Abstract
Abstract
Objectives
Frequent attenders (FAs) visit healthcare settings at higher rates compared with the general population and use disproportionate amounts of healthcare resources. Frequent attendance (FA) has also been associated with greater morbidity and adverse socioeconomic circumstances. Our study aimed to describe the sociodemographic profile, clinical presentation, and healthcare utilisation patterns of adolescent FAs at polyclinics in Singapore and to determine the factors associated with adolescent FA.
Design
Retrospective electronic database analysis.
Setting
A cluster of eight state-subsidised public primary care clinics (polyclinics).
Participants
Multiethnic Asian adolescents aged 10–19 years who attended the eight polyclinics in 2021. FAs were defined as the top 10% of clinic attendees in terms of annual visit frequency.
Results
In 2021, 34 645 adolescents attended the polyclinics for 75 902 visits. Visits were for acute (52.8%), chronic (26.2%) and preventive (27.7%) care. FAs attended ≥4 visits annually, accounting for 14.4% of adolescents and 42.5% of total attendances. Compared with non-FAs, FAs were older (OR 1.16, 95% CI 1.15 to 1.18, p<0.001), more likely to be of non-Chinese ethnicity, and have received financial aid (OR 1.68, 95% CI 1.58 to 1.79, p<0.001). FAs had more underlying psychiatric conditions (p<0.001) but presented less frequently with psychiatric complaints (p<0.001). FAs were more likely to be referred to emergency departments (p<0.001) and psychiatry clinics (p<0.001), to be prescribed potentially addictive medication (p<0.001), and had longer annual medical leave certification (7 days (IQR=4–11) vs 3 days (IQR=1–3, p<0.001)).
Conclusion
Adolescent FA was associated with increasing age, non-Chinese ethnicity and lower socioeconomic status. Despite having more underlying psychiatric conditions, adolescent FAs presented more frequently with acute physical complaints instead of psychiatric symptoms. Adolescent FAs had longer annual medical leave certification and greater healthcare utilisation indicated by more clinic visits and referrals to emergency departments and psychiatry clinics.
Keywords: adolescent, primary care, Singapore, mental health
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study included a large number of multiethnic Asians and used data from approximately a third of the public adolescent primary care population of Singapore.
We used the top 10th percentile definition for frequent attendance in this study, which allows for greater ease of comparison between other frequent attender studies in different healthcare settings.
Due to the retrospective nature of this study, the variables available for analysis were limited to the data recorded in the electronic medical records.
This study was conducted during the COVID-19 pandemic. There may be potential differences in the healthcare utilisation and presentation patterns compared with non-pandemic periods.
Introduction
Frequent attenders (FAs) are a small group of patients who visit healthcare settings at a higher rate compared with the general population and use a disproportionate amount of healthcare resources.1,3 The top 10% of attendees are estimated to account for 30%–50% of all primary care encounters.4 Frequent attendance (FA) has been associated with higher rates of physical illness,5 6 mental health issues,7,9 somatisation,3 9 adverse socioeconomic circumstances9 10 and poorer quality of life5 11 among adult primary care patients.
FA in adolescents poses a unique challenge in primary care as adolescents have different healthcare needs and presentation patterns compared with adults. Adolescents have lower levels of help-seeking behaviour12 and use healthcare at the lowest rates among all age groups.13 Reasons for the disparity may include a distrust of the healthcare system, concerns about confidentiality, stigma and fear of being judged by healthcare providers for their socially disapproved or risk-taking behaviour.14,17 Adolescent FAs also present frequently with somatic symptoms such as abdominal pain, chest pain, headache, lethargy, weight loss, dizziness, syncope or other non-specific symptoms.3 18 This poses a diagnostic challenge and results in unmet mental healthcare needs, which have been subsequently linked to poorer physical and mental health outcomes in adulthood.19 20
Studies on FAs have focused mainly on adults.1 The few studies conducted on adolescent FAs have shown significant associations with female gender,21 22 younger age,3 23 lower socioeconomic factors,3 22 23 somatic complaints,3 21 22 mental illness321,23 and increased hospital visits.3 However, the age range of the study populations and definitions of FA have differed among studies, hampering interstudy comparison.
In Singapore, the profile and healthcare utilisation patterns of adolescent FAs in primary care are unknown. There is little comparative data from neighbouring countries due to a lack of epidemiological data and dissimilar ethnic make-up among the Southeast Asian nations.24 Therefore, this study aimed to describe the sociodemographic profile, clinical presentation and healthcare utilisation patterns of adolescents attending polyclinics in Singapore and to determine the factors associated with adolescent FA.
Methods
Definition of FAs
FAs are defined by their frequency of clinic visits, which is determined either by using the top percentiles by frequency of annual clinic attendances or by identifying patients presenting more than a certain number of visits.25 All visits were considered, including those with scheduled appointments. Using the top percentile definition allows for standardisation among studies where the proportion of FAs remains similar regardless of population size, presentation patterns or differences in primary care settings. This allows for greater ease of comparison between different frequent attender studies. However, this definition requires a retrospective view and limits its applicability in real-time situations, which may result in delayed identification and missed opportunities for intervention in FAs.25
In this study, the top percentile definition of FA was used as there was no prior local primary care data on the frequency of presentations in adolescents to determine an appropriate visit frequency cut-off, in addition to the reasons mentioned above. The 10th percentile was selected as it was the most frequently used percentile number in the literature.25
Study design and setting
During the study period, primary healthcare in Singapore was provided through a network of 22 public outpatient polyclinics and approximately 1800 private general practitioner clinics throughout Singapore.26 Polyclinics are large state-subsidised public healthcare centres that provide primary care services such as outpatient medical treatment, preventive healthcare and health education.26 The study sites were eight polyclinics from the Singapore Health Services (SingHealth) group of public healthcare institutions, which service the eastern region of Singapore (approximately one-third of the population of Singapore). The clinics are situated in the central and eastern regions of the highly urbanised island state, with approximately 1.6 million patient visits in 2021.27 The clinics operate from 08:00 to 17:00 on Mondays to Fridays, from 08:00 to 12:30 on Saturdays and are closed on Sundays.
