Abstract
Most syphilitic aneurysms involve the ascending aorta. Those involving the descending aorta are less common, and those involving the abdominal aorta are unusual. Rarer yet, we present the case of a 40-year-old man with HIV and a history of syphilis with a thoracoabdominal aneurysm. The patient underwent antiretroviral therapy before elective open repair. His postoperative course was uneventful, and he was discharged home. Pathology demonstrated medial necrosis. Postoperatively, he was seen well in our multidisciplinary aorta center clinic. Today's vascular surgeons should be cognizant of cardiovascular syphilis. Successful care requires awareness of atypical presentations in addition to multispecialty care.
Keywords: Aortic aneurysm, Thoracoabdominal aneurysm repair, Syphilitic aneurysm, Cardiovascular syphilis
Syphilitic aortitis is an infrequently encountered yet clinically significant manifestation of tertiary syphilis. Historically considered a leading cause of aortic aneurysms,1 syphilitic aortitis has experienced a resurgence in recent years due to the reemergence of syphilis as a global health concern.2
Nonsyphilitic mycotic aneurysms result from an inflammatory reaction that activates matrix metalloproteinases. The spirochete Treponema pallidum, early in initial infection, will localize to the aortic wall, and subsequently an obliterative endarteritis of the vasa vasorum leads to medial necrosis and predisposes to aneurysmal disease.3 In humans, the infrarenal aorta ceases to be supplied by the vasa vasorum and derives its oxygen by diffusion. Because of this, the abdominal aorta is considered less likely to be affected by syphilitic aneurysms.4
Indeed, a 2018 review suggested that 57.4% of syphilitic aortic aneurysms were limited to the ascending aorta, and 80.9% involved the ascending aorta with or without another portion of the aorta.1 Only 11.3% were reported to affect the aorta distal to the arch. Of these, there was only one reported case of syphilitic thoracoabdominal aortic aneurysm (TAAA).5 Here, we present the case of a 40-year-old man with HIV and a history of syphilis who was treated surgically for a symptomatic and enlarging TAAA. He has consented to publication of his case.
Case report
The patient was a 40-year-old man with HIV presenting with abdominal pain. A computed tomography scan demonstrated the aortic aneurysm, spanning from zone IV to IX. Family history was negative for aneurysm, and genetic testing was negative for aneurysm-related genes. He smoked three or four cigarettes per day. Three months before presentation, he was diagnosed with syphilis after noticing palmar lesions. At that time, he underwent therapy with 2.4 million U penicillin G weekly for 3 weeks, which is the standard treatment for late latent syphilis.6 He was unable to recall the primary infection. When he presented to us 3 months after his diagnosis and treatment of syphilis, his rapid plasma regain titer measured 1:2. It is not uncommon in patients with HIV for the rapid plasma regain to remain reactive with low titers, even after successful treatment, a phenomenon referred to as a serofast reaction.6 Operative intervention was deferred given poorly controlled HIV. His syphilis was surveilled and HIV managed by an infectious disease specialist. After a 6-month surveillance interval, he was found to have expansion in both the thoracic and abdominal components of his aneurysm from 3.6 cm to 4.3 cm and from 5.4 cm to 6.5 cm, respectively (Fig 1). At the time of his operation, HIV RNA levels were undetectable.
Fig 1.
