Abstract
Objectives:
We aimed to evaluate the association between scores on each item of the SARC-F questionnaire and life expectancy in patients undergoing major surgery for urologic cancer.
Methods:
This retrospective study included 1018 patients undergoing elective major urologic cancer surgery. All patients completed the SARC-F questionnaire preoperatively. Demographic and clinical data were collected. The primary endpoint was an association between SARC-F scores and overall survival (OS).
Results:
Of the 1018 patients, the median age was 72 years and 920 (90%) were male. Multivariate analysis revealed four factors significantly and independently associated with shorter OS: assistance with walking score ≥1 (Hazard ratio: HR=2.18, P=0.044), cancer stages ≥ III (HR=7.98, P<0.001), high blood loss ≥78 ml or blood transfusion during surgery (HR=4.53, P=0.007 and HR=2.41, P=0.037, respectively).
Conclusions:
This study found that among the items of the SARC-F questionnaire, assistance with walking was a strong predictor of life expectancy. Incorporating such a simple screening tool into the preoperative assessment would help to ensure more appropriate perioperative care for urologic cancer patients.
Keywords: Geriatric syndrome, Questionnaire, Sarcopenia, Urologic cancer, Urologic surgery
Introduction
As the elderly age, there is a tendency for their physical and cognitive abilities to decline. These health conditions in the elderly are termed geriatric syndromes[1]. Sarcopenia is one of the most important manifestations of geriatric syndromes.
Sarcopenia is defined as a progressive loss of skeletal muscle and strength. The definition of sarcopenia by the European Working Group on Sarcopenia in Older People (EWGSOP) was updated in 2018. The EWGSOP recommends using the SARC-F questionnaire as a screening tool for sarcopenia[2]. The SARC-F questionnaire is a simple questionnaire for screening sarcopenia, representing strength, assistance with walking, rise from a chair, climb stairs, and falls[3]. In many domains, the SARC-F has been shown to be useful in predicting mortality and functional decline in the elderly; including community, emergency department, nursing home, and palliative care[3-7]. Several meta-analyses have also shown an association between SARC-F scores and mortality and functional decline[8,9].
In urologic cancer patients, sarcopenia is also associated with a higher incidence of treatment-related complications and poorer prognosis[10]. Screening for sarcopenia using the SARC-F may also be useful for patients undergoing surgery for urologic cancers, many of whom are elderly[11].
However, to our knowledge, there are only a limited number of reports examining the prognostic impact of each item in this questionnaire[5]. It is not clear which items of the SARC-F questionnaire critically correlate with prognosis in patients with malignant tumors.
In the present study, we investigated the association between scores on each item of the SARC-F questionnaire and life expectancy in patients undergoing major elective surgery for urologic cancer.
Materials and Μethods
Patient selection and study design
This retrospective cohort study comprises consecutive patients who underwent elective major urologic cancer surgery (radical cystectomy [RC], radical prostatectomy [RP], radical nephrectomy [RN], partial nephrectomy [PN], or radical nephroureterectomy [RNU]) at our department between October 2019, and January 2023. Out of a total of 1133 patients, we excluded 115 patients from the study because they did not complete the SARC-F questionnaire at the preoperative clinic. The reasons for not completing the questionnaire were patient age (<40 years, n=7) and conflicting hospital visit schedules (n=108). Therefore, we analysed 1018 patients in this retrospective study. We investigated how each item in the SARC-F questionnaire was related to postoperative life expectancy.
Data collection
As part of hospital protocol, all patients over 40 years of age who were scheduled for surgery completed SARC-F questionnaires. Trained nurses assessed the patients’ functional status by asking them questions about five SARC-F components. The components of the SARC-F were Strength, Assistance with walking, Rise from a chair, Climb stairs, and Falls, with a score of 0-2 for each component[3,12]. We also collected and analysed the following data retrospectively: sex, age, body mass index (BMI), Eastern Cooperative Oncology Group-performance status (ECOG-PS), Charlson comorbidity index (CCI), cancer stages (I–IV) based on the 8th edition of the tumour–node–metastasis (TNM) staging classification for urologic cancers[13], type of surgery (RC, RP, RN, PN, or RNU), surgical approaches (open, laparoscopic, or robot-assisted), operation time, estimated blood loss, whether or not blood transfusion was received, complications within 30 days after surgery according to the Clavien–Dindo classification (CDC), length of hospital stay, and the date of death. We collected these data from the hospital database or the patients’ medical records.