A retrospective database study was conducted using electronic medical records data from 1 January 2021 to 31 December 2021 across the study sites. The study was granted ethics exemption by the SingHealth Centralised Institutional Review Board (Ref: 2022/2072).
Patient and public involvement
The research proposal, including the research questions, methods and outcome measures, was presented to a research forum consisting of current or former patients at SingHealth polyclinics. This was done to gather the patient’s perspective on our study.
Population
All adolescents aged 10–19 years28 at the time of presentation who registered for in-person or video consultation at SingHealth Polyclinics with at least one recorded diagnosis, locals and foreigners alike, were included in the analysis.
Data extraction process and deidentification of data
The study sites use a common electronic platform (Sunrise Clinical Manager) that contains data on clinical notes, diagnosis codes, diagnostic tests and results, medication prescriptions, medical leave certification and specialist referrals. Sociodemographic and financial information is captured via a separate system (Outpatient Administrative System). The relevant data were extracted from the respective databases and uploaded to a single enterprise data repository known as the Electronic Health Intelligence System (eHINTS).
A research informatics staff from the institution’s research department extracted the data via the eHINTS platform. To ensure patient confidentiality, the data were deidentified by an appointed trusted third party. The key linking patient identifiers to the dataset were held securely by the trusted third party who was not involved in the study in any other way. The deidentified data were made available only to members of the research team and stored on a secure device.
Data variables
Sociodemographic variables included age, gender, ethnicity and receipt of financial aid as a surrogate of socioeconomic status. Financial aid encompassed any of the following governmental subsidy programmes: the MediFund scheme (a means-tested governmental endowment fund for patients who have difficulty paying their medical bills after all other means of payment have been exhausted) and the Community Health Assist Scheme (CHAS) Orange and Blue Schemes (a stratified means-tested subsidy for public outpatient treatment available for Singapore citizens). Enrolment in these financial schemes is voluntary and requires application. Adolescents cannot directly apply for the CHAS scheme; instead, their families must apply on behalf of their entire household.
Clinical presentation variables included the category of visits (acute/chronic/preventive), diagnosis categories by systems (online supplemental appendix A) and individual diagnosis codes according to the International Classification of Diseases Tenth Revision.28
Healthcare utilisation variables included the date of presentation, frequency of clinic visits, total duration of medical leave certification, frequency of specialist outpatient clinic and emergency department referrals and frequency of being prescribed potentially addictive medication such as benzodiazepines, opioids, gabapentin and various cough syrups (online supplemental appendix B).
Statistical analysis
Table 1 provides an overview of the total number of adolescents, categorised by FAs and non-FAs and their association with sociodemographic factors. Table 2 presents the total number of clinic visits of all attendees, including the type and related diagnosis of each visit. Table 3 displays the association between FAs and non-FAs and their healthcare utilisation profile. We employed descriptive analysis to summarise baseline demographics, clinical data and healthcare utilisation data. For continuous variables (all continuous variables were skewed), we reported the median and IQR. Categorical variables were presented as frequencies and percentages. Binary logistic regression was used to calculate the crude ORs and adjusted ORs. The adjusted analyses were controlled for potential confounders such as age, gender, ethnicity and financial support, as shown in table 1. χ2 and Mann–Whitney U tests were used to compare the categorical and continuous clinical, healthcare utilisation and medication variables between the frequent attender and non frequent attender groups.
Table 1. Sociodemographic factors associated with FA using multivariable logistic regression.
| Total, n(%) | Non-FAs, n(%) | FAs, n(%) | Crude OR | P value | Adjusted OR | P value | |
| Total adolescents | 34 645 | 29 652 (85.6) | 4993 (14.4) | – | – | – | – |
| Age, Median (IQR) | 16 (13–18) | 15 (13–18) | 17 (15–19) | 1.16 (1.15–1.17) | <0.001 | 1.16 (1.15–1.18) | <0.001 |
| Gender | |||||||
| Male | 17 617 (50.9) | 15 097 (50.9) | 2520 (50.5) | 0.98 (0.93–1.04) | 0.562 | 1.01 (0.95–1.08) | 0.695 |
| Female | 17 028 (49.1) | 14 555 (49.1) | 2473 (49.5) | 1 | 1 | ||
| Ethnicity | |||||||
| Chinese | 20 715 (59.8) | 18 148 (61.2) | 2567 (51.4) | 1 | 1 | ||
| Malay | 8169 (23.6) | 6650 (22.4) | 1519 (30.4) | 1.61 (1.51–1.73) | <0.001 | 1.43 (1.33–1.54) | <0.001 |
| Indian | 3739 (10.8) | 3130 (10.6) | 609 (12.2) | 1.38 (1.25–1.51) | <0.001 | 1.40 (1.27–1.54) | <0.001 |
| Others | 2022 (5.8) | 1724 (5.8) | 298 (6.0) | 1.22 (1.07–1.39) | 0.002 | 1.19 (1.04–1.36) | 0.01 |
| Financial support | |||||||
| Yes* | 13 249 (38.2) | 10 724 (36.2) | 2525 (50.6) | 1.81 (1.70–1.92) | <0.001 | 1.68 (1.58–1.79) | <0.001 |
| No | 21 396 (61.8) | 18 928 (63.8) | 2468 (49.4) | 1 | 1 |
Receipt of any form of financial support.
