Abstract
Non-tuberculous mycobacterial infection (NTM) is rare in healthy children, with lymphadenitis being the most common presentation. Immunocompromised populations are known to be at high risk, but the clinical picture of NTM infection in pediatric hematology/oncology patients is unclear. In this nationwide retrospective analysis of patients under the age of 40 treated in Japanese pediatric hematology/oncology departments who developed NTM infection between January 2010 and December 2020, 36 patients were identified: 21 patients with hematopoietic stem cell transplantation (HSCT) and 15 non-transplant patients. Post-transplant patients were infected with NTM at 24 sites, including the lungs (N=12), skin and soft tissues (N=6), bloodstream (N=4), and others (N=2). Nine of 12 patients with pulmonary NTM infection had a history of pulmonary graft-versus-host disease (GvHD), and rapid-growing mycobacteria (RGM) were isolated from 5 of them. In non-transplant patients, the primary diseases were acute lymphoblastic leukemia (ALL; N=5), inborn errors of immunity (IEI; N=6), and others (N=4). All cases of ALL had bloodstream infections with RGM, whereas all cases of IEI were infected with slow-growing mycobacteria (SGM). In summary, 3 typical clinical scenarios for pediatric hematology/oncology patients have been established: RGM-induced pulmonary disease in patients with pulmonary GvHD, RGM bloodstream infection in patients with ALL, and SGM infection in patients with IEI. Our findings suggest that NTM must be regarded as a pathogen for infections in these high-risk patients, especially those with pulmonary GvHD, who may require active screening for NTM.
Introduction
Non-tuberculous mycobacteria (NTM) were first identified in the 1950s as human pathogenic acid-fast bacilli1 and now involve up to 200 species, excluding M. tuberculosis complex and M. leprae. They are classified according to their growth rate in solid agar into two major groups: rapid-growing mycobacteria (RGM) and slow-growing my-cobacteria (SGM).1,2
According to recent studies from various regions, the incidence and prevalence of NTM pulmonary infection (the most common form of NTM infection) in the general population are estimated to be 18-45 per 100,000 person-years and 15-57 per 100,000 people, respectively.3-6 Epidemiological data show that NTM infection has been increasing worldwide in recent years,7,8 and in some countries, including Japan, the infection rate of NTM has surpassed that of tuberculosis.4,9 The high-risk groups for NTM infection include the elderly, patients with cystic fibrosis (CF), and immunocompromised individuals due to various factors such as human immunodeficiency virus infection, inborn errors of immunity (IEI), chemotherapy, and post-organ transplantation.7
Non-tuberculous mycobacterial infections are extremely rare in children, with an incidence of 0.6-2.2 per 100,000 person-years in the general pediatric population, with the majority occurring <5 years of age and involving lymph nodes.10,11 However, even among children, patients with IEI can develop disseminated NTM infections involving multiple sites such as the lung, bloodstream, and skin/soft tissue, and patients with CF are at high risk for pulmonary NTM infection.12-14 In addition, a variety of NTM infections in pediatric hematology/oncology patients with theoretical defects in immunity have been reported.15-19 However, previous reports have only focused on specific NTM infection sites or species, and there have been no nationwide single-cohort studies that provide a comprehensive view of NTM infection in pediatric hematology/oncology patients.17,20-22 Thus, there is little evidence that differences in underlying diseases, treatments, and complications could influence the nature of NTM infections in this entity.
To assess the overall clinical features of NTM infection in pediatric hematology/oncology patients, this retrospective multicenter study was conducted involving 121 pediatric hematology/oncology institutions in Japan, and the NTM incidence in pediatric hematology/oncology patients was estimated using data from the Japanese public registries.
Methods
Patients
In this study, patients <40 years of age with hematologic diseases, malignancies, and IEI who developed NTM infection between January 2010 and December 2020 were studied retrospectively. Patients already diagnosed with NTM infection at the start of the study, or those with relapse or reinfection, were excluded. A questionnaire was sent to 121 pediatric hematology/oncology institutions throughout Japan asking about their experience with NTM-infected patients (Online Supplementary Figure S1). Of these 121 institutions, 22 provided clinical data on 36 patients with NTM, while the remaining 99 institutions had no patients diagnosed with NTM during the study period. Details of the questionnaire are provided in the Online Supplementary Methods. This study was approved by the Ethics Committee of the Nagoya University Graduate School of Medicine. An opt-out consent process was approved by disseminating the research information; thus, the requirement of informed consent was waived.
Non-tuberculous mycobacteria diagnosis, classification, and treatment
Specimens for microbiological testing were collected at the discretion of each institution. In this study, pulmonary NTM infections were diagnosed using the latest American Thoracic Society/Infectious Diseases Society of America criteria and were cross-checked according to a previous study.17,23,24 In addition, extrapulmonary NTM infections were defined as one or more positive culture or polymerase chain reaction results indicating active infection from normally sterile sites (muscle, joints, bone marrow, and blood, including the central venous line). Disseminated lesions were defined as evidence of NTM infection at >2 different sites. We defined the date of treatment completion as the date of the last dose of medication after one year had passed without NTM relapse.
