Abstract
Background
The control of schistosomiasis is particularly difficult in sub-Saharan Africa, which currently harbours 95% of this disease. The target population for preventive chemotherapy (PC) is expanded to all age group at risk of infection, thus increasing the demands of praziquantel (PZQ) tablets according to the new released guideline by World Health Organization. Due to the gap between available PZQ for PC and requirements, alternative approaches to assess endemicity of schistosomiasis in a community, are urgently needed for more quick and precise methods. We aimed to find out to which degree the infection status of snails can be used to guide chemotherapy against schistosomiasis.
Methods
We searched literature published from January 1991 to December 2022, that reported on the prevalence rates of Schistosoma mansoni, S. haematobium in the intermediate snails Biomphalaria spp. and Bulinus spp., respectively, and in humans. A random effect model for meta-analyses was used to calculate the pooled prevalence estimate (PPE), with heterogeneity assessed using I-squared statistic (I2), with correlation and regression analysis for the exploration of the relationship between human S. mansoni and S. haematobium infections and that in their specific intermediate hosts.
Results
Forty-seven publications comprising 59 field investigations were included. The pooled PPE of schistosomiasis, schistosomiasis mansoni and schistosomiasis haematobium in humans were 27.5% [95% confidence interval (CI): 24.0–31.1%], 25.6% (95% CI: 19.9–31.3%), and 28.8% (95% CI: 23.4–34.3%), respectively. The snails showed an overall infection rate of 8.6% (95% CI: 7.7–9.4%), with 12.1% (95% CI: 9.9–14.2%) in the Biomphalaria spp. snails and 6.9% (95% CI: 5.7–8.1%) in the Bulinus spp. snails. The correlation coefficient was 0.3 (95% CI: 0.01–0.5%, P < 0.05) indicating that the two variables, i.e. all intermediate host snails on the one hand and the human host on the other, were positively correlated.
Conclusions
The prevalence rate of S. mansoni and S. haematobium is still high in endemic areas. Given the significant, positive correlation between the prevalence of schistosomes in humans and the intermediate snail hosts, more attention should be paid to programme integration of snail surveillance in future.
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s40249-024-01233-0.
Keywords: Schistosoma mansoni, Schistosoma haematobium, Bulinus, Biomphalaria, Prevalence, Correlation analysis, Meta-analysis, Africa
Background
Schistosomiasis (bilharziasis), a parasitic disease caused by different species of trematode worms, is prevalent in 78 countries across Asia, Latin America, the Middle East and Africa [1]. Among the six schistosome species infective for humans, Schistosoma japonicum, S. mansoni and S. haematobium are the major species, with extensive distributions and considerable disease burdens [2]. The previous two cause intestinal schistosomiasis, whereas S. haematobium is responsible for the urogenital form of the disease. Over 250 million people worldwide are infected, with more than 95% occurring in sub-Saharan Africa, primarily attributed to S. mansoni and S. haematobium [3–5].
The life cycle of this parasite involves an intermediate snail host and a definitive mammalian host. Infection of the latter occurs through contact with freshwater contaminated by schistosome cercariae (the infectious form of schistosomes) released from infected snails. After maturing into adult male and female worms, the parasites reproduce and release eggs that are excreted into the aquatic environment with faeces (S. mansoni, S. japonicum) or urine (S. haematobium). These eggs hatch and infect certain freshwater snails, where the parasites undergo asexually multiplication and finally develop into cercariae [4, 6]. The endemicity of schistosomiasis is related to the presence of appropriate intermediate host snails, with Biomphalaria spp. serving as intermediate hosts of S. mansoni [7, 8] and Bulinus spp. of S. haematobium [9]. These snail species are hermaphroditic, capable of self- or cross-fertilization and widely distributed in Africa, Latin America and the Middle East as well as countries bordering the Indian and the Mediterranean Seas [10].
In 2001, the World Health Assembly (WHA) proposed a global strategy (resolution 54.19) for controlling schistosomiasis through preventive chemotherapy (PC) programmes predominately to school-age children (SAC) in endemic settings, which rapidly achieved remarkably positive results [3, 11, 12]. This resolution recommends regular treatments by mass drug administration (MDA) with praziquantel (PZQ) which still remains the solely available drug for treating and controlling schistosomiasis [13]. Although PZQ has been the cornerstone for morbidity control of schistosomiasis since the mid-1980s, snail control is not routinely implemented due to higher cost and not considered as important as before PZQ became widely available [14]. However, in the last decade there has been a revival for snail control and it is recommended to also integrate other measures, such as water, sanitation and hygiene (WASH) and health education to accelerate schistosomiasis elimination in Africa [5, 15, 16]. Due to the high heterogeneity of schistosomiasis infection rates in different countries, scientific and reliable data are needed to provide support for improving resource utilization and adjusting countermeasures.
A malacological survey is an important component of epidemiological survey of schistosomiasis. The finding of infected snails and the identification of miracidia in aquatic samples are the two vital components of a malacological survey [17]. However, little attention has been given to malacological approaches as one of the controls of schistosomiasis [18]. Morbidity reduction and ultimate elimination via integrated control actions have been the targets of the existing schistosomiasis control progammes. It has been suggested that precise identification of the infections in humans and intermediate snail hosts, the definitive and intermediate hosts, respectively, is of paramount use in achieving these goals. The vast majority of researches on schistosomiasis have been given major emphasis on disease prevalence and intensity of infection among human populations. Although previous studies reported that snail infections are supposed to indicate the infection rate and magnitude of human schistosomiasis, efforts to identify and target the intermediate snail hosts in endemic areas are apparently overlooked [19]. Therefore, integrating snail distribution with human infection data is quite useful for the ongoing control program.
In 2019, approximately 61.8 million SAC and 1.1 million adults worldwide received PC [20], resulting in significant reduction of schistosomiasis-associated mortality and morbidity [11, 21]. Although the guideline for PC have been revised for the endemic settings, the criteria for frequency of MDA and assessment of effectiveness of interventions are mainly based on the prevalence in SAC and have largely remained the same for the last two decades [22, 23]. In February 2022, World Health Organization (WHO) released updated guideline for the control and elimination [24], and interruption of transmission of human schistosomiasis where feasible in selected endemic countries by 2030 [25]. In the new guideline, the target population for PC has been expanded from SAC to all age groups at risk of infection, thus increasing the demand of PZQ tablets considerably [26]. Considering the gap between available PZQ and requirements, the heterogeneity of schistosomiasis due to the different species and ongoing interventions [27], alternative approaches to assess endemicity of schistosomiasis in a community, especially in Africa, are urgently needed [28].
Previous studies have highlighted the role of the intermediate host for spread the disease [29]. But the relationship of infection rates between intermediate host and humans remains unclear. This systematic review aimed to identify the correlation of prevalence rates in snail hosts and humans for the two major forms of human schistosomiasis, schistosomiasis mansoni and schistosomiasis haematobium, by investigating what has been published on the matter as this could assist policy-making for campaigns against schistosomiasis.
Methods
Literature search strategy and selection criteria
Relevant publications from the literature published from January 1991 to December 2022 were searched in public databases (PubMed, Web of Science, Science Direct). The Scopus and Cochrane databases were also included but did not yield additional data. The following keywords and combinations were used in the search: ((Schistosoma mansoni) OR (S. mansoni) OR (Schistosoma haematobium) OR (S. haematobium)) AND ((schistosome intermediate host) OR (freshwater snails) OR (malacological survey) OR (Biomphalaria) OR (Bulinus)) AND (human) AND ((infection rate) OR (prevalence) OR (positive rate)), without language restrictions. The references of the retrieved literatures were scrutinized and screened to capture any study potentially overlooked during the electronic search process (Additional file 1). Titles and abstracts of papers retrieved were manually screened to remove irrelevant references and the full texts of potentially relevant papers were reviewed further [30]. This process was conducted independently by three reviewers (XYW, KY and JX). The systematic review and selection of relevant literature was done according to the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines [31] with PROSPERO (CRD42023471218).
Relevant studies fulfilling the inclusion and exclusion criteria were enrolled. The main inclusion criterion was that retrospective, descriptive or observational studies should focus on the intermediate and the definitive hosts of S. mansoni and S. haematobium without restrictions. Exclusion criteria included exclusively dealing with intermediate host snails or exclusively with definitive hosts, non-human schistosomes and/or other trematode species. The detailed inclusion and exclusion criteria are described in the Additional file 1.
Data were extracted by QL and YLL and reviewed by SYG. Data were extracted using a standardised form. Discrepancies were resolved by consensus. Where the same study was described in more than one publication, the publication with the highest sample size and most detailed information was used, supplemented by the other publications. A study consists of multiple surveys, with data collected separately for each survey. If a study provided data for one year or more, we used the starting year or year with the most detailed information. The following information was extracted from the selected literature: name of first author, year of study (the years of the studies included in the review were categorized into three groups, namely; the 1991–2000, 2001–2010 and 2011–2022, to assess the trends of infection rates during the periods), study area (e.g., site and country), study type (e.g., cross-sectional or longitudinal), Schistosoma species, target population, number of people assessed, number of positive cases, snail species, number of snails examined, number of infected snails, and diagnostic method(s) used. All extracted data were independently recorded with Microsoft Excel 2016 (Microsoft, Redmond, Washington, USA) by those of the authors involved at this stage.
Quality assessment
The quality of the selected studies was assessed according to the Joanna Briggs Institute (JBI) prevalence critical appraisal Tool [32]. All included studies were scored using the 10 quality control items suggested by the tool. A score of 1 was given for each fulfilled item, with 0 for each unmet item. The overall quality of each included study was classified based on the total number of scores generated, i.e., 0–3 = low, 4–6 = moderate and 7–10 = high (Additional file 1: Table S1) [33].
