Abstract
Background
Non-suicidal self-injury (NSSI) is a significant public health concern among adolescents with major depressive disorders (MDD). Although previous research has linked child maltreatment (CM) to NSSI, the precise mechanisms remain unclear. This study aims to investigate the association between CM, cognitive reappraisal (CR), negative coping styles (NC) and NSSI in adolescents with MDD, from the perspectives of both Latent Variable Theory and the Network Theory of Mental Disorder.
Methods
A sample of 651 adolescents with MDD was recruited from January to December 2023. Data on CM, CR, NC, and NSSI were collected through paper-based self-reported questionnaires. Data analysis primarily involved structural equation modeling and network analysis.
Results
The reporting rate of NSSI among adolescents with MDD was 48.2%. CM showed a significant positive correlation with NSSI. NSSI was affected by CM through three paths: the mediating role of CR, the mediating role of NC, and the chain mediating role of both CR and NC. Emotional abuse (EA) was the central node, while NSSI, EA, and “The urge to cry quietly when faced with troubles“(NC10) were the key bridge nodes.
Conclusions
This study is the first to use both structural equation modeling and network analysis to explore the explore the relationship between CM, CR, NC, and NSSI in adolescents with MDD, providing a theoretical basis for future early prevention and targeted interventions for adolescents with MDD.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12888-024-06041-2.
Keywords: Non-suicidal self-injury, Child maltreatment, Negative coping styles, Cognitive reappraisal, Adolescents, Major depressive disorders
Introduction
In recent times, Non-Suicidal Self-Injury (NSSI) has emerged as a significant global public health concern [1]. It is now included in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) as a condition requiring further study [2]. NSSI is defined as the deliberate act of harming one’s body tissues or organs without suicidal intent [3]. This behavior, while not fatal, is not socially sanctioned. Research indicates that over 66% of adolescents who have attempted suicide have a history of NSSI [4]. The average age of onset for NSSI in non-clinical samples is approximately 13 years [5], and its prevalence is notably high among adolescents [6], with an increasing annual recurrence rate [7, 8]. Globally, the prevalence rates are estimated to be between 18 and 23% [9, 10], posing a serious threat to the psychophysical well-being of adolescents [11]. These include increased risks of social difficulties, psychiatric disorders, and heightened suicidal ideation and attempts [12]. Furthermore, NSSI is prevalently observed within adolescent populations accompanied by major depressive disorder (MDD) and is regarded as one of the prime predictive indicators for suicidal behaviors [13]. MDD is a common, multifactorial, recurrent, and chronic psychological disorder and a leading cause of disability worldwide, considered a major contributor to the global disease burden among adolescents [14, 15]. Previous research has found that roughly 40–60% of adolescents with MDD have a history of NSSI [16, 17]. Therefore, clarifying the pathways of NSSI occurrence in adolescents with MDD is crucial for early identification and prevention of NSSI, as well as for devising targeted intervention strategies. Research indicates that NSSI is influenced by multiple interacting factors [18, 19]. However, the predominant contributing factors remain unconfirmed.
Child maltreatment (CM) is defined as any act or failure to act by parents or other caregivers occurring before the age of 18 [20]. It includes emotional abuse (EA), physical abuse (PA), sexual abuse (SA), emotional neglect (EN), and physical neglect (PN). In a representative sample in the United States, the estimated prevalence of maltreatment by age 18 is 12.5%. In the United Kingdom, the maltreatment rate among children and adolescents aged 11 to 17 is 18.6% [21].Research indicates that CM, particularly EA and EN, serves as distal risk factors for NSSI among adolescents with MDD [22]. A one-year follow-up of outpatients with treatment-resistant depression showed that those with a history of CM had more challenges alleviating depressive symptoms and poorer outcomes [23]. In a retrospective study of 2,232 children, it was reported that those with a history of CM displayed an elevated risk of mental health issues, including depression, anxiety, and self-harm, by age 18 [24]. However, the exact mechanism by which CM influences NSSI remains undetermined at present.
James Gross’s model explains the generation and regulation of emotions in detail, identifying Cognitive Reappraisal (CR) as an adaptive emotion regulation strategy that regulates emotions, reduces perceived threats [25], and mitigates the effects of child maltreatment on adolescent NSSI [26]. CR is an emotion regulation strategy that involves altering one’s emotional response by reinterpreting the initial cognitive assessment of a situation. Specifically, it entails transforming an automatically generated negative thought into a more positive or neutral interpretation, thus changing its emotional impact [27, 28]. Research has discovered a negative correlation between child maltreatment and CR, with maltreated children exhibiting less usage of CR compared to those not maltreated [29]. Some studies have compared CR with Expressive Suppression (ES), which is considered a non-adaptive emotion regulation strategy. Findings from these studies indicate that CR is more effective than ES in reducing both the risk and severity of NSSI [30, 31]. Beyond this, CR has also been demonstrated to enhance individual stress coping mechanisms, subjective well-being, interpersonal relationships, and even alleviate physical discomfort [32]. Among offender populations, CR has been validated to diminish the impact of child maltreatment on NSSI [33]. Therefore, for adolescents who have experienced child maltreatment, effective utilization of CR may serve as a protective factor, aiding in the reduction of the risk associated with NSSI.
Conversely, the coping process model by Compas highlights that negative coping styles (NC), such as avoidance, suppression, and self-blame, may exacerbate negative effects [34]. Particularly for adolescents with a history of maltreatment, these negative strategies may worsen psychological trauma, thereby increasing the risk of NSSI. Coping strategies are cognitive processes and behaviors that an individual employs to manage or prevent harm and loss [35], and can be categorized as either positive or negative [36]. Recent research suggests that NC is associated with an increased risk of NSSI [37], and is significantly and positively correlated with child maltreatment, whereas individuals without a history of child maltreatment are more likely to adopt positive coping strategies [38].
According to the integrative theoretical model by Nock [39], the presence of distal risk factors such as child maltreatment may be associated with individual or interpersonal vulnerability factors for NSSI, such as poorer emotion regulation strategies [29]. A diminished capacity for cognitive reappraisal may exacerbate their reliance on negative coping styles, is associated with individuals adopting excessive or socially non-conforming coping mechanisms in the face of stressful events. Consequently, they may be more likely to resort to NSSI as a means to regulate emotions and navigate social situations.
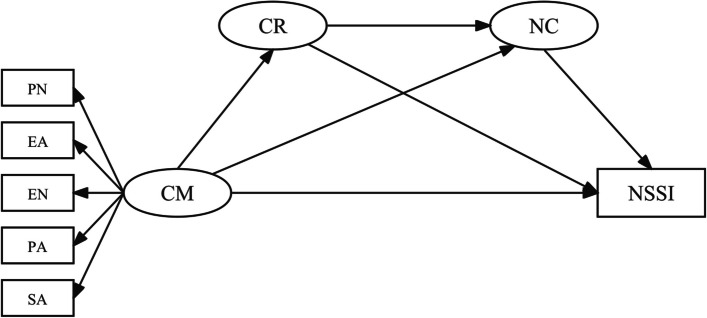
Based on current research, hypotheses are (see Fig. 1): Child maltreatment is positively associated with NSSI; cognitive reappraisal and negative coping styles mediate the association between child maltreatment and NSSI respectively; cognitive reappraisal and negative coping styles play a chained mediating role in the association between child maltreatment and NSSI.
Fig. 1.
The hypothesis model
Despite extensive prior research on the association between child maltreatment and NSSI, no studies have been found to concurrently examine the association among child maltreatment, cognitive reappraisal, negative coping styles, and NSSI from the perspectives of both Latent Variable Theory and the Network Theory of Mental Disorder. Latent Variable Theory posits that some variables (latent variables) cannot be directly observed or measured but can be indirectly inferred and measured through other observable variables (observed variables). While the Structural Equation Model (SEM) is effective in exploring the relationships between multiple latent variables simultaneously, it may overlook individual nuances and dynamic interactions among these variables [40]. In contrast, the Network Theory of Mental Disorder conceptualizes mental disorders as complex systems of interrelated and often mutually reinforcing symptoms [41]. Network analysis (NA) emphasizes direct interactions between individual symptoms and reveals potential complex interaction patterns among variables [42]. This study aims to explore both the associations and potential pathways of child maltreatment on NSSI among adolescents with MDD by using SEM. Concurrently, a symptom network will be established to analyze the interrelationships at the symptom level among child maltreatment, cognitive reappraisal, negative coping styles, and NSSI, identifying key nodes associated with NSSI.
