Abstract
Background
Long-term care (LTC) costs create burdens on aging societies. Maintaining oral health through dental visits may result in shorter LTC periods, thereby decreasing LTC costs; however, this remains unverified. We examined whether dental visits in the past 6 months were associated with cumulative LTC insurance (LTCI) costs.
Methods
This cohort study of the Japan Gerontological Evaluation Study targeted independent adults aged≥65 years in 2010 over an 8-year follow-up. We used data from a self-reported questionnaire and LTCI records from the municipalities. The outcome was cumulative LTCI costs, and exposure was dental visits within 6 months for prevention, treatment, and prevention or treatment. A 2-part model was used to estimate the differences in the predicted cumulative LTCI costs and 95% confidence intervals (CIs) for each dental visit.
Results
The mean age of the 8 429 participants was 73.7 years (standard deviation [SD] = 6.0), and 46.1% were men. During the follow-up period, 17.6% started using LTCI services. The mean cumulative LTCI cost was USD 4 877.0 (SD = 19 082.1). The predicted cumulative LTCI costs were lower among those had dental visits than among those who did not. The differences in predicted cumulative LTCI cost were −USD 1 089.9 (95% CI = −1 888.5 to −291.2) for dental preventive visits, −USD 806.7 (95% CI = −1 647.4 to 34.0) for treatment visits, and −USD 980.6 (95% CI = −1 835.7 to −125.5) for preventive or treatment visits.
Conclusions
Dental visits, particularly preventive visits, were associated with lower cumulative LTCI costs. Maintaining oral health through dental visits may effectively reduce LTCI costs.
Keywords: Epidemiology, Health services, Public health
The demand for long-term care (LTC) services, which are provided to individuals who require assistance with daily living activities owing to chronic illness, disability, or cognitive impairment, has been increasing in aging society (1). In 2021, the total LTC cost in Organization for Economic Co-operation and Development countries comprised 1.8% of the gross domestic product (2). In Japan, where over 28.9% of the population is ≥65 years of age (3), the total medical costs were 44.4 trillion JPY (USD 403.8 billion) in 2019 (4). Moreover, the total expenditure on LTC insurance (LTCI) reached 11.7 trillion JPY (USD 106.4 billion), which was equivalent to a quarter of the total medical costs (5). LTCI services are crucial for preserving the functional capacity of older adults and mitigating the burden on their caregivers (1). Therefore, it is important to minimize the number of individuals requiring LTCI services and reduce related expenditures to ensure the continued availability of LTCI services.
Previous studies suggested oral health as a potential predictor of future LTC needs. Oral health has been associated with the onset of disability (6,7) and even mortality as the final outcome of general health (8,9). Furthermore, oral diseases, such as dental caries and periodontal diseases, can lead to pain and difficulty in eating, smiling, speaking, and socializing (10). Poor oral health is associated with negative health outcomes, such as cardiovascular diseases (11), stroke (11), respiratory infections (12), and cognitive decline (13), which can lead to disability and the need for LTC services (14).
Dental care through clinic visits plays an important role in maintaining oral hygiene and health (15). Individuals who underwent regular dental checkups had low mean decayed-missing-filled tooth surface scores, above-average oral health, and fewer missing teeth (15). Recently, dental visits have been reported to reduce the risk of acute hospitalization owing to systemic diseases (16) and to decrease the risk of LTC requirement (17).
Maintaining good oral health through dental visits may indirectly prevent the need for LTCI services, and consequently decrease LTCI costs. Previous studies have reported an association between better oral health and lower expenditures on healthcare services (18,19). As existing knowledge of costs is limited, investigating the relationship between dental visits and LTCI costs in one of the world’s most aged countries is critical for the improvement and maintenance of the LTCI system. Therefore, we examined whether dental visits within the past 6 months were associated with cumulative LTCI costs in the subsequent 8 years among Japanese older adults. We hypothesized that the LTCI costs would be lower for those who visited dental clinics than for those who did not.
Materials and Methods
Study Design and Population
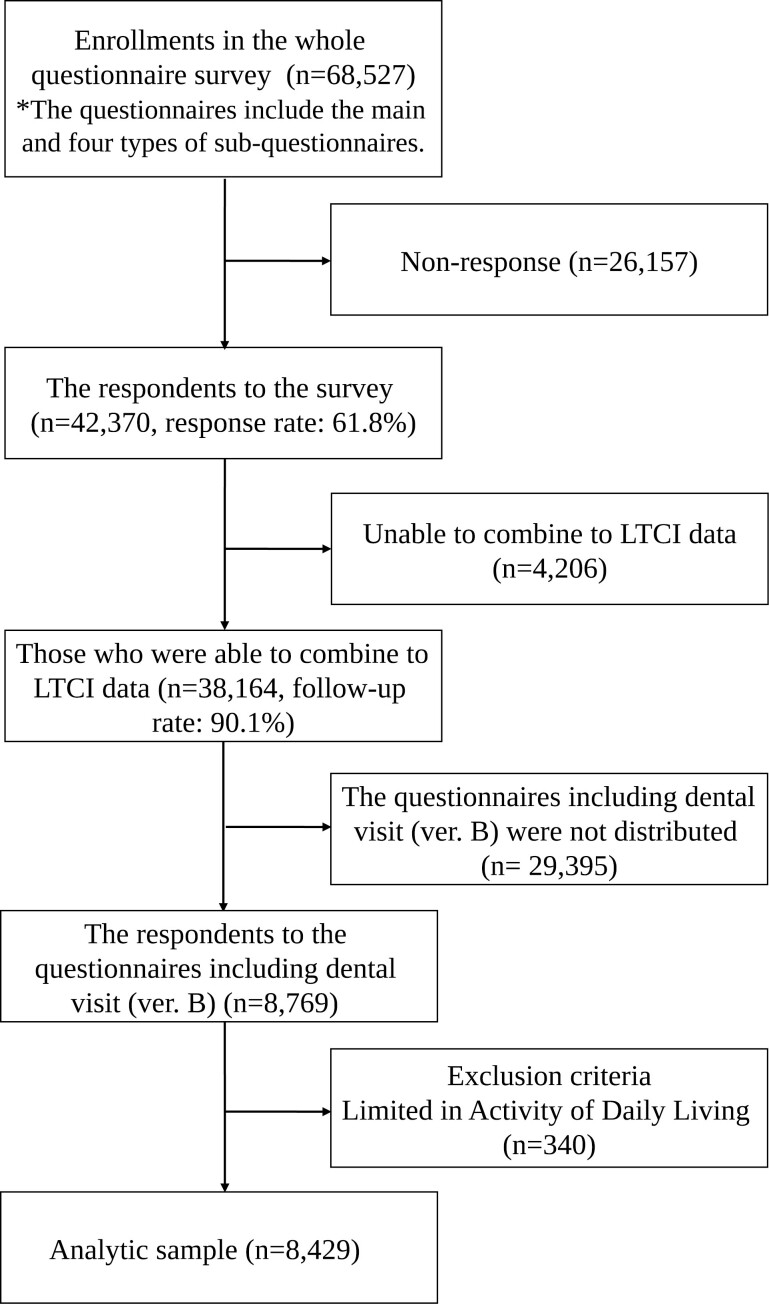
This 8-year follow-up cohort study using the Japan Gerontological Evaluation Study (JAGES) targeted physically and cognitively independent older adults aged ≥65 years, who were not considered eligible for LTCI services at baseline (20). The JAGES is an ongoing long-term cohort study conducted in Japan since 2010 (21). Among the total participants, we targeted those from 7 municipalities in Japan that were connected to LTCI data. In the 2 larger municipalities, the JAGES was conducted with residents through sampling, whereas in the other smaller municipalities, a survey was administered to the entire population. A summary of the surveys for each municipality is shown in Supplementary Table 1. Overall, the self-report questionnaire was distributed to 68 527 participants between August 2010 and January 2012, with a response rate of 61.8% (N = 42 370). Among the respondents, LTCI data obtained from municipalities were available for 38 164 participants after excluding untraceable cases such as out-migrants (follow-up rate: 90.1%). The JAGES questionnaire contained a main questionnaire and 4 sub-questionnaires. The main questionnaire included demographic and basic information. One of the sub-questionnaires, ver. B, included a questionnaire on dental visits. The response rates for each sub-questionnaire did not differ substantially (data not shown). Each of the 4 sub-questionnaires was randomly distributed to one-quarter of the population in each municipality. We targeted participants who completed a questionnaire related to their dental visits and were independent at baseline (n = 8 429). Figure 1 shows a flowchart of the sampling method.