Table 2. Clinical presentation and healthcare utilisation (by number of visits).
| Total, n(%) | Non-FAs, n(%) | FAs, n(%) | P value | |
| Total visits | 75 902 | 43 658 (57.5) | 32 244 (42.5) | – |
| Category of diagnosis | ||||
| Acute | 40 141 (52.9) | 20 880 (46.5) | 19 261 (53.2) | – |
| Chronic | 19 901 (26.2) | 11 596 (25.8) | 8305 (23.0) | – |
| Preventive | 21 025 (27.7) | 12 408 (27.6) | 8617 (23.8) | – |
| Visits with a psychiatric diagnosis in 2021 | ||||
| Yes | 1333 (1.8) | 826 (1.8) | 507 (1.6) | <0.001 |
| No | 74 569 (98.2) | 42 832 (98.2) | 31 737 (98.4) |
Table 3. Clinical presentation and healthcare utilisation (by number of adolescents).
| Total, n(%) | Non-FAs, n(%) | FAs, n(%) | P value | |
| Total adolescents | 34 645 | 29 652 (85.6) | 4993 (14.4) | – |
| Visit count, median (IQR) | 1 (1–2) | 1 (1–2) | 5 (4–7) | – |
| Annual medical leave certification duration, median (IQR) | 3 (2–5) | 3 (1–3) | 7 (4–11) | <0.001 |
| DiagnosisAny psychiatric diagnosis in 2021 | ||||
| Yes* | 1138 (3.3) | 790 (2.7) | 348 (7.0) | <0.001 |
| No | 33 507 (96.7) | 28 862 (97.3) | 4645 (93.0) | |
| Referrals | ||||
| Specialist referral per year, median (IQR) | 1 (1–1) | 1 (1–1) | 1 (1–2) | <0.001 |
| Referred to psychiatry in 2021 | ||||
| Yes † | 600 (1.7) | 430 (1.5) | 170 (3.4) | <0.001 |
| No | 34 045 (98.3) | 29 222 (98.5) | 4823 (96.6) | |
| Referred to emergency department in 2021 | ||||
| Yes‡ | 1139 (3.3) | 736 (2.5) | 403 (8.1) | <0.001 |
| No | 33 506 (96.7) | 28 916 (97.5) | 4590 (91.9) | |
| Prescription of potentially addictive medication | ||||
| Dextromethorphan | 3716 (10.7) | 2402 (8.1) | 1314 (26.3) | <0.001 |
| Procodin (codeine/promethazine) | 58 (0.2) | 24 (0.1) | 34 (0.7) | <0.001 |
| Opioids | 49 (0.1) | 23 (0.1) | 26 (0.5) | <0.001 |
| Gabapentin | 15 (0.0) | 6 (0.0) | 9 (0.2) | <0.001 |
| Benzodiazepines | 10 (0.0) | 6 (0.0) | 4 (0.1) | <0.001 |
| Prescribed potentially addictive medication in 2021 | ||||
| Yes§ | 3777 (10.9) | 2434 (8.2) | 1343 (26.9) | <0.001 |
| No | 30 868 (90.1) | 27 218 (91.8) | 3650 (73.1) |
Individuals with at least one psychiatric diagnosis in 2021
Individuals thatwho were referred to psychiatry at least once in 2021
Individuals thatwho were referred to the emergency department at least once in 2021
Individuals who were prescribed potentially addictive medication at least once in 2021
A p value of <0.05 was considered statistically significant. All statistical analyses were conducted using IBM SPSS V.28.0.
Results
Sociodemographic profile
In 2021, 34 645 adolescents attended the polyclinics with a total of 75 902 visits (table 1). The median age was 16 years (IQR=13–18); the majority were males (50.9%), Chinese (59.8%) and 38.2% were recipients of financial aid. Table 1 provides an overview of the total number of adolescents and the associated sociodemographic factors.
Using the selected definition of FA (top 10th percentile of adolescent clinic attendees), the cut-off threshold for adolescent FA was identified as four visits annually. With this cut-off threshold, 14.4% (n=4993) of adolescents were identified as FAs who were responsible for 42.5% of the total clinic visits.
With multivariable logistic regression analysis (table 1), FA was associated with increasing age (OR 1.16, 95% CI 1.15 to 1.18, p<0.001), non-Chinese ethnic groups (Malays (OR 1.43, 95% CI 1.33 to 1.54, p<0.001), Indians (OR 1.40, 95% CI 1.27 to 1.54, p<0.001), Other races (OR 1.19, 95% CI 1.04 to 1.36, p=0.01)) and receipt of financial aid (OR 1.68, 95% CI 1.58 to 1.79, p<0.001). FA was not significantly associated with gender (OR 1.01, 95% CI 0.95 to 1.08, p=0.695).
