Abstract
Abstract
Background
Occupational diseases are one of the most important health problems related to employment However, in Malaysia, there are few epidemiological studies discussing these issues, especially among workers in the industry. For that, this study aimed to screen workers from high-risk industrial sectors, identify hazards in the workplace and recommend improvement measures in the workplace to prevent occupational diseases.
Methods and analysis
This is a 3-year project in which a survey of 100 000 workers from all 13 states in Malaysia will be conducted using a web-based screening tool that is comprised of two parts: occupational disease screening tool and hazard identification, risk assessment and risk control method. Data will be collected using a multistage stratified sampling method from 500 companies, including seven critical industrial sectors. The independent variables will be sociodemographic characteristics, comorbidities, previous medical history, high-risk behaviour and workplace profile. The dependent variable will be the types of occupational diseases (noise-induced hearing loss, respiratory, musculoskeletal, neurotoxic, skin and mental disorders). Subsequently, suggestions of referral for medium and high-risk workers to occupational health clinics will be attained. The approved occupational health service clinics/providers will make a confirmatory diagnosis of each case as deemed necessary. Subsequently, a walk-through survey to identify workplace hazards and recommend workplace improvement measures to prevent these occupational diseases will be achieved. Both descriptive and inferential statistics will be used in this study. Simple and adjusted binary regression will be used to find the determinants of occupational diseases.
Ethics and dissemination
This study has been approved by the MARA University of Technology Research Ethics Board. Informed, written consent will be obtained from all study participants. Findings will be disseminated to the Department of Occupational Health and Safety, involved industries, and through peer-reviewed publications.
Keywords: occupational & industrial medicine, preventive medicine, surveys and questionnaires
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This is a nationwide study conducted under the control of the Department of Occupational Safety and Health.
This study enhances features as a paperless, digitalised and real-time monitoring web-based application.
Lengthy and the availability of only English and Malay versions of the questionnaire may lead to missing foreign workers.
Obtaining respondents in certain industrial sectors such as fisheries could be a challenge.
Background
The International Labour Organization/WHO (ILO/WHO) joint committee was formed to deliberate on occupational health services (OHS). The committee found that the achievements of OHS in many countries were inadequate, although efforts have been made globally and in developed countries. For instance, the ILO reports nearly three million deaths annually from work-related accidents and diseases, indicating significant room for improvement in global occupational health standards1. The Basic Occupational Health Services (BOHS) guideline adopts the theory of public health and the principle of primary healthcare as in the Alma Ata Declaration and the WHO Global Strategy on Occupational Health for All.2
The concept of BOHS is an essential service in protecting people’s health in the workplace by promoting health, well-being and work capability to prevent unhealthy and accidental injuries. BOHS provides services using appropriate scientific methods and socially acceptable occupational health measures through a primary care approach.3
The Department of Occupational Safety and Health (DOSH), in collaboration with the Social Security Organization (SOCSO) and the National Institute of Occupational Safety and Health Malaysia, also undertakes various programmes for small and medium-sized industry to improve their working environment, but the accessibility is still low.3 One area that requires strengthening to detect early occupational diseases is BOHS.4
The prevention of these OHS includes detecting and managing work-related health problems at an earlier stage; improvement in the workplace with regards to reducing workplace exposures to related hazards and educating and involving working communities in the protection of their health.
In Malaysia, DOSH established its guidelines on OHS in 2005 and the guidelines on BOHS in 2014. The BOHS programme by the DOSH aims to identify the problems related to occupational diseases among workers and then to reduce the incidence of occupational disease and poisoning in Malaysia.
Occupational diseases in Malaysia
One of the most important health problems related to employment hazards is occupational disease. However, there are few epidemiological statistics on this issue, especially among workers in non-government workplaces.5 Due to ignorance and poor implementation of occupational health and safety measures, these workers are more susceptible to occupational health problems. Workers in Malaysia who have little access to basic occupational healthcare may suffer deterioration in their health as a long-term effect.5 In 2010, a total of 1426 cases of occupational disease and poisoning have been reported by DOSH. However, the statistics increased significantly in 2021 with a total reported cases of 5289, which includes noise-related hearing disorders, diseases caused by biological agents, musculoskeletal disorders (MSDs), poisoning, skin disorders, lung disease, diseases caused by physical agents, psychiatric disorders and cancer.6
Noise-induced hearing loss (NIHL) has been recorded as the most common occupational disease compared with other diseases such as MSDs, back pain, skin and lung diseases. This accounts for nearly 70% of reported occupational diseases as NIHL.7 Noise exposure is widely recognised as a major reversible cause of hearing loss8 and is exacerbated when combined with chemical hazards that have a synergistic to traumatic effect on hearing function.9 A recent report by the Department of Statistics Malaysia (2021) shows that noise-induced hearing disorders are the most important occupational disease in Malaysia. Worldwide, the disability-adjusted life year rates for NIHL was 84.23 per 100 000 population.10 Prevalence studies in Asia show that NIHL ranges from 17% to 89%, which varies by industry and sector. The rapid growth of the industrial sector, especially manufacturing, has led to an increased risk of occupational noise exposures that can cause irreversible damage. In 2019, the global age-standardized disability-adjusted life year rates (ASDR) for occupational noise-induced hearing loss (ONIHL) was 84.23 (95% CI 57.46 to 120.52) per 100 000 population disability-adjusted life year rates.
