Abstract
Objectives:
The Benchmarking Exercise Programme for Older People (BEPOP) service improvement project seeks to determine and promote the exercise training characteristics associated with positive outcomes for resistance exercise for older people living with, or at risk of, sarcopenia or physical frailty.
Methods:
Mixed-methods service improvement project. Ten UK National Health Service physiotherapist-led therapy services delivering exercise interventions for older people submitted anonymized data for up to 20 consecutive patients. A multidisciplinary expert panel generated a report and recommendations with site-specific benchmarking data and feedback. In parallel, participating physiotherapy team members were interviewed to elicit feedback on BEPOP rationale, processes and perceived value.
Results:
Data from 188 patients were included, mean age 80 years (range 60-101). 115 (61%) received objective assessment of strength-based physical performance. Bodyweight exercises (173 [92%]) and resistance bands (49 [26%]) were the commonest exercise modalities. Exercises progressed predominantly through increased repetitions (163 [87%]) rather than increased load. 50 (30%) had no reassessment of outcomes; only 68 (41%) were signposted to follow-on exercise services. Staff interviews identified themes around knowledge, diagnosis, data collection and practice reflection.
Conclusion:
BEPOP was feasible to deliver and generated actionable insights for service improvement via improved diagnosis, measurement and progression of resistance exercise.
Keywords: Benchmarking, Older people, Quality improvement, Resistance exercise, Sarcopenia
Introduction
Sarcopenia (the loss of skeletal muscle strength and mass) and physical frailty (a ‘spiral of decline’ characterised by low muscle strength, low activity, weight loss and exhaustion) are key health conditions affecting older people[1,2]. Both are common, and both increase the risk of adverse health outcomes such as falls, hospital admission, longer length of hospital stay, loss of independence, an increased need for care, and earlier death[3-5]. Resistance exercise is established as an evidence-based, effective intervention for treating sarcopenia and physical frailty[6,7]. However, even when these conditions are diagnosed, older people often do not receive this effective treatment.
Survey work undertaken in 2018 by the British Geriatrics Society (BGS)[8] found that many services specialising in the care of older people do not make the diagnosis of sarcopenia, and such services provide exercise therapy for patients with sarcopenia or frailty in only half of cases. Further survey work[9] showed that even where exercise interventions are being offered, the content of these interventions varied significantly, with the majority focusing on falls prevention and balance training rather than on the resistance exercise known to provide the most benefit to people with sarcopenia and physical frailty. Even in those programmes focused on addressing sarcopenia and frailty, resistance training was offered in only two-thirds of programmes. Outcome measures were related in the most part to falls (e.g., balance assessment) rather than assessment of muscle strength. Effective resistance exercise training requires progressive overload of muscles to stimulate physiological adaptation (i.e. increases in strength and size). This in turn requires progressive increases in intensity of the weight or resistance used, with or without increases in the number of repetitions and sets (volume)[10]. Existing data highlight that current practice does not reflect the existing evidence base, demonstrating that there is a need to improve delivery and monitoring of exercise programmes for people living with sarcopenia or frailty.
Data comparing different services (benchmarking) has been a powerful driver for service improvement in other areas of clinical practice, such as hip fracture care[11,12], and can help build the business case for service development both locally and nationally. This approach, grounded in the real-world implementation of evidence, is arguably more likely to drive change in practice than conducting further large-scale clinical trials where sufficient evidence already exists as is the case for resistance exercise. Such an approach empowers individual sites to make changes to improve, to align their practice with current best practice, to learn from high-performing sites, and to adapt recommendations to their local needs, giving them ownership of the change process in a way that would not be the case if a uniform process was externally imposed across sites. The Benchmarking Exercise Programmes for Older People (BEPOP) project aims to develop and implement a UK-wide benchmarking and feedback service improvement system to determine and promote the exercise training characteristics most associated with positive outcomes for older people living with, or at risk of, sarcopenia or physical frailty. In this paper, we describe the design of BEPOP, present quantitative and qualitative data from wave one of BEPOP and summarise key recommendations for practitioners arising from this first wave of data collection.
Methods
Design of BEPOP
BEPOP was designed as a benchmarking and feedback service improvement project. The project was designed around the concept of a cycle of continuous quality improvement, involving: a) collection of data to describe current practice, b) feedback to participating centres on their current practice, benchmarked against other participating centres, c) recommendations to all centres to guide future evolution of their services. We envisaged that participating centres would then use this information to redesign their services before participating in future rounds of data collection. BEPOP planned to collect quantitative data from multiple participating physiotherapy teams in the UK, and based on these data, provide overall feedback of aggregate data from all sites, together with site-specific benchmarking and feedback to individual sites. An expert multidisciplinary panel provided recommendations based on interpretation of the results in the context of the current evidence base on exercise training for people living with sarcopenia or physical frailty. Interviews with staff were embedded within the project to understand the experiences of the physiotherapy teams participating in the project. It is important to note that we did not seek to impose a uniform protocol for exercise delivery or outcome measurement on sites; instead, BEPOP sought to describe existing practice and outcome measurement at participating sites.