Thus, integrating these methods allows researchers a more comprehensive and nuanced understanding of the relationships involved, presenting a methodological innovation that offers fresh insights into the associations underlying NSSI in adolescents with MDD, thereby aiding in effective and precise prevention and intervention strategies.
Methods
Participants and procedure
Participants for the current study were recruited patients diagnosed with MDD from the psychiatry department of Renmin Hospital of Wuhan University from January to December 2023. To ensure diagnostic rigor, two experienced psychiatrists diagnosed the patients using the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) [43]. Inclusion criteria included: (1) Ages 13–25 (The definition of the age of adolescents by the Chinese Public Security Department); (2) Diagnosis of an MDD based on DSM-5 standards; (3) Written consent from both the patient and their family. Exclusion criteria included: (1) Severe suicidal behavior, refusal to eat, or catatonia; (2) Serious drug side effects or major physical illnesses; (3) A history of brain-related organic disorders; (4) Co-occurrence of other psychiatric disorders.
To ensure a high response rate, researchers distributed paper questionnaires in person, assisted participants during the filling process, and collected them on the spot. Out of 700 questionnaires distributed, after excluding those with numerous missing entries due to participants discontinuing midway for personal reasons, 651 questionnaires remained valid, resulting in an effectiveness rate of 93.0%.
All participants signed a written informed consent form before participating in the study. Those under 18 obtained written permission from their parents. It took participants approximately 20 to 30 min to complete all the questions. The survey was conducted according to the latest version of the Declaration of Helsinki. This study was approved by the Ethics Committee of Renmin Hospital of Wuhan University (NO: WDRY2023-K159).
Measures
Non-suicidal self-injury (NSSI)
The Adolescent Non suicidal Self-Injury Behavior Questionnaire (ANSAQ) [44] is often used to assess non-suicidal self-injury behavior and functions in Chinese adolescents. The ANSAQ is divided into two sections: a behavior questionnaire and a function questionnaire. This study utilized the behavior questionnaire (Part One) to measure NSSI behavior, consisting of 12 items, scored using a Likert five-point scale ranging from 0 (never) to 4 (always). Higher scores indicate a greater severity of NSSI. Based on DSM-5 diagnostic criteria [45] and a structured interview with two trained psychiatrists, the patients included in the study were divided into groups with and without NSSI. In this study, the scales demonstrated good internal consistency (Cronbach’s alpha = 0.893).
Child maltreatment
The Childhood Trauma Questionnaire Short Form (CTQ-SF) [46] assesses emotional abuse(EA), physical abuse(PA), sexual abuse(SA), physical neglect(PN), and emotional neglect(EN). The CTQ-SF consists of 28 items, using a Likert five-point scale ranging from 1 (never) to 5 (always), with seven items scored in reverse. If the score for any subscale exceeds the relevant threshold, the participant is considered to have experienced child maltreatment: PA (> 9), SA (> 7), EA (> 12), PN (> 9), and EN (> 14) [47]. The Cronbach’s alpha coefficients for EA, PA, SA, PN, and EN were 0.827, 0.836, 0.849, 0.603, and 0.827, respectively. Except for PN, the four dimensions of the CTQ-SF demonstrated good internal consistency in this study. Therefore, the dimension of PN was excluded from subsequent data analyses.
Cognitive reappraisal
The Emotion Regulation Questionnaire (ERQ) [48] assesses emotion regulation strategies. The ERQ is divided into two subscales: cognitive reappraisal and expression suppression, encompassing a total of 10 items. This study utilized the cognitive reappraisal subscale to measure cognitive reappraisal, consisting of 6 items, with a Likert seven-point scale ranging from 1 (strongly disagree) to 7 (strongly agree). Higher scores indicate a higher frequency of employing cognitive reappraisal strategies. In the current sample, good internal consistency was demonstrated (Cronbach’s alpha = 0.866).
Negative coping styles
The Trait Coping Style Questionnaire [49] evaluates participants’ coping styles in response to life events. The questionnaire consists of two subscales: positive coping and negative coping, with a total of 20 items. This study focused on the negative coping subscale, which includes 10 items, utilizing a Likert five-point scale ranging from 1 (definitely no) to 5 (definitely yes). Higher scores indicate a greater intensity of negative coping methods. In the current sample, good internal consistency was exhibited (Cronbach’s alpha = 0.786).
Data analysis
SPSS (version 25.0) was used for descriptive statistics, Pearson correlation analysis, analysis of variance (ANOVA), and common method bias analysis. All data used in the structural equation model and network analysis were continuous variables.
Amos (version 28.0) was used for structural equation modeling analysis. Within this model, CM, represented by EA, PA, EN, and SA, served as the independent variable, while NSSI was the dependent variable. Cognitive reappraisal and negative coping styles functioned as mediating variables. Model fit indices comprised χ2/df (< 5), the comparative fit index (CFI > 0.90), the Tucker-Lewis index (TLI > 0.90), and the root mean square error of approximation (RMSEA < 0.08) [50]. Bootstrap analysis was used to investigate the mediating effects using 5000 bootstrap samples, with direct, indirect, and total effects being concurrently calculated.
R (version 5.4.1) was used for network analysis. In the network, each item (symptom) is represented as a node, and the associations between items are represented as edges. Thicker edges indicate stronger relationships between nodes. Nodes with stronger and more frequent connections are more concentrated in the network, forming dense areas. A community is a group of nodes (symptoms) that are more closely connected to each other than to nodes outside the group. A bridge is an edge that connects nodes from different communities. Edge color indicates the correlation between nodes: red denotes a negative correlation, while purple denotes a positive correlation. The qgraph package (Version 4.2.3) [51] was used for network estimation. Given that all data are derived from Likert scales, approximating continuous variables, partial correlation analysis is employed to calculate the association of each symptom, after controlling for all other variables included in the network [52]. The Least Absolute Shrinkage and Selection Operator (LASSO) method [53] was used to diminish spurious edges in the network, while the Extended Bayesian Information Criterion (EBIC) was used to select the optimal fitting model, with a tuning parameter of 0.5 [54]. Node centrality was applied to quantitatively describe the structural importance of each node in the network, identifying the more influential nodes [55]. Evidence suggests that EI is particularly apt for determining nodes in networks with both positive and negative connections [56]. Centrality metrics were given as z-score values. The networktools package (version 4.2.2) was used to calculate bridge centrality [57], with bridge expected influence (1-step) serving as the bridge centrality in this study. The mgm package (version 1.2–14) [58] was used for estimating the predictability of each node. The bootnet package (Version 1.4.3) [52] was used to assess the accuracy and stability of network estimation through bootstrap methods. Accuracy was estimated by plotting the 95% confidence intervals (CI) of edge weights, while stability was assessed both graphically and quantitatively by calculating the correlation stability coefficient (CS-coefficient). The CS coefficient should not be lower than 0.25 and is preferably above 0.5.
In studying adolescent NSSI, a strong correlation between age and NSSI persists. Therefore, this study controls for age by including it as a covariate. In this study, 95% CI that did not include zero signified significant effects. A two-sided P-value < 0.05 indicated significant differences.
Results
Test of common method bias
To control for the common method bias problem, Harman’s single-factor test was conducted. Results yielded nine factors with eigenvalues > 1, and the first unrotated factor accounted for 21.91% of the variance, falling below the 40% threshold, indicating no significant common method bias in this study [59].