Non-tuberculous mycobacteria isolation and identification
Detailed information on NTM cultured, isolated, and identified from clinical specimens at each institution was collected using the aforementioned questionnaire (Online Supplementary Methods).
Statistical analysis
A two-sided Fisher’s exact test was used to compare categorical variables. The probabilities of event-free survival and overall survival (OS) were calculated using the Kaplan-Meier method, and the log-rank test was used to compare the 2 groups. The probabilities of treatment completion for NTM were estimated using cumulative incidence methods, and the Gray test was used to compare the 2 groups. The treatment completion for NTM infection was defined as the event of interest with death from any cause as a competing event. P<0.05 was considered statistically significant. Details of other statistical methods and software libraries used for analysis and plotting are described in the Online Supplementary Methods.
Estimation of incidence of non-tuberculous mycobacterial infection
The Japanese Society of Pediatric Hematology/Oncology (JSPHO) patient registry (https://www.jspho.org/disease_record_en.html) and the Japanese Data Center for Hematopoietic Cell Transplantation (JDCHCT) registry25 are both Japanese nationwide registries of children with hematology/oncology disorders and HSCT recipients, respectively. Using the number of patients enrolled in these registries from 2015-2019 as the denominator, the incidence of NTM infections was estimated in children and adolescents (aged 0-19 years) with malignancies (N=16) or receiving allogeneic HSCT (N=17) during the same period (2015-2019) in the current study.
Results
Patients’ characteristics
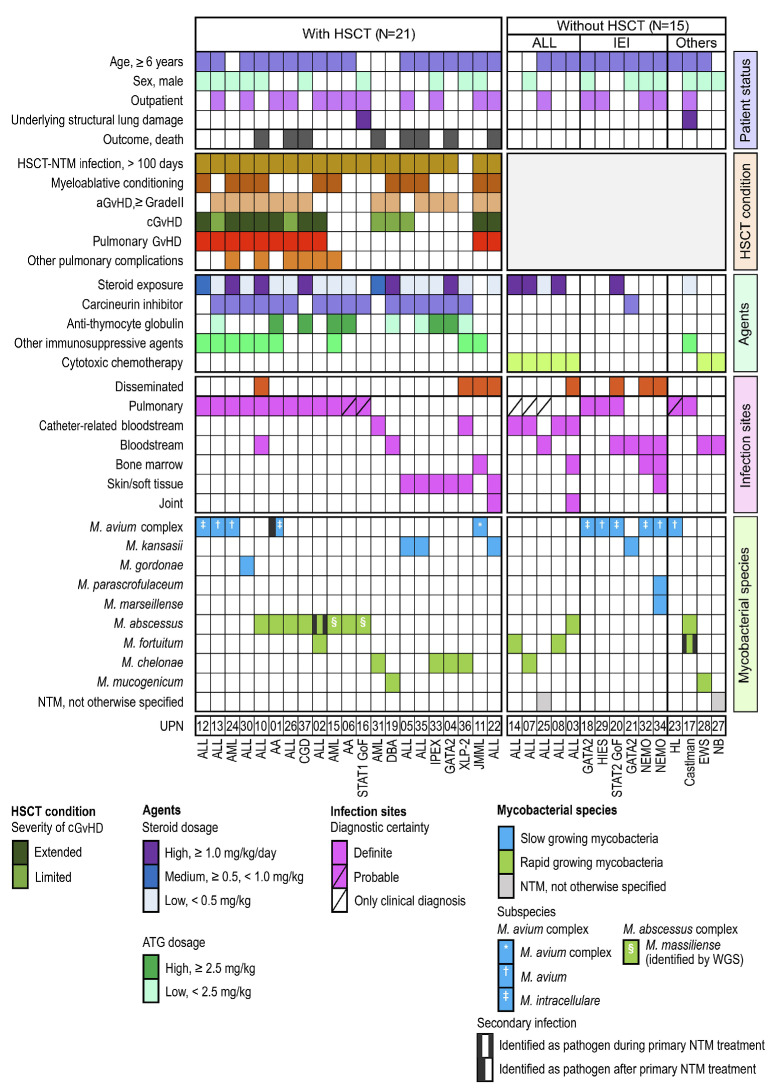
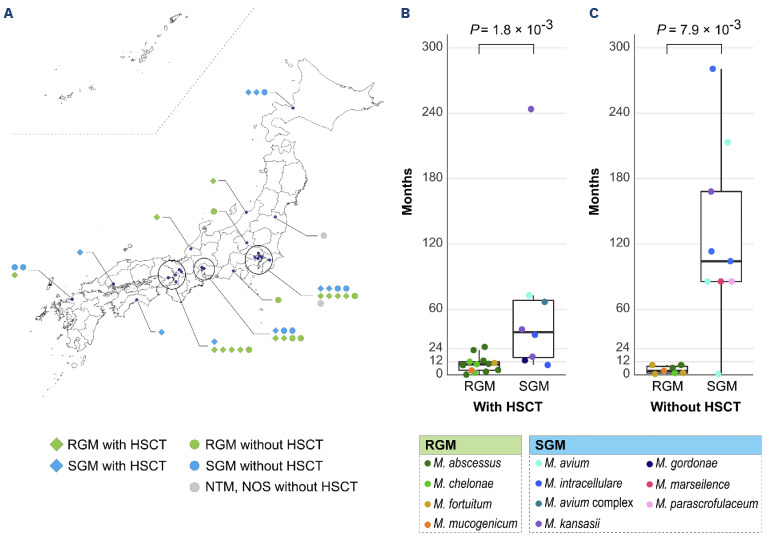
From January 2010 to December 2020, 36 child, adolescent, and young adult patients (18 males and 18 females) with hematologic malignancies, extracranial solid tumors, benign hematologic disorders, or IEI, and developing NTM infection were identified from 22 institutes throughout Japan (Figures 1 and 2A, Online Supplementary Figure 2A, B). Patients’ characteristics are summarized in Table 1. The underlying diseases were hematologic malignancies (N=19), benign hematologic disorders (N=4), solid tumors (N=2), and IEI (N=11), with 21 patients (58%) receiving HSCT. Median age of the entire cohort at the time of NTM infection diagnosis was 13 years (range 3-24 years).
