Abstract
Background
Autism Spectrum Disorder (ASD) is a lifelong neurodevelopmental condition affecting communication, social interaction, and behavior. Evidence suggests that environmental pollutants are associated with ASD incidence. This review aimed to analyze the effect of environmental pollutants on ASD.
Methods
Systematic review and meta-analysis of cohort studies evaluated the association between exposure to environmental pollutants and ASD. We searched COCHRANE CENTRAL, MEDLINE, CINAHL, LILACS, EMBASE, PsycINFO, Web of Science, SciELO, and gray literature from inception to January 2023. The model used for meta-analysis was inverse variance heterogeneity (IVhet). The effect measures were the beta coefficient (β) and the relative risk (RR) with their 95% confidence intervals (95% CI). Sensitivity analyses were carried out using an instrument to screen or diagnose autism.
Results
A total of 5,780 studies were identified; 27 were included in the systematic review, and 22 were included in the meta-analysis. These studies included 1,289,183 participants and 129 environmental pollutants. Individual meta-analyses found a significant association between nitrogen dioxide RR = 1.20 (95% CI: 1.03 to 1.38; I2: 91%), copper RR = 1.08 (95% CI: 1.03 to 1.13; I2: 0%), mono-3-carboxy propyl phthalate β = 0.45 (95% CI: 0.20 to 0.70; I2: 0%), monobutyl phthalate β = 0.43 (95% CI: 0.13 to 0.73; I2: 0%) and polychlorinated biphenyl (PCB) 138 RR = 1.84 (95% CI: 1.14 to 2.96; I2:0%) with ASD. Subgroup meta-analyses found a significant association with carbon monoxide RR = 1.57 (95% CI: 1.25 to 1.97; I2: 0%), nitrogen oxides RR = 1.09 (95% CI: 1.04 to 1.15; I2: 34%) and metals RR = 1.13 (95% CI: 1.01 to 1.27; I2:24%).
Conclusion
This study found positive associations nitrogen dioxide, copper, mono-3-carboxypropyl phthalate, monobutyl phthalate, and PCB 138, and the development of ASD, likewise, with subgroups of pollutants carbon monoxide, nitrogen oxides, and metals. Therefore, it is important to identify these risk factors in children and adolescents to contribute to ASD and identify prevention strategies effectively.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-19742-w.
Keywords: Autism, Environmental pollutants, Systematic review, Cohort studies
Background
Autism spectrum disorder (ASD) is a lifelong neurodevelopmental condition that impacts communication, social interaction, and behavior. Its prevalence has been on the rise globally. In a recent systematic review, it was estimated that 1 in 100 children worldwide are affected by ASD [1]. The Centers for Disease Control and Prevention (CDC), 1 in 36 children aged eight years will be diagnosed with ASD [2]. In the United States, the economic burden of ASD was estimated to be $11.5 billion in 2011 [3]. A complex interplay of biological and environmental factors has been linked to autism spectrum disorder.
Gene-environment interactions are critical factors in ASD development. Environmental pollutants, including toxic metals, are linked to epigenetic modifications and de novo mutations, potentially contributing to ASD onset [4]. These pollutants, particularly during gestation and postnatal periods, pose health risks and are associated with ASD [5]. Toxic heavy metals can disrupt enzymatic functions, interfere with cell signaling, and trigger oxidative stress, potentially leading to cell death pathways. Elevated levels of cadmium and mercury are frequently found in children with ASD [6]. However, more research is needed to fully understand how metal-induced neurotoxicity might play a role in ASD.
Recent systematic reviews and meta-analyses have evaluated the link between environmental pollutants and the development of ASD, but these reviews exhibit notable limitations. Among the 21 identified studies, 18 relied on four or fewer databases [5, 7–23], 11 imposed language restrictions (English, French, or Chinese)) [7, 8, 12, 13, 15, 18–20, 22–24], and six confined their searches to brief periods [9, 13, 15, 19, 20, 22]. This approach potentially overlooks some available evidence. Additionally, most reviews concentrated on air pollutants [7, 8, 10, 12, 13, 15, 18, 20, 23–26], with fewer addressing metals [5, 8, 14, 15, 22, 27], pesticides [9, 11, 16, 17, 27], polychlorinated biphenyls [19], or perfluoroalkyl substances [21]. The evidence primarily stems from cross-sectional, case–control, ecological, and cohort studies, and some reviews failed to stratify results by study type, blending cohort and case–control data [5, 8, 10, 12, 14]. Only one review exclusively considered cohort studies [13], However, it was limited to children under five and focused solely on-air pollution, not accounting for prolonged exposures or older children. This study aims to analyze the association between various environmental pollutants and ASD incidence through cohort studies, evaluating different pollutants and their effects on subgroups.
Methods
Protocol and registration
This study was performed according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses – PRISMA [28] and registered in the International Prospective Register of Systematic Reviews (PROSPERO) under the number CRD42018093510.
Eligibility criteria
The PECOS strategy was defined as follows: Population: children and adolescents from 0 to 18 years old; Exposure: higher levels of environmental pollutants during the prenatal and postnatal period; Comparison: lower levels of environmental pollutants; Outcome: incidence of ASD, Studies: cohort studies.
The exclusion criteria were as follows: (a) studies that only included participants older than 19 years; (b) tobacco exposure; and (c) response letters, reviews, editorials, animal, and duplicate studies. Duplicate studies were considered when they had the same author, title and year. Additionally, when the studies were updating previous versions, the most current version with the largest sample size was chosen.
Environmental pollutant exposure included air pollution; PM; inorganic carbon compounds; lead; sulfur oxides; nitrogen oxides; soot; polychlorinated biphenyls (PCBs), inorganic chemicals; pesticides; volatile organic compounds (VOC); hydrocarbons; endocrine disruptors; plasticizers, and plastics.
The air pollutants were classified according to American international guidelines [29]. The groups were ground-level ozone, PM, carbon monoxide (CO), sulfur oxides (SOx), and nitrogen oxides (NOx). The toxic substances included in this study were classified according to the International Guidelines on Toxic Substances [30]. The categories of these pollutants were coal ash; dioxins, furans, PCBs; benzidines/aromatic amines; inorganic substances; nitrosamines/ethers/alcohols; pesticides; phenols/phenoxy acids; organophosphates and carbamates; phthalates; halogenated pesticides and related compounds; volatile organic compounds; radionuclides (radioactive materials) and warfare and terrorism agents.
