Abstract
Objectives
Safety policies enacted in response to the emergence of coronavirus disease 2019 (COVID‐19) have greatly affected the working environments of emergency medical service (EMS) clinicians. Our objective was to evaluate whether changes in the EMS environment during the COVID‐19 pandemic were associated with increased workplace conflict.
Methods
This evaluation was a cross‐sectional analysis of a random sample of 19,497 national certified EMS clinicians who were selected to receive an electronic survey in April 2022. The survey included an assessment of their level of stress using the Perceived Stress Scale instrument and examined changes in their working environment they perceived had occurred due to the emergence of COVID‐19. Logistic regression modeling was used to evaluate the associations between workforce demographics, infrastructure, scheduling, and policies to and COVID‐19‐induced coworker conflict.
Results
A total of 1686 responses were evaluated (response rate 10%). We found that COVID‐19 was reported to have exacerbated conflict between coworkers in 51% of responses. Respondents who perceived an increase in coworker conflict due to COVID‐19 self‐reported higher levels of stress than the rest of the respondents. Perceptions of the impact of COVID‐19 on conflict had also an association with the level of certification, indicating that national registered paramedics were more likely than emergency medical technicians to report coworker conflict due to COVID‐19 (adjusted odds ratio [AOR] 1.30, 95% confidence interval [CI] 1.05–1.61). Multivariable analysis highlighted the impact of mandatory overtime policies, reported by 27% of the respondents and associated with higher odds of exacerbated coworker conflict in our model (AOR 2.05, 95% CI 1.62–2.60).
Conclusions
These findings indicate that conflict can be considered a potential indicator of high levels of stress in the EMS workforce and may be a reliable signal to monitor when implementing mandates that affect EMS clinicians and their workloads.
Keywords: COVID‐19, coworker conflict, stress, workforce safety
1. INTRODUCTION
1.1. Background
Safety policies enacted in response to the coronavirus disease 2019 (COVID‐19) pandemic have greatly affected the working environments of emergency medical service (EMS) clinicians. These policies resulted in increased workloads, as a consequence of staffing shortages and mandatory overtime, 1 , 2 and the institution of strict infection control protocols, ranging from masking and social distancing to mandatory vaccinations. 3
1.2. Importance
EMS clinicians are normally considered at high risk for occupational stress. Potential stressors for these clinicians are related to the unpredictable nature of their work, which leaves them exposed to potential trauma 4 and to the organizational factors associated with a complex working environment, as well as a risk for conflict between coworkers. 5 Without the necessary resources to recover, these occupational stressors can lead to burnout, a long‐term stress reaction characterized by emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment. 6 In turn, burnout compromises the chances to retain EMS clinicians in the workforce—a longstanding concern in the prehospital community. 7
1.3. Goal of this investigation
It is unknown what impact the COVID‐19 pandemic had on the working environments of EMS clinicians. In this study, we investigate the frequency of the belief among EMS clinicians that COVID‐19 exacerbated coworker disputes, outline the connection between the stress perceived due to the pandemic and such conflicts, and delve into the possible mediating roles of working conditions and imposed safety measures.
2. METHODS
2.1. Study design and population
The present study was developed from a cross‐sectional analysis of a simple random sample of 19,497 EMS clinicians from the National Registry of Emergency Medical Technicians.
Originally designed to assess EMS clinicians’ burnout levels during the COVID‐19 pandemic via the Copenhagen Burnout Inventory, 8 the questionnaire included among its 40 items a request to list the types of workplace policies/programs that were introduced in response to the pandemic, an instrument to measure perceived stress, and a question aimed at establishing whether COVID‐19 was perceived to be responsible for conflict between coworkers.
Emails containing a unique questionnaire link were sent to this random sample of EMS clinicians in April 2022. Participants were not advised of the study goals or objectives. After the initial survey release, follow‐up reminder messages were sent approximately 1 and 2 weeks after the original email invitation, following the tailored Dillman methodology. 9 Completion of this survey had no bearing on National EMS Certification. The study received expedited approval from the Institutional Review Board of the American Institutes for Research in the Behavioral Sciences.
2.2. Measurements
The questionnaire asked: “Do you feel that COVID‐19 has exacerbated conflicts with your coworkers over the past 12 months?” This yes/no question was selected as the dependent variable of the present analysis.
