Abstract
Introduction
Children with retinoblastoma have anesthesia for exams and treatment, but there is little information about how long treatment interventions (laser, cryotherapy, and intravitreal injections) add to routine exams under anesthesia (EUA). This information would be useful for planning operating room schedules, staff schedules, family expectations, and billing.
Methods
A retrospective, single-center, Institutional Review Board (IRB) approved review of anesthesia duration for retinoblastoma children undergoing EUA with laser, cryotherapy, or intravitreal injections performed at MSK between January 2019 and November 2023.
Results
Three hundred eight patients had 2,399 EUAs. The average EUA lasted 24.3 min (range 7–77 min) when no interventions were done. Laser photocoagulation added an average of 18.9 min (range 19–77 min), cryotherapy 26.1 min (range 27–75 min), and intravitreal injection 23.5 min (range 10–71 min) to the basic EUA time. Bilateral laser treatments took 8 min longer than unilateral treatments.
Conclusion
EUAs for children with retinoblastoma can be performed relatively quickly. Interventions such as laser, cryotherapy, or intravitreal injections roughly double the time under anesthesia but in some cases can take much longer (>1 h).
Keywords: Examination under anesthesia, Laser, Injection, Retinoblastoma, Anesthesia, Sevoflurane, Cryotherapy
Introduction
Children diagnosed with retinoblastoma receive anesthesia more than 35 times from diagnosis to completion of treatment [1, 2]. In addition to exams under anesthesia (EUAs), they require anesthesia for diagnostic magnetic resonance imaging (MRI), port placement (and removal), bone marrow biopsy and aspirates, spinal taps, surgery for enucleation and brachytherapy, intra-arterial chemotherapy, prosthesis fabrication and procedures such as laser, cryotherapy, and intravitreal injections [1–3, 6]. Children with bilateral disease have three times as many EUAs and double the anesthesia exposure [1, 2]. Because advanced eyes are often treated with enucleation [2, 3, 6], patients with lower staged disease (who require repeated focal treatments) have considerably more anesthesia [3].
Approximately one third of our EUAs at MSK are combined with diagnostic MRI, laser, cryotherapy, and/or intravitreal injections in addition to fabrication of a prosthesis. There is a paucity of published information about the duration of these procedures. For example, in the multicenter report on “number, frequency, and time interval” of EUAs, there was no mention of the impact of procedures on EUA duration [1]. Similarly, in the recent extensive report on anesthesia duration in 610 procedures in 43 patients, the total anesthesia time was reported for enucleation (152 min), MRI (60 min), port placement/removal (62 min), intra-arterial chemotherapy (274 min), but straightforward EUAs alone were lumped together with EUAs that also had local therapy (45 min), making it impossible to know the time these local therapies added to EUAs [1].
It is important to know the duration for each of these events for patients (and family) teaching, procedure and operating room (OR) scheduling, staffing, billing, and risk assessment. In this study, we report on how much time laser, cryotherapy, or intravitreal injection add to anesthesia time/exposure for children with retinoblastoma.
Methods
This is a single-center, retrospective study from Memorial Sloan Kettering Cancer Center with IRB approval under IRB # 16-1470. We reviewed the anesthesia and medical records (including data from physician billing department) for patients undergoing EUAs for retinoblastoma that were performed in our outpatient retinoblastoma EUA suite between January 2019 and November 2023. Data collected included the age of the child at the time of EUA, sex of the child, race and ethnicity of the child, laterality of disease, whether one or both eyes received treatment on the same day, physician performing the EUA, and day of the week the EUA was performed. Anesthesia documentation at MSKCC includes multiple time points and are documented for the start of anesthesia care, the start of induction, insertion of airway devices, removal of airway devices, emergence of anesthesia, and end of anesthesia care. The authors felt that the most accurate and consistent time point would be insertion and removal of airway devices because it was discrete and not subjective. Below is an actual example of 1 patient’s anesthesia record (shown in Table 1). For this study, we chose the time interval between laryngeal mask airway (LMA) placed and LMA removed (which in this sample case would be 43 min). We excluded EUAs that were the initial (first) visit at our center and exams in which the ocularist fabricated a prosthesis because initial exams are longer and fabrication of a prosthesis also adds to anesthesia time.