Participating services – promotion and selection
Services across the UK providing community-based exercise interventions to older people at risk of sarcopenia or physical frailty were invited to participate in the project. BEPOP was promoted via AGILE (the professional network for physiotherapists working with older people recognised by the Chartered Society of Physiotherapy), through the BGS Special Interest Groups on Sarcopenia and Frailty Research and the Nursing/Allied Health Professionals BGS Council, through National Health Service (NHS) Health Education England, the British Association of Sports and Exercise Sciences (BASES) and through personal contacts and social media (Twitter/X and Facebook). Expressions of interest were reviewed by the BEPOP team. The main inclusion criterion was that services had to deliver exercise-based therapy for older people in outpatient or community settings. This criterion, whilst broad, enabled us to include services where a high proportion of service users were likely to have sarcopenia or physical frailty – groups known to benefit from resistance exercise training. The diagnoses of sarcopenia and physical frailty in clinical practice in the UK are often not made or written down before referral to therapy services and therapy services do not currently select patients on the basis of sarcopenia or physical frailty alone[8,9]. Confining selection to those patients who had already received a diagnosis of sarcopenia or frailty before referral to services would have excluded many patients who have these diagnoses and would benefit from resistance exercise, limiting the utility of the findings. We therefore took a pragmatic approach to service and patient inclusion to reflect the way that therapy services currently operate in the UK. Services based outside the UK National Health Service, inpatient and early supported discharge services, post-operative rehabilitation services, services specific to falls management (where a different type of exercise intervention based on lower limb strength and balance training is indicated)[13], and services offering disease-specific interventions (for example cardiac rehabilitation, post-stroke rehabilitation) were excluded as the goals of these services, measures of service success and types of exercise required may be very different from those required for sarcopenia or frailty. Services operating within the same NHS Trust as another participating service and which covered a similar population were also excluded, as were services where the information provided was insufficient to determine suitability to participate.
Governance
BEPOP was designed and delivered as a service improvement initiative, using anonymised data already collected by clinical teams through their usual practice, and did not impose a standard protocol, standard exercises, standardized outcomes measures or new data collection on sites.
Identification of individuals to include in data reporting
Each service was asked to identify and report data from twenty individuals, consecutively referred to their service. Data from patients could be included if they were aged 65 years or over, undergoing exercise intervention delivered in an outpatient/community-based setting. Data from patients were excluded if they were referred for a disease-specific intervention (for example pulmonary or cardiac rehabilitation); referred for rehabilitation or early supported discharge following a stroke diagnosis, or referred for rehabilitation post-operatively. No checks were performed with participating services to determine whether individuals included in the analysis were consecutive. Given the currently low rates of diagnosis of sarcopenia and the frequent co-existence of multiple reasons for referral to therapy services, we did not specify that individuals had to have received a diagnosis of sarcopenia or physical frailty to be included in data reporting.
Data collection
Participating services entered data into a RedCAP electronic data collection system[14] hosted on Newcastle upon Tyne Hospitals NHS Foundation Trust servers. No identifiable data were uploaded to the RedCAP system. Each data entry was assigned a unique identifier and the analysis team were unable to access patient names, dates of birth, addresses, or other identifying variables. Participating services were asked to upload initial descriptive information on each patient at the start of their assessment period, and then to complete data entry at the end of the period of physiotherapy. Data were collected on patient age and sex, baseline assessments including frailty status using the Rockwood Clinical Frailty Score where collected, means of assessing muscle strength and/or physical performance related to muscle strength, details of prescribed exercise intervention including modalities of exercise training, method of delivery, and planned duration of intervention. Information was also collected on how patients were reviewed and reassessed during and after the course of the prescribed exercise intervention, reasons for discontinuation, and whether patients were signposted to follow-on programmes after the end of their prescribed exercise intervention.
Statistical analysis
Data were checked and cleaned in Newcastle by the BEPOP analysis team before export from RedCAP as comma separated variable files. Simple descriptive analyses were generated with additional statistical analyses performed using SPSS version 25 (IBM, New York, USA). Waterfall plots were used to present comparative data between sites. Individual sites are not identified on these plots; the site number on each graph refers to the order of sites on the waterfall plot and does not identify the site. Given the wide range of different measures of muscle strength and physical performance reported, we converted changes in these measures to the percentage change between baseline and post-exercise measures ([end of exercise programme measure – start of exercise programme measure] * 100). For measures where a reduction in the measure denoted improvement (e.g. 5x sit to stand test, timed up and go test) the reciprocal of the measures were taken before calculating the percentage change. If an individual patient had data on more than one outcome measure related to strength, we used the outcome with the biggest percentage increase for that patient. Percentage changes for different outcomes were merged in the dataset and we explored associations between the best percentage improvement for each individual and different aspects of individual exercise programme characteristics using Mann-Whitney or Kruskal-Wallis tests.
Interview data collection and analysis
All physiotherapy team members involved in the project were invited to take part in a semi-structured interview. The aim was to explore and understand participating team member roles and experiences of being involved in BEPOP. Interviews were conducted by a member of the BEPOP core team experienced in qualitative interviewing (SA). Each participating team member gave verbal consent to be interviewed; interviews were all carried out remotely, via telephone or video conferencing. We used a flexible topic guide with prompts (see Supplementary Material) to encourage those being interviewed to tell us about why they agreed to take part in BEPOP, the training provided in data entry and project participation, their perceptions of what the project is trying to achieve, their overall experiences of collecting and entering data and the impact on their clinical work. All interviews were audio recorded, transcribed verbatim and checked for accuracy. Transcripts were organised using QSR NVivo 12. Based on Braun & Clarke’s six-phase framework[15], thematic analysis was used to identify important and interesting patterns across the data to derive themes.
Using Moran-Ellis et al’s ‘following a thread’ technique[16], the findings from the quantitative and interview components were integrated during analysis of the project data[17]. This involves analysing each data set separately to identify key themes or questions in one that may need further exploration by following them across to the other data set (i.e. following the thread). This in turn helps to create a more in-depth understanding of the question of interest.