Sources of information and search strategy
We searched the Cochrane Central Register of Controlled Trials (COCHRANE CENTRAL), MEDLINE (via PUBMED), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Scientific Electronic Library Online (SciELO), Latin American Caribbean Health Sciences Literature (LILACS), Excerpta Medica Database (EMBASE), American Psychological Association database (PsycINFO), Web of Science (WoS), and gray literature from inception to January 2023. We checked the references of the included studies and reviews (Additional file 1: Supplementary Chart 1. Databases search strategy). Searches were not limited by date or language.
Study selection
Three independent review authors independently (GZ and SK; MDBD and SE; FKN and EM) inspected all titles and abstracts identified. The second review stage consisted of reading the articles selected in the previous step in full text.
When a difference in opinion was found at each stage, the article selection was decided independently by the other two review authors (MDBD and EM).
Data extraction
Two authors (TDC and MDBD) extracted the following study characteristics: a) first author's name, b) publication year, c) population, d) the number of subjects in the studye) study location, f) pollution measurement method, g) types of contaminants, h) ASD diagnostic assessment, i) control group, j) participant age, k) follow-up time and l) results.
Summary measures and data analysis
Table 1 qualitatively summarizes the main characteristics of the included studies. Effect sizes using the beta coefficient (β) or relative risk (RR). The relative risk consolidates various metrics from individual studies, including the incidence rate ratio, odds ratio, hazard ratio, adjusted hazard ratio, cumulative hazard ratio, and Bayesian predictive odds ratio, each accompanied by its corresponding 95% confidence intervals (95% CI). If both the beta coefficient and relative risk were accessible for a specific outcome, both measures were described for comprehensive reporting. The meta-analyses were calculated with MetaXL 5.3 [31] software. The "ContCI" type for studies that report a β value and the "RRCI" type for studies that report an RR value were used for the meta-analysis. The method selected was inverse variance heterogeneity (IVhet) [32]. The meta-analyses were conducted exclusively with studies of high methodological quality (Additional file 1: Table S1). Furthermore, a sensitivity analysis was performed, considering the type of instrument used for ASD detection (either diagnosis or screening).
Table 1.
Characteristics of included studies
| Study, Year | Country | Population | Total cohort | Number of eligible participants | Age of ASD diagnosis (Years), mean ± SD | Follow-up period | Time of exposure | Pollution Detection Method | Subgroup of pollutant | Diagnostic or screening method | Inclusion criteria | Exclusion criteria | Exposure group | Control Group |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alampi JD, 2021 [33] | Canada | Children | 8.716 | 478 | 3–4 (median, 40 months old) | 4 years | The first trimester of pregnancy | Cord blood |
Inorganic substances Metals Pesticides Phthalates Hydrocarbons Plastics Dioxins, Furans, PCBs Phenols/phenoxy acids |
Social Responsiveness Scale- 2 (SRS-2) questionnaire. Preschool-aged version | Pregnant being at least 18 years old, being able to communicate in French or English, and consenting to cord blood collection | Women who carried a fetus with a known abnormality had a primary chronic disease, used illicit drugs, or threatened abortion | Not described | Not described |
| Barkoski JM, 2021 [34] | USA | Children | Not described | 201 | Not described | 3 years | Second and third trimester of pregnancy | Urine | Pesticides |
Autism Diagnostic Observation Scale (ADOS) |
Mother or father had one or more children with ASD and or the gestating younger child had an older half-sibling or an equivalent or closer blood relative with ASD; Mother was at least 18 years of age or older; Mother was already pregnant or planning a pregnancy and biologically able to become pregnant; and Mother lived within 2 h of the Davis/Sacramento region at time of enrollment | Not described |
> LOD (> 0,1 ng/mL) Unit: natural log-transformed |
< LOD (< 0,1 ng/mL) Unit: natural log-transformed |
| Bernardo BA, 2019 [35] | Canada | Children | Not described | 546 | 3.4 ± 0.16 | 4 years | The first trimester of pregnancy | Plasma | Dioxins, Furans, PCBs | Social Responsiveness Scale-2 (SRS-2) | Mothers who had sociodemographic and child neurodevelopment information, plasma PCB concentrations, and total lipid concentrations measured during the first trimester of the pregnancy | Breastfeeding and pregnancy outcomes from our models and biomarkers of other prenatal contaminant exposures, including lead |
Fourth quartile exposure (> 3.6 ng/g) Unit: log 2 transformed |
First quartile exposure (< 1.4 ng/g) Unit: log 2 transformed |
| Braun JM, 2014 [36] | USA | Children | 389 | 175 | 4–5 (mean ± SD Not described) | 5 years | Second trimester of pregnancy and after childbirth | Serum or urine |
Phthalates Dioxins, Furans, PCBs Polyfluoroalkyl substances Pesticides Hydrocarbons |
Social Responsiveness Scale (SRS) |
a) 16 ± 3 weeks of pregnancy, b) age ≥ 18 years, c) residence in a home built before 1978, d) no history of HIV infection, and e) no medications taken for seizures or thyroid disorders |
Not described |
Pollutant unit Unit: log10-transformed |
Pollutant unit Unit: log10-transformed |
| Carter SA, 2022 [37] | USA | Children | Not described | 314.391 | Not described | 1 year | Throughout pregnancy | Freeway traffic load with California line-source dispersion model (CALINE4) | Particular matter | International Classification of Diseases (ICD)-9 codes and, after October 1, 2015, from ICD-10 codes |
Mother–child pairs of singleton deliveries at Kaiser Permanente Southern California (KPSC) hospitals between January 1, 2001, and December 31, 2014. Only geocodes with accuracy scores ≥ 98 and point or street address types were considered sufficiently accurate for traffic exposure assignments |
Missing or errors in birth weight, gender, maternal race/ethnicity and age at delivery, maternal age at delivery < 15 or > 55 years, and incomplete maternal residential address history in pregnancy, or due to geocodes not suitable for exposure assignment |
Five quintile exposure (> 3.80 ppb) |
First quintile exposure (≤ 0.89 ppb) |