Table 1.
Sample of anesthesia log
| Event name | Timestamp |
|---|---|
| Anesthesia start | 10:26:00 |
| Anesthesia induction | 10:26:00 |
| Bypass pre-op | 10:27:00 |
| LMA placed | 10:30:00 |
| Anesthesia ready | 10:30:00 |
| Position changed | 10:32:00 |
| Emergence | 11:10:00 |
| LMA removed | 11:13:00 |
| Stop data collection | 11:13:00 |
| Post-op transfer sign | 11:16:00 |
| Anesthesia stop | 11:16:00 |
| Post-anesthesia Eval Sign | 11:17:00 |
Example of a single patient’s anesthesia record. The time interval between LMA placed and LMA removed was used to calculate anesthesia duration (n = 43 min).
LMA, laryngeal mask airway.
Children who had MRIs (whether they had a focal procedure or not) were also excluded because the MRI increased the duration of anesthesia (i.e., involves transport across floors through the hospital) and confounded our ability to determine the duration of ocular treatments on that day. To determine the mean anesthesia duration, we utilized Isolation Forest linear regression analysis using ordinary least squares to examine the relationship between different treatments and total anesthesia time. Python served as the tool for our analysis. For data manipulation, we used Polars and used the ordinary least squares regression model implemented in statistical models.
Results
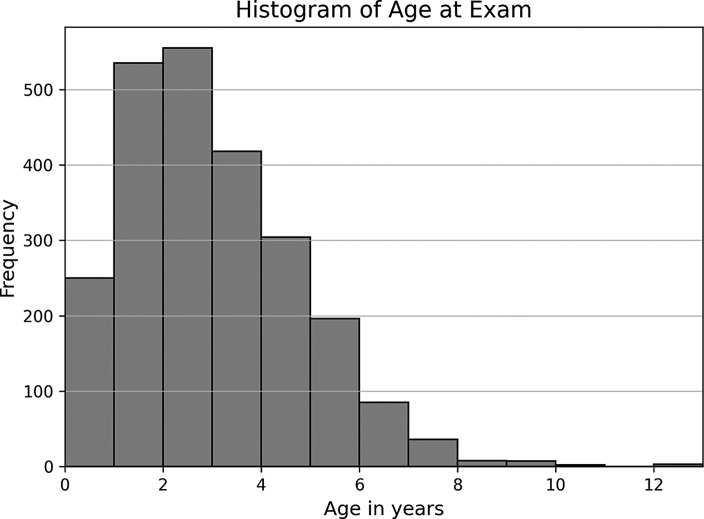
Three hundred eight patients who received 2,399 EUAs fulfilled our inclusion criteria. There were 153 females and 155 males. The mean age of the children at the time of the EUA was 2.52 years (range newborn to 13 years). The histogram of age at exam is shown in Figure 1. The racial and ethnic demographics are presented in Table 2.
Fig. 1.
Distribution of EUAs based on age in years. Number of patients: 308. Number of exams: 2,399. Mean age of EUA: 2.52 years. Range: 0–13 years.
Table 2.
Race and ethnicity
| Category | Number | Percent |
|---|---|---|
| Race | ||
| White | 153 | 49.7 |
| Asian | 82 | 26.6 |
| Other | 35 | 11.4 |
| Black or African American | 23 | 7.5 |
| Unknown | 15 | 4.9 |
| Ethnicity | ||
| Non-Spanish; Non-Hispanic | 228 | 74.3 |
| Hispanic | 40 | 13.0 |
| Unknown | 38 | 12.4 |
| South or Central America | 1 | 0.3 |
Depicts racial and ethnic demographics of the patient cohort.
