Abstract
Here we present a case of atypical manifestation of Sporothrix schenkii infection where the patient complained solely of lymphadenopathy without any prior noticeable skin lesions. A Thai female who had been working in Malaysia presented to a healthcare facility with a three-month history of progressively larger and more painful lymphadenopathy at her right chin.
Keywords: Sporotrichosis, Lymphadenpathy, Sporothrix
Highlights
-
•
Sporothrix schenkii can result in diverse illnesses depending on host and route.
-
•
Sporotrichosis was rarely presented with isolated lymphadenopathy.
-
•
Itraconazole is a drug of choice of Sporotrichosis.
Case report
A 44-year-old Thai female patient who had been working in Malaysia for eight years reported a three-month history of symptoms starting with a small palpable soft mass at her right chin. The mass was approximately one centimeter in size when first noticed and did not impose any other symptoms such as pain or unpleasant feelings such as tingling sensation, tightness, or foreign body sensation. She denied fever, toothache, headache, upper respiratory tract symptoms, or facial pain at that time.
The mass gradually grew over a month into a noticeable lump approximately seven cm in size next to her right mandibular angle (Fig. 1). The mass became rubbery in consistency and appeared mildly erythematous in appearance. She reported intermittent excruciating pain with a pain score of eight out of ten on the Numerical Rating Scale (NRS) for pain intensity, lasting through the majority of her waking hours, which significantly affected her ability to work and carry out daily activities. Oral analgesics were reported to be ineffective in mitigating pain. The patient decided to visit a local assistance center and was diagnosed with an infection of her oral cavity. She was prescribed two weeks of antibiotics. From the way that she described the pill and how it was taken 2 times a day, we presumed it was amoxicillin-clavulanic acid.
Fig. 1.
Side view of the mass at right mandibular angle.
Nearing the end of the prescribed course, the patient clinically deteriorated. She developed fever with chills and reported worsening of both localized pain and dysphagia, leading to significant appetite loss. The patient then visited a hospital in Malaysia and a computer tomography (CT) scan of the neck was performed. The result showed multiple matted necrotic lymph nodes across the C2 to C5 level on the right, strung to intra-parotid nodes. The largest nodes were measured at 3.2 × 1.5 cm at the upper neck. Parotid glands and skeletal structures were normal. No abscesses were seen.
The patient then returned to Thailand for further investigation. At a hospital in Thailand, fine needle aspiration (FNA) was done to her right parotid gland which only yielded benign ductal epithelial and necrotic cells. No malignant cells were observed. She was then referred to a medical center in Northern Thailand.
More information regarding her past and personal history was obtained. The patient was born and raised in the Northern part of Thailand. She then moved to work as a housekeeper in Malaysia for eight years. Three months before her symptoms developed, she began working at a shrimp farm where she oversaw cleaning the vicinity dealing with mostly leaves and soil. She was not involved in the process of crustacean care. Her accommodation also housed eight fully vaccinated cats. She denied prior underlying diseases and was not on any medication. She also denied smoking, alcohol drinking, and illicit drug use.
Upon physical examination, her vital signs were within normal limits. Her body temperature was 36.5 °C, blood pressure 117/80 mmHg, pulse rate 98 beats per minute, and peripheral oximeter reading of 97 % with room air. She was well overall besides general fatigue. The mass at the right chin was mildly tender. The size remained approximately 7 cm with a rubbery consistency. It was slightly mobile and tender to touch, without overlying erythematous skin. The examination of her ears, eyes, nose, and oral cavity was unremarkable. There were no other palpable lymph nodes in axillary, epitrochlear, or inguinal regions. Other systems proved to be unremarkable as well.
Her laboratory tests showed normal blood count (hemoglobin 11.2 g/dL, WBC 7640 cells/cu.mm, neutrophil 48.9 %, lymphocyte 40.8 %, eosinophil 1.4 %, and platelet 221,000 cells/cu.mm), normal renal function and blood chemistry. Her chest x-ray was unremarkable. Blood cultures for bacteria, fungus, and mycobacterium were all negative.
