Abstract
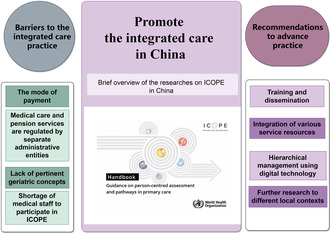
This article presents a brief overview of the researches on ICOPE in China, the barriers influencing the implementation of ICOPE are identified, and the recommendations are proposed to advance the ICOPE practice in China.
Keywords: elderly, geriatrics, ICOPE
The process of population aging in China is intensifying, leading to a pressing need for effective health care services for the elderly people. The World Health Organization(WHO) has introduced the concept of healthy aging in the World report on aging and health, highlighting the significance of preserving the intrinsic capacities(IC)of older individuals. 1 This initiative has been further reinforced by WHO through the publication of the Integrated Care for Older People (ICOPE): guidelines on community‐level interventions to manage declines in IC, which outlined strategies for reversing or delaying the decline of IC at the primary care level. 2 In 2019, WHO further published a specific handbook for ICOPE implementation, which provided guidance for person‐centered assessment and pathways in primary care, with five generic steps. 3 The WHO recommends that different countries carry out practical research on ICOPE, which might be tailored to their own actual conditions.
1. RESEARCH ON THE ICOPE INITIATIVE IN CHINA
Scholars from various countries have undertaken research to validate the pertinent aspects of ICOPE, with Chinese scholars specifically examining the efficacy of IC screening tools, analyzing the characteristics of IC, and investigating the relationship between IC and frailty, as well as adverse outcomes, in alignment with the WHO's plan. 4 , 5 , 6 , 7 However, there is a scarcity of intervention studies globally that adhere to ICOPE implementation steps 1–5. 8 , 9
Preliminary research findings on the implementation of integrated care in China have been published in Age and Aging in January 2024. 10 Conducted by the Department of Geriatrics at Peking Union Medical College Hospital and Qingsong Health Care, this study focused on community‐dwelling elderly individuals in Chaoyang District, Beijing, from 2020 to 2021. Utilizing mobile electronic questionnaires, a total of 33,504 elderly participants were initially screened for impaired IC. Among them, 2148 individuals showing potential signs of decreased IC underwent further evaluation and were randomly assigned to either an intervention group (537 participants) or a control group (1611 participants). The intervention group received personalized services from trained community medical staff acting as integrated care managers (ICMs), following the ICOPE pathway, which encompassed interpreting assessment findings, formulating intervention strategies, offering pertinent advice on medical interventions, nutritional support, rehabilitation, nursing care, environmental modifications, weekly monitoring, and follow‐up, as well as facilitating medical referrals. In contrast, the control group solely received evaluation, interpretation, and health care recommendations from ICMs. Follow‐up evaluations were conducted for both groups after 6 months. The findings indicated that, relative to the baseline, the intervention group demonstrated enhancements in physical functions, cognition, vitality (nutritional status), mobility, and psychological health. There was a notable enhancement in vitality, mobility, and psychological health in the intervention group compared with the control. Additionally, the intervention group exhibited a significant reduction in the frequency of medical visits compared with the control group, although there was no discernible variance in medical expenses. These findings suggest that the implementation of the WHO's ICOPE pathway in urban areas of China can effectively benefit elderly individuals experiencing declining IC.
As of March 10, 2024, there are 19 clinical studies registered in the China National Medical Research Registration System or the Chinese Clinical Trial Registry (ChiCTR) pertaining to the Integrated Care for Older People (ICOPE) or Integrated Care (IC). Among these studies, 12 are observational in nature and focus on the predictive capabilities of IC in relation to adverse outcomes, the development of risk prediction models, validation of screening tools, and theoretical demonstrations. Conversely, only seven studies are interventional. One such study, conducted by Zhejiang Hospital, involved the creation of an integrated home care management platform utilizing 5G network technology to implement behavioral and lifestyle interventions. Another study, conducted by Xiangya School of Nursing, Central South University, utilized mobile health technology to facilitate self‐management of IC declines in elderly populations. Both of these interventional studies primarily relied on network software systems to support their respective interventions for IC. A separate study utilizing an insomnia treatment instrument has been developed to address insomnia in elderly patients in order to enhance their IC, which is not directly linked to the ICOPE pathway. In accordance with the ICOPE pathway, a study conducted by Peking Union Medical College Hospital in three retirement communities is investigating targeted technical approaches for IC assessment and intervention, while a randomized intervention study led by Zhengzhou University in a Shanghai community focuses on elderly individuals with mild IC decline. Additionally, a study conducted by the School of Public Health at Fudan University solely focuses on IC assessment and intervention for elderly individuals with cognitive impairment and frailty. These three studies primarily examine Steps 1–3 of the ICOPE pathway, with the only interventional study addressing Steps 1–5 being the “Pilot study on the application of ICOPE in multiple centers in China,” an extension of the abovementioned ICOPE research conducted in Chaoyang District, Beijing.