| Gong T, 2014 [38] | Sweden | Children | 17.22 | 3.426 | 10.3 ± 1.5 | 9 years | Throughout pregnancy and the postnatal period | Air pollution concentrations at residential addresses during the mother's pregnancy, the child's first year of life, and the a year before the neurodevelopmental assessment was established mated by dispersion models, |
Nitrogen oxides Particular matter |
Autism-Tics, ADHD, and other Comorbidities inventory (A-TAC) | Twins born during 1992–2000 | Not described | High exposure (95th percentile) | Low exposure (5th percentile) |
| Granillo L, 2019 [39] | USA | Children | Not described | 104 | Not described | 3 years | Throughout pregnancy | Plasma | Dioxins, Furans, PCBs |
Autism Diagnostic Observation Schedule (ADOS) and Mullen Scales of Early Learning (MSEL) |
Families must reside within 2.5 h driving distance from the MIND Institute. Confirmed diagnosis of ASD in an older sibling of the child and active status in the MARBLES cohort, meaning participants had no loss to follow-up. They had not declined further participation in the study | The child of interest was a twin or had no final diagnosis | 50% highest concentration of PCB | 50% lowest concentration of PCB |
| Guxens M, 2016 [40] | Italy; the Netherlands; Sweden; Spain | Children | Not described | 8.079 | 4–10 (mean ± SD Not described) | 10 years | Throughout pregnancy | Were estimated for birth addresses by land-use regression models based on monitoring campaigns performed between 2008 and 2011 |
Nitrogen oxides Particular matter |
Swedish cohort: Autism-Tics, Attention deficit and hyperactivity disorders, and other Comorbidities (A-TAC) inventory; Dutch and Italian cohorts: Pervasive Developmental Problems (PDP) subscale of the Child Behavior Checklist for Toddlers (CBCL11⁄2–5); Dutch cohorts: Adapted 18-item version of the Social Responsiveness Scale (SRS); Spanish cohort: Childhood Autism Spectrum Test (CAST); | Mother–child pairs were recruited from 1992 through 2008 | Not described | > cutoff limit | < cutoff limit |
| Haggerty DK, 2021 [41] | USA | Children | Not described | 77 | 3–6 (mean ± SD Not described) | 6 years | The first trimester of pregnancy | Urine | Phthalates | Social Responsiveness Scale (SRS) | Women had to be 18 years of age or older and be able to communicate in English | Not described |
Pollutant unit (ng/mL) Unit: ln-transformed |
Pollutant unit (ng/mL) Unit: ln-transformed |
| Hansen J, 2021 [42] | Denmark | Children | 2.874 | 427 | 2 – 5 (mean ± SD Not described) | 5 years | End of the second trimester or beginning of the third trimester of pregnancy | Urine | Plastics | Child Behavior Checklist; 11⁄2–5 (CBCL/11⁄2–5) | 2010 to 2012, women residing in the municipality of Odense with a newly diagnosed pregnancy before 16 weeks of gestation | Twins and mothers of nonwestern origin |
Third tertile exposure (≥ 1.97 ng/mL) |
First tertile exposure (< 0.87 ng/mL) |
| Jo H, 2019 [43] | USA | Children | 246.42 | 2.471 | 0—5 (mean ± SD Not described) | 5 years | Preconception, each trimester, the entire pregnancy, and the first year of life |
Birth certificate residential addresses were geocoded using MapMarker USA Version 28.0.0.11. Exposure metrics at each geocoded address included regional O3, PM2.5, PM ≤ 10 μm in diameter (PM10), and nitrogen dioxide (NO2) |
Ozone Particular matter Nitrogen oxides |
Autism in Toddlers (CHAT) |
Mother–child pairs with singleton deliveries in KPSC hospitals between January 1, 1999, and December 31, 2009, in 14 service areas located across Southern California |
Children with birth certificate addresses outside Southern California or addresses that could not be accurately geocoded because of an address missing or not matchable to a U.S. postal service address |
> to the scaled average (PM 2.5 > 6.5 µg/m3; PM 10 > 16.1 µg/m3; NO2 > 10.4 ppb and O3 > 15.7 ppb) |
< to scaled average (PM 2.5 < 6.5 µg/m3; PM 10 < 16.1 µg/m3; NO2 < 10.4 ppb and O3 < 15.7 ppb) |
| Joyce EE, 2022 [44] | USA | Children | 256 | 154 | Not described | 3 years | First and second trimester of pregnancy | Dietary information was collected through a modified version of the National Cancer Institute's Dietary History Questionnaire (DHQ), which included additional questions from the validated version to capture contaminant exposure | Pesticides | Social Responsiveness Scale (SRS) | Women had to be 18 years or older, less than 29 weeks pregnant, English or Spanish-speaking, and living no farther than 2 h from recruitment sites | Not have outcome information available (either Social Responsiveness Scale (SRS) or diagnostic evaluation, both conducted at the 36-month visit and if they did not have information on prenatal diet. Twins were excluded due to the small number and correlation in exposures, following these exclusions | Fourth quartile exposure | First quartile exposure |
| Jung CR, 2013 [45] | China | Children | 49.833 | 535 | 6.26 ± 2.91 | 4 years | Early childhood ( up to 6 years) | Taiwan Environmental Protection Agency (EPA) monitoring station on Taiwan's main island. These air pollutants are measured hourly—CO by nondispersive infrared absorption, NO2 by chemiluminescence, O3 by ultraviolet absorption, SO2 by ultraviolet fluorescence, and PM10 by beta-gauge—and continuously |
Carbon monoxide Nitrogen oxides Sulfur oxides Ozone Particular matter |
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) |
Individual's first date of enrollment until the first diagnosis of ASD | Children who had experienced ASD at the baseline and those who had missing information on air pollution | > 75th percentile | < 25th percentile |
| Kim JI, 2021 [46]* | South Korea | Children | 13.484 | 547 | 95.1 ± 1.4 months | 8 years | The second trimester of pregnancy and the postnatal period | Urine | Phthalates | Social Communication Questionnaire (SCQ) | Pregnant women in the second trimester (between 14 and 27 weeks of gestation) were enrolled in the Congenital Anomaly Study from 2008 to 2010 | Children who did not visit at least once between the ages of 4 and 8 years and children who did not see due to missing information on the social communication questionnaire (SCQ) scores | > LOD | < LOD |
| Lizé M, 2022 [47]* | France | Children | 3.421 | 185 | 4–11 (mean ± SD Not described) | 11 years | First and second trimester of pregnancy | Urine samples |
Organophosphates and carbamates Pesticides |
The Childhood Autism Spectrum Test (CAST) | Women with less than 19 weeks of gestation | Not described | Third tertile, > LOD or detectable exposure | First tertile, < LOD or not detectable exposure |
