Abstract
Frailty is a multidimensional syndrome associated with a decline in reserve capacity across multiple organ systems involving physical, psychological, and social aspects. Weakness is the earliest indicator of the frailty process. Multi‐morbidity is the state of presence of two or more chronic diseases. Frailty and chronic diseases are interlinked as frail individuals are more prone to develop chronic diseases and multi‐morbid individuals may present with frailty. They share common risk factors, pathogenesis, progression, and outcomes. Significant risk factors include obesity, smoking, aging, sedentary, and stressful lifestyle. Pathophysiological mechanisms involve high levels of circulating inflammatory cytokines as seen in individuals with frailty and chronic diseases such as hypertension, cardiovascular diseases, type 2 diabetes mellitus, chronic kidney disease, and anemia. Hence, frailty and chronic diseases go hand in hand and it is of utmost importance to identify them and intervene during early stages. Screening frailty and treating multi‐morbidity incorporate both pharmacological and majorly non‐ pharmacological measures, such as physical activities, nutrition, pro‐active care, minimizing polypharmacy and addressing reversible medical conditions. The purpose of this mini‐review is to highlight the interrelation of frailty and chronic diseases through the discussion of their predictors and outcomes and how timely interventions are essential to prevent the progression of one to the other.
Keywords: chronic diseases, frailty
Frailty and chronic diseases are interlinked with shared risk factors, pathogenesis, progression and outcome. Timely identification and intervention with incorporation of both pharmacological and non‐pharmacological measures are essential to prevent the progression of one to other.
1. INTRODUCTION
Frailty is a multidimensional syndrome characterized by a reduction in the reserve capacity that results in an increased risk of disability and death from minor external stresses. 1 Frailty results in a spiral of decline with an increased risk of worsening disability, increased incidence of admission to hospital, long‐term care facility, and death. Phenotypical frailty encompasses unintentional weight loss, weakness, exhaustion, low hand strength, and decreased physical activity. 2 A pre‐frail stage, in which one or two of the mentioned criteria are present, identifies persons with an increased risk of progression to frailty. 2 Nevertheless, frailty is not limited to the physical dimension of health. Psychological dimension includes cognitive frailty, low mood, and anxiety. Social dimensions of frailty include a lack of social support and social interactions.
There is notably a heterogeneity in the frailty process among different individuals, with mostly weakness being the first manifestation followed by slowness, and low physical activity which precedes exhaustion and weight loss. 3 Weakness, the early manifestation of frailty onset, occurs due to sarcopenia. Therefore, weakness may be a clinically meaningful early indicator of the frailty process when preventive intervention could be most effective before initiation of weight loss or exhaustion when it might be too late to implement frailty interventions.
Multi‐morbidity is the concurrent occurrence of two or more chronic diseases. 4 Distinct from multi‐morbidity, frailty is an aggregate of subclinical reserve losses across multiple systems. Thus, frailty occurs parallel with multi‐morbidity. 5
Frailty and multi‐morbidity are associated with increased risk for disability, health care utilization, and mortality among older adults. 6 There is no reported one‐to‐one connection between chronic diseases and frailty yet there might be some biological overlap and bidirectional association between these two conditions. Majority of frail individuals present with multi‐morbidity however fewer multi‐morbid individuals present with frailty. 6 Many chronic diseases may converge to give a prominent symptom of frailty, or there may be a single chronic disease that, when severe, may cause diverse symptoms and signs paralleling to frailty syndrome. Through this mini‐review, we aim to discuss this interplay between frailty and chronic diseases in causation, progression, and possible interventions.
