Abstract
Objective
Social interactions and experiences are increasingly occurring online, including for young adults with psychosis. Healthy social interactions and experiences are widely recognized as a critical component of social recovery, yet research thus far has focused predominantly on offline interactions with limited understanding of these interactions online. We developed the Social Media and Internet sociaL Engagement (SMILE) questionnaire to assess the type, frequency, and nature of online social interactions and experiences among young adults with early psychosis to better assess online social activity and ultimately support personalized interventions.
Methods
Participants (N = 49) completed the SMILE questionnaire which asked about online platforms used, frequency of use, and if positive and negative experiences were more likely to happen online or offline. Participants completed additional self-report measures of victimization, positive psychotic symptoms, social functioning, and demographics. Exploratory factor analysis and correlations between identified factors and clinical measures of interest were completed.
Results
Exploratory factor analysis revealed three factors: positive engagement, victimization, and internalizing experiences. Most participants (6%–37%) experienced positive engagement offline. Victimization occurred equally online and offline (8%–27% and 4%–24%, respectively). Most participants (37%–51%) endorsed internalizing experiences as occurring equally offline and online, but approximately a third of participants reported internalizing experiences more frequently offline (20%–35%). Victimization was moderately (r = 0.34) correlated with overall online social experiences, suggesting more online time may increase the likelihood of victimization. Age was inversely related to the frequency of overall online social experiences.
Conclusion
Young adults with early psychosis experience positive and negative social experiences online and offline. New scales and measures to comprehensively assess the nature and function of online social interactions and experiences are needed.
Keywords: Social media, internet, first episode psychosis, schizophrenia spectrum disorders, social functioning, young adult
Healthy social experiences are widely recognized as a critical component of recovery across psychiatric disorders.1–3 Studies exploring a variety of social constructs such as connectedness, social functioning, social support, and social skills have repeatedly demonstrated that positive social experiences are associated with improvements in physical, mental, and cognitive health in individuals both with and without psychiatric disorders.4,5 Psychotic symptoms including delusions, hallucinations, and disordered thoughts, 6 may disrupt the attainment of healthy developmental milestones and normative social experiences and interactions. First-episode psychosis, affecting 126 per 100,000 individuals aged 15–29 per year, is typically defined as including the first 1–5 years following symptom onset. 7 As the onset of first-episode psychosis is primarily in adolescence or young adulthood,6,7 a critical developmental period for socialization, 8 disrupting healthy social interactions and experiences may hold particular clinical significance. Literature indicates that engagement in social experiences and initiating and maintaining fulfilling social relationships is associated with better mental health outcomes in young adults with first-episode psychosis, 2 including higher levels of positive affect9,10 and increased trust in others. 11 Conversely, limited social experiences in this population have been associated with increased loneliness 12 higher paranoia, 13 and increased risk for suicidal ideation. 14 Given their established clinical and functional benefits, finding avenues for positive social interactions and experiences has become a fundamental component of early psychosis intervention services. 15
In this digital age, an increasing proportion of social experiences are occurring online. For example, it is estimated that about half of young adults under 30 have used a dating site or app to meet partners. 16 Additionally, between 2005 and 2015, the number of American young adults who found a job online doubled. 17 Internet-based social interactions, whether through social media platforms (e.g. Instagram, Twitter, Facebook, etc.) or via text/video messaging platforms, offer a way to extend the frequency, type, content, and availability of social interactions and have become a part of everyday life for many. For many during the COVID-19 pandemic, there was increased reliance on the internet for a range of social interactions (e.g. work, socializing with friends and family, attending school, etc.) with 58% of US adults deeming the internet as “essential to functioning” in April 2021 as compared to 53% reporting it as essential in April 2020. 18 While the effects of the COVID-19 pandemic can be seen in continued frequent use of online platforms for professional and personal social interactions, online behavior of young adults has stayed relatively consistent with research even pointing to 49% of these individuals making an active effort to reduce online time. 18 Before the pandemic, nearly 100% of US youth reported regularly using the Internet and nearly 50% of US teens reported being almost constantly online. 19 Notably, these rates are similar for youth with psychosis pre-pandemic, 20 however, there is an absence of research exploring changes in internet use during and after the pandemic for this population. A recent systematic review exploring pre-COVID-19 internet use as a means of social interaction by individuals with psychosis found that these individuals use the internet as much as the general population and, importantly, that this use was not associated with worsening symptoms. 20 That said, there is limited research on how these patterns may have been affected by the pandemic, and an assessment of these changes is needed.
Online social interactions may be uniquely appealing to youth with psychosis. Social anxiety, stigma, and decreased motivation to initiate and sustain relationships may interfere with in-person social interactions, limiting opportunities for regular social contact.21,22 While some studies have suggested that social media use may be detrimental to mental health23,24 others have found that social media use may be beneficial in overcoming barriers to healthy social experiences in young adults with psychosis 25 and that internet use may increase avenues for illness-related social support.26,27 Of note, some work has found that young adults with psychosis experiencing more negative symptoms use social media less, with possible explanations including decreased social motivation and engagement in activities associated with social interactions and experiences. 28 Similarly, other data suggest that young adults with psychosis use technology less when they are feeling more symptomatic, though these individuals also indicated that using social media and the internet were helpful illness-management strategies. 29 Taken together, more work should be done to clarify how this population uses the internet for social interactions and experiences and how this use may relate to psychotic symptoms. Doing so would further clinicians’ and researchers’ understanding of individuals’ social functioning in this important domain and allow them to better assess the strengths of internet and social media use and targets for intervention.
A related body of work has suggested that the way individuals use the internet may be associated with their mental health, differentiating between “passive” (e.g. scrolling or consuming others’ posts) and “active” use (e.g. posting comments, creating posts, or engaging with content). 30 The passive social media use hypothesis suggests that passive social media use may negatively impact mental health by activating upwards comparison and feelings of envy, whereas active social media use may lead to positive feedback and social connection with others, ultimately benefitting mental health.31,32 Though data to support this position are varied,33,34 there is an absence of research on passive and active use within young adults with psychosis. Collecting more information on the way that this population engages with social media may offer valuable insights into the function of social media and the internet in social interactions and experiences that goes beyond the use of common platforms. In other words, understanding what platforms this population uses and how frequently they use them, as well as how they are used for social interaction are both important areas of exploration. There is also little research on the use of specific internet-based activities in young adults with psychosis, such as online dating, gaming, or blogging, nor style of use (i.e. active or passive), creating a notable gap in our knowledge of the use and function of these online resources for this population.
Given the frequency of social media and internet use among young adults with psychosis, understanding how and why these platforms are being used to interact with others is critical to enhancing our understanding of the scope and nature of their social experiences. It is well-established that healthy social interactions are considered vital to social recovery from psychosis, however, research has focused predominantly on offline (i.e. in-person) interactions to assess social experiences and interactions. Doing so misses an abundant source of social processes that occur online, pointing to the need for better assessment tools to support personalized interventions. Currently, assessment tools are limited in their measurement of online social interactions. A systematic review conducted in 2019 evaluating the inclusion of social media use in measuring the social functioning of young people with and at clinically high risk for psychosis found that of the 58 measures of social functioning identified, only one included social media use, 35 the First-Episode Social Functioning Scale (FESFS 36 ). In their review, Bjornestad and colleagues (2019) noted concerns about the ecological validity of current social functioning scales to evaluate normative social experiences. Put differently, healthy and unhealthy social interactions occur both online and in-person, and using only measures of in-person social functioning may miss other important social interactions and experiences.
