Abstract
Background and Aims
The impact of inflammatory bowel disease [IBD] on work productivity remains unclear. In this systematic review and meta-analysis, we quantify work-related outcomes and employment data among persons with IBD.
Methods
A systematic literature search was conducted in MEDLINE, EMBASE, the Cochrane library, Scopus, ProQuest, and clinicaltrials.gov from inception to February 2023, to identify studies on work productivity in persons with IBD aged > 18 years. Work productivity was defined primarily by the Work Productivity and Activity Impairment [WPAI] questionnaire which includes absenteeism, presenteeism, overall work impairment, and non-work activity impairment. In addition, we included data on employment, sick leaves, disability pensions, and indirect costs due to productivity loss. Pooled effect analysis was conducted using a random-effects model for pooled estimates of continuous and proportional data with 95% confidence intervals.
Results
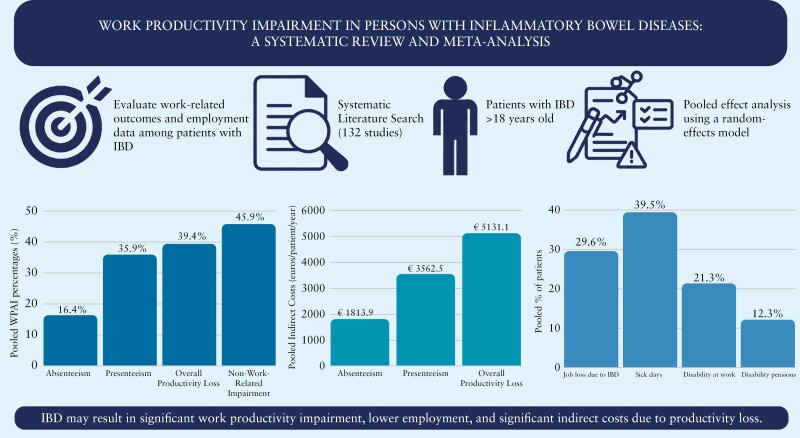
Among all patients with IBD, the pooled estimates were 16.4% for absenteeism, 35.9% for presenteeism, 39.4% for overall work impairment, and 46.0% for non-work activity impairment. Indirect costs from overall work impairment were 5131.09 euros/patient/year. Only two-thirds of IBD patients were employed, and one in three lost their jobs due to IBD. Among those employed, 39.5% report sick days, 21.3% report work disability, and 12.3% receive disability pensions. Most studies demonstrate clinically meaningful improvements in work productivity with medical and/or surgical therapies.
Conclusion
Persons with IBD experience significant work impairment and associated indirect costs. This highlights the need for appropriate workplace accommodations and timely medical therapy to alleviate the burden of disease and improve work outcomes.
Keywords: Inflammatory bowel disease, work productivity, WPAI
Graphical Abstract
Graphical Abstract.
1. Introduction
Inflammatory bowel diseases [IBD], which include Crohn’s disease [CD] and ulcerative colitis [UC], are chronic disorders that affect approximately 6.8 million people globally.1 IBD is associated with debilitating symptoms including diarrhoea, abdominal pain, and significant fatigue. Individuals experiencing severe disease activity and flares may also require hospitalisation and surgical intervention.2 Therefore, the natural history of the disease, often recurring and fluctuating, coupled with these burdensome symptoms, can result in significant impairment in individuals’ quality of life [QOL] and functioning in society.
The average age of disease onset is between 31–34 years, coinciding with peak years of professional life.3 Compared with the general population, individuals with IBD have higher rates of unemployment, sick leave, and work disability.4 Though the effects of disability in IBD have been increasingly documented, it is only recently that standardised measures of impairment have been applied in this population. One such measure is the Work Productivity and Activity Impairment score [WPAI], which measures work time missed and work and activity impairment due to a specified health problem during the past 7 days.5 The WPAI has been validated in both CD and UC, among other disease states.6
Despite the development of this tool, there remains a significant variability in data and outcome definitions regarding work impairment in persons with IBD. This has limited prior attempts to conduct meta-analyses to accurately quantify the extent of work impairment. In addition, the indirect costs associated with productivity losses have yet to be quantified, or reported, systematically. As such, it becomes challenging to clearly describe the socioeconomic burden of the disease and its impact on patients in their workplaces. This research gap is crucial to better understand the psychosocial aspects of the disease and to advocate for workplace accommodations that may mitigate the work disability experienced by patients with IBD. In this systematic review and meta-analysis, we aim to closely quantify the impact of IBD on work productivity and the indirect costs, using the standardised WPAI questionnaire, and to review medical and surgical interventions that may affect work-related outcomes in IBD.
2. Materials and Methods
This systematic review and meta-analysis aimed to determine the impact of IBD on work productivity. The study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [PRISMA] statement guidelines, and a priori registered on PROSPERO [ID: CRD42023399459].
2.1. Search strategy and eligibility criteria
With the assistance of a trained medical librarian, we conducted a literature search on MEDLINE, EMBASE, and Cochrane electronic databases. In addition, we searched Scopus, ProQuest, and clinicaltrials.gov for abstracts, conference presentations, and other grey literature. These databases were searched from inception to February 2023 [full search strategy included as Supplementary Material]. To complement our database search, we also screened the reference lists of the included studies and review articles to identify any additional eligible studies.
We included full texts and abstracts of observational studies and clinical trials that reported work productivity outcomes and indirect costs in adult IBD patients [18 years and older]. Exclusion criteria included non-IBD studies, paediatric populations [<18 years], studies with no work-related outcomes, narrative and systematic review articles, articles with no full text available, non-English studies, and uncompleted studies. Studies with duplicate patient populations were excluded after including the most recent study on that population. Studies were also excluded if employment data was not a study outcome. In addition, we excluded studies where work impairment was not directly related to IBD, but rather solely a consequence of inconveniences with medical treatment [eg, biologic infusions], surgical interventions [eg, post-colectomy], caregiver burnout, or layoffs during the COVID-19 pandemic. Otherwise, we included these studies if they reported IBD-specific work productivity outcomes. Last, we excluded studies that reported data as comparisons between groups or as ‘mean changes’ before and after an intervention with no absolute values. Where there were missing data, we attempted to contact the corresponding authors of the primary studies.
2.2. Study selection
Four reviewers [MY, NJ, TH, and CM] independently performed the initial title and abstract screen and selected abstracts that met inclusion criteria for full text review. The reviewers then independently reviewed the full length manuscripts [or abstracts] and included eligible studies in the final review. Any discrepancies were resolved through consensus agreement.
2.3. Outcome definitions
The primary outcome of this study was to determine the impact of IBD on work productivity outcomes defined primarily by WPAI. The questionnaire generates percentages [0–100%] relating to the past 7 days of work, quantifying absenteeism [percentage of time missed from work], presenteeism [percentage of impaired functionality at work despite physical presence], overall work impairment [percentage of absenteeism + presenteeism], and non-work activity impairment, with higher scores indicating greater impairment.5 Secondary outcomes included other non-WPAI work-related outcomes as aggregated by each study, including sick leaves, number of working days missed, work disability due to IBD, disability pensions, lost jobs due to IBD, and WPAI-related indirect costs. These indirect costs were abstracted directly from studies and reported exactly as calculated in each individual study.
2.4. Data collection
The four reviewers independently completed data extraction using a standardised data collection sheet that was designed a priori. Data collected included: [a] study characteristics such as primary author, year of publication, nature of study [full text vs abstract], study design [prospective vs cross-sectional, and observational vs interventional]; [b] sample size of patients included with IBD [UC and CD]; [c] patient characteristics including age, sex, disease severity and activity; [d] employment data; [e] work-related outcomes defined primarily by WPAI and other non-WPAI outcomes as described above.
2.5. Data analysis
Meta-analysis using the continuous random-effects method was conducted for continuous outcomes to calculate the pooled mean effect sizes with 95% confidence intervals [CI] for WPAI outcomes and indirect costs. For studies that only reported data as means with CI, standard deviation [SD] was estimated using the formula SD= √ N x [upper–lower limit of CI]/3.92, where N is the sample size for which the data are reported.7,8 Binary random-effects method was used to calculate pooled incidence rates with 95% CIs for proportional outcomes. For interventional studies with multiple data points, we used the baseline employment and WPAI data [ie, pre-intervention data] for our meta-analysis. We then conducted subgroup analyses by IBD subtype [CD vs UC], and used mean differences and odds ratios [ORs] to compare patients with moderate/severe IBD vs those in remission or with mild IBD as defined by each individual study. Forest plots were generated for these comparisons where applicable. A pooled analysis was not conducted for interventional studies, given the significant variability in the interventions studied and the differences in data reporting between studies [absolute values vs mean changes].
To explore sources of heterogeneity, sensitivity analyses according to study type [cohort vs cross-sectional] and manuscript type [full length vs abstract] were performed. All summary estimates were determined by DerSimonian-Laird random-effects models. Between-study heterogeneity was assessed by the I2 statistic. An I2 > 50% suggested substantial heterogeneity.9 All statistical analyses were performed using OpenMeta version 10.12.10
2.6. Study quality assessment
Risk of bias for full text cross-sectional studies was assessed using the Appraisal tool for Cross-Sectional Studies [AXIS] tool.13 Full-text cohort and case-control studies were assessed using the National Institutes of Health [NIH] tool.11 Last, the Cochrane risk-of-bias tool [ROB] was used to assess full-text randomised control trials [RCTs].12
3. Results
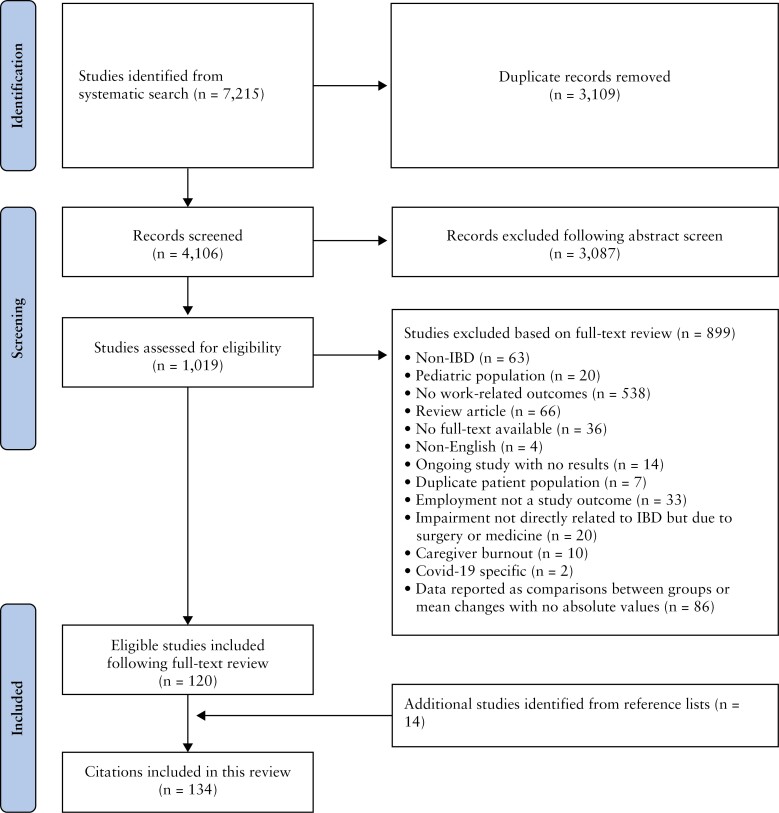
Four thousand one hundred and six references were eligible for title and abstract screening [Figure 1]; 1019 studies were reviewed and 899 were excluded, leaving 120 studies eligible for inclusion. After reviewing the reference lists of included studies, 14 additional studies were included, resulting in 134 studies included in this review. This study included 96 full text articles and 38 abstracts. There were 105 observational studies [Table 1]13–117 and 29 interventional studies.118–146 The study characteristics and outcomes of these observational and interventional studies are included in Supplementary Tables S1 and S2, respectively.