The Perceived Stress Scale, in its 4‐item version (PSS4) 10 was adopted to provide a measure of self‐reported stress. Items on the scale asked respondents to assess the frequency of event‐specific stress (from 0 = never to 4 = very often). The total score was calculated by reverse coding positively worded items; values ranged from 0 to 16, with lower values indicating less perceived stress. We additionally asked about mandatory vaccination required in the workplace, mandatory overtime, and employer‐provided mental health support using a mark‐all‐that‐apply question that assessed the frequency of workplace policies related to the COVID‐19 pandemic. Respondents were also asked whether they had received any COVID‐19 vaccines, the number of days of absence from the job due to illness, the number of days of absence from the job due to COVID‐19, and the typical number of weekly activations.
Demographic characteristics were collected from respondents’ National EMS Certification database profile and linked to the survey results using a common identification number. EMS clinician demographics included sex, age, race/ethnicity, EMS certification level (emergency medical technician [EMT] or nationally registered paramedic [NRP]), and education level. The binary variable of sex was categorically designated as male or female. Age was analyzed as a continuous variable. Due to the small proportion of minority EMS clinicians, and race and ethnicity were dichotomized to non‐Hispanic white or all others. The other category included anyone who self‐identified as Black or African American, Asian, Hispanic or Latino, Asian or Native Hawaiian, or Pacific Islander. Educational level was categorized into less than high school/completed high school, some college, associate's degree, and bachelor's degree or higher. For the agency type where respondents worked, responses were categorized into fire, governmental non‐fire, hospital, private, or other.
The Bottom Line
Did COVID‐19 increase occupational stress for emergency medical services (EMS) clinicians, already known to be at high risk due to their stressful jobs? In this survey of nationally certified EMS clinicians, COVID‐19 was reported to contribute to conflict among coworkers in 51% of the respondents and was associated with higher levels of reported stress. In a profession already prone to burnout, monitoring stress and providing training about conflict management are sensible steps to help EMS clinicians feel more comfortable in their roles and may be especially critical in the event of future disruptions of traditional healthcare delivery.
2.3. Analysis
From this resulting dataset, descriptive statistics were calculated for respondent characteristics, vaccine receipt, and typical workload. Their association with coworker conflict was tested using Pearson's chi‐squared test or Fisher's exact test for categorical variables and the Wilcoxon rank sum test for continuous variables. A Welch's t‐test was performed to study the difference between perceived stress levels reported by the respondents who believed COVID‐19 exacerbated coworker conflict and those who did not. Associations between coworker conflict as a dependent variable, perceived stress, workplace policies related to COVID‐19, and respondent characteristics were tested using logistic regression. The model was developed in a backward stepwise fashion, with a Wald's test cutoff p‐value of 0.200. The final model fit was evaluated using the Hosmer–Lemeshow test and receiver operating characteristic curves.
Due to high rates of missing values, the days of absence due to COVID‐19 and the type of service provided at main EMS employer were not considered in the modeling step. The rate of missing values for the other variables was generally low. No attempts were made at imputation, and missing values were handled via pairwise deletion in univariable analyses and via listwise deletion in the multivariable logistic regression analysis. All analyses were conducted using R version 4.2.0 11 with the lmtest package 12 to implement Wald's test.
3. RESULTS
3.1. Descriptive statistics
The survey received 1881 responses (response rate = 10%). Out of the total survey respondents, 1686 (90%) answered the question: “Do you feel that COVID‐19 has exacerbated conflicts with your coworkers over the past 12 months?”
As shown in Table 1, respondents were almost three‐quarters male, with a median age of 40. A majority of respondents were non‐Hispanic white, while 13% belonged to an ethnic or racial minority group. Over half of them had an associate's degree or a higher level of education. Over three‐quarters of the respondents worked full‐time, and almost 90% had provided patient care in the previous 30 days. Their experience level varied, but over 40% had been in EMS for more than 15 years. EMTs and paramedics worked in various agency types while most worked in 9‐1‐1 services.
TABLE 1.
Demographic and workforce characteristics of survey respondents. Summary statistics are presented for the overall sample, and by the belief that COVID‐19 exacerbated coworker conflict. The reported frequencies are valid percentages calculated after excluding the missing values.