| Nowack N, 2015 [48] | Germany | Children | 234 | 116 | 10.23 ± 0.59 | 12 years | The third trimester of pregnancy and the postnatal period | Blood samples | Dioxins, Furans, PCBs | Social Responsiveness Scale (SRS) |
Babies from German- or Turkish-speaking families are born at term (weeks 38–42 of pregnancy) with an APGAR score of at least 8 Parity 1–3 |
Serious complications or illness during pregnancy or at parturition, and without congenital anomalies | Pollutant unit (pg/g lipid base) | Pollutant unit (pg/g lipid base) |
| Oudin A, 2019 [49] | Sweden | Adolescents | 48.571 | 768 | 8 ± 1.9 | 17 years | Throughout pregnancy | Geocoding | Nitrogen oxides | International Statistical Classification of Diseases and Related Health Problems (ICD-10) | Being born between 1999 and 2009 | Not described | Fourth quartile exposure | First quartile exposure |
| Oulhote Y, 2020 [50] | Canada | Children | 2.001 | 556 | 3.4 ± 0.74 | 4 years | The first trimester of pregnancy | Urine samples | Phthalates | Social Responsiveness Scale (SRS-2) | Pregnant woman older than 18 years |
Have a chronic disease Threatened abortion Consumption of psychoactive substances |
Pollutant unit (µg/L) Unit: Log 2-transformed |
Pollutant unit (µg/L) Unit: Log 2-transformed |
| Pagalan L, 2019 [51] | Canada | Children | 132.256 | 129.439 | 4.2 ± 1.4 | 5 years | Throughout pregnancy and the postnatal period | Land use regression model |
Particular matter Nitrogen oxides |
Autism Diagnostic Observation Schedule (ADOS) Autism Diagnostic Interview–Revised (ADI-R) |
Be registered in the provincial health insurance plan for 275 days or more Reside in the Vancouver metropolitan area during the calendar year of your pregnancy |
Unknown gestational age |
Per interquartile range (PM 2.5 > 1.5 µg/m3; NOX > 10.5 ppb and NO2 > 4.8 ppb) |
Per interquartile range (PM 2.5 < 1.5 µg/m3; NOX < 10.5 ppb and NO2 < 4.8 ppb) |
| Pham C, 2022 [52] | Australia | Children | 1.047 | 676 | 2–4 (mean ± SD Not described) | 4 years | Throughout pregnancy and the postnatal period | Geocoding |
Particular matter Nitrogen oxides |
Child Behavior Checklist for ages 1½–5 (CBCL 1½–5) | Not described |
Pregnant women under 18 years of age Require an interpreter to answer the questionnaires Baby with severe disease before 32 weeks |
Pollutant unit PM 2.5 (µg/m3) NO2 (ppb) |
Pollutant unit PM 2.5 (µg/m3) NO2 (ppb) |
| Philippat C, 2018 [53] | United States | Children | 203 | 101 | Not described | 3 years | Throughout pregnancy | Urine samples | Phthalates | Autism Diagnostic Observation Schedule (ADOS) |
Be at least 18 years of age Be the biological mother of a child with autism spectrum disorder Live within a 2-h drive of Davis/Sacramento |
Not taking the follow-up questionnaire | Not described | Not described |
| Rahman MM, 2022 [54] | United States | Children | 343.813 | 294.937 | 3.5(IQR 2.6 ± 5.3) | 9 years | Throughout pregnancy |
Air Quality System (AQS) Moderate Resolution Imaging Spectroradiometer |
Particular matter Nitrogen oxides Ozone |
International Statistical Classification of Diseases and Related Health Problems (ICD-10) | Mothers with singleton deliveries at Kaiser Permanente Southern California |
Maternal age at delivery < 15 or > 55 years of age Maternal residential address history in pregnancy |
Per interquartile range (PM2.5 > 7.4 μg/m3 NO2 > 17.4 ppb O3 > 19.3 ppb) |
Per interquartile range (PM2.5 < 7.4 μg/m3 NO2 < 17.4 ppb O3 < 19.3 ppb) |
| Rahman MM, 2023 [55] | United States | Children | 370.723 | 318.750 | 3.0 (IQR 2.3 ± 3.7) | 5 years | Throughout pregnancy | Geocoding |
Elemental carbon Organic carbon Metals Inorganic substances |
International Statistical Classification of Diseases and Related Health Problems (ICD-9) | Mothers with singleton deliveries at Kaiser Permanente Southern California |
Maternal age at delivery < 15 or > 55 years of age Maternal residential address history in pregnancy |
Per interquartile range (ng/m3) EC > 329.10 OC > 1249.74 Cu > 11.06 Fe > 169.56 Mn > 2.75 |
Per interquartile range (ng/m3) EC < 329.10 OC < 1249.74 Cu < 11.06 Fe < 169.56 Mn < 2.75 |
| Sagiv SK, 2018 [56] | United States | Adolescents | 601 | 534 | 14.06 ± 0.23 | 14 years | First and third trimester of pregnancy |
Urine samples Geocoding |
Dialkyl phosphates Diethyl phosphates Dimethyl phosphates Chlorpyrifos Diazinon Malathion Oxydemeton-methyl |
Social Responsiveness Scale (SRS-2) |
≥ 18 years old < 20 weeks gestation Spanish or English-speaking Qualifying for low-income health insurance Planning to deliver at the public hospital |
Not described |
Pollutant unit (nmol/L) Unit: Log-normal distribution |
Pollutant unit (nmol/L) Unit: Log-normal distribution |
| Van den Dries MA, 2019 [57] | Netherlands | Children | 9.778 | 622 | Not described | 6 years | Throughout pregnancy and postnatal period | Urine samples | Organophosphates and carbamates | Social Responsiveness Scale (SRS) | Resided in the study area in Rotterdam, the Netherlands | Not described |
Pollutant unit (nmol/g) Unit: log10 transformed |
Pollutant unit (nmol/g) Unit: log10 transformed |
| Von Ehrenstein OS, 2014 [58] | United States | Children | 1′745.754 | 148.722 | Not described | 5 years | Throughout pregnancy | Geocoding |
Volatile organic compounds Inorganic substances Hydrocarbons |
Diagnostic and Statistical Manual of Mental Disorders (DSM IV-R) (code 299.00) | Not described | Not described | > Interquartile range and km Buffers | < Interquartile range and km Buffers |
| Wang SY, 2021 [59]* | China | Adolescents | 1′000.000 | 62.919 | 15.30 ± 2.20 | 17 years | Throughout pregnancy | Automatic monitoring stations |
Particular matter 10 Carbon monoxide Nitrogen Dioxide Sulfur dioxide Ozone |
Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) | Not described |
Those who had missing data on the insurance enrollment date Lived outside the Taiwan main island |
Higher than the average exposure level in each trimester | Less than the average exposure level in each trimester |
LOD Lower Detection Limit, PM Particular matter, NO2 Nitrogen dioxide, NOX Nitrogen oxides, O3 Ozone, EC Elemental carbon, OC Organic carbon, Cu Copper/ Fe Iron, Mn Manganese
* Only studies included in the systematic review
Cochran's Q, tau-squared (tau2) tests and I2 statistics were used to test heterogeneity. The I2 statistic interpretation was 0% to 40% might not be significant; 30% to 60% may represent moderate heterogeneity; 50% to 90% may represent substantial heterogeneity; 75% to 100% means considerable heterogeneity [60].