Participant characteristics
The study included 651 participants, aged 13 to 25 years.48.2% (314 participants) reported engaging in NSSI. The detection rates for emotional abuse, emotional neglect, physical abuse, and sexual abuse were 32.7%, 49.9%, 20.1%, and 14.7%, respectively. Table 1 presents details characteristics on age, gender, nation, religion, only child status, birthplace, education, left-behind children status, and first episode for first occurrence of MDD.
Table 1.
Characteristics of participants, n(%) (N = 651)
| Characteristics | No NSSI | NSSI | χ2 | Cramér’s V | p-value | |
|---|---|---|---|---|---|---|
| Age | 20.897 | 0.179 | < 0.001** | |||
| 13 ~ 19 | 136(40.4) | 183(58.3) | ||||
| 20 ~ 25 | 201(59.6) | 131(41.7) | ||||
| Gender | 13.802 | 0.146 | < 0.001** | |||
| male | 139(41.2) | 86(27.4) | ||||
| female | 198(58.8) | 228(72.6) | ||||
| Nation | 0.000 | 0.001 | 0.986 | |||
| Han | 321(95.3) | 299(95.2) | ||||
| minority | 16(4.7) | 15(4.8) | ||||
| Religion | 5.471 | 0.092 | 0.019* | |||
| yes | 6(1.8) | 16(5.1) | ||||
| no | 331(98.2) | 298(94.9) | ||||
| Only children | 2.833 | 0.066 | 0.092 | |||
| yes | 196(58.2) | 162(51.6) | ||||
| no | 141(41.8) | 152(48.4) | ||||
| Birthplace | 3.554 | 0.074 | 0.169 | |||
| urban | 141(41.8) | 142(45.2) | ||||
| town | 98(29.1) | 101(32.2) | ||||
| rural | 98(29.1) | 71(22.6) | ||||
| Education | 26.554 | 0.202 | < 0.001** | |||
| middle school and below | 33(9.8) | 76(24.2) | ||||
| high school | 113(33.5) | 104(33.1) | ||||
| college | 191(56.7) | 134(42.7) | ||||
| Left-behind children | 5.697 | 0.094 | 0.017* | |||
| yes | 59(17.5) | 79(25.2) | ||||
| no | 278(82.5) | 235(74.8) | ||||
| First episode | 2.845 | 0.066 | 0.092 | |||
| yes | 123(36.5) | 95(30.3) | ||||
| no | 214(63.5) | 219(69.7) | ||||
Age groups are defined per WHO’s adolescent age definition into 10–19 [60] and 20–25 years; Left-behind children [61] defined as those who remain in their hometowns under the care of other relatives such as grandparents, other family members, or guardians, while at least one parent works away from home or is absent for an extended period before the child turns 18. First episode refers to the first occurrence of MDD
*P < 0.05
**P < 0.01
Correlation of child maltreatment, cognitive reappraisal, negative coping styles, and NSSI
The means, standard deviations, and bivariate correlations among the study variables are presented in Table 2. Emotional abuse, physical abuse, sexual abuse, emotional neglect, negative coping styles, and NSSI were all significantly and positively associated with each other (p < 0.05). In contrast, cognitive reappraisal was significantly and negatively associated with the other variables (p < 0.05). Importantly, tolerance values for emotional abuse, physical abuse, sexual abuse, emotional neglect, negative coping styles, and cognitive reappraisal were all above 0.1, and the Variance Inflation Factor (VIF) values were below 5, suggesting no multicollinearity issues.
Table 2.
Means, standard deviations, and bivariate correlations among study variables (N = 651)
| Variables | Emotional Abuse | Emotional Neglect | Physical Abuse | Sexual Abuse | Cognitive Reappraisal | Negative Coping Styles | NSSI |
|---|---|---|---|---|---|---|---|
| Emotional Abuse | 1 | ||||||
| Emotional Neglect | 0.497** | 1 | |||||
| Physical Abuse | 0.603** | 0.358** | 1 | ||||
| Sexual Abuse | 0.279** | 0.176** | 0.234** | 1 | |||
| Cognitive Reappraisal | − 0.318** | − 0.224** | − 0.189** | − 0.086* | 1 | ||
| Negative Coping Styles | 0.360** | 0.152** | 0.213** | 0.145** | − 0.378** | 1 | |
| NSSI | 0.465** | 0.183** | 0.297** | 0.158** | − 0.391** | 0.466** | 1 |
| M | 10.78 | 14.17 | 7.50 | 6.08 | 25.29 | 34.98 | 7.10 |
| SD | 5.02 | 5.57 | 3.63 | 2.57 | 7.47 | 6.68 | 7.90 |
NSSI Non-suicidal self-injury
*P<0.05
**P<0.01
Structural equation Model
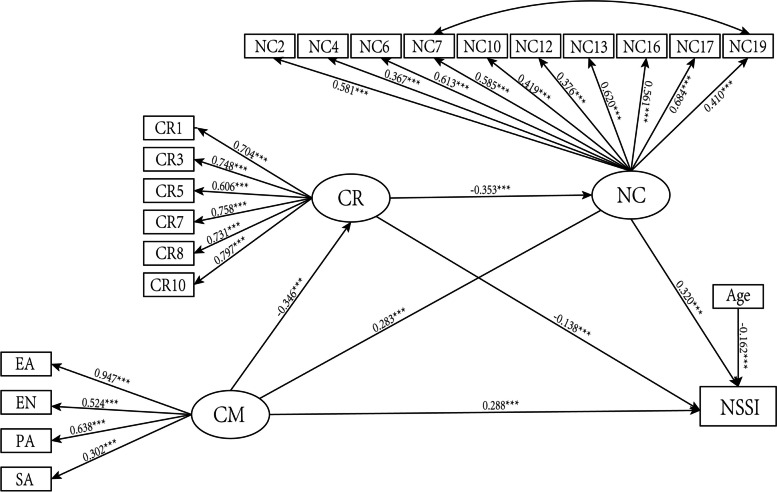
Figure 2 illustrates the chain mediation model depicting the association between child maltreatment, cognitive reappraisal, negative coping styles and NSSI. The mediation values of cognitive reappraisal and negative coping styles in these associations are provided in Table 3. The data fit the hypothesized chain mediation model well, as evidenced by the following fit indices: χ2/df = 2.823, p < 0.001; CFI = 0.913; TLI = 0.901; and RMSEA = 0.053. In line with our expectations, both cognitive reappraisal and negative coping styles were significantly associated with the relationship between child maltreatment and NSSI. The model revealed a total effect of child maltreatment on NSSI of 0.466 (p < 0.001, 95% CI [0.388, 0.538]) and a direct effect of 0.288 (p < 0.001, 95% CI [0.203, 0.376]). Mediation accounted for 38.10% of the total effect. The path from child maltreatment to NSSI through cognitive reappraisal is significant (Estimate = 0.048, p = 0.001, 95% CI [0.021, 0.077]), contributing to 10.2% of the total effect. The path from child maltreatment to NSSI through negative coping styles is significant(Estimate = 0.091, p < 0.001, 95% CI [0.062, 0.129]), contributing to 19.5% of the total effect. The path from child maltreatment to NSSI through both cognitive reappraisal and negative coping styles is significant (Estimate = 0.039, p < 0.001, 95% CI [0.024, 0.061]), contributing to 8.4% of the total effect. The difference between the mediating effects of cognitive reappraisal and negative coping styles (DIFF1) was significant (p < 0.05), as was the difference between the mediating effect of negative coping styles and the chain mediating effect (DIFF3) (p < 0.05). However, the difference between the mediating effect of cognitive reappraisal and the chain mediating effect (DIFF2) was not significant. The negative estimate of DIFF1 indicates that cognitive reappraisal has a weaker effect compared to negative coping styles, while the positive estimate of DIFF3 suggests that negative coping styles have a stronger effect than the chain mediating effect.
Fig. 2.
The chain mediation model for childhood maltreatment, cognitive reappraisal, negative coping styles and NSSI. *** < 0.001
Table 3.