Figure 1.
Flowchart of the participants for the analysis. Note. The questions related to dental visits were only included in ver. B of JAGES questionnaire.
Outcome Variable
The cumulative LTCI cost over 8 years (August 2010 to February 2018, 91 months) was used as the outcome variable. Data on LTCI costs were obtained for each municipality. The LTCI system was introduced in Japan in the year 2000 (1), and all Japanese adults aged ≥65 years are eligible for LTCI certification based on examination by an investigator and the opinion of a family doctor (5). The assessment determines the level of care required and the benefits are determined according to this level. In principle, all eligible people who use these services must pay 10% of the cost (1). In addition, LTCI services include in-home services (home visits and day services such as nursing care, bathing, rehabilitation, and home repair expenses) and facility services (costs at geriatric health service facilities and nursing homes) (22). We used the cumulative LTCI cost over 8 years because LTCI costs differ seasonally (23). Total monthly LTCI costs were calculated and used in the analysis.
Exposure Variables
The exposure variables were dental preventive and treatment visits within the last 6 months, as reported at baseline. A period of 6 months was selected because it accounts for recall bias (24), and a substantial percentage of the sample was expected to have visited dental clinics in the preceding 6 months in Japan (25). For preventive dental visits, we asked the participants, “Within the past 6 months, have you visited a dentist for ‘non-treatment’ purposes (eg, checkups)?” For dental treatment visits, we asked, “Within the past 6 months, have you visited a dentist for ‘treatment’ (including adjustment of dentures)?” The responses for both were recorded as “yes/no.” We also used the combined variable of dental preventive visit or dental treatment visit, wherein “yes” was the response to having received dental treatment or dental preventive treatment in the previous 6 months.
Covariates
According to the existing knowledge and studies related to oral health or dental visit and LTC or onset of disability (6,26), we used the following factors, obtained at baseline, as covariates: sex (men/women), age (65–69/70–74/75–79/80–84/≥85 years), number of teeth (≥20/10–19/1–9/0 teeth), marital status (no partner/having partner), body mass index (BMI) (<18.5/18.5–24.9/≥25.0), education level (<9/10–12/≥13 years), equivalent household income (<1.00/1.00–1.99/2.00–2.99/3.00–3.99/≥4.00 million JPY), walking time (<30/30–59/60–89/≥90 min), drinking status (current/past/ never), smoking status (current/past/never), depression (<5/5–9/≥10), absence of medical history (hypertension/diabetes/cancer/stroke/heart disease), medical checkup (within a year/within 2–3 years/>4 years/none), and region (seven municipalities). Equivalent household income was calculated by dividing household income by the number of household members. Depression was assessed using the Geriatric Depression scale (27). We included the medical checkup variable as a covariate, indicating a proxy for health-seeking behaviors. The regions were adjusted because LTCI costs and access to dental clinics may vary by area.
Statistical Analysis
A 2-part model was used to analyze the cumulative LTCI costs for each type of dental visit, considering that the distribution of cumulative LTCI costs was skewed to the right with a total of 82.4% of participants having zero costs (28). In the first part, we applied the logit model to calculate the odds ratios (ORs) and 95% confidence intervals (CIs) to define the probability of LTCI costs being greater than zero. In the second part, we applied a generalized linear model (GLM) with gamma distribution and a log-link function to calculate the relative cost ratios (RCRs) and 95% CIs of LTCI costs by type of dental visit among people with LTCI costs greater than zero. RCR is the exponential regression coefficient of the GLM with a gamma distribution and a log-link function (29). We used the “twopm” Stata command for the analysis (30). Furthermore, we calculated the predicted cumulative LTCI costs and the differences in the predicted cumulative LTCI costs based on dental preventive visits, dental treatment visits, and dental preventive or treatment visits (31). Bootstrap resampling with 1 000 replications was used to calculate CIs (30). For statistical modeling, we adjusted for sex and age in Model 1. In Model 2, we included the number of teeth, marital status, BMI, education level, income, walking time, drinking status, smoking status, depression, history of hypertension, diabetes, cancer, stroke, heart disease, medical checkups, and region, in addition to the variables included in Model 1.
