Abstract
Background
The European Thyroid Association Thyroid Imaging Data and Reporting Systems (EU-TIRADS) is widely used in the risk stratification of thyroid nodule malignancy. However, data on the subject in Sub-Saharan Africa are limited. The objective of this study is to evaluate the clinical, sonographic and histopathological concordance of thyroid nodules in the diagnosis of thyroid cancer.
Methods
This was an analytical cross-sectional study that examined the clinical, ultrasound and pathological data of 61 patients from 4 hospitals in the city province of Kinshasa over a period of 24 months, from June 01, 2020 to May 31, 2022.
Results
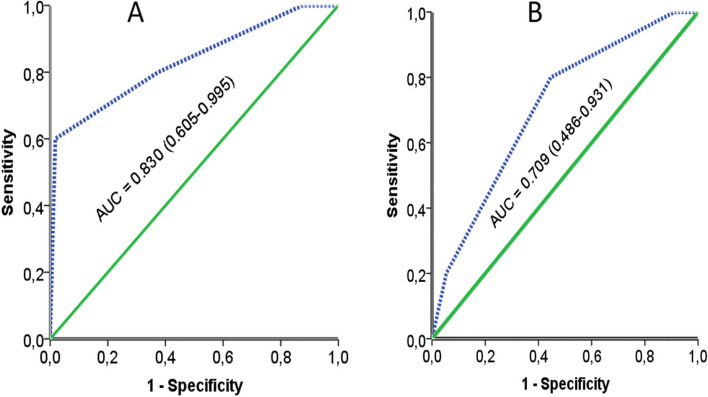
Of the 61 patients, their mean age was 47.38 ± 8.8 years. The mean clinical score of the patients was 3.4 ± 0.84 with the extremes ranging from 1 to 5. The majority of the patients were classified as having an intermediate risk, ie 85.2% of the cases. It was noted that 41% of the nodules had a high risk according to the EU-TIRADS score and 8.2% of the nodules were malignant after histopathological analysis. The ROC curves reported at the diagnosis of malignancy show an area under the curve of 0.709 with 95% CI (0.486–0.931), a Youden index of 0.769 for the clinical score, and an area under the curve of 0.830 with 95% CI (0.605–0.995), a Youden index of 0.772 for the EU-TIRADS score.
Conclusion
In a low-income country, a well-performed thyroid ultrasound and the well-applied clinical score could be an important tool in the selection of thyroid nodules suspected of malignancy and requiring histopathological examination to avoid excessive acts in the patient.
Keywords: Concordance, Clinical Score, EU-TIRADS, Histopathology, Democratic Republic of Congo
Introduction
A thyroid nodule (TN) is defined as a localized enlargement of the thyroid gland, whether palpable and/or clearly identified on ultrasound [1]. It can be single or multiple; in this case we speak of multi nodular goiter. Thyroid nodules represent a pathology with a very high prevalence since it affects approximately 15% of the world's population, with significant variations linked to geographical areas, environment and sex (with a proven female predominance) and age [2]. In the United States, the prevalences observed are on average 10 to 50%; while in Germany they are 20 to 29% [3]. In Africa, thyroid pathologies are dominated by goitres and thyroid nodules, followed by dysthyroidism [4]. In Cameroon, the prevalence of thyroid nodules is 28.3% according to Moifo et al. in 2013 [5]. In the Democratic Republic of Congo (DRC), this prevalence of cancerous nodules was 20% according to the study by Bukasa et al. in 2021 [6]. Surgery currently remains an important option in the treatment of certain thyroid conditions, particularly in the context of oncology. It is also a therapeutic choice in the face of large nodules, multinodular goiter and hyperthyroidism [3]. In its evolution, the TN is the site of morphological changes such as benign degeneration (95% of cases) and malignancy fortunately in a lesser proportion (5–10%); physiological changes by empowerment with inappropriate secretion independently of thyroid hormones (toxic nodule) [7]. Due to their growth, these NTs also cause aesthetic problems with exuberant cervical swellings seriously altering the psyche of the carrier patient and often requiring expensive surgical interventions sometimes enameled with dreadful complications [8]. The discovery of TN casts doubts on the possibility of cancer; the difficulty of defining with certainty its degree of malignancy [9]. This is as true for the patient haunted by the idea of a probable cancer as for the clinician faced with the difficulties of a lack of robust means of investigation to obtain an etiological diagnosis as well as a therapeutic that is not codified in our countries; precarious undergoing hormonal treatment or thyroid excision in principle [7]. In environments lacking robust morphological explorations such as scanner, Magnetic Resonance Imaging (MRI), nuclear medicine and PET-SCAN and anatomopathological examination (too expensive for our population); thyroid and cervical ultrasound as a reference diagnostic tool and an extension of the clinical examination [10] can provide reliable information likely to predict nodular benignity or malignancy to help clinicians in our developing countries to progress in the management and follow-up of nodular thyropathies. Thus, the objective of this study is to evaluate the clinical, sonographic and histopathological concordance of thyroid nodules in the diagnosis of thyroid cancer.