For studies that did not outline the mean and standard deviation, these values were computed using the Hozo et al. method specified in the research conducted by Wan X [61] and colleague.
Risk of bias in studies and certainty of evidence
Two reviewers independently judged the methodological quality of the individual studies (S.K. and E.M.) following the Quality Assessment Tool for Observational Cohort Studies from the National Institute of Health [62]. The studies were classified as good, fair, or poor (Additional file 1: Table S1). The GradePro tool was used to conduct the certainty analysis. The degree of evidence uncertainty was rated as high, moderate, low, and very low.
Results
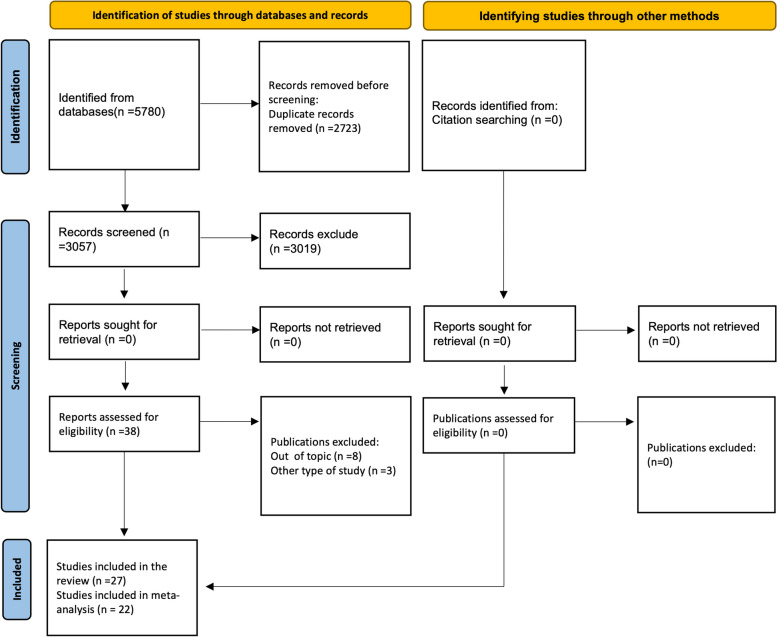
A total of 5,780 studies were identified, of which 2,723 were duplicates. The remaining 3,057 studies of these 3,019 articles were excluded: 2,501 did not evaluate the association between environmental pollutants and ASD; 513 were studies with another type of design (cross-sectional, case studies, case series, experimental models, reviews, response letters or editorials); and five included participants older than 19 years. Thirty-eight articles were selected to read the full text, of which 11 were excluded: eight did not evaluate the association between air pollutants and ASD, and three had another design. Finally, 27 articles were included in the systematic review, and 22 were included in the meta-analysis (Fig. 1).
Fig. 1.
Flowchart of the study selection process
The 27 articles included 1,289,183 individuals aged ranging from childhood to adolescence. Twenty-four studies were conducted on children [33–44, 46–48, 50–55, 57, 58] (n = 1,225,715), and three studies were conducted in adolescents [49, 56, 59] (n = 63,468). The average exposure duration was 6,9 years, with follow-up times ranging from 2 years [52] to 17 years [49, 59] across the studies (Table 1).
The studies reported one hundred twenty-nine pollutants, which are air pollutants and toxic substances. Seven studies reported nitrogen dioxide [40, 43, 45, 51, 52, 54, 59]; six studies reported PM 2.5 [37, 40, 43, 51, 52, 54]; five studies reported PM 10 [38, 40, 43, 45, 59]; four studies reported ozone [43, 45, 54, 59] and mono-n-butyl phthalate [33, 36, 41, 46, 50]. diethyl phosphite [33, 47, 53, 56], mono-ethyl phthalate [33, 36, 41, 50], PCB 118 [33, 35, 36, 39], and PCB 153 [33, 35, 36, 39]. Three studies reported bisphenol A [33, 36, 42], dialkyl phosphates [47, 56, 57], dimethyl phosphate [33, 47, 56], manganese [33, 55, 58], mono-(2-ethyl-5-hydroxyhexyl) phthalate [33, 36, 46], mono-3-carboxy propyl phthalate, mono-benzyl phthalate [33, 36, 50], nitrogen oxides [38, 40, 49], PCB 138 and PCB 180 [33, 35, 39]. 3,5,6-Trichloro-2-pyridinol [47, 53], carbon monoxide [45, 59], copper [55, 58], diazinon [47, 56], dimethylthiophosphate [33, 53], lead [33, 58], mono-(2-ethyl-5-oxohexyl) phthalate [33, 46], mono-2-ethyl-hexyl phthalate, trans-nonachlor, β-hexachlorocyclohexane [33, 36], mono-isobutyl phthalate [36, 41], oxychlordane, p,p-dichlorodiphenyldichloroethylene [33, 36], PCB 101 [36, 39], PCB 187 [35, 36] and sulfur dioxide [45, 59] were described in 2 studies each (Additional file 1: Table S2).