Non-tuberculous mycobacterial infections in pediatric hematology/oncology patients
The NTM species were identified in 34 of 36 pediatric hematology/oncology patients with NTM infections. At the time of diagnosis, one patient had multiple NTM species, and 3 others had other infections of different NTM species during the initial NTM infection treatment course. In total, 39 NTM strains isolated from 34 patients were species-identified, with 18 SGM and 21 RGM (Figure 1, Online Supplementary Figure S3). Notably, M. avium complex (MAC) was the most frequently isolated species from the SGM-infected cases (11 strains: 5 strains of M. avium, 5 strains of M. intracellulare, and one strain that could not be identified further than MAC), followed by M. kansasii (4 strains), and M. gordonae, M. parascrofulaceum, and M. marseillense (one strain each). M. abscessus complex was the most frequently isolated species from the RGM-infected cases (10 strains), followed by M. chelonae (5 strains), M. fortuitum (4 strains), and M. mucogenicum (2 strains). In terms of infection sites, 28 patients had single-site infections: definite pulmonary (N=12), probable pulmonary (N=3), skin and soft tissue (N=4), catheter-related bloodstream infection (CRBSI; N=4), and other bloodstream infections (N=5). Eight patients had disseminated infections (Figure 1).
Characteristics of non-tuberculous mycobacterial infections in patients receiving hematopoietic stem cell transplantation
In this cohort, there were 21 patients with NTM infection who underwent HSCT regardless of the underlying disease (Figure 1, Online Supplementary Table S1). There were 24 infection sites, including the lungs (N=12), skin and soft tissues (N=6), bloodstream (N=4), bone marrow (N=1), and joint (N=1). The infection was localized in 17 cases and disseminated in 4. Furthermore, 14 patients had Grade II-IV acute graft-versus-host disease (GvHD), 14 had chronic GvHD, and 11 had pulmonary GvHD. All patients received immunosuppressive agents, with 19 receiving steroids. Rapid-growing mycobacteria (RGM) strains (M. abscessus [N=8], M. chelonae [N= 4], M. mucogenicum [N=1], and M. fortutium [N=1]) were isolated from 13 patients, slow-growing mycobacteria (SGM) strains (MAC [N=5], M. kansasi [N=3], and M. gordonae [N=1]) from 9 patients, and both RGM (M. abscessus) and SGM (MAC) from one patient. Among 12 patients with pulmonary infection, M. abscessus was isolated from 8 patients and MAC from 4 patients. In contrast, among 6 patients with skin and soft tissue infections, M. chelonae was isolated from 3 patients and M. kansasii from 3 patients (Figure 1). Regarding the duration from transplantation to the onset of NTM infection, RGM infections occurred significantly earlier than SGM infections (10.1 months vs. 39.5 months, P=0.0018) (Figure 2B).
Characteristics of non-tuberculous mycobacterial infections in patients who had not received hematopoietic stem cell transplantation in the past
In the current cohort, 15 patients with no prior HSCT had an NTM infection. The underlying diseases were acute lymphoblastic leukemia (ALL; N=5), IEI (N=6), and others (Hodgkin’s lymphoma, Castleman disease, Ewing sarcoma, and neuroblastoma in one case each) (Figure 1). All patients with ALL had bloodstream RGM infections (4 of which were catheter-related), while all patients with IEI had SGM, with MAC being isolated from 5 of them. The diagnoses of the 6 patients with IEI were all classified into disease subtypes with known mycobacterial susceptibility (GATA2 deficiency [N=2], NEMO deficiency [N=2], hyper immunoglobulin E syndrome [N=1], and STAT1 gain-of-function [N=1]).26,27 RGM infections occurred significantly earlier than SGM infections (3 .7 vs. 104 months, P=0.0079) (Figure 2C).