We dichotomised age, CCI, and ECOG-PS as <75 vs ≥75, <5 vs ≥5, and <2 vs ≥2 respectively based on previous studies[14-16]. We dichotomised other continuous variables as high and low at their median values.
Endpoint
The endpoint of this study was to assess the overall survival (OS) of patients who underwent elective cancer surgery and to explore how each item of the SARC-F questionnaire affected their survival rates. OS was defined as the time span from the date of the planned surgery to the date of death from any cause or to the most recent follow-up date.
Statistical analysis
We reported continuous variables as median and interquartile range (IQR), and categorical variables as counts and percentages. We used Kaplan-Meier curves and log-rank tests to compare OS across different levels of each of the five SARC-F items. We also conducted univariate and multivariate analyses using Cox proportional hazards models to identify clinical factors associated with OS (including the five SARC-F items), respectively. We used hazard ratio (HR) and 95% confidence interval (CI) to estimate the association between different factors and OS.
All P values <0.05 (two-sided) were considered statistically significant. Statistical analyses were performed using JMP 13 software (SAS Institute Inc, Cary, NC, USA) and R version 4.3.1 (R Foundation, Vienna, Austria).
Results
Demographics
Table 1 shows the demographics of 1018 patients. The median age was 72 years (IQR 67–77 years) and 920 patients (90%) were male. In total, 978 patients (96%) were diagnosed with stage I–III disease. The distribution of surgical procedures was as follows: 124 (12%) had RC, 612 (60%) had RP, 55 (5%) had RN, 140 (14%) had PN, and 87 (9%) had RNU. Among the array of surgical approaches, a majority of 812 patients (80%) underwent procedures employing robotic-assisted surgery. Complications categorized as CDC3 or higher were observed in 44 patients (4%).
Table 1.
clinical variables of 1018 patients who underwent major surgery for urological cancer.
| Variables | N (%) or median [IQR] |
|---|---|
| Total | 1018 |
| Age, year | 72 [67-77] |
| Male | 920 (90.4) |
| Body mass index, kg/m2 | 23.2 [21.3-25.1] |
| ECOG-PS; | |
| 0 | 863 (84.9) |
| 1 | 138 (13.6) |
| 2 | 16 (1.6) |
| Charlson comorbidity index | 0 [0-2] |
| Stage groups of cancer; | |
| ≤I | 238 (23.4) |
| II | 534 (52.5) |
| III | 206 (20.2) |
| IV | 40 (3.9) |
| SARC-F questionnaire; | |
| Strength ≥1 | 84 (8.3) |
| Assistance with walking ≥1 | 148 (14.5) |
| Rise from a chair ≥1 | 26 (2.6) |
| Climb stairs ≥1 | 105 (10.3) |
| Falls ≥1 | 83 (8.2) |
| Surgical form; | |
| Radical cystectomy | 124 (12.2) |
| Radical prostatectomy | 612 (60.1) |
| Radical nephrectomy | 55 (5.4) |
| Partial nephrectomy | 140 (13.8) |
| Radical nephroureterectomy | 87 (8.5) |
| Surgical approaches; | |
| Open | 131 (12.9) |
| Laparoscopic | 75 (7.4) |
| Robot-assisted | 812 (79.7) |
| Operative time, minutes | 169 [140-208] |
| Estimated blood loss, ml | 78 [28-203] |
| Blood transfusion | 36 (3.5) |
| Postoperative complications, highest; | |
| CDC ≤1 | 805 (79.0) |
| CDC 2 | 169 (16.6) |
| CDC 3 or more | 44 (4.3) |
| Length of hospital stay, day | 8 [7-10] |
CDC=Clavien-Dindo classification. ECOG-PS=Eastern Cooperative Oncology Group-performance status. IQR=Interquartile range. SARC-F=Simple questionnaire to rapidly diagnose sarcopenia.
Regarding the five SARC-F items, the results showed that 8% of the patients had difficulty with Strength, 14.5% needed Assistance with walking, 2.6% had trouble to Rise from a chair, 10.3% could not Climb stairs easily, and 8.3% had experienced Falls in the past year.