2. THE INTER‐RELATED RISK FACTORS FOR FRAILTY AND CHRONIC DISEASES
Frailty and multi‐morbidity are identified as promising clinical biomarkers when studying underlying mechanisms of aging. Aging is related to frailty and chronic diseases. But, it is important to understand that not all old individuals are frail, and not all frail individuals are old. The aging process represents a significant risk factor for chronic diseases, including insulin resistance, hypertension, and cancers. 7 In recent years, geroscience has emphasized that delaying aging (the most crucial risk factor for frailty) can prevent chronic diseases and aging‐related biomarkers or anti‐aging therapies could prevent and treat chronic diseases. 8 In the future, geroscience may be translated to public health practice in preventing NCDs through anti‐aging targets or interventions. 9
The English Longitudinal Aging Study has shown that obesity, high waist‐hip ratio, smoking or previous smoking, sedentary behavior, and stressful living are significant risk factors for frailty. 10 These modifiable social and behavioral risk factors could delay the development and progression of frailty. Lifestyle‐related risk factors also contribute to non‐communicable diseases. Hence, shared risk factors exist for developing lifestyle diseases and frailty at the entry point. Later, the presence and progression of chronic lifestyle disorders contribute to frailty (Figure 1). In recent years, frailty and multi‐morbidity have been a predictor and an outcome of each other, as well as both predictors of disability and mortality. 11
FIGURE 1.
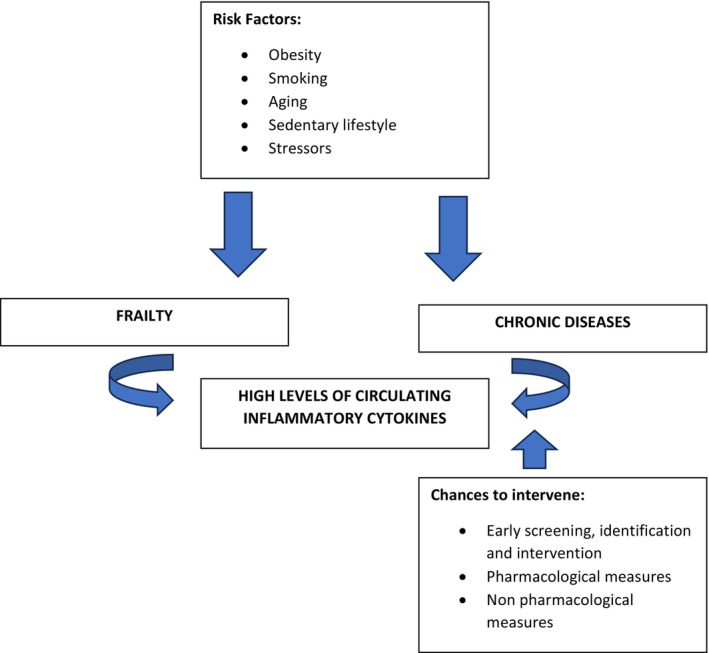
Graphical representation of the bi‐directional relationship between frailty and chronic diseases.
3. STRESSORS IN THE IMPLICATION OF FRAILTY AND CHRONIC DISEASES
The effects of stressful environments result in a glucocorticoid excess that disrupts normal cellular function, causes cellular damage, causes system dysfunction, and accelerates aging and frailty. 12 Moreover, older adults are unable to terminate the stress response system efficiently. There are also the development and progression of stress‐related conditions and diseases, such as hypertension, coronary heart disease, insulin resistance, cerebrovascular disease, anxiety, and depression. Glucocorticoid excess results in loss of muscle mass, osteopenia, diabetes, visceral obesity, anorexia, anxiety, and depression, which contributes to both the development and progression of frailty. 13 Altered diurnal variation of cortisol is observed in the clinical presentation of frail older women. 14
4. INFLAMMAGING AND CHRONIC DISEASES
Inflammaging is a chronic pro‐inflammatory state characterized by high circulating levels of pro‐inflammatory markers, such as interleukin‐1 (IL‐1), interleukin‐6 (IL‐6), interleukin‐8 (IL‐8), interleukin‐13 (IL‐13), interleukin‐18 (IL‐18), high sensitivity C‐ reactive protein (CRP), interferon‐α (IFNα) and interferon‐β (IFNβ), tumor necrosis factor(TNF), transforming growth factor‐ β (TGFβ) and serum amyloid A. 15 Inflammatory cytokines are involved in the pathogenesis of frailty and chronic diseases such as cardiovascular diseases (elevated high‐sensitivity C‐reactive protein, i.e., hs‐CRP when detected early has a significant role in reducing cardiovascular events with statin therapy in patients without dyslipidemia), 16 type 2 diabetes mellitus, chronic kidney disease, cancers, osteoporosis, dementia, sarcopenia, and anemia. Visceral obesity in the form of central obesity predisposes an individual to chronic low‐grade inflammation that leads to aging, frailty, and chronic diseases. 17
5. THE INTERPLAY BETWEEN KEY CHRONIC DISEASES AND FRAILTY
5.1. Frailty and hypertension
Arteriosclerosis, inflammation, and oxidative stress are processes involved in the pathophysiology of hypertension and frailty. In total, 72% of frail individuals present with hypertension, whereas 14% of hypertensive patients present with frailty. 18
