Abstract
The authors report a case of perforated jejunal diverticulitis that was managed nonoperatively in a 60-year-old man. Nonoperative management of perforated jejunal diverticulitis is uncommon but possible, and necessitates close follow up to ensure complete resolution.
Keywords: Perforated jejunal diverticulitis, Nonoperative management, General surgery
Introduction
Jejunal diverticular disease is a rare condition, with a prevalence of only 0.06% to 1.3%, and complications such as diverticulitis, perforation and abscess formation being even rarer [1]. Most cases of perforated jejunal diverticulitis in the literature describe operative management with small bowel resection and anastomosis [2,3]. In this case report, we present a patient with perforated jejunal diverticulitis who was successfully managed with nonoperative management.
Case report
A 60-year-old man presented to the emergency department with a 3-day history of colicky abdominal pain. He reported associated constipation for the same duration but had been passing flatus. He also had nausea, vomiting and dizziness, but denied any recent fevers. His past medical history was significant for hypercholesterolaemia only, and he had no previous surgical history.
On arrival to the emergency department, he was normotensive, not tachycardic and afebrile. His abdomen was distended but soft, tender in the left flank, and had no signs of peritonism. The patient had raised inflammatory markers, with a white cell count of 17.7×109/L and a C-reactive protein of 94.9 mg/L, and normal renal function with a creatinine of 92 μmol/L and estimated GFR of 78.
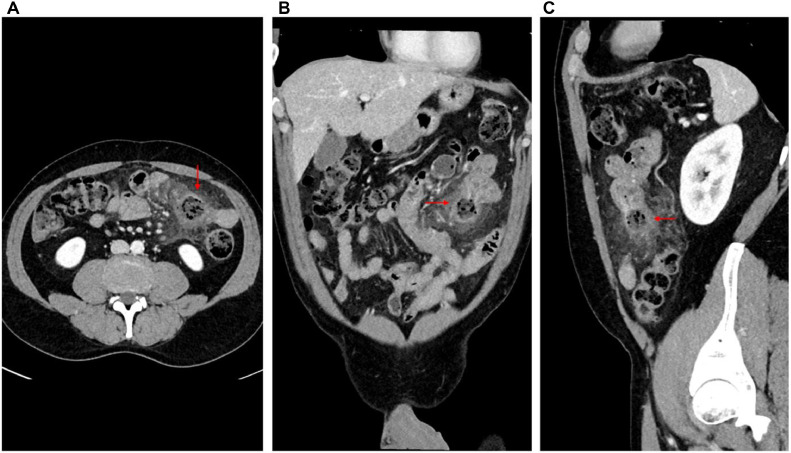
Computed tomography (CT) of the abdomen and pelvis (Fig. 1) showed a thickened loop of jejunum with marked inflammatory fat stranding in the left hemiabdomen with several diverticulae. A mural defect was seen with extraluminal protrusion of fecalised enteric contents into the adjacent mesentery. There were small locules of extraluminal gas around the defect but no free gas in the peritoneal cavity. Small volume of pelvic free fluid was also noted. The patient was promptly commenced on intravenous ceftriaxone 1 g daily and metronidazole 500 mg twice daily and kept nil by mouth. A nasogastric tube was inserted and left on free drainage. Given the patient had normal vital signs and no evidence of generalized peritonitis, it was decided to trial nonoperative management with close observation in hospital.
Fig. 1.
Imaging on initial presentation A. Axial view of perforated jejunal diverticulitis. B. Coronal view of perforated jejunal diverticulitis, with a mural defect and a protusion of faecalised enteric contents in adjacent mesentery. C. Sagittal view of perforated jejunal diverticulitis.
Over the next 24 hours, the patient's abdominal pain improved, bowels opened, and the inflammatory markers reduced (white cell count of 4.7 × 109/L and C-reactive protein of 25.6 mg/L). Hence, the patient continued to be managed nonoperatively with intravenous antibiotics and a slow upgrade in diet. He was discharged from hospital after 5 days with a course of oral amoxicillin and clavulanic acid.