Several sensitivity analyses were conducted to confirm the robustness of the results. First, we conducted stratified analyses by using ≥20 teeth as the number of teeth known to be required for LTCI eligibility (6,7). Second, we conducted an analysis that excluded edentulous participants. Third, we performed propensity score matching to calculate the average treatment effect of dental visits on LTCI costs. We carried out the nearest neighbor matching for the dental visit group and the non-dental visit group, with a caliper value of 0.2 of the standard deviation (SD) of the propensity score logit without replacement. For the analysis, the “psmatch2” Stata command was used. Fourth, a competing risk regression analysis using the Fine and Gray model (32) was performed, with the initiation of LTCI use as the first outcome and all-cause mortality as a competing risk event. The “stccreg” Stata command was applied.
To reduce selection bias owing to missing values, we applied random forest imputation using the R package “missForest” for missing values of exposure variables and covariates (33). “missForest” is the package using the random forest algorithm which is a non-parametric imputation approach. They do not require any assumption for the distribution of data and allow to impute of the mixed variable types (continuous, binary, and categorical). Stata 17.0 (Stata Corporation LP, Windows version) and R (version 4.2.3, Windows) were used for the statistical analyses. We calculated costs by converting JPY 100 to USD 1.00. The significance level was set at p < .05. This study followed the STROBE reporting guidelines.
Ethical Approval
This study was approved by the Ethics Committee on the Research of Human Subjects at Chiba University (approval number: 2493). All participants provided informed consent before participating in the study.
Results
Descriptive characteristics are shown in Table 1. This analysis included 8 429 participants with a mean age of 73.7 years (SD = 6.0) at baseline (range: 65–100 years), of which 3 883 (46.1%) were men. The mean cumulative LTCI cost per participant from 2010 to 2018 was USD 4 877.0 (SD = 19 082.1). During the 8-year follow-up period, 1 487 (17.6%) started using LTCI services and 1 093 (13.0%) died. The mean LTCI service period was 4.5 months (SD = 13.2). Of the total respondents, 35.9%, 52.4%, and 56.3% had dental preventive visits, treatment visits, and preventive or treatment visits, respectively. We found that women, individuals with no dental visits, older age, fewer teeth, lower income, lower education level, no partners, lower BMI, shorter walking time, comorbidities other than hypertension, and those not undergoing medical checkups were more likely to use LTCI services. Descriptive characteristics of the participants with missing values are presented in Supplementary Table 2. There was a relatively higher missingness in the income and comorbidity variables. The characteristics stratified by dental visits are shown in Supplementary Table 3. Characteristics stratified by death are shown in Supplementary Table 4.
Table 1.
Demographic Characteristics of the Study Sample According to the Use of Long-Term Care Insurance Services After Imputation (n = 8 429)
| Using LTCI Services | |||||
|---|---|---|---|---|---|
| Total | No | Yes | |||
| n (%a) | %b | %b | p Valuec | ||
| Dental preventive visit | No | 5 401 (64.1) | 81.5 | 18.5 | .007 |
| Yes | 3 028 (35.9) | 83.9 | 16.1 | ||
| Dental treatment visit | No | 4 013 (47.6) | 80.8 | 19.2 | <.001 |
| Yes | 4 416 (52.4) | 83.8 | 16.2 | ||
| Dental preventive or treatment visit | No | 3 680 (43.7) | 79.9 | 20.1 | <.001 |
| Yes | 4 749 (56.3) | 84.2 | 15.8 | ||
| Sex | Men | 3 883 (46.1) | 83.8 | 16.2 | .001 |
| Women | 4 546 (53.9) | 81.1 | 18.9 | ||
| Age | 65–69 | 2 555 (30.3) | 94.8 | 5.2 | <.001 |
| 70–74 | 2 477 (29.4) | 91.3 | 8.7 | ||
| 75–79 | 1 880 (22.3) | 76.2 | 23.8 | ||
| 80–84 | 1 033 (12.3) | 59.3 | 40.7 | ||
| ≥85 | 484 (5.7) | 44.4 | 55.6 | ||
| Number of teeth | ≥20 teeth | 3 212 (38.1) | 87.5 | 12.5 | <.001 |
| 10–19 teeth | 2 238 (26.6) | 83.9 | 16.1 | ||
| 1–9 teeth | 2 055 (24.4) | 78.2 | 21.8 | ||
| 0 teeth | 924 (11.0) | 70.3 | 29.7 | ||
| Marital status | No partner | 2 354 (27.9) | 74.4 | 25.6 | <.001 |
| Having partner | 6 075 (72.1) | 85.4 | 14.6 | ||
| BMI | <18.5 | 599 (7.1) | 75.1 | 24.9 | <.001 |
| 18.5–24.9 | 6 069 (72.0) | 82.7 | 17.3 | ||
| ≥25.0 | 1 761 (20.9) | 83.7 | 16.3 | ||
| Education level | <9 years | 3 622 (43.0) | 79.1 | 20.9 | <.001 |
| 10–12 years | 3 197 (37.9) | 84.0 | 16.0 | ||
| ≥13 years | 1 610 (19.1) | 86.3 | 13.7 | ||
| Income (Million yen) | <1.00 | 1 367 (16.2) | 74.3 | 25.7 | <.001 |
| 1.00–1.99 | 2 814 (33.4) | 83.8 | 16.2 | ||
| 2.00–2.99 | 1 973 (23.4) | 83.5 | 16.5 | ||
| 3.00–3.99 | 1 272 (15.1) | 85.2 | 14.8 | ||
| ≥4.00 | 1 003 (11.9) | 83.4 | 16.6 | ||
| Walking time | <30 min | 2 895 (34.3) | 75.7 | 24.3 | <.001 |
| 30–59 min | 2 925 (34.7) | 83.5 | 16.5 | ||
| 60–89 min | 1 302 (15.4) | 85.3 | 14.7 | ||
| ≥90 min | 1 307 (15.5) | 91.5 | 8.5 | ||
| Drinking status | Current | 3 090 (36.7) | 87.3 | 12.7 | <.001 |
| Past | 265 (3.1) | 80.8 | 19.2 | ||