CM and NSSI in the mediation effect analysis
| Relationship | Estimate | S.E. | 95%CI | p | Ratio of indirect to total effect | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| CM→CR | -0.346 | 0.044 | -0.431 | -0.258 | < 0.001 | |
| CM→NC | 0.283 | 0.043 | 0.198 | 0.369 | < 0.001 | |
| CR→NC | -0.353 | 0.049 | -0.443 | -0.251 | < 0.001 | |
| CR→NSSI | -0.138 | 0.041 | -0.214 | -0.054 | 0.002 | |
| NC→NSSI | 0.320 | 0.040 | 0.237 | 0.394 | < 0.001 | |
| Direct effect | 0.288 | 0.044 | 0.203 | 0.376 | < 0.001 | |
| Mediating effect of CR | 0.048 | 0.014 | 0.021 | 0.077 | 0.001 | 10.2% |
| The mediating effect of NC | 0.091 | 0.016 | 0.062 | 0.129 | < 0.001 | 19.5% |
| Chain mediating effect | 0.039 | 0.009 | 0.024 | 0.061 | < 0.001 | 8.4% |
| Total indirect effect | 0.177 | 0.022 | 0.139 | 0.226 | < 0.001 | 38.1% |
| Total effect | 0.466 | 0.038 | 0.388 | 0.538 | < 0.001 | |
| DIFF1 | -0.043 | 0.022 | -0.088 | -0.001 | 0.044 | |
| DIFF2 | 0.008 | 0.018 | -0.033 | 0.040 | 0.662 | |
| DIFF3 | 0.052 | 0.019 | 0.017 | 0.091 | 0.005 | |
All variables in the model have been standardized
DIFF1: the difference between the mediating effects of cognitive reappraisal and negative coping styles
DIFF2: the difference between the mediating effect of cognitive reappraisal and the chain mediating effect
DIFF3: the difference between the mediating effect of negative coping styles and the chain mediating effect
Network analysis
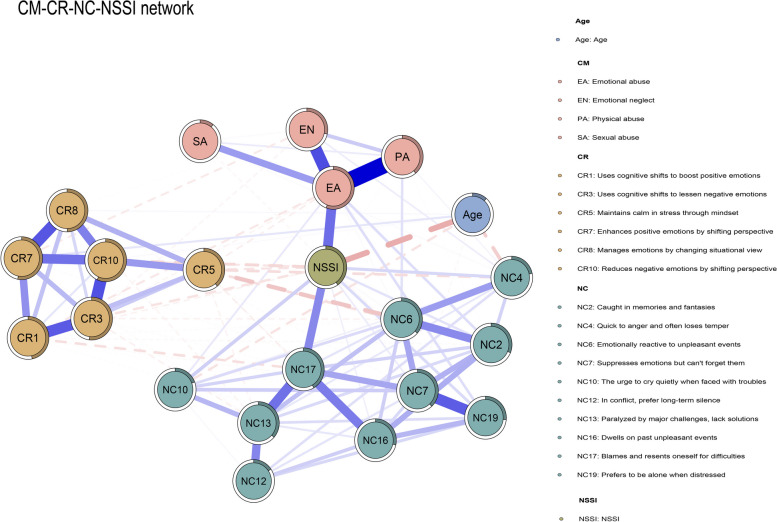
The structure of the CM-CR-NC-NSSI network is depicted in Fig. 3. Four strongest edges are between EA-PA (weight = 0.41), EA-EN (weight = 0.29), CR3-CR10 (weight = 0.28) and CR7-CR8 (weight = 0.27). Within the CM community, EA demonstrated the strongest correlation with NSSI (weight = 0.24). In the CR community, CR10 showed the strongest correlation with NSSI (weight = -0.06). Within the NC community, NC17 had the strongest correlation with NSSI (weight = 0.19). Across the CM and CR communities, the strongest correlation was between EA and CR1 (weight = -0.04); between the CM and NC communities, the strongest was between EA and NC19 (weight = 0.05); and between the CR and NC communities, the strongest link was between CR5 and NC6 (weight = -0.09). All edge weights within the CM-CR-NC-NSSI network can be found in Table S1 (in Supplemental Material). The bootstrapped 95%CI for these edges is relatively narrow, indicating a relatively accurate estimation of the edge weights (Fig. S1 in Supplementary Material).
Fig. 3.
Network structure of CM-CR-NC-NSSI symptoms. Purple edges represent positive correlations, red dashed edges represent negative correlations. The thickness of the edge reflects the magnitude of the correlation. Cut value = 0.05
The network’s overall mean predictability is 0.354, meaning the average variance for each node, as explained by its directly connected nodes, is 35.4%. The predictability of all nodes can be found in Table S2 (in Supplemental Material).
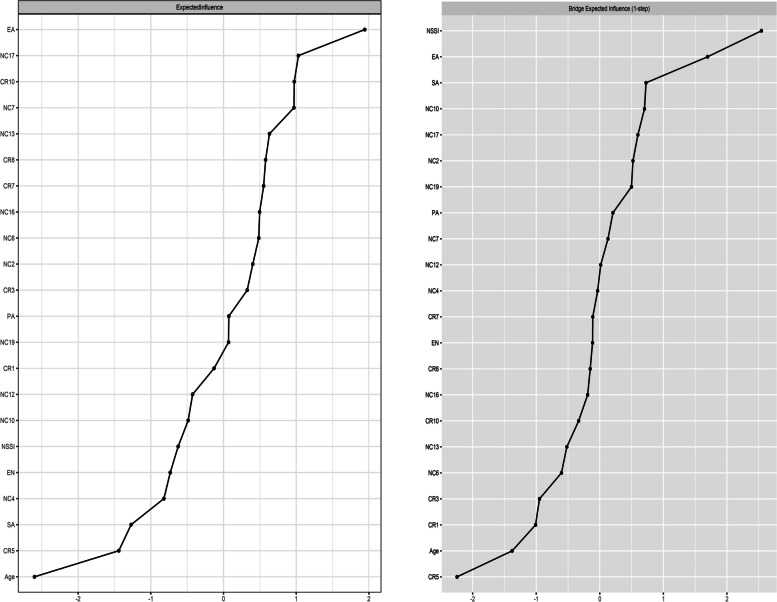
Figure 4 depicts the node and bridge centrality, both expressed as z-scores, within the CM-CR-NC-NSSI network. Within this network, EA (EI:1.110) stands out with the highest node centrality, underscoring its dominant influence. NSSI (BEI:0.389) possesses the greatest bridge centrality, suggesting its significant impact on other communities, followed by EA (BEI:0.259) and “The urge to cry quietly when faced with troubles” (NC10; BEI:0.106). NSSI is most closely connected to “Blames and resents oneself for difficulties” (NC17) from other communities, EA and NC10 are most closely connected to NSSI from other communities. The EI and BEI of all nodes can be found in Table S3 (in Supplemental Material). The CS coefficients for both node and bridge expected influences are 0.594 and 0.673, respectively, demonstrating their substantial stability (Fig. S2 and Fig.S3 in Supplementary Material). Fig. S4 and Fig. S5 (in Supplementary Material) present the bootstrapped difference tests for node centrality and edge weights.
Fig. 4.
The node centrality (EI) and bridge centrality (BEI) of the CM-CR-NC-NSSI network (z-score)
Discussion
This is the first study to explore the association between child maltreatment, cognitive reappraisal, negative coping styles and NSSI in adolescents with MDD from both a macro (Structural Equation Model) and micro (Network Analysis) perspective. In this study, after controlling for age, the associations between variables are as follows: child maltreatment is directly associated with NSSI. Cognitive reappraisal is negatively associated with NSSI and mediates the relationship between child maltreatment and NSSI. Negative coping styles are also directly associated with NSSI and serve as a mediator between child maltreatment and NSSI. Together, cognitive reappraisal and negative coping styles form a serial mediation pathway linking child maltreatment to NSSI. More frequent use of negative coping styles and less frequent use of cognitive reappraisal are associated with a stronger association between child maltreatment and NSSI. Core symptoms identified in the network include emotional abuse (EA); key bridge symptoms at the symptom include NSSI, EA, and “The urge to cry quietly when faced with troubles” (NC10).