Relationship between SARC-F and OS
During the follow-up period (median 487 days, IQR 216–791 days), 30 mortality events were observed with a median time from surgery to mortality of 290 days (IQR 177–471 days). Of the 30 events, 20 occurred in patients who underwent RC with a median time from surgery to mortality of 284 days (IQR 179–495 days). No perioperative mortality event occurred within 30 days of surgery.
Table 2 shows the result of univariate and multivariate analysis for OS in 1018 patients. We found that four factors were significantly and independently associated with shorter OS: needing Assistance in walking (score ≥1) (HR=2.18, 95% CI=1.02–4.64, P=0.044), having advanced cancer stages (III or IV) (HR=7.98, 95% CI=3.52–18.10, P<0.001), and having high blood loss (≥78 ml) or blood transfusion during surgery (HR=4.53, 95% CI=1.52–13.50, P=0.007 and HR=2.41, 95% CI=1.06–5.53, P=0.037, respectively). On the other hand, patients who had RP had a significantly better OS than those who had other types of surgery (HR=0.03, 95% CI=0.01–0.22, P<0.001).
Table 2.
Univariate and multivariate analysis with Cox proportional hazards model for overall survival in 1018 patients undergoing major urologic cancer surgery.
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Age; ≥75 vs <75 years (ref) | 2.66 (1.28-5.52) | 0.009 | ||
| Sex; female vs male (ref) | 4.14 (1.89-9.07) | <0.001 | ||
| SARC-F questionnaire; | ||||
| Strength: ≥1 vs <1 (ref) | 3.07 (1.25-7.51) | 0.014 | ||
| Assistance with walking: ≥1 vs <1 (ref) | 5.01 (2.43-10.31) | <0.001 | 2.18 (1.02-4.64) | 0.044 |
| Rise from a chair: ≥1 vs <1 (ref) | 2.79 (0.66-11.71) | 0.161 | ||
| Climb stairs: ≥1 vs <1 (ref) | 4.42 (2.07-9.44) | <0.001 | ||
| Falls : ≥1 vs <1 (ref) | 1.81 (0.63-5.19) | 0.270 | ||
| Body mass index; low vs high (ref) | 1.04 (0.51-2.12) | 0.923 | ||
| ECOG-PS; ≥2 vs <2 (ref) | 8.91 (2.70-29.39) | <0.001 | ||
| Charlson comorbidity index; ≥5 vs <5 (ref) | 2.74 (0.37-20.13) | 0.322 | ||
| Cancer stage; ≥III vs <III (ref) | 9.60 (4.27-21.57) | <0.001 | 7.98 (3.52-18.10) | <0.001 |
| Surgical form; | ||||
| Radical cystectomy vs others (ref) | 14.59 (6.79-31.36) | <0.001 | ||
| Radical prostatectomy vs others (ref) | 0.02 (0.03-0.15) | <0.001 | 0.03 (0.01-0.22) | <0.001 |
| Radical nephrectomy vs others (ref) | 2.90 (1.01-8.31) | 0.048 | ||
| Partial nephrectomy vs others (ref) | 0.22 (0.03-1.63) | 0.139 | ||
| Radical nephroureterectomy vs others (ref) | 1.96 (0.68-5.62) | 0.213 | ||
| Surgical approaches; open vs others (ref) | 3.42 (1.63-7.20) | 0.001 | ||
| Operative time, minutes; ≥169 vs <169 (ref) | 5.88 (2.05-16.85) | <0.001 | ||
| Estimated blood loss, ml; ≥78 vs <78 (ref) | 5.68 (1.98-16.30) | 0.001 | 4.53 (1.52-13.50) | 0.007 |
| Blood transfusion; yes vs no (ref) | 13.28 (6.21-28.41) | <0.001 | 2.41 (1.06-5.53) | 0.037 |
CI=Confidence interval. ECOG-PS=Eastern Cooperative Oncology Group-performance status. HR=Hazard ratio. SARC-F=Simple questionnaire to rapidly diagnose sarcopenia.