Analysis of published and ongoing scientific research projects reveals a dearth of intervention studies on the ICOPE pathway in China, with a predominant focus on urban communities with favorable conditions. This highlights a notable gap in population or community coverage. The research on the ICOPE pathway is currently undergoing verification, with limited exploration and improvement. There is a short observation period for the research population, and a lack of long‐term health outcome evaluation and health economics analysis.
2. BARRIERS TO THE INTEGRATED CARE PRACTICE IN CHINA
2.1. The mode of payment
The predominant payment system for medical care in China is centered around diagnosis‐related groups (DRG) payment system or fee‐for‐service. However, several tasks within the ICOPE pathway, including assessment, intervention plan formulation, nursing care, and community door‐to‐door service, do not have corresponding payment mechanisms. Long‐term care insurance is currently only available in pilot areas and has not been widely adopted. The ICOPE pathway is not solely centered on disease diagnosis and treatment. Its health management concepts, which emphasize holistic care, long‐term maintenance of function, and quality of life, may be better suited for a pay‐for‐performance mechanism. In select pilot regions, such as Luohu District in Shenzhen, hospital consortiums have been established to offer comprehensive health management services centered on community‐level care, utilizing a “total payment for all people, surplus as reward” payment model. However, this service is for people of all ages and prioritizes early disease prevention and treatment.
2.2. Medical care and pension services are regulated by separate administrative entities
Within the ICOPE framework, numerous nonmedical services, such as living assistance, home environment modifications, and caregiver support, are classified as social services rather than medical care. In China, the National Health Commission is responsible for the administration and policies of health care, while the Ministry of Civil Affairs is tasked with managing pension services. The integration of various services under the purview of different ministries may hamper the successful implementation of the ICOPE pathway.
2.3. Lack of pertinent geriatric concepts
It is worth noting that the current health care system for elderly individuals in China primarily emphasizes disease diagnosis and treatment. Community medical services for the elderly continue to adhere to this model, prioritizing the prevention, screening, and treatment of chronic diseases while neglecting important aspects such as IC and geriatric syndromes. The lack of geriatric training among community‐level medical staff results in limited knowledge and practice skills related to ICOPE, such as comprehensive geriatric assessment (CGA).
2.4. Shortage of medical staff to participate in ICOPE
A sufficient number of health care professionals with expertise in geriatric care and familiarity with the ICOPE pathway should be available to serve as ICMs in order to develop individualized intervention plans for elderly individuals. However, the current health care infrastructure in China lacks designated positions for such professionals in community and nursing facilities, and there is a limited number of geriatric specialists in higher level hospitals to extend coverage to the community. Additionally, there is a shortage of medical professionals in rehabilitation, nutrition, geriatric nursing, and other specialized fields at the community level, hindering the effective implementation of the ICOPE program in China. In addition to financial support, staff training and the establishment of specialized post settings are necessary.
3. PROMOTE THE PRACTICE OF INTEGRATED CARE IN CHINA
It is important to recognize that ICOPE not only benefits older adults experiencing IC decline but also serves the broader elderly population by offering tailored health and living services based on individual needs. The integration of various services and on‐demand provision aligns with China's longstanding policy promoting the combination of medical treatment and elderly care, serving as a valuable complement to the principles of this policy.
Evidence suggests that individualized interventions based on CGA have been successful in enhancing independence, reducing re‐hospitalization rates, and enhancing quality of life for elderly patients with frailty and multiple chronic conditions 11 , 12 The ICOPE program represents a focused intervention strategy rooted in CGA, with the aim of replicating its anticipated effects. Consequently, further validation studies are imperative to gather additional outcome and health economics data, thereby bolstering the case of advancing reforms within China's health care system and policies.
Successful implementation of ICOPE necessitates widespread dissemination and training initiatives to ensure that health care professionals comprehend the varying characteristics and requirements of elderly individuals across different stages of capacity (high and stable, declining, and significantly impaired). The community medical staff must be proficient in basic CGA skills, comprehend the health requirements of the elderly, and communicate effectively with them in order to develop shared intervention decisions. It is imperative that geriatric training be incorporated into the education of community medical staff and primary care providers. Furthermore, knowledge and principles related to healthy aging should be disseminated throughout society to ensure that individuals' perceptions of elderly health extend beyond mere disease diagnosis and treatment to encompass holistic health maintenance and management.
Integration of different service resources is essential for ICOPE, including medical care services such as family doctors, home nursing, rehab, referral services, and remote consultation by professionals. Additionally, community‐based assisted living services, such as elder care facilities, day care centers, and housekeeping services, are essential components. The coordination of multiple service providers requires the role of a “manager” to organize appropriate kinds of services tailored to the needs of the elderly population. In developed nations, professionals including social workers, nurse practitioners, and care managers frequently participate in integrated care within communities, assuming the role of “ICMs.” The emergence of ICMs represents a novel position within community‐based elderly care services. Concurrently, a variety of services in the community, spanning medical care to assisted living, are typically delivered by distinct providers or facilities. The amalgamation of diverse services may serve to optimally address the varied needs of the elderly population, while also maximizing the utilization of existing resources and fostering advancement within the field. The provision of diversified services necessitates an appropriate payment mechanism to uphold service sustainability, along with uniform policies across various administrative ministries and corresponding oversight measures to guarantee service quality. Further exploration and enhancement of relevant supportive mechanisms and policies are imperative.