While the ability to capture online social interactions by existing social functioning scales may be limited by concerns about ecological validity, it is also important to note that many existing measures of social media and internet use among young adults capture only problematic use. These measures have predominantly focused on the frequency of use and emotional attachment to assess internet addiction37,38 or have been limited by focusing on a singular platform (e.g. Facebook or Reddit). 35 Several of these studies have found that problematic social media use (i.e. excessive use and high emotional investment in social media activity) may be associated with poorer mental health in individuals with schizophrenia39,40 and healthy young adults.41,42 Few measures to date have considered social activity across multiple settings (e.g. in-person and online) and none, to our knowledge, have been developed with an intentional lens towards young adults with psychosis. As such, there is a clear need to expand measures of social experiences and social functioning to include a more nuanced appreciation of online social interactions as they play an increasingly important role in the lives of those with psychosis. Doing so may aid clinicians and researchers in developing more individualized interventions for social goals and improve accuracy in the assessment of social functioning.
In the present study, we developed the Social Media and Internet sociaL Engagement (SMILE) questionnaire to assess the type, frequency, and nature of online social interactions and experiences among young adults, defined in our study as adults ages 18–35, with early psychosis. We hypothesized that online social interactions and experiences would include both positive and negative experiences and that positive online interactions and experiences would be reported at a higher frequency than negative interactions for most of our sample. We also explored relationships between items on the SMILE questionnaire and validated self-reported measures of victimization, social functioning, and psychotic symptoms to better understand how online social interactions and experiences of this population may be related to these other well-studied clinical constructs. Our study takes an initial step to examine the frequency and function of online and offline social interactions and subjective experiences to support a more accurate assessment of online social interactions and experiences. By gathering more accurate observations of patients’ social experiences in an increasingly digital world, researchers and clinicians can better target and personalize interventions to support individuals’ needs.
Methods
Participants
Participants between the ages of 18 and 35 were approached at the Zucker Hillside Hospital's inpatient and outpatient departments between July 2021 and August 2022. In total, 170 individuals were assessed for eligibility based on being at least 18 years of age, ability to read English, and having a diagnosis of a primary psychotic disorder or a mood disorder with psychotic features. Exclusion criteria included a diagnosis of autism spectrum disorder, substance-induced psychotic disorder, psychotic disorder due to a general medical condition, and intellectual disability (IQ < 70). Participants were not excluded based on medication, other comorbid diagnoses, or severity of illness. After assessing eligibility, 76 individuals were excluded for not meeting inclusion criteria, and 43 individuals declined to participate. Fifty-one individuals consented to study procedures; however, one individual withdrew consent and one other individual erroneously consented twice. In total, 49 individuals were included in our study with 41 participants holding a primary psychotic disorder diagnosis and eight participants holding a primary mood disorder with psychotic features. All participants provided written informed consent to participate. Procedures were approved by the Northwell Health IRB (#21-0017-ZHH). Study questionnaires were completed in a single study visit, either in person or over two-way video. Study procedures took approximately 30 min to complete.
Development of the SMILE questionnaire
The SMILE questionnaire was developed by clinicians with expertise in research and treatment of young adults with first-episode psychosis (initials omitted for review) and psychometric scale development (initials omitted for review). The authors generated a list of questions relevant to young adults with mental illness concerning their online and offline social interactions and experiences. Questions were based on the authors’ clinical expertise in treating youth with early psychosis and their review of existing scales. Items were designed to evaluate social interactions both online and offline and to capture positive and negative experiences across both settings. Questions were developed iteratively based on experience working with individuals with psychosis and a literature review of existing social functioning and social media measures with input from the entire team to achieve consensus on optimal wording and format. The final questionnaire consisted of 45 individual items, with questions organized into four sections explained below (full questionnaire available in the Supplemental Material).
Assessment of social experiences
For all sections on the SMILE questionnaire, participants (N = 49) were asked to report their answers based on activity in the past month. This time frame was selected as it is considered a standard recall period often used on other validated measures of social functioning for those with psychosis, such as the Global Functioning Scale, 43 Global Assessment of Functioning. 44 Section 1 of the SMILE questionnaire asked participants to select which online platforms they had used in the past month. Section 2 asked participants to select the type and frequency of various online behaviors and activities in the past month (e.g. “passive” actions such as scrolling vs. “active” interactions such as chatting or commenting) using a four-point semantic differential scale from “Daily,” “Weekly,” “Monthly,” and “Never.” Section 3 asked participants to report the degree to which social interactions, interpersonal activities, and subjective experiences took place online versus offline utilizing a five-point semantic differential scale as Offline (1), About the Same (3), Online (5), or Not Applicable in response to each item. Specifically, Section 3A focused on positive experiences and interactions with others (e.g. “Interacting with people,” “Initiating contact with others” and “Feel authentic,” “Feel confident”). Section 3B focused on negative experiences (e.g. “Feel nervous,” “Feel misunderstood”), and Section 3C described negative interactions with others (e.g. “Experience bullying,” “Get into arguments”). Participants were also asked whether they perceived online social activities to have positively or negatively impacted their mental health.
Demographic and self-report clinical measures
All participants self-reported sociodemographic information. Additional validated scales were used to assess relevant clinical constructs and copyright permission was obtained for each. These scales (discussed below) were completed by 44 participants (five participants were concurrently enrolled in another study and were not asked to complete additional scales to avoid participant fatigue). Social functioning was assessed with the FESFS. 36 This validated measure of social functioning was chosen because it matched our population of interest and is notably one of the only social functioning measures to inquire about social activity online.31,38 The FESFS shows good convergent validity with other valid measures of social functioning (i.e. the Global Assessment of Functioning 44 and the Social and Occupational Functioning Assessment Scale 45 ) and good internal consistency. 36 Experiences of victimization were measured with the Multidimensional Peer-Victimization Scale (MPVS), a validated measure of negative experiences of victimization in peer interactions. 46 Given our interest in learning about the types and frequency of social experiences online and offline, we selected the MPVS to understand what relationship, if any, existed between experiences of victimization and online or offline interactions. This scale demonstrates good internal consistency and reliability, and concurrent and convergent validity with other validated measures of victimization. 47 Finally, self-reported psychotic symptoms were measured with the PRIME questionnaire. 48 This measure is one of only a few validated self-report measures of psychotic symptoms. Additionally, research has indicated that screeners such as the PRIME may be used as valid monitoring tools for psychotic symptoms. 49 We opted to use a self-report measure of positive psychotic symptoms rather than clinician-assessed symptom severity to capture participants’ subjective experience of psychosis as recent research has emphasized the utility of collecting patients’ experiences in improving the accuracy of intervention and research.50–52 By including this measure, we aimed to explore the relationship between positive psychotic symptoms and social experiences across online and offline settings.