| Reported COVID‐19 exacerbated coworker conflict | ||||
|---|---|---|---|---|
| Characteristic | Overall, N = 1686 | No, N = 829 | Yes, N = 857 | p‐value a |
| Received any COVID‐19 vaccination | 0.2 | |||
| Yes | 1403 (84%) | 680 (83%) | 723 (85%) | |
| No | 263 (16%) | 139 (17%) | 124 (15%) | |
| Unknown | 20 | 10 | 10 | |
| Sex | >0.9 | |||
| Female | 448 (27%) | 220 (27%) | 228 (27%) | |
| Male | 1224 (73%) | 602 (73%) | 622 (73%) | |
| Unknown | 14 | 7 | 7 | |
| Age (median, IQR) | 40 (31, 51) | 41 (31, 52) | 40 (31, 51) | 0.2 |
| Race/Ethnicity | 0.4 | |||
| White, non‐Hispanic | 1410 (87%) | 692 (86%) | 718 (88%) | |
| All others | 208 (13%) | 108 (14%) | 100 (12%) | |
| Unknown | 68 | 29 | 39 | |
| Certification level | 0.007 | |||
| EMT | 551 (33%) | 297 (36%) | 254 (30%) | |
| NRP | 1135 (67%) | 532 (64%) | 603 (70%) | |
| Education | 0.5 | |||
| High school or less | 189 (11%) | 89 (11%) | 100 (12%) | |
| Some college | 523 (31%) | 248 (30%) | 275 (32%) | |
| Associate's degree | 321 (19%) | 157 (19%) | 164 (19%) | |
| Bachelor's degree or higher | 653 (39%) | 335 (40%) | 318 (37%) | |
| Agency type | >0.9 | |||
| Fire | 489 (35%) | 233 (35%) | 256 (36%) | |
| Private | 348 (25%) | 166 (25%) | 182 (25%) | |
| Gov Non‐Fire | 247 (18%) | 120 (18%) | 127 (18%) | |
| Hospital | 184 (13%) | 87 (13%) | 97 (13%) | |
| Other | 121 (8.7%) | 62 (9.3%) | 59 (8.2%) | |
| Unknown | 297 | 161 | 136 | |
| Type of service provided at main EMS employer | 0.8 | |||
| 911 | 535 (72%) | 261 (74%) | 274 (71%) | |
| Medical transport | 37 (5.0%) | 15 (4.2%) | 22 (5.7%) | |
| 911 & Medical transport | 128 (17%) | 58 (16%) | 70 (18%) | |
| Clinical services | 0 (0%) | 0 (0%) | 0 (0%) | |
| MIHCP | 9 (1.2%) | 4 (1.1%) | 5 (1.3%) | |
| Other | 34 (4.6%) | 17 (4.8%) | 17 (4.4%) | |
| Unknown | 943 | 474 | 469 | |
| Years of experience | 0.2 | |||
| Less than 5 years | 361 (21%) | 193 (23%) | 168 (20%) | |
| 5–15 years | 634 (38%) | 301 (36%) | 333 (39%) | |
| More than 15 years | 691 (41%) | 335 (40%) | 356 (42%) | |
| Employment status | 0.3 | |||
| Part time | 154 (11%) | 80 (12%) | 74 (10%) | |
| Full time | 1049 (77%) | 493 (75%) | 556 (78%) | |
| Volunteer | 168 (12%) | 88 (13%) | 80 (11%) | |
| Unknown | 315 | 168 | 147 | |
| Pt care professional in the past 30 days | 0.6 | |||
| Yes | 1498 (89%) | 740 (90%) | 758 (89%) | |
| No | 181 | 86 (10%) | 95 (11%) | |
| Unknown | 7 | 3 | 4 | |
| No. of weekly calls | 0.5 | |||
| Less than 5 calls | 393 (23%) | 203 (24%) | 190 (22%) | |
| 5–9 calls | 265 (16%) | 126 (15%) | 139 (16%) | |
| 10–19 calls | 425 (25%) | 205 (25%) | 220 (26%) | |
| 20–29 calls | 294 (17%) | 153 (18%) | 141 (16%) | |
| 30 or more calls | 309 (18%) | 142 (17%) | 167 (19%) | |
| Days absent in the past 12 months due to illness (Median, IQR) | 0.0 (0.0, 3.0) | 0.0 (0.0, 3.0) | 0.0 (0.0, 3.0) | 0.3 |
| Unknown | 33 | 12 | 21 | |
| Days absent in the past 12 months due to COVID‐19 illness (Median, IQR) | 1.0 (0.0, 5.0) | 1.0 (0.0, 5.0) | 1.0 (0.0, 5.0) | 0.7 |
| Unknown | 1035 | 521 | 514 | |
Abbreviations: COVID‐19, coronavirus disease 2019; EMT, emergency medical technician; NRP, national registry paramedic; Gov Non‐Fire, government non‐fire; MIHCP, mobile integrated health community paramedicine; Pt, patient; IQR, interquartile range.
