Video
Background
Hepatic artery pseudoaneurysm is a rare and potentially fatal condition that may develop following hepatobiliary procedures.1, 2, 3 It is a serious adverse event of liver transplantation with an incidence of 2% to 4% and a mortality rate of 50% to 75%.4, 5, 6 Clinical presentation may include rupture into the bile ducts resulting in hemobilia, which presents as Quincke’s triad of right upper quadrant abdominal pain, jaundice, and upper GI bleeding.7 We report a case of massive hemobilia detected during ERCP that was found to be caused by a hepatic artery pseudoaneurysm fistulizing with the common bile duct after liver transplantation.
Case
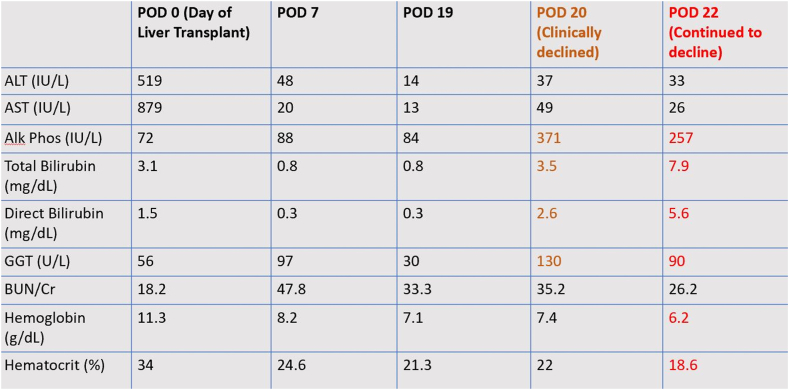
A 66-year-old male with decompensated alcoholic cirrhosis underwent an uneventful orthotopic liver transplantation with near normalization of liver enzymes by postoperative day (POD) 7. On POD 20, the patient developed abdominal pain and melena, with new hyperbilirubinemia of total bilirubin 3.5 mg/dL and direct bilirubin 2.6 mg/dL (Fig. 1). MRCP revealed thickening of the biliary anastomosis consistent with postsurgical edema, and no biliary obstruction, ductal dilatation, or pseudoaneurysm was seen. On POD 22, total bilirubin and direct bilirubin continued to rise to 7.9 mg/dL and 5.6 mg/dL, respectively, whereas hemoglobin dropped 1 g/dL to below 7 g/dL, now newly requiring blood transfusion. The patient remained hemodynamically stable and underwent an urgent ERCP for suspected biliary stenosis as the primary cause for the hyperbilirubinemia, given the higher likelihood of this to occur particularly in the posttransplant population. The patient’s worsening anemia was unexplained but was not thought to be relevant to the suspected biliary stenosis; therefore, concern for hemobilia at this time was low.
Figure 1.
Liver enzyme trends.