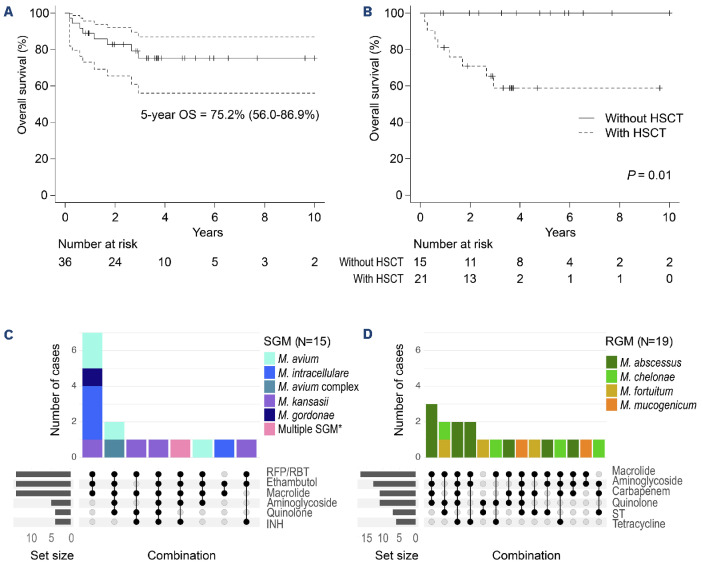
Treatment outcomes
In our pediatric hematology/oncology patient cohort, there were no instances in which NTM infection was the primary cause of death. The 5-year OS for the entire cohort was 75% (95% confidence interval [CI]: 56-87), with transplant-related complications (N=7) and primary disease progression (N=1) being the leading causes of death (Figure 3A). The 5-year OS for the 21 NTM-infected patients with prior HSCT was 59% (95% CI: 34-77), whereas no deaths were observed in the 15 patients without prior HSCT during the observation period (Figure 3B).
The 3-year cumulative incidence of treatment completion was 81% (95% CI: 62-91), with a median duration of treatment completion of 1.5 years (95% CI: 0.9-2.4) (Online Supplementary Figure S4A). While the median duration of treatment completion was longer with SGM (1.9 years) than with RGM (0.9 years), there was no significant difference in 3-year treatment completion rates between SGM (74%, 95% CI: 44-89) and RGM (66%, 95% CI: 22-89) (Online Supplementary Figure S4B). Similarly, cumulative treatment completion rates did not differ significantly, regardless of HSCT history or infection sites (Online Supplementary Figure S4C, D).
Antibiotic combinations used to treat non-tuberculous mycobacterial infection
In the entire cohort, 32 of 36 patients (89%) with NTM infection were treated with >3 antibiotics (Online Supplementary Figure S5). The drug combinations for the top 6 most frequently used antibiotics in SGM and RGM are presented in Figure 3C and D, respectively, for each NTM species. In addition, detailed combination patterns for all antibiotics are shown in Online Supplementary Figure S5B and C. In cases of SGM infection, 12 of 15 cases were treated with regimens that included rifampicin/rifabutin, ethambutol, and macrolides (Figure 3C). However, macrolide-based regimens of >3 antimycobacterial agents were administered in 16 of 19 RGM-infected patients and in all 10 cases of M. abscessus infection (Figure 3D).
Figure 1.
Clinical characteristics of 36 patients diagnosed with non-tuberculous mycobacterial infection in Japanese pediatric hematology/oncology institutions. Each column represents one patient. AA: aplastic anemia; aGvHD: acute graft-versus-host disease; ALL: acute lymphoblastic leukemia; AML: acute myelogenous leukemia; CGD: chronic granulomatous disease; cGvHD: chronic graft-versus-host disease; DBA: Diamond-Blackfan anemia; EWS: Ewing sarcoma; HIES: hyper-IgE syndrome; HL: Hodgkin lymphoma; HSCT: hematopoietic stem cell transplantation; IEI: inborn errors of immunity; IPEX syndrome: immunodysregulation polyendocrinopathy enteropathy X-linked syndrome; JMML: juvenile myelomonocytic leukemia; NBL: neuroblastoma; NTM: non-tuberculous mycobacterium; STAT1 GoF: STAT 1 gain-of-function mutation; STAT2 GoF: STAT 2 gain-of-function mutation; UPN: unique patient number; WGS: whole genome sequencing; XLP2: X-linked lymphoproliferative disease 2.
Figure 2.
Geographic distribution and duration from primary disease diagnosis to non-tuberculous mycobacterial infection in Japanese pediatric hematology/oncology patients. (A) Blue dots represent the locations of the 22 facilities where patients with non-tuberculous mycobacterial (NTM) infections were identified. Black circles indicate the three Japanese megalopolis areas (Tokyo, Nagoya, and Osaka/Kyoto). (B) Box plots depict the time from hematopoietic stem cell transplantation to the onset of NTM infection in transplant cases. (C) Box plots depict the time from primary disease diagnosis to NTM onset in non-transplant cases. HSCT: hematopoietic stem cell transplantation; NOS: not otherwise specified; RGM: rapid-growing mycobacteria; SGM: slow-growing mycobacteria.