In the present study, the prevalence of NSSI among adolescents with MDD was 48.2%, aligning with previous studies where it exceeded 40% [17, 62], underscoring the severity of NSSI in this demographic. Compared to other types of child maltreatment, emotional neglect had the highest prevalence (49.9%), while sexual abuse had the lowest prevalence (14.7%), which is consistent with the study by Yu et al. [63]. However, prevalence rates may vary across studies depending on factors such as research methodology, sample selection criteria (e.g., age and gender distribution), measurement instruments used for assessing child maltreatment as well as regional and cultural differences.
This study validated the association between child maltreatment and NSSI in adolescents with MDD. The results of the network analysis revealed that emotional abuse (EA) was most strongly associated with NSSI in both communities, child maltreatment and NSSI, which is consistent with previous research [64]. Multiple studies have demonstrated that there is a positive correlation between EA and NSSI. Adolescents and adults who have endured EA are more prone to turn to NSSI as a coping strategy to alleviate their psychological distress [65, 66], a behavior that may stem from their attempts to control or escape the negative emotions associated with their abusive experiences. Simultaneously, EA emerges as a central node within the overarching network, significantly influencing the its stability. However, Misiak et al. found sexual abuse to be the most central symptom in their network analysis, a finding inconsistent with this study [67]. This discrepancy may stem from regional or cultural differences. In China, traditional educational approaches often emphasize authority and obedience. High expectations and strict discipline might lead to emotional abuse being overlooked or normalized within family and school settings, exacerbating its impact [68, 69].The prevention of EA, along with subsequent interventions, is crucial in averting long-term psychological damage and fostering recovery.
The current study suggests that cognitive reappraisal may partially mediate the association between child maltreatment and NSSI. When a person experiences a traumatic event, such as child maltreatment, their brain may develop a heightened stress response. This response may be associated with a greater tendency toward negative emotions when faced with stress [70]. To cope with these emotions, they may use different emotion regulation strategies, including cognitive reappraisal. However, not all individuals who have experienced child maltreatment use cognitive reappraisal effectively. Several studies have suggested that abuse experiences may be associated with changes in certain brain areas, such as the prefrontal cortex and amygdala, which are associated with emotion regulation and decision-making [71]. Additionally, Schore’s psychoneurobiological model suggests that individuals with insecure attachments in infancy may be less likely to develop effective emotion regulation skills [72]. Thus, for these individuals, even if they try to use cognitive reappraisal, it may be difficult to effectively regulate emotion, resulting in NSSI. This may be one of the reasons why cognitive reappraisal had a lesser mediating role in the results of this study. Helping infants develop secure attachments may be an effective method for enhancing emotional regulation skills in adolescents. Attachment-based family therapy can enable adolescents to identify and express emotions to their parents, potentially re-establishing secure attachment relationships [73].
The greater association of negative coping styles compared to cognitive reappraisal in mediating the association between child maltreatment and NSSI was evident in both SEM and NA results. Individuals with extensive child maltreatment histories are more likely to rely on negative coping styles such as wishful thinking, problem avoidance, social withdrawal, and self-criticism [74], and elevated levels of negative coping styles have been linked to an increased risk of NSSI [36]. Child maltreatment often imposed by parents or caregivers, creates an unhealthy environmental backdrop where children may develop significant interpersonal trust issues and learned helplessness. Consequently, these individuals might resort to maladaptive coping strategies such as smoking, excessive alcohol consumption, drug dependency, or engaging in NSSI. These behaviors may serve as means to alleviate their profound feelings of emptiness and insecurity [36, 75]. Among the three communities of child maltreatment, negative coping styles, and NSSI, EA is strongly associated with “Preferring to be alone when distressed” (NC19). This tendency to be “alone” may be an avoidance strategy to avoid confronting problems or painful emotions. Excessive solitude may hinder effective problem-solving and restrict access to support or other forms of assistance, potentially leading to chronic low levels of social support and an increased risk of depression. Research indicates that support sources differ by age, with parental support playing a crucial role for children and adolescents [76]. The “Blames and resents oneself for difficulties” (NC17) shows the strongest correlation with NSSI. Such intense self-blame and guilt may be associated with low self-esteem, feelings of helplessness, or diminished self-efficacy, all of which are prevalent in various mental health issues and are linked to an increased risk of NSSI [77, 78].
We also illustrated the potential chain mediation pathway of cognitive reappraisal and negative coping styles in the association between child maltreatment and NSSI, a contribution that may deepen our comprehension of this complex interrelation. When faced with negative life events such as child maltreatment, the failure of cognitive reappraisal as an emotion regulation strategy may result in individuals exhibiting negative coping behaviors, which could be associated with NSSI. This finding is consistent with Nock’s integrative theoretical model [39].
In the network model, a higher bridge EI indicates a greater likelihood of activating the communities connected by the nodes. We identified three key bridge symptoms: NSSI, emotional abuse (EA), and “The urge to cry quietly when faced with troubles” (NC10). Notably absent was a node for cognitive reappraisal, further corroborating the SEM outcomes of this study, which highlighted the mediating effect of negative coping styles as the most substantial among the three intermediary pathways examined. This is consistent with the findings of Voon et al., suggesting that adolescents who engage in NSSI are more likely to use emotion regulation processes that exacerbate negative emotional states compared to their non-NSSI peers, rather than those that could reduce these emotions (i.e., cognitive reappraisal) [31]. Within this framework, prioritizing the prevention of EA and education on appropriate coping strategies becomes particularly critical. Preventing EA requires efforts not just at the individual level, but also a collective commitment from various sectors of society, especially within educational and familial settings. This may involve enhancing awareness of EA, increasing public consciousness of its potential dangers, and establishing effective intervention mechanisms. Additionally, providing essential psychological support to patients who have endured child maltreatment, including counseling, emotion management skills training, and the establishment of support networks, is a crucial step. Concurrently, patients can be taught proper coping techniques through well-established psychological therapies, such as cognitive-behavioral therapy (CBT), coping skills training, and mindfulness practices. These approaches aim to assist patients in developing more adaptive coping mechanisms, bolstering psychological resilience, and thereby maintaining emotional stability when confronted with negative life events [79, 80]. In terms of cognitive reappraisal, due to the association between MDD in adolescents and difficulties with cognitive reassessment, adolescents with MDD report using cognitive reappraisal less frequently [81]. It is crucial to focus on teaching them effective cognitive reappraisal strategies, enabling adolescents with MDD to better and more effectively use cognitive reappraisal strategies. Emotion Regulation Training [82], Cognitive Behavioral Therapy (CBT) and Mindfulness-Based Cognitive Therapy (MBCT) [83] can all be instrumental in this regard.