Analyses
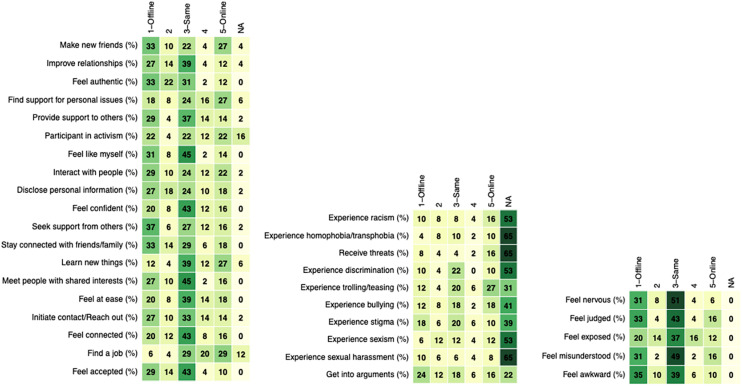
Counts and proportions of different responses to the SMILE items were noted and tallied for Sections 1–3, assessing usage, frequency, and experiences (Figure 1). Selections of “Not Applicable” (NA) were noted in analyses. A principal axis exploratory factor analysis was conducted on the items from Section 3 to explore their underlying relationship. The psych package in R was used. 53 A three-factor solution was selected based on analysis of the scree plot, with an oblique promax rotation. The factor analysis was done using pairwise deletion for missing data. Internal consistency within each factor was assessed using Cronbach's alpha. The power to detect moderate effect sizes of r = 0.40 in this sample (n = 49) is 0.83 (assuming two-sided a = 0.05). 54 There was no missing data in SMILE responses for the sample reported. However, five of the participants did not complete the additional self-reports (MPVS, FESFS, and PRIME) due to the burden of other unrelated study activities. Factor scores for each participant were calculated after NA values were imputed using random forest imputation (rfImpute). 55 Spearman correlations were used to evaluate relationships between factor scores from the SMILE questionnaire and other clinical measures and one-way ANOVA was used to examine the effect of gender and race. The relationship between age and online social experiences was evaluated using Spearman correlations. All analyses were completed in R (v.4.2.0). Raw p-values are reported along with adjusted p-values after correction for multiple comparisons using the Benjamini-Hochberg method. 56 Note that, because we are not testing explicit hypotheses here, the corrected p-values do not carry the same importance as they would if hypotheses were being tested. They are provided here for thoroughness, reflecting the probability that the obtained results would be observed by chance given random data with the same properties.
Figure 1.
Frequency of experiences offline or online. (A) Demonstrates positive engagement (Factor 1), (B) demonstrates victimization (Factor 2), and (C) demonstrates internalizing experience (Factor 3). The frequency in each square is represented as a percentage. “Not Applicable” responses are omitted.
Results
Descriptive statistics and demographic characteristics
In total, 49 participants enrolled in the study. Participants had a mean age of 25.47 years (SD = 4.51) with 63% of the sample identifying as male (Table 1). The largest proportion of our sample identified as White/Caucasian (39%) and most of our sample had received a primary diagnosis of a psychotic disorder (84%) with a smaller number having been diagnosed with a primary mood disorder with psychotic features (16%). Across both primary diagnoses, approximately half of our sample (53%) reported comorbid secondary and tertiary diagnoses including alcohol and substance use disorders, generalized anxiety disorder, major depressive disorder, obsessive-compulsive disorder, post-traumatic stress disorder, antisocial personality disorder, attention-deficit/hyperactivity disorder, and social anxiety disorder.
Table 1.
Sample characteristics.
| Characteristics | Total (N = 49) | Mean (SD) |
|---|---|---|
| Age | 25.47 (4.51) | |
| Gender | ||
| Male | 31 (63.3%) | |
| Female | 12 (24.5%) | |
| Nonbinary | 2 (4.1%) | |
| Not specified | 4 (8.2%) | |
| Sex | ||
| Male | 33 (68.8%) | |
| Female | 15 (31.2%) | |
| Race | ||
| White | 19 (39.6%) | |
| Black/African American | 14 (29.2%) | |
| Asian | 6 (12.5%) | |
| Other | 9 (18.8%) | |
| Ethnicity | ||
| Hispanic | 8 (19.0%) | |
| Not Hispanic | 34 (81.0%) | |
| Diagnosis | ||
| Primary psychotic disorder | 41 (83.7%) | |
| Mood disorder with psychotic features | 8 (16.3%) | |
| Highest level of education attained | ||
| Some high school | 2 (4.2%) | |
| High school graduate/GED | 13 (27.1%) | |
| Some college/associate's degree | 19 (39.6%) | |
| Bachelor's degree | 1 (22.9%) | |
| Graduate degree | 3 (6.2%) | |
| Marital status | ||
| Never married | 42 (87.5%) | |
| Living with partner | 1 (2.1%) | |
| Married | 4 (8.3%) | |
| Divorced | 1 (2.1%) | |
| Employment status | ||
| Not employed | 31 (66.0%) | |
| Part-time | 5 (10.6%) | |
| Full-time | 11 (23.4%) | |
| Convergent and discriminant validity Questionnaires | Mean (SD) | |
| Prime screen | 32.02 (20.79) | |
| FESFS | 58 (10.07) | |
| MPVS | 48.18 (12.92) | |
SMILE: Social Media and Internet sociaL Engagement; FESFS: First-Episode Social Functioning Scale.
Online behaviors and platforms used
Forty-nine (49) participants reported use and frequency of use for seven categories of online platforms (Table 2). The three most used online platforms were social media (88%), messaging, and multiway video platforms (53%), followed by multiplayer online gaming/streaming (37%). The least used platforms were dating apps (25%), blogs (18%), and chatrooms (12%). Regarding the frequency of specific online behaviors, the most frequent were scrolling/viewing content (88% occurring daily or weekly), followed by chatting/messaging (82% occurring daily or weekly), and commenting/posting (57% occurring daily or weekly), while dating/developing intimate or romantic connections (20% occurring daily or weekly), multiplayer gaming/streaming (33% occurring daily or weekly), and professional activities/networking (33% occurring daily or weekly), occurred least frequently (Table 2). The total frequency of use of online platforms was not significantly affected by gender (p = 0.57), race (p = 0.25), or age (p = 0.09).
Table 2.
Online platforms used by respondents and frequency of activities.
| Which of the following platforms did you use to interact with other people online? (In the last month) | Total “yes” | Total “no” | ||
|---|---|---|---|---|
| Social media | 43 (87.8%) | 6 (12.2%) | ||
| Messaging and multiway video platforms | 26 (53.1%) | 23 (46.9%) | ||
| Multiplayer online gaming/streaming | 18 (36.7%) | 31 (63.2%) | ||
| Professional networking sites | 14 (28.6%) | 35 (71.4%) | ||
| Dating apps | 12 (24.5%) | 37 (75.5%) | ||
| Blogs | 9 (18.4%) | 40 (81.6%) | ||
| Chatrooms | 6 (12.2%) | 43 (87.8%) | ||
| When thinking about your online interactions in the past month, how often did you do each of the following? | Daily | Weekly | Monthly | Never |
| Scrolling/viewing content | 34 (69.4%) | 9 (18.4%) | 3 (6.1%) | 3 (6.1%) |
| Chatting/messaging | 26 (53.1%) | 14 (28.6%) | 5 (10.2%) | 4 (8.2%) |
| Commenting/posting | 16 (32.6%) | 12 (24.5%) | 12 (24.5%) | 9 (18.4%) |
| Professional/networking | 9 (18.4%) | 7 (14.3%) | 13 (26.5%) | 20 (40.8%) |
| Multiplayer gaming/streaming | 5 (10.2%) | 11 (22.4%) | 13 (26.5%) | 20 (40.8%) |
| Dating/intimate or romantic connections | 5 (10.2%) | 5 (10.2%) | 10 (20.4%) | 29 (59.2%) |
Online and offline social interactions and experiences
Factor analysis: Three latent factors were identified in the exploratory factor analysis (Table 3). Factor 1, labeled “Positive Engagement” (20.1% of total variance) generally described positive experiences and social interactions and most prominently included items such as “Make new friends,” “Improve relationships,” “Feel authentic,” and “Find support for personal issues.” Factor 2, labeled “Victimization” (18.2% of total variance) generally described negative social interactions of victimization by others, and included “Experience racism directed at me,” “Experience homophobia/transphobia,” “Receive threats,” and “Experience discrimination.” Factor 3, labeled “Internalizing Experiences” (8.8% of total variance) generally described negative experiences, such as “Feel nervous,” “Feel judged,” and “Feel exposed or vulnerable.”