| Never | 5 074 (60.2) | 79.4 | 20.6 | ||
| Smoking status | Current | 929 (11.0) | 81.2 | 18.8 | <.001 |
| Past | 2 417 (28.7) | 85.2 | 14.8 | ||
| Never | 5 083 (60.3) | 81.2 | 18.8 | ||
| Depression (Geriatric Depression scale) | <5 | 6 031 (71.6) | 84.5 | 15.5 | <.001 |
| 5–9 | 1 778 (21.1) | 78.0 | 22.0 | ||
| ≥10 | 620 (7.4) | 73.9 | 26.1 | ||
| Hypertension | No | 4 036 (47.9) | 81.7 | 18.3 | .153 |
| Yes | 4 393 (52.1) | 82.9 | 17.1 | ||
| Diabetes | No | 7 289 (86.5) | 82.8 | 17.2 | .010 |
| Yes | 1 140 (13.5) | 79.6 | 20.4 | ||
| Cancer | No | 8 062 (95.6) | 82.6 | 17.4 | .007 |
| Yes | 367 (4.4) | 77.1 | 22.9 | ||
| Stroke | No | 8 333 (98.9) | 82.5 | 17.5 | .030 |
| Yes | 96 (1.1) | 74.0 | 26.0 | ||
| Heart diseases | No | 7 403 (87.8) | 83.2 | 16.8 | <.001 |
| Yes | 1 026 (12.2) | 76.3 | 23.7 | ||
| Medical checkup | Within a year | 5 314 (63.0) | 84.4 | 15.6 | <.001 |
| Within 2–3 years | 968 (11.5) | 83.2 | 16.8 | ||
| ≥4 years | 822 (9.8) | 79.7 | 20.3 | ||
| None | 1 325 (15.7) | 75.3 | 24.7 | ||
| Regions | A | 1 103 (13.1) | 77.2 | 22.8 | <.001 |
| B | 552 (6.5) | 86.2 | 13.8 | ||
| C | 773 (9.2) | 84.9 | 15.1 | ||
| D | 2 635 (31.3) | 84.7 | 15.3 | ||
| E | 846 (10.0) | 81.4 | 18.6 | ||
| F | 1 545 (18.3) | 80.8 | 19.2 | ||
| G | 975 (11.6) | 81.0 | 19.0 | ||
| Total | 8 429 (100.0) | 82.4 | 17.6 | ||
Notes: BMI = body mass index; LTCI = long-term care insurance.
aColumn percentage.
bRow percentage.
cPearson’s χ2 test.
Table 2 shows the mean duration of LTCI service use and the cumulative LTCI cost attributed to dental visits. The cumulative LTCI cost was higher among those not having any dental visits than among those who did, and the difference in the mean cumulative LTCI cost was higher for dental preventive visits than for dental treatment visits (USD 1 406.2 vs 1 311.9). Those who had no dental visits used the LTCI services for a longer period.
Table 2.
Mean duration of using long-term care insurance services and cumulative long-term care insurance costs during the 8-year follow-up period by dental visit among Japanese older adults after imputation (n = 8 429)
| Use of LTCI Services (months) | Cumulative LTCI Cost (USD) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Dental Visit | n | Mean | SD | Difference | p Value | Mean | SD | Difference | Median (IQR) | p Value | |
| Dental preventive visit | No | 5,401 | 4.7 | 13.5 | 0.6 | .007 | 5,382.2 | 20,383.8 | 1,406.2 | 0 (0–0) | .004 |
| Yes | 3,028 | 4.1 | 12.7 | 3,976.0 | 16,472.4 | ||||||
| Dental treatment visit | No | 4,013 | 4.9 | 13.6 | 0.7 | <.001 | 5,564.3 | 20,625.9 | 1,311.9 | 0 (0–0) | <.001 |
| Yes | 4,416 | 4.2 | 12.8 | 4,252.5 | 17,541.0 | ||||||
| Dental preventive or treatment visit | No | 3,680 | 5.1 | 13.8 | 1.0 | <.001 | 5,847.4 | 21,137.9 | 1,722.2 | 0 (0–0) | <.001 |
| Yes | 4,749 | 4.1 | 12.7 | 4,125.1 | 17,287.0 | ||||||
| Total | 8,429 | 4.5 | 13.2 | 4,877.0 | 19,082.1 | ||||||
Notes: IQR = interquartile range; LTCI = long-term care insurance; SD = standard deviation.
1 USD ≈ JPY 100.
p value was calculated by Wilcoxon rank-sum test.
Table 3 shows the results of the multivariate regression analysis. In the first part of the 2-part model, having preventive or treatment visits within the past 6 months was associated with the use of LTCI services after considering all covariates (OR = 0.86, 95% CI = 0.76–0.98). Dental preventive visits and dental treatment visits also show similar trends (preventive visit: OR = 0.95, 95% CI = 0.83–1.08 and treatment visit: OR = 0.89, 95% CI = 0.78–1.01); however, they were not statistically significant. In the second part, having preventive dental visits within the past 6 months was significantly associated with lower cumulative LTCI costs (RCR = 0.82, 95% CI = 0.71–0.95). Although not statistically significant, having a treatment visit and a preventive or treatment visit exhibited a similar trend (treatment visit: RCR = 0.91, 95% CI = 0.79–1.06 and preventive or treatment visit: RCR = 0.90, 95% CI = 0.78–1.04).
Table 3.
Association Between Dental Visits and Cumulative Long-Term Care Insurance Costs During the 8-Year Follow-Up Period Among Japanese Older Adults (n = 8 429)
| Model 1 | Model 2 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First Part | Second Part | First Part | Second Part | ||||||||||
| OR | 95%CI | p Value | RCR | 95%CI | p Value | OR | 95%CI | p Value | RCR | 95%CI | p Value | ||
| Dental preventive visit (Ref. No) | Yes | 0.91 | (0.80–1.04) | .169 | 0.84 | (0.72–0.98) | .025 | 0.95 | (0.83–1.08) | .435 | 0.82 | (0.71–0.95) | .009 |
| Dental treatment visit (Ref. No) | Yes | 0.85 | (0.75–0.96) | .011 | 0.92 | (0.79–1.06) | .242 | 0.89 | (0.78–1.01) | .072 | 0.91 | (0.79–1.06) | .228 |
| Dental preventive or treatment visit (Ref. No) | Yes | 0.82 | (0.73–0.93) | .002 | 0.90 | (0.78–1.04) | .155 | 0.86 | (0.76–0.98) | .023 | 0.90 | (0.78–1.04) | .162 |
Model 1: Sex and age adjusted.
Model 2: Adjusted for number of teeth, marital status, BMI, education level, income, walking time, drinking status, smoking status, depression, hypertension, diabetes, cancer, stroke, heart diseases, medical checkup, and regions in addition to model 1.