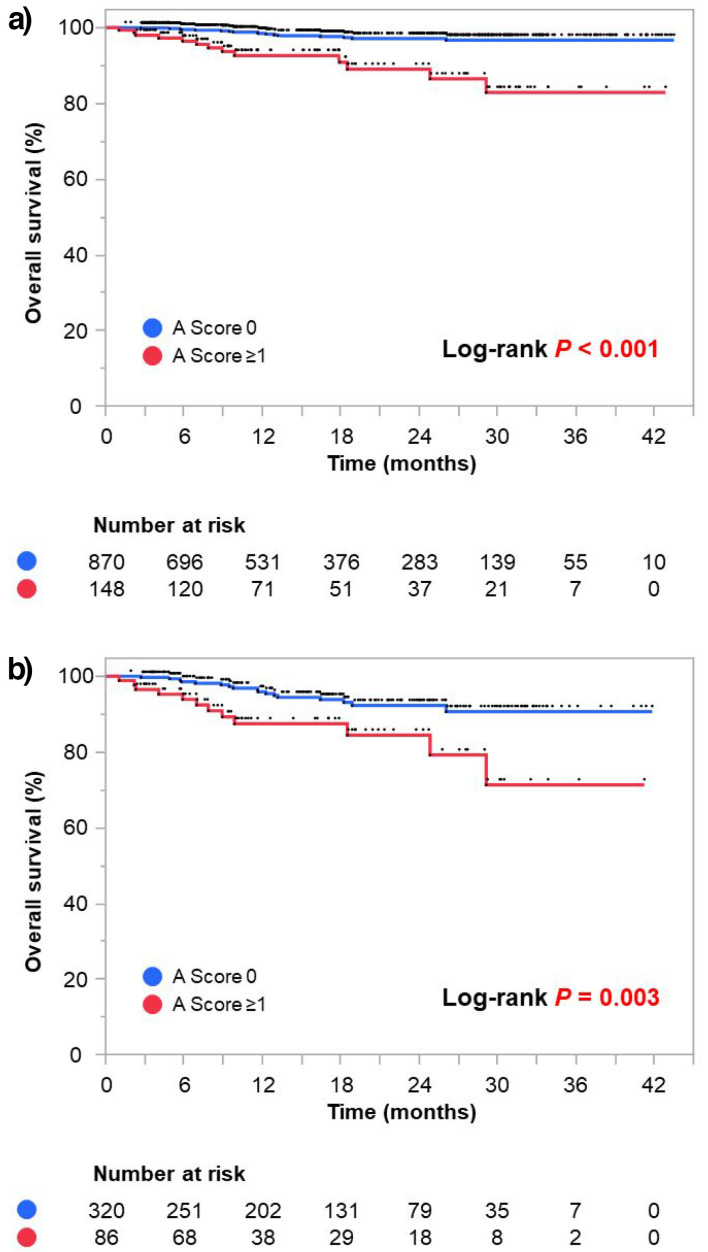
We plotted the Kaplan-Meier curves for “Assistance with walking” score of the SARC-F questionnaire, and compared the OS of patients with different scores. We found that patients who needed Assistance with walking (≥1 points) had shorter OS than those who did not (0 points) in the whole cohort (P<0.001, Figure 1-a) and in the 406 patients excluding those who underwent RP (P=0.003; Figure 1-b).
Figure 1.
Kaplan–Meier analyses demonstrating overall survival between Assistance with walking score ≥1 points vs 0 point in the entire cohort (a) and in a subgroup of 406 patients excluding those who underwent RP (b). RP= radical prostatectomy.
Discussion
In this study, we examined the relationship between the SARC-F questionnaire and the outcomes of patients who had major, elective surgery for urologic cancer. We found that the item “A” in the SARC-F score, which means “Assistance with walking,” was strongly linked to the life prognosis (HR=2.18, 95% CI=1.02-4.64, P=0.044) by multivariate analysis.
Previous studies have shown that sarcopenia significantly worsens the prognosis of patients who undergo radical surgery for bladder[10,17], prostate[18], kidney[19], and upper urinary tract cancer[20] in urology. Cross-sectional studies, which have already published from our cohort, have also suggested that a SARC-F score of 4 or higher may predict postoperative ambulation failure and poor prognosis in patients who underwent major urologic cancer surgery[21]. In this study of 1018 patients who had elective surgery for urologic cancer, all the SARC-F items, “S”, “A”, “R”, and “C”, were useful for stratifying the prognosis on the Kaplan-Meier curve. On the other hand, the study did not provide a detailed analysis of the association between the scores for each item of the questionnaire and OS.