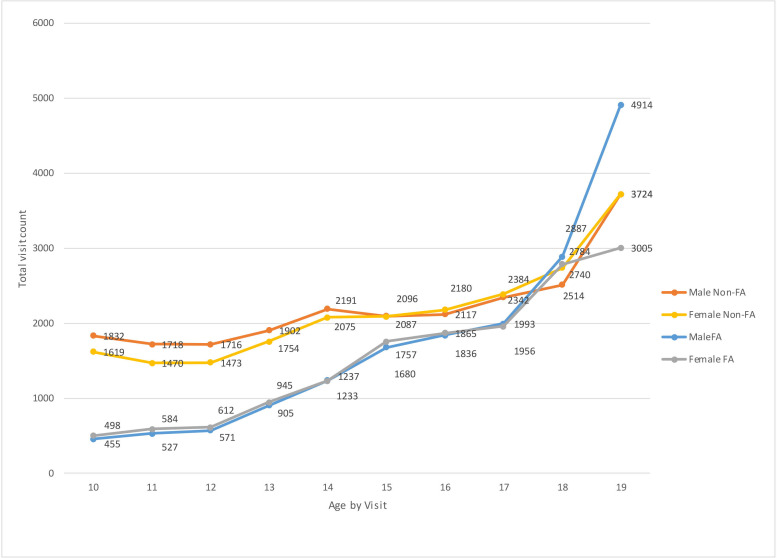
Overall, older adolescents presented more to the polyclinics compared with younger adolescents (figure 1). In the frequent attender group, the number of visits for males and females was similar in all ages except for a large disparity seen in the 19-year-old age group (4914 male visits vs 3005 female visits).
Figure 1. Total visits by age, gender and frequent attender status. Overall, older adolescents presented more to the polyclinics compared with younger adolescents. In the frequent attender group, the number of visits for males and females was similar in all ages except for a large disparity seen in the 19-year-old age group (4914 male visits vs 3005 female visits). FA, frequent attender.
Clinical presentation profile
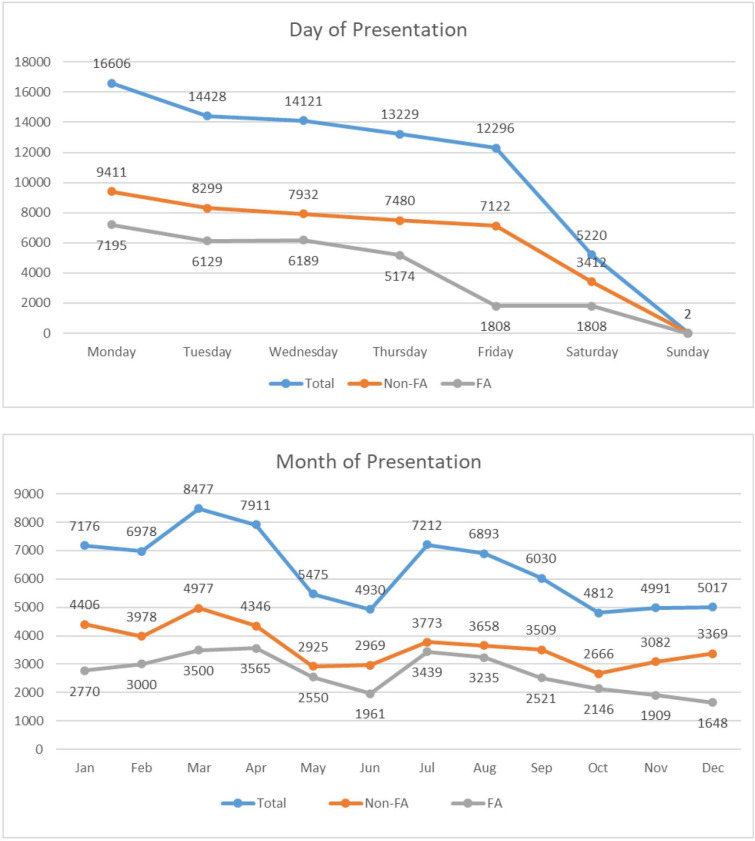
Mondays had the highest overall patient attendance. Increases in patient attendance were seen in the months of March–April and July–August (figure 2).
Figure 2. Day and month of presentation by visit count. Mondays had the highest overall patient attendance. Increases in patient attendance were seen in the months of March–April and July–August. *Polyclinics operate full days from Mondays to Fridays, half days (mornings) on Saturdays and are closed on Sundays. †The two patient visits recorded on Sunday were from temporary clinics set up during the COVID-19 pandemic. FA, frequent attender.
Table 2 presents the total number of clinic visits of all attendees, including the type and related diagnosis of each visit. The visits were predominantly for acute conditions (52.9%), followed by preventive (27.7%) and chronic conditions (26.2%) (table 2). Online supplemental figures A and B provides a summary of the most frequently encountered diagnosis categories by system groups and individual diagnoses.
Psychiatric diagnoses were present in 1.8% of all visits among all adolescents (table 2). The most common psychiatric conditions seen were anxiety (0.6%), depression (0.5%) and insomnia (0.3%).
Table 3 displays the total number of adolescents and their healthcare utilisation profile. FAs were more likely to have presented with at least one psychiatric diagnosis in 2021 compared with non-FAs (p<0.001) (table 3). However, FAs presented less frequently for psychiatric complaints compared with non-FAs (p<0.001) (table 2).
Healthcare utilisation patterns
The total number of clinic visits for all adolescents ranged from 1 to 127 (the individual with 127 clinic visits was a statistical outlier who presented mostly for directly observed therapy for the treatment of tuberculosis) with a median of 1 (IQR=1–2) (table 3). FAs attended more frequently than non-FAs (median of five visits (IQR=4–7) vs one visit (IQR=1–2), p<0.001). The median duration for medical leave certification for all adolescents was 3 days per annum (IQR=2–5). FAs had longer medical leave certification of 7 days (IQR=4–11) versus 3 days (IQR=1–3) in non-FAs (p<0.001).