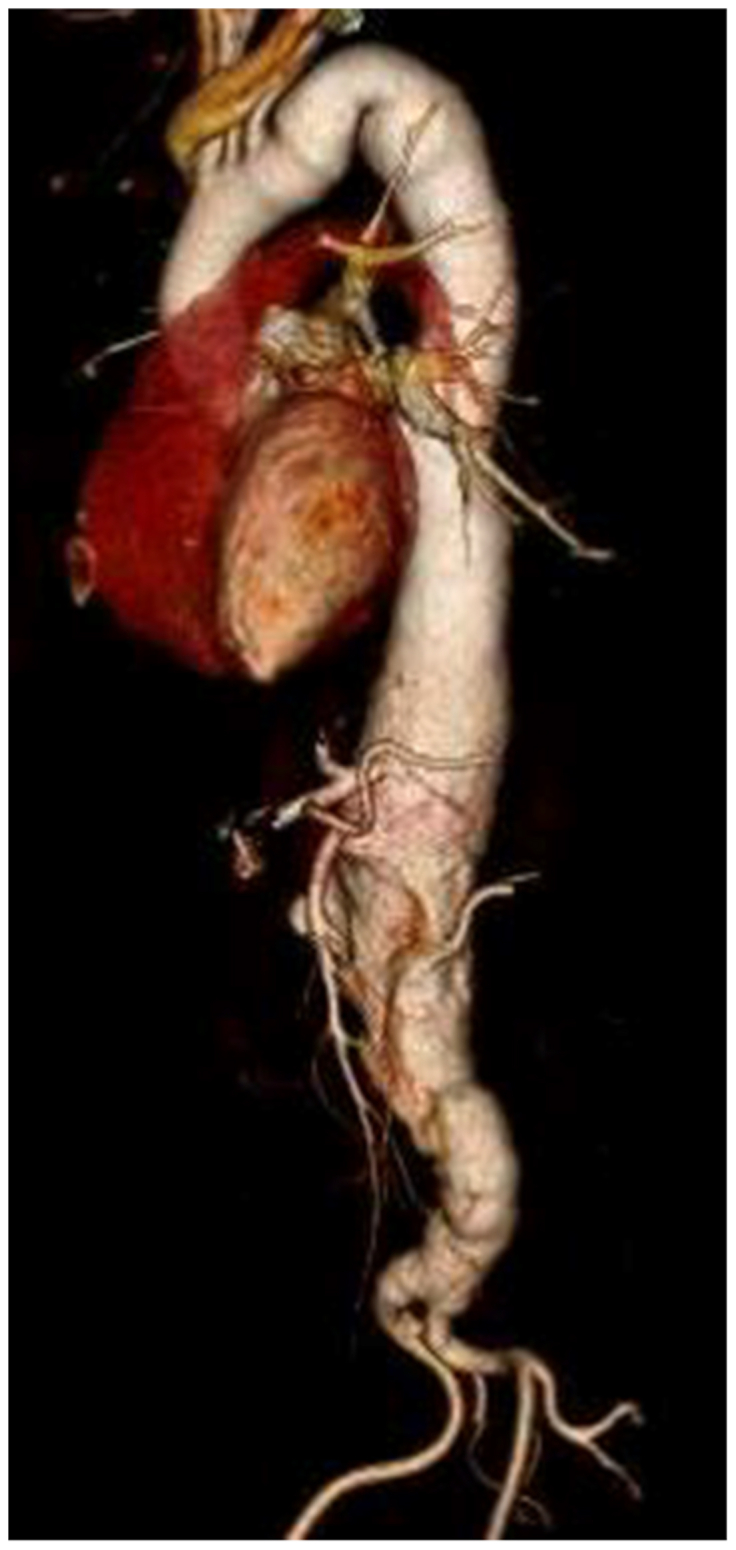
Three-dimensional reconstruction of our patient's syphilitic thoracoabdominal aneurysm before repair.