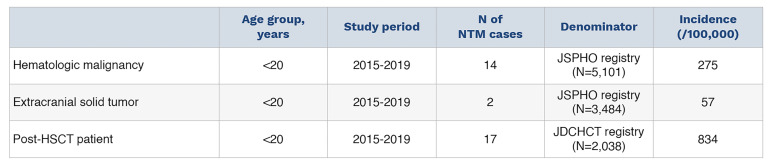
Estimated incidence of non-tuberculous mycobacterial infection in children with hematologic malignancies and extracranial solid tumors
From 2015 to 2019, the JSPHO registry enrolled 5,101 children and adolescents (aged 0-19 years) with hematologic malignancies (ALL [N=2,333], acute myeloid leukemia [N=770], and other hematologic malignancies [N=1,998]) and extracranial solid tumors (N=3,484). At the same time, our nationwide retrospective cohort included 14 pediatric patients with hematologic malignancies and 2 with extra-cranial solid tumors (Table 2). Based on these data, the incidences of NTM infection in children with hematologic malignancies and extracranial solid tumors were calculated to be 0.27% and 0.06%, respectively.
Estimated incidence of post-hematopoietic stem cell transplantation non-tuberculous mycobacterial infection in children
From 2015 to 2019, the JDCHCT registry enrolled 2,038 children (aged 0-19 years). At the same time, our nationwide retrospective cohort included 17 children with post-HSCT NTM infection (Table 2). Based on these data, the incidence of NTM infection in pediatric recipients of HSCT was calculated to be 0.83% (Table 2).
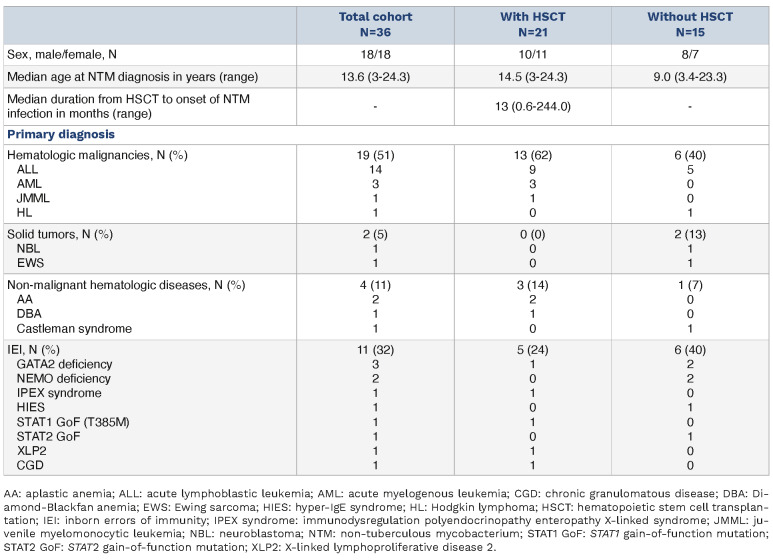
Table 1.
Patients’ characteristics.
Discussion
In this current nationwide retrospective study, NTM infection was identified in 36 child, adolescent, and young adult patients with hematologic malignancies, extracranial solid tumors, benign hematologic disorders, or IEI. To the best of our knowledge, previous reports of NTM infections in pediatric hematology/oncology patients have been limited to literature reviews of small case series or single-center reports, with no cross-sectional analyses of a single cohort.17,20-22 While lymphadenitis with MAC is the canonical form of NTM infection in immunocompetent children, the current pediatric hematology/oncology cohort demonstrated a characteristic clinical picture, with a variety of SGM and RGM species infecting various sites.10,11 This cohort has revealed several clinical scenarios of NTM infections in this particular group of patients.