Notes: BMI = body mass index; CI = confidence interval; OR = odds ratio; RCR = relative cost ratio.
From the calculation of the mean cost difference (USD) for each dental visit (Table 4), the predicted cumulative LTCI cost was lower among those who had dental visits in the past 6 months than among those who did not. The differences in predicted cumulative LTCI cost were −USD 1 089.9 (95% CI = −1 888.5 to −291.2) for dental preventive visit, −USD 806.7 (95% CI = −1 647.4 to 34.0) for dental treatment visit, and −USD 980.6 (95% CI = −1 835.7 to −125.5) for dental preventive or treatment visit.
Table 4.
Predictive Cumulative Long-Term Care Insurance Costs During the 8-Year Follow-Up Period by Dental Visit Among Japanese Older Adults (n = 8 429)
| Predictive Estimate of LTCI Cost (USD) | 95%CI | Difference of LTCI Cost (USD) | 95%CI | p Value | ||
|---|---|---|---|---|---|---|
| Dental preventive visit | No | 5 250.3 | (4 720.8–5 779.9) | Ref | ||
| Yes | 4 160.4 | (3 570.3–4 750.5) | −1 089.9 | (−1 888.5 to −291.2) | .007 | |
| Dental treatment visit | No | 5 283.6 | (4 668.3–5 899.0) | Ref | ||
| Yes | 4 476.9 | (3 935.0–5 018.8) | −806.7 | (−1 647.4–34.0) | .060 | |
| Dental preventive or treatment visit | No | 5 397.8 | (4 751.4–6 044.3) | Ref | ||
| Yes | 4 417.2 | (3 893.4–4 941.1) | −980.6 | (−1 835.7 to −125.5) | .025 |
Adjusted for sex, age, number of teeth, marital status, BMI, education level, income, walking time, drinking status, smoking status, depression, hypertension, diabetes, cancer, stroke, heart diseases, medical checkup, and regions.
Notes: CI = confidence interval; LTCI = long-term care insurance; Ref = Reference.
1 USD ≈ JPY 100.
In the sensitivity analysis, the stratified analyses (having ≥ 20/0–19 teeth) revealed a tendency similar to that of the main analysis (Supplementary Tables 5–7). The difference in the cumulative LTCI cost was largest for preventive dental visits among those with ≥20 teeth (−USD 1 309.8, 95% CI = −2 574.4 to −45.2). Analyses targeting only individuals with teeth revealed a similar tendency (Supplementary Tables 8 and 9). The analysis using propensity score matching also revealed a tendency similar to that of the main analysis (Supplementary Table 10). In the analysis considering death as a competing risk, the results showed similar trends to those in the first part of the 2-part model (Supplementary Table 11).
Discussion
Our study revealed that dental visits, especially preventive dental visits in the past 6 months were associated with lower cumulative LTCI costs. The predicted cumulative LTCI cost was USD 980.6 lower among those with any dental visit in the preceding 6 months. Specifically, the predicted cumulative LTCI cost was USD 1 089.9 lower among those with preventive dental visits. These results provide important insights for policymakers on how to sustain the LTCI system from an oral health perspective.
Our finding that dental visits are associated with lower LTCI costs is supported by the results of previous studies. Another study that used the same cohort data as ours reported that deterioration of oral function was associated with LTCI cost (34). Dental visits are associated with a lower onset of severe disabilities (17), which often require LTCI services. Our findings are consistent with the results of these studies, as dental visits reportedly have a protective effect on oral function by preventing tooth loss, and LTCI costs reflect LTCI utilization.
There are several possible explanations for these results. First, dental visits can help to prevent or identify oral health problems at an early stage. Early detection and treatment can prevent the development of more severe conditions, such as tooth loss or chewing difficulty (17), which could lead to disability (6). Second, regular dental visits, an important factor in maintaining better oral health (15), could encourage social relationships. People who have better oral health and use dental prostheses have better social relationships (35), which in turn, can help improve their overall well-being and quality of life and reduce the LTC burden (22).
In fact, our results in the first part of the 2-part model showed that any dental visit within the past 6 months was associated with LTCI use. Particularly for dental treatment, maintaining and improving chewing ability through dental prosthesis treatment may lead to having social relationships and thus prevent the initiation of LTC (35,36). In the second part of our 2-part model, the estimates showed that a lack of preventive dental visits was associated with higher LTCI costs. Preventive dental visits may have contributed to good oral health, including the prevention of periodontal disease, resulting in a reduced incidence of systemic diseases and minimized LTCI costs. Periodontal disease has been reported to be associated with the development of heart disease (37) and stroke (38). Furthermore, periodontal disease and tooth loss have also been associated with an increased risk of cognitive decline (39). These diseases are the leading causes of higher LTCI costs (40). However, the mechanisms underlying the relationship between LTCI costs and dental visits for treatment and prevention require further investigation.
With regard to public health implications, these findings provide important insights into LTCI costs. As of 2021, the number of adults aged ≥65 years in Japan was 36.2 million (41). Based on the current results, it is estimated that 15.8 million (43.7%) older adults have not visited dental clinics in the last 6 months. The difference in LTCI costs at 91 months between those without versus with dental visits was USD 980.6 per person—or, USD 15.5 billion when aggregated over 15.8 million people (that is, approximately USD 2.0 billion per 15.8 million person-years). This equates to 1.8% of the total LTCI expenditure in Japan in 2021 of USD 112.9 billion (20).
In addition, Universal Health Coverage (UHC) has been promoted worldwide (42), and the achievement of an environment where all individuals have access to preventive dental visits within their budgets should be encouraged to achieve healthy longevity and reduce LTCI costs. A previous systematic review reported differences in dental visits among countries (43,44); hence, affordable access to dental care should be offered. In Japan, UHC covers almost all dental treatments, and 30% of the out-of-pocket expenditures for dental treatment are required (45). In 2022, the Japanese government announced the aim of implementing a “universal oral health check” as part of its basic policy for the Japanese people (46). However, treatment-oriented systems for dental care are still common in Japan, and inequalities in preventive dental care remain (44). Our study showed that the relative LTCI cost ratio was low among those with preventive dental visits, suggesting that promoting preventive dental visits through UHC may reduce LTCI costs. These findings indicate that maintaining oral health through dental visits may help reduce LTCI service costs. Future research investigating the detailed underlying mechanisms of this association and the potential cost savings associated with regular dental visits for the healthcare system is warranted.