Regarding lung diseases, the number of occupational cases reported to DOSH Malaysia increased from 86 cases in 2015 to 150 cases in 2016, but only 10 occupational lung disease cases were confirmed by the Department of Statistics Malaysia (2021). This shows that the number of reported cases of occupational lung disease is still low, even though we know that the hazards in the construction industry pose a higher risk than in any other industry.
In addition, there are no specific studies that provide an accurate picture of occupational neurotoxicity in Malaysia. Most studies only look at the frequency of neurotoxicity symptoms in different groups of industrial workers exposed to different chemicals. All these studies also do not consider the associated factors that may increase the risk of workers developing neurotoxicity. A previous study by Yusof et al showed that the prevalence of neurotoxic symptoms ranged from 14.9% to 17.7% due to exposure to white spirits, ketones, formaldehyde and pesticides. In addition, the prevalence of concurrent exposure to biomechanical factors and neurotoxic chemicals was higher among male workers in the construction sector (12.7%), followed by men working in agriculture (7.6%) and industry (6.1%), respectively.5
Regarding occupational skin diseases (OSD), even though OSD is a common occupational disease, the number of reported cases of OSD in Malaysia is low. According to statistics from DOSH, only 137 OSDs were reported in 2019, representing only 1% of the total reported occupational diseases.5 Previous data showed that OSDs accounted for 7.8% of the 5377 cases for which benefits were paid in 2019.11 While DOSH and SOCSO data are the main data sources used to measure the incidence of occupational diseases, they may underestimate the prevalence of occupational diseases. Therefore, no specific statistic provides an accurate picture of the burden of OSD in the country.
In regard to MSDs, A 2019 report by Cieza et al showed that 427 million people in the WHO Western Pacific region suffer from MSDs, including osteoarthritis, rheumatoid arthritis, low back pain, neck pain, fractures and other injuries.12 In Malaysia itself, a total number of 553 MSD-related claims were recorded from 2009 to 2014. This number represents 25.22% of the total occupational diseases and all MSDs associated with temporary and permanent disability.13
Mental illness is one of the diseases that are thoroughly monitored by the WHO, as it is one of the targets under the Sustainable Development Goals to promote mental health through prevention and treatment to reduce mortality from non-communicable diseases. WHO reported that 15% of working-age adults were estimated to have a mental disorder in 2019.14 In Malaysia, According to the National Health and Morbidity Survey 2023, the prevalence of mental illness in Malaysia is 4.6%15 Factors causing increased stress in the workplace include workload, unpleasant tasks and conflicts between personal and professional demands.16
Hence, this study aims to conduct an Occupational Disease Related Health Screening Programme on 100 000 workers based on appropriate sampling methods representing workers in critical industrial sectors (manufacturing sector, construction sector, mining and extraction sectors, trade wholesale and retail sector, hotel sector and restaurant, facilities sector, agriculture, forestry and fisheries sector). This is subsequently followed by a walk-through survey (by sampling) to identify hazards in the workplace and recommend improvement measures in the workplace to prevent these occupational diseases. Moreover, to refer cases of suspected occupational diseases to participating approved Hospitals/Health Centres/Occupational Health Clinics within Malaysia for occupational disease confirmation and obtain occupational disease confirmation results for employees who have been referred to public/private health clinics and to ensure occupational disease reporting is reported to DOSH. At the same time, we will act as a secretariat for the activities under this programme such as meetings, workshops and engagement sessions with stakeholders and others. In the end, we will analyse and prepare programme reports and suggestions for improvement of the workplaces.