Our NTM cohort of 21 post-HSCT patients, which included 13 RGM and 8 SGM infections, revealed a skewed incidence in the early post-HSCT phase for RGM and late post-HSCT phase for SGM (Figure 2B). Previous studies on HSCT adult recipients demonstrated that the incidence of NTM infection after transplantation ranged from 0.4% to 4.9%, with a median onset time ranging from 251 to 343 days.28 This is roughly consistent with the incidence and median onset time of NTM infection in our pediatric cohort of 0.83% and 390 days, respectively, indicating that NTM infection should be noted even in children after transplantation. Furthermore, we have demonstrated for the first time that, to the best of our knowledge, the susceptible timing of infection differs between RGM and SGM, providing new insight into the infectious timeline after HSCT.29
Although pulmonary NTM was uncommon in healthy children, it was the most common form in our post-HSCT cohort. In this cohort, M. abscessus was the predominant pathogen, followed by MAC, accounting for 86% of all isolated species. These two species are also predominant in NTM infections of patients with CF,30 suggesting the presence of a common mechanism of NTM susceptibility in post-HSCT and CF cohorts. In fact, 9 of 12 post-HSCT patients (75%) with pulmonary NTM infection developed pulmonary GvHD. Because of the allogeneic immune response in pulmonary GvHD and recurrent infections in CF, the airways are exposed to persistent inflammation, resulting in pulmonary organization and bronchiectasis. To evaluate the incidence of NTM infection in patients with pulmonary GvHD, we estimated the number of patients with pulmonary GvHD based on the number of transplants obtained from the Transplant Registry Unified Management Program (TRUMP) registry and previous epidemiological data.31-33 Using this as the denominator, the incidence of pulmonary NTM infection was calculated to be at least 5% in patients with pulmonary GvHD, comparable to the incidence in patients with CF, suggesting the need for aggressive NTM screening in patients with pulmonary GvHD.13,34
Figure 3.
Clinical outcomes and the pattern of combinations of the top 6 chemotherapeutic agents used in the treatment of non-tuberculous mycobacterial infections in pediatric hematology/oncology patients. (A) Kaplan-Meier estimates of the overall survival (OS) rate in pediatric hematology/oncology patients with non-tuberculous mycobacterial (NTM) infection. The 5-year OS rate for all patients was 75.2% (95% confidence interval [CI]: 56-87) in the entire cohort. (B) Patients receiving hematopoietic stem cell transplantation (HSCT) had a 10-year OS rate of 59% (95% CI: 34-77, P=0.012 by log-rank test), whereas those who did not had no deaths from NTM infection. (C and D) Top 6 major antibiotic combinations used to treat NTM infection are summarized by UpSet plots. Panels depict drug combinations used to treat slow-growing mycobacteria (SGM; N=15) and rapid-growing mycobacteria (RGM; N=19), respectively. Each colored bar represents a different NTM species. Color codes are displayed in the right-hand column of each panel. INH: isoniazid; RBT: rifabutin; RFP: rifampicin; ST: sulfamethoxazole-trimethoprim. *M. avium, M. parascrofulaceum, and M. marseillense.
Table 2.
Estimated incidence of non-tuberculous mycobacterium infection.
In the non-HSCT group, our findings in patients with ALL and IEI were consistent with patterns reported in previous literature. Catheter- or non-catheter-related bloodstream infections associated with RGM have been reported sporadically in patients with ALL, while other forms of infection have been reported anecdotally.20,22 RGM is known for its ability to form biofilms and for its high compatibility with artificial materials, both of which predispose to catheter infection.35 In our cohort of 5 NTM-infected patients with ALL, all 4 patients with an identified species also had CRBSI due to RGM. In contrast, NTM infection in immunocompromised individuals has been previously studied in human immunodeficiency virus-infected adults and children with Mendelian susceptibility to mycobacterial disease, where MAC is predominantly isolated and infection patterns vary, including disseminated and pulmonary infections.12,36,37 Although our cohort of IEI with NTM infection did not include classical Mendelian susceptibility to mycobacterial disease, disease subtypes in all 6 patients with IEI were reported to be susceptible to NTM.26,27,38,39 SGM was isolated from all 6 cases of IEI, 5 of which were MAC. Dissemination was observed in 3 cases and pulmonary disease in 2. Thus, we established that CRBSI caused by RGM is a representative form of patients with ALL, and that MAC-induced pulmonary disease and dissemination are the most common in IEI.
This study has some limitations due to the scarcity of prior research and its retrospective nature. First, there were no epidemiological data in the Japanese general pediatric population to serve as a reference point for specifying high-risk groups for NTM infections. Therefore, the estimated prevalence of NTM infection in Japanese children was calculated using a regional claim database and found to be equal to or lower than that of other countries (Online Supplementary Table S2).10,40 Second, the incidence of NTM infection might be underestimated due to potential incomplete enrollment and undiagnosed cases at the institutions. Third, diagnostic methods and identification of NTM subspecies were based on institutional diagnosis and were not standardized. Finally, detailed subspecies-specific statistical analysis was insufficient because of the small number of cases involving rare infections in a rare population. However, single-cohort studies in the pediatric hematology/oncology field that provide an overview of NTM infection are scarce, and our study is one of the largest ever. In addition, even if a potential underestimation is considered, our estimated high NTM incidence is still remarkable.
In conclusion, the current study identified high-risk groups of NTM infections in patients with pediatric hematology/ oncology diseases and provided representative clinical pictures in each group. These findings may justify aggressive NTM screening in high-risk groups, which may improve diagnostic rates and reveal a more accurate clinical picture of NTM infections in pediatric hematology/oncology patients in the future.