Figure 1.
PRISMA flowchart.
Table 1.
Observational studies—baseline characteristics.
| Study | Country of study | Sample size | %Male, female | Mean age ± SD | Employment [%] | WPAI reported? | Indirect costs reported? | Miscellaneous outcomes reported? |
|---|---|---|---|---|---|---|---|---|
| Ding 202213 | USA | Total = 563 [CD = 281, UC = 282] | CD—M:52.3, F:47.7 UC—M:55.7, F:44.3 |
CD: 40.0 ± 12.1 UC: 40.5 ± 12.1 |
- | ✓ | ✓ | - |
| Decker 202214 | Czech Republic | Total = 161 [CD = 102, UC = 59] | M:41.6, F:58.4 | 41.2 | - | ✓ | ✓ | ✓ |
| Holko 202215 | Belgium, Bulgaria, Cyprus, Czech Republic, Denmark, Greece, Hungary, Italy, Poland, Portugal, Romania, Spain | Total = 3687 [CD = 1930, UC = 1693, IC = 63] | M:34, F:66 | 43.03 ± 13.76 | 67 | ✓ | ✓ | ✓ |
| Varma 202216 | USA | CD = 403 | M:26.5, F:73.5 | 49.5 ± 15.9 | 64.3 | - | - | ✓ |
| Paulides 202217 | The Netherlands | Total = 229 [CD = 155, UC = 66, IC = 8] | M:31, F:69 | 38.0 ± 17 | 66.8 | ✓ | - | ✓ |
| Viazis 202218 | Greece | UC = 95 | M:47, F:53 | 42 ± 13.69 | - | - | - | - |
| Paulides 202019 | New Zealand | Total = 123 [CD = 83, UC = 40] | M:41, F:59 | 42.5 ± 13.5 | 100 | - | - | ✓ |
| Topal 202020 | Turkey | Total = 180 [CD = 115, UC = 86] | M:57.5, F:42.5 | - | - | - | - | ✓ |
| Yamabe 201921 | Japan | Total = 441 | M:61.7, F:38.3 | 48.2 ± 14.8 | 66.2 | ✓ | - | ✓ |
| Kawalec 201822 | Poland | UC = 147 | M:46.94, F:53.06 | 39.0 ± 13.4 | 64.6 | ✓ | ✓ | ✓ |
| Sciberras 202223 | 8 European centres [not specified] + Israel | Total = 585 [CD = 363, UC = 222] | M:53, F:47 | - | Total [n = 585]: 74.5 UC [n = 222] = 79.9 CD [n = 363] = 71.3 |
- | - | ✓ |
| vanGennep 202124 | The Netherlands | Total = 510 [CD = 268, UC = 242] | M:41, F:59 | - | - | ✓ | ✓ | ✓ |
| Ruiz-Casas 202125 | Denmark, Norway, Poland, Romania, and Turkey | Total: 299 [Remission/mild = 1131, Moderate/severe = 1835] | Total—M:55, F:45 Remission/mild—M:53, F:47 Moderate/severe—M:56, F:44 |
Total: 47 ± 15 Remission/mild: 48 ± 15 Moderate/severe: 46 ± 15 |
- | ✓ | ✓ | - |
| Rankala 202126 | Finland | Total = 320 [CD = 102, UC = 218] | M:50.6, F:49.4 | 46.2 | 100 | - | ✓ | - |
| Khalili 202027 | Sweden | Prevalent: 29,879 [CD = 10117, UC = 19762] Incident: 12,687 [CD = 4028, UC = 8659] |
Prevalent—M:51.4, F:48.6 Prevalent—M:48.9, F:51.1 |
Prevalent: 50.1 ± 17.6 Incident: 45.6 ± 19.1 |
Prevalent CD: 80 Prevalent UC: 86 |
- | ✓ | ✓ |
| Yu 202128 | China | Total = 3000 [CD = 1922, UC = 973] | M:59.6, F:40.4 | 34 | 54.9 | - | - | ✓ |
| deSaBritoFroes 202129 | Brazil | Total = 413 | M:45, F:55 | 39.4 | - | - | - | ✓ |
| Walter 202030 | Austria | Total = 510 [CD = 345, UC = 165] | M:26.3, F:73.3 | 40.4 ± 13.1 | 63.9 | ✓ | ✓ | ✓ |
| Manceur 202031 | USA | Total = 6715 | M:45.7, F:54.3 | 44.8 | - | - | ✓ | - |
| Moon 202032 | South Korea | UC = 355 | M:59.2, F:40.8 | - | 48.6 | ✓ | - | - |
| Chao 201933 | Canada | Total = 207 [CD = 144, UC = 63] | M:42.5, F:57.5 | - | 79.2 | ✓ | - | ✓ |
| Parra 201934 | Brazil | Total = 407 [CD = 264, UC = 143] | CD—M:45.8, F:54.2 UC—M:43.4, F:56.6 |
CD: 42.9 ± 13.0 UC: 45.9 ± 13.8 |
CD: 44.3 UC: 53 |
✓ | - | ✓ |
| Christiansen 201935 | Denmark | Total = 185 [CD = 78, UC = 107] | CD—M:55.1, F:44.9 UC—M:43.9, F:56.1 |
- | CD: 73.3 UC: 74 |
✓ | - | ✓ |
| Pillai 201936 | Switzerland | Total = 2365 [CD = 1353, UC = 1012] | CD—M:46, F:54 UC—M:52, F:48 |
CD: 41 ± 15 UC: 43 ± 14 |
73 | - | ✓ | ✓ |
| LeBerre 201937 | France | Total = 1410 [CD = 874, UC = 493] | M:24, F:76 | 38 ± 10.1 | 80 | ✓ | - | ✓ |
| Gonczi 201938 | Canada | Total = 525 [CD = 374, UC = 151] | M:41.7, F: 52.9 | - | 73 | ✓ | - | - |
| Everhov 201939 | Sweden | Total = 2015 [CD = 1920, UC = 6, IC = 89] | M:50, F:50 | - | - | - | - | ✓ |
| Everhov 201840 | Sweden | CD = 20638 | M:48, F:52 | - | - | - | - | ✓ |
| Spekhorst 201741 | The Netherlands | Total = 2794 [CD = 1740, UC = 1054] | CD—M:37, F:63 UC—M:47, F:53 |
- | CD: 56 UC: 63 |
- | - | ✓ |
| Kamat 201742 | India | Total = 84 [CD = 25, UC = 59] | CD—M:80, F:20 UC—M:71, F:29 |
CD: 21 ± 5.1 UC: 37.3 ± 4.4 |
CD: 72 UC: 78 |
- | ✓ | ✓ |
| Williet 201743 | France | Total = 1185 [CD = 721, UC = 462] | Total—M:38.5, F:61.5 CD—M:37.9, F:62.1 UC—M:39.7, F:60.3 |
- | Total: 59.4 CD: 60.5 UC: 57.9 |
✓ | - | ✓ |
| Holko 201644 | Poland | CD = 200 | M:42.2, F:57.8 | 31.80 ± 10.41 | Total: 60 Active: 55.2 Remission: 64.5 |
- | ✓ | ✓ |
| DeBoer 201645 | The Netherlands | Total = 202 [CD = 128, UC = 74] | M:43, F:57 | 41 ± 12 | 61 | - | ||
| Aldeguer 201646 | Spain | UC = 285 | M:51.2, F:49.8 | 44.5 ± 15.6 | 67 | - | ✓ | ✓ |
| Vester-Andersen 201547 | Denmark | Total = 379 [CD = 155, UC = 224] | CD—M:44.5, F:55.5 UC—M:52.2, F:47.8 |
- | CD: 92.1 UC: 88.7 |
- | - | ✓ |
| Zand 201548 | USA | Total = 440 [CD = 221, UC = 219] | M:49.8, F:50.2 | - | 64.4 | ✓ | ✓ | ✓ |
| Cohen 201549 | USA | UC = 4314 | M:63.6, F:36.4 | 45.1 | - | - | ✓ | ✓ |
| vanderHave 201550 | The Netherlands | Total = 1108 [CD = 554, UC = 424, IC = 130] | CD—M:42, F:58 UC—M:55, F:45 |
CD: 55 UC: 56.4 |
- | - | - | ✓ |
| Michael 201451 | Hungary | Total = 443 [CD = 260, UC = 183] | CD—M:47, F:53 UC—M:43.7, F:56.2 |
CD: 35 ± 11.3 UC: 40.7 ± 14.1 |
48 | ✓ | ✓ | ✓ |
| Lonnfors 201452 | 25 countries [not specified] | Total = 4670 [CD = 2895, UC = 1774] | M:33, F:66 | 35 | - | - | - | ✓ |
| vanderValk 201453 | The Netherlands | Total = 2282 [CD = 1373, UC = 909] | CD—M:34.3, F:65.7 UC—M:43.8, F:56.2 |
CD: 44.1 ± 11.8 UC: 46.1 ± 11.4 |
CD: 53 UC: 66.6 |
- | - | ✓ |
| Gibson 201454 | Australia | UC = 175 | M:47.4, F:52.6 | 41.7 ± 15.1 | - | ✓ | - | ✓ |
| Siebert 201355 | Switzerland | Total = 1187 [CD = 699, UC = 488] | CD—M:46.1, F:53.9 UC—M:49.8, F:50.2 |
CD: 41.8 ± 14.7 UC: 42.6 ± 13.9 |
- | - | - | ✓ |
| Gunnarsson 201356 | USA | Total = 200 | M:46, F:54 | 42.95 | - | - | ✓ | ✓ |
| Hoivik 201357 | Norway | Total = 516 [CD = 341, UC = 160] | CD—M:50.6, F:49.4 UC—M:49.6, F:50.4 |
UC: 45.6 CD: 38.1 |
- | - | - | ✓ |
| Ramos 201558 | Spain | Total = 293 [CD = 151, UC = 142] | CD—M:54, F:46 UC—M:53, F:46 |
CD: 43.1 ± 11 UC: 48 ± 10.2 |
73 | - | - | ✓ |
| Vaizey 201459 | UK | UC = 173 | M:44.5, F:55.5 | 47 | Full-time: 42.8, Part-time:13.3 Active: 58.5%, Remission: 54% |
✓ | - | ✓ |
| Viazis 201360 | Greece | Total = 1181 [CD = 539, UC = 642] | CD—M:52, F:48 UC—M:52, F:48 |
- | - | - | - | ✓ |
| Benedini 201261 | Italy | CD = 162 | M:50, F:50 | 43 | - | - | ✓ | - |
| Zhou 201062 | China | Total = 92 [CD = 52, UC = 40] | CD—M:67.55, F:32.5 UC—M:55.8, F:44.2 |
CD: 35.7 ± 11.6 UC: 45 ± 16.7 |
CD: 75 UC: 90.4 |
- | - | ✓ |
| Gibson 200863 | USA | Total = 15539 [CD = 6569, UC = 8970] | CD—M:43.26, F:56.74 UC—M:46.38, F:53.62 |
CD: 43.61 UC: 45.28 |
- | - | ✓ | - |
| Stark 200664 | Germany | Total = 483 [CD = 241, UC = 242] | CD—M:35, F:65 UC—M:45, F:55 |
CD: 41 ± 11 UC: 43 ± 12 |
CD: 63 UC: 67 |
- | ✓ | ✓ |
| Bernklev 200665 | Norway | Total = 495 [CD = 334, UC = 161] | M:51, F:49 | 41.2 ± 13.7 | CD: 76.4 UC: 81.4 |
- | - | ✓ |
| Boonen 200266 | The Netherlands | Total = 680 [CD = 282, UC = 359, IU = 39] | M:45.7, F:54.3 | 41 ± 11.4 | CD: 71.6 [M], 56.2 [F] UC: 74.9 [M], 62.4 [F] |
- | - | ✓ |
| Bernstein 200167 | Canada | Study A = 2476 [CD = 1231, UC = 1245] Study B = 80 [CD = 33, UC = 47] |
Study A—M:43.4, F:56.6 Study B—M:48.2, F:51.8 |
Study A: 42 [MEDIAN] | Study A: All IBD [M, N = 1074]: 79.9% All IBD [F, N = 1402]: 51.5% CD [M, N = 495]: 78.5% CD [F, N = 736]: 49.2% UC [M, N = 579]: 80.5% UC [F, N = 666]: 53.4% |
- | - | ✓ |
| Sorensen 198768 | Denmark | CD = 106 | - | 44 | 65 | - | - | ✓ |