And finally, the following pollutants were described in a single study: 1,3-butadiene, acetaldehyde, benzene, chloroform, chromium, ethyl benzene, formaldehyde, hexavalent chromium, meta/para-xylen, methylene chloride, molybdenum, nickel, ortho-dichlorobenzene, ortho-xylene, paradichlorobenzene, perchloroethylene, polycyclic aromatic hydrocarbon, selenium, toluene, trichloroethylene, vanadium [58], 3-phenoxybenzoic acid [34], arsenic, cadmium, mercury, triclosan [33], brominated biphenyl 153, hexachlorobenzene, mono-2-ethyl-5-carboxypentyl phthalate, p,p-dichlorodiphenyltrichloroethane, perfluorohexane sulfonate, perfluorononanoate, perfluorooctane sulfate, perfluorooctanoate, polybrominated diphenyl ether (PBDE) 100, PBDE 153, PBDE 154, PBDE 183, PBDE 28, PBDE 47, PBDE 85, PBDE 99, PCB 172, PCB 105, PCB 138/158, PCB 146, PCB 156, PCB 157, PCB 167, PCB 170, PCB 177, PCB 178, PCB 183, PCB 194, PCB 195, PCB 196/203, PCB 199, PCB 206, PCB 209, PCB 28, PCB 66, PCB 74, PCB 99 [36], chlorpyrifos, malathion, oxydemeton-methyl [56], chlropyrifos-oxon, terbufos, [47], di-(2-ethylhexyl) phthalate [41], diethyl alkyl phosphates, dimethyl alkyl phosphates [57], elemental carbon, iron, organic carbon [55], nitric oxide [51], organochlorine, organophosphate [44], PM 2.5 absorbance, PM coarse [40], PCB 11, PCB 132, PCB 136, PCB 174, PCB 175, PCB 176, PCB 196, PCB 52, PCB 77, PCB 84, PCB 91, PCB 95 [39], polychlorinated biphenyls, polychlorinated dibenzo-p-dioxins and dibenzofurans [48] and three metabolites of di-(2-ethylhexyl) phthalate [50] (Additional file 1: Table S2).
Results of the association between environmental pollutants and ASD from individual studies
Individual studies reported a significant association with the following contaminants: cadmium, bisphenol A [33], PCB 138 [35], PBDE 28, PBDE 47, PBDE 99, PBDE 100, PBDE 154 [36], PM 2.5 [37, 43, 51, 52, 54], PCB 101 [39], mono-i-butyl phthalate [41], nitrogen dioxide [43, 45, 51, 59], carbon monoxide [45, 59], sulfur dioxide [45], chlropyrifos-oxon [47], nitrogen oxides [49], mono-n-butyl phthalate, mono-3-carboxypropyl phthalate [33, 50], nitric oxide [51], elemental carbon, organic carbon, iron, manganese [55], dialkylphosphates, dimethylphosphate [56], benzene, perchloroethylene, 1,3-butadiene, toluene, ortho-xylene, meta/para-xylen, ethyl benzene, lead, acetaldehyde, formaldehyde, trichloroethylene [58] and copper [55, 58] (Additional file 1: Table S3).
A significant association was also reported with PCB 74, PCB 146, PCB 153, PCB 156, PCB 157, PCB 170, PCB 172, PCB 177, PCB 178, PCB 183, PCB 187, PCB 194, PCB 195, PCB 196/203, PCB 199, PCB 209, β-hexachlorocyclohexane [36], brominated biphenyl 153, PCB 136, PCB 175, PCB 176 [39], ozone [45], polychlorinated dibenzo-p-dioxins and dibenzofurans [48], diethyl alkyl phosphates [57], vanadium [58] and PM 10 [59] (Additional file 1: Table S3). No significant associations were reported with the remaining pollutants.
Quality of studies
The evaluation of the quality of the studies is presented in Additional file 1: Table S1 and Figure S2. When carrying out this analysis, it was found that the majority of the included studies (n = 22) showed high quality [33–35, 37–40, 42, 43, 45, 46, 48–55, 57–59], a smaller proportion (n = 5) presented fair quality [36, 41, 44, 47, 56], and none presented poor quality.
Meta-analysis
The results of the individual and subgroup meta-analyses are presented below. It should be noted that, on some occasions, meta-analyses included the same study because they provide results for different environmental pollutants.
Meta-analysis of each pollutant and its association with ASD
The first meta-analysis was performed separately for each pollutant, and a significant association was found with nitrogen dioxide, copper, mono-3-carboxypropyl phthalate, monobutyl phthalate and PCB 138 (Additional file 1: Figure S2). Additionally, these meta-analyses suggest a potential association with PM 10 (Additional file 1: Figure S3). No associations were found with the other pollutants.
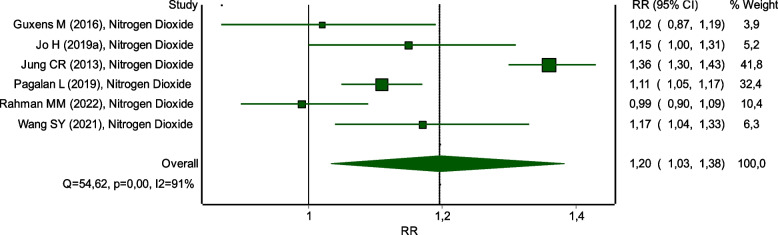
The association between nitrogen dioxide and ASD was significant RR 1.20 (95% CI: 1.03 to 1.38). However, this association showed high heterogeneity among studies (I2 = 91%) (Fig. 2). Conversely, copper exposure displayed a significant association with ASD, with an RR of 1.08 (95% CI: 1.03 to 1.13) and low heterogeneity (I2 = 0%) (Fig. 3A).
Fig. 2.