The median number of specialist referrals for all adolescents overall was 1 (IQR=1–1) (table 3). Online supplemental figure C provides a summary of the top specialist referrals. Compared with non-FAs, FAs were more likely to be referred to a psychiatrist (p<0.001) and the emergency department (p<0.001) (table 3).
Potentially addictive medication prescriptions were generally low except for prescriptions for dextromethorphan (table 3). Considering all potentially addictive medications as a whole, FAs were more likely to be prescribed any potentially addictive medication compared with non-FAs (p<0.001).
Discussion
Our study has shown that adolescent FA was associated with increasing age, non-Chinese ethnicity, lower socioeconomic status and higher rates of underlying psychiatric conditions. FAs presented with acute physical complaints more frequently than psychiatric symptoms, had longer annual medical leave certification, and had greater healthcare utilisation indicated by a higher frequency of clinic visits and more referrals to the emergency department and psychiatry clinics.
Socio-demographic profile
Adolescent FA was associated with increasing age with no significant gender differences. This is discordant with current literature: adolescent FA is usually associated with younger age3 22 29 and female gender.22 30 We postulate that this may be due to the effect of full-time conscripted military personnel. In Singapore, all males around the age of 18–20 are required to serve 2 years of mandatory military service. These full-time conscripted military personnel have been shown to consult the polyclinics at higher rates for medical leave certification to remain absent from duty.31 Local emergency department studies on FA have also described this phenomenon, where the largest proportion of FAs seen were males aged 16–25 years who presented mostly for low acuity, self-limiting illnesses.32 This hypothesis is further supported in our study with a large increase in male FA visits seen in the 19-year-old age group. To our knowledge, literature on frequent medical consultations among conscripted male adolescents in primary care is scarce. This subgroup of adolescents is subject to unique challenges; more research is required to ascertain the causes and impact that conscripted national service has on FA in the primary care setting and strategies to decrease FA in this population group.
Lower socioeconomic status, as measured by the receipt of means-tested governmental subsidies, was significantly associated with FA in our study. Most other frequent attender studies have found similar associations.1 3 6 11 22 Socioeconomic status is complex and multifaceted, encompassing multiple factors such as parental marital status, housing and place of residence, rurality, education levels, occupation and income, social class and economic status.10 Although the association between low socioeconomic status and FA is clear, the precise relationships between each of these factors and their contributing roles to FA are still not well established.10
Clinical presentation profile
The presence of mental health issues has been shown to have the strongest association with FA among all factors, with up to 89% of studies reporting a positive correlation.25 Our results revealed that FAs were more likely to have received at least one psychiatric diagnosis and be referred to a psychiatrist compared with non-FAs. This suggests that FAs are more likely to have underlying psychiatric conditions and are more likely to require escalation of care to mental health specialists. Despite this, FAs were less likely to present to primary care with mental health complaints. Instead, they presented frequently with acute physical complaints such as upper respiratory tract infections, headaches and enteritis. This pattern of presentation has also been highlighted in other adolescent frequent attender studies, where the most common presentations were respiratory, gastrointestinal and a range of ill-defined symptoms.3 23
One plausible explanation for this pattern of presentation seen in adolescents is somatisation, which is defined as the manifestation of psychological distress by the presentation of physical symptoms that cannot be explained by medical reasons.33 Somatic complaints are a result of reluctance or the inability to verbalise emotional distress, which is commonly encountered in adolescents.33 The reported primary care prevalence of somatisation in adolescents is as high as 31%.34 However, detection of somatisation requires active screening for psychosocial issues, which is time-consuming and may be impractical in busy primary care settings.
Mental disorders and chronic stress have also been linked to changes in cellular immunity, which leads to decreased immune function increasing susceptibility to infections and illnesses.35 36 Thus, the acute physical symptoms that adolescents frequently present with may be partially explained by underlying physiological causes.
Our study has identified multiple gaps concerning the relationship between FA, possible somatisation and mental and physical health among adolescents. The low level of help-seeking behaviour for mental health concerns has resulted in great difficulty in identifying at-risk adolescents with mental health issues. This results in missed opportunities for early intervention which may further contribute to the looming global crisis in adolescent mental health.37 Given the strong correlation between FA and mental health disorders, interventional studies targeting high-risk adolescents are needed to determine if FA status can be used as an indicator for identifying unmet mental health needs in this population. It is also unclear whether the pattern of presentation highlighted above was due to somatisation or true physiological causes. To explore this, we suggest actively screening for somatisation using screening tools validated for local populations38 and consider including biomarker investigations such as proinflammatory cytokines in future adolescent frequent attender studies.
Healthcare utilisation patterns
In our study, adolescent FAs had higher healthcare utilisation in terms of a disproportionate number of clinic attendances, longer annual medical leave certification duration and more referrals to psychiatrists and emergency departments. In addition to higher healthcare costs, there are other indirect costs to consider such as productivity loss from increased absence from school or work and future morbidity costs from unmet psychosocial needs.