Patients and methods
Study population and design
This was a multicenter analytical cross-sectional study carried out at the Center Hospitalier Initiative Plus de Bibwa (CHIP/BIBWA), at the NGALIEMA Clinic, at the Center Médico-Chirurgical de Pigeon (CMCP) and at the University Clinics of Kinshasa (CUK) on a period of 24 months, from June 01, 2020 to May 31, 2022.
The population of this study was composed of all patients operated on for thyroid nodules during the study period at the hospitals mentioned above. Any patient with a thyroid nodule with available clinical, ultrasound and histopathological data. Patients with no histopathological data were not included in this study. Referring to the inclusion criteria, 61 patients met these criteria and constituted the sample size of the study.
Data collection and procedure
Variables of interests included: age, gender, Clinical Score, EU-TIRADS score, Histopathological diagnostics. A clinical malignancy risk score was designed based on the clinical elements [1] Table 1.
Table 1.
Elements of the clinical score
| Scoring elements | Points allocated |
|---|---|
| Extreme ages (< 21 and > 65 years old) | 1 |
| History of cervical irradiation | 1 |
| Family history of thyroid cancer | 1 |
| Presence of lymphadenopathy | 1 |
| Fixed node | 1 |
| Painless nodule | 1 |
| Male sex | 1 |
| Signs of local compression | 1 |
| Cervical swelling | 1 |
| Absence of information listed on the interrogation | 1 |
Ultrasound scanners used to have: linear transducer of high frequency (10–13 MHz) with broad band, convex and sectoral (endocavitary) reproducing high quality images; Doppler mode (color and pulsed) and/or elastography module.
The patient was installed in supinate position. We give below the protocol for ultrasound exploration of the thyroid in two points. The clinical information included the indications and the old report.
The technique consisted of performing basic transverse and longitudinal ultrasound sections to assess the following parameters: study of the thyroid (3D biometry, echogenicity, echostructure, vascularization and calcification); nodular characterizations (size, contours, shape; echostructure, echogenicity, calcification). The size, volume, the 5 ultrasound characteristics of the nodules (composition, echogenicity, shape, margin and echogenic foci) and the EU-TIRADS score of the nodules were systematically recorded and noted in the patient's file. The EU-TIRADS are guidelines by the European Thyroid Association (ETA) [11]. These 6 elements were used to calculate the EU-TIRADS score. This score has a minimum of 0 and a maximum of 5. The study of the cervical lymph nodes, looking for any cervical lymphadenopathy (short axis and pejorative ultrasound characters). After excision, the surgical specimens were brought to the anatomopathology laboratory of the University Clinics of Kinshasa, the Ngaliema Clinic, CHIP (BIBWA) and the LEBOMA Anatomopathology Center of Kalamu. The reading of the slides was carried out by specialists in the field. The anatomopathological diagnosis collected was recorded in the anatomopathology registers of each laboratory mentioned above.
Operational definitions
T his score varies on a scale of 1 to 5. Only data from patients with an EU-TIRADS score greater than or equal to 2 were used for the statistical analyses, based on the assumption that patients with EU-TIRADS score of 1 corresponded to a normal ultrasound examination [12]. An EU-TIRADS score of 2 and 3 suggested nodules at low risk of malignancy and that of 4 and 5 corresponded to intermediate and high-risk nodules.
After summing all the elements composing the score, we obtained a minimum score of 0 and a maximum score of 11. Patients with a clinical score between 0 and 2 had a low risk and those with a score between 3–11 had a high risk.
Sensitivity (Se) is determined on a population of patients whose "sick" status is known thanks to the reference test. It is the probability (p) of the positive result of the test (T +) in subjects carrying the disease (M +) as defined by the gold standard also called true positive rate. Se = p(T + /M +).