Meta-analysis association between nitrogen dioxide and ASD
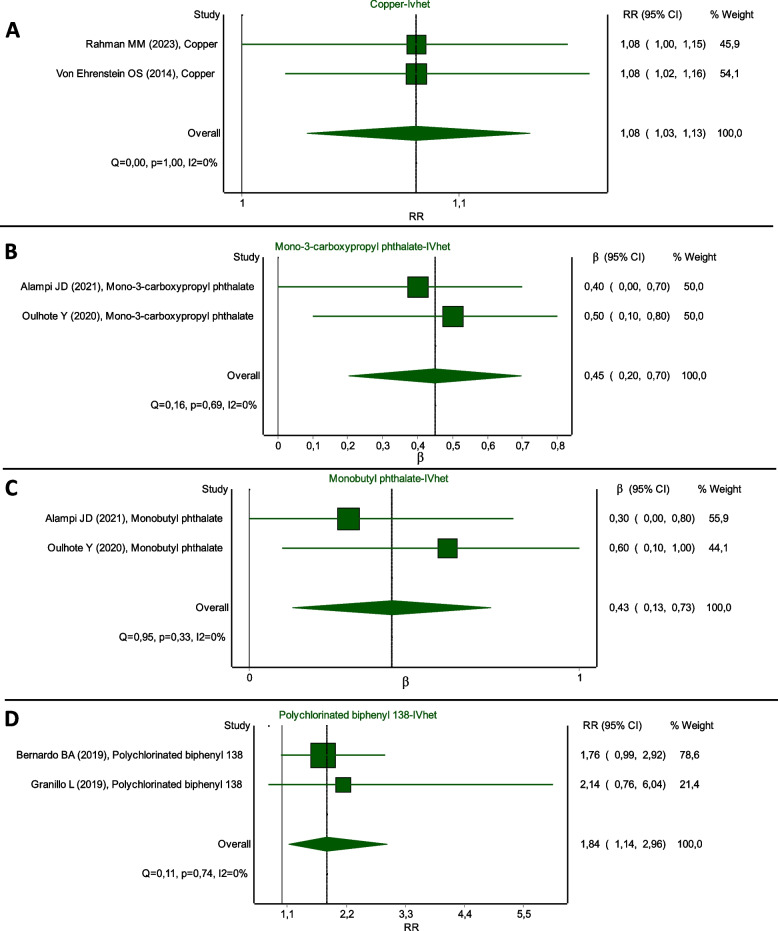
Fig. 3.
Meta-analysis association (A) copper; B mono-3-carboxypropyl phthalate; C monobutyl phthalate; D PCB 138 with ASD
Similarly, exposure to mono-3-carboxy propyl phthalate was associated with ASD (β = 0.45, 95% CI: 0.20 to 0.70), with low heterogeneity (I2 = 0%) (Fig. 3B). Monobutyl phthalate also exhibited a positive coefficient (β = 0.43, 95% CI: 0.13 to 0.73) with low heterogeneity (I2 = 0%) (Fig. 3C). Lastly, PCB 138 showed an association with ASD, reflected in an RR of 1.84 (95% CI: 1.14 to 2.96) and low heterogeneity (I2 = 0%) (Fig. 3D).
Meta-analysis by subgroups of pollutants and their association with ASD
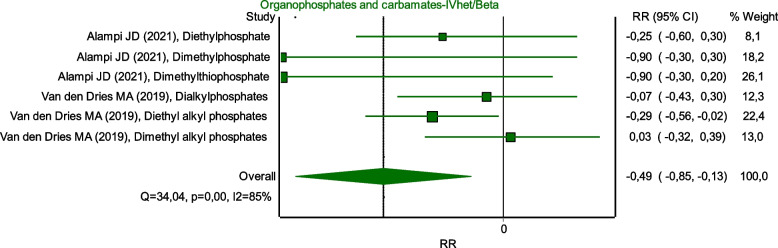
The pollutants were classified into 16 subgroups: ground-level ozone; PM; carbon monoxide; sulfur oxides; nitrogen oxides; volatile organic compounds; dioxins, furans, PCBs; hydrocarbons; inorganic substances; metals; organophosphates and carbamates; pesticides; phthalates; phenols/phenoxy acids; polyfluoroalkyl substances and plastics. Positive associations were found with carbon monoxide, nitrogen oxides, and metals (Fig. 4) (Additional file 1: Figure S2). A negative association with organophosphates and carbamates was observed (Fig. 5). Finally, potential associations with ozone (Additional file 1: Figure S4), PM (Additional file 1: Figure S5), inorganic substances (Additional file 1: Figure S6), pesticides (Additional file 1: Figure S7), dioxins, furans, and PCBs (Additional file 1: Figure S8).
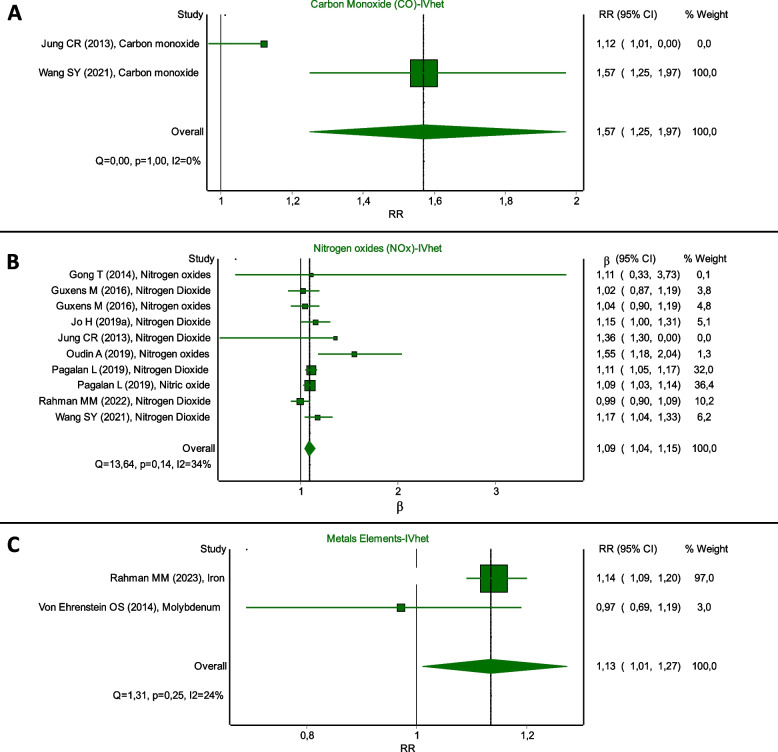
Fig. 4.
Meta-analysis association of (A) carbon monoxide, B nitrogen oxides, and (C) metals with ASD
Fig. 5.
Meta-analysis association between organophosphates and carbamates and ASD
Also, the association between carbon monoxide and ASD was found to be significant, with an RR of 1.57 (95% CI: 1.25 to 1.97) and low heterogeneity (I2 = 0%), (Fig. 4A). Nitrogen oxides, including nitrogen dioxide and nitric oxides, were also associated with ASD, with an RR of 1.09 (95% CI: 1.04 to 1.15) and moderate heterogeneity (I2 = 34%) (Fig. 4B).