Methods and analysis
Industry engagement programme
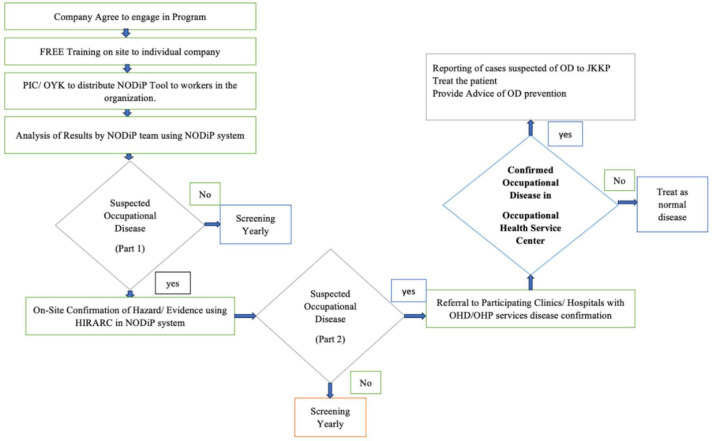
To kickstart the project, the industry engagement programme will be first organised promoting the project and recruiting companies involving the collaboration between DOSH and UiTM. The expected duration of the programme is 3 years (October 2022–July 2025). However, the length of involvement for each company is between 2 months and 1 year: from the initial health survey of workers, eventual hazard identification and confirmation of hazard at the workplace and subsequent suggestions of referral for medium and high-risk workers to occupational health clinics/centres. The approved Occupational Health Service Clinics/Providers will make a confirmatory diagnosis of each case as deemed necessary (figure 1 study flowchart).
Figure 1. Study flowchart. HIRARC, Hazard Identification, Risk Assessment and Risk Control; JKKP, Department of Occupational Health and Safety (Malay abbreviation); NODiP, National Occupational Disease Prevention Programme; OD, occupational disease, OHD/OHP, occupational health doctor, occupational health psychologist; PIC/OYK, person in charge/ competent person (Malay abbreviation).
Tool used for occupational disease screening
All tools to be used for this project will be taken from DOSH and some may require revision based on current disease development and suitability for it to be administered. The tool will consist of two sections. Section A contains information on sociodemographic background, company profile and medical history. All tools used have been validated in the local setting. Additional risk factors and associated hazards for each disease will be included in the medical history. Tables1 2 show the research tools and their interpretation.
Table 1. Research tools.
| Occupational diseases | Name of questionnaire | Citation | Sensitivity (specificity) |
| Noise injury hearing loss (NIHL) | Deafness and Communication Disorders (NIDCD) questionnaire | Rosso et al20 | 32%, (79%) |
| Occupational respiratory | British Medical Research Council (BMRC) | Cotes et al21Jones22 | Validated questionnaire |
| Occupational neurotoxicity | Q16 questionnaire | Lundberg et al23 | 73% (69%) |
| Occupational skin | Nordic Occupational Skin Questionnaire (NOSQ-2002) | Susitaival et al24Shamout and Adisesh25 | 32% (79%)70.3% (99.8%) |
| Occupational musculoskeletal | Standardised Nordic questionnaires | Kuorinka et al26 | Validated questionnaire |
| Occupational mental illness |
|
Husain et al27Netsereab et al28van der Westhuizen et al29Salleh30Krishnaswamy and Kyaw31 | 87.5% (80.6%)Validated questionnaire |
Table 2. Interpretation of a positive screening of suspected occupational diseases.
| Occupational NIHL | The total number of ‘yes’ answers is at least 3 for items 1–14. | |||
| Occupational skin disease | Criteria 1‘Yes’ for at least 1 item in question 1And‘Yes’ for question 2Criteria 2‘Yes’ for any symptoms in question 4 | |||
| Occupational musculoskeletal disorder | ‘Yes’ at least 1 from item 1.1And‘Yes’ at least 1 from items 1.2–1.3AndScore>5 for item 2.1AndScore>2 for item 2.2 | |||
| Occupational respiratory disease | The number of ‘Yes’ answers is at least 1 for items 1 to 4. | |||
| Occupational neurotoxicity | If the number of ‘Yes’ answers is a minimum of 3. | |||
| Occupational mental illness | DASS-21 scoring | |||
| Meaning | Depression | Anxiety | Stress | |
| Normal | 0–9 | 0–7 | 0–14 | |
| Mild | 10–13 | 8–9 | 15–18 | |
| Moderate | 14–20 | 10–14 | 19–25 | |
| Severe | 21–27 | 15–19 | 26–33 | |
| Extremely severe | 28+ | 20+ | 34+ | |
| JSL scoringScores of 17–39 were categorised into a low level of job stress, scores of 40–61 were grouped under moderate levels of job stress, and scores between 62 and 85 were classified under the high level of job stress. | ||||
DASS-21Depression Anxiety and Stress Scale 21JSLJob Stress Level
Pilot study
The purposes of conducting it are various, which include testing the adequacy of the research tool, assessing the feasibility of the full-scale study, collecting preliminary data, determining resource requirements and identifying logistical problems that might occur. According to Connelly, the sample size should be 10% of the full-scale study’s sample, while Hill suggested the sample size of a pilot study to be between 10 and 30 participants (Connelly and Hill). Pilot testing of 30 workers in a selected company will be conducted using simple random computer-generated sampling. Male and female aged 18 years or more, at least 1 year of work experience in the current company, able to read, understand Malay/English language (written and verbal), willing to participate in the study will be included. We are going to exclude part-time workers, industrial trainees and project consultants. The analysis will be performed to test Malay language occupational disease screening (OHS) tools for critical industries in Malaysia.
