ABSTRACT
Background:
Occupational lung diseases (OLDs) contribute a significant proportion to the global burden of pulmonary morbidities but are grossly misdiagnosed due to the relative lack of attribution given to occupational exposures. Obstructive lung diseases are known to be associated with long-lasting disability and loss of earning capacity (LOEC) among workers in industrial setups, thus reducing nationwide productivity.
Objective:
In this context, the study aimed to find out the pattern of OLD and factors associated with the severity of it among patients in a tertiary care hospital.
Materials and Methods:
The study was a record-based secondary data analysis conducted in the Medical Records Department of a Medical College in Kolkata. A computerized database of patients attending Special Medical Board (SMB) examinations from the Department of Medical Records was utilized for data collection. A data abstraction format was constructed to collect information on pulmonary morbidity, occupational exposure, and sociodemographic and behavioral variables. Extracted data were analyzed in Microsoft Excel and Statistical Package for Social Sciences (SPSS) software
Results:
After a review of records, it was shown that 62.3% (66 out of 106 people) of the study subjects had an obstructive type of OLD, the most common being Jute Byssinosis. A negative correlation (Spearman’s ρ = -0.136) was found between pulmonary function (FEV1/FVC) and LOEC (%) in the study subjects. In the multivariable logistic regression, exposure to organic dust was found to be significantly associated with worsened lung function {adjusted-Odd’s Ratio (95% Confidence Interval) =3.11 (1.1–8.8), P value = 0.03}.
Conclusion:
OLD is an understated health issue, especially in an industrial diaspora of developing countries, like India. Healthcare facilities should utilize their resources properly for the advancement of medical surveillance in industries where organic dust is produced. Health education of the stakeholders regarding the consequences of OLDs and the benefits of preventive primary approaches will go a long way in alleviating the burden of disease.
Keywords: Industrial workers, lung disease, occupational exposure
Introduction
Occupational lung disease (OLD), essentially arising from occupational exposures, comprises a substantial proportion of the total disease burden in modern industrial societies globally.[1] Most of OLDs are caused by repeated and long-lasting exposure to certain hazardous agents, such as inorganic dust of asbestos, silica, coal dust, and organic dust from hemp, flax, and cotton processing, also due to inhalation of fungal spores from moldy hay.[2] OLDs encompass a wide range of morbidities—occupational asthma being the most diagnosed condition. Other OLDs consist of both acute and chronic conditions, like from hypersensitivity pneumonitis, and chronic obstructive pulmonary disease (COPD) to pulmonary fibrosis.[3] There is an increasingly evidential association between COPD and brassware workers, glass bangle workers, or workers in cotton/jute industries.[4] Most OLDs, like silicosis, asbestosis, anthracosis, occupational asthma, and byssinosis, are mostly under or misdiagnosed because of a lack of adequate surveillance systems or healthcare facilities available for industrial workers. Many such cases are first seen by primary care physicians, and it often becomes difficult for them to distinguish OLDs from general pulmonary morbidities as they are ignorant about the detrimental effects of occupational exposures.[5] However, these diseases are preventable by appropriate control of risk factors and the implementation of proper medical surveillance systems in the workplace. The rationale for the surveillance of occupational respiratory diseases is prevention. Prevention aims, ideally, to eliminate or reduce exposure to occupational risks to avoid any subsequent disease onset and, when not possible, to detect any disease at a pre-clinical stage to reduce its severity and progression.[6] Diagnosis of OLDs commences from the occupational and environmental exposure history, with pulmonary function tests like spirometry which can evaluate the severity of the disease, and lastly, imaging technology like chest radiograph which remained globally the primary mode of screening for pneumoconiosis and any other interstitial lung diseases in occupational setup.[7]