Operative strategy
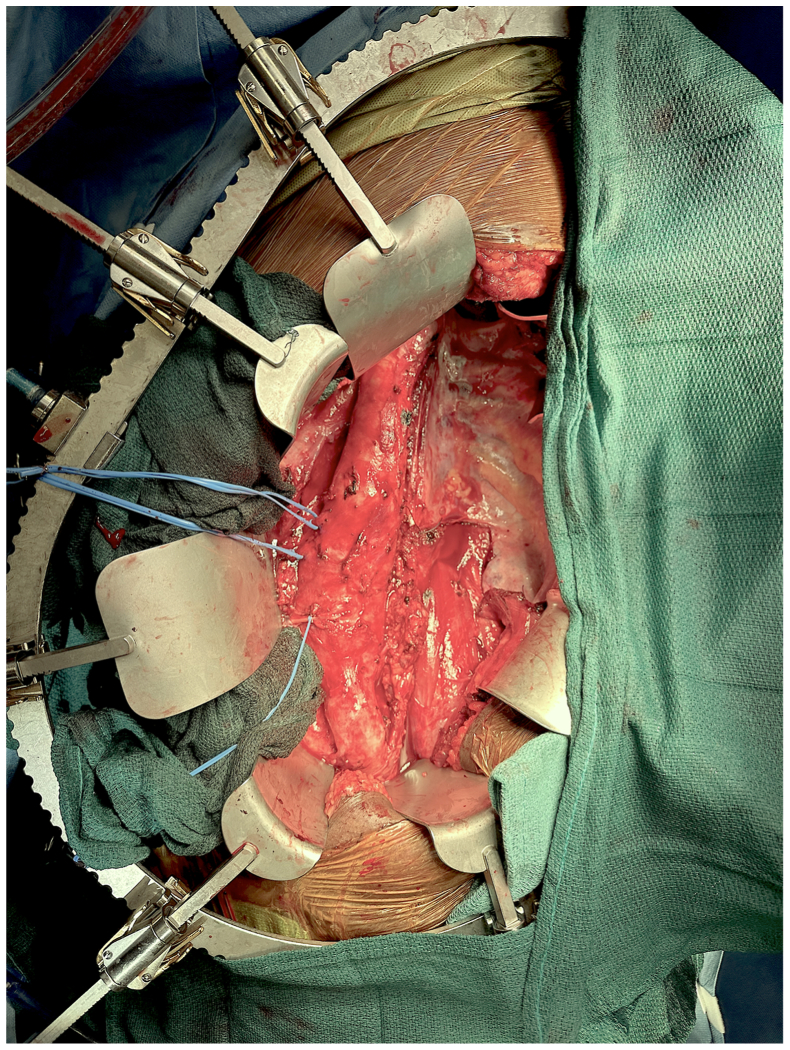
After a lumbar drain was placed, central venous access was established, and invasive monitoring was accomplished with a Swan-Ganz catheter. Neuromonitoring was configured. General anesthesia was induced via a double-lumen endotracheal tube, and the patient was positioned in right lateral decubitus. The operative field was prepared from chin to knees. A sixth interspace thoracotomy was carried inferiorly in a paramedian fashion. Retroperitoneal exposure of the abdominal aorta was accomplished, and the diaphragm was divided circumferentially. The thoracic aorta was exposed by division of the inferior pulmonary ligament. With adequate exposure established (Fig 2), the patient was placed on left heart bypass and cooled to 30°C to 32°C per institutional protocol. A rifampin-soaked 28-mm Gelweave Coselli TAAA (Terumo, Somerset, NJ) graft was used. The proximal anastomosis was undertaken in an end-to-end fashion. The aorta just distal to this was resected and passed off the field for Gram stain, culture, and pathologic analysis. The celiac, superior mesenteric, and renal arteries were serially bypassed. Prior to their respective bypasses, cold crystalloid perfusate (4°C lactated Ringer solution with 25 g/L of mannitol and 1 g/L methylprednisolone) was administered to the kidneys via the native renal arteries. An end-to-end anastomosis was performed in zone IX (Fig 3).
Fig 2.
Operative exposure of syphilitic thoracoabdominal aortic aneurysm (TAAA).
Fig 3.
Repair of the thoracoabdominal aortic aneurysm (TAAA) with rifampin-soaked Dacron.
The patient suffered a transient acute kidney injury with an increase in serum creatinine to a peak of 1.89 mg/dL from a baseline of 1.23 mg/dL. He had a mild, hemodynamically insignificant tachycardia that did not preclude safe discharge. Otherwise, there was no organ dysfunction or failure perioperatively. The lumbar drain was removed on postoperative day 1 after demonstration of normal use of his lower extremities. Bowel function returned on postoperative day 2, and subsequently he tolerated a serially advanced diet. He was discharged in ambulatory condition on postoperative day 7. The final pathology suggested cystic medial necrosis and atherosclerosis. Cultures from this specimen did not grow any organisms. One month postoperatively, he was seen for follow-up and found to be well. He underwent imaging demonstrating a patent graft (Fig 4). He follows with an infectious disease specialist for syphilis surveillance and management of HIV.
Fig 4.

Three-dimensional reconstruction of our patient's syphilitic thoracoabdominal aneurysm 1 month postoperatively.