In addition, blood pressure management is complex when frailty and other chronic diseases co‐exist with hypertension. Due to the influence of frailty on the specific risk of treatment for hypertension and its high prevalence, it becomes essential to assess the presence of frailty in persons with hypertension. 19 Orthostatic hypotension in frail individuals can induce falls and fractures, leading to disability soon after initiation or modification of antihypertensive treatment due to blood pressure variability, which is essential to consider. 20 Guidelines recommend frail hypertensive patients target for a systolic blood pressure between 140 and 150 mmHg. 21
5.2. Frailty and cardiovascular diseases
Lifestyle risk factors and normal aging pathophysiological mechanisms are associated with increased risk of cardiovascular diseases and frailty. Conversely, cardiac and cerebrovascular diseases are associated with increased risk of frailty. Frail heart failure patients have more co‐morbidities, inflammation, sarcopenia, and global dysfunction. 22
Recently, it was known that frailty is an essential determinant in predicting the risk of poor outcomes in heart failure patients, predicting death and hospitalization. This relationship is consistent across varied income countries. The same study reveals that frailty might be an important therapeutic target, distinct from established effective treatments in improving heart failure outcomes. 23 In older adults with Acute Coronary Syndrome (ACS), frailty was associated with increased risk of cardiovascular diseases (CVD), major bleeding and hospital readmission. 24 Frailty significantly increases all‐cause mortality by 6.51 times in ST‐elevation myocardial infarction (STEMI) patients. 25
5.3. Frailty and kidney disease
In individuals older than 70 years of age, there is a decline in the glomerular filtration rate (GFR) by 2 mL/min/year. 26 Similarly, an aging kidney has a diminished ability to adapt to alterations in sodium intake and the homeostasis of electrolytes. These points are essential to consider in patients with frailty, impaired kidney function, multiple chronic conditions, and concurrent polypharmacy.
Frailty increases the risk of acute kidney injury and progression to end‐stage renal disease. 27 Frail individuals quickly become volume‐depleted during acute stressors with decreased salt and water intake. Similarly, Chronic Kidney Disease (CKD) patients with frailty are also at increased risk of harm from the effects of polypharmacy and use of non‐steroidal anti‐inflammatory drugs.
Factors that increase the progression of frailty in CKD include the presence of anemia, uremia, vitamin D deficiency, hypocalcemia, undernutrition, and anorexia. In frail individuals with end‐stage CKD, their vitality is negatively impacted by reduced dietary due to uremic symptoms (nausea, anorexia, and dysgeusia). 28
5.4. Frailty and diabetes mellitus
There is a shared pathophysiology among frailty and diabetes mellitus: sarcopenic obesity, chronic inflammation, hormonal and metabolic changes, oxidative stress, and mitochondrial dysfunction. Frailty is an independent risk factor for morbidity and mortality in older diabetes mellitus patients. Similarly, high blood sugar levels predict a transition to higher frailty levels. Also, vascular complications of diabetes mellitus and malnutrition lead to functional decline in frail older adults.
The treatment of type 2 diabetes is particularly demanding in co‐existing frailty and chronic diseases is due to relative inability to tolerate the adverse effects of oral anti‐diabetic agents. 29
5.5. Frailty and anemia
The hemoglobin levels for defining anemia in the older population is a matter of discussion, especially in those with frailty. The reference population for WHO's definition of anemia did not include subjects aged >65 years, making the extension of such criteria to the older population highly questionable. Concerning chronic inflammation and frailty, Interleukin‐6 co‐relates best with anemia in several chronic disease states. 30
Anemia is associated with an increased risk of falls, impaired activities of daily living (ADL) and reduced strength, physical performance, mobility and cognition. 31 These are clinical parameters directly implicated in frailty. Hence, reversing anemia is an integral part of management in older adults living with frailty.