In India, the burden of occupational respiratory morbidity is mostly concentrated among the working population in the industrial diaspora which is mostly in a low socio-economic profile. Occupational factors that have serious ill pulmonary consequences for the health of the workers need extra attention from governmental agencies to formulate policies that ensure a healthy working environment in India. Therefore, government infrastructures or social insurance institutes that ensure social security to workers are ideal for addressing the issue in question. Indian Factories Act (1948) lists 29 notifiable diseases among which the following are OLDs—coal miners’ pneumoconiosis, asbestosis, silicosis, byssinosis, poisoning by inhalation of fumes, any pathological changes due to X-ray, and occupational cancer.[8] However, the Employee State Insurance (ESI) Act mandates insured workers, who contracted the following lung diseases due to occupational exposures, medical and extended sickness benefits: bronchiectasis, interstitial lung disease, and COPD with Cor Pulmonale.[9] Chronic lung diseases might lead to temporary or permanent disability or loss of earning capacity (LOEC). The medical board of ESI corporation hospitals evaluates the extent of occupational disease in employees by estimating LOEC, and therefore, medical records from ESI healthcare facilities would provide a fair estimation of the magnitude and pattern of occupational diseases (including pulmonary morbidities) among industrial workers. In this aforementioned context, the present study aims to determine the pattern of OLDs among industrial workers who underwent evaluation at a tertiary care hospital from the records of the medical board and also the factors associated with the severity of this diseased condition.
Materials and Methods
Study design, settings, and participants
This institution-based observational study was conducted from July 2023 to September 2023 with the data of the patients attending Special Medical Board (SMB) examination for their OLDs in the designated Medical College in Kolkata in the past 10 years (2013 to present). Patients who had incomplete data according to the data abstraction form were excluded from the study.
Sample size determination
Cochran’s formula for determining the sample size was applied.[10] The standard normal variate was taken as 1.96 (5% type-I error); the prevalence of severe OLD among industrial workers was 31% in a study by Chakraborti B et al.[11] and the relative error in precision was taken as 20%. Thus, a minimum sample size of 102 was estimated.
Sampling design and methods of data collection
A complete enumeration method was used to study the patients with OLDs who attended the SMB examination from the year 2013 to the present. Thus, a total of 106 patients were studied from the records. After obtaining permission from the competent authority of the Medical Records Department (MRD), the purpose of the study was explained to the staff members of MRD. Relevant sources of information were identified. Relevant data regarding pulmonary morbidity were searched, identified, and extracted in accordance with the data abstraction form and operational definitions agreed upon beforehand, collated, and refined according to the exclusion criteria and any spontaneous need during the data collection period. Important information, found during the data collection period, was archived, and disseminated to corresponding authorities.
Data collection tools and parameters
A pre-designed structured data abstraction form was utilized to collect OLD data through the process of record review. These records were made and maintained at the MR Department during the SMB examination of the patients with OLDs. Various data sources include manual registers, hardcopy files, and computerized databases in the MRD. The data abstraction form encompassed the following domains,
Background variables, such as age, sex, nature of work, type of occupational exposure, duration of exposure, smoking habit, history of past illness, etc.
Another important independent variable was the loss of earning capacity [LOEC (%)], which is measured by the diseased person’s work life expectancy, projected earnings, and living cost.
As the outcome variable, patterns of OLD (occupational diseases as per ESIC hospitals are the diseases which are contracted because of employment and listed under Sections A, B, and C of Schedule III of ESI Act 1948) were taken and it was determined by spirometry findings (carried out during the medical examination). Patterns of pulmonary morbidity (obstructive/non-obstructive) were determined by spirometry data. FEV1/FVC < 0.7 was considered an obstructive type of pulmonary disease and deteriorated lung function.
Institutional Ethical clearance was taken from the ethics committee of the medical college vide letter no. 412 (Dean jfmpc_1981_23X)/IEC (jfmpc_1981_23X)/2014-15/Vol.I dated 29.08.2023. Permission was taken from the competent authority to conduct secondary data analysis from the Department of Medical Records by maintaining confidentiality and anonymity.