Table 3.
Factor loadings from principal component analysis of online experiences.
| Factor 1: Positive engagement | Factor 2: Victimization | Factor 3: Internalizing experiences | |
|---|---|---|---|
| Factor 1 | |||
| Making new friends | 0.73 | – | – |
| Feeling authentic | 0.70 | – | – |
| More likely to provide support | 0.63 | – | – |
| Spending more time interacting with people | 0.57 | – | – |
| Disclosing more information about self | 0.54 | – | – |
| More likely to seek support | 0.54 | – | – |
| Staying more connected | 0.52 | – | – |
| Meeting more people who shared interest | 0.49 | – | – |
| More likely to initiate contact | 0.48 | – | – |
| Feeling at ease | 0.48 | – | – |
| Improving an existing relationship | 0.72 | – | – |
| Finding support for personal issues | 0.64 | – | – |
| Participating in activism | 0.63 | – | – |
| Feeling like oneself | 0.60 | – | – |
| Feeling confident | 0.54 | −0.45 | – |
| Learning new things | 0.50 | – | 0.46 |
| Feeling connected | 0.45 | −0.47 | – |
| Find a job | 0.42 | ||
| Feeling accepted | 0.40 | −0.53 | – |
| Factor 2 | |||
| Experiencing racism directed at viewer | – | 0.91 | – |
| Receiving threats | – | 0.86 | – |
| Experiencing discrimination directed at viewer | – | 0.77 | – |
| Experiencing bullying | – | 0.71 | – |
| Experiencing trolling directed at viewer | – | 0.75 | – |
| Experiencing stigma toward one's mental illness | – | 0.55 | – |
| Getting into arguments | – | 0.43 | – |
| Experiencing homophobia/Transphobias directed at viewer | – | 0.89 | −0.51 |
| Experiencing sexism directed at viewer | 0.55 | 0.50 | – |
| Experiencing sexual harassment | 0.56 | 0.47 | – |
| Factor 3 | |||
| Feeling judged | – | – | 0.70 |
| Feeling nervous | – | 0.77 | |
| Feeling exposed or vulnerable | – | – | 0.68 |
| Feeling misunderstood | – | – | 0.60 |
| Feeling awkward | – | – | 0.42 |
Of note, some items were cross-loaded across factors. Sexism and sexual harassment were cross-loaded on both the positive engagement and victimization factors. Feeling confident, feeling connected, and feeling accepted were each positively loaded on Factor 1, and negatively loaded on Factor 2. Feeling better was also negatively loaded on Factor 2.
Internal consistency within the factors was excellent for Factors 1 and 2, and acceptable for Factor 3: Factor 1 alpha = 0.92, 95% CI [0.85, 0.95]; Factor 2 alpha = 0.95, 95% CI [0.71, 1.00]; Factor 3 alpha = 0.77, 95% CI [0.62, 0.85].
Frequencies of online and offline experiences: Figure 1 illustrates participant responses for items in each of the three factors. For Factor 1, termed positive engagement, which included positive social experiences and interactions, responses ranged widely with regard to whether these experiences took place more frequently online or offline. While the modal response for most items was “offline,” a sizeable proportion of participants (10%–29%) answered “online” for each of these items. In addition, more participants (27%) answered “online” than “offline” for being more likely to “find support for personal issues.” Items in Factor 2, termed victimization, which included negative experiences of victimization and conflict, were roughly evenly divided between “online” and “offline.” Experiences of racism, trolling/teasing, bullying, and receiving threats directed at the individual user (i.e. participant) were more likely to occur online for most participants, however, a large proportion of responses stated that these experiences were not applicable. Participants reported experiencing stigma towards one's mental illness and arguments more offline than online (18% and 25%, respectively). Items in Factor 3, termed internalizing experiences, included negative internalizing experiences such as feeling “nervous” (51%) or “misunderstood” (49%) and all were most frequently reported as occurring equally or the “Same” offline and online. A large proportion of participants also reported experiencing internalizing experiences more frequently “offline” (20%–35%) and relatively fewer reported being more likely to experience them “online” (6%–16%).
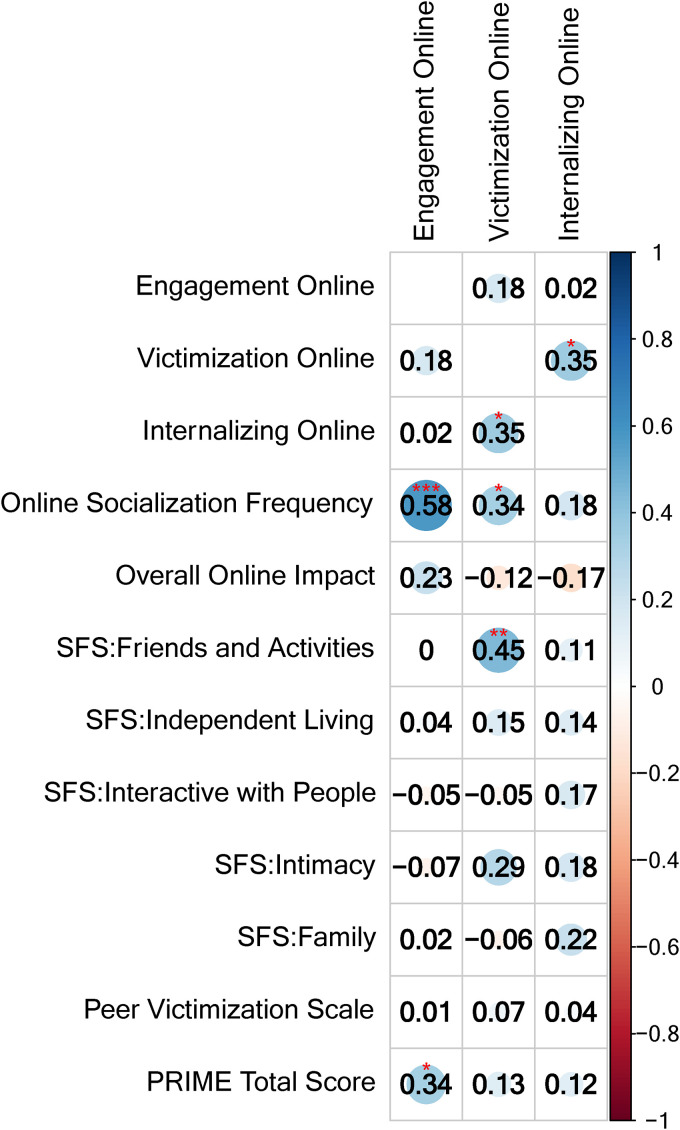
Relationship between SMILE, self-reported measures of victimization, psychotic symptoms, and social functioning
Figure 2 illustrates exploratory findings of correlations between the SMILE questionnaire and three clinical measures of interest (MPVS, FESFS, and PRIME). Within the SMILE questionnaire, a moderate correlation (r = 0.35, p = 0.04) between victimization (Factor 2) and internalizing experiences (Factor 3) was observed. Overall online social experience frequency as measured on SMILE was moderately positively correlated to positive engagement (Factor 1; r = 0.58, p = 0.001) and victimization (Factor 2; r = 0.34, p = 0.04). Higher reporting of victimization (Factor 2) online than offline was associated with better global social functioning on the friends and activities subscale of the FESFS (r = 0.45, p = 0.005), however, no other significant associations were observed. After correcting for multiple comparisons, only the relationship between the frequency of online social experiences and positive engagement (Factor 1) remained significant (p = 0.002). No significant correlations between SMILE and PRIME nor the MPVS were observed.