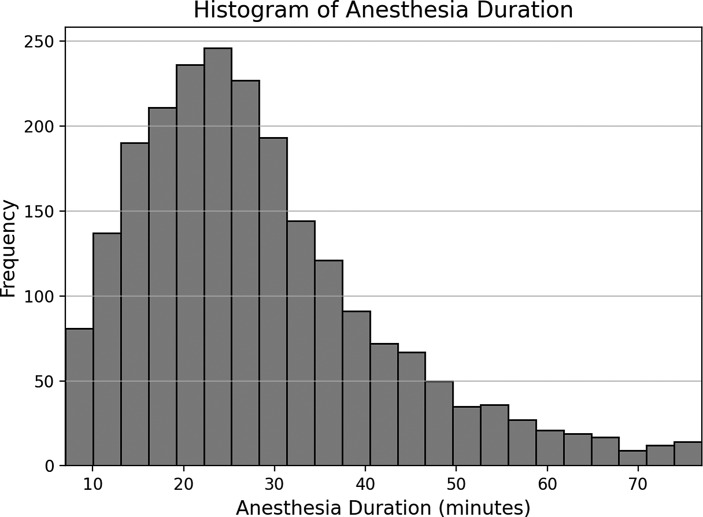
After using Isolation Forest, we calculated the anesthesia duration without any interventions which was 24.3 min (range: 7–77 min, 9.6 SD) and is presented in Figure 2. Two hundred seventy-eight lasers were performed (33 had both eyes treated at the same encounter), 54 cryotherapy procedures, 101 intravitreal injections (2 had both eyes injected on the same visit), and 80 exams for prostheses fabrication.
Fig. 2.
Distribution of EUAs based on duration of anesthesia in minutes. Mean anesthesia duration: 28.5 min. Range: 7–78 min, standard deviations: 13.65.
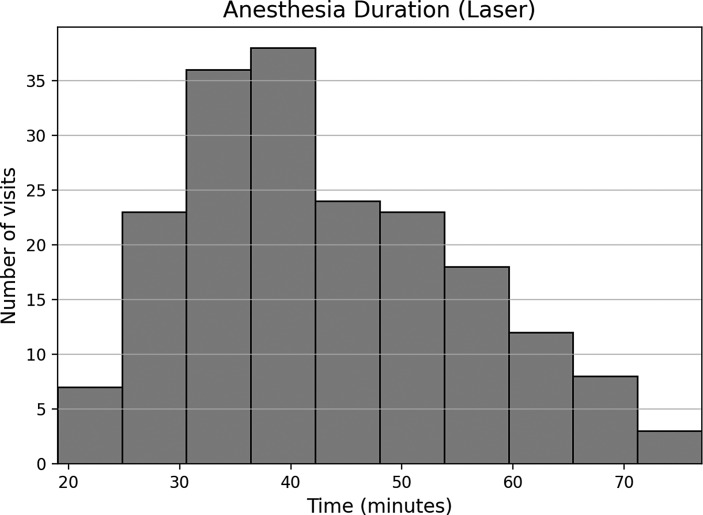
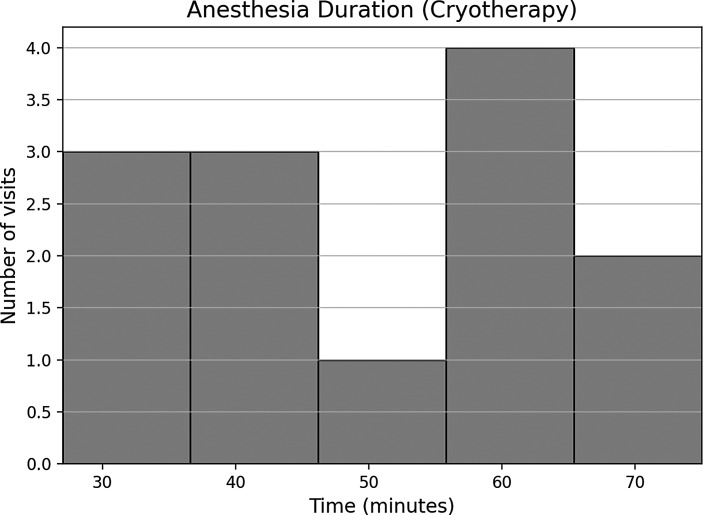
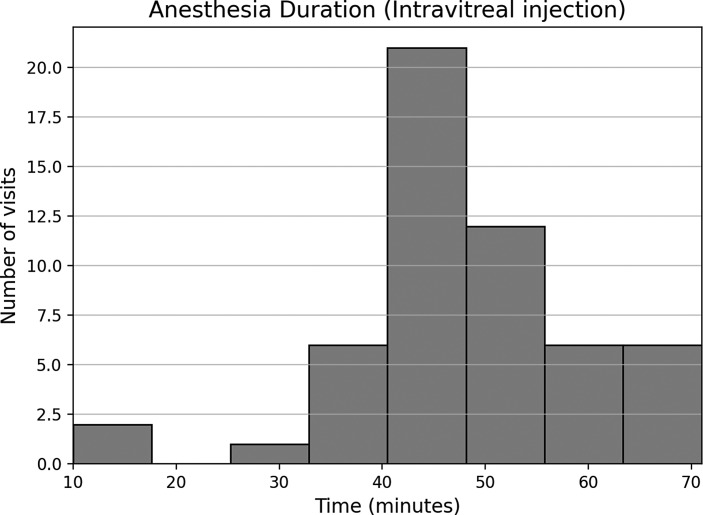
Each additional procedure type was associated with an increase in anesthesia duration. Laser alone increased the anesthesia time by an average of 18.9 min (range 7–77 min/standard deviation: 9.6) (shown in Fig. 3). When only one eye received laser, the time (13.8 min, range 11–75 min) was shorter than if both eyes were treated on the same day (53.8 min, range 27–75 min). The difference in time was significant (p = 0.001). Cryotherapy alone increased anesthesia time by 26.1 min (range 27–75 min/standard deviation: 16.3) (shown in Fig. 4) and intravitreal injection by 23.5 min (range 11–71 min) (shown in Fig. 5).
Fig. 3.
Distribution of EUAs when laser was administered.
Fig. 4.
Distribution of EUAs when cryotherapy was administered.
Fig. 5.
Distribution of EUAs when intravitreal injection was administered.