Statistical analysis
Data were analyzed using SPSS (IBM Corp., Armonk, N.Y., USA, Version 28). Appropriate descriptive statistics were utilized for denoting the outcome variables as well as the independent variables. Spearman correlation analysis was done. Multiple logistic regression analysis was performed to identify the association between dependent and independent variables.
Results
Patterns of occupational lung disease
Out of a total of 106 study participants, more than half (62.3%) were found to be suffering from the obstructive type of OLD, according to the spirometry findings (FEV1/FVC < 0.7). The rest (40 out of 106) were having non-obstructive types of lung diseases.
In the present study, more than half of the study participants (54.7%) were exposed to organic dust and 35.8% of them were known smokers. History of tuberculosis was present in the case of 23 study participants. The mean duration of occupational exposures among the 106 participants was found to be 30.49 years (Standard Deviation 8.5 years) [Table 1].
Table 1.
Distribution of the study participants according to selected variables (n=106)
| Variables | Number (percentage)/Mean±SD$ (for continuous variable) |
|---|---|
| Type of exposure agents | |
| Organic dust | 58 (54.7) |
| Inorganic dust | 48 (45.3) |
| History of pulmonary tuberculosis | |
| Present | 23 (21.7) |
| Absent | 83 (78.3) |
| Smoking status | |
| Smoker | 38 (35.8) |
| Non-smoker | 68 (64.2) |
| BMI (Kg/m2) | 23.2±3.9 |
| LOEC (%) | 0.44±0.2 |
| Duration of exposure (years) | 30.49±8.5 |
$SD=Standard Deviation
According to the distribution of the study participants as per the history of occupational exposure, it was found that 50% of them were exposed to cotton dust followed by exposure to silica (26%) [Figure 1].
Figure 1.
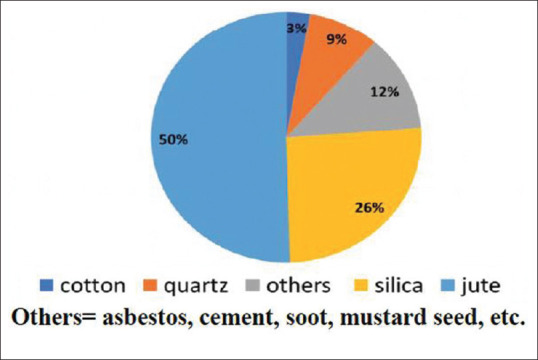
Pie diagram showing the distribution of the study participants according to their occupational agent of exposure (N = 106)
Also, there was a significant negative correlation between the FEV1/FVC ratio and LOEC (Spearman Rho -0.136) [Figure 2].
Figure 2.
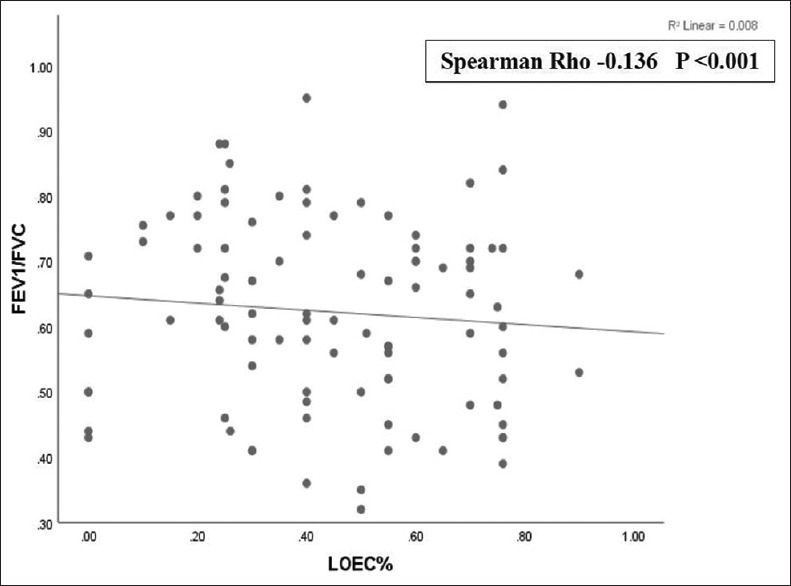
Scatter plot showing correlation between FEV1/FVC ratio and loss of earning capacity (%) of the study participants (N = 106)
Factors associated with the obstructive type of occupational lung disease
In the final multivariable regression model, increased BMI (aOR 1.12, 95% CI 1.01-1.26) and occupational exposure to organic dust (aOR 3.11; 95% CI 1.09-8.77) were found to be significantly associated with the obstructive type of OLD. The model was fit to use as per the insignificant P (>0.05) in the Hosmer–Lemeshow test while 36% (Cox and Snell’s R2) and 47% (Nagelkerke’s R2) of the variance of dependent variables could be explained by this multivariable model [Table 2].