Development of web-based and mobile apps embedded with artificial intelligence
The web-based screening tool is comprised of two parts: occupational disease screening tool and hazard identification, risk assessment, and risk control method (HIRARC). An informed consent form will be included at the beginning of the survey. The occupational disease screening tool consists of a self-worker’s report of workers profiling (full profile of disease, workers reporting on work-related history and symptoms ranged approach based on the types of occupational diseases). Based on the screening tool—a scoring system will be used and grouped into low, medium or high risk. The HIRARC will explain the method used for risk assessment engaged as part of the activity for accomplishing the project. The occupational health risk assessment which will take place in the sectors selected shall address the hazards of the process involved in different activities and acquire a semiquantitative evaluation of the possible health and safety effects of failure of controls. The process of HIRARC requires four simple steps: classify work activities; identify hazards; conduct a risk assessment by calculating or estimating—the likelihood of occurrence, and severity of hazard; and decide if risk is tolerable and apply control measures (if necessary). Artificial intelligence will be embedded in mobile and web-based apps and an expert review of mobile and web-based application and usability study will be conducted. Web-based application data will be confidential and can only be accessed by the organisation to ensure the integrity of the user information, thus preventing data loss through unauthorised access. The interface can be seen by the employee, employer, Occupational Health Doctor, Occupational Health Psychologist (OHD/OHP), DOSH and administrator. The employee site will be used to collect employee’s information and health condition by using the research tool. In addition, it will be served as a medium to connect (receive an appointment from OHD/OHP) with the referred clinic for medium and high-risk employees and to see the result after the clinical assessment, whether the employee is diagnosed with the occupational disease or not for medium and high-risk category. The employer site will serve as a medium to declare a hazard at their company by submitting the HIRARC form. It has a dashboard, which consists of the number of low, medium or high-risk employees after filling in the questionnaires and the number of employees who are diagnosed with an occupational disease. The OHD/OHP site is a medium to connect with their patients (employees) to make appointments, update the result after clinical assessment of whether the employee is diagnosed with the occupational disease or not for the medium and high-risk categories, and upload the JKKP 7 form for employee that diagnosed with the occupational disease. The administrator (DOSH) site is where users can see the information that employees fill in the questionnaires and the result, whether they have a low, medium or high risk of that particular occupational disease. Moreover, the users can see the hazard declaration from the company, assign medium and high-risk employees to their referral clinic for further action see the JKKP form submitted by OHD/OHP about employees diagnosed with occupational disease and see the real-time dashboard. The real-time dashboard consists of the number of employees that are suspected or not suspected of having occupational disease by sector, the prevalence of diseases, the number of employees that have seen or not seen by OHD/OHP by clinic and the number of employees has been reported to DOSH as being diagnosed with occupational diseases.
Quality checks will be performed periodically by the research team. This process will include bi-weekly feedback from DOSH and OHD/OHP on-site via online feedback form. Any misunderstanding regarding parts of the web-based tool will be clarified in a monthly meeting with all project stakeholders. Additionally, training sessions tailored to different industries will be conducted to clarify the use of the tool.
Data collection
Study design and target population
This is a cross-sectional study that will be conducted among workers and managers from selected industries throughout Malaysia.