| Sikirica 202269 | USA, France, Germany, Italy, Spain, and UK | CD = 2354 | M:51.4, F:48.6 | 39 | - | ✓ | - | - |
| Tiankanon 202170 | Thailand | Total = 209 [CD = 103, UC = 106] | M:49.3, F:50.7 | 47.3 ± 15.7 | - | ✓ | - | - |
| Humberto 202171 | USA [Puerto Rico] | Total = 120 [CD = 91, UC = 29] | M:49.2, F:50.8 | 27.0 ± 9.71 | 69.17 | - | ✓ | |
| Wong 202072 | USA | UC = 697 | M:42.2, F:57.8 | Mild: 51.36 ± 16.91 Moderate/severe: 43.76 ± 14.84 |
Mild: 56.3 Mod/sev: 62.7 |
✓ | - | ✓ |
| Armuzzi 201973 | Italy | CD = 552 | M:51, F:49 | 41 | 54 | ✓ | - | ✓ |
| Limdi 201974 | Not specified | UC = 1649 | - | - | - | ✓ | - | - |
| Carels 201975 | Belgium | CD = 18 | M:67, F:33 | 25 ± 2.3 | - | ✓ | - | - |
| Raimundo 201876 | USA | Total = 1020 | M:45, F:55 | 46 | - | ✓ | ✓ | - |
| Armuzzi 201877 | USA, France, Germany, Italy, Spain, UK | UC = 1037 | M:55.6, F:44.4 | 39.2 ± 13.8 | - | ✓ | - | - |
| Sebastian 201878 | UK | UC = 52 | M:50, F:50 | 40 ± 13.5 | 74 | ✓ | - | - |
| Aiello 201879 | Italy | UC = 77 | M:53.3, F:46.7 | 47.1 ± 13 | 49.4 | ✓ | - | ✓ |
| DeLima 201880 | Brazil | CD = 95 | M:48.5, F:51.5 | 41 | - | - | - | ✓ |
| Hellstrom 201781 | Sweden | Total = 1843 [CD = 698, UC = 1145] | - | - | - | - | ✓ | ✓ |
| Ghosh 201782 | Not specified | UC = 1816 | M:54.1, F:45.9 | 38.5 ± 14.6 | - | ✓ | - | ✓ |
| Ganz 201683 | USA | CD = 539 | M:46.6, F:53.4 | 48.2 | 57 | - | ✓ | ✓ |
| KatzAvitan 201684 | Israel | Total = 405 [CD = 255, UC = 150] | - | CD: 40.4 ± 14.9 UC: 52.8 ± 15.8 |
CD: 61.6 [active: 52, inactive: 73] UC: 59.3 [active: 52, inactive: 63] |
✓ | ||
| Camacho 201685 | Spain | Total = 127 | - | - | 53.5 | ✓ | - | ✓ |
| Schwartz 201686 | Israel | CD = 597 | M:42.6, F:57.4 | 37.9 ± 11.2 | M: 72.3, F: 54.9 | ✓ | ||
| VanAssche 201587 | 11 European countries [not specified] | UC = 250 | M:59, F:41 | 46.6 ± 16.3 | - | ✓ | ||
| Huascar 201588 | Not specified | Total = 292 [CD = 151, UC = 141] | M:43, F:47 | 45 ± 11 | - | - | ||
| Carpio 201589 | Spain | UC = 436 | M:53, F:47 | 46 ± 13 | - | - | ||
| Geccherle 201590 | Italy | CD = 47 | - | - | - | ✓ | ||
| Piercy 201591 | France, Germany, Italy, Spain, and USA | Total = 2065 [CD = 1084, UC = 981] | CD—M:49.5, F:50.5 UC—M:49.2, F:50.8 |
CD: 39.6 UC: 39.4 |
- | ✓ | - | - |
| Miller 201492 | USA | Total = 68 [CD = 27, UC = 41] | - | - | 72 | - | - | ✓ |
| Wladysiuk 201493 | Poland | CD = 464 | - | - | 56 | ✓ | - | - |
| Zand 201494 | USA | Total = 365 | - | - | - | ✓ | - | ✓ |
| Kroeker 201295 | Canada | Table 1: Total = 202 [CD = 129, UC = 73] Table 2: Total = 138 [CD = 83, UC = 55] |
CD—M:38.8, F:61.2 UC—M:39.7, F:60.3 |
CD: 24.6 ± 0.35 UC: 24.8 ± 0.33 |
- | - | ✓ | |
| Cohen 201296 | USA | UC = 5157 | M:63.7, F:36.3 | 48 | 100 | - | ✓ | ✓ |
| Wilson 201297 | Not specified | Total = 4990 [CD = 3143, UC = 1647] | - | - | - | - | - | ✓ |
| Naim 201198 | USA | Total = 534 | M:33, F:67 | - | 55 | ✓ | - | ✓ |
| Gomollon 201199 | Spain | CD = 1688 | M:49, F:51 | 42.5 ± 11.2 | 57 | ✓ | - | ✓ |
| Kane 2009100 | USA | CD = 247 | M:38.5, F:61.5 | 43 | Full-time: 46 Part-time: 13 |
- | - | ✓ |
| Procaccini 2007101 | USA | Total = 173 | - | - | - | - | - | ✓ |
| Yan 2020102 | China | Total = 891 [CD = 522, UC = 363, IC = 6] | Total—M:59, F:41 CD—M:61.5, F:38.5 UC—M:59.9, F:40.1 |
Total: 40 CD: 37 UC: 44 |
Employee—CD: 53.8, UC: 60.1, Total: 56.2 Self-employed—CD: 10.5, UC: 14.3, Total: 12.2 |
- | - | ✓ |
| Ueno 2017103 | Japan | Total = 172 [CD = 83, UC = 84, IU = 1] | M:66, F:32 | - | - | - | - | ✓ |
| VanDerValk 2014104 | The Netherlands | Total = 2252 [CD = 1315, UC = 937] | CD—M:37.3, F:62.7 UC—M:51.4, F:48.6 |
CD: 47.8 ± 13.6 UC: 49.8 ± 13.3 |
CD: 53.6 UC: 61.2 |
- | ✓ | ✓ |
| Hendrikson 1980105 | Denmark | UC = 122 | M:43, F:57 | - | 71 | - | - | ✓ |
| Binder 1985106 | Denmark | CD = 185 | M:40, F:60 | - | - | - | - | ✓ |
| Nurmi 2013107 | Finland | Total = 556 [CD = 153, UC = 365, IC = 37] | Total—M:47.5, F:52.5 CD—M:40.5, F:59.5 UC—M:51, F:49 IC—M:43.2, F:56.8 |
- | - | - | - | ✓ |
| Ghosh & Mitchell 2007108 | UK | Total = 5636 [CD = 3025, UC = 2333] | Total—M:42.8, F:56.9 CD—M:40, F:59.7 UC—M:46, F:53.7 |
- | - | - | - | - |
| Stjernman 2011109 | Sweden | Total = 505 [CD = 497, UC = 284] | CD—M:40.8, F:59.2 UC—M:55.6, F:44.4 |
CD: 46 UC: 46 |
- | - | - | ✓ |
| Longobardi 2003110 | USA | Total = 187 [105 with symptoms in the past 12 months, 82 without symptoms in the past 12 months] |
With symptoms—M:33.5 ± 5.6; F:66.5 ± 5.6 No symptoms—M:36.7 ± 5.5; F:63.3 ± 5.5 |
- | - | - | ✓ | ✓ |
| Longobardi 2003111 | Canada | Total = 187 | M:31.6, F:68.4 | - | - | - | ✓ | ✓ |
| Mayberry 1992112 | UK | CD = 58 | - | 31 ± 5 | 79 | - | - | ✓ |
| Gazzard 1978113 | Not specified | CD = 85 | M:33, F:67 | 35 ± 6 | - | - | - | ✓ |
| Juan 2003114 | Spain | CD = 635 | M:47.9, F:52.1 | 33.1 ± 11.9 | 48 | - | ✓ | ✓ |
| Ananthakrishnan 2008115 | USA | CD = 737 | M:37.8, F:62.2 | 45.8 | - | - | - | ✓ |
| Blomqvist 1997116 | Sweden | Total = 77 [CD = 39, UC = 38] | - | - | - | - | ✓ | ✓ |
| Mesterton 2009117 | Sweden | CD = 420 | M:45.6; F:54.4 | 50.2 ± 15.1 | - | - | ✓ | - |
IBD, Inflammatory bowel disease; CD, Crohn’s disease; UC, ulcerative colitis; IC, indeterminate colitis; M, male; F, female.
3.1. WPAI work outcomes
Table 2 provides a summary of the pooled estimates for WPAI outcomes and related indirect costs for all patients with IBD, CD only, and UC only. Among all patients with IBD, the pooled estimates were 16.4% [95% CI 13.9-18.9] for absenteeism, 35.9% [95% CI 31.1-40.7] for presenteeism, 39.4% [95% CI 33.9-44.9] for overall work impairment, and 46.0% [95% CI 39.5-52.5] for non-work activity impairment [Table 2]. The pooled estimates for indirect costs from absenteeism, presenteeism, and overall work impairment were 1813.9 [95% CI 907.8-2720.2], 3562.5 [95% CI 1,409.4-5,715.6], and 5131.1 [95% CI 800.9-9461.3] euros/patient/year, respectively [Table 2]. We were unable to estimate the costs of non-work activity impairment in IBD patients, nor the costs of presenteeism and overall work impairment by IBD subtype.
Table 2.
Pooled mean estimates of WPAI outcomes and indirect costs.
| WPAI outcome | No. of studies | Pooled mean estimate [%] [95% CI] | Heterogeneity [I2] |
|---|---|---|---|
| Absenteeism | |||
| Total IBD | 27 | 16.4 [13.9-18.9] | 95.5 |
| CD only | 13 | 18.9 [14.9-22.9] | 93.3 |
| UC only | 13 | 16.5 [13.0-20.1] | 95.4 |
| Presenteeism | |||
| Total IBD | 27 | 35.9 [31.1-40.7] | 98.8 |
| CD only | 13 | 41.3 [37.2-45.5] | 94.9 |
| UC only | 13 | 33.6 [27.8-39.5] | 98.3 |
| Overall work impairment | |||
| Total IBD | 27 | 39.4 [33.9-44.9] | 98.9 |
| CD only | 13 | 45.5 [40.0-50.9] | 96.5 |
| UC only | 12 | 38.0 [30.9-45.2] | 98.6 |
| Non-work activity impairment | |||
| Total IBD | 24 | 46.0 [39.5-52.5] | 99.4 |
| CD only | 12 | 52.6 [49.0-56.3] | 95.7 |
| UC only | 11 | 40.8 [32.2-49.5] | 99.3 |
| Indirect costsa | No. of studies | Pooled mean estimate [95% CI] [euro/patient/year] | Heterogeneity [I2] |
|---|---|---|---|
| Absenteeism | |||
| Total IBD | 8 | 1,813.9 [907.8-2720.2] | 98 |
| CD only | 3 | 1,541.2 [955.1-2127.4] | 79.1 |
| UC only | 3 | 1,170.5 [395.8-1945.1] | 97.7 |
| Presenteeism | |||
| Total IBD | 6 | 3,562.5 [1,409.4-5,715.6] | 99.3 |
| Overall work impairment | |||
| Total IBD | 5 | 5,131.1 [800.9-9,461.3] | 99.9 |
WPAI, Work Productivity and Activity Impairment questionnaire; IBD, inflammatory bowel disease; UC, ulcerative colitis; CD, Crohn’s disease.
aThere were not enough studies to determine pooled estimates of indirect costs separately for CD and UC with regards to presenteeism and overall work impairment.