According to the scoring results, we selected literatures with high scores for inclusion in the study. We assessed methodological quality and risk of bias for all included studies using RevMan 5.4 (The Cochrane Centre Collaboration, Copenhagen, Denmark), and assessed evidence of publication bias by generating funnel plots [34]. We considered the presence of such a bias risk across the selected studies assessing them by funnel plot as introduced by Light and Pillemer [35]. Briefly: a symmetric funnel shape arises from an acceptable dataset makes publication bias unlikely, while an asymmetrical plot indicates the opposite. Publication bias was evaluated by visual inspection of funnel plots method.
Statistical analysis
The pooled prevalence estimate (PPE) of schistosomes in humans and snails were pooled using random effect model for meta-analysis from the eligible studies [36]. Forest plot, a tool that sums up information on studies in a figure that gives a visual indication (https://s4be.cochrane.org/blog/2016/07/11/tutorial-read-forest-plot/), was used to estimate the overall pooled effect size with 95% confidence interval (CI). The percentage of total variation due to interstudy heterogeneity was evaluated using the I2 measure by RevMan 5.4 software, the values of which at 25%, 50% and 75% are considered low, moderate and high heterogeneity, respectively. Subgroup analysis was further performed based on Schistosoma species, snail species, years of studies conducted, population and country to explore the source of heterogeneity. The data analysis was conducted using RevMan software.
The normality distribution of prevalence values of schistosome infections between intermediate host and humans was quantified by the Kolmogorov–Smirnov (K-S) test [37]. The correlation coefficient (r) was calculated to assess the strength of the linear relationship between two variables. At r ≤ 0.4, the strength of correlation was stratified as weak, at 0.4 < r < 0.8 moderate and at r ≥ 0.8 strong [38, 39]. Regression analysis was used to calculate the regression coefficient and the regression equation. The F test conducts a significant test of the regression equation. If the P value of the overall F test is significant, the regression model predicts the response variable better than the mean of the response [40]. Outliers were tested for using residuals and q-q plots when warranted. Analysis of these variable is not always straightforward and standard linear analysis could be problematic. We present the most common approach to dealing with this problem: a logit, a double arcsine and an exponential transformation of the percentages, following which standard linear association analysis can be conducted on the transformed value. The strength of the linear association is expressed by the coefficient of determination (R2), which ranges from 0 (no linear association) to 1 (perfect linear association, whether positive or negative). All analytical functions were analyzed by the statistical software SPSS 20.0 (International Business Machines Corporation, Armonk, New York, USA). P < 0.05 was considered statistically significant.
Results
Search results
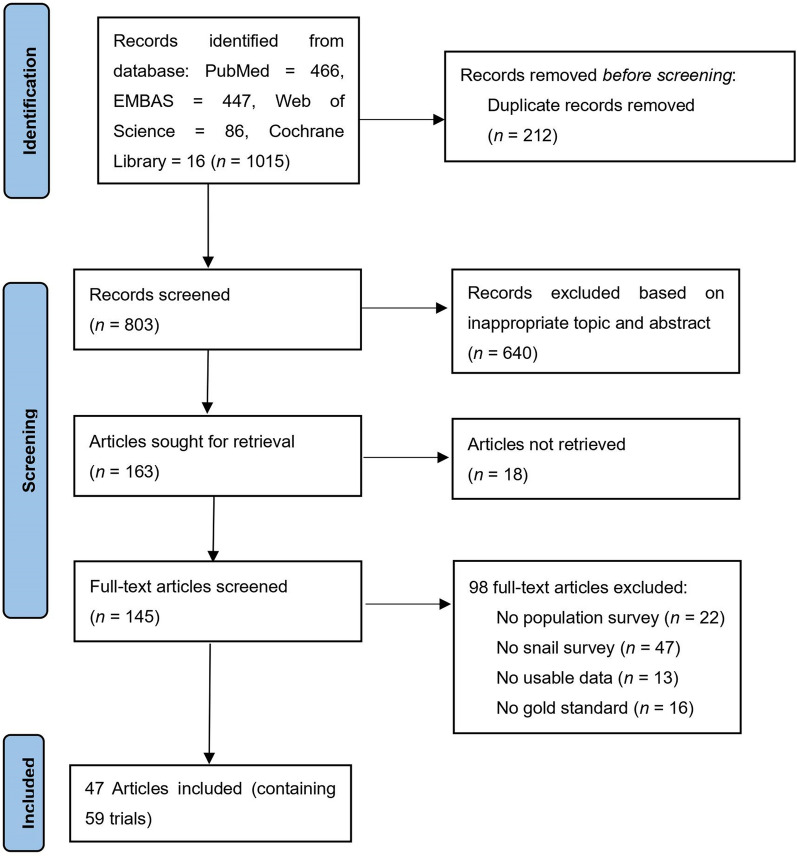
An initial number of 1015 relevant studies were identified, 212 of which were removed due to duplications and 640 based on the title and abstract screening. The remaining 145 full-text articles were assessed for eligibility, which led to the exclusion of 98 arriving at a final count of 47 articles containing 59 field investigations of schistosomiasis in human and snail hosts to be used for meta-analysis. The flow diagram of the process is shown in Fig. 1.
Fig. 1.
PRISMA flow diagram of studies identified for the study of the correlation of human and snail schistosome infections
The 47 studies [5, 41–87] included in this review had been conducted in 21 countries (Additional file 1: Fig S1), mostly in Africa, with special reference to Ethiopia (n = 7), Tanzania (n = 5) and Nigeria (n = 5), with Brazil (n = 4). Among the included 47 studies, 26 focused exclusively on the prevalence of S. haematobium in humans and Bulinus spp. snails and 13 exclusively on infection rates of S. mansoni in humans and Biomphalaria spp. snails, while the 8 studies included both species in humans and their specific snail hosts. All diagnoses had been carried out by microscopy: in humans for S. haematobium after filtration [88] and for S. mansoni by Kato-Katz faecal smears [89], while cercarial shedding technique [90] had been used for all snail studies. 35 of the included studies were cross-sectional and 12 longitudinal. According to the JBI prevalence critical appraisal method, all studies covered by this review were deemed to be of high quality with scores ranging from 8 to 9 (Tables 1, 2).
Table 1.
Schistosoma haematobium studies included in the meta-analysis
| First author (Published year) [reference no.] | Study year | Population investigated (n) | No. infected humans (prevalence, %) | Examined snail species (n) | No. infected snails (prevalence, %) | Location | Sampling approach | JBI score |
|---|---|---|---|---|---|---|---|---|
| Rudge et al. (2008) [76] | 2005 |
Students (150) |
76 (50.7) |
Bulinus globosus (120) |
6 (5.0) |
Tanzania | Cross-sectional | 8 |
| Léger et al. (2020) [a] [63] | 2016–2018 |
Others (869) |
581 (66.9) |
B. globosus, B. truncatus (2532) |
91 (3.6) |
Senegal | Longitudinal | 9 |
| Léger et al. (2020) [b] [63] | 2016–2019 |
Others (716) |
211 (29.5) |
B. umbilicatus (4694) |
6 (0.1) |
Senegal | Longitudinal | 9 |
| Tchuenté et al. (2018) [79] | 2015–2017 |
Others (1173) |
275 (23.4) |
B. camerunensis, B. truncates, B. forskalii (1064) |
5 (0.5) |
Cameroon | Longitudinal | 9 |
| Ivoke et al. (2014) [60] | 2012–2013 |
Students (894) |
137 (15.3) |
B. globosus (308) |
62 (20.1) |
Nigeria | Longitudinal | 9 |
| Vera et al. (1992) [81] | 1988 |
Students (92) |
77 (83.7) |
B. senegalensis (600) |
3 (0.5) |
Niger | Cross-sectional | 8 |
| Medhat et al. (1993) [65] | 1993 |
Others (920) |
75 (8.2) |
B. truncates (1039) |
1 (0.1) |
Egypt | Cross-sectional | 9 |
| Verle et al. (1994) [82] | 1994 |
Community (352) |
306 (86.9) |
B. globosus, B. truncatus, B. forskalii, B. senegalensis (601) |