The model’s R2 value was 0.402, indicating approximately 40.2% of the variance in anesthesia duration can be explained by the independent variables included in the model. The F-statistic was 506.1, with a statistically significant p value of 1.97e−251. There was no significant difference in the anesthesia duration for the two physicians (Dr. Abramson and Dr. Francis), the day of the week on which the procedure was performed, the sex, race, or ethnicity of the patients.
Discussion
Children with retinoblastoma have many anesthesia encounters for diagnosis and treatment. Prior studies have detailed how long EUAs take, how many separate anesthesia exposures children experience and adverse effects [1–6]. For example, one center reported that the average child had more than 35 separate anesthesias and that bilateral patients received more anesthesias than unilateral patients. Patients with lower stage disease also required more anesthesia than advanced cases because advanced cases were usually enucleated while less advanced eyes required repeated combinations of focal treatments. But it is impossible to compare one center with another. At MSK, we have our own space – outside the formal ORs – where a dedicated team of physicians, nurses, advanced practice providers, technicians, and pediatric anesthesiologists routinely and repeatedly perform EUAs. In contrast, most centers do their exams in a true OR. In addition, what is done in an EUA varies from center to center. Our exams frequently include ERGs which are not standard in all other centers. Some centers utilize fluorescein angiography commonly – which we do not. In some centers, residents and fellows participate which extends the anesthesia. In our center, the average EUA takes 24.3 min.