Three studies reported WPAI absenteeism and presenteeism as time [hours] rather than percentages. The pooled estimate for absenteeism was 4.1 h per week [95% CI 3.1-5.2] [I2 = 54.3%] of missed work time due to IBD, whereas the pooled estimate for presenteeism was 3.9 h per week [95% CI 2.2-5.6] [I2 = 98.0%] of time experiencing impairment while at work. Five studies reported mean annual sick days, with a pooled estimate of 23.9 working days [95% CI 12.5-35.2] [I2 = 97.4%] lost due to IBD.
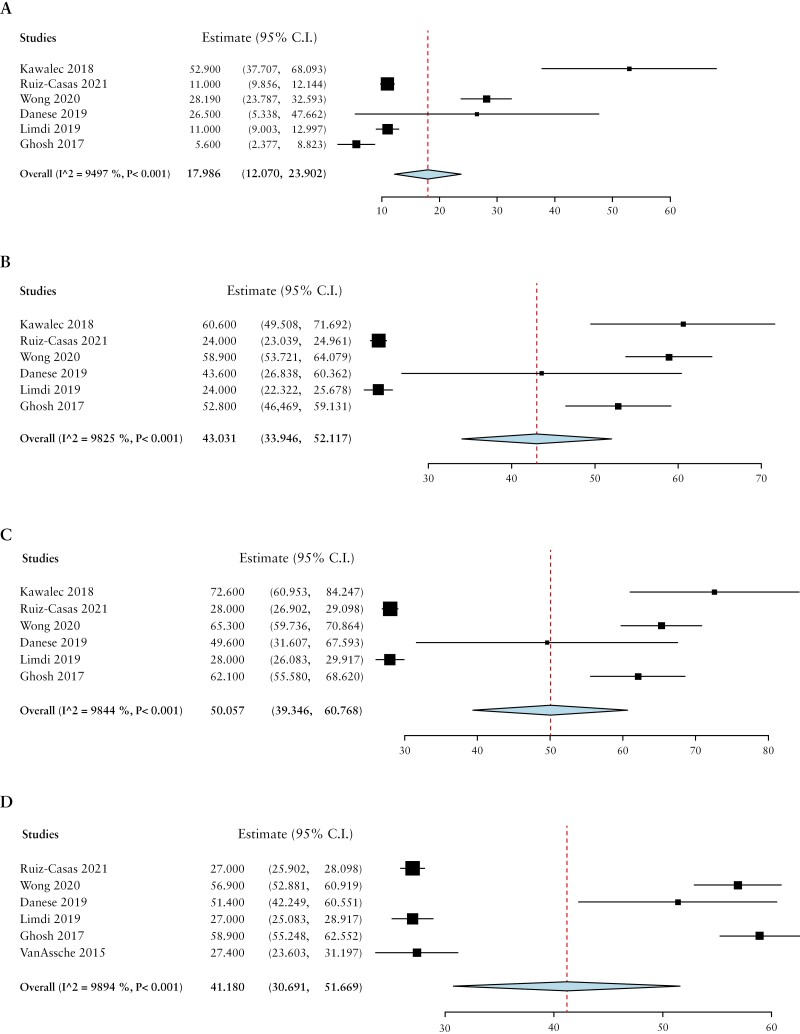
Patients with active or moderate-severe disease had higher absenteeism [mean difference 18.0%, 95% CI 12.1-23.9], presenteeism [mean difference 43.0%, 95% CI 33.9-52.1], overall work impairment [mean difference 50.1%, 95% CI 39.3-60.8], and non-work activity impairment [mean difference 41.2%, 95% CI 30.7-51.7] than those in remission or with mild disease [Figure 2].
Figure 2.
Comparison of A] absenteeism, B] presenteeism, C] total work impairment, D] non-work activity impairment, by mean differences based on disease activity.
3.2. Non-WPAI work outcomes
The pooled estimate for employment among all patients with IBD was 65.6% [95% CI 61.9-69.3%] [Table 3]. Unemployment was considered as a separate outcome in most studies and not directly related to employment values. The pooled percentage of unemployment was 16.4% [95% CI 14.5-18.3] in all patients with IBD. Among all patients with IBD, 39.5% [95% CI 16.8-62.3] reported sick days, 21.3% [95% CI 16.6-26.0] reported disability at work specifically due to IBD, 12.3% [95% CI 10.7-13.9] reported receiving disability pensions, and 29.6% [95% CI 19.0-40.1] reported losing jobs due to IBD.
Table 3.
Pooled proportions [percentages] of non-WPAI work-related outcomes.
| Work outcome | No. of studies | Pooled percentage [95% CI] | Heterogeneity [I2] |
|---|---|---|---|
| Employment | |||
| Total IBD | 73 | 65.6% [61.9-69.3] | 99.7 |
| CD only | 36 | 63.5% [57.9-69.0] | 99 |
| UC only | 35 | 68.1% [64.9-73.3] | 99.6 |
| Unemploymenta | |||
| Total IBD | 51 | 16.4% [14.5-18.3] | 98.7 |
| CD only | 22 | 15.2% [11.8-18.6] | 98 |
| UC only | 25 | 13.0% [10.2-15.8] | 98.3 |
| % reporting sick days | |||
| Total IBD | 25 | 39.5% [16.8-62.3] | 99.9 |
| CD only | 10 | 28.5% [22.8-34.2] | 99.3 |
| UC only | 15 | 34.8% [5.1-64.5] | 99.9 |
| % Disability due to IBD | |||
| Total IBD | 28 | 21.3% [16.6-26.0] | 99.3 |
| CD only | 16 | 21.0% [14.6-27.4] | 98.8 |
| UC only | 15 | 17.8% [12.0-23.6] | 98.8 |
| % Disability pensions | |||
| Total IBD | 23 | 12.3% [10.7-13.9] | 96.7 |
| CD only | 10 | 14.4% [12.0-16.8] | 95.2 |
| UC only | 10 | 9.7% [6.4%-13.0] | 98.3 |
| % losing jobs due to IBD | 4 | 29.6% [19.0-40.1] | |
| Total IBD | 98.8 | ||
WPAI, Work Productivity and Activity Impairment questionnaire; IBD, inflammatory bowel disease; UC, ulcerative colitis; CD, Crohn’s disease.
aPatient employment data was not solely limited to employment vs unemployment. Accordingly, unemployment was analyzed as a separate outcome [as opposed to 1-employment]
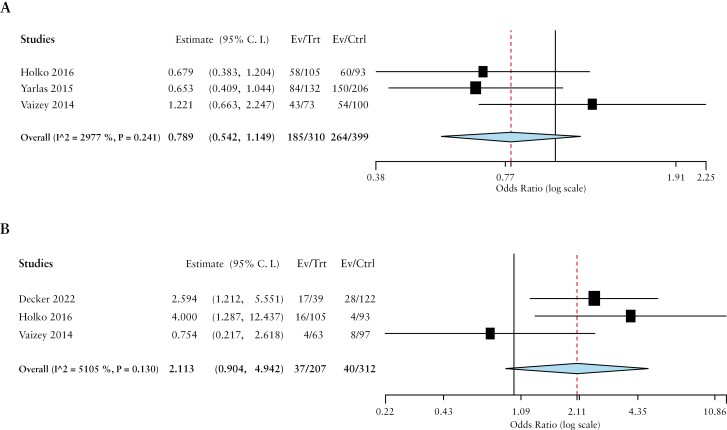
With respect to disease activity, IBD patients with active disease had lower odds of being employed (OR 0.8, 95% CI 0.5-1.1 [I2 = 29.7%]) and higher disability pension rates (OR 2.1, 95% CI 0.9-4.9 [I2 = 51.0%]) than those in remission or with mild disease [Figure 3].
Figure 3.
Comparison of A] employment and B] disability pensions by ORs based on disease activity.
3.3. Interventional studies
Twenty nine interventional studies [26 medical and three surgical] were included in this systematic review. Most studies showed statistically significant and clinically meaningful differences in all WPAI subcategories with respect to medical interventions such as mesalamine, biologics, and/or small molecules. In studies on adalimumab, at different times of follow-up, the mean change in absenteeism ranged from -6.7 to -11.4, presenteeism from -14.5 to -24.5, total work impairment from -14.5 to -29.2, and non-work activity impairment from -16.7 to -27.2.123,125 Similar findings were observed with other biologics, such as infliximab and golimumab, as well as with small molecules.118,129,133,135–137,139–143 Three studies with surgical interventions were included and had conflicting results with regards to work outcomes.144–146 One study reported improved capacity to work with J-pouch surgery,145 whereas another study showed more sick days following colectomy.144 A third study investigated different surgical approaches and reported different morbidities and work impairment with each approach.146
3.4. Risk of bias
As per the AXIS tool, most cross-sectional studies were scored at 15/20 or above, suggesting overall moderate or high quality studies. Most cohort and case-control studies had a ‘good’ overall rating and some were rated as ‘fair’ as per the NIH tool. The risk of bias assessment as using the ROB tool revealed ‘some concerns’ in most of the included RCTs [Supplementary Tables S3–5].
4. Discussion
In this systematic review and meta-analysis, we demonstrate that two-thirds of patients with IBD report being employed and almost one in three lose their job specifically due to IBD. Among patients who are employed, almost half report taking sick days, a quarter experience disability at work, and one in 10 receives disability pensions. Furthermore, patients with IBD reported missing approximately 16% of their working hours [absenteeism] and experiencing significant functional impairment for almost half of their total working time [presenteeism]. Absenteeism and presenteeism related to IBD are significantly higher than in the general population, where health-associated absenteeism is reported to be within 1.5–3% and presenteeism around 23%.147–149 The overall productivity loss, through absenteeism and presenteeism, among patients with IBD is estimated around 40% of their working time. In addition, almost half of their non-work activity time is impaired due to IBD. Importantly, in using the WPAI questionnaire, we show a significantly high burden of disease on work productivity outcomes that are consistent and standardised across studies. This may clarify the true impact of the disease and highlight the need for evidence-based interventions to improve work productivity outcomes.
Persons with IBD experience significant challenges at work due to IBD-related symptoms including fatigue, chronic abdominal pain, and diarrhoea requiring frequent bathroom use.150 Up to 70% of patients may experience difficulty focusing at work and completing tasks, and many have shorter work days due to IBD symptoms.92 Additionally, the fluctuating nature of symptoms and unexpected flare-ups may lead to unplanned absences and difficulties committing to future work tasks or making career plans.37,151 Interestingly, IBD often affects absenteeism to a lesser extent than presenteeism,43 which is consistent with our results. This is important to note, given that productivity losses associated with presenteeism are significantly higher than those from absenteeism. One explanation is that patients may feel obliged to attend work for fear of financial repercussions or job insecurity, but continue to have debilitating symptoms at work, affecting their productivity.152 This may reflect patients’ fear of discussing their diagnosis at their workplace or requesting accommodations to feel comfortable at work.150
Previously published studies on work impairment in IBD have significant variability which has led to inconsistent findings. For instance, absenteeism has been estimated between 5% and 20%,24,48 and presenteeism and total work impairment have ranged from 20% to 65% and 20% to 50%, respectively.24,34,43 The variability in data might be due to residual confounding from underlying disease activity. Furthermore, studies have differed by proportion of patients on advanced IBD therapies, which in turn alters IBD activity and subsequently patients’ work productivity.153 We observed significant variability in the proportion of biologic use across the included studies, ranging from 0% to 94%. Furthermore, we noted significant variability in the definitions for work status and employment across studies. For example, some studies included any working individual with IBD [including students or stay-at-home parents], and others included only full-time, part-time, and/or self-employment. Finally, fluctuations within the labour market over time and between different countries may have also resulted in significant variability in overall employment and work outcomes in IBD.154
We also demonstrated that compared with those with UC, persons with CD have a greater degree of absenteeism, presenteeism, overall work, and total activity impairment. This is consistent with previous literature.21,51,53 Overall, CD patients face a greater degree of disability in multiple life domains compared with those with UC.155 These findings may be due to a greater systemic and psychological impact of CD.65,156 In addition, the incidences of chronic fatigue and depression are often greater among patients with CD, and these may subsequently interfere with work performance.157,158 Another important factor associated with poor work outcomes is disease activity. In particular, we observed higher WPAI scores among patients with active and moderate–severe disease, which is consistent with previous studies.159,160 Patients with more severe disease experience more significant work impairment, likely due to increased fatigue and poor health-related QOL.161In fact, twice as many patients with active IBD report fatigue, compared with those in remission.162 As such, disease activity is an important factor to consider when caring for patients with IBD.