Overall, FAs were more likely to have been prescribed potentially addictive medication compared with non-FAs. It has been suggested that abuse of prescription medication in Singapore is common with its prevalence similar to the use of recreational drugs.39 Commonly abused prescription medications include benzodiazepines, codeine-based medication, methylphenidate, baclofen and gabapentin,39 most of which are available at the polyclinics. There are strong correlations between drug abuse and FA in adult studies.25 The frequency of potentially addictive medication prescribed in our study was low (<1% except for dextromethorphan). This was expected because addictive medication such as benzodiazepines is not as frequently used in adolescents compared with adults,40 possibly due to local conservative prescribing patterns as well as strict governmental prescription regulations for these medications.41 Moreover, conclusions about prescription medication abuse cannot be drawn from our study as our results only reflect medication prescription trends with no data on actual abuse.
Definition of FA
The definition of FA is variable in the current literature, which has hampered comparisons between study populations.1 By applying the ‘top 10th percentile of attendees’ definition in our study population of multiethnic Asians, adolescent FA corresponded with having ≥4 primary care consultations annually. In contrast, Shukla et al (2020) suggested using the definition of at least 10 visits annually in their systematic review.25 However, this suggested definition was based on adult studies. In current adolescent studies, the annual visit frequency cut-off ranges from 1–4 visits.3 23 42 The difference between Shukla et al’s suggested cut-off visit frequency and our study’s findings may also be explained by differences in healthcare settings. Patients in Singapore are not restricted to a single primary care clinic and are free to visit any public or private clinic of their choice. The wide availability of primary care services and the relatively small geographical size of Singapore further contribute to the ease of visiting different clinics. Therefore, the true annual visit frequency for FAs may be higher than what is reported in our study when considering possible additional visits to other primary care clinics.
For future retrospective studies on adolescent FAs, we recommend using the top 10th percentile definition for greater ease of comparison across different patient populations and healthcare settings. For prospective studies which require real-time identification of adolescent FAs, we suggest using the cut-off of ≥4 annual visits based on our findings.
Strengths and limitations
To our knowledge, our study is the first large multiethnic Asian study describing the profile and healthcare utilisation patterns of adolescent FAs in primary care. Our study included a large number of adolescents and involved data from a third of the public primary care population of Singapore.
Our study had limitations. Being a retrospective database analysis study, the variables available for analysis were limited to the data recorded in the electronic medical records. Other sociodemographic factors (type of residence, family income, parental employment and education levels) and important psychosocial factors (parental separation, presence of family conflict, child abuse and neglect, delinquent behaviour and bullying by peers) were not available for analysis. The financial aid status of patients used as a surrogate of socioeconomic status in our study may also not be representative of their true socioeconomic status. Receipt of the financial aid programmes are application-based; not all patients from lower socioeconomic statuses may have applied for financial aid. Moreover, database studies are subject to coding inaccuracy and may result in misclassification bias. Due to internal database coding descriptions, certain medical diagnoses such as ‘backache’, ‘migraine’ and ‘dysmenorrhea’, which some clinicians consider acute conditions, were classified as chronic conditions. Additionally, over a quarter of all visits in our study were attributed to preventive care. This may be over-represented due to a large number of diagnosis codes recorded for preventive health services received during acute or chronic presentations such as ‘Health education’, ‘Other screening/Growth monitoring Questionnaires’ or ‘Medical examination/investigations’. Furthermore, the period of study was during the COVID-19 pandemic, with shifting protocols of patient management throughout the study period. Patients were encouraged to present to the clinics for COVID-19 testing, which may account for the large number of respiratory conditions seen in both FAs and non-FAs. There was also mandatory issuance of a 5-day medical leave certification for all patients presenting with upper respiratory tract symptoms, which may confound the data on annual medical leave certification duration. Additionally, presentations for infectious diseases and respiratory illnesses may have surged during the pandemic, but we did not specifically investigate these disease categories in our analysis as they were not among the predetermined hypotheses for our study. Finally, the frequency of potentially addictive medication prescribed was low (<1% except for dextromethorphan), and hence, the conclusions regarding this variable should be interpreted with caution. Only the frequency of each medication was recorded, and the actual quantity prescribed was not known.
Conclusion
Our study has described the sociodemographic profile, clinical presentation and healthcare utilisation patterns of adolescent FAs attending polyclinics in Singapore, as well as the factors associated with adolescent FA in the local context.
Adolescent FA was associated with increasing age, non-Chinese ethnicity, lower socioeconomic status and underlying psychiatric conditions. FAs presented with acute physical complaints more frequently than psychiatric symptoms, had longer annual medical leave certification, and had greater healthcare utilisation indicated by a higher frequency of clinic visits and more referrals to the emergency department and psychiatry clinics.
Further research is recommended to explore the reasons for FA, the relationships between the factors associated with FA and methods of early identification of adolescent FAs who may have underlying psychiatric conditions.
supplementary material
Acknowledgements
The authors would like to acknowledge Wai Keong Aau from the SingHealth Department of Research for services rendered in data extraction and handling.
Footnotes
Funding: This research is supported by the National Medical Research Council (NMRC) through the SingHealth PULSES II Centre Grant (CG21APR1013).
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-080429).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Patient and public involvement: Patients and/or the public were involved in the design, conduct, reporting or dissemination plans of this research. Refer to the Methods section for further details.
Ethics approval: This study was granted ethics exemption by the SingHealth Centralised Institutional Review Board (Ref: 2022/2072) as the data was deidentified by a trusted third party prior to analysis by the study team.
Contributor Information
Jeremy Wei Mei Koh, Email: jeremy.koh.w.m@singhealth.com.sg.
Ngiap Chuan Tan, Email: tan.ngiap.chuan@singhealth.com.sg.
Jeremy Wei Song Choo, Email: jeremy.choo.w.s@singhealth.com.sg.
Helen Yu Chen, Email: helen.chen.y@singhealth.com.sg.