Strengths and Limitations
This study has some limitations. First, medical care costs were not considered. Future studies should conduct cost-effectiveness analyses from the perspective of medical and LTCI expenses. Second, we cannot deny the possibility that participants may have received the state of care they required before their oral conditions worsened. Furthermore, people with limited activities of daily living may be unable to make dental visits, tend to have LTCI certification delays, or refrain from using LTCI services. However, we included older adults who were independent at baseline in the analysis, and considered their baseline physical activity. Third, dental visits may indicate higher health literacy and favorable lifestyle habits, which might work as an unmeasured confounding factor; therefore, we cannot rule out the possibility of residual confounding. However, we considered medical checkups, smoking status, and drinking status as proxy variables. Fourth, self-reported exposure variables and covariates were used. Therefore, we cannot deny the effect of recall bias. In particular, for dental visits, future studies using objective measurements, such as receipt data, are needed to supplement information on the details of dental treatments. Fifth, the response rate of the study participants was not high (61.8%). Therefore, we cannot rule out the possibility of bias in the inclusion of healthier individuals in the target population. Therefore, caution should be needed with generalizability. Sixth, there were relatively higher missing values such as income (17.3%) and comorbidities (23.2%) as our covariates were self-reported. However, we imputed them to reduce the selection bias. Finally, deaths preceding LTCI were not considered in the main analysis. When a competing risk model was performed as a sensitivity analysis, with LTCI use as the primary outcome and death as the secondary outcome, the results showed trends similar to our results in the first part of the 2-part model. Conversely, those who died before the start of LTC were mostly in the non-dental visit group, and their LTCI costs were estimated to be zero. A possible reason could be that poor dental visit behavior was associated with an increased risk of mortality (47). Therefore, the present analysis may have underestimated the difference in LTCI costs between the groups with and without dental visits.
This study has several strengths. First, this is the first study to investigate the association between dental visits and cumulative LTCI costs using a large community-based study that includes small and large municipalities in Japan, the most aged country in the world. These findings will be useful to policymakers in aging countries. Second, we used public claim records regarding LTCI services obtained from municipalities with relatively higher follow-up rates (90.1%). This enabled us to analyze LTCI cost data with a lower bias compared to surveys that asked respondents about LTCI use.
Conclusion
Dental preventive and treatment visits within the past 6 months were associated with lower cumulative LTCI costs over the subsequent 8 years. Our findings suggest that maintaining oral health through dental visits can effectively reduce LTCI costs.
Supplementary Material
Contributor Information
Sakura Kiuchi, Frontier Research Institute for Interdisciplinary Sciences, Tohoku University, Aoba-ku, Sendai, Japan; Department of International and Community Oral Health, Tohoku University Graduate School of Dentistry, Aoba-ku, Sendai, Japan.
Kenji Takeuchi, Department of International and Community Oral Health, Tohoku University Graduate School of Dentistry, Aoba-ku, Sendai, Japan; Division of Statistics and Data Science, Liaison Center for Innovative Dentistry, Tohoku University Graduate School of Dentistry, Aoba-ku, Sendai, Japan.
Masashige Saito, Faculty of Social Welfare, Nihon Fukushi University, Mihama, Aichi, Japan; Center for Well-Being and Society, Nihon Fukushi University, Nagoya, Aichi, Japan.
Taro Kusama, Department of International and Community Oral Health, Tohoku University Graduate School of Dentistry, Aoba-ku, Sendai, Japan; Division of Statistics and Data Science, Liaison Center for Innovative Dentistry, Tohoku University Graduate School of Dentistry, Aoba-ku, Sendai, Japan.
Noriko Nakazawa, Department of International and Community Oral Health, Tohoku University Graduate School of Dentistry, Aoba-ku, Sendai, Japan.
Kinya Fujita, Department of Gerontological Evaluation, Center for Gerontology and Social Science, Research Institute, National Center for Geriatrics and Gerontology, Obu, Aichi, Japan.
Katsunori Kondo, Department of Gerontological Evaluation, Center for Gerontology and Social Science, Research Institute, National Center for Geriatrics and Gerontology, Obu, Aichi, Japan; Department of Social Preventive Medical Sciences, Center for Preventive Medical Sciences, Chiba University, Inage-ku, Chiba, Chiba, Japan.
Jun Aida, Department of Oral Health Promotion, Tokyo Medical and Dental University, Bunkyo-ku, Tokyo, Japan.
Ken Osaka, Department of International and Community Oral Health, Tohoku University Graduate School of Dentistry, Aoba-ku, Sendai, Japan.
Funding
This study was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI (18H00953, 19H03861, 19H03860, 22H03299, 22K20984, 23H00060, 23K24557, and 23H03117) and the Japan Agency for Medical Research and Development (AMED) (19dk0110037h0001). The baseline survey was conducted as a part of the Japan Gerontological Evaluation Study (JAGES). This survey was supported by JSPS (Japan Society for the Promotion of Science) KAKENHI (grant number 15H01972), Health Labour Sciences Research Grant (H28-Choju-Ippan-002), Japan Agency for Medical Research and Development (AMED) (JP18dk0110027, JP18ls0110002, JP18le0110009, JP20dk0110034, JP21lk0310073, JP21dk0110037, JP22lk0310087), Open Innovation Platform with Enterprises, Research Institute and Academia (OPERA, JPMJOP1831), a grant from Innovative Research Program on Suicide Countermeasures (1–4), a grant from Sasakawa Sports Foundation, a grant from Japan Health Promotion & Fitness Foundation, a grant from Chiba Foundation for Health Promotion & Disease Prevention, the 8020 Research Grant for fiscal 2019 from the 8020 Promotion Foundation (adopted number: 19-2-06), grants from Meiji Yasuda Life Foundation of Health and Welfare and the Research Funding for Longevity Sciences from National Center for Geriatrics and Gerontology (29–42).
Conflict of Interest
None.
Data Availability
Data were obtained from the JAGES study. All inquiries will be addressed by the Data Management Committee via e-mail: dataadmin.ml@jages.net. All JAGES datasets have ethical or legal restrictions for public deposition, owing to the inclusion of sensitive information from human participants.
Author Contributions
S.K.: Conceptualization, Formal analysis, Investigation, Methodology, Writing of the original draft. K.T.: Conceptualization, Investigation, Methodology, Supervision. T.K. and N.N.: Investigation, Methodology. M.S., K.F., K.K., J.A., K.O.: Data curation, Funding acquisition, and Project administration. All authors: validation, writing, review, editing, and approval of the final manuscript.