Frailty and chronic diseases, thus, go hand in hand. Therefore, individuals must be screened to identify frailty and facilitate discussions around future treatment plans for all chronic diseases. A pre‐planned and proactive treatment pathway for management should be established. It is also imperative for chronic diseases to be screened in individuals with frailty. Non‐pharmacological interventions are common to all chronic diseases and frailty status.
6. INTERVENTIONS COMMON TO BOTH FRAILTY AND CHRONIC DISEASES
6.1. Physical activity
Weakness is the first initial manifestation of frailty. Weakness in hand grip strength has been shown to be associated with the risk of morbidity and mortality in various chronic diseases. 32 In people who develop cardiovascular diseases, lower grip strength is associated with increased susceptibility to mortality. 33 A person's muscle mass starts to decrease with age; hence, exercise interventions to prevent sarcopenia can, in turn, help prevent frailty and its development and progression in old age.
Exercise is associated with neurogenesis, release of vascular growth factors, Toll‐like receptors (TLR) expression, long‐term memory potentiation, and reduced vascular risk factors. 34 Similarly, physical exercise and yoga have been shown to reduce oxidative and psychological stress and improve glycemic control, which undoubtedly has beneficial effects for maintaining health and reversing chronic lifestyle‐related disorders. Studies of meditation also suggest a possible benefit on reducing cardiovascular risks and other non‐communicable diseases. 35 This, in turn, halts the progression of frailty in people living with multi‐morbidity.
The Asia Pacific Clinical Practice guidelines for managing frailty recommend that adults with frailty perform progressive, individualized physical activity programs with resistance training. 36
6.2. Nutrition
Greater adherence to a Mediterranean‐type diet has shown a 60 percent reduction in risk of frailty. 37 Similar to plant‐based foods like the Dietary Approaches to Stop Hypertension (DASH), vegetarian and vegan diets seem beneficial in developing and progressing lifestyle diseases. 38 Protein intake of approximately 1 gram per kilogram of body weight per day may be more beneficial for older adults to counteract age related sarcopenia and support overall physical function and strength. 39 Nevertheless, undernutrition and obesity are associated with the development and progression of frailty. Sarcopenic obesity is a risk factor for cardiovascular disease‐related morbidity and mortality.
In addition, caloric restriction and intermittent fasting have been shown to slow cell growth and metabolism, improve physiologic reserve capacity, cause a shift of cellular metabolism from cell proliferation to repair activities, and decrease the accumulation of senescent cells and inflammation, thus halting frailty. 40 Fasting, or calorie restriction, has been found to induce a shift of gut microbiota composition that stimulates the browning of white adipose tissue and increases the activity of brown adipose tissue. 41 This assists in fat loss and weight loss, thus reversing the process of lifestyle disorders, chronic diseases, and frailty.
7. INTERVENTIONS FOR FRAILTY IN A PATIENT WITH CHRONIC DISEASE
7.1. Pro‐active care more than reactive care
Unfortunately, frail older adults with chronic diseases present late and in crisis with acute issues such as delirium, falls, fractures, and immobility and are treated in the hospital in an episodic, disruptive, and disjointed manner. Timely identification of pre‐frailty and frailty is therefore essential. Timely identification can result in preventative, proactive care by supported management and planning. Pro‐active preventative care should be community‐based and coordinated with various sectors, along with screening and treatment of chronic diseases. Physical, nutritional, and psychological interventions such as walking, incentive spirometry, smoking cessation, and nutrition can delay the development and progression of both frailty and chronic diseases.
7.2. Addressing reversible medical conditions
Treatable chronic causes of fatigue should be identified and treated, including depression, sleep apnea, anemia, hypothyroidism, vitamin B12 deficiency, and hypotension. Treatment of symptomatic medical conditions should be the top priority, along with timely care of underlying complications of chronic diseases.