Procedure and outcome
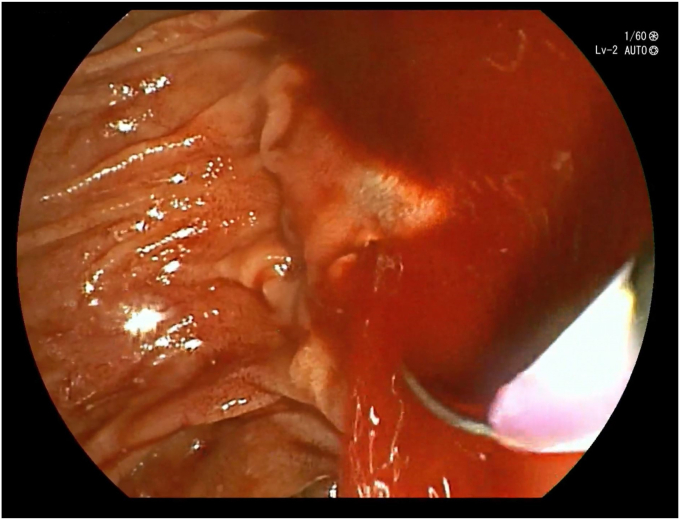
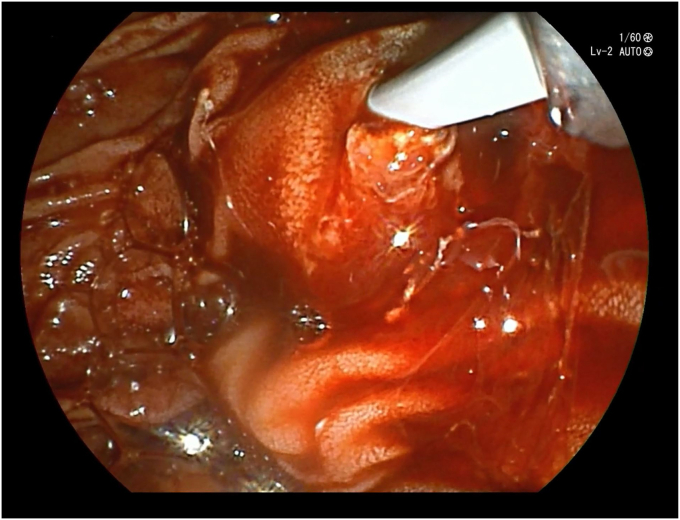
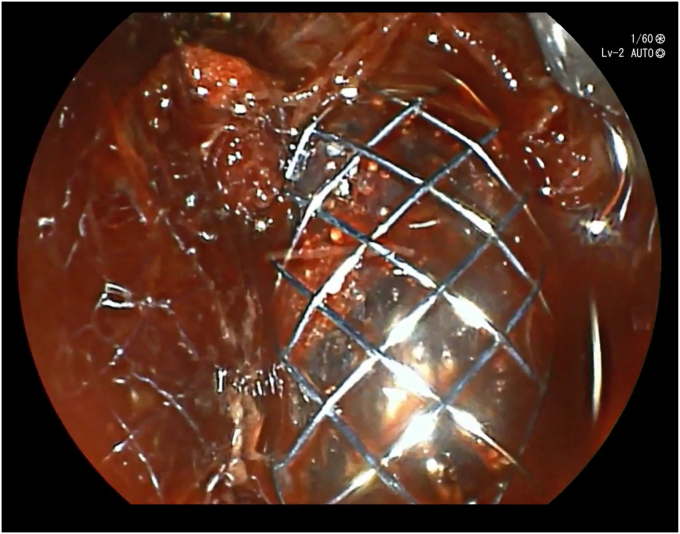
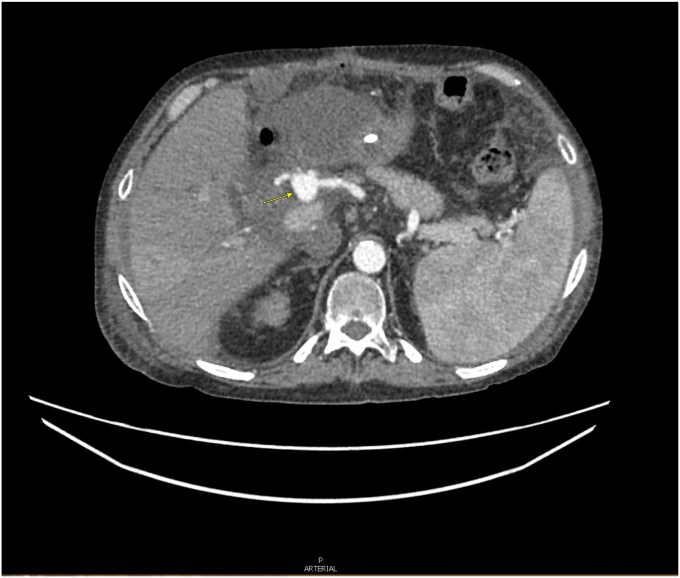
During the ERCP (Video 1, available online at www.videogie.org), initial inspection revealed minimal hematin already seeping out from the ampulla, but following cannulation, there was brisk and massive hemorrhage that may have been triggered by clot dislodgement (Fig. 2). The etiology of the bleeding was unclear but was suspected to be from surgical adverse events from the liver transplant surgery. The patient became hypotensive and required vasopressors and blood transfusions. The transplant surgery, interventional radiology, and intensive care unit teams were notified. The decision was made to tamponade the bleeding area with an inflatable balloon, which slowed down the bleeding (Fig. 3). However, the bleeding resumed immediately upon balloon removal. The origin site of the bleeding was not visualized because of the massive hemorrhage; therefore, a 10-mm × 8-cm fully covered self-expandable metal stent (FCSEMS) was deployed to cover most of the common bile duct with the goal of large area pressure hemostasis. The FCSEMS placement allowed for stabilization of hemodynamics and prompt discontinuation of vasopressor support (Fig. 4). The ERCP findings were discussed with the multidisciplinary team, and a quick literature search suggested hepatic artery pseudoaneurysm as a cause. An abdominal CT angiography scan obtained immediately after revealed a hepatic artery pseudoaneurysm (Fig. 5). Upon further discussion with the multidisciplinary team, it was decided that the patient would undergo surgical repair instead of more common endovascular or percutaneous interventions due to the patient’s complex anatomical changes from the recent transplant surgery.