Study variables
Data collected consist of individual factors including sociodemographic characteristics such as gender, age, marital status, family size, occupation, educational level, income level, nationality, ethnicity, race, religion, location, comorbidities, previous medical or surgical history, allergic history, high-risk behaviour and Occupational Safety and Health (OSH) attitude and culture.17 In addition to workplace profile, which includes industries (types, size, location), managerial support, organisational measures, policies and legislations on occupational diseases, human resources and OSH-related specialties (availability of team expertise), creating awareness and risk communications.18 Work-related factors will be collected, which include the type of occupational, job tasks, hazards at work and exposures, working hours/shift, working experience, duration of exposure to hazards and previous job history/hazard exposure.19 The dependent variable will be types of occupational diseases in the company (NIHL, respiratory, musculoskeletal, neurotoxic, skin and mental disorders) and critical sector industries that consist of the manufacturing sector, construction sector, mining and extraction sector, trade wholesale and retail sector, hotel sector and restaurant, facility sector (gas, electricity, water service cleanliness), agriculture, forestry, and fisheries sector.
Sampling methods
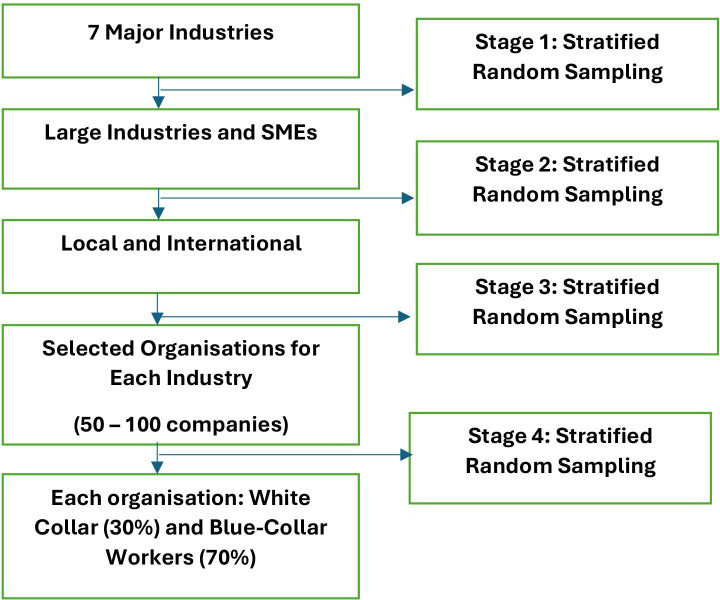
This is a 3-year project (October 2022–July 2025) including 100 000 workers from various industries in Malaysia. The 100 000 workers’ sample was the least sample size that proposed by the Department of Occupational Health and Safety in Malaysia to include as many as possible of workers in this health screening. As a result, this study can improve the reporting of cases and can be followed by conducting an appropriate intervention to improve workers’ well-being in the country. The industries selected for the research will be from the seven major industrial sectors. A line listing of the companies based on the category of industries will be obtained from DOSH. Multistage stratified random sampling from seven major industries in Malaysia by sector type and size of industry will be used (figure 2). It will involve all 13 states in Malaysia. Total companies are 500. The number of workers required for each company is 50–300 workers.
Figure 2. Sampling flowchart. SEM, small and medium-sized industry.
According to Department of Statistics Malaysia (DOSM) in 2024, there are around 17 million workers in Malaysia. As for the distribution of workers by sector, the manufacturing sector is the highest focus with 45 000 respondents, constituting 45% of the total 100 000 respondents. The hotel and restaurant sector will account for 19%, representing 19 000 respondents, followed by construction with 15 000 (15%) and trade wholesale and retail with 6000 (6%). Both the mining and quarry and utility sectors will be allocated 5000 respondents each (5%), and agriculture, forestry and fisheries will have 5000 respondents, accounting for 5% of the total. This distribution ensures that the representation is proportional to each sector’s importance or relevance to the study.
Data collection
The project will be done sequentially according to industries. The tools used will have some additional components where applicable based on the types of industries. For example, for the manufacturing industry involving ergonomics issues, the focus might be more on MSDs. Then, the on-site data collection will be achieved by walk through a visit of the selected industries as per the sampling methods and risk characterisation of the hazards. It will involve the administration of questionnaires using web-based and mobile app applications. However, to count for sampling bias, a hard copy of the questionnaire will be given to those lacking internet access.
Plan for data analysis
Due to the large amount of data that require sorting and characterisation, R statistics will be employed throughout this project. Data analysis will be conducted based on research objectives. Descriptive statistical analysis will be displayed in an aggregate manner using percentages, percentiles, means, SD, tables and plots. Inferential statistical analysis will follow that includes simple and adjusted logistic regression. Logistic regression will be performed to analyse the relationship between various factors such the sociodemographic factors, disease profiling, psychological well-being, OSH attitude and culture and industrial preparedness with occurrences of OD. In addition, it will be used to control for the confounders. The study findings will be presented using p value, crude OR and adjusted OR (AOR). A value of p<0.05 will be considered statistically significant with alpha=0.05.