We also reported significant indirect costs associated with decreased workplace productivity and sick leave in patients with IBD. In particular, we observed that the average annual indirect costs from total work impairment due to IBD was estimated to be greater than 5000 euros/patient/year. These costs are higher among those with a greater degree of absenteeism, among those living with CD compared with UC,64,104,155,163,164 and those with active inflammation.24,165 Overall, these findings suggest a high economic burden related to absenteeism and work productivity loss from IBD. Absenteeism may also be related to the lack of workplace accommodations, which makes the work environment challenging. Studies show that almost 90% of persons with IBD needed workplace accommodations, yet many find it difficult to ask or arrange for accommodations. This may certainly contribute to absenteeism and decreased productivity at work.166 In contrast, providing appropriate workplace accommodations such as flexible working hours and locations and employer benefits [eg, paid sick leave and health insurances] can certainly improve work productivity and mitigate many of these indirect costs.167
Medical and surgical interventions in IBD may reduce work impairment. We observed that most interventional studies demonstrated clinically meaningful and statistically significant improvements in work outcomes. This was consistent across studies using mesalamine, biologics, and/or small molecules.119,131,141 Furthermore, following effective treatment with anti-tumour necrosis factor [anti-TNF] therapy, patients reported significant improvement in all elements of the WPAI regardless of their initial level of disability.123,129,135,136 In contrast, the impact of surgical interventions on work impairment in IBD remains controversial.41,145 Whereas some patients’ productivity may improve after surgery,145 others may experience an increased risk of work-related disability and sick days due to post-surgical complications such as anastomotic leaks.53,58 Overall, medical and surgical therapies may improve work productivity among persons with IBD, although patient-specific factors should guide treatment decisions to determine the best therapeutic plan for each patient.
This study has several strengths. We employed a broad literature search which allowed us to identify a large number of eligible studies and approximate the burden of IBD across a number of jurisdictions worldwide. We used the WPAI questionnaire to standardise work productivity outcomes and accurately estimate effect sizes, despite the inherent limitations of the literature data. Additionally, we were able to delineate the association of disease subtype [CD vs UC], severity, and treatment modality [medical vs surgical] with work productivity outcomes. Despite this, the study has inherent limitations. First, there is significant heterogeneity across the IBD literature with regards to work productivity. This is likely due to significant variations in study populations, study design, definition of the underlying IBD diagnosis, and definitions of work outcomes across studies. For example, some studies defined IBD through self-reported questionnaires, and others used case history and endoscopic criteria. Similarly, employment was defined differently across studies as described above. Study results also varied across different geographical regions, reflecting differences in the workforce across countries. Furthermore, indirect costs were calculated based on the average wage and number of weeks worked per year, which may also be different across countries. Ultimately, this limits the generalisability of the study results when applying to specific jurisdictions. Second, there was a large number of excluded studies due to missing data or incomplete information. Furthermore, due to the lack of standardised outcome reporting in the literature, many studies did not include WPAI outcomes or compare them by disease severity. This limited our analyses to only a few eligible studies and may have led to selection bias. Additionally, we were unable to quantify the therapeutic effect of medical or surgical interventions on WPAI indices in a formal meta-analysis, due to the considerable heterogeneity in data reporting across studies. Overall, this highlights the need for standardisation of study designs and outcome definitions to guide future research in this important field.
Conclusion
In conclusion, this study uses standardised tools to highlight the significant burden of IBD on work productivity. IBD type, disease severity, and medical therapy are all important factors that may affect work productivity outcomes. Future studies are needed to explore different workplace accommodations and their impact in improving work productivity for persons with IBD.
Supplementary Data
Supplementary data are available at ECCO-JCC online.
Acknowledgements
We would like to thank Julia Martyniuk, education librarian at the University of Toronto, for her support in developing the search strategy for this review.
Contributor Information
Michael Youssef, Department of Internal Medicine, University of Toronto, Toronto, ON, Canada.
Nariman Hossein-Javaheri, Department of Internal Medicine, University at Buffalo, Buffalo, NY, USA.
Tedi Hoxha, Department of Internal Medicine, University of Toronto, Toronto, ON, Canada.
Christina Mallouk, Faculty of Medicine, University of Ottawa, Ottawa, ON, Canada.
Parul Tandon, Division of Gastroenterology and Hepatology, University Health Network, University of Toronto, Toronto, ON, Canada.
Funding
This work was supported by the Mount Sinai Resident Research Funding.
Conflict of Interest
None of the authors have any relevant conflicts of interest to declare.
Author Contributions
PT, MY, and NH conceived and designed the study and the search strategy. MY, NH, TH, and CM screened the references, identified eligible articles, and abstracted the relevant data. PT and MY performed the statistical analysis. All authors participated in writing and critically reviewing the manuscript. All authors reviewed and approved the final version of the manuscript. Guarantor of the article: Dr. Parul Tandon.
Data Availability
The data underlying this article are available and will be shared on reasonable request to the corresponding author.
References
- 1. Alatab S, Sepanlou SG, Ikuta K, et al. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 2020;5:17–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Leso V, Gervetti P, Macrini MC, Russo F, Iavicoli I.. Inflammatory bowel diseases and work disability: a systematic review of predictive factors. Eur Rev Med Pharmacol Sci 2021;25:165–81. [DOI] [PubMed] [Google Scholar]
- 3. Mak WY, Zhao M, Ng SC, Burisch J.. The epidemiology of inflammatory bowel disease: east meets west. J Gastroenterol Hepatol 2020;35:380–9. [DOI] [PubMed] [Google Scholar]
- 4. van Gennep S, de Boer NKH, Gielen ME, et al. Impaired quality of working life in inflammatory bowel disease patients. Dig Dis Sci 2021;66:2916–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Reilly MC, Zbrozek AS, Dukes EM.. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEcon 1993;4:353–65. [DOI] [PubMed] [Google Scholar]
- 6. Tse CS, Hunt MG, Brown LA, Lewis JD.. Inflammatory Bowel Diseases-related disability: risk factors, outcomes, and interventions. Inflamm Bowel Dis 2023;30:501–7. [DOI] [PubMed] [Google Scholar]
- 7. Higgins JPT, Li T, Deeks JJ (editors). Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane, 2023. www.training.cochrane.org/handbook [Google Scholar]
- 8. Higgins JPT, Thomas J, Chandler J, et al. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane, 2023. www.training.cochrane.org/handbook [Google Scholar]
- 9. West SL, Gartlehner G, Mansfield AJ, et al. Comparative Effectiveness Review Methods: Clinical Heterogeneity [Internet]. Rockville MD: Agency for Healthcare Research and Quality [US]; 2010. [AHRQ Methods for Effective Health Care]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK53310/ [PubMed] [Google Scholar]
- 10. OpenMetaAnalyst: Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH.. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw 2012;49:1–5. [Google Scholar]
- 11. National Institutes of Health. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. 2014. https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort.Accessed October 20, 2023. [Google Scholar]
- 12. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:14898. [DOI] [PubMed] [Google Scholar]
- 13. Ding Z, Muser E, Izanec J, Lukanova R, Kershaw J, Roughley A.. Work-related productivity loss and associated indirect costs in patients with crohn’s disease or ulcerative colitis in the United States. Crohns Colitis 360 2022;4:otac023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Decker B, Tuzil J, Lukas M, et al. Patient-reported symptoms are a more reliable predictor of the societal burden compared to established physician-reported activity indices in inflammatory bowel disease: a cross-sectional study. Expert Rev Gastroenterol Hepatol 2023;17:99–108. [DOI] [PubMed] [Google Scholar]
- 15. Holko P, Kawalec P, Sajak-Szczerba M, Avedano L, Mossakowska M.. Indirect costs of inflammatory bowel diseases: a comparison of patient-reported outcomes across 12 European countries. Inflamm Bowel Dis 2023;29:752–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Varma A, Weinstein J, Seabury J, et al. Patient-reported impact of symptoms in crohn’s disease. Am J Gastroenterol 2022;117:2033–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Paulides E, Cornelissen D, de Vries AC, van der Woude CJ.. Inflammatory bowel disease negatively impacts household and family life. Frontline Gastroenterol 2022;13:402–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Viazis N, Stefanidou A, Mantzaris GJ.. The ulcerative colitis narrative Greece survey: patients’ and physicians’ perspective on quality of life and disease management. Ann Gastroenterol 2022;35:267–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Paulides E, Daker C, Frampton C, et al. Overcoming workplace disability in IBD patients: an observational study. Inflamm Intest Dis 2020;5:84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Topal F, Camyar H, Saritas Yuksel E, Gunay S, Topal F, Gür EO.. Work productivity loss in inflammatory bowel disease patients in Turkey. Gastroenterol Res Pract 2020;2020:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yamabe K, Liebert R, Flores N, Pashos CL.. Health-related quality of life outcomes and economic burden of inflammatory bowel disease in Japan. Clin Outcomes Res 2019;11:221–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kawalec P, Stawowczyk E.. Relationship between physician-based assessment of disease activity, quality of life, and costs of ulcerative colitis in Poland. Prz Gastroenterol 2018;13:61–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sciberras M, Karmiris K, Nascimento C, et al. Mental health, work presenteeism, and exercise in Inflammatory Bowel Disease. J Crohns Colitis 2022;16:1197–201. [DOI] [PubMed] [Google Scholar]
- 24. van Gennep S, Evers SW, Rietdijk ST, et al. High disease burden drives indirect costs in employed inflammatory bowel disease patients: the WORK-IBD Study. Inflamm Bowel Dis 2021;27:352–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ruiz-Casas L, Evans J, Rose A, et al. The LUCID study: Living with ulcerative colitis; identifying the socioeconomic burden in Europe. BMC Gastroenterol 2021;21:456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rankala R, Mattila K, Voutilainen M, Mustonen A.. Inflammatory bowel disease-related economic costs due to presenteeism and absenteeism. Scand J Gastroenterol 2021;56:687–92. [DOI] [PubMed] [Google Scholar]
