. [PubMed] [Google Scholar]
- Nelson A.J., Collins C.L., Yard E.E., Fields S.K., Comstock R.D. (2007) Ankle injuries among United States high school sports athletes, 2005-2006. Journal of Athletic Training 42, 381-387. [PMC free article] [PubMed] [Google Scholar]
- Olds M., McLaine S., Magni N. (2023). Validity and Reliability of the Kinvent Handheld Dynamometer in the Athletic Shoulder Test. Journal of Sport Rehabilitation, 32, 764-772. https://doi.org/10.1123/jsr.2022-0444 10.1123/jsr.2022-0444 [DOI] [PubMed] [Google Scholar]
- Robinson R.H., Gribble P.A. (2008) Support for a reduction in the number of trials needed for the star excursion balance test. Archives of Physical Medicine and Rehabilitation 89, 364-370. https://doi.org/10.1016/j.apmr.2007.08.139 10.1016/j.apmr.2007.08.139 [DOI] [PubMed] [Google Scholar]
- Sefton J.M., Yarar C., Hicks-Little C.A., Berry J.W., Cordova M.L. (2011) Six weeks of balance training improves sensorimotor function in individuals with chronic ankle instability. The Journal of Orthopaedic and Sports Physical Therapy 41, 81-89. https://doi.org/10.2519/jospt.2011.3365 10.2519/jospt.2011.3365 [DOI] [PubMed] [Google Scholar]
- Sekir U., Yildiz Y., Hazneci B., Ors F., Aydin T. (2007) Effect of isokinetic training on strength, functionality and proprioception in athletes with functional ankle instability. Knee Surgery, Sports Traumatology, Arthroscopy 15, 654-664. https://doi.org/10.1007/s00167-006-0108-8 10.1007/s00167-006-0108-8 [DOI] [PubMed] [Google Scholar]
- Shah S., Thomas A.C., Noone J.M., Blanchette C.M., Wikstrom E.A. (2016) Incidence and Cost of Ankle Sprains in United States Emergency Departments. Sports Health 8, 547-552. https://doi.org/10.1177/1941738116659639 10.1177/1941738116659639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B.I., Docherty C.L., Simon J., Klossner J., Schrader J. (2012) Ankle strength and force sense after a progressive, 6-week strength-training program in people with functional ankle instability. Journal of Athletic Training 47, 282-288. https://doi.org/10.4085/1062-6050-47.3.06 10.4085/1062-6050-47.3.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valderrabano V., Hintermann B., Horisberger M., Fung T.S. (2006) Ligamentous posttraumatic ankle osteoarthritis. The American Journal of Sports Medicine 34, 612-620. https://doi.org/10.1177/0363546505281813 10.1177/0363546505281813 [DOI] [PubMed] [Google Scholar]
- Valderrabano V., Horisberger M., Russell I., Dougall H., Hintermann B. (2009) Etiology of ankle osteoarthritis. Clinical Orthopaedics and Related Research 467, 1800-1806. https://doi.org/10.1007/s11999-008-0543-6 10.1007/s11999-008-0543-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walankar P.P., Panhale V.P., Vyas K.M. (2021) Impact of kinesiophobia on physical function and quality of life in functional ankle instability individuals: An observational study. Bulletin of Faculty of Physical Therapy 26, 1-6. https://doi.org/10.1186/s43161-021-00032-0 10.1186/s43161-021-00032-0 [DOI] [Google Scholar]
- Watanabe K., Koshino Y., Kawahara D., Akimoto M., Mishina M., Nakagawa K., Ishida T., Kasahara S., Samukawa M., Tohyama H. (2023) Kinesiophobia, self-reported ankle function, and sex are associated with perceived ankle instability in college club sports athletes with chronic ankle instability. Physical Therapy in Sport 61, 45-50. https://doi.org/10.1016/j.ptsp.2023.02.008 10.1016/j.ptsp.2023.02.008 [DOI] [PubMed] [Google Scholar]
- Willems T., Witvrouw E., Verstuyft J., Vaes P., De Clercq D. (2002) Proprioception and muscle strength in subjects with a history of ankle sprains and chronic instability. Journal of Athletic Training 37, 487-493. [PMC free article] [PubMed] [Google Scholar]
- Wisthoff B., Matheny S., Struminger A., Gustavsen G., Glutting J., Swanik C., Kaminski T.W. (2019) Ankle strength deficits in a cohort of college athletes with chronic ankle instability. Journal of Sport Rehabilitation 28, 752-757. https://doi.org/10.1123/jsr.2018-0092 10.1123/jsr.2018-0092 [DOI] [PubMed] [Google Scholar]
- Wright C.J., Arnold B.L., Ross S.E., Linens S.W. (2014) Recalibration and validation of the Cumberland Ankle Instability Tool cutoff score for individuals with chronic ankle instability. Archives of Physical Medicine and Rehabilitation 95, 1853-1859. https://doi.org/10.1016/j.apmr.2014.04.017 10.1016/j.apmr.2014.04.017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