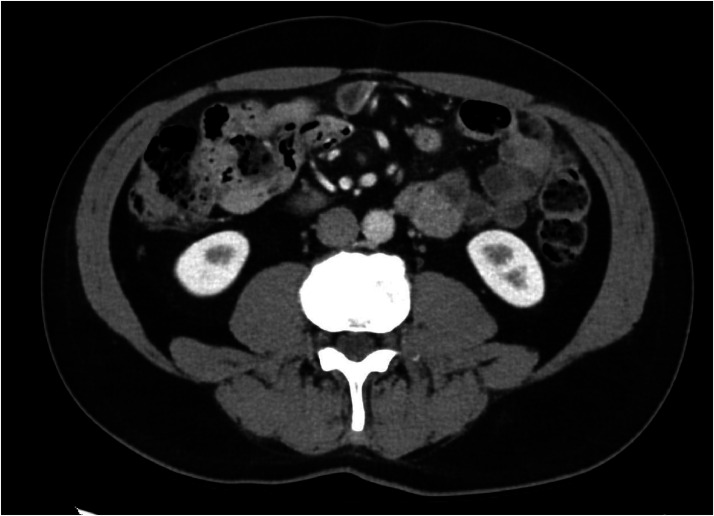
The patient represented 2 weeks later with a recurrence of their abdominal pain. However, he had no clinical evidence of sepsis or peritonitis, and inflammatory markers were unconcerning (white cell count of 9.2 × 109/L and C-reactive protein of 18.0 mg/L). A repeat CT of the abdomen and pelvis (Fig. 2) displayed a reduction in size of the localized perforation, measuring 5.6 × 5.5 mm, compared to 6.7 × 6.2 mm two weeks prior. There was a reduced degree of inflammatory fat stranding and less prominent mesenteric lymph nodes in the left upper quadrant of the abdomen. There was no new perforation seen, and the previous pelvic free fluid was no longer present. As a result, the patient was monitored for 24 hours in hospital and discharged home with analgesia.
Fig. 2.
2 weeks after initial CT-scan. Localised perforation of jejunum reduced in size, no new perforation seen.
The patient was followed up a month after their last presentation to hospital in the outpatient clinic. He reported absence of abdominal pain, tolerance of diet, and normal bowel motions. A CT of the abdomen and pelvis (Fig. 3) showed complete resolution of the perforated jejunal diverticulitis, with no evidence of small bowel thickening or fat stranding. The patient was subsequently discharged from the clinic.
Fig. 3.
6 weeks after the initial CT-scan. Resolution of previous perforated jejunal diverticulitis.
Discussion
Due to the rarity of jejunal diverticular disease, the natural history of the disease is not well known in comparison to colonic diverticular disease. Jejunal diverticular disease is usually asymptomatic, and clinical presentations are usually vague, with nonspecific symptoms such as intermittent abdominal pain, constipation, diarrhoa, and dyspepsia [1]. About 10%-30% of patients with jejunal diverticular disease present with complications such as perforation, intestinal obstruction and bleeding [2].
There is currently no consensus on management of perforated jejunal diverticular disease, especially regarding when nonoperative management may be a safe and effective alternative to operative management, or the duration of follow up that should be provided [3]. Case reports currently make up the bulk of the literature about this topic, and most case reports describe segmental small bowel resection and anastomosis as the primary treatment option for perforated jejunal diverticulitis [[4], [5], [6], [7]].
Our case is uncommon as the patient was successfully managed with nonoperative management, consisting of bowel rest and broad-spectrum intravenous antibiotics. Leigh et al compiled 23 cases of perforated jejunal diverticulitis from 2010 to 2019, of which only 3 cases were managed nonoperatively [2]. Likewise, Zafouri et al compiled 14 cases of perforated jejunal diverticulitis from 2015 to 2021, with only 2 cases (both of which were included in Leigh et al) that were managed nonoperatively [3].
Cases of perforated jejunal diverticulitis that have been initially managed nonoperatively usually had stable vital signs, localized peritonitis and a diagnosis of contained perforation confirmed with CT, as with our case [[8], [9], [10]]. However, there is a risk that such patients may fail nonoperative management. The same 2 cases in Leigh et al and Zafouri et al. eventually proceeded from nonoperative management to surgical resection within 2-6 days from initial presentation as their clinical condition worsened [11,12]. Our case report demonstrates clinical and radiological evidence of resolution of perforated jejunal diverticulitis 6 weeks after nonoperative management . Similarly, Levack et al. [10] described a case that was managed nonoperatively with resolution of inflammation on imaging 6 weeks later, which was the third case identified by Leigh that was initially managed nonoperatively. This should inform follow up plans after patients with perforated jejunal diverticulitis are managed nonoperatively.