- 27. Khalili H, Everhov AH, Halfvarson J, et al.; SWIBREG Group. Healthcare use, work loss and total costs in incident and prevalent Crohn’s disease and ulcerative colitis: results from a nationwide study in Sweden. Aliment Pharmacol Ther 2020;52:655–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yu Q, Zhu C, Feng S, et al. Economic burden and health care access for patients with inflammatory bowel diseases in China: web-based survey study. J Med Internet Res 2021;23:e20629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. de Sá Brito Fróes R, da Luz Moreira A, de V Carneiro AJ, et al. Prevalence, indirect costs, and risk factors for work disability in patients with Crohn’s Disease at a Tertiary Care Center in Rio de Janeiro. Dig Dis Sci 2021;66:2925–34. [DOI] [PubMed] [Google Scholar]
- 30. Walter E, Hausberger SC, Groß E, Siebert U.. Health-related quality of life, work productivity and costs related to patients with inflammatory bowel disease in Austria. J Med Econ 2020;23:1061–71. [DOI] [PubMed] [Google Scholar]
- 31. Manceur AM, Ding Z, Muser E, et al. Burden of Crohn’s disease in the United States: long-term healthcare and work-loss related costs. J Med Econ 2020;23:1092–101. [DOI] [PubMed] [Google Scholar]
- 32. Moon JR, Lee CK, Hong SN, et al.; MOSAIK study group of the Korean Association for Study of Intestinal Diseases. Unmet psychosocial needs of patients with newly diagnosed Ulcerative Colitis: results from the nationwide prospective cohort study in Korea. Gut and Liver 2020;14:459–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chao CY, Lemieux C, Restellini S, et al. Maladaptive coping, low self-efficacy and disease activity are associated with poorer patient-reported outcomes in inflammatory bowel disease. Saudi J Gastroenterol 2019;25:159–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Parra RS, Chebli JM, Amarante HM, et al. Quality of life, work productivity impairment and healthcare resources in inflammatory bowel diseases in Brazil. World J Gastroenterol 2019;25:5862–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Christiansen LK, Lo B, Bendtsen F, Vind I, Vester-Andersen MK, Burisch J.. Health-related quality of life in inflammatory bowel disease in a Danish population-based inception cohort. United European Gastroenterol J 2019;7:942–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Pillai N, Dusheiko M, Maillard MH, et al.; Swiss IBD Cohort Study Group. The evolution of health care utilisation and costs for Inflammatory Bowel Disease over ten years. J Crohns Colitis 2019;13:744–54. [DOI] [PubMed] [Google Scholar]
- 37. Le Berre C, Peyrin-Biroulet L, Buisson A, et al. Impact of inflammatory bowel diseases on working life: a French nationwide survey. Dig Liver Dis 2019;51:961–6. [DOI] [PubMed] [Google Scholar]
- 38. Gonczi L, Kurti Z, Verdon C, et al. Perceived quality of care is associated with disease activity, quality of life, work productivity, and gender, but not disease phenotype: a prospective study in a high-volume IBD centre. J Crohns Colitis 2019;13:1138–47. [DOI] [PubMed] [Google Scholar]
- 39. Everhov AH, Khalili H, Askling J, et al. Work loss before and after diagnosis of Crohn’s Disease. Inflamm Bowel Dis 2019;25:1237–47. [DOI] [PubMed] [Google Scholar]
- 40. Everhov AH, Khalili H, Askling J, et al. Sick leave and disability pension in prevalent patients with Crohn’s Disease. J Crohns Colitis 2018;12:1418–28. [DOI] [PubMed] [Google Scholar]
- 41. Spekhorst LM, Oldenburg B, van Bodegraven AA, et al.; Parelsnoer Institute and the Dutch Initiative on Crohn and Colitis. Prevalence of- and risk factors for work disability in Dutch patients with inflammatory bowel disease. World J Gastroenterol 2017;23:8182–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kamat N, Ganesh Pai C, Surulivel Rajan M, Kamath A.. Cost of illness in inflammatory bowel disease. Dig Dis Sci 2017;62:2318–26. [DOI] [PubMed] [Google Scholar]
- 43. Williet N, Sarter H, Gower-Rousseau C, et al. Patient-reported outcomes in a French Nationwide Survey of Inflammatory Bowel Disease Patients. J Crohns Colitis 2017;11:165–74. [DOI] [PubMed] [Google Scholar]
- 44. Holko P, Kawalec P, Mossakowska M, Pilc A.. Health-related quality of life impairment and indirect cost of Crohn’s Disease: a self-report study in Poland. PLoS One 2016;11:e0168586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. De Boer AGEM, Bennebroek Evertsz’ F, Stokkers PC, et al. Employment status, difficulties at work and quality of life in inflammatory bowel disease patients. Eur J Gastroenterol Hepatol 2016;28:1130–6. [DOI] [PubMed] [Google Scholar]
- 46. Aldeguer X, Sicras-Mainar A.. Costs of ulcerative colitis from a societal perspective in a regional health care area in Spain: a database study. Gastroenterol Hepatol 2016;39:9–19. [DOI] [PubMed] [Google Scholar]
- 47. Vester-Andersen MK, Prosberg MV, Vind I, Andersson M, Jess T, Bendtsen F.. Low risk of unemployment, sick leave, and work disability among patients with Inflammatory Bowel Disease: a 7-year follow-up study of a Danish Inception Cohort. Inflamm Bowel Dis 2015;21:2296–303. [DOI] [PubMed] [Google Scholar]
- 48. Zand A, van Deen WK, Inserra EK, et al. Presenteeism in Inflammatory Bowel Diseases: a hidden problem with significant economic impact. Inflamm Bowel Dis 2015;21:1623–30. [DOI] [PubMed] [Google Scholar]
- 49. Cohen R, Skup M, Ozbay AB, et al. Direct and indirect healthcare resource utilization and costs associated with ulcerative colitis in a privately-insured employed population in the US. J Med Econ 2015;18:447–56. [DOI] [PubMed] [Google Scholar]
- 50. van der Have M, Fidder HH, Leenders M, et al.; COIN study group. Self-reported disability in patients with inflammatory bowel disease largely determined by disease activity and illness perceptions. Inflamm Bowel Dis 2015;21:369–77. [DOI] [PubMed] [Google Scholar]
- 51. Michael MD, Bálint A, Lovász BD, et al. Work disability and productivity loss in patients with inflammatory bowel diseases in Hungary in the era of biologics. Eur J Health Econ 2014;15:121–8. [DOI] [PubMed] [Google Scholar]
- 52. Lönnfors S, Vermeire S, Avedano L.. IBD and health-related quality of life—discovering the true impact. J Crohns Colitis 2014;8:1281–6. [DOI] [PubMed] [Google Scholar]
- 53. van der Valk ME, Mangen MJJ, Leenders M, et al.; COIN study group. Risk factors of work disability in patients with inflammatory bowel disease: A Dutch nationwide web-based survey: work disability in inflammatory bowel disease. J Crohns Colitis 2014;8:590–7. [DOI] [PubMed] [Google Scholar]
- 54. Gibson PR, Vaizey C, Black CM, et al. Relationship between disease severity and quality of life and assessment of health care utilization and cost for ulcerative colitis in Australia: a cross-sectional, observational study☆. J Crohns Colitis 2014;8:598–606. [DOI] [PubMed] [Google Scholar]
- 55. Siebert U, Wurm J, Gothe RM, et al.; Swiss IBD Cohort Study Group. Predictors of temporary and permanent work disability in patients with inflammatory bowel disease: results of the Swiss Inflammatory Bowel Disease Cohort Study. Inflamm Bowel Dis 2013;19:847–55. [DOI] [PubMed] [Google Scholar]
- 56. Gunnarsson C, Chen J, Rizzo JA, Ladapo JA, Naim A, Lofland JH.. The employee absenteeism costs of inflammatory bowel disease: evidence from US National Survey Data. J Occup Environ Med 2013;55:393–401. [DOI] [PubMed] [Google Scholar]
- 57. Høivik ML, Moum B, Solberg IC, Henriksen M, Cvancarova M, Bernklev T; IBSEN Group. Work disability in inflammatory bowel disease patients 10 years after disease onset: results from the IBSEN Study. Gut 2013;62:368–75. [DOI] [PubMed] [Google Scholar]
- 58. Ramos A, Calvet X, Sicilia B, et al. IBD-related work disability in the community: prevalence, severity and predictive factors. a cross-sectional study. United European Gastroenterol J 2015;3:335–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Vaizey CJ, Gibson PR, Black CM, et al. Disease status, patient quality of life and healthcare resource use for ulcerative colitis in the UK: an observational study. Frontline Gastroenterol 2014;5:183–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Viazis N, Mantzaris G, Karmiris K, et al.; Hellenic Foundation of Gastroenterology and Nutrition. Inflammatory bowel disease: Greek patients’ perspective on quality of life, information on the disease, work productivity and family support. Ann Gastroenterol 2013;26:52–8. [PMC free article] [PubMed] [Google Scholar]
- 61. Benedini V, Caporaso N, Corazza GR, et al. Burden of Crohn’s disease: economics and quality of life aspects in Italy. Clinicoecon Outcomes Res 2012;4:209–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Zhou Y, Ren W, Irvine EJ, Yang D.. Assessing health-related quality of life in patients with inflammatory bowel disease in Zhejiang, China. J Clin Nurs 2010;19:79–88. [DOI] [PubMed] [Google Scholar]
- 63. Gibson TB, Ng E, Ozminkowski RJ, et al. The Direct and Indirect Cost Burden of Crohn’s Disease and Ulcerative Colitis. J Occup Environ Med 2008;50:1261–72. [DOI] [PubMed] [Google Scholar]
- 64. Stark R, König HH, Leidl R.. Costs of inflammatory bowel disease in Germany. PharmacoEcon 2006;24:797–814. [DOI] [PubMed] [Google Scholar]
- 65. Bernklev T, Jahnsen J, Henriksen M, et al. Relationship between sick leave, unemployment, disability, and health-related quality of life in patients with inflammatory bowel disease. Inflamm Bowel Dis 2006;12:402–12. [DOI] [PubMed] [Google Scholar]
- 66. Boonen A, Dagnelie PC, Feleus A, et al. The impact of inflammatory bowel disease on labor force participation: results of a population sampled case-control study. Inflamm Bowel Dis 2002;8:382–9. [DOI] [PubMed] [Google Scholar]
- 67. Bernstein CN, Kraut A, Blanchard JF, Rawsthorne P, Yu N, Walld R.. The relationship between inflammatory bowel disease and socioeconomic variables. Am J Gastroenterol 2001;96:2117–25. [DOI] [PubMed] [Google Scholar]
- 68. Sørensen VZ, Olsen BG, Binder V.. Life prospects and quality of life in patients with Crohn’s disease. Gut 1987;28:382–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Sikirica M, Lynch J, Kershaw J, Lukanova R, Baker S, Milligan G.. P152 Impact of disease location on burden of illness in patients with moderate-severe Crohn’s disease: a real-world survey in the United States, France, Germany, Italy, Spain, and United Kingdom [5EU]. J Crohns Colitis 2022;16:i230–i230. [Google Scholar]
- 70. Tiankanon K, Limsrivilai J, Poocharoenwanich N, et al. Burden of Inflammatory Bowel Disease on patient mood, fatigue, work, and health-related quality of life in Thailand: a case-control study. Crohn’s & Colitis 360 2021;3:otab077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Nieves-Jiménez H, Matos-Jiménez F, Colón-Terrón M, Torres E.. P015 Impact of IBD on Daily Lives: a Descriptive Insight to Patient’s Experience in the Work and Study Settings. Am J Gastroenterol 2021;116[Suppl 1]:S4. https://journals.lww.com/ajg/abstract/2021/12001/p015_impact_of_ibd_on_daily_lives__a_descriptive.16.aspx [DOI] [PubMed] [Google Scholar]
- 72. Wong G, Solon C, Way N, Martin A, Sciscione J.. S0691 worsening patient-reported outcomes with increasing disease severity in ulcerative colitis in the USA: The National Health and Wellness Survey. Am J Gastroenterol 2020;115:346. https://journals.lww.com/ajg/fulltext/2020/10001/s0691_worsening_patient_reported_outcomes_with.692.aspx. [Google Scholar]
- 73. Armuzzi A, Riegler G, Furfaro F, et al. Epidemiological features and disease-related concerns of a large cohort of Italian patients with active Crohn’s disease. Dig Liver Dis 2019;51:804–11. [DOI] [PubMed] [Google Scholar]