Ethical Approval Statement
The JAGES and its follow-up survey followed the procedures approved by the Ethics Committee on Research of Human Subjects at Chiba University (No. 2943).
Patient Consent Statement
Informed consent was obtained from all participants.
References
- 1. Ikegami N. Financing long-term care: lessons from Japan. Int J Health Policy Manag. 2019;8(8):462–466. 10.15171/ijhpm.2019.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. OECD. Health at a Glance 2023: OECD Indicators. Paris: OECD Publishing; 2023. 10.1787/7a7afb35-en. [DOI] [Google Scholar]
- 3. Japan Cabinet Office. White paper on aging society 2022; 2022. https://www8.cao.go.jp/kourei/whitepaper/w-2022/zenbun/04pdf_index.html. Accessed December 10, 2022. [Google Scholar]
- 4. Ministry of Health, Labour and Welfare. Handbook of health and welfare statistics 2021; 2021. https://www.mhlw.go.jp/english/database/db-hh/5-1.html. Accessed January 6, 2023. [Google Scholar]
- 5. Yamada M, Arai H.. Long-term care system in Japan. Ann Geriatr Med Res. 2020;24(3):174–180. 10.4235/agmr.20.0037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Komiyama T, Ohi T, Tomata Y, et al. Dental status is associated with incident functional disability in community-dwelling older Japanese: a prospective cohort study using propensity score matching. J Epidemiol. 2020;30(2):84–90. 10.2188/jea.JE20180203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maekawa K, Ikeuchi T, Shinkai S, et al. ; Kusatsu ISLE Study Working Group Collaborators. Impact of number of functional teeth on independence of Japanese older adults. Geriatr Gerontol Int. 2022;22(12):1032–1039. 10.1111/ggi.14508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Peng J, Song J, Han J, et al. The relationship between tooth loss and mortality from all causes, cardiovascular diseases, and coronary heart disease in the general population: systematic review and dose-response meta-analysis of prospective cohort studies. Biosci Rep. 2019;39(1). 10.1042/BSR20181773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kusama T, Takeuchi K, Kiuchi S, Aida J, Kondo K, Osaka K.. Weight loss mediated the relationship between tooth loss and mortality risk. J Dent Res. 2023;102(1):45–52. 10.1177/00220345221120642 [DOI] [PubMed] [Google Scholar]
- 10. Peres MA, Macpherson LMD, Weyant RJ, et al. Oral diseases: a global public health challenge. Lancet. 2019;394(10194):249–260. 10.1016/S0140-6736(19)31146-8 [DOI] [PubMed] [Google Scholar]
- 11. Cheng F, Zhang M, Wang Q, et al. Tooth loss and risk of cardiovascular disease and stroke: a dose-response meta analysis of prospective cohort studies. PLoS One. 2018;13(3):e0194563. 10.1371/journal.pone.0194563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Son M, Jo S, Lee JS, Lee DH.. Association between oral health and incidence of pneumonia: a population-based cohort study from Korea. Sci Rep. 2020;10(1):9576. 10.1038/s41598-020-66312-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Qi X, Zhu Z, Plassman BL, Wu B.. Dose-response meta-analysis on tooth loss with the risk of cognitive impairment and dementia. J Am Med Dir Assoc. 2021;22(10):2039–2045. 10.1016/j.jamda.2021.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. GBD 2019 Ageing Collaborators. Global, regional, and national burden of diseases and injuries for adults 70 years and older: systematic analysis for the Global Burden of Disease 2019 Study. BMJ. 2022;376:e068208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Thomson WM, Williams SM, Broadbent JM, Poulton R, Locker D.. Long-term dental visiting patterns and adult oral health. J Dent Res. 2010;89(3):307–311. 10.1177/0022034509356779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mitsutake S, Ishizaki T, Edahiro A, Kitamura A, Hirata T, Saito A.. The effects of dental visits on the occurrence of acute hospitalization for systemic diseases among patients aged 75 years or older: a propensity score-matched study. Arch Gerontol Geriatr. 2023;107:104876. 10.1016/j.archger.2022.104876 [DOI] [PubMed] [Google Scholar]
- 17. Tomioka K, Kurumatani N, Saeki K.. Regular dental visits may prevent severe functional disability: a community-based prospective study. Arch Gerontol Geriatr. 2020;88:104019. 10.1016/j.archger.2020.104019 [DOI] [PubMed] [Google Scholar]
- 18. Iwasaki M, Sato M, Yoshihara A, Ansai T, Miyazaki H.. Association between tooth loss and medical costs related to stroke in healthy older adults aged over 75 years in Japan. Geriatr Gerontol Int. 2017;17(2):202–210. 10.1111/ggi.12687 [DOI] [PubMed] [Google Scholar]
- 19. Saito M, Shimazaki Y, Nonoyama T, Tadokoro Y.. Associations of number of teeth with medical costs and hospitalization duration in an older Japanese population. Geriatr Gerontol Int. 2019;19(4):335–341. 10.1111/ggi.13622 [DOI] [PubMed] [Google Scholar]
- 20. Ministry of Health, Labour and Welfare. Summary of statistics on conditions of long-term care benefit expenses; 2021. Published online 2022. https://www.mhlw.go.jp/toukei/saikin/hw/kaigo/kyufu/21/dl/11.pdf. Accessed August 27, 2024. [Google Scholar]
- 21. Kondo K, Rosenberg M, eds. Advancing Universal Health Coverage through Knowledge Translation for Healthy Ageing Lessons Learnt from the Japan Gerontological Evaluation Study. World Health Organization; 2018. [Google Scholar]
- 22. Saito M, Aida J, Kondo N, et al. Reduced long-term care cost by social participation among older Japanese adults: a prospective follow-up study in JAGES. BMJ Open. 2019;9(3):e024439. 10.1136/bmjopen-2018-024439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Akiyama N, Shiroiwa T, Fukuda T, Murashima S, Hayashida K.. Healthcare costs for the elderly in Japan: analysis of medical care and long-term care claim records. PLoS One. 2018;13(5):e0190392. 10.1371/journal.pone.0190392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gilbert GH, Duncan RP, Vogel WB.. Determinants of dental care use in dentate adults: six-monthly use during a 24-month period in the Florida Dental Care Study. Soc Sci Med. 1998;47(6):727–737. 10.1016/s0277-9536(98)00148-8 [DOI] [PubMed] [Google Scholar]