Discussion
Today, syphilis is an increasing public health concern. According to the most recent data from the Centers for Disease Control and Prevention, the incidence of primary and secondary syphilis has increased every year since its nadir in 2000 and 2001.2 Cardiovascular syphilis is a manifestation of tertiary syphilis and develops typically after 10 to 25 years. It may affect the aortic valve, coronary ostia, and the aorta. Overall, syphilitic aortitis affects approximately 10% of untreated cases of syphilis.7 Coinfection with HIV differentiates this era of syphilis, and their effects on each other are known to be synergistic.8 This factor may or may not account for atypical manifestations of cardiovascular syphilis. One case-control study suggested a higher incidence of cardiovascular syphilis among patients also seropositive for HIV, and additionally a faster onset and at a younger age than HIV-seronegative patients.9
In a young patient with limited tobacco exposure, no family history of aneurysm, no identified genetic predisposition, and no history of hypertension or related aortic pathology, syphilis is the most likely etiology of this aneurysm. Although we had the luxury of a preexisting diagnosis, for those cases in which a diagnosis of syphilis did not precede operation, gross identification of syphilitic aortitis has been well-described by Roberts et al.10,11 Intraoperative examination of our patient's aorta was consistent with their gross descriptions of thickened yet weak walls with involvement of the total surface area, and pathologic examination confirmed classic findings of medial necrosis without demonstration of the organism.4,12
An increasing number of cases of syphilitic aneurysms are being repaired via an endovascular approach,7,13, 14, 15 the first being described in 2003 after open arch reconstruction.13 Regarding the treatment of mycotic aneurysms, it is generally agreed that endovascular repair should await successful management of the infectious process with a course of antibiotics. Infection of an endovascular device is a sporadic occurrence and is reported usually in situations where the device was implanted on an emergency basis in an infected field.14,16,17 Although its sensitivity and specificity are currently unknown, some authors have reported the use of positron emission tomography combined with computed tomography to exclude active vasculitis before endovascular repair of a patient's syphilitic aneurysm.18,19 Given that most syphilitic aneurysms affect the ascending aorta, endovascular repairs have limited use in the treatment of syphilitic aneurysms as a whole. However, once the infection is treated successfully, surgical repair of syphilitic aneurysms could be approached similarly to aneurysms of other etiologies. In our patient's case, the abdominal aneurysm met the criteria for repair on size alone. Additionally, the alarming growth rate for both the thoracic and abdominal components of the aneurysm warranted repair.
Conclusions
A syphilitic aneurysm sparing the ascending aorta and affecting the descending and abdominal aorta is exceedingly rare. We present a case with a favorable outcome after open repair. The rising incidence in syphilis may result in increasing operative interventions for related aortic disease. The care of these patients is multi-faceted, involving infectious disease experts, cardiac surgeons, vascular and endovascular surgeons, and case management specialists.
Disclosures
M.F. is a member of the endovascular division of the vascular advisory board at Terumo Aortic.
Acknowledgments
The authors thank Charles S. Roberts, MD, for expertise in aortic pathology, particularly that which is associated with syphilis and John F. Eidt, MD, for style.