There are several limitations to this study. First, as a single-center cross-sectional study, it primarily reveals correlations between child maltreatment, cognitive reappraisal, negative coping styles, and NSSI without establishing causality. The findings, therefore, may not be generalizable across different populations or settings. To address this, future research should consider multicenter longitudinal studies. Such studies would not only clarify causality but also offer insights into the temporal dynamics of these relationships and their variation across diverse demographic and cultural backgrounds. Additionally, the questionnaires used in this study were self-reported, and recall bias may occur. A significant limitation was the exclusion of the PN dimension due to poor internal consistency in the measurement tools. This low internal consistency could be attributed to the tools themselves or potentially to issues in the data collection process, such as inconsistencies in how participants understood or responded to the questions. This exclusion limits our understanding of the full spectrum of child maltreatment. Future research should not only focus on developing or identifying more reliable and valid tools to assess the PN dimension but also ensure that the data collection process is rigorous and standardized. This could involve pilot testing the tools to refine questions for clarity and consistency, training researchers to ensure uniform administration of the survey, and employing methodologies that reduce the likelihood of misinterpretation or inconsistent responses. Another significant limitation of our study is its exclusive focus on MDD, intentionally excluding other psychiatric disorders to reduce confounding factors and accentuate the unique characteristics of MDD. However, the high prevalence of comorbidity between MDD and other psychiatric conditions, especially among individuals with a history of trauma, constrains the generalizability of our findings. This methodological decision limits our insights to a narrow subgroup of MDD patients who do not present with additional psychiatric disorders. Future research should include a more diverse sample of psychiatric comorbidities to enhance the generalizability and practical utility of the findings. Finally, regarding the inclusion criteria of this study, the age range for adolescents with MDD was determined based on the standards set by China’s Ministry of Public Security. However, early adulthood (e.g., 21–25 years) is characterized by significantly different neural and cognitive development compared to adolescence (13–15 years), and individuals in these age groups face different challenges and environmental influences. Therefore, a more detailed comparative analysis of MDD patients in middle/high school versus those in university or the workforce would be beneficial. Future research should consider factors such as neural and cognitive development to more accurately define adolescence. This approach will enhance the comparability of findings across different cultural contexts and improve the targeting of prevention and intervention strategies.
Conclusions
This study is the first to use both structural equation modeling and network analysis to explore the association between child maltreatment, cognitive reappraisal, negative coping styles, and NSSI in adolescents with MDD. This study found that in the mediation between child maltreatment and NSSI, the mediating role of negative coping styles is relatively more pronounced. This might be associated with the physiological mechanisms impacted by child maltreatment, which affect the effective use of cognitive reappraisal in adolescents with MDD. Concurrently, the study identified both central symptom (EA) and bridge symptoms (NSSI, EA, and NC10 "The urge to cry quietly when faced with troubles”). The integration of these two approaches, examining both macroscopic and microscopic (symptomatic) perspectives, mutually reinforces their validity, providing a theoretical basis for early prevention and targeted intervention of NSSI in adolescents with MDD. The study emphasizes the importance of incorporating strategies to enhance cognitive reappraisal and reduce negative coping styles in therapeutic interventions for adolescents who have experienced child maltreatment.
Supplementary Information
Acknowledgements
We thank all the participants for completing the questionnaires.
Authors’ contributions
Yinglin Li: Methodology, Data collection, Formal analysis, Investigation, Writing - original draft. Zhiying Wan: Methodology, Data collection, Formal analysis, Investigation, Writing - original draft. Zhongxiang Cai: Conceptualization, Methodology, Supervision. Xuan Gong: Methodology, Writing - review & editing, Supervision. Li Wen: Conceptualization, Methodology, Supervision. Ting Sun: Investigation, Writing - review & editing. Jingfang Liu: Data collection, Investigation.Xiangying Xie: Data collection, Writing - review & editing, Investigation. Chunlong Zhang: Data collection, Investigation.
Funding
This work was supported by grants from the Hubei Province Key Laboratory Open Project (2021KFH013, 2022KFH001), the Cross Innovative Talent Project of Renmin Hospital of Wuhan University (JCRCGW-2022-010), the Wuhan Nursing Association Research Project (WHHL202202), and Wuhan University Clinical Nursing Special Research and Cultivation Fund Project (LCHL202301).
Availability of data and materials
The datasets generated andanalyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
We obtained written informed consent from patients or their legal guardians.
The survey was conducted according to the latest version of the Declaration of Helsinki. This study was approved by the Ethics Committee of Renmin Hospital of Wuhan University (NO: WDRY2023-K159).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
The original version of this article was revised: the ethics approval number has been corrected.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yinglin Li and Zhiying Wan contributed equally to this work.
Change history
12/4/2024
A Correction to this paper has been published: 10.1186/s12888-024-06242-9
References
- 1.Mars B, Heron J, Klonsky ED, et al. Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: a population-based birth cohort study. Lancet Psychiatry. 2019;6:327–37. 10.1016/S2215-0366(19)30030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hooley JM, Fox KR, Boccagno C. Nonsuicidal Self-Injury: Diagnostic challenges and current perspectives. Neuropsychiatr Dis Treat Volume. 2020;16:101–12. 10.2147/NDT.S198806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nock MK. Self-Injury. Annu Rev Clin Psychol. 2010;6:339–63. 10.1146/annurev.clinpsy.121208.131258. [DOI] [PubMed] [Google Scholar]
- 4.Voss C, Hoyer J, Venz J, et al. Non-suicidal self‐injury and its co‐occurrence with suicidal behavior: an epidemiological‐study among adolescents and young adults. Acta Psychiatr Scand. 2020;142:496–508. 10.1111/acps.13237. [DOI] [PubMed] [Google Scholar]
- 5.Swannell SV, Martin GE, Page A, et al. Prevalence of Nonsuicidal Self-Injury in Nonclinical samples: systematic review, Meta‐Analysis and Meta‐Regression. Suicide Life Threat Behav. 2014;44:273–303. 10.1111/sltb.12070. [DOI] [PubMed] [Google Scholar]
- 6.Ammerman BA, McCloskey MS. The development of a measure to assess social reactions to Self-Injury Disclosure. Assessment. 2021;28:225–37. 10.1177/1073191120903081. [DOI] [PubMed] [Google Scholar]
- 7.Liu RT, Walsh RFL, Sheehan AE, et al. Prevalence and correlates of suicide and nonsuicidal self-injury in children: a systematic review and Meta-analysis. JAMA Psychiatry. 2022;79:718. 10.1001/jamapsychiatry.2022.1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poudel A, Lamichhane A, Magar KR, Khanal GP. Non suicidal self injury and suicidal behavior among adolescents: co-occurrence and associated risk factors. BMC Psychiatry. 2022;22:96. 10.1186/s12888-022-03763-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steinhoff A, Ribeaud D, Kupferschmid S, et al. Self-injury from early adolescence to early adulthood: age-related course, recurrence, and services use in males and females from the community. Eur Child Adolesc Psychiatry. 2021;30:937–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.You J, Leung F, Fu K, Lai CM. The prevalence of Nonsuicidal Self-Injury and different subgroups of self-injurers in Chinese adolescents. Arch Suicide Res. 2011;15:75–86. 10.1080/13811118.2011.540211. [DOI] [PubMed] [Google Scholar]
- 11.Mannekote Thippaiah S, Shankarapura Nanjappa M, Gude JG, et al. Non-suicidal self-injury in developing countries: a review. Int J Soc Psychiatry. 2021;67:472–82. 10.1177/0020764020943627. [DOI] [PubMed] [Google Scholar]
- 12.Wichstrøm T, Wichstrøm L. Childhood predictors of nonsuicidal self-injury in adolescence: a birth cohort study. J Am Acad Child Adolesc Psychiatry S089085672400073X. 2024. 10.1016/j.jaac.2023.12.013. [DOI] [PubMed] [Google Scholar]
- 13.Castellví P, Lucas-Romero E, Miranda-Mendizábal A, et al. Longitudinal association between self-injurious thoughts and behaviors and suicidal behavior in adolescents and young adults: a systematic review with meta-analysis. J Affect Disord. 2017;215:37–48. 10.1016/j.jad.2017.03.035. [DOI] [PubMed] [Google Scholar]
- 14.Gore FM, Bloem PJ, Patton GC, et al. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet. 2011;377:2093–102. 10.1016/S0140-6736(11)60512-6. [DOI] [PubMed] [Google Scholar]