Conclusion
Perforated jejunal diverticulitis is a rare cause of an acute abdomen. The most common treatment described in the literature is surgical resection, yet nonoperative management can be achieved in appropriately selected patients. Within the literature, our case represents the second case managed nonoperatively with complete resolution after 6 weeks. Patients that are managed nonoperatively are at risk of developing recurrence or worsening of their symptoms, as with our case, and may require operative management. Thus, we would advise close follow up (both inpatient and outpatient) of patients with perforated jejunal diverticulitis who are managed nonoperatively.
Patient consent
All patient data was anonymized and consent was obtained for scientific work and publication.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Kassir R, Boueil-Bourlier A, Baccot S, Abboud K, Dubois J, Adina Petcu C, et al. Jejuno-ilieal diverticulitis: etiopathogenicity, diagnosis and management. Int J Surg Case rep. 2015;10:151–153. doi: 10.1016/j.ijscr.2015.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leigh N, Sullivan B, Anteby R, Talbert S. Perforated jejunal diverticulitis: a rare but important differential in the acute abdomen. Surg Case Rep. 2020;6:162. doi: 10.1186/s40792-020-00929-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zafouri E, Ismail I, Sghaier M, Rebii S, Zoghlami A. Jejunal diverticulitis: a new case report and review of the literature. Int J Surg Case Rep. 2022;97:107395. doi: 10.1016/j.ijscr.2022.107395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sammartino F, Selvaggio I, Montalto G, Pasecinic C, Dhimolea S, Krizzuk D. Acute abdomen in a 91-year-old male due to perforated jejunal diverticulitis. Case Rep Gastroenterol. 2020;14(3):598–603. doi: 10.1159/000509529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mejri A, Arfaoui K, Hedfi M, Znaidi H. Perforated jejunal diverticulum as an unusual cause of acute abdomen: a case report. Int J Surg Case Rep. 2022;94:107130. doi: 10.1016/j.ijscr.2022.107130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martins B, Galletti R, Neto J, Mendes C. A case of perforated jejunal diverticulum: an unexpected cause of pneumoperitoneum in a patient presenting with an acute abdomen. Am J Case Rep. 2018;19:549–552. doi: 10.12659/AJCR.909131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saritas A, Topal U, Eray I, Dalci K, Akcami A, Erdogan K. Jejunal diverticulosis complicated with perforation: a rare acute abdomen etiology. Int J Surg Case Rep. 2019;63:101–103. doi: 10.1016/j.ijscr.2019.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jambulingam R, Nanayakkara G. Non-operatively managed case of contained jejunal diverticular perforation. BMJ Case Rep. 2019;12(7) doi: 10.1136/bcr-2018-228811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Colvin H, Kuenfoo C., Rajab T, Sayadatas T. Non-surgical management of recurrent perforation of a jejunal diverticulum following previous segmental bowel resection: a case report. J Med Case Reports. 2009;3:7318. doi: 10.4076/1752-1947-3-7318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levack M, Madariaga M, Kaafarani H. Non-operative successful management of a perforated small bowel diverticulum. World J Gastroenterol. 2014;20(48):18477–18479. doi: 10.3748/wjg.v20.i48.18477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tenreiro N, Moreira H, Silva S, Marques R, Monteiro A, Gaspar J, et al. Jejunoilieal diverticulosis, a rare cause of ileal perforation: case report. Ann Med Surg (Lond) 2016;6:56–59. doi: 10.1016/j.amsu.2016.01.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gurala D, Idiculla P, Patibandla P, Philipose J, Krzyzak M, Mukherjee I. Perforated jejunal diverticulitis. Case Rep Gastroenterol. 2019;13(3):521–525. doi: 10.1159/000503896. [DOI] [PMC free article] [PubMed] [Google Scholar]