Figure 2.
Spearman correlations between SMILE factors of online experiences and other clinical measures of interest. SMILE: Social Media and Internet sociaL Engagement. FESFS: First-Episode Social Functioning Scale. Color scale reflects the correlation coefficient (rho) ranging from − 1 (red, bottom) to + 1 (blue, top). A darker color indicates the strength of the coefficient. * = p < 0.05, ** = p < 0.01, *** = p < 0.001.
Relationship between SMILE and demographic variables
There was a small, negative correlation between age and score on Engagement (Factor 1; r = -0.29; p = 0.04), however, gender and race were not related (p > 0.05). Chi-square analysis revealed no significant differences across gender, race, and age in relation to the frequency of online social interactions and experiences, impact of online activity on mental health, victimization (Factor 2), or internalizing experiences (Factor 3; p > 0.05).
Discussion
This study aimed to advance our understanding of online social interactions and experiences among youth with psychosis. Given adolescents’ and young adults’ widespread use of the internet and social media for social experiences and interactions, and the limited number of validated assessments to assess these interactions online, we developed the SMILE questionnaire to evaluate the type, frequency, and nature of online social interactions and experiences.
Our study found that social media was the most widely used online platform among young adults with psychosis, followed by two-way messaging and multiway video platforms. Our findings align with current usage patterns across the US demonstrating that adolescents and young adults regularly use social media sites like Instagram (62% and 71%, respectively), Snapchat (59% and 65%, respectively), and TikTok (48% and 67, respectively)19,57 and is consistent with prior research in young adults with psychosis reporting that social media sites are the most commonly used platform within this population, followed by texting and chatting.20,27,29,58 Additionally, our analyses indicated that increased age was slightly negatively correlated with positive engagement online, which is consistent with age-related patterns in prior research reflecting negative correlations between age and use of online social platforms.20,28,59 It is important to note that our data were collected during the COVID-19 pandemic, a time when internet social interactions increased for many. 18 The paucity of research looking at online social experiences of young adults with psychosis even before the pandemic makes it difficult to examine how the behaviors and subjective experiences of online interactions and experiences reported in our study may compare. That said, specific findings from our study, such as the tendency for our sample to find support online more so than in-person and to regularly engage in chatting/messaging, speak to the utility of the internet to support continued engagement with others even in circumstances like a pandemic where in-person social contact is limited. Put differently, the lack of research on this population's online social interaction makes it difficult to compare pandemic and pre-pandemic behaviors and experiences; however, our data suggest that interactions with others regularly occurred online, and these included positive experiences.
We additionally found that the most frequently reported online behavior was scrolling/viewing content, providing important information about ways young adults with psychosis engage with their peers online. Commenting/posting, on the other hand, which can be considered a more active way of engaging with others online, occurred less frequently in our sample. It has been argued that posting or commenting may be considered a healthier way to engage with others online and has been equated with the more active processes required by in-person social interactions and experiences.32,34 While there is limited literature on active and passive use patterns in young adults with psychosis, some data has suggested that passively viewing social media content (i.e. scrolling) is associated with greater positive affect and increased self-esteem in individuals with psychosis. 60 On the other hand, it is possible that passive use may represent a behavioral manifestation of cognitive limitations often present in young adults with psychosis, or perhaps relate to negative symptoms or stigma impacting motivation to actively engage with others online.20,29 Of note, while our study found that young adults with psychosis post or comment online less frequently (i.e. “active” internet use), there was no identified relationship between this behavior and measures of psychotic symptoms. One interpretation of this finding is that posting and commenting behaviors may be a personal preference or are tied to some other individual-level variable such as extraversion, rather than tied to the presence of a psychotic spectrum disorder diagnosis. More work is needed to delineate the potential benefits and drawbacks of active versus passive use in this population and to explore how the type of online engagement impacts the well-being of young adults with psychosis.
In our study, the least commonly used platforms were dating apps, blogs, and chatrooms. In general, the use of blogs and chatrooms has decreased significantly over the past 15 years in the general population, 61 so it is likely that the relatively low frequency of blog and chatroom use may be due to the fact that they are now outdated. On the other hand, the frequency of dating app use in our sample was significantly lower than usage rates among young adults under 30 in the general population. 16 While specific data on dating app use within individuals with psychosis is very limited, a recent systematic review on the impact of romantic relationships on the well-being of adults with psychosis found both positive and negative effects. 62 Related research has indicated barriers to dating in this population include stigma, lack of experience or confidence in dating, perceived “risk” of romantic relationships, and social anxiety,63–65 and it is likely that these perceived barriers also translate to lower dating app usage. Recent intervention research has proven successful in improving dating confidence and increasing romantic interactions of young men with psychosis, 66 however, more work is needed to explore this outcome across other demographic characteristics, as well as barriers to dating and dating app use as identified by young people with psychosis.