7.3. Reduction of harmful polypharmacy and “Do no harm” policy
Frailty leads to polypharmacy, and harmful prescription cascades and webs may worsen the health status of the aging frail individual with multi‐morbidity. Never more than today, Hippocrates' oath of “First, do no harm” is essential to drive our clinical decisions in frailty and chronic diseases. Also, it is imperative to understand that an inappropriate prescription could be an exogenous stressor precipitating frailty status is important.
7.4. Addressing what matters and end‐of‐life goals
The principles of end‐of‐life care apply to frail individuals with progressive chronic conditions from the time of diagnosis throughout decline.
8. CONCLUSION
The causality and pathophysiological mechanisms behind frailty and chronic diseases share a common pathway and entry point. The progression of both frailty and chronic diseases are interlinked. Therefore, individuals must be screened to identify frailty and facilitate discussions around future treatment plans in patients with chronic diseases and vice versa. The establishment of a standardized definition of frailty and the application of a standard tool for frailty assessment is imperative among individuals living with chronic conditions. A pre‐planned and proactive treatment pathway for management should be established.
Since non‐pharmacological interventions are common to chronic diseases and frailty, these lifestyle interventions are essential in routine clinical implementation. Future research is needed to focus more on the causality and targeted interventions for those with frailty and chronic diseases, as well as on their prevention, and the interplay in between.
AUTHOR CONTRIBUTIONS
UB: Conceptualization, Writing original draft and editing, Literature review. BB, AS: Writing, review and editing. BK: Review, Supervision. SKS: Conceptualization, Review and Supervision.
FUNDING INFORMATION
No funding received.
CONFLICT OF INTEREST STATEMENT
None.
ACKNOWLEDGMENTS
We would like to acknowledge the KHDC (Kidney, Hypertension, Diabetes and Cardiovascular Disease) Nepal team and Department of Internal Medicine, B.P. Koirala Institute of Health Sciences, Nepal for the support in conceptualization of the manuscript.
Bhattarai U, Bashyal B, Shrestha A, Koirala B, Sharma SK. Frailty and chronic diseases: A bi‐directional relationship. Aging Med. 2024;7:510‐515. doi: 10.1002/agm2.12349
REFERENCES
- 1. Rodríguez‐Mañas L, Féart C, Mann G, et al. Searching for an operational definition of frailty: a delphi method based consensus statement. The frailty operative definition‐consensus conference project. J Gerontol Ser A Biol Sci Med Sci. 2013;68(1):62‐67. doi: 10.1093/gerona/gls119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Ser A Biol Sci Med Sci. 2001;56(3):146‐157. doi: 10.1093/gerona/56.3.m146 [DOI] [PubMed] [Google Scholar]
- 3. Xue QL, Bandeen‐Roche K, Varadhan R, Zhou J, Fried LP. Initial manifestations of frailty criteria and the development of frailty phenotype in the women's health and aging study II. J Gerontol Ser A Biol Sci Med Sci. 2008;63(9):984‐990. doi: 10.1093/gerona/63.9.984 [DOI] [PubMed] [Google Scholar]
- 4. Chew‐Graham C, O'Toole L, Taylor J, Salisbury C. Editorials “Multimorbidity”: An acceptable term for patients or time for a rebrand? Br J Gen Pract. 2019;69(685):372‐373. doi: 10.3399/bjgp19X704681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Weiss CO. Frailty and chronic diseases in older adults. Clin Geriatr Med. 2011;27(1):39‐52. doi: 10.1016/j.cger.2010.08.003 [DOI] [PubMed] [Google Scholar]
- 6. Vetrano DL, Palmer K, Marengoni A, et al. Frailty and multimorbidity: a systematic review and meta‐analysis. J Gerontol Ser A Biol Sci Med Sci. 2019;74(5):659‐666. doi: 10.1093/gerona/gly110 [DOI] [PubMed] [Google Scholar]