- 25. Kiuchi S, Aida J, Kusama T, et al. Does public transportation reduce inequalities in access to dental care among older adults? Japan gerontological evaluation study. Community Dent Oral Epidemiol. 2019;48(2):109–118. 10.1111/cdoe.12508 [DOI] [PubMed] [Google Scholar]
- 26. Tu RY, Liang P, Tan AJM, et al. Factors associated with regular dental attendance by aged adults: a systematic review. Gerodontology. 2023;40(3):277–287. 10.1111/ger.12661 [DOI] [PubMed] [Google Scholar]
- 27. Schreiner AS, Hayakawa H, Morimoto T, Kakuma T.. Screening for late life depression: cut-off scores for the geriatric depression scale and the Cornell scale for depression in dementia among Japanese subjects. Int J Geriatr Psychiatry. 2003;18(6):498–505. 10.1002/gps.880 [DOI] [PubMed] [Google Scholar]
- 28. Deb P, Norton EC.. Modeling health care expenditures and use. Annu Rev Public Health. 2018;39:489–505. 10.1146/annurev-publhealth-040617-013517 [DOI] [PubMed] [Google Scholar]
- 29. Yu AYX, Krahn M, Austin PC, et al. Sex differences in direct healthcare costs following stroke: a population-based cohort study. BMC Health Serv Res. 2021;21(1):619. 10.1186/s12913-021-06669-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Belotti F, Deb P, Manning WG, Norton EC.. Twopm: two-part models. Stata J. 2015;15(1):3–20. 10.1177/1536867x1501500102 [DOI] [Google Scholar]
- 31. Basu A, Rathouz PJ.. Estimating marginal and incremental effects on health outcomes using flexible link and variance function models. Biostatistics. 2005;6(1):93–109. 10.1093/biostatistics/kxh020 [DOI] [PubMed] [Google Scholar]
- 32. Fine JP, Gray RJ.. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509. 10.1080/01621459.1999.10474144 [DOI] [Google Scholar]
- 33. Stekhoven DJ, Bühlmann P.. MissForest-non-parametric missing value imputation for mixed-type data. Bioinformatics. 2012;28(1):112–118. 10.1093/bioinformatics/btr597 [DOI] [PubMed] [Google Scholar]
- 34. Kojima K, Saito M, Miyaguni Y, Okada E, Ojima T.. Oral function and cumulative long-term care costs among older Japanese adults: a prospective 6-year follow-up study of long care receipt data. BMJ Open. 2023;13(2):e066349. 10.1136/bmjopen-2022-066349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Koyama S, Saito M, Cable N, et al. Examining the associations between oral health and social isolation: a cross-national comparative study between Japan and England. Soc Sci Med. 2021;277:113895. 10.1016/j.socscimed.2021.113895 [DOI] [PubMed] [Google Scholar]
- 36. Kino S, Tamada Y, Takeuchi K, et al. Exploring the relationship between oral health and multiple health conditions: an outcome-wide approach. J Prosthodont Res. 2023;68:415–424. 10.2186/jpr.jpr_d_23_00091. [DOI] [PubMed] [Google Scholar]
- 37. Humphrey LL, Fu R, Buckley DI, Freeman M, Helfand M.. Periodontal disease and coronary heart disease incidence: a systematic review and meta-analysis. J Gen Intern Med. 2008;23(12):2079–2086. 10.1007/s11606-008-0787-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lafon A, Pereira B, Dufour T, et al. Periodontal disease and stroke: a meta-analysis of cohort studies. Eur J Neurol. 2014;21(9):1155–1161, e66. 10.1111/ene.12415 [DOI] [PubMed] [Google Scholar]
- 39. Asher S, Stephen R, Mäntylä P, Suominen AL, Solomon A.. Periodontal health, cognitive decline, and dementia: a systematic review and meta-analysis of longitudinal studies. J Am Geriatr Soc. 2022;70(9):2695–2709. 10.1111/jgs.17978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Terada T, Nakamura K, Seino K, Kizuki M, Inase N.. Cost of shifting from healthcare to long-term care in later life across major diseases: analysis of end-of-life care during the last 24 months of life. J. Rural Med. 2018;13(1):40–47. 10.2185/jrm.2955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.. Statistics Bureau of Japan. Statistical handbook of Japan 2022. Published online 2022. https://www.stat.go.jp/english/data/handbook/pdf/2022all.pdf#page=23. Accessed August 27, 2024. [Google Scholar]
- 42. Winkelmann J, Listl S, van Ginneken E, Vassallo P, Benzian H.. Universal health coverage cannot be universal without oral health. Lancet Public Health. 2023;8(1):e8–e10. 10.1016/S2468-2667(22)00315-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Reda SM, Krois J, Reda SF, Thomson WM, Schwendicke F.. The impact of demographic, health-related and social factors on dental services utilization: systematic review and meta-analysis. J Dent. 2018;75:1–6. 10.1016/j.jdent.2018.04.010 [DOI] [PubMed] [Google Scholar]
- 44. Aida J, Takeuchi K, Furuta M, Ito K, Kabasawa Y, Tsakos G.. Burden of oral diseases and access to oral care in an ageing society. Int Dent J. 2022;72(4S):S5–S11. 10.1016/j.identj.2022.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Aida J, Fukai K, Watt RG.. Global neglect of dental coverage in universal health coverage systems and Japan’s broad coverage. Int Dent J. 2021;71(6):454–457. 10.1016/j.identj.2020.12.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Japan Cabinet Office. Basic policy on economic and fiscal management and reform. Cabinet Office. https://www5.cao.go.jp/keizai-shimon/kaigi/cabinet/honebuto/2022/decision0607.html. Accessed August 27, 2024; 2022 For a New Form of Capitalism: Achieving a Sustainable Economy by Harnessing Processes to Overcome Challenges to Drive Growth. [Google Scholar]
- 47. Xu K, Ma S, Gu J, et al. Association between dental visit behavior and mortality: a nationwide longitudinal cohort study from NHANES. Clin Oral Investig. 2023;28(1):37. 10.1007/s00784-023-05471-8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data were obtained from the JAGES study. All inquiries will be addressed by the Data Management Committee via e-mail: dataadmin.ml@jages.net. All JAGES datasets have ethical or legal restrictions for public deposition, owing to the inclusion of sensitive information from human participants.