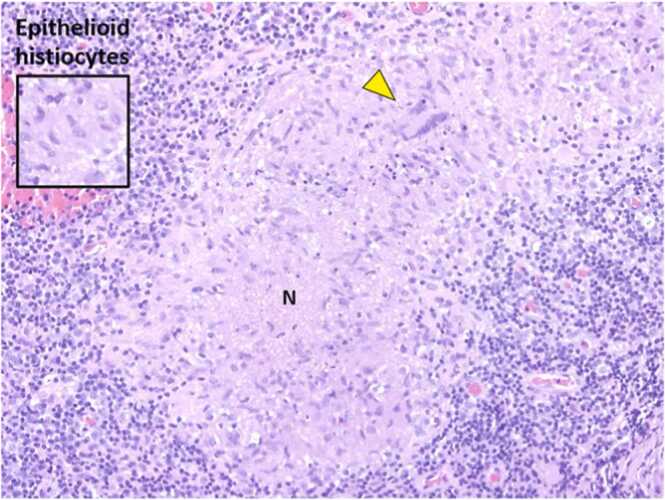
A biopsy was done on the right cervical lymph node. Gram stain showed no bacteria and bacterial culture showed no growth. Acid Fast Bacteria (AFB) stain and modified AFB (mAFB) stain showed no organism. Polymerase chain reaction (PCR) for mycobacterium did not detect M. tuberculosis complex. Pathology showed granuloma which was defined as aggregation of epithelioid histiocytes. Multinucleated giant cells (yellow arrowhead) and necrotic foci were also noted (Fig. 2).
Fig. 2.
Pathology of lymph node tissue.
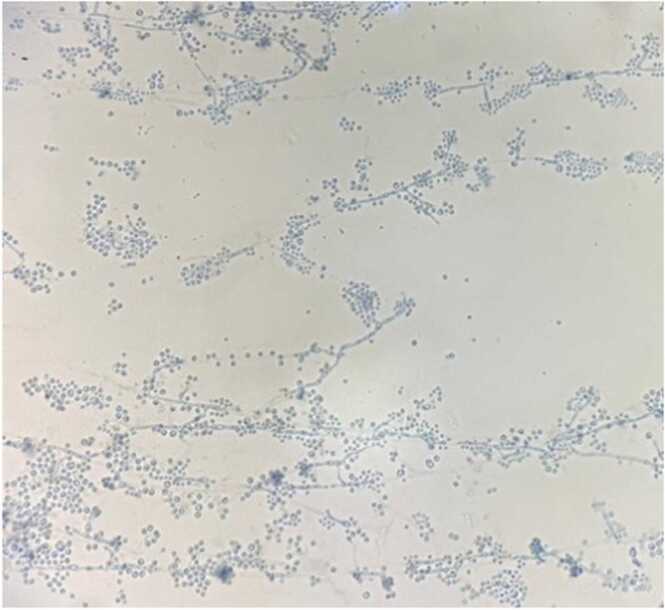
The fungal culture on Sabouraud dextrose agar from the lymph node tissue showed a single large cream-colored colony with melanin production on top and a finely wrinkled surface after being incubated at 25 degrees Celsius for two weeks (Fig. 3). The mold was then scrutinized under microscope with lactophenol cotton blue staining, which revealed branching hyphae with delicately arranged pyriform conidia, some of which was found to be in rosette pattern (Fig. 4). These phenotypes answered that the mold belong to Sporothrix genus. Then we employed the use of MALDI-TOF (Matrix-Assisted Laser Desorption/Ionization Time-Of-Flight mass spectrometry) to identify specie of Sporothrix which was identified as Sporothrix schenkii.
Fig. 3.
The fungal culture on Sabouraud dextrose agar from the lymph node tissue showed a single large cream-colored colony with melanin production on top and finely wrinkled surface.
Fig. 4.
Microscopic examination with lactophenol cotton blue revealed multiple, blue-stained thin hyaline septate hyphae with ovoid-shaped conidia arranged into floral or rosette pattern.
After establishing the diagnosis of sporotrichosis, the patient was prescribed 400 mg of itraconazole daily, divided into two doses per day. After one month of treatment, the cervical lymph node was no longer palpable, and the pain completely resolved. Itraconazole was continued for three months and stopped without any complications.