Figure 2.
Brisk hemorrhage following cannulation of the major papilla.
Figure 3.
Bleeding temporarily slowed down by balloon tamponade.
Figure 4.
Successful 10-mm × 8-cm fully covered self-expandable metal stent placement into the common bile duct.
Figure 5.
Abdominal CT angiography scan showing the hepatic artery pseudoaneurysm.
Exploratory laparotomy revealed a fistula between the common bile duct and extrahepatic pseudoaneurysm of the common hepatic artery. The arteriobiliary fistula was corrected and the pseudoaneurysm was resected. Revascularization with vessel re-anastomoses and biliary reconstruction was achieved. The patient did well postoperatively and was discharged in stable condition 5 weeks later with normal liver function on laboratory findings.
Conclusion
Given the rarity of hepatic artery pseudoaneurysms, there are no clear guidelines on their management.4,5 Once significant hemobilia is identified on endoscopy, there are no endoscopic procedures to achieve therapeutic hemostasis. Endovascular arterial embolization with coil or liquid vehicle is a primary method of treatment.7 The dual vascular supply of the liver allows for embolization of the hepatic artery and its branches without significant concern for ischemia.8 Surgical intervention is reserved for failed endovascular approaches, or for cases with altered anatomy such as in transplant or tumor invasion.
The anatomic changes from the liver transplant likely led to pseudoaneurysm formation in our patient, making surgical intervention the treatment of choice. Our case demonstrates that FCSEMS placement may be an important endoscopic technique to consider in managing pseudoaneurysms, particularly with bleeding localized to the extrahepatic bile duct. The efficacy of FCSEMS placement in intrahepatic bile duct bleeding remains unclear, as we do not know what would have happened if the bleeding source was from within the liver. Even though we were unable to obtain a cholangiogram or visualize the pseudoaneurysm endoscopically, FCSEMS placement allowed for large area compression within the extrahepatic bile duct to temporarily tamponade the bleed while providing for time to coordinate definitive treatment plans. It is likely that without the FCSEMS placement, the patient may have expired before anything else could have been done.
Disclosure
The authors disclosed no financial relationships relevant to this publication.
Supplementary data
Hemobilia due to hepatic artery pseudoaneurysm fistulizing with the common bile duct following liver transplantation.
References
- 1.Thomas W.E., May R.E. Hepatic artery aneurysm following cholecystectomy. Postgraduate Med J. 1981;57:393–395. doi: 10.1136/pgmj.57.668.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ribeiro A., Williams H., May G., et al. Hemobilia due to hepatic artery pseudoaneurysm thirteen months after laparoscopic cholecystectomy. J Clin Gastroenterol. 1998;26:50–53. doi: 10.1097/00004836-199801000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Roche-Nagle G., Macenaeney H.P. Pseudo-aneurysm of the hepatic artery after laparoscopic cholecystectomy: a case report. J Minimal Access Surg. 2006;2:73–75. doi: 10.4103/0972-9941.26652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reznichenko A.A., Bondoc A., Paterno F., et al. Hepatic artery pseudoaneurysm after liver transplantation. J Gastrointest Surg. 2016;20:1405–1406. doi: 10.1007/s11605-016-3097-z. [DOI] [PubMed] [Google Scholar]
- 5.Craig E.V., Matthew T.H. Complications of liver transplant. Abdom Radiol. 2021;46:43–67. doi: 10.1007/s00261-019-02340-5. [DOI] [PubMed] [Google Scholar]
- 6.St Michel D.P., Goussous N., Orr N.L., et al. Hepatic artery pseudoaneurysm in the liver transplant recipient: a case series. Case Rep Transplant. 2019;2019 doi: 10.1155/2019/9108903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berry R., Han J.Y., Kardashian A.A., et al. Hemobilia: etiology, diagnosis, and treatment. Liver Res. 2018;2:200–208. doi: 10.1016/j.livres.2018.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cardona J.D., Rivero O.M., Pinto R., et al. Endovascular and endoscopic treatment of hemobilia: a report of two cases. Cureus. 2022;14 doi: 10.7759/cureus.28383. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Hemobilia due to hepatic artery pseudoaneurysm fistulizing with the common bile duct following liver transplantation.