Table 2.
Variables associated with obstructive type of occupational lung disease among the study participants: Multivariable logistic regression (n=106)
| Parameters | Total numbers | Obstructive type of lung disease (n=66) | Adjusted Odd’s Ratio (95% CI) | P # |
|---|---|---|---|---|
| Duration of exposure (in years) | 106 | 66 (62.3%) | 0.98 (0.92-1.03) | 0.39 |
| BMI | 106 | 66 (62.3%) | 1.12 (1.01-1.26) | 0.04 |
| Loss of earning capacity (%) | 106 | 66 (62.3%) | 0.18 (0.02-1.55) | 0.12 |
| Occupational exposure to organic dust (Ref: Exposure to inorganic dust) | 58 | 44 (75.9%) | 3.11 (1.09-8.77) | 0.03 |
| Current smoker (Ref: Non-smoker) | 38 | 25 (65.8%) | 1.11 (0.42-2.9) | 0.84 |
| History of pulmonary tuberculosis (Ref: No history of pulmonary tuberculosis) | 23 | 14 (60.9%) | 0.65 (0.21-1.9) | 0.45 |
Hosmer–Lemeshow model fitting information χ2=5.643, P=0.582. Cox and Snell’s R2=0.36, Nagelkerke’s R2=0.47. CI: Confidence Interval Adjusted OR: Adjusted Odds Ratio. #P<0.05 considered significant
Discussion
The primary objective of the present study was to delineate the pattern of occupational lung disorders among factory workers who are also the beneficiaries of social security schemes like ESI. A heavy burden of lung diseases is seen in countries like India where a large section of the population is not well protected against harmful exposure to various organic and inorganic dust due to their occupational background.
Through secondary data review, this present study included a total of 106 participants who are insured under the ESI scheme and were subjected to the SMB examination for the screening of any OLDs. Among a total of 106 study participants, 62.3% were found to have obstructive type of lung disease. Their mean duration of exposure was 30.49 years and the most common dust to which the participants were exposed was found to be organic materials (jute, cotton). Important factors associated with the presence of an obstructive type of lung disease were increased BMI and organic dust exposure.