Development of recommendations and feedback of results
Data from the quantitative and interview results were considered by a panel comprising physiotherapists with expertise in the care of older people (SDB, SA, CB), geriatricians including those with expert knowledge on sarcopenia (AAS, LC, MDW), and sport science and exercise physiologists (DAS, CH). This panel developed a series of recommendations based on current evidence with the aim of supporting services to address the issues highlighted by the results. A report of the results was distributed to all participating sites along with individualised, specific feedback highlighting how each site had performed relative to peer sites. A slide deck with overall results and a one-slide site-specific summary of results was shared with each site to facilitate discussion within services. The main findings and draft recommendations were presented at a Chartered Society of Physiotherapists event (The Complexity Summit, October 2022) and refined prior to finalisation of the report in response to discussion at this event. Main results were also disseminated via the British Geriatrics Society conference and via webinars with physiotherapy colleagues from across the UK. A training and learning webinar was hosted by AGILE in September 2023 to provide on-line training for physiotherapists from across the UK (not just those engaged in BEPOP) on how to deliver effective resistance exercise training, and for participating BEPOP sites to share how they had made use of the findings of wave 1 to start improving their local services.
Results
Fifty-two expressions of interest were received, of which 26 services were eligible to participate and were invited to take part. Of these, 12 progressed to obtaining local Caldicott Guardian approval. Two of these services did not submit any data, leaving ten services that contributed data to the first round of BEPOP. One service was in Scotland, one in Northern Ireland, one was on the Isle of Man, and the others were in England.
Quantitative data collection
Data on a total of 188 individuals were collected between 18th October 2021 and 27th September 2022, as detailed in Table 1. Most patients were referred for multiple reasons, with fewer than half (36%) referred explicitly for management of sarcopenia or physical frailty. Not all sites returned data on 20 consecutive patients, thus fewer than the requested 200 patient data sets were collected. Of 75 individuals with either a handgrip strength measure or five times sit to stand measure recorded, 65/75 (87%) met the current European Working Group definition[18] for probable sarcopenia.
Table 1.
Details of individuals included in BEPOP Wave 1 analysis.
| Mean age (years) (range) | 80 (60 to 101) | |
| Female sex (%) | 110 (59) | |
| Living in own home (%) | 155 (92) | |
| Reason for referral (%): | Falls prevention* | 150 (80) |
| Improve physical performance | 143 (76) | |
| Mobility assessment | 93 (50) | |
| Treat sarcopenia/frailty | 67 (36) | |
| Other | 5 (3) | |
| Mean Rockwood Clinical Frailty Scale (range) | 4.8 (1 to 7) | |
| Diagnosis of sarcopenia made before referral** (%) | 32 (17) | |
Not sole reason for referral, but falls were a frequent coexisting reason for referral.
Criteria by which diagnosis was made by referring teams were not interrogated.
Baseline assessments
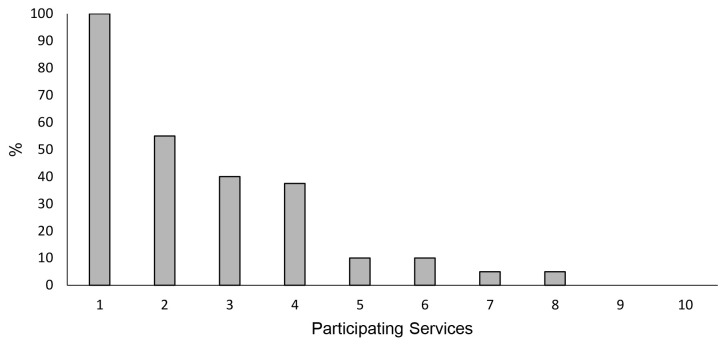
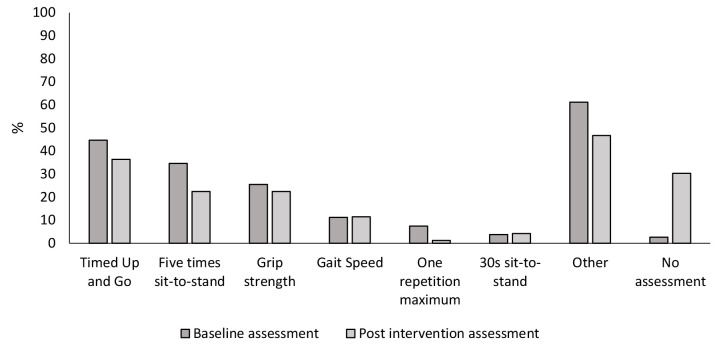
Figure 1 shows the percentage of individuals assessed at baseline using a range of different strength-based assessment methods. Timed up and go was included as an assessment which includes a strength-based component despite also being a test of mobility and balance. Many individuals were assessed using more than one method, with a high percentage of individuals undergoing non strength-based assessments (for example Tinetti score or Berg balance score, labelled as ‘other’), which reflects the large number of older people referred for broad-based exercise interventions who also had a history of falls. Overall, 115 (61%) individuals received at least one objective strength-based assessment of physical performance, such as grip strength, timed up and go (TUG) test, one-repetition maximum, five times sit-to-stand test, and 30-second sit-to-stand test. Supplementary Figure 1 demonstrates the percentage of individuals who received any assessment using an objective strength-based assessment method at baseline at each participating service.
Figure 1.
Baseline assessment methods reported in BEPOP wave 1.