Specificity (Sp) is determined on a population of patients whose non-diseased status is known. It is the probability of a negative test result (T-) in patients defined as non-diseased (M-) also called the true negative rate. Sp = p(T-/M-).
Positive predictive value (PPV) is the probability that the condition is present when the test is positive.
Negative predictive value (NPV) is the probability that the condition is not present when the test is negative.
Youden Index: the Youden Index is a measure of the overall accuracy of a diagnostic test, combining sensitivity and specificity. What does a high Youden Index indicate? A high Youden Index indicates that the test has high sensitivity and specificity, making it an effective diagnostic tool. Youden index = (Se + Sp)-100.
Statistical analysis
The encoded and validated data were entered on the computer using Excel version 13 software. The cleaning of the file made it possible to harmonize the data and then export them to SPSS Windows version 24 software. The qualitative data were represented as form of frequencies (%). Quantitatives data as means ± standard deviations. Sensitivity, specificity, PPV and NPV predictive value of the EU-TIRADS score, clinical score and thyroid pathology diagnosis were calculated. The concordance between the different risk categories was estimated using the area under the curve and reinforced by the Youden index. The variables studied were clinical, sonographic and histopathological malignancy risk categories and concordance between clinical, sonographic and pathologic malignancy risk categories. A good concordance was classified if the Youden index is greater than 0.70 and the AUC ≥ 0.70.
Ethical considerations
The research protocol had obtained the favorable opinion of the Ethics Committee of the School of Public Health of the University of Kinshasa at No. ESP / CE / 078 / 2023. The data was collected and analyzed anonymously with rigor respecting the standards of confidentiality to be used only for the drafting of the work. The study was carried out in accordance with the Declaration of Helsinki.
Results
In view of this table, we note that the nodules were found less in men in 3.3%, i.e. a sex ratio of 1H/29F. The average age was 47.38 ± 8.8 years, the age group of less than 21 years and more than 65 years represented 4.9%. After stratification of the nodules according to the EU-TIRADS score, we note the majority of the patients were classified at stage 3 and 4 respectively with a frequency of 47.5% and 34.4%. The most frequent histopathological diagnosis was colloidal multi-hetero-nodular goiter in 80.3%, followed by thyroid papillary carcinomas and adenomatoid nodules with an identical frequency of 6.6%. The average clinical score of the patients was 3.4 ± 0.84 with the extremes ranging from 1 to 5. The majority of the patients were classified as having an intermediate risk, i.e. 85.2% of the cases. The high risk was found in 6.6% of patients. By grouping the different binary scores on the basis of the criteria found in the literature, we note 41% of the nodules had a high risk according to the EU-TIRADS score and 8.2% of the nodules were malignant (Table 2).
Table 2.
General characteristics of the study population
| Variables | All patients (61) | |
|---|---|---|
| n | % | |
| Average age (year) | 47.38 ± 8.8 | |
| Extreme ages < 21 and > 65 years old | 3 | 4.9 |
| Male sex | 2 | 3.3 |
| Presence of lymphadenopathy | 8 | 13.1 |
| Fixed node | 22 | 36.1 |
| Painless nodule | 56 | 91.8 |
| Signs of local compression | 57 | 93.4 |
| exophthalmos | 2 | 3.3 |
| Cervical swelling | 61 | 100.0 |
| Average clinical score | 3.4 ± 0.84 | |
| EU-TIRADS score | ||
| 2 | 7 | 11.5 |
| 3 | 29 | 47.5 |
| 4 | 21 | 34.4 |
| 5 | 4 | 6.6 |
| Histopathological diagnostics | ||
| Colloidal GMHTN | 49 | 80.3 |
| Adenomatoid nodule | 4 | 6.6 |
| Chronic thyroiditis | 3 | 4.9 |
| Papillary carcinoma | 4 | 6.6 |
| Gallbladder carcinoma | 1 | 1.6 |
| Clinical Score | ||
| Low risk | 32 | 52.5 |
| High risk | 29 | 47.5 |
| EU-TIRADS | ||
| Low risk | 36 | 59.0 |
| High risk | 25 | 41.0 |
| Histopathology | ||
| Benign nodule | 56 | 91.8 |
| Malignant nodule | 5 | 8.2 |
These probabilities were reinforced by the reproduction of the ROC curves. These reported to the diagnosis of malignancy show an area under the curve of 0.709 with 95% CI (0.486–0.931), a Youden index of 0.769 for the clinical score, and an area under the curve of 0.830 with 95% CI (0.605–0.995), a Youden index of 0.772 for the EU-TIRADS score (Table 3 and Fig. 1).