Patient and public involvement
Participants were not involved in the design, recruitment and conduct of the study. The findings will be disseminated to the Department of Occupational Health and Safety and involved industries.
Ethics and dissemination
This study has been approved by the MARA University of Technology Research Ethics Board REC/03/2023 (ST/MR/70). Informed, written consent will be obtained from all study participants. Findings will be disseminated to the Department of Occupational Health and Safety, involved industries and through peer-reviewed publications.
Discussion
The National Occupational Disease Prevention Programme (NODiP) involves substantial numbers of various inter-relationship and intra-relationships of many entities mainly the workers, industrial companies and health institutions with the programme secretariat and consultants. Robust data influx, remote monitoring and complex analytics of these relationships warrant a centralised and integrated system for efficient data management. This study proposed to design an integrated and efficient data system architecture with enhanced features as a paperless, digitalised and real-time monitoring web-based and mobile applications. Implementation of this system is timely and shall mark a significant milestone in the digital transformation of reporting, analytics, and monitoring in the field of OSH in Malaysia.
The proposed NODiP data management system shall be an integrated, sustainable and centralised system that caters to six occupational diseases, HIRARC assessment of the workplace and doctor’s confirmatory examination and diagnosis of 100 000 workers, approximately 500 companies from seven critical industries, and approximately 300 health institutions. The five main users identified, that is, workers, workplace, clinic/hospital and administrators from UiTM and DOSH will be given different login and interphases according to their roles. Each worker user is screened via an online questionnaire of each occupational disease, resulting in a Questionnaire Scoring (QS) category (suspected, mixed and unlikely) while each workplace is assessed via an online HIRARC assessment resulting in HIRARC scoring (HS) category (high, intermediate and low). Both QS and HS scorings will be matched resulting in an Occupational Disease Risk Scoring (RS) category (suspected, mixed and unlikely). Subsequently, workers with suspected and mixed-picture categories of occupational disease will be referred to appointed clinics or hospital panels for confirmatory diagnosis via examination and investigation. Data input from clinics or hospitals will be matched to the RS scoring resulting in a confirmatory occupational disease diagnosis with disease classification (occupational disease, work-related disease or non-occupational related). All confirmed occupational diseases will be notified to DOSH via DOSH Form 7 (JKKP 7) and evidence of notification will be also made available in the system as reporting evidence. Remote monitoring by programme administrators will be made available via direct monitoring as well as in real-time dashboard view at websites. This system will be using server, domain and data storage with cloud computing subscriptions under University Technology MARA with interphases cybersecurity and confidentiality of data.
Benefits of organisation joining this programme
(1) Organisational benefit
The organisation will get a reduction in the number and prevalence of occupational diseases in the future, an increase in worker productivity and an improvement in overall well-being. This is done through early disease identification and referral, free on-site training of occupational diseases and webinars which will be provided for remote areas. In addition, they will be provided with free usage of the NODiP system for the duration of the project and free hazard confirmation.
(2) Competent person (OYK) in the organisation
The OYK will be provided with free training on hazard identification, continuous education programme (CEP) points, free usage of the NODiP system for the duration of the project and free consultation by the NODiP consulting team on issues about occupational diseases.
(3) Workers in the organisation
The workers in the organisation will get an early disease detection, disease diagnosis and referral of cases—based on the suspected occupational diseases only.
Benefits of OHS providers joining NODiP programme
OSH will get training on Occupational Diseases and NODiP System Usage with minimal cost, free usage of NODiP system for confirmatory diagnosis of occupational diseases during the period of programme, CEP points for OHD based on involvement in this programme and becoming an NODIP-OHC (Approved NODiP Occupational Health Service Referral Center) for referral of cases suspected of occupational diseases from organisations in Malaysia.
Study limitations
This study has some limitations, first, the questionnaire is lengthy and can only be translated into two languages due to time limitations. We may miss a significant number of foreign workers in certain sectors, and some companies might choose to translate the questionnaire for their foreign employees, potentially introducing additional biases. Second, the difficulty of getting company approval, especially internationally based companies, and difficulty in accessing locations with less than 50 workers, hence may miss out on small-sized industries. Third, we may also face difficulty obtaining respondents in certain industrial sectors with a limited number of workers scattered throughout Malaysia, for example, fisheries, agricultural and logging industries.
Acknowledgements
We would like to thank DOSH Malaysia and all collaborators of this project for their support during the development phase of the project.
Footnotes
Funding: This project is being funded by a research grant FRGS/1/2021/SKK05/UITM/03/1.
Prepublication history for this paper is available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-083796).