Three dimensions emerged from the latent factor analysis on items describing whether a range of experiences were felt to occur more online versus offline. Across the three dimensions of social experiences (positive engagement, victimization, and internalizing experiences), we found preliminary evidence that participants who reported better functioning in the friends and activities dimension of the FESFS reported experiencing less victimization (i.e. Factor 2) offline and more victimization online. Activities listed on this FESFS dimension were qualitatively positive, 36 and this finding suggests that people who do better with social functioning with friends and activities may be less likely to experience victimization offline. An additional interpretation is that the more interactions young people with psychosis have with others overall, even if positive, the greater the possibility of experiencing victimization or negative social interactions. This interpretation is consistent with prior research findings that internet use within this population may be both beneficial for social connection and can contribute to negative affective states and experiences depending on the type and frequency of use.20,31,32,60 Interestingly, while there was a moderate relationship between victimization (Factor 2) and internalizing experiences (Factor 3), the latter was not associated with the frequency of overall online social experiences. This aligns with the notion that it is not online time alone that contributes to negative internal experiences, but rather specific negative processes such as unhealthy social comparisons 41 , 67 or negative experiences (i.e. victimization), as evidenced by our findings. Additionally, our findings indicated that greater frequency of overall online social experiences was related to both positive engagement and victimization, again supporting the conclusion that exposure to online social interactions and experiences could have both positive and negative impact on young people with psychosis. There was no correlation, however, between the frequency of online social experiences and psychotic symptoms. One explanation could be that patterns of online social experience frequency may be less related to symptoms of psychosis and more related to individual differences (e.g. affective state, age, etc.) or situational variables, as observed in our findings and past research.20,27,28
Our study found that social interactions in both online and offline settings are associated with a range of positive and negative subjective experiences for young people with psychosis. This finding highlights that positive and/or negative social interactions and experiences are not limited to a single setting (i.e. online or offline). Importantly, 8%–27% of our sample reported that they were more likely to engage in positive social experiences online rather than offline, suggesting that the internet and social media are important outlets for healthy social activity. It is likely that young people with psychosis select the setting that best aligns with their needs, desires, and available resources (e.g. meeting others with similar mental health experiences) and thus, having the option to leverage the internet and social media is critical, especially for those who may not be able to experience positive social interactions offline. Future research should seek to identify the most effective avenues to address social interactions and experiences, both online and offline to fully support individuals’ social goals. On one hand, individuals with psychosis may gravitate toward the comfort of the Internet, given established barriers to in-person social interactions (e.g. stigma, social anxiety, and isolation), which is consistent with our finding that negative internalizing experiences were more likely to occur offline than online. On the other hand, stigma and victimization are known to occur frequently online, especially in individuals with psychiatric disorders 68 , 69 Notably, this latter pattern was not observed in our sample, suggesting that online outlets sought by young people with psychosis may be generally positive. It is also important to note that content individuals are exposed to online is guided by many factors including intentional actions (e.g. search terms, contacting specific people) and algorithms based on internet use data. This latter factor has been shown to impact wellbeing and affect following online activity 70 and in the context of our results, may indicate that our sample's online activities did not expose them to negative content. Our sample largely reported negative experiences, as “Not Applicable” neither online nor offline, suggesting that our sample may have had overall fewer negative social experiences and interactions directed at them, regardless of setting. However, our findings do not account for witnessing racism, sexism, and other negative experiences directed at others. Taken together, our findings suggest that a new way of understanding social patterns in young adults with early psychosis is necessary. Clinicians and researchers alike need to redefine normative, healthy, and unhealthy social interactions and behaviors and to include both online and offline interactions and experiences when assessing social habits and supporting social recovery.
There are a few noteworthy limitations to our study. Our sample's size was relatively small, and future research may wish to sample a larger and more diverse group of individuals, over multiple timepoints. Questionnaire development did not include direct input from our population of interest. Future work should consider focus groups or involvement from individuals with psychosis to better incorporate the lived experiences of young people. This may aid in more accurately capturing the breadth of online interactions and experiences of emerging adults with psychosis. While we captured the relative degree to which experiences occurred online and offline, the absolute degree (i.e. quantity) of these experiences occurred was not captured. We also chose to explore the relationship between SMILE and peer victimization, symptoms of psychosis, and a measure of social functioning selected for its inclusion of social functioning online, however, there are other relevant clinical measures such as measures of anxiety, mood, and negative symptoms of psychosis that should be considered. By exploring relationships between the SMILE questionnaire and these well-established clinical constructs, future research may be able to draw clearer conclusions on the mechanisms underlying social experiences and preferences for social interactions across both in-person and online settings. Finally, we collected cross-sectional data at a single timepoint from individuals with psychosis. Past research has indicated that online activity patterns may fluctuate depending on psychotic symptom severity. 71 Future research would benefit from collecting data across multiple timepoints, across a range of psychotic symptom severity (e.g. clinical high-risk versus first episode psychosis or recurrent psychosis), or measuring time since diagnosis to better understand changes, if any, in social interactions and experiences across settings and stage of illness.
Conclusions and future directions:
Our findings support the hypothesis that young people with psychosis have both positive and negative experiences online, and that interactions online are not consistently associated with negative outcomes (e.g. victimization or internalizing experiences) at rates greater than offline interactions. Our results provide further support for the need to redefine our understanding and assessment of healthy and unhealthy social interactions and experiences in young adults with psychosis.
The distinction between offline activities and online activities is becoming increasingly blurred. To truly support the social goals of young adults with early psychosis, we need to fully appreciate their online interactions without the outdated assumption that online social interactions are somehow negative or a lesser form of in-person interactions. Based on our findings, young adults with psychosis rely on online and offline settings for a range of social experiences and interactions, and at minimum, clinicians should inquire about platform preferences for social interactions. Additionally, our results indicate that both active (e.g. commenting/posting) and passive (e.g. scrolling and watching) behaviors are common in young adults with psychosis and clinicians could query about these activities’ relationship to emotions and cognitions to better understand the function that online experiences have in patients’ broader social experiences.
Additionally, more research is needed to better delineate the many ways in which young adults with psychiatric disorders engage with others online beyond the type and frequency of use. This will require the development of new scales and measures designed to comprehensively assess the nature and function of online social experiences. This information can then be used to support the development of novel interventions aiming to leverage the benefits of social media and the internet while reducing their risks. Additionally, clinicians and researchers will need to remain actively engaged and up-to-date as new online opportunities to interact emerge and the online landscape continues to evolve.
Supplemental Material
Supplemental material, sj-docx-1-dhj-10.1177_20552076241277186 for Exploring online and offline social experiences and interaction patterns of young adults with psychosis with the social media and internet social engagement questionnaire: Analyses and future directions by Ivy Tran, Sunny X Tang, Amit Baumel, Tyler Moore, Sarah Berretta, Leily Behbehani and Michael L Birnbaum in DIGITAL HEALTH
Acknowledgements
We would like to acknowledge Moein Foroughi, MD, for his technical assistance in this research.
Footnotes
Contributorship: IT, ST, and MB conceived the study. IT completed the literature review and wrote the first draft and incorporated subsequent revisions to the manuscript. All authors reviewed and edited the manuscript and approved the final version. ST conducted all statistical analyses of data. AB was involved in questionnaire refinement and provided consultation on considerations for scale development. TM provided consultation on statistical plans and analyses. LB and SB recruited participants, conducted study visits, and participated in brainstorming questionnaire items and refinement.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The data reported in this article were collected with approval from the Institutional Review Board of the Feinstein Institute for Medical Research, Northwell Health, 125 Community Drive, Great Neck, NY 11021, (516) 465-1910, (IRB# 21-0017).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Publication of this article was supported by funding from New York State Psychiatric Institute.
Guarantor: IRT.
ORCID iD: Ivy Tran https://orcid.org/0000-0002-5781-5097
Supplemental material: Supplemental material for this article is available online.