Table 3.
Diagnostic agreement of clinical score, EU-TIRADS versus histopathology
| Variables | Clinical score | EU-TIRADS | ||
|---|---|---|---|---|
| Value | 95% CI | Value | 95% CI | |
| Se (%) | 80.0 | 60.3–99.7 | 80.0 | 60.3–99.7 |
| Sp (%) | 96.9 | 88.4–100.0 | 97.2 | 89.1–100.0 |
| PPV (%) | 75.4 | 71.0–89.8 | 82.5 | 78.7–96.3 |
| NPV (%) | 74.6 | 70.2–89.0 | 87.5 | 73.7–91.3 |
| Youden Indix | 0.769 | 0.562–0.976 | 0.772 | 0.566–0.978 |
| AUC | 0.709 | 0.486–0.931 | 0.830 | 0.605–0.995 |
Abbreviations: Se Sensitivity, Sp Specificity, PPV Positive predictive value and NPV Negative predictive value
Fig. 1.
ROC curve A = EU-TIRADS B = Clinical score in the diagnosis of malignant nodule
Discussion
Of 61 thyroidectomized patients included in this series, 59 subjects were female against 2 subjects male. The sex ratio was 1H/29F. However, of the 2 male subjects, neither of them had presented with thyroid cancer. The male sex is a classic element of presumption of malignancy [13]. The finding of a thyroid tumor in a man should raise fears of cancer [12, 14, 15]. It has not been proven in our series. The female predominance in terms of thyroid nodules is very classic, unanimity has emerged for all the authors as to this [16]. The high parity in Africa is favorable for the outbreak of thyroid nodules, nodular changes in goiters, the presence of estrogen receptors on vesicular cells and corollary mechanisms of immunity.
The median age in our study is around 47.38 years with extremes ranging from 21 and 71 years. The groups most affected are those aged 40–49 and 50–59 with a cumulative frequency of 66%. Our results corroborate those found by Lew JI et al. [17]; that the age group of 45–60 years was the most affected by thyroid nodules [18]. The table below clearly illustrates this concordance of frequencies between the different authors.
In our series, we compared six parameters to assess the performance of the EU-TIRADS score against the histological diagnosis taken as the gold standard with the results of BUKASSA J [19]. We had found points of convergence as well as divergences concerning the said indicators: first, points of divergence; a Se (80% against 96.6%), a Sp (97.2% against 59.3%), a PPV (82.5% against 98.5%) and a NPV (87.5 against 98, 5%). The difference could be due to several factors including the large sample size at BUKASSA J et; 8 times higher than ours, ie 519 cases against 61 cases, with a counter-expertise of the sample slides in the study by Bukassa J. after refixation and re-staining; second of the points of the convergences like; the Youden index greater than 0.5 indicating the performance of the EU-TIRADS score (0.772 against 0.559). This performance is also reinforced by a better area under the curve, ie 0.830 against 0.862. We used six parameters to assess the performance of the EU-TIRADS score against the clinical score taken as a reference. The results show a performance of the EU-TIRADS score on the clinical score (apart from their sensitivities remaining identical at 80%); a superiority of five out of six indicators: its specificity (97.2% against 96.9%), its PPV (82.5% against 75.4%), its low NPV (87.5 against 74.6%) Youden index slightly higher (0.772 against 0.769) and finally the area under the curve reinforcing this performance (0.803 against 0.709). Apart from performance tests, we could evaluate these two scores compared to the level of malignancy risk estimate. It is noted that in this series the risk of malignancy for the EU-TIRADS score (41%) is practically comparable to the risk of malignancy obtained with the clinical score (47.5%). This shows that both scores on the epidemiological level can be used for the diagnosis of malignant thyroid nodule. Moreover, Gharib H [16] assessed this risk of clinical malignancy at least 68.5% for the single slice of the intermediate risk category. This could be explained by the fact that the elements of their samples include patients with cervical swellings and palpable nodules, the majority of which fall into the intermediate risk category.