But the definition of how long an EUA takes is also not standard. Many papers do not even define what they mean by “anesthesia time,” while others use the time the anesthesiologist is in charge of the patient to be a surrogate for anesthesia time. That will include the time after anesthesia has stopped but the patient has not been transferred to the recovery area/nurse. As we demonstrated in Table 1, these times are logged in, and since our endpoint was anesthesia exposure, we used “tube in-tube out” as our reference number. In our center, the recovery area is just feet from the examination suite, so transport time is less than 30 s. In other centers, transit time may be minutes and even involve transfer to another floor. We do not routinely use intravenous medications for anesthesia and have published on the safety of this approach [4, 5]. In other centers, intravenous medications are routinely used. This extra step too contributes to different anesthesia exposure times as inserting an IV in a baby can sometimes prolong anesthesia by more than 10 min.
We have performed more than 20,000 EUAs in our dedicated suite for retinoblastoma children since the inception of the Ophthalmic Oncology Service at MSK in 2004. In 2004, we were using nitrous oxide and halothane via mask anesthesia, but we cannot report on anesthesia times during that time period because those records were not computerized and are no longer available. For more than 16 years, we have used only sevoflurane. In the early days, that was delivered by mask but for more than 15 years by LMA, again without IVs. Computerized records recording precise anesthesia time (as illustrated above) have been available since 2019 and that is the reason this series begins in 2019.
The reader could ask why these three interventions took so long. For example, it may be surprising to note that an intravitreal injection took 25 min. Most of our intravitreal injections are planned in advance, and the drug is in the room when the EUA starts. However, we exit the room during the EUA to discuss the procedure with the family, and at times, the discussion is prolonged. But in some cases, we only recognize the need for an intravitreal injection during the EUA. In that case, orders need to be placed, consent needs to be signed, we meet with the family – at that point, we contact our pharmacy team, and the drug is prepared and delivered and verified at the bedside. That time varies but is often 20 or more minutes. Because this study was retrospective, we are unable to precisely document that time.
Similarly, it seems surprising that a laser to one eye took on average about 19 min and at times over an hour. In our center, the decision to use laser and/or cryotherapy is made in real time during the examination under anesthesia. The equipment for the procedures is always in the EUA suite, but before doing the procedure, the attending physician leaves the room and meets with the family. The discussion about the procedure, alternatives, risks, and complications takes time and that time varies from family to family and even from visit to visit. For some families, that discussion is a minute, but for others, it can be half an hour. It was of interest that lasering both eyes increased the anesthesia time by only 8 min. This suggests that the actual laser time is only 8 min for the first eye, and the other 11 min are for other reasons. This is useful information because if we and other centers wish to further decrease anesthesia exposure, attentions need to be directed at the surrounding reasons for the longer anesthesia – not just the actual lasering time.
In addition, because well-dilated pupils are mandatory for most lasers and cryotherapy, some children require installation of additional dilating drops before the procedure is performed and that too prolongs anesthesia exposure. Due to this study being retrospective, we do not have a precise record of the duration of these discussions or the additional time needed to adequately dilate the pupils, but the histograms emphasize the variation in time it took. We included the time discussing risks, benefits, and alternatives as procedure time because in the real world, those discussions would not have been done if the procedure had not been done.
There may be other reasons for some of the prolonged anesthesia times, but these were difficult to quantify because of the retrospective nature of our study. For example, many of our families require interpreters. In some cases, the interpreter is with the family for the entire encounter, but at other times, they need to be called to come to our area. In other cases, interpreter services need to be done through the phone (or video), and this too adds to anesthesia time. For patients who receive laser or cryotherapy, IVs are started and medication given (pain medication) – that too can take time.
The duration of anesthesia in patients who received laser, cryotherapy, or intravitreal injection did not vary by sex of the patient, race, ethnicity, or by the physician who performed the EUA (Dr. Abramson or Dr. Francis). We perform EUAs two or three times a week and, on 1 day, host students and trainees. That too did not influence the duration of anesthesia. Patients who had fabrication of the prosthesis by our prosthodontists and those who had MRIs on the same day did have longer anesthesias of course, and initial exams were longer than follow-up exams.