Supplementary Material
Acknowledgments
The authors would like to thank all of the patients and families who provided data for this study, as well as the staff of the participating institutions. A complete list of participating institutions has been provided in Online Supplementary Appendix 1. The authors are grateful to the investigators at all 20 centers for their assistance in providing patient data. These investigators are listed in Online Supplementary Appendix 2. The authors are grateful to Ms. Hiroko Ono and Ms. Chie Amahori for their valuable assistance. The authors would like to thank Enago (www.enago.jp) for the English language review.
Funding Statement
Funding: This work was supported by a grant (JP22fk0108608, to YH) from the Japan Agency for Medical Research and Development (AMED).
Data-sharing statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.Timpe A, Runyon EH. The relationship of atypical acid-fast bacteria to human disease; a preliminary report. J Lab Clin Med. 1954;44(2):202-209. [PubMed] [Google Scholar]
- 2.Armstrong DT, Parrish N. Current updates on mycobacterial taxonomy, 2018 to 2019. J Clin Microbiol. 2021;59(7):e0152820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim JY, Kwak N, Yim JJ. The rise in prevalence and related costs of nontuberculous mycobacterial diseases in South Korea, 2010-2021. Open Forum Infect Dis. 2022;9(12):ofac649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Namkoong H, Kurashima A, Morimoto K. Epidemiology of pulmonary nontuberculous mycobacterial disease, Japan. Emerg Infect Dis. 2016;22(6):1116-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin C, Russell C, Soll B. Increasing prevalence of nontuberculous mycobacteria in respiratory specimens from US-affiliated pacific island jurisdictions. Emerg Infect Dis. 2018;24(3):485-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blakney RA, Ricotta EE, Frankland TB. Incidence of nontuberculous mycobacterial pulmonary infection, by ethnic group, Hawaii, USA, 2005-2019. Emerg Infect Dis. 2022;28(8):1543-1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ratnatunga CN, Lutzky VP, Kupz A. The rise of non-tuberculosis mycobacterial lung disease. Front Immunol. 2020;11:303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prevots DR, Marras TK. Epidemiology of human pulmonary infection with nontuberculous mycobacteria: a review. Clin Chest Med. 2015;36(1):13-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brode SK, Daley CL, Marras TK. The epidemiologic relationship between tuberculosis and non-tuberculous mycobacterial disease: a systematic review. Int J Tuberc Lung Dis. 2014;18(11):1370-1377. [DOI] [PubMed] [Google Scholar]
- 10.Zimmermann P, Curtis N, Tebruegge M. Nontuberculous mycobacterial disease in childhood-update on diagnostic approaches and treatment. J Infect. 2017;74(Suppl 1):S136-S142. [DOI] [PubMed] [Google Scholar]
- 11.Ford TJ, Silcock RA, Holland SM. Overview of nontuberculous mycobacterial disease in children. J Paediatr Child Health. 2021;57(1):15-18. [DOI] [PubMed] [Google Scholar]
- 12.Lee WI, Huang JL, Yeh KW. Immune defects in active mycobacterial diseases in patients with primary immunodeficiency diseases (PIDs). J Formos Med Assoc. 2011;110(12):750-758. [DOI] [PubMed] [Google Scholar]
- 13.Floto RA, Olivier KN, Saiman L. US Cystic Fibrosis Foundation and European Cystic Fibrosis Society consensus recommendations for the management of non-tuberculous mycobacteria in individuals with cystic fibrosis. Thorax. 2016;71;(Suppl 1):i1-i22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lamb GS, Starke JR. Mycobacterium abscessus infections in children: a review of current literature. J Pediatric Infect Dis Soc. 2018;7(3):e131-e144. [DOI] [PubMed] [Google Scholar]
- 15.Suryanarayan K, Campbell J, Eskenazi AE. Nontuberculous mycobacterial infections in pediatric acute leukemia. J Pediatr Hematol Oncol. 2002;24(7):558-560. [DOI] [PubMed] [Google Scholar]
- 16.Nicholson O, Feja K, LaRussa P. Nontuberculous mycobacterial infections in pediatric hematopoietic stem cell transplant recipients: case report and review of the literature. Pediatr Infect Dis J. 2006;25(3):263-267. [DOI] [PubMed] [Google Scholar]
- 17.Unal E, Yen C, Saiman L. A low incidence of nontuberculous mycobacterial infections in pediatric hematopoietic stem cell transplantation recipients. Biol Blood Marrow Transplant. 2006;12(11):1188-1197. [DOI] [PubMed] [Google Scholar]
- 18.Takemori-Sakai Y, Iwata Y, Oe H, Sakai Y, Wada T. Bloodstream infection caused by Mycobacterium chelonae. Pediatr Int. 2018;60(6):599-600. [DOI] [PubMed] [Google Scholar]
- 19.Chan WY, Ho PL, To KK. A child with acute myeloid leukemia complicated by calcaneal osteomyelitis due to Mycobacterium abscessus infection after induction chemotherapy successfully salvaged with bedaquiline and clofazimine. Int J Infect Dis. 2021;103:9-12. [DOI] [PubMed] [Google Scholar]