- 74. Limdi JK, Rose A, Noone D, et al. 744 The impact of Ulcerative Colitis on quality of life and productivity across Europe: a burden of illness study. Am J Gastroenterol 2019;114:436–7. https://journals.lww.com/ajg/Abstract/2019/10001/744_The_Impact_of_Ulcerative_Colitis_on_Quality_of.744.aspx [Google Scholar]
- 75. Carels C, Wauters L, Outtier A, et al. Health literacy, quality of life, work productivity and activity impairment in young adults with Crohn’s Disease compared to diabetes mellitus patients: long-term follow-up from the Belgian Crohn’s Disease Registry. Front Pediatr 2021;9:624416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Karina R, Teresa M, Natalia F.. The economic burden associated with Inflammatory Bowel Disease severity: P-043. Am J Gastroenterol 2018;113:S11. [Google Scholar]
- 77. Armuzzi A, Tarallo M, DiBonaventura M, et al. The association between disease activity and patient-reported outcomes in patients with moderate-to-severe ulcerative colitis in the United States and Europe. BMC Gastroenterol 2020;20:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Sebastian S, Roberts J, Waller J, et al. PRO2 Based remote monitoring in ulcerative colitis: a prospective real world study. Value Health 2018;21:S258. [Google Scholar]
- 79. Aiello AF, Scrivo B, Calvaruso V, et al. P.07.18 Assessment of costs, health resources utilization and impact on work productivity in ulcerative colitis. Dig Liver Dis 2018;50:e200–1. [Google Scholar]
- 80. de Lima I, Andrade A, Leite A.. N007 Productivity and work reduced capacity in Crohn’s disease. J Crohns Colitis 2018;12:S571–2. [Google Scholar]
- 81. Hellström PM, Stålhammar J, Beydogan H, Huetson P, Skup M, Agréus L.. P735 Indirect burden of patients with moderate inflammatory bowel disease in Uppsala County Council, Sweden: A retrospective study using real-world data. J Crohns Colitis 2017;11:S457. [Google Scholar]
- 82. van Haaren S, Ghosh S, Peyrin-Biroulet L, et al. OP018 Healthcare resource utilization and quality of life in patients with ulcerative colitis by disease severity: baseline data from iconIC. Gut 2018;67[Suppl 1]:A100.2. [Google Scholar]
- 83. Ganz ML, Sugarman R, Wang R, Hansen BB, Håkan-Bloch J.. The Economic and Health-related Impact of Crohn’s Disease in the United States: Evidence from a Nationally Representative Survey. Inflamm Bowel Dis 2016;22:1032–41. [DOI] [PubMed] [Google Scholar]
- 84. Avitan AK, Schwartz D, Greenberg D, et al. The impact of Inflammatory Bowel Disease on work productivity: comparison of a real-world sample of patients with Crohn’s Disease and Ulcerative Colitis. Value Health 2016;19:A511. [Google Scholar]
- 85. Camacho L, Camargo R, Lopez S, et al. Influence of inflammatory bowel disease on work-related outcomes and activity impairment and its relation with health-related quality of life. J Crohns Colitis 2016;10:S217. [Google Scholar]
- 86. Schwartz D, Greenberg D, Chernin E, et al. Absenteeism and presenteeism amongst Crohn’s disease patients: results from a real-world cohort in Israel. J Crohns Colitis 2016:S400. [Google Scholar]
- 87. Van Assche G, Peyrin-Biroulet L, Ding Q,et al. P1604 Health-Related Quality of Life and Productivity Loss Among Moderate to Severe Ulcerative Colitis Patients Treated with Conventional Therapies in Europe: The UC Cares [Ulcerative Colitis Condition, Attitude, Resources and Educational Study]. UEG Week 2015 Poster Presentations. UEG Journal2015;3:146–687. 10.1177/2050640615601623. [DOI] [Google Scholar]
- 88. Huascar A, Xavier C, Beatriz S, Mercedes V, Ariadna F, Fernando G.. Work disability in IBD: prevalence, severity and predictive factors. J Crohns Colitis 2015:S425–S425. [Google Scholar]
- 89. Carpio D, Argueelles F, Calvet X, Juliá B, Romero C, López-Sanromán A.. Perception of social and emotional impact of Ulcerative Colitis by Spanish patients-UC-life survey. J Crohns Colitis 2015;9:S405–S405. [Google Scholar]
- 90. Geccherle E, Fortuna M, Montanari R, Geccherle A.. Quality of life and coping mechanisms in patients with Crohn’s disease treated with biological therapy. J Crohns Colitis 2015;9:S100. [Google Scholar]
- 91. Piercy J, Ozbay AB, Roughley A, Chao J, Skup MT. Comparison of Ulcerative Colitis with Crohn’s Disease from the perspective of patient burden. Gastroenterology 2015;148:S–839. [Google Scholar]
- 92. Miller J, Gessner G, Charabaty A.. IBD in young adult patients: impact on early professional life experience: 2210. In: Am J Gastroenterol 2014;109:S641. https://journals.lww.com/ajg/Fulltext/2014/10002/IBD_in_Young_Adult_Patients__Impact_on_Early.2210.aspx [Google Scholar]
- 93. Wladysiuk M, Bebrysz M, Fedyna M, Haldas M, Rutkowski J.. What determines work productivity loss in Rheumatoid Arthtiris [ra], Crohn’s Disease [cd] and Psoriasis [ps] in Poland? Results Of Move to Work [m2w] Study. Value Health 2014;17:A45–6. [DOI] [PubMed] [Google Scholar]
- 94. Zand A, Van Deen W, Ha C, et al. DOP026 Work related problems and impaired productivity in patients with inflammatory bowel diseases [IBD]. J Crohns Colitis 2014;8:S27. [Google Scholar]
- 95. Kroeker KI, Goodman KJ, Fedorak RNM.. Absenteeism and short-term disability are higher in young adults with Inflammatory Bowel Disease. Gastroenterology 2012;5:S–668. [Google Scholar]
- 96. Cohen R, Rizzo J, Yang M, et al. Direct and indirect utilization and costs associated with ulcerative colitis. Am J Gastroenterol 2012;107:S608. [Google Scholar]
- 97. Wilson B, Lonnfors S, Hommes DW, et al. P406 A European Crohn’s and ulcerative colitis patient life IMPACT survey. J Crohns Colitis 2012;6:S171. [Google Scholar]
- 98. Naim A, DiBonaventura M, Lofland J, Freedman D.. PSY25 Relationship between monthly out-of-pocket healthcare costs and work productivity among patients with inflammatory bowel disease. Value Health 2011;14:A63. [Google Scholar]
- 99. Gomollon F, Gonzalez Y, Hinojosa J, et al. Health-related quality of life, work productivity and psychological well-being in Spanish Crohn Disease Patients. Gastroenterology 2011;140:S–395. [Google Scholar]
- 100. Kane SV, Wolf DC, Plevy SE, et al. S1038 factors influencing workforce participation and productivity among Crohn’s Disease Patients. Gastroenterology 2009;136:A–175. [Google Scholar]
- 101. Procaccini NJ, Bickston SJ.. Disability in the Inflammatory Bowel Diseases: impact of awareness of the Americans with Disabilities Act. Am J Gastroenterol 2006;101:S431. [Google Scholar]
- 102. Yan X, Qiao Y, Tong J, et al.; Young Investigators for the study of Inflammatory Bowel Diseases [YIIBD]. Assessment of patient-centered outcomes [PROs] in inflammatory bowel disease [IBD]: a multicenter survey preceding a cross-disciplinary [functional] consensus. Health Qual Life Outcomes 2020;18:241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Ueno F, Nakayama Y, Hagiwara E, Kurimoto S, Hibi T.. Impact of inflammatory bowel disease on Japanese patients’ quality of life: results of a patient questionnaire survey. J Gastroenterol 2017;52:555–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. van der Valk ME, Mangen MJJ, Leenders M, et al.; COIN study group and the Dutch Initiative on Crohn and Colitis. Healthcare costs of inflammatory bowel disease have shifted from hospitalisation and surgery towards anti-TNFα therapy: results from the COIN study. Gut 2014;63:72–9. [DOI] [PubMed] [Google Scholar]
- 105. Hendriksen C, Binder V.. Social prognosis in patients with ulcerative colitis. Br Med J 1980;281:581–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Binder V, Hendriksen C, Kreiner S.. Prognosis in Crohn’s disease, based on results from a regional patient group from the county of Copenhagen. Gut 1985;26:146–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Nurmi E, Haapamäki J, Paavilainen E, Rantanen A, Hillilä M, Arkkila P.. The burden of inflammatory bowel disease on health care utilization and quality of life. Scand J Gastroenterol 2013;48:51–7. [DOI] [PubMed] [Google Scholar]
- 108. Ghosh S, Mitchell R.. Impact of inflammatory bowel disease on quality of life: results of the European Federation of Crohn’s and Ulcerative Colitis Associations [EFCCA] patient survey. J Crohns Colitis 2007;1:10–20. [DOI] [PubMed] [Google Scholar]
- 109. Stjernman H, Tysk C, Almer S, Ström M, Hjortswang H.. Unfavourable outcome for women in a study of health-related quality of life, social factors and work disability in Crohn’s disease. Eur J Gastroenterol Hepatol 2011;23:671–9. [DOI] [PubMed] [Google Scholar]
- 110. Longobardi T, Jacobs P, Bernstein CN.. Work losses related to inflammatory bowel disease in the United States: results from the National Health Interview Survey. Am J Gastroenterol 2003;98:1064–72. [DOI] [PubMed] [Google Scholar]
- 111. Longobardi T, Jacobs P, Wu L, Bernstein CN.. Work losses related to inflammatory bowel disease in Canada: results from a national population health survey. Am J Gastroenterol 2003;98:844–9. [DOI] [PubMed] [Google Scholar]
- 112. Mayberry MK, Probert C, Srivastava E, Rhodes J, Mayberry JF.. Perceived discrimination in education and employment by people with Crohn’s disease: a case control study of educational achievement and employment. Gut 1992;33:312–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Gazzard BG, Price HL, Libby GW, Dawson AM.. The social toll of Crohn’s disease. Br Med J 1978;2:1117–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Juan J, Estiarte R, Colomé E, Artés M, Jiménez FJ, Alonso J.. Burden of illness of Crohn’s disease in Spain. Dig Liver Dis 2003;35:853–61. [DOI] [PubMed] [Google Scholar]
- 115. Ananthakrishnan AN, Weber LR, Knox JF, et al. Permanent work disability in Crohn’s disease. Am J Gastroenterol 2008;103:154–61. [DOI] [PubMed] [Google Scholar]
- 116. Blomqvist P, Ekbom A.. Inflammatory bowel diseases: health care and costs in Sweden in 1994. Scand J Gastroenterol 1997;32:1134–9. [DOI] [PubMed] [Google Scholar]
- 117. Mesterton J, Jönsson L, Almer SHC, Befrits R, Friis-Liby I, Lindgren S.. Resource use and societal costs for Crohn’s disease in Sweden. Inflamm Bowel Dis 2009;15:1882–90. [DOI] [PubMed] [Google Scholar]
- 118. Reilly MC, Gerlier L, Brabant Y, Brown M.. Validity, reliability, and responsiveness of the work productivity and activity impairment questionnaire in Crohn’s disease. Clin Ther 2008;30:393–404. [DOI] [PubMed] [Google Scholar]
- 119. Yarlas A, Yen L, Hodgkins P.. The relationship among multiple patient-reported outcomes measures for patients with ulcerative colitis receiving treatment with MMX ® formulated delayed-release mesalamine. Qual Life Res 2015;24:671–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Willian MK, D’Haens G, Yarlas A, Joshi AV.. Changes in health-related quality of life and work-related outcomes for patients with mild-to-moderate ulcerative colitis receiving short-term and long-term treatment with multimatrix mesalamine: a prospective, open-label study. J Patient Rep Outcomes 2018;2:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Yarlas A, Willian M, Joshi A.. P456 Impact of short-term and long-term daily therapy with MMX mesalazine on work-related outcomes in patients with mild-to-moderate ulcerative colitis. J Crohns Colitis 2014;8:S256. [Google Scholar]
- 122. West R, Russel M, Bodelier A, et al. Lower risk of recurrence with a higher induction dose of mesalazine and longer duration of treatment in Ulcerative Colitis: results from the Dutch, Non-Interventional, IMPACT Study. J Gastrointestin Liver Dis 2022;31:18–24. [DOI] [PubMed] [Google Scholar]