Discussion
Sporothrix schenkii, a dimorphic fungus that causes sporotrichosis, can give rise to varied diseases depending on the host as well as its route of infection. Sporothrix thrives well on humid tropical soil and decaying vegetation as a saprophyte [1], [2] and most commonly enters the human body via traumatic implantation [3]. Despite that, a significant portion of infected individuals could not recall a history of trauma [4]. The fungus prefers armadillo’s nest [5], [6] and sphagnum moss [2] as its reservoir but can also transmit from cats, dogs, squirrels, parrots, and horses [6]. To date, there is no human-to-human transmission reported.
Clinical presentations also depend on the pathogenicity, the load and depth of inoculation, and the degree of thermotolerance of that species [7]. Most infections can be classified into three forms, namely cutaneous, mucosal, and extracutaneous forms. The cutaneous form is usually caused by direct trauma while the mucosal form might be caused by either inhalation of conidia, hematogenous spreading, or self-inoculation by the patient’s own hands [8]. On the other hand, an extracutaneous form of sporotrichosis may warrant a suspicion of a certain degree of immunosuppression or immunodeficiency [9].
Constant exposure to environmental conidia is found to be associated with a low level of immunity against sporotrichosis, especially in endemic areas of the fungus [3]. As a result, those patients would present more frequently as cutaneous disease alone rather than lymphocutaneous involvement [10]. Our patient did indeed stay in Malaysia which is known for its endemicity of sporotrichosis. However, instead of presenting as a cutaneous disease, she presented with isolated lymphadenopathy.
After a thorough literature review, the author compiled previous case reports where patients with sporotrichosis presented solely with lymph node involvement without skin lesions, as shown in Table 1. Notably, all the cases were young patients under the age of 14 years old who presumably did not experience sufficient exposure to environmental Sporothrix to form immunity. With itraconazole in three cases and potassium iodide in one case, all the patients were cured.
Table 1.
Case Reports of Sporotrichosis Patients Solely with Lymphadenopathy.
| Report | Host | Presentation | Suspected route | Treatment received | Outcome |
|---|---|---|---|---|---|
| McKinney et al. 2022[11] | 6 year old boy Previously healthy |
Painless cervical lymph nodes 2 months | Numerous cats on his farm | Itraconazole x4 weeks | Lymphadenopathy resolved in the second week |
| Picollo et al. 2021[12] | 4 year old girl Previously healthy |
Subacute axillar lymphadenopathy | Forearm injury. Lived with cats and dogs | Itraconazole x3 months | Clinically resolved at 3 months, no remission at 1 year |
| Tilak et al. 2012[13] | 13 years old girl Previously healthy |
Inguinal lymphadenopathy for 4 years (with a small non-healing ulcer at the foot) | Thorn prick 2 years before the onset | Itraconazole x6 weeks | Marked clinical response at fourth week, resolution in 6 weeks |
| Whitefield et al. 1995[14] | 10 year old boy Previously healthy |
Tender right axillar lymphadenopathy | Direct inoculation from playground | Potassium iodide x 4 months | Clinically resolved at 3 months, no remission at 18 months |
In conclusion, while the classic presentation of cutaneous sporotrichosis is well-known, it is important to be aware of atypical manifestations, such as chronic lymphadenopathy. A thorough history and exposure risk assessment should prompt testing for fungal infections, including Sporothrix schenckii, in patients under suspicion.
Ethical approval
This study was reviewed by the Research Ethics Committee of the Faculty of Medicine, Chiang Mai University (study code: MED-2567–0248).
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Consent
The patient provided written consent for the publication of this case report. A copy of the written consent can be made available for review by the Editor-in-Chief of this journal upon request.
CRediT authorship contribution statement
Parichat Salee: Supervision, Data curation, Conceptualization. Saikhuan Towachiraporn: Data curation. Sarawut Kongkarnka: Writing – original draft, Data curation. Kawisara Krasaewes: Writing – review & editing, Supervision, Project administration, Conceptualization. Jetanat Chantrapitak: Writing – original draft, Data curation, Conceptualization.
Declaration of Competing Interest
Authors declare no conflicts of Interests for this article.
Acknowledgement
None.