Pearson's chi‐squared test; Wilcoxon rank sum test; Fisher's exact test.
We found that COVID‐19 was reported to contribute to conflict among coworkers in 51% of the cases. When we compared individuals who reported conflict with those who did not, we found no significant differences in their demographic characteristics, whether they had received a COVID‐19 vaccine, or their overall work qualifications—except for their level of certification.
3.2. Perceived stress among EMS clinicians
Table 2 summarizes the four items comprising the reduced PSS4. Each item was associated with the perception of COVID‐19 as a factor in coworker conflict.
TABLE 2.
EMS clinicians’ perceived stress assessed by the Perceived Stress Scale (PSS4), overall and stratified by respondent experience of coronavirus disease 2019 (COVID‐19) and coworker conflict. Frequencies are valid percentages calculated after excluding the missing values.
| COVID‐19 exacerbated coworker conflict | ||||
|---|---|---|---|---|
| Perceived Stress Scale | Overall, N = 1686 a | No, N = 829 a | Yes, N = 857 a | p‐value b |
| Over the past 4 weeks, how often have you felt you were unable to control important things? | <0.001 | |||
| Very often | 61 (3.6%) | 28 (3.4%) | 33 (3.9%) | |
| Fairly often | 165 (9.8%) | 78 (9.4%) | 87 (10%) | |
| Sometimes | 600 (36%) | 232 (28%) | 368 (43%) | |
| Almost never | 520 (31%) | 274 (33%) | 246 (29%) | |
| Never | 333 (20%) | 215 (26%) | 118 (14%) | |
| Unknown | 7 | 2 | 5 | |
| Over the past 4 weeks, how often have you felt confident about your ability to handle problems? | <0.001 | |||
| Very often | 546 (33%) | 317 (39%) | 229 (27%) | |
| Fairly often | 550 (33%) | 274 (33%) | 276 (32%) | |
| Sometimes | 409 (24%) | 156 (19%) | 253 (30%) | |
| Almost never | 109 (6.5%) | 45 (5.5%) | 64 (7.5%) | |
| Never | 61 (3.6%) | 31 (3.8%) | 30 (3.5%) | |
| Unknown | 11 | 6 | 5 | |
| Over the past 4 weeks, how often have you felt things were going your way? | <0.001 | |||
| Very often | 189 (11%) | 122 (15%) | 67 (7.9%) | |
| Fairly often | 583 (35%) | 315 (38%) | 268 (31%) | |
| Sometimes | 637 (38%) | 287 (35%) | 350 (41%) | |
| Almost never | 221 (13%) | 83 (10%) | 138 (16%) | |
| Never | 46 (2.7%) | 17 (2.1%) | 29 (3.4%) | |
| Unknown | 10 | 5 | 5 | |
| Over the past 4 weeks, how often have you felt difficulties were piling up so high you that you could not overcome them? | <0.001 | |||
| Very often | 58 (3.5%) | 20 (2.4%) | 38 (4.5%) | |
| Fairly often | 155 (9.2%) | 63 (7.6%) | 92 (11%) | |
| Sometimes | 565 (34%) | 232 (28%) | 333 (39%) | |
| Almost never | 566 (34%) | 294 (36%) | 272 (32%) | |
| Never | 334 (20%) | 216 (26%) | 118 (14%) | |
| Unknown | 8 | 4 | 4 | |
n (%).
Pearson's chi‐squared test.
The summary PSS4 scores for the EMS clinicians who experienced exacerbated conflict with coworkers and those who did not are shown in Figure 1. The first group reported a level of perceived stress that was, on average, 1.22 points higher than the latter (95% confidence interval [CI] 0.93–1.52, Welch's t‐test = 8.13, df = 1654.29, p < 0.001).
FIGURE 1.
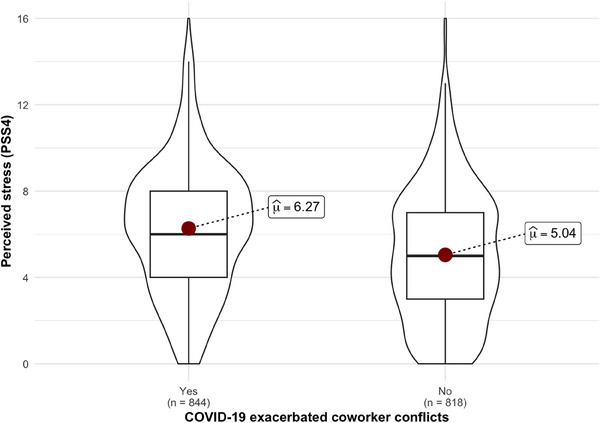
Emergency medical service (EMS) clinicians’ perceived stress.