Exercise Delivery
Table 2 shows the planned frequency and duration of prescribed exercise interventions. The majority of individuals were reviewed once a week with a quarter being reviewed less frequently. Self-directed practice made up the majority of sessions prescribed (n=1771, 64%). Of the 865 supervised sessions 476 (55%) were individual sessions; the others were group sessions. 49 (29%) of individuals did not complete the prescribed exercise intervention as planned with illness being cited as the most common reason (n=27, 55%). Figure 2 shows the modes of resistance exercise training prescribed across the cohort. Almost all services included some element of resistance exercise training in the prescribed exercise programmes (Supplementary Figure 2). Bodyweight resistance training exercises were the most common method of resistance training (n=173, 92%). For 82 (45%) of individuals this was the only modality of resistance exercise prescribed. 98 (52%) of individuals were prescribed an additional mode of resistance exercise, most commonly involving the use of resistance bands (n=49, 26%) or ankle/wrist weights (n=40, 21%).
Table 2.
Details of exercise session frequency, duration, and delivery route.
| Frequency of contacts (%) | Less than once a week | 48 (26) |
| Once a week | 120 (64) | |
| Twice a week | 16 (9) | |
| More than twice a week | 4 (2) | |
| Median planned duration of intervention (weeks) (range) | 8 (4 to 14) | |
| No. of supervised sessions delivered face to face (excl. self-directed practice) (%) | 865 (88) | |
| Median number of sessions delivered face to face per patient (range) | 4 (0 to 23) | |
| Number who discontinued prior to end of planned programme (%) | 49 (29) | |
Figure 2.
Modes of resistance exercise training reported in BEPOP wave 1.
Exercise Progression
Figure 3 shows methods used to progress resistance exercises. Most individuals had resistance exercise training progressed by an increase in volume (for example increased number of repetitions), with only 48 (26%) progressed via an increase in intensity, for example by an increase in weights used, stronger resistance band, or progression based on one-repetition maximum. Supplementary Figure 3 shows the differences between participating services in the percentage of individuals whose resistance exercises were progressed by intensity.
Figure 3.
Methods of progressing resistance exercise training reported in BEPOP wave 1.
Post-intervention assessment and outcomes
Post-exercise intervention assessment data were submitted for 165 (88%) of individuals as shown in Supplementary Figure 4. Across almost all methods of assessment, rates of assessment following an intervention were lower than at baseline and 50 individuals (30%) had no assessment following completion of the prescribed exercise programme. Rates of paired outcome assessment, using the same assessment method before and after an exercise intervention, varied across assessment methods, as demonstrated in Supplementary Figure 5. All individuals who performed the 30-second sit-to-stand test at baseline underwent the same test after completion of the prescribed exercise intervention but other baseline tests had lower rates of paired completion. We did not assess how many patients met the diagnostic criteria for sarcopenia at the end of their exercise programme.
Factors associated with greater improvement in strength and physical performance measures
Percentage change in strength and physical performance measures in relation to different aspects of exercise programme delivery are shown in Supplementary Table 1. Supplementary Figure 6 shows the association between the number of face-to-face sessions and the percentage change in strength-related measures. No significant association was seen between the number of face-to-face sessions and the percentage improvement in strength-related measures; (Spearmans rho 0.07, p=0.53); this remained non-significant in a sensitivity analysis when the 38 individuals who received no face-to-face input were excluded (Spearmans rho 0.16, p=0.19). No significant association was seen between the total number of supervised sessions (face to face, remote or telephone combined) and the percentage improvement in strength-related measures (Spearmans rho 0.05, p=0.69).
Referral and signposting to exercise services
A total of 68 (41%) individuals were signposted or referred on to further exercise services following completion of the prescribed exercise intervention. Supplementary Figure 7 shows how this metric varied between services.
Interview results
Seventeen physiotherapy team members from ten services participated in data collection for BEPOP. All were invited to take part in the interview process. Eight agreed to be interviewed from five different services, one declined due to lack of time, and eight did not respond. Six of the therapy team members were qualified physiotherapists and two were rehabilitation assistants (PT1-8 denoted under quotes). Six interviews were conducted via Microsoft Teams and two over the telephone. Mean duration of the interviews was 30 minutes (range 18 to 38 minutes).
Key Themes
Four overarching themes were developed from the interview data:
“Never quite knowing if we are doing the right thing”
“Are we diagnosing sarcopenia?”
“We collect a lot of that data anyway”, and
“It has made us think”
i) Never quite knowing if we are doing the right thing
Physiotherapy team members were willing to participate in BEPOP to find out more about their own practice and reflect on their service provision in comparison to others, as well as exercise guidelines:
“I thought it would be interesting to reflect on what I’m providing; you know what my service is doing and how that measures up to the guidance” (PT5)
The project also raised questions for some about their knowledge and skills in prescribing strength exercises for older people:
“I just don’t think it is something that we’re terribly good at as physios. Which is bizarre because exercise is supposed to be our thing. But we’re not very well trained in strength training” (PT2)
ii) Are we diagnosing sarcopenia?