106 (17.6) |
Senegal | Cross-sectional | 9 |
| Traquinho et al. (1998) [80] | 1995 |
Students (994) |
839 (84.4) |
Bulinus spp. (407) |
345 (84.8) |
Mozambique | Cross-sectional | 9 |
| Pennance et al. (2016) [74] | 2014 |
Students (744) |
125 (16.8) |
B. globosus (1111) |
26 (2.3) |
Tanzania | Cross-sectional | 9 |
| Angelo et al. (2018) [40] | 2015–2017 |
Students (250) |
42 (16.8) |
B. nasutus (4899) |
132 (2.7) |
Tanzania | Longitudinal | 9 |
| Dabo et al. (2015) [50] | 2011–2012 |
Students (1761) |
259 (14.7) |
B. globosus, B. truncatus, B. forskalii (438) |
11 (2.5) |
Mali | Longitudinal | 9 |
| Anyan et al. (2019) [42] | 2012–2013 |
Students (383) |
149 (38.9) |
B. truncates (896) |
7 (0.8) |
Ghana | Cross-sectional | 9 |
| Ofoezie et al. (1997) [a] [72] | 1991–1992 |
Students (128) |
51 (39.8) |
B. globosus (1472) |
55 (3.7) |
Nigeria | Longitudinal | 8 |
| Ofoezie et al. (1997) [b] [72] | 1992–1993 |
Students (99) |
33 (33.3) |
B. globosus (1343) |
37 (2.8) |
Nigeria | Longitudinal | 8 |
| Chimbari et al. (2003) [49] | 2001–2002 |
Others (570) |
45 (7.9) |
B. globosus (120) |
4 (3.3) |
Zimbabwe | Longitudinal | 9 |
| De Clercq et al. (2000) [52] | 1997–1999 |
Community (233) |
84 (36.1) |
B. senegalensis, B. truncates, B. forskalii (257) |
15 (5.8) |
Senegal | Longitudinal | 9 |
| Emejulu et al. (1994) [53] | 1990–1992 |
Community (1773) |
736 (41.5) |
B. globosus, B. truncates (2323) |
117 (5.0) |
Nigeria | Longitudinal | 9 |
| Dahesh et al. (2016) [51] | 2016 |
Students (1285) |
52 (4.1) |
B. truncates (74) |
8 (10.8) |
Egypt | Cross-sectional | 9 |
| Kaiglová et al. (2020) [61] | 2018 |
Community (451) |
69 (15.3) |
B. globosus (68) |
6 (8.8) |
Kenya | Cross-sectional | 8 |
| Okeke et al. (2013) [73] | 2012 |
Students (323) |
15 (4.6) |
B. senegalensis, B. globosus (857) |
5 (0.6) |
Nigeria | Cross-sectional | 9 |
| Chaula et al. (2014) [48] | 2013 |
Students (488) |
73 (15.0) |
Bulinis spp. (46) |
6 (13.0) |
Tanzania | Cross-sectional | 9 |
| Anosike et al. (2006) [41] | 2001–2002 |
Others (2104) |
466 (22.2) |
B. globosus, B. truncatus, B. senegalensis (210) |
45 (21.4) |
Nigeria | Cross-sectional | 9 |
| Mutuku et al. (2011) [70] | 2009–2010 |
Community (777) |
336 (43.2) |
B. truncates (156) |
6 (3.9) |
Kenya | Cross-sectional | 9 |
| Zongo et al. (2012) [83] | 2009–2010 |
Students (648) |
138 (21.3) |
B. senegalensis, B. globosus, B. truncates (291) |
13 (4.5) |
Burkina Faso | Cross-sectional | 9 |
| Krauth et al. (2017) [62] | 2014–2015 |
Community (743) |
16 (2.2) |
B. globosus, B. truncates, B. forskalii (76) |
0 (0.0) |
Côte d’Ivoire | Cross-sectional | 8 |
| Tchuem-Tchuenté et al. (2001) [78] | 1999 |
Community (241) |
1 (0.4) |
B. forskalii (300) |
0 (0.0) |
Cameroon | Cross-sectional | 8 |
| Ibikounlé et al. (2014) [59] | 2010–2012 |
Students (1585) |
466 (29.4) |
B. globosus, B. forskalii (165) |
0 (0.0) |
Benin | Cross-sectional | 9 |
| Poole et al. (2014) [75] | 2012 |
Students (373) |
63 (16.9) |
B. globosus (250) |
0 (0.0) |
Malawi | Cross-sectional | 9 |
| Gbalégba et al. (2017) [54] | 2014–2015 |
Students (2162) |
86 (4.0) |
B. senegalensis, B. truncates, B. forskalii (284) |
0 (0.0) |
Mauritania | Cross-sectional | 9 |
| Assaré et al. (2020) [44] | 2016 |
Students (274) |
7 (2.6) |
B. globosus, B. truncates, B. forskalii (42) |
0 (0.0) |
Côte d’Ivoire | Cross-sectional | 8 |
| Campbell et al. (2017) [47] | 2016 |
Others (338) |
96 (28.4) |
B· camerunensis, B· truncates, B· forskalii (451) |
2 (0.4) |
Cameroon | Cross-sectional | 9 |
| Ndyomugyenyi et al. (2001) [71] | 1991–1992 |
Students (483) |
230 (47.6) |
B. globosus, B. nastus, B. africanus (148) |
0 (0.0) |
Tanzania | Cross-sectional | 9 |
| Arbaji et al. (1998) [43] | 1996 |
Others (5637) |
49 (0.9) |
B. truncates (195) |
0 (0.0) |
Jordan | Cross-sectional | 9 |
| Moser et al. (2022) [69] | 2019 |
Community (258) |
101 (39.2) |
B. truncates (38) |
0 (0.0) |
Chad | Cross-sectional | 9 |
| Mushi et al. (2022) [84] | 2021 |
Students (649) |
342 (52.7) |
B. globosus, B. nastus (947) |
18 (1.8) |
Tanzania | Cross-sectional | 9 |
JBI = Joanna Briggs Institute; [a] and [b] represent studies carried out in different regions of area country but published in one article
Table 2.
Schistosoma mansoni studies included in the meta-analysis
| First author (Published year) [reference no.] | Study year | Population investigated (n) | No. infected humans (prevalence, %) | Examined snail Species (n) | No. infected snails (prevalence, %) | Location | Sampling approach | JBI score |
|---|---|---|---|---|---|---|---|---|
| Ibikounle et al. (2009) [58] | 2003–2006 |
Others (35) |
26 (74.3) |
Biomphalaria pfeifferi (357) |
200 (56.0) |
Benin | Longitudinal | 8 |
| Léger et al. (2020) [c] [63] | 2016–2018 |
Others (671) |
80 (11.9) |
Bi. pfeifferi (407) |
9 (2.2) |
Senegal | Longitudinal | 9 |
| Traquinho et al. (1998)[c] [80] | 1995 |
Students (994) |
5 (0.5) |
Biomphalaria spp. (31) |
19 (61.3) |
Mozambique | Cross-sectional | 9 |
| Dabo et al. (2015)[c] [50] | 2011–2012 |
Students (1491) |
22 (1.5) |
Bi. pfeifferi (189) |
2 (1.1) |
Mali | Longitudinal | 9 |
| Anyan et al. (2019)[c] [42] | 2012–2013 |
Students (383) |
222 (58.0) |
Bi. pfeifferi (780) |
14 (1.8) |
Ghana | Cross-sectional | 9 |
| Chimbari et al. (2003)[c] [49] | 2001–2002 |
Others (464) |
32 (6.9) |
Bi. pfeifferi (42) |
2 (4.8) |
Zimbabwe | Longitudinal | 9 |
| Alebie et al. (2014) [38] | 2013 |
Students (384) |
293 (76.3) |
Bi. pfeifferi (375) |
32 (8.5) |
Ethiopia | Cross-sectional | 9 |
| Amsalu et al. (2015) [39] | 2010 |
Students (384) |
172 (44.8) |
Bio. pfeifferi (31) |
1 (3.2) |
Ethiopia | Cross-sectional | 9 |
| Mengistu et al. (2011) [68] | 2007 |
Community (517) |
136 (26.3) |
Biomphalaria spp. (560) |
325 (58.0) |
Ethiopia | Cross-sectional | 9 |
| Calasans et al. (2018) [46] | 2013–2014 |
Community (232) |
7 (3.0) |
Bi. glabrata (10,270) |
912 (8.9) |
Brazil | Longitudinal | 9 |
| Mekonnen et al. (2012) [66] | 2011 |
Students (403) |
106 (26.3) |
Bi. pfeifferi (80) |
2 (2.5) |
Ethiopia | Cross-sectional | 9 |
| Zongo et al. (2012)[c] [83] | 2009–2010 |
Students (203) |
36 (17.7) |
Bi. pfeifferi (64) |
4 (6.3) |
Burkina Faso | Cross-sectional | 9 |
| Guerra et al. (1991) [57] | 1988 |
Community (162) |