In this study, item “A”, or “Assistance with walking”, was the only significant predictor of the outcome among all the SARC-F items in the multivariate analysis. Previous reports have shown that items “A” and “C” can predict death within 30 days in the emergency department[5]. Item “A” reflects walking, an activity directly related to ADLs, and might indicate the general condition more promptly. The fact that item “A” alone can predict certain outcomes may make it a simpler and more useful preoperative screening tool for the prognosis of patients with cancer. For example, in institutions which completing all the SARC-F questions is difficult, simply asking preoperatively whether the patient needs assistance with walking may identify patients at high risk for sarcopenia and allow for more appropriate and tailored perioperative care.
In the present study, item “F” was not associated with prognosis. This could be because the SARC-F score is based on self-reported answers, which may vary depending on how people perceive their own falls. For instance, a healthy young person who trips and falls may still report it as a “fall”, even though it was not a serious incident.
This study has several limitations. First, this single-center study may be biased due to its retrospective design, despite the relatively large number of patients included. Second, the median follow-up period of 487 days may be too short for a study with life expectancy as the primary endpoint. Moreover, the cohort consisted of various urologic cancers with different characteristics, which may have affected the validity of the prognostic analysis. Third, the study did not assess the factors required for the diagnosis of sarcopenia (e.g., grip strength and gait speed), nor the relationship between SARC-F screening and sarcopenia diagnosis, thus only evaluating the prognostic value of the screening test itself. Furthermore, the present study was a retrospective cohort study and we did not calculate the sample size in advance. Finally, the study did not examine the inter- and intra-observer reliability of SARC-F scoring, which may affect the reproducibility of SARC-F scores.
To conclude, we investigated the relationship between the SARC-F questionnaire items and the outcomes of patients who had elective surgery for urologic cancer. We found that item “A”, or “Assistance with walking”, was strongly related to life prognosis. Proper screening for cancer surgery may improve perioperative care.
Ethics approval
The National Cancer Center Institutional Review Board (2018-159) approved the study. The research related to human use has been complied with all the relevant national regulations, institutional policies and in accordance the tenets of the Helsinki Declaration.
Consent to participate
All included patients provided written informed consent for elective surgery and could opt-out of participating in the study.
Authors’ contributions
Kohei Hirose: Conception and drafting of the manuscript, Shugo Yajima: Supervision, drafting of the manuscript and editing, Ryo Andy Ogasawara: Review and editing, Naoki Imasato: Review and editing, Madoka Kataoka: Review and editing, Yasukazu Nakanishi: Review and editing, Hitoshi Masuda: Supervision, review and editing
Footnotes
Edited by: Yannis Dionyssiotis
References
- 1.Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes:clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55(5):780–91. doi: 10.1111/j.1532-5415.2007.01156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia:revised European consensus on definition and diagnosis. Age Ageing. 2019;48(4):601. doi: 10.1093/ageing/afz046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE. SARC-F:a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle. 2016;7(1):28–36. doi: 10.1002/jcsm.12048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chong E, Bao M, Goh EF, Lim WS. SARC-F at the Emergency Department:Diagnostic Performance for Frailty and Predictive Performance for Reattendances and Acute Hospitalizations. J Nutr Health Aging. 2021;25(9):1084–9. doi: 10.1007/s12603-021-1676-5. [DOI] [PubMed] [Google Scholar]
- 5.Ueshima J, Maeda K, Ishida Y, Shimizu A, Inoue T, Nonogaki T, et al. SARC-F Predicts Mortality Risk of Older Adults during Hospitalization. J Nutr Health Aging. 2021;25(7):914–20. doi: 10.1007/s12603-021-1647-x. [DOI] [PubMed] [Google Scholar]