Sarcopenia was rarely given as a reason for referral into the services. This raises the question as to whether it is being diagnosed formally, diagnosed but not recorded on referrals, or whether (like the therapists who were interviewed), clinicians just ‘think’ or ‘assume’ that older people have it based on clinical judgement and experience:
“Sarcopenia is never given as a diagnosis but I’m sure they have it” (PT4)
“There’s some people I’ve actually ticked that they’ve got sarcopenia… because I know they have… but that’s just because I know they have” (PT2)
iii) We collect a lot of that data anyway
The practicalities of being involved in and collecting data for BEPOP were not considered too onerous as the necessary information was already being collected routinely:
“it’s part of the stuff we do on a normal day-to day basis…the data we collect, we’re now collecting for BEPOP” (PT1)
However, some questions were perceived as not mapping easily to current practice:
“One thing that has been difficult to interpret onto the form is the frequency of sessions. There is no option for less than once a week” (PT5)
And whilst the importance of objective measures was acknowledged, it was suggested that what is matters to the patient may be equally important:
“…but it hasn’t picked up the kind of more subjective stuff. Although I’m putting in Berg’s and TUGTs, what’s making the difference to the patient is they can get out of a chair, they can get off the floor” (PT2)
iv) It has made us think
At the time of the interviews the project was not complete, but the participants were keen to hear the results. In some instances, being involved had already made some clinicians revise their approach to prescribing and progressing strength exercises for older people:
“… we prescribe an exercise programme and our assistants will do it. We haven’t particularly thought about how we’re going to progress people” (PT3)
“…it has highlighted the lack of strength training that we do. And I still think we still don’t always prescribe it. I think we’re a little too cautious” (PT5)
“Progressing resistance exercises is more in our minds than it was” (PT6)
Summary of key findings
Physiotherapists wanted guidance on best practice and recommendations for managing sarcopenia and physical frailty.
There was a need identified for physiotherapists who provide community-based exercise interventions for older people to assess and diagnose sarcopenia and physical frailty.
Physiotherapy teams acknowledged the need to ensure they are prescribing and progressing appropriate resistance exercises.
Discussion
We have shown that it is possible to develop and implement a UK-wide benchmarking and feedback programme which aims to improve the quality of resistance exercise training in services treating older people living with, or at risk of, sarcopenia or physical frailty. The programme was well received by participating sites, successfully collected data and delivered actionable insights which could be fed back to participating sites. Key issues highlighted as areas for improvement activities included a need to improve sarcopenia diagnosis, heterogeneity of outcome measures hindering comparisons across sites, low levels of repeat outcome measurement during and at the end of exercise programmes to evaluate progress, a lack of progression of intensity of resistance exercise during programmes and low levels of signposting to follow on programmes after the end of an exercise prescription. We have developed five key recommendations (shown in Box 1) for practice to address these issues. Nevertheless, the majority of patients reported on received some component of resistance exercise training and some progression of exercise, mostly through increased repetitions. Guidance on how to assess, prescribe and progress effective resistance exercise was identified as a key educational need.
Box 1.
Key Recommendations from Wave 1 of BEPOP benchmarking.
| 1. | Assessment: All older people referred for exercise programmes should be assessed using an objective strength-based assessment method, such as grip strength and/or chair stand test (five times or 30 second sit to stand), before starting an exercise programme. |
| 2. | Diagnosis: Probable sarcopenia can be diagnosed, as per European Working Group on Sarcopenia in Older People 2019 guidelines and diagnostic cut-offs, using objective strength-based assessment methods. This should be clearly documented and shared with the patient’s GP. |
| 3. | Exercise prescription: Progressive resistance exercise training, including use of resistance equipment, should be included in all exercise prescriptions for older people living with sarcopenia (probable or confirmed) and physical frailty. |
| 4. | Progress and Re-assess: Resistance exercises should be progressed by increasing intensity of exercises, not just by increasing the volume of exercises. At the end of an exercise programme, all older people should be re-assessed using the same objective strength-based assessment method that was used at baseline (paired outcome assessment), to assess progress, guide ongoing prescription and identify those that need onward signposting to community exercise services. |
| 5. | Take forwards: All older people completing an exercise programme should be offered education about the benefits of exercise, importance of continuation beyond discharge, signposting or referral onwards to ongoing exercise services where possible. |
To our knowledge, this is the first attempt to implement a national benchmarking and feedback programme specific to exercise training for sarcopenia or physical frailty. It is important to reiterate that we did not seek to impose a uniform exercise delivery protocol as part of this work. Similar benchmarking and feedback programmes have been successfully deployed in other areas of the care of older people, most notably for patients with hip fracture, but also patients in intermediate care facilities[19,20]. These programmes rely on data collection from a large number of participating sites, collation of data, and individualised feedback to participating sites to enable comparison with peers. Such approaches have been successful in driving up quality and improving outcomes. The participation of large number of sites has been key to the impact of such programmes, highlighting an imperative to expand BEPOP to more sites in subsequent waves of data collection.
Current evidence confirms that resistance exercise is an effective intervention for older people with sarcopenia or physical frailty[6,7]. Resistance exercise is a necessary component of any programme targeted towards people with sarcopenia or physical frailty[21], and the diagnosis of sarcopenia or physical frailty should therefore be a trigger to employ this exercise modality. One challenge in clinical practice is that the diagnosis of sarcopenia is infrequently made and thus practitioners may not be directed to prescribe resistance exercise[8]. For maximum benefit, resistance training may need to be performed at higher relative intensities, although lower intensities can also be beneficial, particularly in the early stages of exercise programmes. To ensure that resistance training programmes provide an appropriate overload stimulus throughout the duration of a training programme, the intensity, not just the volume (i.e. the number of repetitions) of exercise should be progressed[22]. Monitoring of individual resistance exercise training sessions, as well as monitoring recovery from exercise sessions, is necessary to inform effective exercise prescription through the manipulation of exercise intensity and volume to ensure progressive overload[10]. As well as this, regular re-assessment of the desired outcome (e.g., muscle strength) during and at the end of an exercise programme is needed to enable adaptation of the exercise prescription to meet goals and can also support patient motivation and engagement[23]. However, the potential usefulness of this is dependent on using an appropriate outcome measure to evaluate muscle strength or physical performance both at the start of the training programme and also as the programme progresses. It is clear that outcomes that measure strength or physical performance (rather than less relevant outcomes such as balance) are not always collected, hence the first of our five recommendations. Finally, as benefits of exercise are lost upon cessation, and most reviews suggest exercise programmes should be six-months or more in duration[24], signposting of patients to community-based exercise programme is essential as most physiotherapy teams cannot work with patients for this length of time. Yet, currently, only 41% were signposted on to other programmes.