A study by He et al., assessing workers’ occupational dust exposure and pulmonary function in China found that increasing age (age >50 years), was associated with abnormal lung function (pneumoconiosis-like changes and decreased FEV1/FVC).[12] Another study conducted by Fan Y et al.[13] in China reported a COPD prevalence of 32.7% among the workers who were exposed to silica and coal dust and this finding was positively associated with the smoking pack-years, and dust exposure duration. The current study showed similar findings. A hospital-based case-control study on occupational exposures and COPD by Govender et al. found that high cumulative organic dust, mineral dust, and fumes were associated with the risk of development of obstructive lung diseases. In that study, smoking and tuberculosis were also strong risk factors with ORs ranging from 5.0 to 5.5 and 7.7 to 8.1, respectively.[14] In the current study, tuberculosis was found to be a significant risk factor in univariate logistic regression (aOR 1.59, 95% CI 1.58–4.52). A study done in the USA by Hunting et al.[15] among sheet metal workers found that the number of pack-years smoked and the duration of exposure were the major risk factors behind the obstructive type of OLDs. Another study done in the United States showed that the highest prevalences of COPD were among industrial workers aged ≥ 65 years (4.6%), and women (3.0%).[16] Rafeemanesh et al.[17] conducted a study on agate grinding workers and the study’s findings showed that the mean duration of exposure of the workers was 13 ± 8.2 years, and it was the major determinant of contracting OLD which is also similar to the findings of the current study. A Swedish cohort study among construction workers showed significantly high mortality rates associated with COPD patients who had a history of exposure to inorganic dust.[18] Nguyen T C. et al.[19] conducted a study in Vietnam which reported that occupational exposure accounted for 66% of the COPD cases. A study done in the stone grinding industry of Gujrat; India showed spirometry findings where 12.8% of the subjects were suffering from an obstructive type of lung disease whereas the present study’s finding is 62.3% for the same category (obstructive type lung disease).[20]
It is evident that compromising health at the workplace is a worldwide phenomenon, and these diseases can be effectively prevented through strategic implementation of the principles of primary health care. The idea to address the impact of work and work environment on health as shared primary healthcare–occupational healthcare responsibility was already included in the WHO 1978 Alma Ata Declaration to bring primary healthcare as close as possible to where people live and work but the reality turns out to be different in most of the countries, especially in resource-poor settings.[21] This present study indicates the burden of OLDs as well as the importance of linking primary healthcare centers and occupational healthcare services.
Although this study has few limitations as the study participants came from a unique population, the generalizability of the study had been compromised. Moreover, as the information obtained was based on secondary data analysis, a lack of accuracy in the data set might be possible.
Conclusion
The ILO Protocol of 2002 to the Occupational Safety and Health Convention describes the systems for recording and notification and highlights the need for the annual publication of national statistics based on occupational accidents and occupational disease notifications.[22] Despite this fact, the situation and extent of OLDs are quite neglected. Evidently, OLD is an understated health issue, especially in the industrial diaspora of developing countries, like India. The findings of this study substantiate the need for healthcare facilities to utilize their resources properly for the advancement of medical surveillance in industries where organic dust is produced. Health education of the stakeholders regarding the consequences of OLDs and the benefits of preventive primary approaches will go a long way in alleviating the burden of disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
General support from the departmental chair and participants of the study.
References
- 1.Cohen RA, Go LHT, Rose CS. Global trends in occupational lung disease. Semin Respir Crit Care Med. 2023;44:317–26. doi: 10.1055/s-0043-1766117. [DOI] [PubMed] [Google Scholar]
- 2.Ratanachina J, Amaral AFS, De Matteis S, Lawin H, Mortimer K, Obaseki DO, et al. Association of respiratory symptoms and lung function with occupation in the multinational Burden of Obstructive Lung Disease (BOLD) study. Eur Respir J. 2023;61:2200469. doi: 10.1183/13993003.00469-2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vlahovich KP, Sood A. A 2019 update on occupational lung diseases: A narrative review. Pulm Ther. 2020;7:75–87. doi: 10.1007/s41030-020-00143-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walia GK, Vellakkal R, Gupta V. Chronic obstructive pulmonary disease and its non-smoking risk factors in India. COPD J Chronic Obstr Pulm Dis. 2016;13:251–61. doi: 10.3109/15412555.2015.1057807. [DOI] [PubMed] [Google Scholar]
- 5.Murgia N, Gambelunghe A. Occupational COPD—The most under-recognized occupational lung disease? Respirology. 2022;27:399–410. doi: 10.1111/resp.14272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Matteis S, Heederik D, Burdorf A, Colosio C, Cullinan P, Henneberger PK, et al. Current and new challenges in occupational lung diseases. Eur Respir Rev. 2017;26:170080. doi: 10.1183/16000617.0080-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cox CW, Rose CS, Lynch DA. State of the art: Imaging of occupational lung disease. Radiology. 2014;270:681–96. doi: 10.1148/radiol.13121415. [DOI] [PubMed] [Google Scholar]
- 8.Ministry of Labour and Employment. Delhi: The Factories Act. 1948. Available from: https://labour.gov.in/sites/default/files/factories_act_1948.pdf .