91 (56.2) |
Bi. glabrata (356) |
30 (8.4) |
Brazil | Cross-sectional | 8 |
| Gryseels et al. (1991) [56] | 1982 |
Community (23,955) |
6,017 (25.1) |
Bi. pfeifferi (29,199) |
249 (0.9) |
Burundi | Longitudinal | 9 |
| Massara et al. (2004) [64] | 2001–2003 |
Students (1186) |
101 (8.5) |
Bi. glabrata (2733) |
17 (0.6) |
Brazil | Cross-sectional | 9 |
| Krauth et al. (2017)[c] [62] | 2014–2015 |
Community (743) |
7 (1.0) |
Bi. pfeifferi (43) |
0 (0.0) |
Côte d’Ivoire | Cross-sectional | 9 |
| Assaré et al. (2020)[c] [44] | 2016 |
Students (274) |
26 (9.5) |
Bi. pfeifferi (92) |
0 (0.0) |
Côte d’Ivoire | Cross-sectional | 9 |
| Bekana et al. (2022) [45] | 2018–2019 |
Students (492) |
363 (73.8) |
Bi. pfeifferi (1463) |
357 (24.4) |
Ethiopia | Cross-sectional | 9 |
| Gomes et al. (2022) [d] [55] | 2000 |
Community (2012) |
653 (32.5) |
Bi. glabrata (2214) |
357 (16.1) |
Brazil | Cross-sectional | 9 |
| Gomes et al. (2022) [e] [55] | 2010 |
Community (2459) |
409 (16.6) |
Bi. glabrata (4707) |
272 (5.8) |
Brazil | Cross-sectional | 9 |
| Gomes et al. (2022) [f] [55] | 2020 |
Community (2028) |
179 (8.8) |
Bi. glabrata (1607) |
115 (7.2) |
Brazil | Cross-sectional | 9 |
| Tamir et al. (2022) [77] | 2021 |
Students (421) |
20 (4.8) |
Bi. pfeifferi (27) |
2 (7.4) |
Ethiopia | Cross-sectional | 9 |
| Meleko et al. (2022) [67] | 2021 |
Community (206) |
41 (19.9) |
Bi. pfeifferi, Bi. sudanica (505) |
66 (13.1) |
Ethiopia | Cross-sectional | 9 |
JBI = Joanna Briggs Institute. [c] represents S. mansoni results published in articles that also show S. haematobium results; [d], [e] and [f] represent studies carried out in different regions of a country but published in one article
Subgroup pooled prevalence estimates of human schistosomiasis
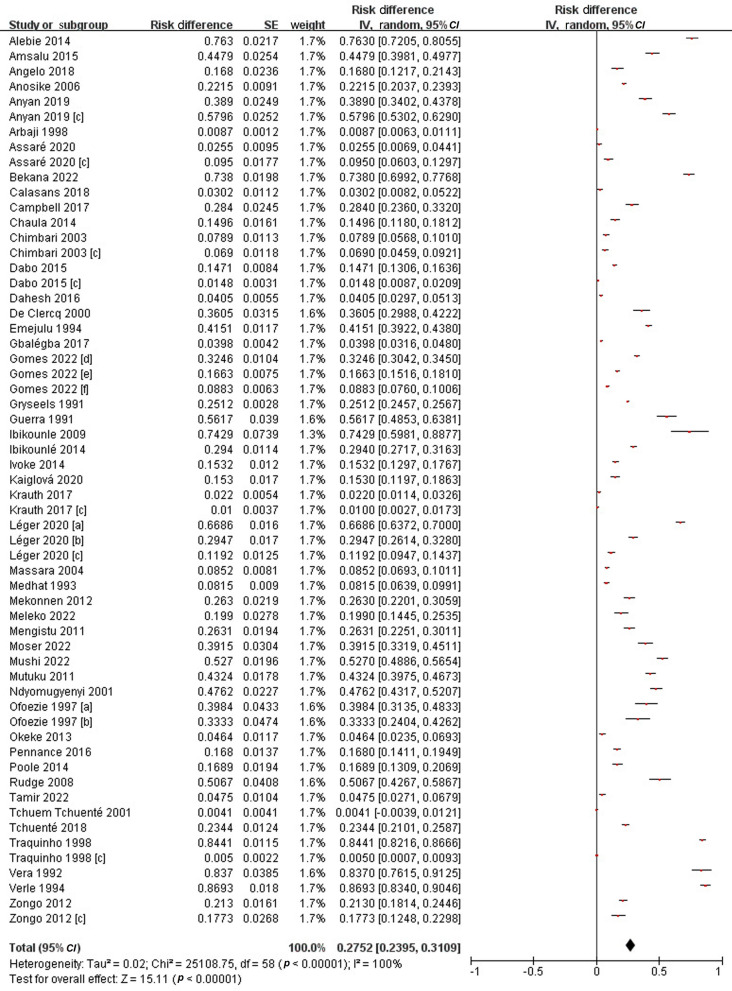
In the 47 included articles, a total of 71,019 people were examined and 15,751 of them were found to be infected, either by S. mansoni or by S. haematobium. The PPE was 27.5% (95% CI: 24.0–31.1%), with the prevalence varying from 0.4% to 86.9%, thus showing a high degree of heterogeneity (I2 = 100%, P < 0.01) (Fig. 2).
Fig. 2.
Forest plot diagram showed the prevalence of infecting human schistosomes. * Each red dot represents risk difference of individual studies, and the horizontal line represents the 95% CI. The diamond indicates the pooled effect. a and b represent studies carried out in different regions of a country but published in one article. c represents S. mansoni results published in articles that also show S. haematobium results
Subgroup analyses were performed based on publication year, areas surveyed, Schistosoma species and various populations. Accordingly, the PPE of schistosomiasis in humans was 38.2% (95% CI: 30.0–46.4%) from 1991 to 2000; 26.9% (95% CI: 20.5–33.4%) from 2001 to 2010; and 22.7% (95% CI: 18.1–27.3%) from 2011 to 2022. Geographically, the highest PPE was obtained from Africa 29.0% (95% CI: 24.5–33.4%); followed by Latin America 20.3% (95% CI: 11.7–28.8%); and only Jordan from West Asia 0.9% (95% CI: 0.6–1.1%). Specifically, the PPE of schistosomiasis haematobium in humans was 28.8% (95% CI: 23.4–34.3%), while that of schistosomiasis mansoni was 25.6% (95% CI: 19.9–31.3%). Among populations, the PPE was 29.3% (95% CI: 23.4–35.1%) obtained from students, 26.5% (95% CI: 19.0–34.1%) for community populations, and 24.7% (95% CI: 14.9–34.5%) for all others (Additional file 1: Fig. S2–S5).
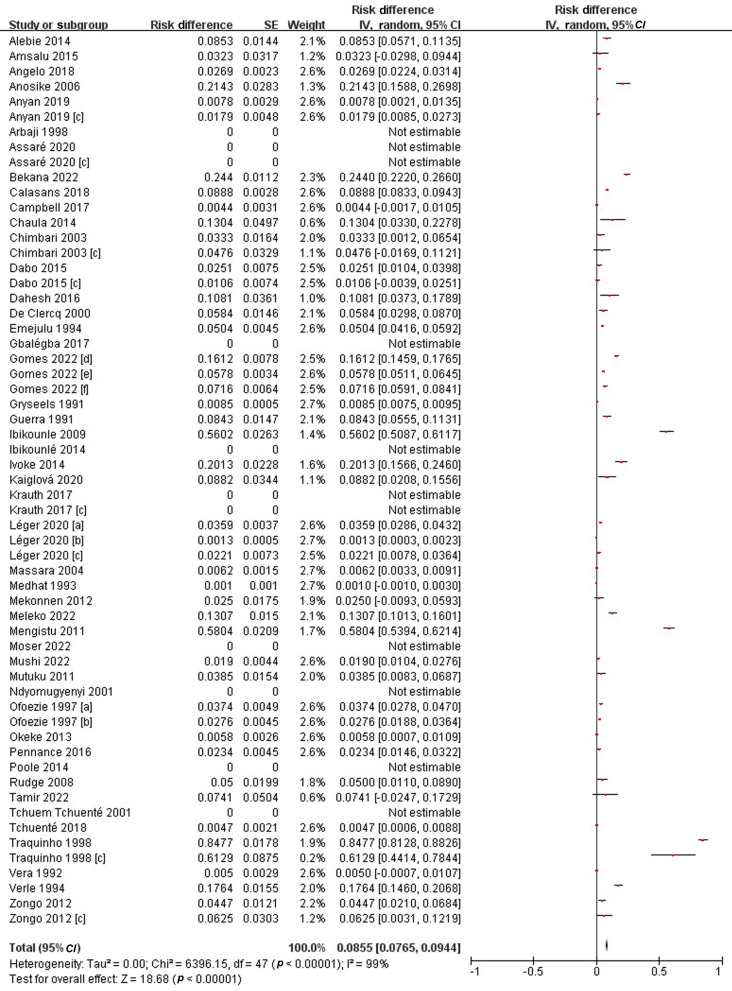
Subgroup pooled prevalence estimates of infected snails
A total of 84,954 snails were examined and 4125 of them were infected by either S. mansoni or S. haematobium. The overall PPE of schistosome cercariae in snails was 8.6% (95% CI: 7.7–9.4%). The prevalence extracted from included studies ranged from 0 to 84.8%, with substantial heterogeneity across studies (I2 = 99%, P < 0.01) (Fig. 3).
Fig. 3.
Forest plot diagram showing the prevalence of schistosomes cercariae in snails. * Each red dot represents risk difference of individual studies, and the horizontal line represents the 95% CI. The diamond indicates the pooled effect. a and b represent studies carried out in different regions of a country but published in one article. c represents S. mansoni results published in articles that also show S. haematobium results
Subgroup analysis was performed using the year of publication, areas surveyed and snail species. From 1991 to 2000, the PPE in snails was 12.9% (95% CI: 10.6–15.2%); from 2001 to 2010 it was 14.2% (95% CI: 9.2–19.3%); and from 2011 to 2022, it decreased to 5.2% (95% CI: 3.8–6.5%). The highest PPE in snails was observed in Africa, i.e. 8.5% (95% CI: 7.6–9.4%); followed by Latin America (Brazil) with 7.8% (95% CI: 3.5–12.1%); and Asia without infection snails [43]. The infection rate of schistosomes in Bulinus spp. was 6.9% (95% CI: 5.7–8.1%), while it was 12.1% (95% CI: 9.9–14.2%) in Biomphalaria spp. (Additional file 1: Fig. S6–S8).
Publication bias
The funnel plot dissymmetry demonstrated the presence of publication bias among intermediate host and definitive host studies included in this meta-analysis (Additional file 1: Fig. S9–S10). A high level of heterogeneity was observed (I2 > 90%), something which could not be reduced through subgroup analysis.
Correlation analysis between the infection rates in the intermediate host and definitive host
The results of the K-S test indicated that the data didn’t follow a normal distribution, so the rank correlation from a non-parametric correlation analysis was used to describe the degree and direction of the correlation between the two variables. The non-parametric correlation analysis indicated that the correlation was statistically significant. The correlation coefficient r was 0.3 (95% CI: − 0.01–0.5, P < 0.05) indicating that the two variables of all intermediate host snails and definitive hosts were positively correlated. The non-parametric correlation analysis of different schistosomiasis subgroup indicated that the correlation of S. haematobium and Bulinus spp. was statistically significant (r = 0.3, 95% CI: − 0.04–0.6, P < 0.05), while the correlation of S. mansoni and Biomphalaria spp. was not statistically significant (r = 0.3, 95% CI: − 0.02–0.7, P = 0.17).