Our initiative had several strengths. Use of a benchmarking and feedback process enables engagement of a wide range of sites, reflects usual clinical practice without excluding data from patients (which is often not the case for randomised controlled trials), and provides a robust methodology for rapid continuous learning and improvement. With this approach, individual sites have the flexibility to adapt changes to their local needs and constraints, taking into account local culture, service organisation and resources. Such approaches have been shown to be effective at driving up quality of healthcare services[25]. We included sites from across the UK with a wide range of geography and service types, and we sought data already recorded by physiotherapy teams to minimise burden to participating sites. Our study design enabled us to obtain interview data to complement the quantitative data obtained from sites and to triangulate these data sources for deeper insights than would have been the case from one source alone. In particular, the qualitative insights highlighted where physiotherapists felt they needed further training, highlighted areas for refinement of quantitative data collection in future waves and helped to confirm the perceived value of the programme within the physiotherapy community. The use of a transparent methodology and the development of a set of tools and processes should facilitate scale-up of this initiative to a larger number of UK sites.
Some limitations deserve comment, both with respect to the processes underpinning the initiative and also the data obtained. Comparisons across sites in benchmarking initiatives may be difficult to interpret; variation in outcomes between sites may reflect differences in casemix, differences in measurement or reporting, or differences in the remit of the service under study[26]. These issues undoubtedly complicate interpretation of our results and point to the need to further evolve data collection processes, taxonomies and definitions used in future waves of data collection. Some sites were reluctant to participate due to challenges navigating approvals and information governance despite the fact that this project was not classed as research, used fully anonymised data and that we sought to provide standard documentation and support to sites. Although participating sites were enthusiastic, we lack information on the reasons for non-participation by other sites or an understanding of what changes would be required to enable these other sites to engage with the programme; the results shown here apply to those sites participating in BEPOP but cannot be assumed to generalise to other sites. Although the focus of BEPOP is on resistance training for older people living with, or at risk of, sarcopenia and physical frailty, not every individual whose data were included had sarcopenia. Available measures suggest that the great majority did have sarcopenia, and even for those lacking measures to confirm this diagnosis, a majority of individuals were living with frailty as defined by the Rockwood Clinical Frailty Scale. Some participants had other conditions or comorbidities (e.g. falls) requiring therapy in addition to sarcopenia or frailty. This is to be expected as sarcopenia or frailty rarely occur in isolation, and although this makes interpretation of the results more difficult, it more accurately reflects what happens in real-world clinical services. Future larger waves of data collection may enable more detailed characterisation of individual exercise programmes at different sites.
The wide range of outcome measures used, and incomplete post-intervention measurement data, make it challenging to analyse which aspects of exercise programme delivery are associated with greater gains from exercise programmes, which in turn limits the scope of recommendations that can be made on how best to optimise practice. The heterogeneity of exercise programmes used by sites did not permit us to describe every combination of intensity, progression and volume for individual exercise programmes. Even if the outcomes data were more consistent, the observational nature of the data makes it difficult to draw causal inferences about the relationship between exercise programme characteristics and outcomes. Differences in the degree to which outcomes improved do not necessarily reflect differences in the effectiveness of different type of exercise progression but are more likely to reflect differences in the progress of the individuals concerned – those who are doing well are more likely to be given more repetitions or sets than those who are struggling to complete the starting level of exercise. It is however possible that the lack of association between the number of sessions and outcomes may simply reflect that exercise sessions were insufficiently challenging to deliver progression regardless of the number of sessions undertaken. Future, larger waves of data collection may be able to explore some of these issues further by stratifying by initial measures of physical performance or physical frailty.
Future iterations of BEPOP (or a similar benchmarking and feedback programme) should seek to expand the number of participating sites; this will improve our ability to examine what exercises, and what characteristics of these exercises, are most likely to deliver the best improvements in outcomes for patients. One of our key recommendations for site development is implementation of a minimum core outcome measurement dataset (for example handgrip strength, sit to stand test) which would greatly facilitate future data collection and analysis. Additional support for sites in obtaining data approvals and uploading data would also be desirable, as would national consensus on appropriate information governance requirements for similar projects. BEPOP has already led to the development of a nascent community of practice to exchange learning around the delivery of effective programmes of exercise for sarcopenia and physical frailty, and we anticipate that this will grow in importance and activity. Another area for future work is to better understand what components of the BEPOP process of benchmarking and feedback are most effective at driving quality improvement, possibly via embedded process evaluation work. Future rounds of data collection should also seek to capture what changes in policies and processes (for example sarcopenia diagnosis, patient selection, outcome measures, frequency, duration and progression of programmes) were made in response to feedback from this first round of data collection and feedback, and how participation in the programme is facilitating continuous quality improvement between rounds of data collection. Taken together, these changes should improve the ability of BEPOP or a future similar programme to maximise the translation of evidence on resistance exercise into effective clinical care for older people with sarcopenia or physical frailty.
Ethics approval
Following UK Health Research Authority (www.hra-decisiontools.org.uk) guidance, the project was not classed as research and did not require research ethics approval. Although no identifiable patient data were transferred outside participating Trusts, services were encouraged to obtain Caldicott approval for use of data and were supported to do so by sample documentation, project descriptions and lists of data points provided by the central BEPOP team.
Funding
This work was funded by a British Geriatrics Society specialist registrar start-up grant (SPR/03/2020) awarded to Dr Lorna Caulfield.