- 123. Bessissow T, Nguyen GC, Tarabain O, et al. Impact of adalimumab on disease burden in moderate-to-severe ulcerative colitis patients: the one-year, real-world UCanADA study. World J Gastroenterol 2022;28:5058–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. LoftusReinisch EVW, Panaccione R, Berg S, et al. Adalimumab effectiveness up to six years in adalimumab-naïve patients with Crohn’s Disease: results of the PYRAMID Registry. Inflamm Bowel Dis 2019;25:1522–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Travis S, Feagan BG, Peyrin-Biroulet L, et al. Effect of adalimumab on clinical outcomes and health-related quality of life among patients with ulcerative colitis in a clinical practice setting: results from InspirADA. J Crohns Colitis 2017;11:1317–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Louis E, Löfberg R, Reinisch W, et al. Adalimumab improves patient-reported outcomes and reduces indirect costs in patients with moderate to severe Crohn’s disease: results from the CARE trial. J Crohns Colitis 2013;7:34–43. [DOI] [PubMed] [Google Scholar]
- 127. Lichtiger S, Binion DG, Wolf DC, et al. The CHOICE trial: adalimumab demonstrates safety, fistula healing, improved quality of life and increased work productivity in patients with Crohn’s disease who failed prior infliximab therapy. Aliment Pharmacol Ther 2010;32:1228–39. [DOI] [PubMed] [Google Scholar]
- 128. Panaccione R, Loftus EV, Binion D, et al. Efficacy and safety of adalimumab in Canadian patients with moderate to severe Crohn’s disease: results of the Adalimumab in Canadian SubjeCts with ModErate to Severe Crohn’s DiseaSe [ACCESS] trial. Can J Gastroenterol 2011;25:419–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Toruner M, Basaranoglu M, Atug O, et al. Improvement of work productivity and quality of life with anti-tumor necrosis factor treatment used in Crohn’s Disease in Routine Clinical Practice in Turkey. Turk J Gastroenterol 2022;33:406–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Ding Z, Muser E, Hoops T, et al. S723 Improvements in work productivity loss and associated cost reductions with ustekinumab and adalimumab in biologic-naïve patients with moderately-to-severely active Crohn’s Disease: results from the SEAVUE Study. Am J Gastroenterol 2021;116:S330. [Google Scholar]
- 131. Dignass A, Waller J, Cappelleri JC, et al. Living with ulcerative colitis in Germany: a retrospective analysis of dose escalation, concomitant treatment use and healthcare costs. J Med Econ 2020;23:415–27. [DOI] [PubMed] [Google Scholar]
- 132. Feagan BG, Bala M, Yan S, Olson A, Hanauer S.. Unemployment and disability in patients with moderately to severely active Crohn’s disease. J Clin Gastroenterol 2005;39:390–5. [DOI] [PubMed] [Google Scholar]
- 133. Teich N, Bläker M, Holtkamp-Endemann F, Jörgensen E, Stallmach A, Hohenberger S.. Effect of originator infliximab treatment on disease-related hospitalizations, work productivity and activity impairment, and health resource utilization in patients with Crohn’s Disease in a real-life setting: results of a prospective multicenter study in Germany. Inflamm Bowel Dis 2020;6:48–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Perampaladas K, Jones J.. Use of infliximab for inflammatory bowel disease [IBD] within a nationwide case management system: an assessment from the patient’s perspective. Am J Gastroenterol 2013;108:S475. [Google Scholar]
- 135. Gatopoulou A, Christodoulou DK, Katsanos KH, et al. Effect of golimumab on health-related quality of life, other patient-reported outcomes and healthcare resource utilization in patients with moderate-to-severe ulcerative colitis: a real-world multicenter, noninterventional, observational study in Greece. Eur J Gastroenterol Hepatol 2021;33:e615–24. [DOI] [PubMed] [Google Scholar]
- 136. Teich N, Grümmer H, Jörgensen E, et al. Golimumab in real-world practice in patients with ulcerative colitis: twelve-month results. World J Gastroenterol 2020;26:2852–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Feagan BG, Reilly MC, Gerlier L, Brabant Y, Brown M, Schreiber S.. Clinical trial: the effects of certolizumab pegol therapy on work productivity in patients with moderate-to-severe Crohn’s disease in the PRECiSE 2 study. Aliment Pharmacol Ther 2010;31:1276–85. [DOI] [PubMed] [Google Scholar]
- 138. Carlucci C, Lueza B, Colonier AF, et al. S0463 economic costs associated with reduction in work productivity loss for ulcerative colitis patients receiving ustekinumab using results from the UNIFI Clinical Trial. Am J Gastroenterol 2020;115:S233. [Google Scholar]
- 139. D’Haens G, Sandborn W, Zhang W, Kisfalvi K, Wang S, Md PS.. Effects of subcutaneous vedolizumab on health-related quality of life and work productivity in patients with Crohn’s Disease: results from the phase 3 visible 2 study. Gastroenterology 2020;158:S–437. [Google Scholar]
- 140. Danese S, Adsul S, Lindner D, Jones S, Patel H, Colombel JF.. P376 effects of IV vedolizumab on health-related quality of life and work productivity in patients with Crohn’s disease: results from the Phase 3b VERSIFY trial. J Crohns Colitis 2019;13:S293–4. [Google Scholar]
- 141. Ghosh S, Colombel JF, Vermeire S, et al. P0336 Improved patient-reported outcomes with upadacitinib as an induction therapy for patients with Ulcerative Colitis: data from U-Achieve. United Eur Gastroenterol J 2018;6:A240–1. https://onlinelibrary.wiley.com/doi/abs/10.1177/2050640618792819 [Google Scholar]
- 142. Reinisch W, Sandborn WJ, Bala M, et al. Response and remission are associated with improved quality of life, employment and disability status, hours worked, and productivity of patients with ulcerative colitis. Inflamm Bowel Dis 2007;13:1135–40. [DOI] [PubMed] [Google Scholar]
- 143. Cross RK, Naegeli AN, Harrison RW, et al. Disease burden and patient-reported outcomes among Ulcerative Colitis Patients according to therapy at Enrollment Into CorEvitas’ Inflammatory Bowel Disease Registry. Crohn’s & Colitis 360 2022;4:otac007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Neovius M, Arkema EV, Blomqvist P, Ekbom A, Smedby KE.. Patients with ulcerative colitis miss more days of work than the general population, even following colectomy. Gastroenterology 2013;144:536–43. [DOI] [PubMed] [Google Scholar]
- 145. Damgaard B, Wettergren A, Kirkegaard P.. Social and sexual function following ileal pouch-anal anastomosis. Dis Colon Rectum 1995;38:286–9. [DOI] [PubMed] [Google Scholar]
- 146. Wyke RJ, Edwards FC, Allan RN.. Employment problems and prospects for patients with inflammatory bowel disease. Gut 1988;29:1229–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Bryan ML, Bryce AM, Roberts J.. The effect of mental and physical health problems on sickness absence. Eur J Health Econ 2021;22:1519–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Groenewold M, Burrer S, Ahmed F, Uzicanin A.. National surveillance for health-related workplace absenteeism, United States 2017-18. Online J Public Health Inform 2019;11:e398. [Google Scholar]
- 149. Navarro A, Salas-Nicás S, Moncada S, Llorens C, Molinero-Ruiz E.. Prevalence, associated factors and reasons for sickness presenteeism: a cross-sectional nationally representative study of salaried workers in Spain, 2016. BMJ Open 2018;8:e021212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Restall GJ, Simms AM, Walker JR, et al. Understanding Work Experiences of People with Inflammatory Bowel Disease: Inflammatory Bowel Diseases. Inflamm Bowel Dis 2016;22:1688–97. [DOI] [PubMed] [Google Scholar]
- 151. Paulides E, Gearry RB, de Boer NKH, Mulder CJJ, Bernstein CN, McCombie AM.. Accommodations and adaptations to overcome workplace disability in inflammatory bowel disease patients: a systematic review. Inflamm Intest Dis 2018;3:138–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Munir F, Yarker J, Haslam C, et al. Work factors related to psychological and health-related distress among employees with chronic illnesses. J Occup Rehabil 2007;17:259–77. [DOI] [PubMed] [Google Scholar]
- 153. van Linschoten RCA, Visser E, Niehot CD, et al. Systematic review: societal cost of illness of inflammatory bowel disease is increasing due to biologics and varies between continents. Aliment Pharmacol Ther 2021;54:234–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Büsch K, da Silva SA, Holton M, Rabacow FM, Khalili H, Ludvigsson JF.. Sick leave and disability pension in inflammatory bowel disease: a systematic review. J Crohns Colitis 2014;8:1362–77. [DOI] [PubMed] [Google Scholar]
- 155. Argyriou K, Kapsoritakis A, Oikonomou K, Manolakis A, Tsakiridou E, Potamianos S.. Disability in patients with inflammatory bowel disease: correlations with quality of life and patient’s characteristics. Can J Gastroenterol Hepatol 2017;2017:6138105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Bernabéu Juan P, Cabezos Sirvent P, Sempere Robles L, van-der Hofstadt Gomis A, Rodríguez Marín J, van-der Hofstadt Román CJ.. Differences in the quality of life of patients recently diagnosed with Crohn’s disease and ulcerative colitis. Int J Environ Res Public Health 2023;20:6576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Jelsness-Jørgensen LP, Bernklev T, Henriksen M, Torp R, Moum BA.. Chronic fatigue is associated with impaired health-related quality of life in inflammatory bowel disease. Aliment Pharmacol Ther 2011;33:106–14. [DOI] [PubMed] [Google Scholar]
- 158. Romberg-Camps M, Bol Y, Dagnelie P, et al. Fatigue and health-related quality of life in inflammatory bowel disease: results from a population-based study in the Netherlands: the IBD-South Limburg cohort. Inflamm Bowel Dis 2010;16:2137–47. [DOI] [PubMed] [Google Scholar]
- 159. Armuzzi A, Tarallo M, Lucas J, et al. The association between disease activity and patient-reported outcomes in patients with moderate-to-severe ulcerative colitis in the United States and Europe. BMC Gastroenterol 2020;20:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Jackson BD, Con D, Gorelik A, Liew D, Knowles S, De Cruz P.. Examination of the relationship between disease activity and patient-reported outcome measures in an inflammatory bowel disease cohort. Intern Med J 2018;48:1234–41. [DOI] [PubMed] [Google Scholar]
- 161. van Gennep S, Gielen ME, Rietdijk ST, et al. Work productivity loss is determined by fatigue and reduced quality of life in employed inflammatory bowel disease patients: a prospective multicentre cohort study. Eur J Gastroenterol Hepatol 2021;33:e594–602. [DOI] [PubMed] [Google Scholar]
- 162. Radford SJ, McGing J, Czuber-Dochan W, Moran G.. Systematic review: the impact of inflammatory bowel disease-related fatigue on health-related quality of life. Frontline Gastroenterol 2020;12:11–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Pakdin M, Zarei L, Bagheri Lankarani K, Ghahramani S.. The cost of illness analysis of inflammatory bowel disease. BMC Gastroenterol 2023;23:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Kawalec P. Indirect costs of inflammatory bowel diseases: Crohn’s disease and ulcerative colitis. A systematic review. Arch Med Sci 2016;12:295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Nasr S, Dahmani W, Jaziri H, et al. Exploring work productivity loss in patients with inflammatory bowel disease. Future Sci OA 2023;9:FSO872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Chhibba T, Walker JR, Sexton K, et al. Workplace accommodation for persons with IBD: what is needed and what is accessed. Clin Gastroenterol Hepatol 2017;15:1589–95.e4. [DOI] [PubMed] [Google Scholar]
- 167. Cheng L, Jetha A, Cordeaux E, Lee K, Gignac MA.. Workplace challenges, supports, and accommodations for people with inflammatory bowel disease: a scoping review. Disabil Rehabil 2022;44:7587–99. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available and will be shared on reasonable request to the corresponding author.