References
- 1.Baumeister RF, Leary MR. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol Bull 1995; 117: 497–529. [PubMed] [Google Scholar]
- 2.Fowler D, Hodgekins J, French P, et al. Social recovery therapy in combination with early intervention services for enhancement of social recovery in patients with first-episode psychosis (SUPEREDEN3): a single-blind, randomised controlled trial. Lancet Psychiatry 2018; 5: 41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reis HT, Clark MS, Holmes JG. Perceived partner responsiveness as an organizing construct in the study of intimacy and closeness. In: Handbook of closeness and intimacy. Mahwah, New Jersey, USA: Lawrence Erlbaum Associates Publishers, 2004, pp.201–225. [Google Scholar]
- 4.Berkman LF. Which influences cognitive function: living alone or being alone? Lancet 2000; 355: 1291. [DOI] [PubMed] [Google Scholar]
- 5.Sandoval LR, Lopez Gonzalez B, Stone WS, et al. Effects of peer social interaction on performance during computerized cognitive remediation therapy in patients with early course schizophrenia: a pilot study. Schizophr Res 2019; 203: 17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Psychiatric Association. Schizophrenia spectrum and other psychotic disorders. In: American Psychiatric Association (ed) Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013, pp.87–90. [Google Scholar]
- 7.Simon GE, Coleman KJ, Yarborough BJH, et al. First presentation with psychotic symptoms in a population-based sample. Psychiatr Serv 2017; 68: 456–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gomes FV, Rincón-Cortés M, Grace AA. Adolescence as a period of vulnerability and intervention in schizophrenia: insights from the MAM model. Neurosci Biobehav Rev 2016; 70: 260–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Granholm E, Ben-Zeev D, Fulford Det al. et al. Ecological momentary assessment of social functioning in schizophrenia: impact of performance appraisals and affect on social interactions. Schizophr Res 2013; 145: 120–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mote J, Gard DE, Gonzalez Ret al. et al. How did that interaction make you feel? The relationship between quality of everyday social experiences and emotion in people with and without schizophrenia. PLoS One 2019; 14: e0223003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lemmers-Jansen I, Fett A, Hanssen E, et al. Learning to trust: social feedback normalizes trust behavior in first-episode psychosis and clinical high risk. Psychol Med 2019; 49: 780–790. [DOI] [PubMed] [Google Scholar]
- 12.Eglit GML, Palmer BW, Martin AS, et al. Loneliness in schizophrenia: construct clarification, measurement, and clinical relevance. PLoS One 2019; 13: e0194021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fett AJ, Hanssen E, Eemers M, et al. Social isolation and psychosis: an investigation of social interactions and paranoia in daily life. Eur Arch Psychiatry Clin Neurosci 2020; 272: 119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bornheimer LA, Li J, Im V, et al. The role of social isolation in the relationships between psychosis and suicidal ideation. Clin Soc Work J 2020; 48: 54–62. [Google Scholar]
- 15.Solmi M, Croatto G, Piva G, et al. Efficacy and acceptability of psychosocial interventions in schizophrenia: systematic overview and quality appraisal of the meta-analytic evidence. Mol Psychiatry 2023; 28: 354–368. [DOI] [PubMed] [Google Scholar]
- 16.Vogels EA, McClain C. Key findings about online dating in the U.S. Pew Research Center, https://pewrsr.ch/3HulOib (2023, accessed 10 November 2023).
- 17.Smith A. The internet and job seeking. Pew Research Center, https://www.pewresearch.org/internet/2015/11/19/1-the-internet-and-job-seeking/ (2015, accessed 19 November 2023).
- 18.McClain C, Vogels EA, Perrin A, et al. The internet and the pandemic. Pew Research Center, https://www.pewresearch.org/internet/2021/09/01/the-internet-and-the-pandemic/ (2021, accessed 24 May 2024).
- 19.Anderson M, Faverio M, Gottfried J. Teens, social media and technology 2023. Pew Research Center, https://pewrsr.ch/3pc9pXn. (2023, accessed 6 May 2024).
- 20.Jakubowska A, Kaselionyte J, Priebe Set al. et al. Internet use for social interaction by people with psychosis: a systematic review. Cyberpsychol Behav Soc Network 2019; 22: 336–343. [DOI] [PubMed] [Google Scholar]
- 21.Veling W, Pot-Kolder R, Counotte JM, et al. Environmental social stress, paranoia and psychosis liability: a virtual reality study. Schizophr Bull 2016; 42: 1363–1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hasan AA, Musleh M. Self-stigma by people diagnosed with schizophrenia, depression and anxiety: cross-sectional survey design. Perspect Psychiatr Care 2018; 54: 142–148. [DOI] [PubMed] [Google Scholar]
- 23.Hunt MG, Marx R, Lipson Cet al. et al. No more FOMO: limiting social media decreases loneliness and depression. J Soc Clin Psychol 2018; 37: 751–768. [Google Scholar]
- 24.Twenge JM, Joiner TE, Rogers MLet al. et al. Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time. Clin Psychol Sci 2018; 6: 3–17. [Google Scholar]
- 25.McEnery C, Lim MH, Knowles A, et al. Social anxiety in young people with first-episode psychosis: pilot study of the EMBRACE moderated online social intervention. Early Interv Psychiatry 2021; 15: 76–86. [DOI] [PubMed] [Google Scholar]
- 26.Athanasopoulou C, Välimäki M, Koutra K, et al. Internet use, eHealth literacy and attitudes toward computer/internet among people with schizophrenia spectrum disorders: a cross-sectional study in two distant European regions. BMC Med Inform Decis Mak 2017; 17: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gay K, Torous J, Joseph A, et al. Digital technology use among individuals with schizophrenia: results of an online survey. JMIR Ment Health 2016; 3: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller BJ, Stewart A, Schrimsher J, et al. How connected are people with schizophrenia? Cell phone, computer, email, and social media use. Psychiatry Res 2015; 225: 458–463. [DOI] [PubMed] [Google Scholar]
- 29.Rekhi G, Ang MS, Lee J. Clinical determinants of social media use in individuals with schizophrenia. PLoS One 2019; 14: e0225370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Valkenburg PM, Peter J, Walther JB. Media effects: theory and research. Annu Rev Psychol 2016; 67: 315–338. [DOI] [PubMed] [Google Scholar]
- 31.Verduyn P, Ybarra O, Résibois M, et al. Do social network sites enhance or undermine subjective well-being? A critical review. Soc Issues Policy Rev 2017; 11: 274–302. [Google Scholar]
- 32.Verduyn P, Gugushvili N, Massar K, et al. Social comparison on social networking sites. Curr Opin Psychol 2020; 36: 32–37. [DOI] [PubMed] [Google Scholar]
- 33.Meier A, Krause V. Does passive social media use harm well-being? J Media Psychol 2022; 35: 169–180. [Google Scholar]
- 34.Valkenburg PM, Beyens I, Pouwels JL, et al. Social media browsing and adolescent well-being: challenging the “passive social media use hypothesis”. J Comput Mediat Commun 2022: 27: zmab020. [Google Scholar]
- 35.Bjornestad J, Hegelstad WTV, Berg H, et al. Social media and social functioning in psychosis: a systematic review. J Med Internet Res 2019; 21: e13957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lecomte T, Corbière M, Ehmann T, et al. Development and preliminary validation of the First Episode Social Functioning Scale for early psychosis. Psychiatry Res 2016; 216: 412–417. [DOI] [PubMed] [Google Scholar]