3.3. Predictors of coworker conflict
The final model, built via backward stepwise regression, included six survey variables: the respondent's perceived stress level, the three indicators of COVID‐19‐related workplace policies, the respondent certification, and the volume of calls answered weekly (Table 3). Logistic regression analysis confirmed that higher stress levels were associated with a higher likelihood of coworker conflict perceived to be due to COVID‐19 (odds ratio [OR] 1.14, 95% CI 1.10–1.18; adjusted odds ratio [AOR] 1.12, 95% CI 1.09–1.16).
TABLE 3.
Univariable and multivariable logistic regression model results.
| Univariable regression | Multivariable regression | |||
|---|---|---|---|---|
| Outcome: Conflict | OR (95% CI)a | p‐value | AOR (95% CI)a | p‐value |
| Perceived stress (PSS4) | 1.14 (1.10–1.18) | <0.001 | 1.12 (1.09–1.16) | <0.001 |
| Mandatory overtime | <0.001 | <0.001 | ||
| No | Ref. | Ref. | ||
| Yes | 2.19 (1.76–2.74) | 2.05 (1.62–2.60) | ||
| Mandatory vaccination | 0.019 | 0.065 | ||
| No | Ref. | Ref. | ||
| Yes | 1.26 (1.04–1.53) | 1.21 (0.99–1.48) | ||
| Mental health support | 0.006 | 0.076 | ||
| No | Ref. | Ref. | ||
| Yes | 0.72 (0.58–0.91) | 0.80 (0.63–1.02) | ||
| Certification level | 0.007 | 0.018 | ||
| EMT | Ref. | Ref. | ||
| NRP | 1.33 (1.08–1.63) | 1.30 (1.05–1.61) | ||
| No. of weekly calls | 0.46 | 0.19 | ||
| Less than 5 calls | Ref. | Ref. | ||
| 5–9 calls | 1.18 (0.86–1.61) | 1.16 (0.84–1.61) | ||
| 10–19 calls | 1.15 (0.87–1.51) | 0.95 (0.71–1.27) | ||
| 20–29 calls | 0.98 (0.73–1.33) | 0.76 (0.55–1.05) | ||
| 30 or more calls | 1.26 (0.93–1.69) | 0.91 (0.66–1.25) | ||
Abbreviations: AOR, adjusted odds ratio; CI, confidence Interval; EMT, emergency medical technician; NRP, national registered paramedic; OR, odds ratio.
In addition, all three variables derived from the survey and connected to workplace‐related policies were retained in the analysis: mandatory overtime (reported by 460 or 27% of the respondents), vaccine mandate (738; 44%), and mental health support (381; 23%). In univariable logistic regression models, increased odds of exacerbated conflict were found in the presence of workplace policies regulating mandatory overtime (OR 2.19, 95% CI 1.76–2.74) and obligatory COVID‐19 vaccinations (OR 1.26, 95% CI 1.04–1.53). However, employer‐provided mental health support demonstrated a mitigating effect (OR 0.72, 95% CI 0.58–0.91). Mandatory overtime policies continued to be associated with higher odds of exacerbated coworker conflict in the multivariable model (AOR 2.05, 95% CI 1.62–2.60).
Finally, while the volume of calls addressed by the respondents did not reflect a relationship with the dependent variable, the analysis of the certification type showed that national registered paramedics were more likely than EMTs to report experiences of coworker conflict due to COVID‐19 (OR 1.33, 95% CI 1.08–1.63; AOR 1.30, 95% CI 1.05–1.61).
4. LIMITATIONS
The Perceived Stress Scale from Cohen and Williamsons is not a diagnostic scale and therefore cannot be used to classify respondents as suffering from stress. Other studies that addressed the issue of stress among EMS clinicians relied on the DASS‐21, 4 a psychological scale used to assess the prevalence of depression, and stress and assign case–control status. 13 Nonetheless, the PSS4 instrument remains a useful tool for highlighting the link between stress and conflict in the workplace at the center of the present investigation.
Despite the relatively large number of respondents who completed the survey, this study was also limited by the survey response rate and the accompanying likely response bias as well as by incomplete or missing responses in a small percentage of participants. Finally, this cross‐sectional survey examined the associations between our variables of interest and could not determine causality.