Due to the absence of ICM positions in China and the scarcity of community medical personnel, ICOPE may be difficult to implement directly. Implementing hierarchical management based on the health status of elderly individuals and encouraging self‐management among those in better health, using digital technology to aid in self‐assessment, self‐management, and providing guidance for interventions, is anticipated to complement the ICOPE pathway.
In addition to the aforementioned recommendations for addressing barriers and promoting facilitators, further research is warranted to explore more measures that account for the extensive geographical expanse of China, significant urban–rural disparities, diverse economic statuses, and varying cultural norms across regions. Nonetheless, regardless of the specific strategies implemented, the primary goal remains unchanged: to efficiently integrate and leverage available resources to support successful aging and improve healthy life expectancy.
AUTHOR CONTRIBUTIONS
Lin Kang conceptualized the manuscript. Minglei Zhu did the literature search, wrote the manuscript draft and revised the English text with AI tools. Lin Kang and Xiaohong Liu revised the manuscript draft. All authors read and approved the final version of the manuscript.
FUNDING INFORMATION
National High Level Hospital Clinical Research Funding (2022‐PUMCH‐B‐129).
CONFLICT OF INTEREST STATEMENT
The authors declare that the article was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
ACKNOWLEDGMENTS
The authors express their gratitude to “HOME for Researchers” for providing English‐language editing services for a draft of this manuscript using the AI tools developed by the organization.
Zhu M, Kang L, Liu X. Promote the integrated care in China. Aging Med. 2024;7:449‐452. doi: 10.1002/agm2.12351
Contributor Information
Lin Kang, Email: kangl@pumch.cn.
Xiaohong Liu, Email: xhliu41@sina.com.cn.
REFERENCES
- 1. World Health Organization . World Report on Ageing and Health. 2015. Accessed 7 March 20224. https://www.who.int/publications/i/item/9789241565042
- 2. World Health Organization . Integrated care for older people: guidelines on community‐level interventions to manage declines in intrinsic capacity. 2017. Accessed 7 March 2024. https://apps.who.int/iris/handle/10665/258981 [PubMed]
- 3. World Health Organization . Integrated care for older people (ICOPE): guidance for person‐centred assessment and pathways in primary care. 2019. Accessed 7 March 2024. https://iris.who.int/handle/10665/326843
- 4. Ma L, Chhetri JK, Zhang Y, et al. Integrated care for older people screening tool for measuring intrinsic capacity: preliminary findings from ICOPE pilot in China. Front Med. 2020;7:576079. doi: 10.3389/fmed.2020.576079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lu F, Li J, Liu X, Liu S, Sun X, Wang X. Diagnostic performance analysis of the integrated Care for Older People (ICOPE) screening tool for identifying decline in intrinsic capacity. BMC Geriatr. 2023;23(1):509. doi: 10.1186/s12877-023-04180-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Liu S, Yu X, Wang X, et al. Intrinsic capacity predicts adverse outcomes using integrated Care for Older People screening tool in a senior community in Beijing. Arch Gerontol Geriatr. 2021;94:104358. doi: 10.1016/j.archger.2021.104358 [DOI] [PubMed] [Google Scholar]
- 7. Liu S, Kang L, Liu X, et al. Trajectory and correlation of intrinsic capacity and frailty in a Beijing elderly community. Front Med. 2021;8:751586. doi: 10.3389/fmed.2021.751586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sum G, Lau LK, Jabbar KA, et al. The World Health Organization (WHO) integrated Care for Older People (ICOPE) framework: a narrative review on its adoption worldwide and lessons learnt. Int J Environ Res Public Health. 2022;20(1):154. doi: 10.3390/ijerph20010154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization . Integrated care for older people (ICOPE) implementation pilot programme: findings from the ‘ready’ phase. 2022. Accessed 7 March 2024. https://iris.who.int/handle/10665/353553
- 10. Ninie YW, Xiaohong L, Xiangrong K, et al. Implementation and impact of the World Health Organization integrated care for older people (ICOPE) program in China: a randomised controlled trial. Age Ageing. 2024;53(1):1‐10. doi: 10.1093/ageing/afad249 [DOI] [PubMed] [Google Scholar]
- 11. Chen Z, Ding Z, Chen C, et al. Effectiveness of comprehensive geriatric assessment intervention on quality of life, caregiver burden and length of hospital stay: a systematic review and meta‐analysis of randomised controlled trials. BMC Geriatr. 2021;21(1):377. doi: 10.1186/s12877-021-02319-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wu J, Zhang H, Shao J, et al. Healthcare for older adults with multimorbidity: a scoping review of reviews. Clin Interv Aging. 2023;18:1723‐1735. doi: 10.2147/CIA.S425576 [DOI] [PMC free article] [PubMed] [Google Scholar]