The regression test indicated that there was a relationship between the infection rates in humans and snail intermediate hosts. The optimal model equation is obtained by fitting the linear and nonlinear models with two sets of parameters. The equation is Y = 0.001x3 − 0.056x2 + 1.790x + 20.761 (where y is the infection rate of schistosomes in definitive hosts, and x is the infection rate in intermediate hosts). Through this equation, the known infection rate in snail intermediate hosts can predict the human schistosomiasis infection rate. The results of the F test gave F = 2.9 (P < 0.05), which means that the nonlinear relationship between the explained variable and its predictors was significant. The R2 = 0.14, suggests that the intermediate host snail is a factor affecting the changes in local epidemic of schistosomiasis.
Discussion
Although schistosomiasis is a vector-borne disease and the appropriate intermediate host snail is regarded as an important factor impacting the distribution and endemicity of schistosomiasis, the correlations of the prevalence of schistosomiasis in definitive host and intermediate host is not well known. To the best of our knowledge, this study is the first systematic review and meta-analysis aiming at exploring the relationship of infection rates of schistosomes between intermediate host and humans worldwide, particularly focusing on S. haematobium and S. mansoni.
The results of this review indicate a persistently high global infection rate, primarily concentrated in sub-Saharan African countries. The PPE of students was highest in all populations. However, it is worth noting that the prevalence of schistosomiasis in the community and others was almost the same as SAC, indicating that the frequency of MDA against schistosomiasis and assessment of effectiveness of interventions only based on the prevalence in SAC are unreasonable [91, 92]. It supports the recommendation of the WHO’s new guideline for control and elimination of human schistosomiasis to extend PC from SAC to all age groups at risk of schistosome infection, with aims to eliminate schistosomiasis as a public health problem or interrupt the transmission of schistosomiasis in endemic communities. The infection rate of S. haematobium and S. mansoni in humans, seen in the subgroup analysis, was 28.8% and 25.6% respectively, basically identical with the results obtained by Feleke et al. [93] and Cando et al. [94]. The pooled prevalence of schistosomiasis in humans was 38.2% from 1991 to 2000, 26.9% from 2001 to 2010 and 22.7% from 2011 to 2022, showing a slowly decreasing trend over time. In addition, the demographic differences, the years of investigations conducted, as well as the number of snails in each area, may contribute to the difference detected in prevalence of schistosomiasis in humans across countries.
The overall pooled prevalence of schistosome cercariae was 8.6%, emphasizing the importance of snail control. This finding is very similar to the reports on freshwater snails in Brazil and other meta-analyses [95]. The downward PPE trend in snails from 12.9% in 1991−2000 over 14.2% in 2001−2010 to 5.2% in 2011−2022 confirms the decreasing trend presented by Nwoko et al., who reported that the pooled prevalence of schistosome cercariae decreased from 6.0% in the 1990s to 1.0% in the 2000s [49]. PC together with improved sanitation, environmental modification, better health education and behaviour changes might contribute to the recent lowering infection rates among freshwater snails. The highest pooled prevalence of schistosome cercariae obtained from Africa, with 8.5%, followed by Brazil (7.8%), is in line with the geographical prevalence tendency of schistosomiasis in humans.
The regression test indicated that there was a relationship between human schistosomiasis and the infection rate in the intermediate host. The optimal model equation suggests that the intermediate host snail can be a factor affecting the local variations in human schistosomiasis prevalence. We also found a statistical correlation between the prevalence of all schistosomiasis in intermediate host snails and definitive hosts locally, but the correlation was considered weak as the r value was less than 0.4. By subgroup analysis, this correlation existed between the prevalence of S. haematobium in humans and infection in Bulinus spp. snails, but was not detected between the prevalence of S. mansoni in humans and Biomphalaria spp. snails. This could be explained by many factors influencing human schistosomiasis levels, such as frequency of water contact, human behaviour with respect to water contact, the distance between villages and water bodies, intervention strength, capacity of snail survey and case finding [23, 96]. However, mapping the geographical distribution of schistosomiasis in humans as well as in the snail hosts would benefit targeted interventions in critical areas and support resource allocation.
Snail control, mainly by molluscicides, is the cornerstone of schistosomiasis control before the strategy for morbidity control, and has contributed to many successful control outcomes [5]. Early large-scale global schistosomiasis control programmes also emphasized on snail control. However, snail control had been challenged as excessive mollusciciding was considered to lead environmental pollution, destruct aquatic resources and require high cost [97]. WHO recommends WASH interventions, environmental interventions (water engineering and focal snail control with molluscicides) and behavioural change interventions as essential measures to help reduce transmission of Schistosoma spp. in endemic areas [23]. This study is the first meta-analysis to prove that the prevalence of schistosomiasis in humans and snails presented statistically significant relationships, supporting that policymakers should pay more attention to the integration of snail control to the ongoing deworming programmes against schistosomiasis.
There are a few limitations in this study, although valuable information was generated specially on the prevalence of S. mansoni and S. haematobium among freshwater snails and humans. First, available prevalence data were only obtained from 47 studies in 21countries, accounting for only a part of all endemic settings or countries. The pooled prevalence may not fully represent the real infection status of S. mansoni or S. haematobium in humans and snails, leading to a correlation bias. Second, the study was limited by the conventional microscopic techniques as the shortcomings of less sensitivity of these techniques might have a certain impact on the results. We didn’t include data based on molecular techniques for meta-analysis because most research based on molecular techniques were laboratory-based and the methods have not been completely unified [98]. Third, there are limited data on the prevalence of schistosomiasis in West Asia. Some surveys done in Asia could not be included in this analysis because the data were not readily available for both humans and snails. More high-quality research, e.g., high-sensitivity diagnostics is needed to assess whether data obtained from snail survey can be used to guide interventions against schistosomiasis.
Conclusions
Our findings showed that the overall PPE of either S. haematobium or S. mansoni in human host was 27.5% and the prevalence of schistosome cercariae was 8.6%, highlighting the need of sustained PC programme and snail control. The prevalence of schistosomiasis in humans and snails presented statistically significant relationships, so the distributions and strengths of infection in the intermediate host snail can be used as an indicator of the level of schistosomiasis risk. Further studies are needed to understand the ecology and transmission of the parasite between the snails and definitive hosts. In addition, policymakers should pay more attention to integration of snail control strategies to the ongoing de-worming programmes against schistosomiasis. This analysis has laid the foundation for the follow-up work and providing a scientific basis for decision-making.
Supplementary Information
Additional file 1. Table S1. The Joanna Briggs Institute (JBI) Prevalence Critical Appraisal Tool. Figure S1. Global distribution showing country location of included studies. Figure S2. Forest plot of subgroup PPE analysis of infection in the students, community and others. Figure S3. Forest plot of subgroup PPE analysis of infection in different years. Figure S4. Forest plot of subgroup PPE analysis of infection in Africa, South America and Asia. Figure S5. Forest plot of subgroup PPE analysis of infection in the S. mansoni and S. haematobium. Figure S6. Forest plot of subgroup PPE analysis of snail infectivity indifferent years. Figure S7. Forest plot of subgroup PPE analysis of infectivity in the Africa, South America and Asia. Figure S8. Forest plot of subgroup PPE analysis of infection in the Biomphalaria spp. and Bulinus spp. Figure S9. Funnel plot with 95% confidence limit showing publication bias across studies on the prevalence of S. mansoni and S. haematobium. Figure S10. Funnel plot with 95% confidence limit showing publication bias across studies on the prevalence of S. mansoni and S. haematobium among freshwater snails.
Acknowledgements
We thank the China-Zanzibar cooperation project for schistosomiasis, Pemba NTD office and Ministry of Health for their great support in facilitating this work. We would like to thank everyone for their kind help during the preparation of this manuscript.
Author contributions
XYW, QL, YLL and SYG collected and analyzed the data, prepared figures and tables, authored drafts of the paper. SZL, XNZ, GJG conceived and designed the study. XYW, KY and JX screened titles and abstracts of papers to remove irrelevant references and the full texts of potentially relevant papers were reviewed further. SJ, JFZ, RB and JX revised the report. JX reviewed drafts of the paper, and approved the final draft. All authors have agreed to the published version of the manuscript. All authors read and approved the final manuscript.
Funding
This study was funded by the grants from the National Science Foundation of China (82073619), the National Key Research and Development Program of China (2021YFC2300800, 2021YFC2300804), the General Programs of Jiangsu Commission of Health (H202309 and the Schistosomiasis and Parasitic Diseases Project of Jiangsu Province (× 202103).
Availability of data and materials
All datasets generated and analysed, including the search strategy, list of the included and excluded studies, data extracted, and quality assessment, are available in the Article and on request from the corresponding author Jing Xu.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All authors declare no competing interests.