5. DISCUSSION
Our study shows that stress reported by EMS clinicians was strongly associated with the belief that COVID‐19 increased conflict in the workplace. Effective teamwork is crucial in EMS, but workplace incivility can disrupt team dynamics and communication and can be particularly harmful in the high‐stress environment of emergency response. 14 Breakdowns in teamwork can also potentially impact the quality of care provided during public health emergencies such as experienced with the COVID‐19 pandemic. Previous EMS studies 15 , 16 found that nearly half of EMS clinicians experienced incivility from supervisors or coworkers on a weekly basis, and this was associated with factors such as female sex, higher certification levels, and higher call volumes. Exposure to incivility has also been linked to burnout, with consequent dissatisfaction with work, increased stress levels, intent to leave the job, and higher workplace absences. 15 Furthermore, Kfouri and Lee 5 found that healthcare professionals feel undertrained and unprepared to manage workplace conflict and need more conflict management training, suggesting additional stressors from workplace incivility.
During the recent pandemic, an increase in job demands in the form of mandatory overtime, while necessary to address the challenges presented by the spread of COVID‐19, might have lessened the sense of control that workers felt over their workloads and schedules. 17 It is likely that mandatory overtime exacerbated worker perceptions of environmental stress (related to allocation of human resources), unreasonable work expectations (in the form of policies, rules, and time restrictions), and unrealistic expectations (regarding workload), all of which have been previously identified as sources of conflict. 5 , 18 In fact, staffing difficulties and being overworked was a prominent theme in our analysis of EMS worker descriptions of the nature of workplace conflict, and found to co‐occur with stress and burnout‐related fatigue. 19 Although not reported by most survey respondents, mandated overtime was the organizational factor with the biggest impact on our model, not offset by mental health support offered by employers to manage the stress inherent in prehospital settings during a pandemic. This finding echoes previous research in the field 20 that highlighted an association between job demands and burnout in EMS clinicians, on the one hand, and job benefits and less burnout, on the other hand. Taken together, these findings highlight the importance of addressing stress and burnout at the agency level, rather than focusing on the psychological characteristics of the individual EMS clinician.
Nationally registered paramedics in our sample had a higher likelihood of reporting coworker conflicts due to COVID‐19 when compared with the EMTs in our sample (AOR 1.30, 95% CI 1.05–1.61). The difference is significant, and in line with the results of other studies that see paramedics more at risk of experiencing workplace incivility 15 and burnout. 21 NRPs have different duties and responsibilities in relationship to their scope of practice that may impact workplace relationships and conflict in medical team performance. For example, NRPs more commonly care for higher acuity patients that require prehospital interventions and resuscitation, leading to more stressful interactions. Given that pandemic‐related staffing difficulties and mandatory overtime likely disrupted common workflow, with the added stress of clinically challenging cases presenting with COVID‐19, increased conflict may have been inevitable.
Respondents in our sample had slightly higher vaccination rates compared to other recently published studies on the topic, where COVID‐19 vaccination rates averaged around 75%. 22 , 23 Still, in our model, obligatory vaccinations could be described as a stressor. Critics of mandatory vaccinations argue that they infringe on individual rights and may not be effective in achieving desired outcomes. 24 In the study by Hubble and colleagues, only 18.7% of respondents supported mandatory vaccination for EMS clinicians. 23 In this regard, health care workers are not different from the general population, despite being exposed to more risks and tasked with caring for vulnerable patients. 25 All these factors should be considered when evaluating how potential stress and conflict affect worker well‐being and workplace dynamics, particularly during widespread emergencies. This evaluation remains a sensitive topic that needs to be addressed.
With an annual national demand for prehospital medical responses estimated at 28 million before the COVID‐19 pandemic, 26 both the mitigation of workforce‐reducing factors 27 and the ability to recruit clinicians in adequate numbers 28 are considered pressing issues. Furthermore, studies indicate that EMS clinicians would be more willing to work during pandemic events, provided they have training specific to responding to the related surges. 29
In conclusion, these findings indicate that conflict is a potential indicator of high levels of stress in the EMS workforce and may be a reliable signal to monitor when implementing mandates that affect EMS clinicians and their workloads. Given the aforementioned relationship between lack of preparation and stress, our findings also underscore that training related explicitly to pandemic care could include modules that anticipate or assuage some of the stress and conflict workers experience as they navigate these situations. Our results are aligned with other data in pointing to paramedics as a first group to target for such training, given that they are especially affected by these kinds of stress. These steps may be required because maintaining a robust EMS workforce and, by extension, the health of these professionals in its operational sphere is unquestionably essential to our preparedness for future interruptions in traditional healthcare delivery.