- 9.Delhi: Extended Sickness Benefit; Ministry of Labour and Employment. Available from: https://www.esic.gov.in/extended-sickness-benefit . [Google Scholar]
- 10.Saha I, Paul B. 3rd ed. Kolkata: Academic Publishers; 2020. Essential of Biostatistics and Research Methodology. [Google Scholar]
- 11.Chakrabarti B, Purkait S, Gun P, Moore VC, Choudhuri S, Zaman M, et al. Chronic airflow limitation in a rural Indian population: Etiology and relationship to body mass index. Int J Chron Obstruct Pulmon Dis. 2011;6:543–9. doi: 10.2147/COPD.S24113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.He W, Jin N, Deng H, Zhao Q, Yuan F, Chen F, et al. Workers’ occupational dust exposure and pulmonary function assessment: Cross-sectional study in China. Int J Environ Res Public Health. 2022;19:11065. doi: 10.3390/ijerph191711065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fan Y, Xu W, Wang Y, Wang Y, Yu S, Ye Q. Association of occupational dust exposure with combined chronic obstructive pulmonary disease and pneumoconiosis: A cross-sectional study in China. BMJ Open. 2020;10:e038874. doi: 10.1136/bmjopen-2020-038874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Govender N, Lalloo UG, Naidoo RN. Occupational exposures and chronic obstructive pulmonary disease: A hospital based case–control study. Thorax. 2011;66:597–601. doi: 10.1136/thx.2010.149468. [DOI] [PubMed] [Google Scholar]
- 15.Hunting KL, Welch LS. Occupational exposure to dust and lung disease among sheet metal workers. Br J Ind Med. 1993;50:432–42. doi: 10.1136/oem.50.5.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Syamlal G, Doney B, Mazurek JM. Chronic obstructive pulmonary disease prevalence among adults who have never smoked, by industry and occupation-United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2019;68:303–7. doi: 10.15585/mmwr.mm6813a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rafeemanesh E, Majdi MR, Ehteshamfar SM, Fahoul MJ, Sadeghian Z. Respiratory diseases in agate grinding workers in Iran. Int J Occup Environ Med. 2014;5:130–6. [PMC free article] [PubMed] [Google Scholar]
- 18.Torén K, Järvholm B. Effect of occupational exposure to vapors, gases, dusts, and fumes on COPD mortality risk among Swedish construction workers: A longitudinal cohort study. Chest. 2014;145:992–7. doi: 10.1378/chest.13-1429. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen TC, Tran HVT, Nguyen TH, Vo DC, Godin I, Michel O. Identification of modifiable risk factors of exacerbations chronic respiratory diseases with airways obstruction, in Vietnam. Int J Environ Res Public Health. 2022;19:11088. doi: 10.3390/ijerph191711088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tiwari RR, Sharma YK. Respiratory health of female stone grinders with free silica dust exposure in Gujarat, India. Int J Occup Environ Health. 2008;14:280–2. doi: 10.1179/oeh.2008.14.4.280. [DOI] [PubMed] [Google Scholar]
- 21.Buijs P, Gunnyeon B, van Weel C. Primary health care: What role for occupational health? Br J Gen Pract. 2012;62:623–4. doi: 10.3399/bjgp12X659141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ales E. ILO Convention 155. Occupational Safety and Health Convention, 1981 (No. 155) International and European Labour Law. 2018 [Google Scholar]