- 7. Prasad S, Sung B, Aggarwal BB. Age‐associated chronic diseases require age‐old medicine: role of chronic inflammation. Prev Med. 2012;54(Suppl):S29‐S37. doi: 10.1016/j.ypmed.2011.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kennedy BK, Berger SL, Brunet A, et al. Geroscience: linking aging to chronic disease. Cell. 2014;159(4):709‐713. doi: 10.1016/j.cell.2014.10.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ungvari Z, Adany R. The future of healthy aging: translation of geroscience discoveries to public health practice. Eur J Public Health. 2021;31(3):455‐456. doi: 10.1093/eurpub/ckaa212 [DOI] [PubMed] [Google Scholar]
- 10. Niederstrasser NG, Rogers NT, Bandelow S. Determinants of frailty development and progression using a multidimensional frailty index: evidence from the English longitudinal study of ageing. PLoS One. 2019;14(10):1‐16. doi: 10.1371/journal.pone.0223799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Villacampa‐Fernández P, Navarro‐Pardo E, Tarín JJ, Cano A. Frailty and multimorbidity: two related yet different concepts. Maturitas. 2017;95:31‐35. doi: 10.1016/j.maturitas.2016.10.008 [DOI] [PubMed] [Google Scholar]
- 12. Vitlic A, Lord JM, Phillips AC. Stress, ageing and their influence on functional, cellular and molecular aspects of the immune system. Age (Omaha). 2014;36(3):1169‐1185. doi: 10.1007/s11357-014-9631-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yiallouris A, Tsioutis C, Agapidaki E, et al. Adrenal aging and its implications on stress responsiveness in humans. Front Endocrinol (Lausanne). 2019;10:1‐12. doi: 10.3389/fendo.2019.00054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Varadhan R, Walston J, Cappola AR, Carlson MC, Wand GS, Fried LP. Higher levels and blunted diurnal variation of cortisol in frail older women. J Gerontol Ser A Biol Sci Med Sci. 2008;63(2):190‐195. doi: 10.1093/gerona/63.2.190 [DOI] [PubMed] [Google Scholar]
- 15. Ferrucci L, Fabbri E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol. 2018;15(9):505‐522. doi: 10.1038/s41569-018-0064-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C‐reactive protein. N Engl J Med. 2008;359:2195‐2207. doi: 10.1056/NEJMoa0807646 [DOI] [PubMed] [Google Scholar]
- 17. Shemtov SJ, Emani R, Bielska O, et al. The intestinal immune system and gut barrier function in obesity and ageing. FEBS J. 2023;290(17):4163‐4186. doi: 10.1111/febs.16558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Liu P, Li Y, Zhang Y, Mesbah SE, Ji T, Ma L. Frailty and hypertension in older adults: current understanding and future perspectives. Hypertens Res. 2020;43(12):1352‐1360. doi: 10.1038/s41440-020-0510-5 [DOI] [PubMed] [Google Scholar]
- 19. Vetrano DL, Palmer KM, Galluzzo L, et al. Hypertension and frailty: a systematic review and meta‐analysis. BMJ Open. 2018;8(12):1‐8. doi: 10.1136/bmjopen-2018-024406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yamamoto K. Current issues in frailty and hypertension management. Hypertens Res. 2023;46(8):1917‐1922. doi: 10.1038/s41440-023-01310-1 [DOI] [PubMed] [Google Scholar]
- 21. Ferri C, Ferri L, Desideri G. Management of hypertension in the elderly and frail elderly. High Blood Press Cardiovasc Prev. 2017;24(1):1‐11. doi: 10.1007/s40292-017-0185-4 [DOI] [PubMed] [Google Scholar]
- 22. Ambarish P, Dalane K, Gordon R. Frailty is intertwined with heart failure. JACC Hear Fail. 2019;7(12):1001‐1011. doi: 10.1016/j.jchf.2019.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Leong DP, Joseph P, McMurray JJV, et al. Frailty and outcomes in heart failure patients from high‐, middle‐, and low‐income countries. Eur Heart J. 2023;44(42):4435‐4444. doi: 10.1093/eurheartj/ehad595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dou Q, Wang W, Wang H, et al. Prognostic value of frailty in elderly patients with acute coronary syndrome: a systematic review and meta‐analysis. BMC Geriatr. 2019;19(1):222. doi: 10.1186/s12877-019-1242-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Borovac JA, Mohamed MO, Kontopantelis E, et al. Frailty among patients with acute ST‐elevation myocardial infarction in the United States: the impact of the primary percutaneous coronary intervention on in‐hospital outcomes. J Invasive Cardiol. 2022;34(1):E55‐E64. [DOI] [PubMed] [Google Scholar]