AUTHOR CONTRIBUTIONS
All authors conceived and designed the study. Jonathan R. Powell, Christopher B. Gage, and Ashish R. Panchal collected the data. Gennaro Di Tosto, Eben Kenah, and Ashish R. Panchal analyzed and interpreted the data. Gennaro Di Tosto drafted the manuscript in collaboration with all co‐authors. All authors contributed substantially to the revision of the manuscript. Gennaro Di Tosto takes responsibility for the paper as a whole.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Biography
Gennaro Di Tosto holds a PhD in cognitive science from the University of Padova, Italy. Before joining The Ohio State University School of Medicine in Columbus, OH, he was a research associate at the Cathie Marsh Institute for Social Research of the University of Manchester, UK.

Di Tosto G, Melnyk H, Powell JR, et al. COVID‐19 and coworker conflict among emergency medical service clinicians. JACEP Open. 2024;5:e13282. 10.1002/emp2.13282
A preliminary version of this work was presented as a poster during the Second annual NCI's Serological Science Network (SeroNet) Investigators Meeting, March 21‐23, 2023, Bethesda, MD.
Supervising editor: Karl Sporer, MD.
REFERENCES
- 1. Basting J, Wong J, Berger D, Caldwell C, Saggi S, Mann J. Prevalence of social needs & social risks among EMS providers. JEMS Exclus. 2023;2023. https://www.jems.com/administration‐and‐leadership/prevalence‐social‐needs‐social‐risks‐ems‐providers/ [PMC free article] [PubMed] [Google Scholar]
- 2. Sampaio F, Sequeira C, Teixeira L. Nurses’ mental health during the Covid‐19 outbreak: a cross‐sectional study. J Occup Environ Med. 2020;62(10):783‐787. doi: 10.1097/JOM.0000000000001987 [DOI] [PubMed] [Google Scholar]
- 3. Gostin LO, Salmon DA, Larson HJ. Mandating COVID‐19 vaccines. JAMA. 2021;325(6):532. doi: 10.1001/jama.2020.26553 [DOI] [PubMed] [Google Scholar]
- 4. Bentley MA, Crawford JM, Wilkins JR, Fernandez AR, Studnek JR. An assessment of depression, anxiety, and stress among nationally certified EMS professionals. Prehosp Emerg Care. 2013;17(3):330‐338. doi: 10.3109/10903127.2012.761307 [DOI] [PubMed] [Google Scholar]
- 5. Kfouri J, Lee PE. Conflict among colleagues: health care providers feel undertrained and unprepared to manage inevitable workplace conflict. J Obstet Gynaecol Can. 2019;41(1):15‐20. doi: 10.1016/j.jogc.2018.03.132 [DOI] [PubMed] [Google Scholar]
- 6. National Academy of Science, Engineering, and Medicine . Taking Action Against Clinician Burnout: A Systems Approach to Professional Well‐Being. The National Academies Press; 2019. doi: 10.17226/25521 [DOI] [PubMed] [Google Scholar]
- 7. Rivard MK, Cash RE, Woodyard KC, Crowe RP, Panchal AR. Intentions and motivations for exiting the emergency medical services profession differ between emergency medical technicians and paramedics. J Allied Health. 2020;49(1):53‐59. [PubMed] [Google Scholar]
- 8. Kristensen TS, Borritz M, Villadsen E, Christensen KB, The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress. 2005;19(3):192‐207. doi: 10.1080/02678370500297720 [DOI] [Google Scholar]
- 9. Dillman DA, Smyth JD, Christian LM. Internet, Phone Mail, and Mixed‐mode Surveys: The Tailored Design Method. 3rd ed. John Wiley & Sons Inc.; 2009. [Google Scholar]
- 10. Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapam S, Oskamp S, eds. The Social Psychology of Health. The Claremont Symposium on Applied Social Psychology. Sage Publications, Inc; 1988:31‐67. [Google Scholar]
- 11. R Core Team . R: a language and environment for statistical computing. Published online 2021. http://www.R‐project.org
- 12. Zeileis A, Hothorn T. Diagnostic checking in regression relationships. R News. 2002;2(3):7‐10. [Google Scholar]
- 13. Henry JD, Crawford JR. The short‐form version of the Depression Anxiety Stress Scales (DASS‐21): construct validity and normative data in a large non‐clinical sample. Br J Clin Psychol. 2005;44(2):227‐239. doi: 10.1348/014466505X29657 [DOI] [PubMed] [Google Scholar]