Acknowledgements
Dawn Skelton is a director of Later Life Training, a not for profit training provider, delivering training to exercise instructors and therapists in evidence-based delivery of strength training and falls prevention programmes. She is also the chair of the British Geriatrics Society rehabilitation group.
We thank the 10 sites who participated in this first wave of BEPOP.
Supplementary files
Supplementary Table 1.
Association between exercise programme characteristics and outcomes
| Characteristic | % improvement* (median, IQR) | P |
|---|---|---|
| Frequency face to face: | ||
| Less than once a week (n=11) | 33 [23 to 46] | - |
| At least once a week but less than twice a week (n=67) | 35 [18 to 60] | 0.71 |
| Twice a week or more (n=3) | 79 [30 to 89] | 0.77 |
| Completed exercise plan as scheduled (n=74) | 36 [20 to 73] | 0.11 |
| Discontinued before end of scheduled exercise plan (n=8) | 20 [0 to 51] | |
| Progression: | ||
| No progression of intensity or volume (n=2) | 13 [0 to 25] | - |
| Progression of number of repetitions (n=76) | 37 [20 to 70] | 0.03 |
| No progression of number of repetitions (n=6) | 12 [0 to 25] | |
| Progression of number of sets (n=27) | 47 [25 to 129] | 0.02 |
| No progression of number of sets (n=55) | 32 [16 to 55] | |
| Progression of duration of each session (n=30) | 33 [17-58] | 0.60 |
| No progression of duration of each session (n=52) | 36 [18 to 75] | |
| Any progression of volume (reps, sets or duration (n=79) | 35 [18-67] | 0.38 |
| No progression of volume (n=3) | 25 [13 to 36] | |
| Progression of intensity (n=25) | 36 [20 to 56] | 0.67 |
| No progression of intensity (n=57) | 34 [17 to 69] | |
best improvement from grip strength, gait speed, 5x sit to stand, 30s sit to stand or timed up and go. 5xSTS and TUG times converted to reciprocals before analysis.
Supplementary Figure 1.
Percentage of individuals undergoing any objective strength-based assessment method at baseline at each participating service.
Supplementary Figure 2.
Percentage of individuals by participating service whose exercise prescription included any method of resistance exercise.
Supplementary Figure 3.
Percentage of individuals whose resistance exercise prescription was progressed by intensity.
Supplementary Figure 4.
Percentage of individuals who received re-assessment following completion of exercise intervention by assessment method.
Supplementary Figure 5.
Percentage of individuals who had a paired outcome assessment (before and after intervention), using an objective strength-based assessment method.
Supplementary Figure 6.
Percentage improvement* vs total number of face-to-face therapy sessions. *best improvement from grip strength, gait speed, 5x sit to stand (5xSTS), 30s sit to stand or timed up and go (TUG). 5xSTS and TUG times converted to reciprocals before analysis. NB. Outlier (900% improvement) omitted from graph for clarity but included in correlation calculation.
Supplementary Figure 7.
Percentage of individuals signposted or referred on to further services after the end of exercise intervention.
Supplementary material
Process Evaluation: BEPOP Qualitative Interview Topic Guide
Aim: Qualitative interviews using semi-structured questions to aid research team to understand participants role and experience of being a participant in BEPOP
Target group: aim to capture feedback from participants:
a) working in different contexts e.g., delivering exercise for sarcopenia through different service models/care pathways and/or
b) working with different populations (e.g., at risk versus confirmed sarcopenic)
Introduction
Interviewer to introduce themselves and recap on the aims of the interview.
Explain what will happen during the interview.
Discuss confidentiality.
Ask the interviewee if they have any questions.
Professional experience
Can you tell me a little about your clinical/professional role and your role in BEPOP?
Experiences of BEPOP
-
How did you hear about BEPOP? What made you decide to participate?
- Explore what made them want to participate, if relevant.
- Was it what you expected?
-
What information/training were you given about BEPOP?
- Was it adequate?
- Is there anything that you think was missing from the information/training?
How would you describe BEPOP? What do you think the study is trying to achieve?
-
What was your experience of being a participant?
- What did it involve for you?
- What did being a participant of BEPOP mean to you? Tell us how it felt to participate?
-
What materials, investments, time etc were required of you to be a participant?
- How does BEPOP fit with your normal working methods for this patient group/your existing clinical pathways?
- Did your team meet the full set of inclusion criteria for involvement? If not, why apply? If not, why do you think you were selected?
What impact does recruiting and recording data for patients in the study have on the day to day running of your service?
-
What has helped you contribute to BEPOP? Has your participation gone according to plan?
- What problems did you encounter?
Can you tell me about the specific data that you were required to enter and how you go about doing it?
What is your understanding of the reasons why you were asked to enter that data requested through the REDCAP data collection system?
What might have made the data collection process more user friendly (or acceptable) to you/others responsible for entering the data e.g., more information; training on using REDCAP etc.
-
Can you tell me about the data entry targets/project aims?
- Did you/your team meet these? If not, why not?
Has your practice changed, or have you implemented anything new based on BEPOP since starting the study?
Was else might have been done to support you participating? What changes would you make for future participants which might support more participation?
Closing and thanks
Is there anything else you’d like to tell me about your experiences of BEPOP?
Conclude the discussion and thank the participant for their time and contribution.
Footnotes
Edited by: Yannis Dionyssiotis
Disclaimer
Prof. Dawn Skelton is co-Editor-in-Chief of the Journal of Frailty, Sarcopenia and Falls. The manuscript underwent peer review process by independent experts.