- 26. Garasto S, Fusco S, Corica F, et al. Estimating glomerular filtration rate in older people. Passarino G, editor. Biomed Res Int. 2014;2014:916542. doi: 10.1155/2014/916542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jiesisibieke ZL, Tung TH, Xu QY, et al. Association of acute kidney injury with frailty in elderly population: a systematic review and meta‐analysis. Ren Fail. 2019;41(1):1021‐1027. doi: 10.1080/0886022X.2019.1679644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mayes J, Young HML, Blacklock RM, Lightfoot CJ, Chilcot J, Nixon AC. Targeted non‐pharmacological interventions for people living with frailty and chronic kidney disease. Kidney Dial. 2022;2(2):245‐261. doi: 10.3390/kidneydial2020025 [DOI] [Google Scholar]
- 29. Abbatecola AM, Paolisso G, Corsonello A, Bustacchini S, Lattanzio F. Antidiabetic oral treatment in older people. Drugs Aging. 2009;26(1):53‐62. doi: 10.2165/11534660-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 30. Roy CN. Anemia in frailty. Clin Geriatr Med. 2011;27(1):67‐78. doi: 10.1016/j.cger.2010.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lee CT, Chen MZ, Yip CYC, Yap ES, Lee SY, Merchant RA. Prevalence of anemia and its association with frailty, physical function and cognition in community‐dwelling older adults: findings from the HOPE study. J Nutr Health Aging. 2021;25(5):679‐687. doi: 10.1007/s12603-021-1625-3 [DOI] [PubMed] [Google Scholar]
- 32. Vancampfort D, Stubbs B, Firth J, Koyanagi A. Handgrip strength, chronic physical conditions and physical multimorbidity in middle‐aged and older adults in six low‐ and middle income countries. Eur J Intern Med. 2019;61:96‐102. doi: 10.1016/j.ejim.2018.11.007 [DOI] [PubMed] [Google Scholar]
- 33. Leong DP, Teo KK, Rangarajan S, et al. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet. 2015;6736(14):1‐8. doi: 10.1016/S0140-6736(14)62000-6 [DOI] [PubMed] [Google Scholar]
- 34. Bonanni R, Cariati I, Tarantino U, D'arcangelo G, Tancredi V. Physical exercise and health: a focus on its protective role in neurodegenerative diseases. J Funct Morphol Kinesiol. 2022;7(2):38. doi: 10.3390/jfmk7020038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Baker JH. Meditation for reducing CVD risk. Integr Med Alert. 2018;21(5):57‐60. [Google Scholar]
- 36. Dent E, Lien C, Lim WS, et al. The Asia‐Pacific clinical practice guidelines for the management of frailty. J Am Med Dir Assoc. 2017;18(7):564‐575. doi: 10.1016/j.jamda.2017.04.018 [DOI] [PubMed] [Google Scholar]
- 37. Feart C. Nutrition and frailty: current knowledge. Prog Neuropsychopharmacol Biol Psychiatry. 2019;95:109703. doi: 10.1016/j.pnpbp.2019.109703 [DOI] [PubMed] [Google Scholar]
- 38. Le LT, Sabaté J. Beyond meatless, the health effects of vegan diets: findings from the adventist cohorts. Nutrients. 2014;6(6):2131‐2147. doi: 10.3390/nu6062131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Daccache A. Assoc between protein intake preval frailty among community‐dwelling leban older adults. [Doctoral Diss Leban Am Univ]. doi: 10.1093/cdn/nzac047.045 [DOI]
- 40. Harvie M, Howell A. Potential benefits and harms of intermittent energy restriction and intermittent fasting amongst obese, overweight and normal weight subjects – a narrative review of human and animal evidence. Behav Sci (Basel). 2017;7(1):4. doi: 10.3390/bs7010004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kassam Z, Smith M, Alm E, Larsen N, Vogensen FK, van den Berg FW. Bariatric surgery versus intensive medical therapy for diabetes. N Engl J Med. 2014;14(371):680‐682. doi: 10.1056/NEJMc1407393 [DOI] [PubMed] [Google Scholar]