References
- 1.Thétiot-Laurent SAL, Boissier J, Robert A, Meunier B. Schistosomiasis chemotherapy. Angew Chem Int Ed Engl. 2013;52(31):7936–56. 10.1002/anie.201208390 [DOI] [PubMed] [Google Scholar]
- 2.McManus DP, Dunne DW, Sacko M, Utzinger J, Vennervald BJ, Zhou XN. Schistosomiasis. Nat Rev Dis Primers. 2018;4(1):13. 10.1038/s41572-018-0013-8 [DOI] [PubMed] [Google Scholar]
- 3.Colley DG, Bustinduy AL, Secor WE, King CH. Human schistosomiasis. Lancet. 2014;383(9936):2253–64. 10.1016/S0140-6736(13)61949-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gryseels B, Polman K, Clerinx J, Kestens L. Human schistosomiasis. Lancet. 2006;368(9541):1106–18. 10.1016/S0140-6736(06)69440-3 [DOI] [PubMed] [Google Scholar]
- 5.Muhsin MA, Wang X, Kabole FM, Zilabumba J, Yang K. The indispensability of snail control for accelerating schistosomiasis elimination: evidence from Zanzibar. Trop Med Infect Dis. 2022;7(11):347. 10.3390/tropicalmed7110347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ross AGP, Bartley PB, Sleigh AC, Olds GR, Li Y, Williams GM, et al. Schistosomiasis. N Engl J Med. 2002;346(16):1212–20. 10.1056/NEJMra012396 [DOI] [PubMed] [Google Scholar]
- 7.Hailegebriel T, Nibret E, Munshea A. Prevalence of Schistosoma mansoni and S. haematobium in snail intermediate hosts in Africa: a systematic review and meta-analysis. J Trop Med. 2020;2020:8850840. 10.1155/2020/8850840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown DS. Freshwater snails of Africa and their medical importance. London: CRC Press; 1994. [Google Scholar]
- 9.Jarne P, Finot L, Delay B, Thaler L. Self-fertilization versus cross-fertilization in the hermaphroditic freshwater snail Bulinus globosus. Evolution. 1991;45(5):1136–46. 10.2307/2409721 [DOI] [PubMed] [Google Scholar]
- 10.Wang X, Juma S, Li W, Suleman M, Muhsin MA, He J, et al. Potential risk of colonization of Bulinus globosus in the mainland of China under climate change. Infect Dis Poverty. 2022;11(1):52. 10.1186/s40249-022-00980-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lo NC, Bezerra FSM, Colley DG, Fleming FM, Homeida M, Kabatereine N, et al. Review of 2022 WHO guidelines on the control and elimination of schistosomiasis. Lancet Infect Dis. 2022;22(11):e327–35. 10.1016/S1473-3099(22)00221-3 [DOI] [PubMed] [Google Scholar]
- 12.Kokaliaris C, Garba A, Matuska M, Bronzan RN, Colley DG, Dorkenoo AM, et al. Effect of preventive chemotherapy with praziquantel on schistosomiasis among school-aged children in sub-Saharan Africa: a spatiotemporal modelling study. Lancet Infect Dis. 2022;22(1):136–49. 10.1016/S1473-3099(21)00090-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bergquist R, Utzinger J, Keiser J. Controlling schistosomiasis with praziquantel: how much longer without a viable alternative? Infect Dis Poverty. 2017;6(1):74. 10.1186/s40249-017-0286-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sokolow SH, Wood CL, Jones IJ, Lafferty KD, Kuris AM, Hsieh MH, et al. To reduce the global burden of human schistosomiasis, use “old fashioned” snail control. Trends Parasitol. 2018;34(1):23–40. 10.1016/j.pt.2017.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Civitello DA-O, Fatima H, Johnson LR, Nisbet RM, Rohr JR. Bioenergetic theory predicts infection dynamics of human schistosomes in intermediate host snails across ecological gradients. Ecol Lett. 2018;21(5):692–701. 10.1111/ele.12937 [DOI] [PubMed] [Google Scholar]
- 16.Yasin MG, Alim MA, Anisuzzaman, Ahasan SA, Munsi MN, Chowdhury EH, et al. Trematode infections in farm animals and their vector snails in Saint Martin's Island, the southeastern offshore area of Bangladesh in the Bay of Bengal. J Vet Med Sci. 2018; 80(4): 684–8. [DOI] [PMC free article] [PubMed]
- 17.Kamel B, Laidemitt MR, Lu L, Babbitt C, Weinbaum OL, Mkoji GM, et al. Detecting and identifying Schistosoma infections in snails and aquatic habitats: a systematic review. PLoS Negl Trop Dis. 2021;15(3): e0009175. 10.1371/journal.pntd.0009175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vidigal Teofânia HDA, Coscarelli D, Montresor Lângia C. Molecular studies in Brazilian malacology: tools, trends and perspectives. Lundiana. 2013;11(1/2):47–63. 10.35699/2675-5327.2013.23840 [DOI] [Google Scholar]
- 19.Chala B. Advances in diagnosis of schistosomiasis: focus on challenges and future approaches. Int J Gen Med. 2023;16:983–95. 10.2147/IJGM.S391017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.WHO. Schistosomiasis and soil-transmitted helminthiasis: number of people treated in 2019. Wkly Epidemiol Rec. 2020;50(95):629–40. [Google Scholar]
- 21.Xu J, Dong LL, Sun H, Huang P, Zhang RZ, Wang XY, et al. Small change, big difference: a promising praziquantel derivative designated P96 with broad-spectrum antischistosomal activity for chemotherapy of schistosomiasis japonica. PLoS Negl Trop Dis. 2023;17(7): e0011215. 10.1371/journal.pntd.0011215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li EY, Gurarie D, Lo NC, Zhu X, King CH. Improving public health control of schistosomiasis with a modified WHO strategy: a model-based comparison study. Lancet Glob Health. 2019;7(10):e1414–22. 10.1016/S2214-109X(19)30346-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lo NC, Lai YS, Karagiannis-Voules DA, Bogoch II, Coulibaly JT, Bendavid E, et al. Assessment of global guidelines for preventive chemotherapy against schistosomiasis and soil-transmitted helminthiasis: a cost-effectiveness modelling study. Lancet Infect Dis. 2016;16(9):1065–75. 10.1016/S1473-3099(16)30073-1 [DOI] [PubMed] [Google Scholar]
- 24.WHO. Ending the neglect to attain the sustainable development goals: a road map for neglected tropical diseases 2021–2030. Jan 28, 2021. https://www.who.int/publications/i/item/9789240010352. Accessed Oct 19, 2023.
- 25.Oluwole AS, Ekpo UF, Nebe OJ, Akpan NM, Jacob SM, Amazigo UV, et al. The new WHO guideline for control and elimination of human schistosomiasis: implications for the Schistosomiasis Elimination Programme in Nigeria. Infect Dis Poverty. 2022;11(1):111. 10.1186/s40249-022-01034-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.WHO. WHO guideline on control and elimination of human schistosomiasis. Geneva: World Health Organization, 2022. Feb 14, 2022. https://www.who.int/publications/i/item/9789240041608. Accessed Oct 22, 2023. [PubMed]
- 27.Mari L, Ciddio M, Casagrandi R, Perez-Saez J, Bertuzzo E, Rinaldo A, et al. Heterogeneity in schistosomiasis transmission dynamics. J Theor Biol. 2017;432:87–99. 10.1016/j.jtbi.2017.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lengeler C, Utzinger J, Tanner M. Questionnaires for rapid screening of schistosomiasis in sub-Saharan Africa. Bull World Health Organ. 2002;80(3):235–42. [PMC free article] [PubMed] [Google Scholar]
- 29.WHO. Schistosomiasis and soil-transmitted helminthiases: progress report 2020. Wkly Epidemiol Rec. 2021;48(96):585–95. [Google Scholar]
- 30.Liang S, Ponpetch K, Zhou Y-B, Guo J, Erko B, Stothard JR, et al. Diagnosis of Schistosoma infection in non-human animal hosts: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2022;16(5): e0010389. 10.1371/journal.pntd.0010389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339: b2535. 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag. 2014;3(3):123–8. 10.15171/ijhpm.2014.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Isaiah PM, Sólveig Palmeirim M, Steinmann P. Epidemiology of pediatric schistosomiasis in hard-to-reach areas and populations: a scoping review. Infect Dis Poverty. 2023;12(1):37. 10.1186/s40249-023-01088-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Song F, Parekh S, Hooper L, Loke YK, Ryder J, Sutton AJ, et al. Dissemination and publication of research findings: an updated review of related biases. Health Technol Assess. 2010;14(8):1–193. 10.3310/hta14080 [DOI] [PubMed] [Google Scholar]
- 35.Wilkinson I. Summing up: the science of reviewing research. J Educ Stat. 1987;12(3):302–8. [Google Scholar]
- 36.Bruni L, Albero G, Rowley J, Alemany L, Arbyn M, Giuliano AR, et al. Global and regional estimates of genital human papillomavirus prevalence among men: a systematic review and meta-analysis. Lancet Glob Health. 2023;11(9):e1345–62. 10.1016/S2214-109X(23)00305-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cui Y, Peng L. Assessing dynamic covariate effects with survival data. Lifetime Data Anal. 2022;28(4):675–99. 10.1007/s10985-022-09571-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shi R, Conrad SA. Correlation and regression analysis. Ann Allergy Asthma Immunol. 2009;103(4):S35–41. 10.1016/S1081-1206(10)60820-4 [DOI] [PubMed] [Google Scholar]
- 39.Zou KH, Tuncali K, Silverman SG. Correlation and simple linear regression. Radiology. 2003;227(3):617–28. 10.1148/radiol.2273011499 [DOI] [PubMed] [Google Scholar]
- 40.Bardsley WG, McGinlay PB. The use of non-linear regression analysis and the F test for model discrimination with dose-response curves and ligand binding data. J Theor Biol. 1987;126(2):183–201. 10.1016/S0022-5193(87)80228-X [DOI] [PubMed] [Google Scholar]