Some clinical information was missing from medical records during data collection. Thyroid ultrasounds were performed by several doctors specializing in medical imaging, with different brands of ultrasound scanners as well as a multitude of semantics. No uniform protocol was previously submitted to the patients for carrying out the examination and was not imposed. This could be the limit of our study. The strength of this study is that it is the first in the DRC to compare the concordance of the clinical, ultrasound and histopathology score in the diagnosis of thyroid nodule.
Conclusion
This study shows that the EU-TIRADS score and the clinical score showed higher concordance in diagnosing thyroid nodules. Of this effect, these scores allow in a low-income country, with a well-performed thyroid ultrasound using the EU-TIRADS score and a well-informed anamnesis would be an important tool in the selection of thyroid nodules suspected of malignancy and requiring histopathological examination.
Acknowledgements
We would like to thank all those who accompanied us in the data collection as well as in the writing of this article; especially the doctors of four hospitals in Kinshasa as well as the technicians of the anatomopathological laboratories, who willingly approved and supervised the collection of data for this study.
Abbreviations
- EU-TIRADS
European association thyroid imaging data and reporting systems
- TN
Thyroid nodule
- DRC
Democratic Republic of Congo
- IRM
Magnetic resonance imaging
- CUK
University clinics of Kinshasa
- CMCP
Center Médico-Chirurgical de Pigeon
- PPV
Positive predictive value
- NPV
Negative predictive value
- CI
Confidence interval
- AUC
Area under the curve
Authors’ contributions
JMK and ANN conceptualized the research topic, JTM, AAM and MTL drafted the protocol with input from JMK and ANN for the methods, prepared the submission for institutional review board approval, supervised the data collection and drafted the manuscript. JNK provided guidance for the statistical analysis. CBM, ATM, SFB, JBL, OMK, RS, FKB, CRA, BFN, MKM, ONM, AWO, EMT, SVT, HYK and RVM provided content oversight for the manuscript. All authors read and approved the final manuscript.
Funding
This research received no external funding.
Availability of data and materials
The datasets analyzed during this study are available from corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with relevant guidelines and regulations. The study was reviewed and approved by the Ethics Committee of the School of Public Health of the University of Kinshasa at No. ESP / CE / 078 / 2023. Written informed consent was obtained from all the participants and/or their legally acceptable representatives. Non-literate participants were accompanied by a literate peer of their choice. Participants under 18 years of age were accompanied by their parent or guardian. Their informed assents and consent from parent or guardian were requested and signed before the enrolment to the study. Participants had the right to provide consent or not and to withdraw from the study at any time during the interview, without having to provide a reason. Risks to participants in this study were expected to be minimal, as the invasiveness of the ultrasound and pathology examination was minimal.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mbede M, Vagoda Sinbai C, Mossus Y, Godkoye M, Etoa M, Wafeu Sadeu G, et al. Clinical, ultrasound and histological concordance of thyroid nodules Yaounde. Health Sci Dis. 2021;22(12):77–80. [Google Scholar]
- 2.Bukasa JK, Bayauli PM, Mbunga BK, Bangolo A, Kavula W, Mukaya J, et al. The spectrum of thyroid nodules at kinshasa university hospital, democratic Republic of Congo: a cross-sectional study. Int J Environ Res Public Health. 2022;19:16203. 10.3390/ijerph192316203. 10.3390/ijerph192316203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joseph-Auguste J, Lin L, Demar M, Duffas O, Molinie V, Sulpicy C, et al. Epidemiologic, clinical, ultrasonographic, and cytological features of thyroid nodules in predicting malignancy risk: a retrospective study of 442 french afro-caribbean patients. Int J Endocrinol. 2020;2020:1–8. 10.1155/2020/4039290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moifo B, Takoeta EO, Tambe J, Blanc F, Fotsin JG. Reliability of Thyroid Imaging Reporting and Data System (TIRADS) classification in differentiating benign from malignant thyroid nodules. OJRad. 2013;03(03):103–7. 10.4236/ojrad.2013.33016 [DOI] [Google Scholar]