- 15.Messaoud A, Mensi R, Mrad A, et al. Is low total cholesterol levels associated with suicide attempt in depressive patients? Ann Gen Psychiatry. 2017;16:20. 10.1186/s12991-017-0144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hu C, Jiang W, Wu Y, et al. Microstructural abnormalities of white matter in the cingulum bundle of adolescents with major depression and non-suicidal self-injury. Psychol Med. 2023;1–9. 10.1017/S003329172300291X. [DOI] [PubMed]
- 17.Wang L, Liu J, Yang Y, Zou H. Prevalence and risk factors for non-suicidal self-injury among patients with depression or bipolar disorder in China. BMC Psychiatry. 2021;21:389. 10.1186/s12888-021-03392-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forster M, Grigsby TJ, Gower AL, et al. The role of Social Support in the Association between Childhood Adversity and adolescent self-injury and suicide: findings from a Statewide Sample of High School Students. J Youth Adolesc. 2020;49:1195–208. 10.1007/s10964-020-01235-9. [DOI] [PubMed] [Google Scholar]
- 19.Gromatsky MA, He S, Perlman G, et al. Prospective prediction of First Onset of Nonsuicidal Self-Injury in adolescent girls. J Am Acad Child Adolesc Psychiatry. 2020;59:1049–57. 10.1016/j.jaac.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 20.Gilbert R, Widom CS, Browne K, et al. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68–81. 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- 21.Angelakis I, Austin JL, Gooding P. Association of Childhood Maltreatment with suicide behaviors among Young people: a systematic review and Meta-analysis. JAMA Netw Open. 2020;3:e2012563. 10.1001/jamanetworkopen.2020.12563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shao C, Wang X, Ma Q, et al. Analysis of risk factors of non-suicidal self-harm behavior in adolescents with depression. Ann Palliat Med. 2021;10:9607613–9613. 10.21037/apm-21-1951. [DOI] [PubMed] [Google Scholar]
- 23.Yrondi A, Aouizerate B, Bennabi D, et al. Childhood maltreatment and clinical severity of treatment-resistant depression in a French cohort of outpatients (FACE‐DR): one‐year follow‐up. Depress Anxiety. 2020;37:365–74. 10.1002/da.22997. [DOI] [PubMed] [Google Scholar]
- 24.Newbury JB, Arseneault L, Moffitt TE, et al. Measuring childhood maltreatment to predict early-adult psychopathology: comparison of prospective informant-reports and retrospective self-reports. J Psychiatr Res. 2018;96:57–64. 10.1016/j.jpsychires.2017.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gross JJ. The emerging field of emotion regulation: an integrative review. Rev Gen Psychol. 1998;2:271–99. 10.1037/1089-2680.2.3.271. [Google Scholar]
- 26.Gu H, Yao Y, He F, Cheng Y. Harsh parenting and adolescent non-suicidal self-injury: a moderated mediation model of alienation and cognitive reappraisal. Child Abuse Negl. 2023;141:106188. 10.1016/j.chiabu.2023.106188. [DOI] [PubMed] [Google Scholar]
- 27.Toh WX, Keh JS, Gross JJ, Carstensen LL. The role of executive function in cognitive reappraisal: a meta-analytic review. Emotion. 2024. 10.1037/emo0001373. [DOI] [PubMed] [Google Scholar]
- 28.Buhle JT, Silvers JA, Wager TD, et al. Cognitive reappraisal of emotion: a Meta-analysis of human neuroimaging studies. Cereb Cortex. 2014;24:2981–90. 10.1093/cercor/bht154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sistad RE, Simons RM, Mojallal M, Simons JS. The indirect effect from childhood maltreatment to PTSD symptoms via thought suppression and cognitive reappraisal. Child Abuse Negl. 2021;114:104939. 10.1016/j.chiabu.2021.104939. [DOI] [PubMed] [Google Scholar]
- 30.Voon D, Hasking P, Martin G. The roles of emotion regulation and ruminative thoughts in non-suicidal self-injury. Br J Clin Psychol. 2014;53:95–113. 10.1111/bjc.12030. [DOI] [PubMed] [Google Scholar]
- 31.Voon DTW. (2017) Emotion regulation processes in adolescent non-suicidal self-injury (NSSI): the roles of cognitive reapprasxpressive suppression, and rumination. 6933274 Bytes. 10.4225/03/58AE659E0EEEE
- 32.Marroquín B, Tennen H, Stanton AL. Coping, emotion regulation, and Well-Being: Intrapersonal and interpersonal processes. In: Robinson MD, Eid M, editors. The happy mind: cognitive contributions to well-being. Cham: Springer International Publishing; 2017. pp. 253–74. [Google Scholar]
- 33.Gu H, Xia T, Wang L. Childhood maltreatment and non-suicidal self-injury in prisoners: the mediating role of psychopathy and moderating role of cognitive reappraisal. Curr Psychol. 2023;42:8963–72. 10.1007/s12144-021-02213-5. [Google Scholar]
- 34.Compas BE, Connor-Smith JK, Saltzman H, et al. Coping with stress during childhood and adolescence: problems, progress, and potential in theory and research. Psychol Bull. 2001;127:87. [PubMed] [Google Scholar]
- 35.Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer publishing company; 1984. [Google Scholar]
- 36.Wan Y, Chen R, Wang S, et al. Associations of coping styles with nonsuicidal self-injury in adolescents: do they vary with gender and adverse childhood experiences? Child Abuse Negl. 2020;104:104470. 10.1016/j.chiabu.2020.104470. [DOI] [PubMed] [Google Scholar]
- 37.Castro K, Kirchner T. Coping and Psychopathological Profile in Nonsuicidal Self-injurious Chilean adolescents. J Clin Psychol. 2018;74:147–60. 10.1002/jclp.22493. [DOI] [PubMed] [Google Scholar]
- 38.Cao H, Zhang R, Li L, Yang L. Coping style and Resilience mediate the Effect of Childhood Maltreatment on Mental Health Symptomology. Children. 2022;9:1118. 10.3390/children9081118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nock MK. Why do people Hurt themselves? New insights into the Nature and functions of Self-Injury. Curr Dir Psychol Sci. 2009;18:78–83. 10.1111/j.1467-8721.2009.01613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McIntosh CN. Rethinking fit assessment in structural equation modelling: a commentary and elaboration on Barrett (2007). Personal Individ Differ. 2007;42:859–67. [Google Scholar]
- 41.Hofmann SG, Curtiss J. A complex network approach to clinical science. Eur J Clin Invest. 2018;48:e12986. 10.1111/eci.12986. [DOI] [PubMed] [Google Scholar]
- 42.Borsboom D, Cramer AOJ. Network Analysis: an Integrative Approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9:91–121. 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- 43.McGuire A. Diagnosing the diagnostic and statistical manual of mental disorders. Taylor & Francis; 2015. [Google Scholar]
- 44.Hu Z, Yu H, Zou J, et al. Relationship among self-injury, experiential avoidance, cognitive fusion, anxiety, and depression in Chinese adolescent patients with nonsuicidal self‐injury. Brain Behav. 2021;11. 10.1002/brb3.2419. [DOI] [PMC free article] [PubMed]
- 45.Buelens T, Luyckx K, Kiekens G, et al. Investigating the DSM-5 criteria for non-suicidal self-injury disorder in a community sample of adolescents. J Affect Disord. 2020;260:314–22. 10.1016/j.jad.2019.09.009. [DOI] [PubMed] [Google Scholar]
- 46.Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27:169–90. 10.1016/S0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 47.Sun T, Zhang L, Liu Y, et al. The relationship between childhood trauma and insomnia among college students with major depressive disorder: mediation by the role of negative life events and dysfunctional attitudes. Compr Psychiatry. 2023;122:152368. 10.1016/j.comppsych.2023.152368. [DOI] [PubMed] [Google Scholar]
- 48.Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85:348–62. 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- 49.Jiang Q, Zhu Y. Further explorations for a coping style questionnaire. Chin J Behav Med Sci. 1999;8:167–9. [Google Scholar]
- 50.Browne MW, Cudeck R. Alternative ways of assessing Model Fit. Sociol Methods Res. 1992;21:230–58. 10.1177/0049124192021002005. [Google Scholar]
- 51.Epskamp S, Cramer AO, Waldorp LJ, et al. Qgraph: Network visualizations of relationships in psychometric data. J Stat Softw. 2012;48:1–18. [Google Scholar]
- 52.Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. 2018;50:195–212. 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Friedman J, Hastie T, Tibshirani R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics. 2008;9:432–41. 10.1093/biostatistics/kxm045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hevey D. Network analysis: a brief overview and tutorial. Health Psychol Behav Med. 2018;6:301–28. 10.1080/21642850.2018.1521283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: generalizing degree and shortest paths. Soc Netw. 2010;32:245–51. 10.1016/j.socnet.2010.03.006. [Google Scholar]
- 56.Robinaugh DJ, Millner AJ, McNally RJ. Identifying highly influential nodes in the complicated grief network. J Abnorm Psychol. 2016;125:747–57. 10.1037/abn0000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jones PJ, Ma R, McNally RJ. Bridge centrality: A Network Approach to understanding Comorbidity. Multivar Behav Res. 2021;56:353–67. 10.1080/00273171.2019.1614898. [DOI] [PubMed] [Google Scholar]
- 58.Haslbeck JMB, Waldorp LJ. How well do network models predict observations? On the importance of predictability in network models. Behav Res Methods. 2018;50:853–61. 10.3758/s13428-017-0910-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mao L, Wu Y, Hong X, et al. The influence of childhood maltreatment on trait depression in patients with major depressive disorder: a moderated mediation model of rumination and mindful attention awareness. J Affect Disord. 2023;331:130–8. 10.1016/j.jad.2023.03.052. [DOI] [PubMed] [Google Scholar]
- 60.World Mental Health Day. 2022 - Make mental health & well-being for all a global priority. https://www.who.int/news-room/events/detail/2022/10/10/default-calendar/world-mental-health-day-2022---make-mental-health-and-well-being-for-all-a-global-priority. Accessed 6 Nov 2023.