Yi Ling Eileen Koh, Email: eileen.koh.y.l@singhealth.com.sg.
Angelina Su Yin Ang, Email: angelina.ang.s.y@singhealth.com.sg.
Vicknesan Jeyan Marimuttu, Email: vicknesan.jeyan.marimuttu@singhealth.com.sg.
Ryan Song Lian Wu, Email: ryan.wu.s.l@singhealth.com.sg.
Sharon Cohan Sung, Email: sharon.sung@duke-nus.edu.sg.
Chirk Jenn Ng, Email: ng.chirk.jenn@singhealth.com.sg.
Data availability statement
Data are available upon reasonable request.
References
- 1.Vedsted P, Christensen MB. Frequent attenders in general practice care: a literature review with special reference to methodological considerations. Public Health. 2005;119:118–37. doi: 10.1016/j.puhe.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 2.Neal RD, Heywood PL, Morley S, et al. Frequency of patients’ consulting in general practice and workload generated by frequent attenders: comparisons between practices. Br J Gen Pract. 1998;48:895–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Vila M, Kramer T, Obiols JE, et al. Adolescents who are frequent attenders to primary care: contribution of psychosocial factors. Soc Psychiatry Psychiatr Epidemiol. 2012;47:323–9. doi: 10.1007/s00127-010-0326-8. [DOI] [PubMed] [Google Scholar]
- 4.Taylor RE, Marshall T, Mann A, et al. Insecure attachment and frequent attendance in primary care: a longitudinal cohort study of medically unexplained symptom presentations in ten UK general practices. Psychol Med. 2012;42:855–64. doi: 10.1017/S0033291711001589. [DOI] [PubMed] [Google Scholar]
- 5.Patel S, Kai J, Atha C, et al. Clinical characteristics of persistent frequent attenders in primary care: case-control study. Fam Pract. 2015;32:624–30. doi: 10.1093/fampra/cmv076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robles R, Gili M, Gelabert J, et al. Sociodemographic and psychopathological features of frequent attenders in Primary Care. Actas Esp Psiquiat. 2009;37:320–5. [PubMed] [Google Scholar]
- 7.Gili M, Luciano JV, Serrano MJ, et al. Mental disorders among frequent attenders in primary care: a comparison with routine attenders. J Nerv Ment Dis. 2011;199:744–9. doi: 10.1097/NMD.0b013e31822fcd4d. [DOI] [PubMed] [Google Scholar]
- 8.Ferrari S, Galeazzi GM, Mackinnon A, et al. Frequent attenders in primary care: impact of medical, psychiatric and psychosomatic diagnoses. Psychother Psychosom. 2008;77:306–14. doi: 10.1159/000142523. [DOI] [PubMed] [Google Scholar]
- 9.Smits FTM, Brouwer HJ, ter Riet G, et al. Epidemiology of frequent attenders: a 3-year historic cohort study comparing attendance, morbidity and prescriptions of one-year and persistent frequent attenders. BMC Public Health. 2009;9:36. doi: 10.1186/1471-2458-9-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scaife B, Gill P, Heywood P, et al. Socio-economic characteristics of adult frequent attenders in general practice: secondary analysis of data. Fam Pract. 2000;17:298–304. doi: 10.1093/fampra/17.4.298. [DOI] [PubMed] [Google Scholar]
- 11.Strömbom Y, Magnusson P, Karlsson J, et al. Health-related quality of life among frequent attenders in Swedish primary care: a cross-sectional observational study. BMJ Open. 2019;9:e026855. doi: 10.1136/bmjopen-2018-026855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jorm AF. Mental health literacy: empowering the community to take action for better mental health. Am Psychol. 2012;67:231–43. doi: 10.1037/a0025957. [DOI] [PubMed] [Google Scholar]
- 13.Ma J, Wang Y, Stafford RS. U.S. adolescents receive suboptimal preventive counseling during ambulatory care. J Adolesc Health. 2005;36:441. doi: 10.1016/j.jadohealth.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 14.Tylee A, Haller DM, Graham T, et al. Youth-friendly primary-care services: how are we doing and what more needs to be done? Lancet. 2007;369:1565–73. doi: 10.1016/S0140-6736(07)60371-7. [DOI] [PubMed] [Google Scholar]
- 15.Lawrence RS, Gootman JA, Sim LJ. Adolescent health services: Missing opportunities. National Academies Press; 2009. [PubMed] [Google Scholar]
- 16.World Health Organisation Making health services adolescent friendly developing national quality standards for adolescent-friendly health services. 2012. https://iris.who.int/bitstream/handle/10665/75217/9789241503594_eng.pdf;jsessionid=7F3E38FB5F96FE47AA50C8F2BEA403CE?sequence=1 Available.