- 41.Alebie G, Erko B, Aemero M, Petros B. Epidemiological study on Schistosoma mansoni infection in Sanja area, Amhara region, Ethiopia. Parasit Vectors. 2014;7(1):1–10. 10.1186/1756-3305-7-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Amsalu G, Mekonnen Z, Erko B. A new focus of schistosomiasis mansoni in Hayk town, northeastern Ethiopia. BMC Res Notes. 2015;8(1):1–6. 10.1186/s13104-014-0965-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Angelo T, Buza J, Kinung’hi SM, Kariuki HC, Mwanga JR, Munisi DZ, et al. Geographical and behavioral risks associated with Schistosoma haematobium infection in an area of complex transmission. Parasit Vectors. 2018;11(1):1–9. 10.1186/s13071-018-3064-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Anosike JC, Oguwuike UT, Nwoke BE, Asor J, Ikpeama C, Nwosu D, et al. Studies on vesical schistosomiasis among rural Ezza farmers in the southwestern border of Ebonyi State, Nigeria. Ann Agric Environ Med. 2006;13(1):13–9. [PubMed] [Google Scholar]
- 45.Anyan WK, Abonie SD, Aboagye-Antwi F, et al. Concurrent Schistosoma mansoni and Schistosoma haematobium infections in a peri-urban community along the Weija dam in Ghana: a wake up call for effective National Control Programme. Acta Trop. 2019;199: 105116. 10.1016/j.actatropica.2019.105116 [DOI] [PubMed] [Google Scholar]
- 46.Arbaji A, Amr Z, Abbas A, Al-Oran R, Al-Kharabsheh S, Al-Melhim W. New sites of Bulinus truncatus and indigenous cases of urinary schistosomiasis in Jordan. Parasite. 1998;5(4):379–82. 10.1051/parasite/1998054379 [DOI] [PubMed] [Google Scholar]
- 47.Assaré RK, N’Tamon RN, Bellai LG, Koffi JA, Mathieu TI, Ouattara M, et al. Characteristics of persistent hotspots of Schistosoma mansoni in western Côte d’Ivoire. Parasit Vectors. 2020;13(1):1–16. 10.1186/s13071-020-04188-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bekana T, Abebe E, Mekonnen Z, Tulu B, Ponpetch K, Liang S, et al. Parasitological and malacological surveys to identify transmission sites for Schistosoma mansoni in Gomma District, south-western Ethiopia. Sci Rep. 2022;12(1):17063. 10.1038/s41598-022-21641-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Calasans TAS, Souza GTR, Melo CM, Madi RR, Jeraldo VDLS. Socioenvironmental factors associated with Schistosoma mansoni infection and intermediate hosts in an urban area of northeastern Brazil. PLoS ONE. 2018;13(5): e0195519. 10.1371/journal.pone.0195519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Campbell SJ, Stothard JR, O’Halloran F, Sankey D, Durant T, Ombede DE, et al. Urogenital schistosomiasis and soil-transmitted helminthiasis (STH) in Cameroon: an epidemiological update at Barombi Mbo and Barombi Kotto crater lakes assessing prospects for intensified control interventions. Infect Dis Poverty. 2017;6(01):36–48. 10.1186/s40249-017-0264-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chaula SA, Tarimo DS. Impact of praziquantel mass drug administration campaign on prevalence and intensity of Schistosoma haemamtobium among schoolchildren in Bahi district, Tanzania. Tanzan J Health Res. 2014;16(1):1–8. 10.4314/thrb.v16i1.1 [DOI] [PubMed] [Google Scholar]
- 52.Chimbari M, Dhlomo E, Mwadiwa E, Mubila L. Transmission of schistosomiasis in Kariba, Zimbabwe, and a cross-sectional comparison of schistosomiasis prevalences and intensities in the town with those in Siavonga in Zambia. Ann Trop Med Parasitol. 2003;97(6):605–16. 10.1179/000349803225001508 [DOI] [PubMed] [Google Scholar]
- 53.Dabo A, Diarra AZ, Machault V, Touré O, Niambélé DS, Kanté A, et al. Urban schistosomiasis and associated determinant factors among school children in Bamako, Mali, West Africa. Infect Dis Poverty. 2015;4(1):1–13. 10.1186/2049-9957-4-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dahesh S, Farid BE. Epidemiological situation of urinary schistosomiasis in Tamwah area, Giza, Egypt: assessment and control. J Egypt Soc Parasitol. 2016;46(3):485–96. 10.21608/jesp.2016.78043 [DOI] [PubMed] [Google Scholar]
- 55.De Clercq D, Vercruysse J, Sène M, Seck I, Sall CS, Ly A, et al. The effects of irrigated agriculture on the transmission of urinary schistosomiasis in the Middle and Upper Valleys of the Senegal River basin. Ann Trop Med Parasitol. 2000;94(6):581–90. 10.1080/00034983.2000.11813581 [DOI] [PubMed] [Google Scholar]
- 56.Emejulu A, Alabaronye F, Ezenwaji H, Okafor F. Investigation into the prevalence of urinary schistosomiasis in the Agulu Lake area of Anambra State, Nigeria. J Helminthol. 1994;68(2):119–23. 10.1017/S0022149X00013638 [DOI] [PubMed] [Google Scholar]
- 57.Gbalégba NGG, Silué KD, Ba O, Ba H, Tian-Bi NTY, Yapi GY, et al. Prevalence and seasonal transmission of Schistosoma haematobium infection among school-aged children in Kaedi town, southern Mauritania. Parasit Vectors. 2017;10:1–12. 10.1186/s13071-017-2284-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gomes ECS, Silva IEP, Nascimento WRC, Loyo RM, Domingues ALC, Barbosa CS. Urban schistosomiasis: an ecological study describing a new challenge to the control of this neglected tropical disease. Lancet Reg Health Am. 2022;8: 100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gryseels B. The epidemiology of schistosomiasis in Burundi and its consequences for control. Trans R Soc Trop Med Hyg. 1991;85(5):626–33. 10.1016/0035-9203(91)90371-5 [DOI] [PubMed] [Google Scholar]
- 60.Guerra H, Guimarães C, França M, Rocha R, Katz N. Identification of a new focus of Schistosoma mansoni (Municipality of Nova Lima, MG, Brazil). Rev Soc Bras Med Trop. 1991;24(3):169–72. 10.1590/S0037-86821991000300008 [DOI] [PubMed] [Google Scholar]
- 61.Ibikounlé M, Mouahid G, Sakiti N, Massougbodji A, Moné H. Freshwater snail diversity in Benin (West Africa) with a focus on human schistosomiasis. Acta Trop. 2009;111(1):29–34. 10.1016/j.actatropica.2009.02.001 [DOI] [PubMed] [Google Scholar]
- 62.Ibikounlé M, Ogouyèmi-Hounto A, de Tové YSS, Dansou A, Courtin D, Kindé-Gazard D, et al. Épidémiologie de la schistosomose urinaire chez les enfants scolarisés de la commune de Péhunco dans le Nord Bénin: prospection malacologique. Bull Soc Pathol Exot. 2014;107:177–84. 10.1007/s13149-014-0345-x [DOI] [PubMed] [Google Scholar]
- 63.Ivoke N, Ivoke O, Nwani C, Ekeh FN, Asogwa CN, Atama CI, et al. Prevalence and transmission dynamics of Schistosoma haematobium infection in a rural community of southwestern Ebonyi State, Nigeria. Trop Biomed. 2014;31(1):77–88. [PubMed] [Google Scholar]
- 64.Kaiglová A, Changoma M, Špajdelová J, Jakubcová D, Bírová K. Urinary schistosomosis in patients of rural medical health centers in Kwale county, Kenya. Helminthologia. 2020;57(1):19–27. 10.2478/helm-2020-0001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Krauth SJ, Wandel N, Traoré SI, Penelope V, Hattendorf J, Achi LY, et al. Distribution of intermediate host snails of schistosomiasis and fascioliasis in relation to environmental factors during the dry season in the Tchologo region, Côte d’Ivoire. Adv Water Resour. 2017;108:386–96. 10.1016/j.advwatres.2016.11.016 [DOI] [Google Scholar]
- 66.Léger E, Borlase A, Fall CB, Diouf ND, Diop SD, Yasenev L, et al. Prevalence and distribution of schistosomiasis in human, livestock, and snail populations in northern Senegal: a One Health epidemiological study of a multi-host system. Lancet Planet Health. 2020;4(8):e330–42. 10.1016/S2542-5196(20)30129-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Massara CL, Peixoto SV, Barros HdS, Enk MJ, Carvalho OdS, Schall V. Factors associated with schistosomiasis mansoni in a population from the municipality of Jaboticatubas, State of Minas Gerais, Brazil. Mem Inst Oswaldo Cruz. 2004;99:127–34. 10.1590/S0074-02762004000900023 [DOI] [PubMed] [Google Scholar]
- 68.Medhat A, Abdel-Aty MA, Nafeh M, Hammam H, Abdel-Samia A, Strickland GT. Foci of Schistosoma mansoni in Assiut province in middle Egypt. Trans R Soc Trop Med Hyg. 1993;87(4):404–5. 10.1016/0035-9203(93)90013-G [DOI] [PubMed] [Google Scholar]
- 69.Mekonnen Z, Haileselassie H, Medhin G, Erko B, Berhe N. Schistosomiasis mansoni focus in Mekele City, northern Ethiopia. Ethiop Med J. 2012;50(4):331–6. [PubMed] [Google Scholar]
- 70.Meleko A, Li S, Turgeman DB, Bruck M, Kesete NZ, Zaadnoordijk W, et al. Schistosomiasis control in Ethiopia: the role of snail mapping in endemic communities. Trop Med Infect Dis. 2022;7(10):272. 10.3390/tropicalmed7100272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mengistu M, Shimelis T, Torben W, Terefe A, Kassa T, Hailu A. Human intestinal schistosomiasis in communities living near three rivers of Jimma town, south western Ethiopia. Ethiop J Health Sci. 2011;21(2):111–8. 10.4314/ejhs.v21i2.69051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Moser W, Batil AA, Ott R, Abderamane M, Clements R, Wampfler R, et al. High prevalence of urinary schistosomiasis in a desert population: results from an exploratory study around the Ounianga lakes in Chad. Infect Dis Poverty. 2022;11(1):5. 10.1186/s40249-021-00930-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mutuku FM, King CH, Bustinduy AL, Mungai PL, Muchiri EM, Kitron U. Impact of drought on the spatial pattern of transmission of Schistosoma haematobium in coastal Kenya. Am J Trop Med Hyg. 2011;85(6):1065. 10.4269/ajtmh.2011.11-0186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ndyomugyenyi R, Minjas J. Urinary schistosomiasis in schoolchildren in Dar-es-Salaam, Tanzania, and the factors influencing its transmission. Ann Trop Med Parasitol. 2001;95(7):697–706. 10.1080/00034983.2001.11813687 [DOI] [PubMed] [Google Scholar]