- 61.Chen Z, Hu Z, Zheng Q. Research on the Mental health problems of left-behind children in Rural China. China: Chongqing; 2022. [Google Scholar]
- 62.Zhang B, Zhang W, Sun L, et al. Relationship between alexithymia, loneliness, resilience and non-suicidal self-injury in adolescents with depression: a multi-center study. BMC Psychiatry. 2023;23:445. 10.1186/s12888-023-04938-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yu G, Li S, Zhao F. Childhood maltreatment and prosocial behavior among Chinese adolescents: roles of empathy and gratitude. Child Abuse Negl. 2020;101:104319. 10.1016/j.chiabu.2019.104319. [DOI] [PubMed] [Google Scholar]
- 64.Hu C, Huang J, Shang Y, et al. Child maltreatment exposure and adolescent nonsuicidal self-injury: the mediating roles of difficulty in emotion regulation and depressive symptoms. Child Adolesc Psychiatry Ment Health. 2023;17:16. 10.1186/s13034-023-00557-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Brown RC, Heines S, Witt A, et al. The impact of child maltreatment on non-suicidal self-injury: data from a representative sample of the general population. BMC Psychiatry. 2018;18:181. 10.1186/s12888-018-1754-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gu H, Ma P, Xia T. Childhood emotional abuse and adolescent nonsuicidal self-injury: the mediating role of identity confusion and moderating role of rumination. Child Abuse Negl. 2020;106:104474. 10.1016/j.chiabu.2020.104474. [DOI] [PubMed] [Google Scholar]
- 67.Misiak B, Szewczuk-Bogusławska M, Samochowiec J, et al. Unraveling the complexity of associations between a history of childhood trauma, psychotic-like experiences, depression and non-suicidal self-injury: a network analysis. J Affect Disord. 2023;337:11–7. 10.1016/j.jad.2023.05.044. [DOI] [PubMed] [Google Scholar]
- 68.Chen X, Zhou Y, Li L, et al. Influential factors of non-suicidal Self-Injury in an Eastern Cultural Context: a qualitative study from the Perspective of School Mental Health Professionals. Front Psychiatry. 2021;12:681985. 10.3389/fpsyt.2021.681985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu H, Wang W, Yang J, et al. The effects of alexithymia, experiential avoidance, and childhood sexual abuse on non-suicidal self-injury and suicidal ideation among Chinese college students with a history of childhood sexual abuse. J Affect Disord. 2021;282:272–9. 10.1016/j.jad.2020.12.181. [DOI] [PubMed] [Google Scholar]
- 70.Kuzminskaite E, Penninx BWJH, Van Harmelen A-L, et al. Childhood trauma in adult depressive and anxiety disorders: an Integrated Review on Psychological and Biological mechanisms in the NESDA Cohort. J Affect Disord. 2021;283:179–91. 10.1016/j.jad.2021.01.054. [DOI] [PubMed] [Google Scholar]
- 71.Peverill M, Sheridan MA, Busso DS, McLaughlin KA. Atypical prefrontal–amygdala circuitry following Childhood exposure to abuse: Links with adolescent psychopathology. Child Maltreat. 2019;24:411–23. 10.1177/1077559519852676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schore AN. Effects of a secure attachment relationship on right brain development, affect regulation, and infant mental health. Infant Ment Health J. 2001;22:7–66. 10.1002/1097-0355(200101/04)22:1<7::AID-IMHJ2>3.0.CO;2-N.
- 73.Tatnell R, Hasking P, Newman L, et al. Attachment, emotion regulation, childhood abuse and assault: examining predictors of NSSI among adolescents. Arch Suicide Res. 2017;21:610–20. 10.1080/13811118.2016.1246267. [DOI] [PubMed] [Google Scholar]
- 74.Leitenberg H, Gibson LE, Novy PL. Individual differences among undergraduate women in methods of coping with stressful events: the impact of cumulative childhood stressors and abuse. Child Abuse Negl. 2004;28:181–92. 10.1016/j.chiabu.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 75.Xie X, Li Y, Liu J, et al. The relationship between childhood maltreatment and non-suicidal self-injury in adolescents with depressive disorders. Psychiatry Res. 2024;331:115638. 10.1016/j.psychres.2023.115638. [DOI] [PubMed] [Google Scholar]
- 76.Gariépy G, Honkaniemi H, Quesnel-Vallée A. Social support and protection from depression: systematic review of current findings in western countries. Br J Psychiatry. 2016;209:284–93. 10.1192/bjp.bp.115.169094. [DOI] [PubMed] [Google Scholar]
- 77.Forrester RL, Slater H, Jomar K, et al. Self-esteem and non-suicidal self-injury in adulthood: a systematic review. J Affect Disord. 2017;221:172–83. 10.1016/j.jad.2017.06.027. [DOI] [PubMed] [Google Scholar]
- 78.Gong T, Ren Y, Wu J, et al. The associations among self-criticism, hopelessness, rumination, and NSSI in adolescents: a moderated mediation model. J Adolesc. 2019;72:1–9. 10.1016/j.adolescence.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 79.De Vibe M, Solhaug I, Rosenvinge JH, et al. Six-year positive effects of a mindfulness-based intervention on mindfulness, coping and well-being in medical and psychology students; results from a randomized controlled trial. PLoS ONE. 2018;13:e0196053. 10.1371/journal.pone.0196053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Finkelstein-Fox L, Park CL, Riley KE. Mindfulness’ effects on stress, coping, and mood: a daily diary goodness-of-fit study. Emotion. 2019;19:1002–13. 10.1037/emo0000495. [DOI] [PubMed] [Google Scholar]
- 81.Capitão LP, Chapman R, Filippini N, et al. Acute neural effects of fluoxetine on emotional regulation in depressed adolescents. Psychol Med. 2023;53:4799–810. 10.1017/S0033291722001805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Greimel E, Feldmann L, Piechaczek C, et al. Study protocol for a randomised-controlled study on emotion regulation training for adolescents with major depression: the KONNI study. BMJ Open. 2020;10:e036093. 10.1136/bmjopen-2019-036093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Weintraub MJ, Denenny D, Ichinose MC, et al. A randomized trial of telehealth mindfulness-based cognitive therapy and cognitive behavioral therapy groups for adolescents with mood or attenuated psychosis symptoms. J Consult Clin Psychol. 2023;91:234–41. 10.1037/ccp0000782. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated andanalyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.