References
- 1.Kenyon E.M., Russell L.H., McMurray D.N. Isolation of Sporothrix schenckii from potting soil. Mycopathologia. 1984;87(1-2):128. doi: 10.1007/BF00436641. [DOI] [PubMed] [Google Scholar]
- 2.Mehta K.I., Sharma N.L., Kanga A.K., Mahajan V.K., Ranjan N. Isolation of Sporothrix schenckii from the environmental sources of cutaneous sporotrichosis patients in Himachal Pradesh, India: results of a pilot study. Mycoses. 2007;50(6):496–501. doi: 10.1111/j.1439-0507.2007.01411.x. [DOI] [PubMed] [Google Scholar]
- 3.Staib F. Medical Mycology. The Pathogenic Fungi and the Pathogenic Actinomycetes, Third Edition, J.W. Rippon. W. B. Saunders Company/Harcourt Brace Jovanovich Inc., Philadelphia (1988), Hard cover £ 50. Zentralblatt Fur Bakteriologie-international Journal of Medical Microbiology Virology Parasitology and Infectious Diseases. 1989;272.
- 4.Barros M.B., Schubach Ade O., do Valle A.C., Gutierrez Galhardo M.C., Conceicao-Silva F., Schubach T.M., et al. Cat-transmitted sporotrichosis epidemic in Rio de Janeiro, Brazil: description of a series of cases. Clin Infect Dis. 2004;38(4):529–535. doi: 10.1086/381200. [DOI] [PubMed] [Google Scholar]
- 5.Wenker C.J., Kaufman L., Bacciarini L.N., Robert N. Sporotrichosis in a nine-banded armadillo (Dasypus novemcinctus) J Zoo Wildl Med. 1998;29(4):474–478. [PubMed] [Google Scholar]
- 6.Saravanakumar P.S., Eslami P., Zar F.A. Lymphocutaneous sporotrichosis associated with a squirrel bite: case report and review. Clin Infect Dis. 1996;23(3):647–648. doi: 10.1093/clinids/23.3.647. [DOI] [PubMed] [Google Scholar]
- 7.Arrillaga-Moncrieff I., Capilla J., Mayayo E., Marimon R., Marine M., Gene J., et al. Different virulence levels of the species of Sporothrix in a murine model. Clin Microbiol Infect. 2009;15(7):651–655. doi: 10.1111/j.1469-0691.2009.02824.x. [DOI] [PubMed] [Google Scholar]
- 8.de Lima Barros M.B., de Oliveira Schubach A., Galhardo M.C., Schubach T.M., dos Reis R.S., Conceicao M.J., et al. Sporotrichosis with widespread cutaneous lesions: report of 24 cases related to transmission by domestic cats in Rio de Janeiro, Brazil. Int J Dermatol. 2003;42(9):677–681. doi: 10.1046/j.1365-4362.2003.01813.x. [DOI] [PubMed] [Google Scholar]
- 9.Rodrigues A.M., Fernandes G.F., de Camargo Z.P. In: Emerging and Re-emerging Infectious Diseases of Livestock. Bayry J., editor. Springer International Publishing; Cham: 2017. Sporotrichosis; pp. 391–421. [Google Scholar]
- 10.Lavalle P., Mariat F. Sporotrichosis. Bull Inst Pasteur. 1983;81:295–322. [Google Scholar]
- 11.McKinney J.A., Baykoca-Arslan B., Levent F. Uncommon aetiology of lymphadenopathy in a healthy child: a sporotrichosis case with painless lymphadenopathy. BMJ Case Rep. 2022;15(3) doi: 10.1136/bcr-2021-245057. PMID:PMC8900024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Picollo M., Epelbaum C., Bustos A.C., Carnovale S., Rosanova M.T. [Lymphocutaneous sporotrichosis in a pediatric patient, a case report] Rev Chil Infectol. 2021;38(6):811–815. doi: 10.4067/s0716-10182021000600811. [DOI] [PubMed] [Google Scholar]
- 13.Tilak R., Kumari V., Bansal M., Sharma T., Pandey S.S. Lymphocutaneous sporotrichosis in an adolescent girl presenting as mycetoma. Int J Low Extrem Wounds. 2012;11(3):184–186. doi: 10.1177/1534734612457571. [DOI] [PubMed] [Google Scholar]
- 14.Whitfeld M.J., Faust H.B. Lymphocutaneous sporotrichosis. Austral J Dermatol. 1995;36(3):161–163. doi: 10.1111/j.1440-0960.1995.tb00960.x. [DOI] [PubMed] [Google Scholar]