Footnotes
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Yuan S.M. Syphilitic aortic aneurysm. Z Rheumatol. 2018;77:741–748. doi: 10.1007/s00393-018-0519-1. [DOI] [PubMed] [Google Scholar]
- 2.Syphilis. [Internet]. Centers for Disease Control and Prevention (CDC) 2024.. https://www.cdc.gov/std/statistics/2022/overview.htm#Syphilis
- 3.Duncan J.M., Cooley D.A. Surgical considerations in aortitis. Part III: syphilitic and other forms of aortitis. Tex Heart Inst J. 1983;10:337–341. [PMC free article] [PubMed] [Google Scholar]
- 4.Heggtveit H.A. Syphilitic aortitis. A clinicopathologic autopsy study of 100 cases, 1950 to 1960. Circulation. 1964;29:346–355. doi: 10.1161/01.cir.29.3.346. [DOI] [PubMed] [Google Scholar]
- 5.Kisis K., Krievins D., Gedins M., Savlovskis J., Ezite N., Ivanova P. Patient with syphilitic thoracic and abdominal aortic aneurysms. Acta Chir Latv. 2010;10:131–133. [Google Scholar]
- 6.Trovato E., Tognetti L., Campoli M., Cinotti E., Rubegni P. Syphilis diagnosis and treatment: state of the art. EMJ Dermatology. 2021;9(Suppl 4):1–11. [Google Scholar]
- 7.Yasuda S., Imoto K., Uchida K., et al. Stent-graft implantation for clinically diagnosed syphilitic aortic aneurysm in an HIV-infected patient. Ann Thorac Cardiovasc Surg. 2014;20(Suppl):862–866. doi: 10.5761/atcs.cr.12.02211. [DOI] [PubMed] [Google Scholar]
- 8.Lynn W.A., Lightman S. Syphilis and HIV: a dangerous combination. Lancet Infect Dis. Jul 2004;4:456–466. doi: 10.1016/S1473-3099(04)01061-8. [DOI] [PubMed] [Google Scholar]
- 9.Maharajan M., Kumaar G.S. Cardiovascular syphilis in HIV infection: a case-control study at the institute of sexually transmitted diseases, Chennai, India. Sex Transm Infect. 2005;81:361. doi: 10.1136/sti.2004.013599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roberts W.C., Bose R., Ko J.M., Henry A.C., Hamman B.L. Identifying cardiovascular syphilis at operation. Am J Cardiol. 2009;104:1588–1594. doi: 10.1016/j.amjcard.2009.06.071. [DOI] [PubMed] [Google Scholar]
- 11.Roberts C.S., Roberts W.C. Diagnosing aortic syphilis. SAVE Proc. 2022;35:822–823. doi: 10.1080/08998280.2022.2104528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roberts W.C., Ko J.M., Vowels T.J. Natural history of syphilitic aortitis. Am J Cardiol. 2009;104:1578–1587. doi: 10.1016/j.amjcard.2009.07.031. [DOI] [PubMed] [Google Scholar]
- 13.Goldstein B., Carroccio A., Ellozy S.H., et al. Combined open and endovascular repair of a syphilitic aortic aneurysm. J Vasc Surg. 2003;38:1422–1425. doi: 10.1016/s0741-5214(03)00943-1. [DOI] [PubMed] [Google Scholar]
- 14.Li W., Yin X.J., Liu H.Y., Yang R. Syphilitic aortic aneurysm with a pulmonary lesion: a case report and literature view. SpringerPlus. 2016;5:1725. doi: 10.1186/s40064-016-3397-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chitragari G., Laux A.T., Hicks T.D., Davies M.G., Haidar G.M. Rare presentation of a syphilitic aneurysm of the infrarenal aorta with contained rupture. Ann Vasc Surg. 2018;47:279.e13–279.e17. doi: 10.1016/j.avsg.2017.07.041. [DOI] [PubMed] [Google Scholar]
- 16.Hiratzka L.F., Bakris G.L., Beckman J.A., et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Catheter Cardiovasc Interv. 2010;76:E43–E86. doi: 10.1002/ccd.22537. [DOI] [PubMed] [Google Scholar]
- 17.Luo C.M., Chan C.Y., Chen Y.S., Wang S.S., Chi N.H., Wu I.H. Long-term outcome of endovascular treatment for mycotic aortic aneurysm. Eur J Vasc Endovasc Surg. 2017;54:464–471. doi: 10.1016/j.ejvs.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 18.Ghazy T., Matschke K., Kappert U. A monstrous aneurysm of the descending aorta as a sole manifestation of tertiary syphilis treated endovascularly. Eur Heart J. 2011;32:2411. doi: 10.1093/eurheartj/ehr095. [DOI] [PubMed] [Google Scholar]
- 19.De Rango P., Vittorio De Socio G., Silvestri V., Simonte G., Verzini F. An unusual case of epigastric and back pain expanding descending thoracic aneurysm resulting from tertiary syphilis diagnosed with positron emission tomography. Circ Cardiovasc Imaging. 2013;6:1120–1121. doi: 10.1161/CIRCIMAGING.113.001136. [DOI] [PubMed] [Google Scholar]