References
- 1.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–62. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393:2636–46. doi: 10.1016/S0140-6736(19)31138-9. [DOI] [PubMed] [Google Scholar]
- 3.Liu P, Hao Q, Hai S, Wang H, Cao L, Dong B. Sarcopenia as a predictor of all-cause mortality among community-dwelling older people:A systematic review and meta-analysis. Maturitas. 2017;103:16–22. doi: 10.1016/j.maturitas.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 4.Yeung SSY, Reijnierse EM, Pham VK, Trappenburg MC, Lim WK, Meskers CGM, et al. Sarcopenia and its association with falls and fractures in older adults:A systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2019;10:485–500. doi: 10.1002/jcsm.12411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults:evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–56. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 6.Moore SA, Hrisos N, Errington L, Rochester L, Rodgers H, Witham M, et al. Exercise as a treatment for sarcopenia:an umbrella review of systematic review evidence. Physiotherapy. 2020;107:189–201. doi: 10.1016/j.physio.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Apostolo J, Cooke R, Bobrowicz-Campos E, Santana S, Marcucci M, Cano A, et al. Effectiveness of interventions to prevent pre-frailty and frailty progression in older adults:a systematic review. JBI Database System Rev Implement Rep. 2018;16:140–232. doi: 10.11124/JBISRIR-2017-003382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Offord NJ, Clegg A, Turner G, Dodds RM, Sayer AA, Witham MD. Current practice in the diagnosis and management of sarcopenia and frailty - results from a UK-wide survey. J Frailty Sarcopenia Falls. 2019;4:71–7. doi: 10.22540/JFSF-04-071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Witham MD, Chawner M, De Biase S, Offord N, Todd O, Clegg A, et al. Content of exercise programmes targeting older people with sarcopenia or frailty - findings from a UK survey. J Frailty Sarcopenia Falls. 2020;5:17–23. doi: 10.22540/JFSF-05-017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hurst C, Robinson SM, Witham MD, Dodds RM, Granic A, Buckland C, et al. Resistance exercise as a treatment for sarcopenia:prescription and delivery. Age Ageing. 2022;51:afac003. doi: 10.1093/ageing/afac003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johansen A, Boulton C, Hertz K, Ellis M, Burgon V, Rai S, et al. The National Hip Fracture Database (NHFD) - Using a national clinical audit to raise standards of nursing care. Int J Orthop Trauma Nurs. 2017;26:3–6. doi: 10.1016/j.ijotn.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 12.Goubar A, Ayis S, Beaupre L, Cameron ID, Milton-Cole R, Gregson CL, et al. The impact of the frequency, duration and type of physiotherapy on discharge after hip fracture surgery:a secondary analysis of UK national linked audit data. Osteoporos Int. 2022;33:839–50. doi: 10.1007/s00198-021-06195-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Montero-Odasso M, van der Velde N, Martin FC, Petrovic M, Tan MP, Ryg J, et al. World guidelines for falls prevention and management for older adults:a global initiative. Age Ageing. 2022;51:afac205. doi: 10.1093/ageing/afac205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris PT, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Informatics. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 16.Moran-Ellis J, Alexander VD, Cronin A, Dickinson M, Fielding J, Sleney J, et al. Triangulation and Integration:processes, claims and implications. Qual Res. 2006;6:45–59. [Google Scholar]
- 17.O'Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ. 2010;341:c4587. doi: 10.1136/bmj.c4587. [DOI] [PubMed] [Google Scholar]
- 18.Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia:revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31. doi: 10.1093/ageing/afy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Royal College of Physicians of London. National Hip Fracture Database. 2023. [[accessed 21st August 2023]]. Available from: https://www.nhfd.co.uk/20/hipfractureR.nsf/
- 20.NHS Benchmarking Network. National Audit of Intermediate Care. 2023. [[accessed 21st August 2023]]. Available from: https://www.nhsbenchmarking.nhs.uk/naic .
- 21.Fragala MS, Cadore EL, Dorgo S, Izquierdo M, Kraemer WJ, Peterson MD, et al. Resistance Training for Older Adults:Position Statement From the National Strength and Conditioning Association. J Strength Cond Res. 2019;33:2019–52. doi: 10.1519/JSC.0000000000003230. [DOI] [PubMed] [Google Scholar]
- 22.Hurst C, Sayer AA. Improving muscle strength and physical function in older people living with sarcopenia and physical frailty:Not all exercise is created equal. J R Coll Physicians Edinb. 2022;52:166–71. doi: 10.1177/14782715221104859. [DOI] [PubMed] [Google Scholar]
- 23.Collado-Mateo D, Lavin-Perez AM, Penacoba C, Del Coso J, Leyton-Román M, Luque-Casado A, et al. Key Factors Associated with Adherence to Physical Exercise in Patients with Chronic Diseases and Older Adults:An Umbrella Review. Int J Environ Res Public Health. 2021;18:2023. doi: 10.3390/ijerph18042023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Silva RB, Aldoradin-Cabeza H, Eslick GD, Phu S, Duque G. The Effect of Physical Exercise on Frail Older Persons:A Systematic Review. J Frailty Aging. 2017;6:91–6. doi: 10.14283/jfa.2017.7. [DOI] [PubMed] [Google Scholar]
- 25.Willmington C, Belardi P, Murante AM, Vainieri M. The contribution of benchmarking to quality improvement in healthcare. A systematic literature review. BMC Health Serv Res. 2022;22:139. doi: 10.1186/s12913-022-07467-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lovaglio PG. Benchmarking strategies for measuring the quality of healthcare:problems and prospects. Sci World J. 2012;2012:606154. doi: 10.1100/2012/606154. [DOI] [PMC free article] [PubMed] [Google Scholar]