Patient consent for publication: Not applicable.
Provenance and peer review: Not commissioned; externally peer-reviewed.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Contributor Information
Siti Munira Yasin, Email: smunira@uitm.edu.my.
Nurhuda Ismail, Email: yuda@uitm.edu.my.
Mohd Izwan Masngut, Email: izwan7698@uitm.edu.my.
Nik Nairan Abdullah, Email: nairan@uitm.edu.my.
Nooni Ezdiani Yasin, Email: nooniezdiani@gmail.com.
Mazlifah Omar, Email: mazlifahomar@uitm.edu.my.
Sazzli Shahlan Kasim, Email: sazzlishahlan@uitm.edu.my.
Ameran Saiman, Email: ameran@uitm.edu.my.
Kamarulzaman Muzaini, Email: kamarulzaman@uitm.edu.my.
Anza Elias, Email: anzaamin@gmail.com.
Ely Zarina Samsudin, Email: elyzarina@uitm.edu.my.
Ahmad Izuanuddin Ismail, Email: izuanuddin@uitm.edu.my.
Sazreza Shahadan, Email: sazreza@uitm.edu.my.
Khairul Hafezad Abdullah, Email: khairul085@uitm.edu.my.
Ismassabah Ismail, Email: ismassabah@uitm.edu.my.
Khairul Mizan Taib, Email: khairulmizan@uitm.edu.my.
Mariam Mohamad, Email: mariammd@uitm.edu.my.
Nur-Hasanah Ruslan, Email: nur-hasanah@uitm.edu.my.
Mohd Azli Abdul Malek, Email: abekenobiwan@gmail.com.
Mohd. Ridzuan Anuar, Email: mridzuan.anuar@mohr.gov.my.
Nazrai Ahmad Zabidi, Email: nazrai_a@yahoo.com.
Anis Syamimi Mohamed, Email: anissyamimimohamed@gmail.com.
Nurul Izzah Kamarudin, Email: nurul.izzah@uitmpuncakalam.com.
Mohd Hafiz Abdul Manan, Email: hafiz.manan@uitmpuncakalam.com.
Ahmad Fitri Abdullah Khai, Email: ahmadfitri@mohr.gov.my.
Ahmad Faiz Azhari Noor, Email: ahmadfaiz@mohr.gov.my.
Meram Azzani, Email: dr_memeazzani@yahoo.com.
References
- 1.International Labour Organization . Nearly 3 million people die of work-related accidents and diseases . International Labour Organization; 2023. [Google Scholar]
- 2.WHO . ALMA Ata 1978: primary health care. Geneva & New York: World Health Organization & United Nations Children’s Fund; 1978. [Google Scholar]
- 3.Samsuddin N, Razali A, Rahman NAA, et al. The proposed future infrastructure model for basic occupational health services in Malaysia. Malays J Med Sci. 2019;26:131–7. doi: 10.21315/mjms2019.26.2.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rantanen JH. Basic occupational health services—their structure, content and objectives. 2005.
- 5.Yusof MZ, Nik Mahmod NAK, A. Rahman NA, et al. Prevalence of occupational diseases among small and medium industry workers in Malaysia: a systematic review. JCHS. 2019;4:4. doi: 10.24191/jchs.v4i2.7508. [DOI] [Google Scholar]
- 6.Department of Statistics Malaysia. 2021. https://www.dosm.gov.my/v1/index.php?r=column/pdfPrev&id=YzI2NWE2U0tXS1VEdnFsWHpqM1Fudz09 Available.
- 7.DOSH Noise-related hearing disorders. 2021. https://www.dosh.gov.my/index.php/guidelines-on-management-of-occupational-noise-related-hearing-disorders/file Available.
- 8.Johnson TA, Cooper S, Stamper GC, et al. Noise exposure questionnaire: A tool for quantifying annual noise exposure. J Am Acad Audiol. 2017;28:14–35. doi: 10.3766/jaaa.15070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Razali A, Azmy FI, Khairul Anwar AM. Development and validation of Malaysian noise and chemical exposure questionnaire towards hearing among hospital workers. Med J Malaysia. 2022;77:420–6. [PubMed] [Google Scholar]
- 10.Liu C, He L, Shan X, et al. The Burden of occupational noise-induced hearing loss from 1990 to 2019: An analysis of global Burden of disease data. E H. 2024 doi: 10.1097/AUD.0000000000001505. [DOI] [PubMed] [Google Scholar]
- 11.DOSH . Guidelines for Hazard Identification, Risk Assessment and Risk Control (HIRARC) Malaysia: Department of Occupational Safety and Health, Ministry of Human Resources; 2008. [Google Scholar]
- 12.Cieza A, Causey K, Kamenov K, et al. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2021;396:2006–17. doi: 10.1016/S0140-6736(20)32340-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rohani JM, Mohd-Zainal A, Johari MF, et al. Analysis of compensation cost related to musculoskeletal disorders (MSDs) against younger and older malaysian manufacturing workers. the International Conference on Industrial Engineering and Operations Management; 2016 8-10 March; Kuala Lumpur, Malaysia n.d.