- 14. Abolfazl Vagharseyyedin S. Workplace incivility: a concept analysis. Contemp Nurse. 2015;50(1):115‐125. doi: 10.1080/10376178.2015.1010262 [DOI] [PubMed] [Google Scholar]
- 15. Cash RE, White‐Mills K, Crowe RP, Rivard MK, Panchal AR. Workplace incivility among nationally certified EMS professionals and associations with workforce‐reducing factors and organizational culture. Prehosp Emerg Care. 2019;23(3):346‐355. doi: 10.1080/10903127.2018.1502383 [DOI] [PubMed] [Google Scholar]
- 16. Lu DW, Shin J, Wan C, et al. Burnout and workplace incivility among emergency medical services practitioners: a preliminary report. Prehosp Emerg Care. 2023;27(4):413‐417. doi: 10.1080/10903127.2023.2175088 [DOI] [PubMed] [Google Scholar]
- 17. Häusser JA, Mojzisch A, Niesel M, Schulz‐Hardt S. Ten years on: a review of recent research on the Job Demand–Control (‐Support) model and psychological well‐being. Work Stress. 2010;24(1):1‐35. doi: 10.1080/02678371003683747 [DOI] [Google Scholar]
- 18. Parvaresh‐Masoud M, Cheraghi MA, Imanipour M. Workplace interpersonal conflict in prehospital emergency: concept analysis. J Educ Health Promot. 2021;10:347. doi: 10.4103/jehp.jehp_213_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Melnyk H, Di Tosto G, Powell J, Panchal AR, McAlearney AS. Conflict in the EMS workforce: an analysis of an open‐ended survey question reveals a complex assemblage of stress, burnout, and pandemic‐related factors influencing well‐being. Int J Environ Res Public Health. 2023;20(10):5861. doi: 10.3390/ijerph20105861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Crowe RP, Fernandez AR, Pepe PE, et al. The association of job demands and resources with burnout among emergency medical services professionals. JACEP Open. 2020;1(1):6‐16. doi: 10.1002/emp2.12014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Powell JR, Crowe RP, Gage CB, et al. National EMS clinician burnout levels demonstrate alarming increase from 2015 to 2022. Prehosp Emerg Care. 2023;27(Suppl 1):S1‐S96. doi: 10.1080/10903127.2022.2138658 [DOI] [PubMed] [Google Scholar]
- 22. Gregory ME, Powell JR, MacEwan SR, et al. COVID‐19 vaccinations in EMS professionals: prevalence and predictors. Prehosp Emerg Care. 2021. doi: 10.1080/10903127.2021.1993391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hubble MW, Renkiewicz GK, Hunter S, Kearns RD. Predictors of COVID‐19 vaccination among EMS personnel. West J Emerg Med. 2022;23(4):570‐578. doi: 10.5811/westjem.2022.4.54926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hayes L, Pollock AM. Mandatory covid‐19 vaccination for care home workers. BMJ. 2021;374:n1684. doi: 10.1136/bmj.n1684 [DOI] [PubMed] [Google Scholar]
- 25. Emanuel EJ, Skorton DJ. Mandating COVID‐19 vaccination for health care workers. Ann Intern Med. 2021;174:1308‐1310. doi: 10.7326/M21-3150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wang HE, Mann NC, Jacobson KE, et al. National characteristics of emergency medical services responses in the United States. Prehosp Emerg Care. 2013;17(1):8‐14. doi: 10.3109/10903127.2012.722178 [DOI] [PubMed] [Google Scholar]
- 27. Crowe RP, Bower JK, Cash RE, Panchal AR, Rodriguez SA, Olivo‐Marston SE. Association of burnout with workforce‐reducing factors among EMS professionals. Prehosp Emerg Care. 2018;22(2):229‐236. doi: 10.1080/10903127.2017.1356411 [DOI] [PubMed] [Google Scholar]
- 28. Powell JR, Cotto J, Kurth JD, Cash RE, Gugiu MR, Panchal AR. Impact of COVID‐19 on initial emergency medical services certification in the United States. J Am Coll Emerg Physicians Open. 2022;3(4). doi: 10.1002/emp2.12808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rebmann T, Charney RL, Loux TM, Turner JA, Abbyad YS, Silvestros M. Emergency medical services personnel's pandemic influenza training received and willingness to work during a future pandemic. Prehosp Emerg Care. 2020;24(5):601‐609. doi: 10.1080/10903127.2019.1701158 [DOI] [PMC free article] [PubMed] [Google Scholar]