- 75.Ofoezie I, Asaolu S. Water level regulation and control of schistosomiasis transmission: a case study in Oyan Reservoir, Ogun State, Nigeria. Bull World Health Organ. 1997;75(5):435. [PMC free article] [PubMed] [Google Scholar]
- 76.Okeke OC, Ubachukwu PO. Urinary schistosomiasis in urban and semi-urban communities in South-Eastern Nigeria. Iran J Parasitol. 2013;8(3):467. [PMC free article] [PubMed] [Google Scholar]
- 77.Pennance T, Person B, Muhsin MA, Khamis AN, Muhsin J, Khamis IS, et al. Urogenital schistosomiasis transmission on Unguja Island, Zanzibar: characterisation of persistent hot-spots. Parasit Vectors. 2016;9(1):1–13. 10.1186/s13071-016-1847-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Poole H, Terlouw DJ, Naunje A, Mzembe K, Stanton M, Betson M, et al. Schistosomiasis in pre-school-age children and their mothers in Chikhwawa district, Malawi with notes on characterization of schistosomes and snails. Parasit Vectors. 2014;7:1–12. 10.1186/1756-3305-7-153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rudge JW, Stothard JR, Basáñez M-G, Mgeni AF, Khamis IS, Khamis AN, et al. Micro-epidemiology of urinary schistosomiasis in Zanzibar: local risk factors associated with distribution of infections among schoolchildren and relevance for control. Acta Trop. 2008;105(1):45–54. 10.1016/j.actatropica.2007.09.006 [DOI] [PubMed] [Google Scholar]
- 80.Tamir Z, Animut A, Dugassa S, Gebreselassie A, Tsegaye A, Kassa T, et al. Intestinal helminthiasis survey with emphasis on schistosomiasis in Koga irrigation scheme environs, northwest Ethiopia. PLoS ONE. 2022;17(8): e0272560. 10.1371/journal.pone.0272560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tchuem Tchuenté L, Southgate V, Webster B, De Bont J, Vercruysse J. Impact of installation of a water pump on schistosomiasis transmission in a focus in Cameroon. Trans R Soc Trop Med Hyg. 2001;95(3):255–6. 10.1016/S0035-9203(01)90228-7 [DOI] [PubMed] [Google Scholar]
- 82.Tchuenté LT, Ombede DE, Noumedem CD, Chuinteu GND, Nono BF, Lemegne ACN, et al. Prospects for the elimination of schistosomiasis and soil-transmitted helminthiasis: exploring disease trends through time at the Barombi crater lakes, South-West Cameroon. Parasitology. 2018;145(13):1700–14. 10.1017/S0031182018001531 [DOI] [PubMed] [Google Scholar]
- 83.Traquinho G, Quintó L, Nalá R, Vaz RG, Corachan M. Schistosomiasis in northern Mozambique. Trans R Soc Trop Med Hyg. 1998;92(3):279–81. 10.1016/S0035-9203(98)91011-2 [DOI] [PubMed] [Google Scholar]
- 84.Vera C, Mouchet F, Bremond P, Sidiki A, Sellin E, Sellin B. Natural infection of Bulinus senegalensis by Schistosoma haematobium in a temporary pool focus in Niger: characterization by cercarial emergence patterns. Trans R Soc Trop Med Hyg. 1992;86(1):62. 10.1016/0035-9203(92)90442-F [DOI] [PubMed] [Google Scholar]
- 85.Verle P, Stelma F, Desreumaux P, Dieng A, Diaw O, Kongs A, et al. Preliminary study of urinary schistosomiasis in a village in the delta of the Senegal river basin, Senegal. Trans R Soc Trop Med Hyg. 1994;88(4):401–5. 10.1016/0035-9203(94)90400-6 [DOI] [PubMed] [Google Scholar]
- 86.Zongo D, Kabre B, Dayeri D, Savadogo B, Poda J. Comparative study of schistosomiasis transmission (urinary and intestinal forms) at 10 sites in Burkina Faso (in sub-Saharan Africa). Med Sante Trop. 2012;22(3):323–9. [DOI] [PubMed] [Google Scholar]
- 87.Mushi V, Zacharia A, Shao M, Mubi M, Tarimo D. Persistence of Schistosoma haematobium transmission among school children and its implication for the control of urogenital schistosomiasis in Lindi, Tanzania. PLoS ONE. 2022;17(2): e0263929. 10.1371/journal.pone.0263929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Keller D, Rothen J, Dangy J-P, Saner C, Daubenberger C, Allan F, et al. Performance of a real-time PCR approach for diagnosing Schistosoma haematobium infections of different intensity in urine samples from Zanzibar. Infect Dis Poverty. 2020;9(1):128. 10.1186/s40249-020-00726-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Katz N, Coelho PM, Pellegrino J. Evaluation of Kato’s quantitative method through the recovery of Schistosoma mansoni eggs added to human feces. J Parasitol. 1970;56(5):1032–3. 10.2307/3277532 [DOI] [PubMed] [Google Scholar]
- 90.Gaye PM, Doucouré S, Sow D, Sokhna C, Ranque S. Identification of Bulinus forskalii as a potential intermediate host of Schistosoma haematobium in Senegal. PLoS Negl Trop Dis. 2023;17(5): e0010584. 10.1371/journal.pntd.0010584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Burnim M, Ivy JA, King CH. Systematic review of community-based, school-based, and combined delivery modes for reaching school-aged children in mass drug administration programs for schistosomiasis. PLoS Negl Trop Dis. 2017;11(10): e0006043. 10.1371/journal.pntd.0006043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Joof E, Sanyang AM, Camara Y, Sey AP, Baldeh I, Jah SL, et al. Prevalence and risk factors of schistosomiasis among primary school children in four selected regions of The Gambia. PLoS Negl Trop Dis. 2021;15(5): e0009380. 10.1371/journal.pntd.0009380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Feleke DG, Alemu Y, Bisetegn H, Debash H. Accuracy of diagnostic tests for detecting Schistosoma mansoni and S. haematobium in sub-Saharan Africa: a systematic review and meta-analysis. Biomed Res Int. 2023;2023:3769931. 10.1155/2023/3769931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cando LF, Perias GAS, Tantengco OAG, Dispo MD, Ceriales JA, Girasol MJG, et al. The global prevalence of Schistosoma mansoni, S. japonicum, and S. haematobium in pregnant women: a systematic review and meta-analysis. Trop Med Infect Dis. 2022;7(11):354. 10.3390/tropicalmed7110354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Nwoko OE, Kalinda C, Chimbari MJ. Systematic review and meta-analysis on the infection rates of schistosome transmitting snails in Southern Africa. Trop Med Infect Dis. 2022;7(5):72. 10.3390/tropicalmed7050072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Grimes JET, Croll D, Harrison WE, Utzinger J, Freeman MC, Templeton MR. The roles of water, sanitation and hygiene in reducing schistosomiasis: a review. Parasit Vectors. 2015;8(1):156. 10.1186/s13071-015-0766-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sokolow SH, Wood CL, Jones IJ, Swartz SJ, Lopez M, Hsieh MH, et al. Global assessment of schistosomiasis control over the past century shows targeting the snail intermediate host works best. PLoS Negl Trop Dis. 2016;10(7): e0004794. 10.1371/journal.pntd.0004794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rohr JR, Sack A, Bakhoum S, Barrett CB, Lopez-Carr D, Chamberlin AJ, et al. A planetary health innovation for disease, food and water challenges in Africa. Nature. 2023;619:782–7. 10.1038/s41586-023-06313-z [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Table S1. The Joanna Briggs Institute (JBI) Prevalence Critical Appraisal Tool. Figure S1. Global distribution showing country location of included studies. Figure S2. Forest plot of subgroup PPE analysis of infection in the students, community and others. Figure S3. Forest plot of subgroup PPE analysis of infection in different years. Figure S4. Forest plot of subgroup PPE analysis of infection in Africa, South America and Asia. Figure S5. Forest plot of subgroup PPE analysis of infection in the S. mansoni and S. haematobium. Figure S6. Forest plot of subgroup PPE analysis of snail infectivity indifferent years. Figure S7. Forest plot of subgroup PPE analysis of infectivity in the Africa, South America and Asia. Figure S8. Forest plot of subgroup PPE analysis of infection in the Biomphalaria spp. and Bulinus spp. Figure S9. Funnel plot with 95% confidence limit showing publication bias across studies on the prevalence of S. mansoni and S. haematobium. Figure S10. Funnel plot with 95% confidence limit showing publication bias across studies on the prevalence of S. mansoni and S. haematobium among freshwater snails.
Data Availability Statement
All datasets generated and analysed, including the search strategy, list of the included and excluded studies, data extracted, and quality assessment, are available in the Article and on request from the corresponding author Jing Xu.