- 37.Andreassen CS. Online social network site addiction: a comprehensive review. Curr Addict Rep 2015; 2: 175–184. [Google Scholar]
- 38.Kuss DJ, Griffiths MD. Social networking sites and addiction: ten lessons learned. Int J Environ Res Public Health 2017; 14: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abdel-Baki A, Lal S, Charron OD, et al. Understanding access and use of technology among youth with first-episode psychosis to inform the development of technology-enabled therapeutic interventions. Early Interv Psychiatry 2017; 11: 72–76. [DOI] [PubMed] [Google Scholar]
- 40.Lee J-Y, Chung Y-C, Song J-H, et al. Contribution of stress and coping strategies to problematic Internet use in patients with schizophrenia spectrum disorders. Compr Psychiatry 2018; 87: 89–94. [DOI] [PubMed] [Google Scholar]
- 41.Lee S, Lohrmann DK, Luo Jet al. et al. Social media use and its prospective association with mental health problems in a representative panel sample of US adolescents. Journal of Adolescent Health 2022; 70: 796–803. [DOI] [PubMed] [Google Scholar]
- 42.Scott ES, Canivet C, Östergren P-O. Investigating the effect of social networking site use on mental health in an 18–34 year-old general population; a cross-sectional study using the 2016 Scania Public Health Survey. BMC Public Health 2020; 20: 1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cornblatt BA, Auther AM, Naidich J, et al. Preliminary findings for two new measures of social and role functioning in the schizophrenia spectrum. Schizophr Bull 2007; 33: 484–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Endicott J, Spitzer RL, Fleiss JLet al. et al. The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976; 33: 766–771. [DOI] [PubMed] [Google Scholar]
- 45.Goldman HH, Skodol AE, Lave TR. Revising axis V for DSM-IV: a review of measures on social functioning. Am J Psychiatry 1992; 149: 1148–1156. [DOI] [PubMed] [Google Scholar]
- 46.Mynard H, Joseph S. Development of the multidimensional peer victimization scale. Aggress Behav 2000; 26: 169–178. [Google Scholar]
- 47.Joseph S, Stockton H. The multidimensional peer victimization scale: a systematic review. Aggress Violent Behav 2018; 42: 96–114. [Google Scholar]
- 48.Miller TJ, Cicchetti D, Markovich PJet al. et al. The SIPS screen: a brief self-report screen to detect the schizophrenia prodrome. Schizophr Res 2004; 70: 78. [Google Scholar]
- 49.Kline E, Wilson C, Ereshefsky S, et al. Psychosis risk screening in youth: a validation study of three self-report measures of attenuated psychosis symptoms. Schizophr Res 2012; 141: 72–77. [DOI] [PubMed] [Google Scholar]
- 50.Pagdon S, Jones N. Psychosis outside the box: a user-led project to amplify the diversity and richness of experience described as psychosis. Psychiatr Serv 2013; 74: 760–763. [DOI] [PubMed] [Google Scholar]
- 51.Pelizza L, Azzali S, Garlassi S, et al. A 2-year longitudinal study on subjective experience of social cognition in young people with first episode psychosis. Acta Esp Psiquiatr 2020; 48: 287–301. [PubMed] [Google Scholar]
- 52.Ritunnano R, Kleinman J, Oshodi DW, et al. Subjective experience and meaning of delusions in psychosis: a systematic review and qualitative evidence synthesis. Lancet Psychiatry 2022; 9: 458–476. [DOI] [PubMed] [Google Scholar]
- 53.Revelle W. psych: procedures for psychological, psychometric, and personality research. (R package version 2.1.9). Northwestern University, https://CRAN.R-project.org/package=psych. (2021).
- 54.Champely S. pwr: Basic functions for power analysis [internet]. R package version 1.3-0. 2020 [cited 2024 May 24].
- 55.Breiman L. Manual for setting up, using, and understanding random forest V4.0, https://www.stat.berkeley.edu/∼breiman/Using_random_forests_v4.0.pdf. (2003, accessed November 2023).
- 56.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B: Stat Methodol 1995; 57: 289–300. https://www.jstor.org/stable/2346101 . [Google Scholar]
- 57.Auxier B, Anderson M. Social media use in 2021. Pew Research Center, https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/ (2021, accessed November 2023).
- 58.Torous J, Keshavan M. The role of social media in schizophrenia: evaluating risks, benefits, and potential. Curr Opin Psychiatry 2016; 29: 190–195. [DOI] [PubMed] [Google Scholar]
- 59.Villagonzalo K, Arnold C, Farhall J, et al. Predictors of overall and mental health-related internet use in adults with psychosis. Psychiatry Res 2019; 278: 12–18. [DOI] [PubMed] [Google Scholar]
- 60.Berry N, Emsley R, Lobban Fet al. et al. Social media and its relationship with mood, self-esteem and paranoia in psychosis. Acta Psychiatr Scand 2018; 138: 558–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Social Media and young adults. Pew Research Center: Internet, Science & Tech, https://www.pewresearch.org/internet/2010/02/03/social-media-and-young-adults/. (2010, accessed 9 February 2024).
- 62.White E, Haddock G, Campodonico C, et al. The influence of romantic relationships on mental wellbeing for people who experience psychosis: a systematic review. Clin Psychol Rev 2021; 86: 102022. [DOI] [PubMed] [Google Scholar]
- 63.Cloutier B, Francoeur A, Samson C, et al. Romantic relationships, sexuality, and psychotic disorders: a systematic review of recent findings. Psychiatr Rehabil J 2021; 44: 22–42. [DOI] [PubMed] [Google Scholar]
- 64.Pillay E, Lecomte T, Abdel-Baki A. Factors limiting romantic relationship formation for individuals with early psychosis. Early Interv Psychiatry 2018; 12: 645–651. [DOI] [PubMed] [Google Scholar]
- 65.Redmond C, Larkin M, Harrop C. The personal meaning of romantic relationships for young people with psychosis. Clin Child Psychol Psychiatry 2010; 2: 151–170. [DOI] [PubMed] [Google Scholar]
- 66.Cloutier B, Lecomte T, Diotte F, et al. Improving romantic relationship functioning among young men with first-episode psychosis: impact of a novel group intervention. Behav Modif 2023; 47: 1170–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Appel H, Gerlach AL, Crusius J. The interplay between Facebook use, social comparison, envy, and depression. Curr Op in Psych 2016; 9: 44–49. [Google Scholar]
- 68.Korchmaros JD, Mitchell KJ, Ybarra ML. Technology-based interpersonal victimization: predictors of patterns of victimization over time. J Interpers Violence 2014; 29: 1297–1317. [DOI] [PubMed] [Google Scholar]
- 69.van den Eijnden R, Vermulst A, van Rooij AJ, et al. The bidirectional relationships between online victimization and psychosocial problems in adolescents: a comparison with real-life victimization. J Youth Adolesc 2014; 43: 790–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ostic D, Qalati SA, Barbosa B, et al. Effects of social media use on psychological well-being: a mediated model. Front Psychol 2021; 12: 678766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Birnbaum ML, Ernala SK, Rizvi AF, et al. Detecting relapse in youth with psychotic disorders utilizing patient-generated and patient-contributed digital data from Facebook. NPJ Schizophr 2019; 5: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dhj-10.1177_20552076241277186 for Exploring online and offline social experiences and interaction patterns of young adults with psychosis with the social media and internet social engagement questionnaire: Analyses and future directions by Ivy Tran, Sunny X Tang, Amit Baumel, Tyler Moore, Sarah Berretta, Leily Behbehani and Michael L Birnbaum in DIGITAL HEALTH