- 14.World Health Organization Mental health at work 2022. https://www.who.int/news-room/fact-sheets/detail/mental-health-at-work n.d. Available.
- 15.Institute for Public Health 2024 National Health and Morbidity Survey (NHMS) 2023: Non-communicable diseases and healthcare demand- key findings 2023. https://iku.gov.my/nhms-2023 Available.
- 16.Maulik PK. Workplace stress: A neglected aspect of mental health wellbeing. Indian J Med Res. 2017;146:441–4. doi: 10.4103/ijmr.IJMR_1298_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ashraf MA. Demographic factors, compensation, job satisfaction and organizational commitment in private university: an analysis using SEM. JGR . 2020;11:407–36. doi: 10.1108/JGR-01-2020-0010. [DOI] [Google Scholar]
- 18.Lumayag Codilla K, Evangelista Quinal J. Work attitudes among office personnel at MSU-Iligan Institute of Technology, Iligan City Philippines. JGPP. 2019;6 doi: 10.18196/jgpp.61105. [DOI] [Google Scholar]
- 19.Trkulja V, Hrabač P. Hazard ratio. Croat Med J. 2019;60:293–6. doi: 10.3325/cmj.2019.60.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosso M, Agius R, Calleja N. Development and validation of a screening questionnaire for noise-induced hearing loss. Occup Med (Lond) 2011;61:416–21. doi: 10.1093/occmed/kqr059. [DOI] [PubMed] [Google Scholar]
- 21.Cotes JE, Zejda J, King B. Lung function impairment as a guide to exercise limitation in work-related lung disorders. Am Rev Respir Dis. 1988;137:1089–93. doi: 10.1164/ajrccm/137.5.1089. [DOI] [PubMed] [Google Scholar]
- 22.Jones PW. Quality of life measurement for patients with diseases of the airways. Thorax. 1991;46:676–82. doi: 10.1136/thx.46.9.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lundberg I, Högberg M, Michélsen H, et al. Evaluation of the Q16 questionnaire on neurotoxic symptoms and a review of its use. Occup Environ Med. 1997;54:343–50. doi: 10.1136/oem.54.5.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Susitaival P, Flyvholm M ‐A., Meding B, et al. Nordic Occupational Skin Questionnaire (NOSQ‐2002): a new tool for surveying occupational skin diseases and exposure. Contact Derm. 2003;49:70–6. doi: 10.1111/j.0105-1873.2003.00159.x. [DOI] [PubMed] [Google Scholar]
- 25.Shamout Y, Adisesh A. The nordic occupational skin questionnaire. OCCMED. 2016;66:82. doi: 10.1093/occmed/kqv059. [DOI] [PubMed] [Google Scholar]
- 26.Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233–7. doi: 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- 27.Husain N, Chaudhry N, Rhouma A, et al. Validation of the self-reporting questionnaire (SRQ 20) in British Pakistani and White European population in the United Kingdom. J Affect Disord. 2016;189:392–6. doi: 10.1016/j.jad.2015.08.068. [DOI] [PubMed] [Google Scholar]
- 28.Netsereab TB, Kifle MM, Tesfagiorgis RB, et al. Validation of the WHO self-reporting questionnaire-20 (SRQ-20) item in primary health care settings in Eritrea. Int J Ment Health Syst. 2018;12:61. doi: 10.1186/s13033-018-0242-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van der Westhuizen C, Wyatt G, Williams JK, et al. Validation of the Self Reporting Questionnaire 20-Item (SRQ-20) for use in a low- and middle-income country emergency centre setting. Int J Ment Health Addict. 2016;14:37–48. doi: 10.1007/s11469-015-9566-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Salleh MR. Psychiatric morbidity in schizophrenic relatives--use of Self-Reporting Questionnaires (SRQ) Singapore Med J. 1990;31:457–62. [PubMed] [Google Scholar]
- 31.Krishnaswamy S, Kyaw OH. A pilot study on the use of the World Health Organisation self reporting questionnaires (S.R.Q.) on A Malaysian population. Singapore Med J. 1985;26:431–4. [PubMed] [Google Scholar]