Conclusion
Retinoblastoma children who have EUAs have the procedure extended by another 18.9 min if laser is done, 26.1 min if cryotherapy is done, and 23.5 min if intravitreal injection is performed, but in some cases, the procedures increase anesthesia time by much longer (almost an hour). Lasering both eyes took 8 min longer than lasering only one eye which suggests that most of the time attributed to these treatments was not doing the actual treatment but issues of getting consent, discussing the procedure/options/risks with the family, further dilating the pupils, getting interpreters, ordering chemotherapy (and verifying drug at the beside), or even putting in IVs for pain medicines. A prospective study might be able to quantify the relative contributions of these factors. This information is useful for planning OR usage, staff scheduling, billing, and educating the family about how long each procedure will add to the standard EUA.
Statement of Ethics
This study protocol was reviewed and approved by the Institutional Review Board of Memorial Sloan Kettering Cancer Center, approval No. 16-1470. A waiver of consent was obtained for this retrospective study. This study has been granted an exemption from requiring written informed consent from participants by the Institutional Review Board of Memorial Sloan Kettering Cancer Center.
Conflict of Interest Statement
D.H.A., J.G., C.B., T.L., E.G., A.B., A.F., M.A.R., R.D.R., and J.H.F. have no conflicts of interest to declare.
Funding Sources
This work was supported in part by the Fund for Ophthalmic Knowledge, Inc. and the National Institutes of Health Cancer Center Support Grant (P30 CA008748). The funders had no role in the design, data collection, data analysis, and reporting of this study.
Author Contributions
Substantial contributions to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; drafting the work; reviewing it critically for important intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: D.H.A., J.G., C.B., T.L., E.G., A.B., A.F., M.A.R., R.D.R., and J.H.F.
Funding Statement
This work was supported in part by the Fund for Ophthalmic Knowledge, Inc. and the National Institutes of Health Cancer Center Support Grant (P30 CA008748). The funders had no role in the design, data collection, data analysis, and reporting of this study.
Data Availability Statement
Data are available upon request. All data relevant to the study are included in the article. Further inquiries can be directed to the corresponding author.
References
- 1. McInnis-Smith K, Chen K, Klanderman M, Abruzzo T, Ramsaubramanian A. Quality and duration of exposure to general anesthesia for pediatric patients with retinoblastoma. J AAPOS. 2022;26(6):313.e1–e5. [DOI] [PubMed] [Google Scholar]
- 2. Fabian ID, Shah V, Kapelushnik N, Naeem Z, Onadim Z, Price EA, et al. Number, frequency and time interval of examinations under anesthesia in bilateral retinoblastoma. Graefes Arch Clin Exp Ophthalmol. 2020;258(4):879–86. [DOI] [PubMed] [Google Scholar]
- 3. Fabian ID, Shah V, Kapelushnik N, Naeem Z, Onadim Z, Price E, et al. Examinations under anaesthesia as a measure of disease burden in unilateral retinoblastoma: the London experience. Br J Ophthalmol. 2020;104(1):17–22. [DOI] [PubMed] [Google Scholar]
- 4. Vigoda MM, Latiff A, Murray TG, Tutiven JL, Berrocal AM, Gayer S. Can children undergoing ophthalmologic examinations under anesthesia be safely anesthetized without using an IV line? Clin Ophthalmol. 2011;5:503–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hung CW, Licina L, Abramson DH, Arslan-Carlon V. Anesthetic complications during general anesthesia without intravenous access in pediatric ophthalmologic clinic: assessment of 5216 cases. Minerv Anestesiol. 2017;83(7):712–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fabian ID, Stacey AW, Johnson KC, Chowdhury T, Duncan C, Reddy MA, et al. Primary enucleation for group D retinoblastoma in the era of systemic and targeted chemotherapy: the price of retaining an eye. Br J Ophthal. 2018;102(2):265–71. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon request. All data relevant to the study are included in the article. Further inquiries can be directed to the corresponding author.