- 17.Pang S, Liu J, Mahesh M, et al. Stigma among Singaporean youth: a cross-sectional study on adolescent attitudes towards serious mental illness and social tolerance in a multiethnic population. BMJ Open. 2017;7:e016432. doi: 10.1136/bmjopen-2017-016432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wolraich M, Felice M, Drotar D. The classification of child and adolescent mental diagnoses in primary care: diagnostic and statistical manual for primary care (DSM-PC) child and adolescent version. 1996. [DOI]
- 19.Yassaee AA, Hargreaves DS, Chester K, et al. Experience of primary care services among early adolescents in England and Association With Health Outcomes. J Adolesc Health. 2017;60:388–94. doi: 10.1016/j.jadohealth.2016.09.022. [DOI] [PubMed] [Google Scholar]
- 20.Hargreaves DS, Elliott MN, Viner RM, et al. Unmet health care need in US adolescents and adult health outcomes. Pediatrics. 2015;136:513–20. doi: 10.1542/peds.2015-0237. [DOI] [PubMed] [Google Scholar]
- 21.Kramer T, Iliffe S, Murray E, et al. Which adolescents attend the GP? Br J Gen Pract. 1997;47:327. [PMC free article] [PubMed] [Google Scholar]
- 22.Kekkonen VK, Kivimäki P, Valtonen H, et al. Psychosocial problems in adolescents associated with frequent health care use. Fam Pract. 2015;32:305–10. doi: 10.1093/fampra/cmu090. [DOI] [PubMed] [Google Scholar]
- 23.Garralda ME, Bowman FM, Mandalia S. Children with psychiatric disorders who are frequent attenders to primary care. Eur Child Adolesc Psychiatry. 1999;8:34–44. doi: 10.1007/s007870050081. [DOI] [PubMed] [Google Scholar]
- 24.Lim CG, Ong SH, Chin CH, et al. Child and adolescent psychiatry services in Singapore. Child Adolesc Psychiatry Ment Health . 2015;9:7. doi: 10.1186/s13034-015-0037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shukla DM, Faber EB, Sick B. Defining and characterizing frequent attenders: Systematic literature review and recommendations. J Patient Cent Res Rev. 2020;7:255–64. doi: 10.17294/2330-0698.1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ministry of Health Singapore Primary healthcare services. https://www.moh.gov.sg/home/our-healthcare-system/healthcare-services-and-facilities/primary-healthcare-services n.d. Available.
- 27.Singhealth Duke-NUS Academic Medical Centre Singhealth annual report 2021-2022. 2022. https://www.singhealth.com.sg/about-singhealth/newsroom/Documents/SingHealth%20Annual%20Report%2021-22_facts_and_figures.pdf Available.
- 28.World Health Organization . International statistical classification of diseases and related health problems. World Health Organization; 2011. [Google Scholar]
- 29.Al-Saffar MN, Hayhoe BW, Harris MJ, et al. Children as frequent attenders in primary care: a systematic review. BJGP Open. 2020;4:1–8. doi: 10.3399/bjgpopen20X101076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nordin JD, Solberg LI, Parker ED. Adolescent primary care visit patterns. Ann Fam Med. 2010;8:511–6. doi: 10.1370/afm.1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ng DCC, Lew YJ, Koh EYL, et al. Sickness certification in Singapore’s public primary healthcare system: A cross-sectional analysis. Proc Singap Healthc. 2018;27:167–74. doi: 10.1177/2010105817741661. [DOI] [Google Scholar]
- 32.Paul P, Heng BH, Seow E, et al. Predictors of frequent attenders of emergency department at an acute general hospital in Singapore. Emerg Med J. 2010;27:843–8. doi: 10.1136/emj.2009.079160. [DOI] [PubMed] [Google Scholar]
- 33.Karkhanis DG, Winsler A. Somatization in Children and Adolescents: practical implications. J Indian Assoc Child Adolesc Ment Health. 2016;12:79–115. doi: 10.1177/0973134220160105. [DOI] [Google Scholar]
- 34.Vesterling C, Schütz-Wilke J, Bäker N, et al. Epidemiology of somatoform symptoms and disorders in childhood and adolescence: A systematic review and meta-analysis. Health Soc Care Community. 2023;2023:1–16. doi: 10.1155/2023/6242678. [DOI] [Google Scholar]
- 35.Herbert TB, Cohen S. Depression and immunity: a meta-analytic review. Psychol Bull. 1993;113:472–86. doi: 10.1037/0033-2909.113.3.472. [DOI] [PubMed] [Google Scholar]
- 36.Robles TF, Glaser R, Kiecolt-Glaser JK. Out of balance a new look at chronic stress, depression, and immunity. Curr Dir Psychol Sci. 2015;14:111. doi: 10.1111/j.0963-7214.2005.00345.x. [DOI] [Google Scholar]
- 37.Benton TD, Boyd RC, Njoroge WFM. Addressing the global crisis of child and adolescent mental health. JAMA Pediatr. 2021;175:1108–10. doi: 10.1001/jamapediatrics.2021.2479. [DOI] [PubMed] [Google Scholar]
- 38.Ang SH, Tan JSK, Lee J, et al. Screening for somatisation in an Asian children’s hospital emergency setting. Ann Acad Med Singap. 2022;51:507–9. doi: 10.47102/annals-acadmedsg.2022101. [DOI] [PubMed] [Google Scholar]
- 39.Chan WL, Dargan PI, Haynes CM, et al. Misuse of prescription medicines is as prevalent as the use of recreational drugs and novel psychoactive substances in Singapore: an unrecognised public health issue? Sing Med J. 2022;63:572–6. doi: 10.11622/smedj.2020024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Witek MW, Rojas V, Alonso C, et al. Review of benzodiazepine use in children and adolescents. Psychiatr Q. 2005;76:283–96. doi: 10.1007/s11126-005-2982-5. [DOI] [PubMed] [Google Scholar]
- 41.Ministry of Health Singapore . Prescribing of Benzodiazepines. Singapore: 2008. [Google Scholar]
- 42.Shraim M, Blagojevic-Bucknall M, Mallen CD, et al. Repeated primary care consultations for non-specific physical symptoms in children in UK: a cohort study. 2014. http://www.biomedcentral.com/1471-2296/15/195 Available. [DOI] [PMC free article] [PubMed]