- 20.Apiwattankul N, Flynn PM, Hayden RT, Adderson EE. Infections caused by rapidly growing Mycobacteria spp in children and adolescents with cancer. J Pediatric Infect Dis Soc. 2015;4(2):104-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Redelman-Sidi G, Sepkowitz KA. Rapidly growing mycobacteria infection in patients with cancer. Clin Infect Dis. 2010;51(4):422-434. [DOI] [PubMed] [Google Scholar]
- 22.Arlotta A, Cefalo MG, Maurizi P, Ruggiero A, Dodi I, Riccardi R. Critical pulmonary infection due to nontuberculous mycobacterium in pediatric leukemia: report of a difficult diagnosis and review of pediatric series. J Pediatr Hematol Oncol. 2014;36(1):66-70. [DOI] [PubMed] [Google Scholar]
- 23.Gaviria JM, Garcia PJ, Garrido SM, Corey L, Boeckh M. Nontuberculous mycobacterial infections in hematopoietic stem cell transplant recipients: characteristics of respiratory and catheter-related infections. Biol Blood Marrow Transplant. 2000;6(4):361-369. [DOI] [PubMed] [Google Scholar]
- 24.Daley CL, Iaccarino JM, Lange C, et al. Treatment of nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline. Clin Infect Dis. 2020;71(4):905-913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The Japanese Data Center for Hematopoietic Cell Transplantation/The Japanese Society for Transplantation and Cellular Therapy. Hematopoietic cell transplantation in Japan. Annual Report of Nationwide Survey 2020. http://www.jdchct.or.jp/data/report/2021/ Accessed November 22, 2022. [Google Scholar]
- 26.Wu UI, Holland SM. Host susceptibility to non-tuberculous mycobacterial infections. Lancet Infect Dis. 2015;15(8):968-980. [DOI] [PubMed] [Google Scholar]
- 27.Toubiana J, Okada S, Hiller J. Heterozygous STAT1 gain-of-function mutations underlie an unexpectedly broad clinical phenotype. Blood. 2016;127(25):3154-3164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Philley JV, Safdar A, Daley CL. Nontuberculous mycobacterial disease in transplant recipients. In: Safdar A, editor. Principles and Practice of Transplant Infectious Diseases. New York: Springer; 2019: p. 503-517. [Google Scholar]
- 29.Wingard JR. Overview of infections following hematopoietic cell transplantation. In: UpToDate PTE. UpToDate, Waltham, MA. https://www.uptodate.com/contents/overview-of-infections-following-hematopoietic-cell-transplantation Accessed Nov 22, 2022. [Google Scholar]
- 30.Skolnik K, Kirkpatrick G, Quon BS. Nontuberculous mycobacteria in cystic fibrosis. Curr Treat Options Infect Dis. 2016;8(4):259-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Broglie L, Fretham C, Al-Seraihy A. Pulmonary complications in pediatric and adolescent patients following allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2019;25(10):2024-2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hayakawa A, Sato I, Kamibeppu K. Impact of chronic GVHD on QOL assessed by visual analogue scale in pediatric HSCT survivors and differences between raters: a cross-sectional observational study in Japan. Int J Hematol. 2022;115(1):123-128. [DOI] [PubMed] [Google Scholar]
- 33.Duncan CN, Buonanno MR, Barry EV, Myers K, Peritz D, Lehmann L. Bronchiolitis obliterans following pediatric allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2008;41(11):971-975. [DOI] [PubMed] [Google Scholar]
- 34.Bryant JM, Grogono DM, Rodriguez-Rincon D. Emergence and spread of a human-transmissible multidrug-resistant nontuberculous mycobacterium. Science. 2016;354(6313):751-757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.El Helou G, Viola GM, Hachem R, Han XY, Raad II. Rapidly growing mycobacterial bloodstream infections. Lancet Infect Dis. 2013;13(2):166-174. [DOI] [PubMed] [Google Scholar]
- 36.Henkle E, Winthrop KL. Nontuberculous mycobacteria infections in immunosuppressed hosts. Clin Chest Med. 2015;36(1):91-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Havlik JA, Horsburgh CR, Metchock B, Williams PP, Fann SA, Thompson SE. Disseminated Mycobacterium avium complex infection: clinical identification and epidemiologic trends. J Infect Dis. 1992;165(3):577-580. [DOI] [PubMed] [Google Scholar]
- 38.Bousfiha A, Moundir A, Tangye SG. The 2022 update of IUIS phenotypical classification for human inborn errors of immunity. J Clin Immunol. 2022;42(7):1508-1520. [DOI] [PubMed] [Google Scholar]
- 39.Oleaga-Quintas C, de Oliveira-Júnior EB, Rosain J. Inherited GATA2 deficiency is dominant by haploinsufficiency and displays incomplete clinical penetrance. J Clin Immunol. 2021;41(3):639-657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee H, Myung W, Koh WJ, Moon SM, Jhun BW. Epidemiology of nontuberculous mycobacterial infection, South Korea, 2007-2016. Emerg Infect Dis. 2019;25(3):569-572. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.