- 6.Yang M, Jiang J, Zeng Y, Tang H. Sarcopenia for predicting mortality among elderly nursing home residents:SARC-F versus SARC-CalF. Medicine (Baltimore) 2019;98(7):e14546. doi: 10.1097/MD.0000000000014546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mori N, Maeda K, Fukami Y, Matsuyama R, Nonogaki T, Kato R, et al. High SARC-F score predicts poor survival of patients with cancer receiving palliative care. Support Care Cancer. 2022;30(5):4065–72. doi: 10.1007/s00520-022-06845-6. [DOI] [PubMed] [Google Scholar]
- 8.Ho KC, Gupta P, Fenwick EK, Man REK, Gan ATL, Lamoureux EL. Association between age-related sensory impairment with sarcopenia and its related components in older adults:a systematic review. J Cachexia Sarcopenia Muscle. 2022;13(2):811–23. doi: 10.1002/jcsm.12930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ida S, Kaneko R, Imataka K, Okubo K, Shirakura Y, Azuma K, et al. Verification of the predictive validity for mortality of the SARC-F questionnaire based on a meta-analysis. Aging Clin Exp Res. 2021;33(4):835–42. doi: 10.1007/s40520-020-01585-1. [DOI] [PubMed] [Google Scholar]
- 10.Fukushima H, Takemura K, Suzuki H, Koga F. Impact of Sarcopenia as a Prognostic Biomarker of Bladder Cancer. Int J Mol Sci. 2018;19(10) doi: 10.3390/ijms19102999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bahat G, Ozkok S, Kilic C, Karan MA. SARC-F Questionnaire Detects Frailty in Older Adults. J Nutr Health Aging. 2021;25(4):448–53. doi: 10.1007/s12603-020-1543-9. [DOI] [PubMed] [Google Scholar]
- 12.Soares JDP, Gomes TLN, Siqueira JM, Oliveira ICL, Mota JF, Laviano A, et al. Muscle function loss is associated with anxiety in patients with gastrointestinal cancer. Clin Nutr ESPEN. 2019;29:149–53. doi: 10.1016/j.clnesp.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 13.Paner GP, Stadler WM, Hansel DE, Montironi R, Lin DW, Amin MB. Updates in the Eighth Edition of the Tumor-Node-Metastasis Staging Classification for Urologic Cancers. Eur Urol. 2018;73(4):560–9. doi: 10.1016/j.eururo.2017.12.018. [DOI] [PubMed] [Google Scholar]
- 14.Mandel P, Chandrasekar T, Chun FK, Huland H, Tilki D. Radical prostatectomy in patients aged 75 years or older:review of the literature. Asian J Androl. 2017;21(1):32–6. doi: 10.4103/aja.aja_43_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mainardi LG, Borges TC, Gomes TLN, Pichard C, Laviano A, Pimentel GD. Association of SARC-F and dissociation of SARC-F +calf circumference with comorbidities in older hospitalized cancer patients. Exp Gerontol. 2021;148:111315. doi: 10.1016/j.exger.2021.111315. [DOI] [PubMed] [Google Scholar]
- 16.Hara T, Matsuyama H, Kamiryo Y, Hayashida S, Yamamoto N, Nasu T, et al. Use of preoperative performance status and hemoglobin concentration to predict overall survival for patients aged ≥75 years after radical cystectomy for treatment of bladder cancer. Int J Clin Oncol. 2016;21(1):139–47. doi: 10.1007/s10147-015-0857-9. [DOI] [PubMed] [Google Scholar]
- 17.Psutka SP, Carrasco A, Schmit GD, Moynagh MR, Boorjian SA, Frank I, et al. Sarcopenia in patients with bladder cancer undergoing radical cystectomy:impact on cancer-specific and all-cause mortality. Cancer. 2014;120(18):2910–8. doi: 10.1002/cncr.28798. [DOI] [PubMed] [Google Scholar]
- 18.Ohtaka A, Aoki H, Nagata M, Kanayama M, Shimizu F, Ide H, et al. Sarcopenia is a poor prognostic factor of castration-resistant prostate cancer treated with docetaxel therapy. Prostate Int. 2019;7(1):9–14. doi: 10.1016/j.prnil.2018.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Psutka SP, Boorjian SA, Moynagh MR, Schmit GD, Costello BA, Thompson RH, et al. Decreased Skeletal Muscle Mass is Associated with an Increased Risk of Mortality after Radical Nephrectomy for Localized Renal Cell Cancer. J Urol. 2016;195(2):270–6. doi: 10.1016/j.juro.2015.08.072. [DOI] [PubMed] [Google Scholar]
- 20.Fukushima H, Nakanishi Y, Kataoka M, Tobisu K, Koga F. Prognostic significance of sarcopenia in upper tract urothelial carcinoma patients treated with radical nephroureterectomy. Cancer Med. 2016;5(9):2213–20. doi: 10.1002/cam4.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yajima S, Fukushima H, Oda S, Yasujima R, Hirose K, Okubo N, et al. The significance of SARC-F scores in predicting postoperative outcomes of older adults undergoing elective major surgery for urologic cancer. Clin Nutr. 2023;42(9):1537–44. doi: 10.1016/j.clnu.2023.07.005. [DOI] [PubMed] [Google Scholar]