- 5.Skowrońska A, Milczarek-Banach J, Wiechno W, Chudziński W, Żach M, Mazurkiewicz M, et al. Accuracy of the European Thyroid Imaging Reporting and Data System (EU-TIRADS) in the valuation of thyroid nodule malignancy in reference to the post-surgery histological results. Pol J Radiol. 2018;83:e579-86. 10.5114/pjr.2018.81556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bukasa JK, Sabbah N, Bayauli P, Massicard M, Bidingija J, Nkodila AN, et al. Thyroid cancer in the Democratic Republic of the Congo: Frequency and risk factors. Annales d’Endocrinologie. 2021;82(6):606–12. 10.1016/j.ando.2021.09.002 [DOI] [PubMed] [Google Scholar]
- 7.Bukasa JK, Bangolo AI, Sabbah N, Waykole T, Nkodila A, Mbunga B, et al. Hyperthyroidism and Thyroid Cancer in the Congolese Hospital Setting. J Community Med Health Care. 2022;7(1):1054. [Google Scholar]
- 8.Hartl DM, Didault S, Girard E, Guerlain J, Breuskin I, Lamartina L, et al. Ultrasound visualization of the vagus nerve for intraoperative neuromonitoring in thyroid surgery. Eur Radiol. 2021;31(6):4063–70. 10.1007/s00330-020-07472-7. 10.1007/s00330-020-07472-7 [DOI] [PubMed] [Google Scholar]
- 9.Bouaity B, Darroussin Y, Chihani M, Mliha M. Analyse des facteurs prédictifs de malignité des goitres nodulaires : à propos de 500 cas. Pan Afr Med J. 2016;23(88):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kangelaris GT, Kim TB, Orloff LA. Rôle de l’échographie dans les troubles thyroïdiens. Otolaryngol Clin North Am. 2010;43(6):1209–27. 10.1016/j.otc.2010.08.006 [DOI] [PubMed] [Google Scholar]
- 11.Darouassi Y, Chihani M, Touati MM, Ammar H. Analysis of predictors of malignancy of nodular goiters: about 500 cases Brahim Bouaity, Service d’Oto-rhino-laryngologie, Hôpital Militaire Avicenne, Marrakech. Maroc Pan Afr Med J. 2016;23:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Russ G, Bonnema SJ, Erdogan MF, Durante CD, Leenhardt LA. European thyroid association guidelines for ultrasound malignancy risk stratification of thyroid nodules in adults the EU-TIRADS. Eur Thyroid J. 2017;6(5):225–323. 10.1159/000478927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Russ G, Royer B, Bigorgne C, Rouxel A, Bienvenu-Perrard M, Leenhardt L. Prospective evaluation of thyroid imaging reporting and data system on 4,550 nodules with and without elastography. Eur J Endocrinol. 2013;168:649–55. [DOI] [PubMed]
- 14.Moon HJ, Kwak JY, Kim MJ, Son EJ, Kim E-K. Can vascularity at power doppler us help predict thyroid malignancy? Radiology. 2010;255(1):260–9. 10.1148/radiol.09091284 [DOI] [PubMed] [Google Scholar]
- 15.Leenhardt L. Ménégaux F, Franc B, Hoang C, Salem S, Bernier MO et al. Cancers de la thyroïde. Endocrinologie-Nutrition, 2016 — [10–008-A-50] - 10.1016/S1155-1941(16)64254-3.
- 16.Gharib H, Papini E, Valcavi R, Baskin HJ, Crescenzi A, Dottorini ME, et al. American Association of Clinical Endocrinologists et Associazione Medici Endocrinologi directives médicales pour la pratique clinique pour le diagnostic et la gestion des nodules thyroïdiens. Endocr Pract. 2006;12:63–102. 10.4158/EP.12.1.63 [DOI] [PubMed] [Google Scholar]
- 17.Lew JI, Snyder RA, Sanchez YM, Solorzano CC. Fine needle aspiration of the thyroid: correlation with final histopathology in a surgical series of 797 patients. J Am Coll Surg. 2011;213(1):188–94. 10.1016/j.jamcollsurg.2011.04.029 [DOI] [PubMed] [Google Scholar]
- 18.Taali L, Baghdadi T, Fassih M, Abada A, Rouadi S, Roubal M et al. Lymphome de la thyroide : à propos d’un cas et revue de littérature. Rev. Méd. Gd, Lacs.2016;5(1):104–111.
- 19.Bukasa JK, Bayauli1 P, Sabbah N, Bidingija J, Atoot A, Mbunga B et al. Ultrasound performance using the EU-TIRADS scores in the diagnosis of thyroid cancer in Congolese hospitals. Sci Rep. 2022;12:18442. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during this study are available from corresponding author on reasonable request.