Metal elements such as iron and molybdenum were linked to ASD with an RR of 1.13 (95% CI: 1.01 to 1.27) and low heterogeneity (I2 = 24%) (Fig. 4C). Conversely, exposure to organophosphates and carbamates, which include compounds such as diethyl phosphate, dimethyl phosphate, dimethyl thiophosphate, dialkyl phosphates, diethyl alkyl phosphates, and dimethyl alkyl phosphates, showed a negative association with ASD (β = -0.49, 95% CI: -0.85 to -0.13) and high heterogeneity (I2 = 85%) (Fig. 5).
Sensitivity analysis
For the sensitivity analysis, we pooled the studies by pollutant and according to the instrument applied to determine autism, either diagnosis or screening. Once the meta-analyses were carried out, the results remained constant for nitrogen dioxide with diagnostic tools (Additional file 1: Figure S9), copper (Additional file 1: Figure S10), mono-3-carboxy propyl phthalate (Additional file 1: Figure S11), and mono-n-butyl phthalate (Additional file 1: Figure S12) with screening instruments. PCB 138 could not be meta-analyzed because there were not enough studies with either of the two types of tools.
In the case of the subgroups, the association between pollutants and ASD was maintained in carbon monoxide with diagnostic instruments (Additional file 1: Figure S13), nitrogen oxides with diagnostic and monitoring tools (Additional file 1: Figure S14-15), metals with diagnostic instruments (Additional file 1: Figure S16), and organophosphates and carbamates with monitoring instruments (Additional file 1: Figure S17). Finally, when meta-analyzed only with tracking instruments, the PM found as a possible association reported a significant association (Additional file 1: Figure S18).
Certainty of evidence
The analysis of evidence certainty using the GradePro tool consistently reveals a landscape characterized by low or very low certainty across all conducted analyses. The main factors contributing to this were heterogeneity between studies and the risk of publication bias (Additional file 1: Table S4-S7).
Discussion
This systematic review and meta-analysis investigated the association between environmental pollutants and the incidence ASD in children and adolescents. The results indicated that exposure to individual pollutants such nitrogen dioxide, copper, mono-3-carboxy propyl phthalate, monobutyl phthalate, and PCB 138 increases the risk of developing ASD. Subgroup analyses further linked carbon monoxide, nitrogen oxides, and metals to higher ASD risk. Additionally, trends suggested associations between ASD and exposure to particulate matter, inorganic substances, and pesticides. The associations found in this study can be explained according to the pollutant type, individually or by subgroup.
The associations with PCB 138 [19, 63], carbon monoxide [7], nitrogen oxides [10], and metals [64, 65] and risk of ASD were consistent with findings from other systematic reviews. However, there were discrepancies between those with nitrogen dioxide [10, 15], copper [66], mono-3-carboxypropyl phthalate and monobutyl phthalate [67, 68] and other reviews.
Differences can justify the possible differences between our findings from other reviews can be justified that some studies carried out subgroup analyses by exposure time [10, 15], did not only include a cohort study [15], considering the exposure window [15], the differences between pollutant concentrations and other methodologies for estimating associations [67, 68].
It is recognized that environmental pollutants disrupt cellular metabolism through mechanisms like breaching cell membranes, intracellular accumulation, and inhibition of critical metabolic pathways [69]. For instance, heavy metals can trigger oxidative stress by generating reactive oxygen species, which can harm lipids, proteins, and DNA and compromise mitochondrial function, potentially leading to cell death, tissue damage, or neurological disorders [70]. Particulate matter and polycyclic aromatic hydrocarbons can breach the blood–brain barrier, initiating brain inflammation that may disrupt neurotransmitter systems and synaptic function [69]. Persistent immune system activation by pollutants can induce chronic neuroinflammation, disrupting brain architecture connectivity and impeding normal brain development [71].
Moreover, pollutants can cause DNA damage, leading to epigenetic alterations like DNA methylation and histone modifications that influence gene expression tied to brain development and function [72, 73]. This, in turn, could potentially contribute to the pathophysiology of ASD. Compelling evidence suggests that environmental contaminants significantly impact cellular metabolism and neurological well-being, connecting these molecular changes to broader neurodevelopmental consequences [55, 74].
Exposure routes to environmental pollutants are crucial in ASD pathogenesis. Alterations in neuronal connectivity, occurring from prenatal to early adulthood, can result from genetic and epigenetic factors [76]. The ENVIRONAGE cohort study found that increased PM 2.5 exposure during pregnancy was associated with relationship and prosocial behavior problems in preschoolers [76]. These effects may be due to higher mutation rates and DNA repair alterations during fetal and neonatal stages [72]. Conversely, low-pollution maternal environments are associated with beneficial DNA methylation in neurodevelopmental genes, highlighting the importance of pollution levels and particulate matter composition in understanding ASD risk [73].
The characteristics of the population may impact the associations identified in this meta-analysis study and the timing of exposure. ASD symptoms typically manifest early in life, exerting significant developmental effects during the prenatal and early postnatal periods [76]. Both acute and chronic exposure to environmental pollutants during these critical phases can influence neurogenesis and neuronal maturation [76]. Evidence suggests that prenatal and postnatal exposure to contaminants can bring about developmental alterations in children, with the developing nervous system being especially vulnerable to environmental toxins, even at low exposure levels [76]. Accurate assessment of the timing of contaminant exposure is crucial for comprehending the underlying mechanisms and crafting effective interventions.
Recognizing that the absence of significant associations with specific contaminants, individually or in combination, or inconclusive findings does not imply their non-existence is crucial. Further research is imperative to pinpoint the risk factors contributing to our understanding of ASD and to inform the development of enhanced preventive measures.
Strengths and limitations of the systematic review
Our systematic review stands out for several key reasons. Firstly, it adopts a broad approach, incorporating a wide array of databases and gray literature sources. Unlike other reviews, our search was not constrained by time or language, ensuring inclusivity and breadth of scope. Additionally, we excluded observational studies, which often present limitations for causal inference, thereby enhancing the robustness of our findings.
Furthermore, our review maintained a stringent focus on studies of high methodological quality, ensuring the reliability of our results. Unlike comparable reviews, our analysis encompassed a broad range of contaminants, facilitating a deeper understanding of their impact on ASD incidence. Moreover, our study evaluated the effects of both individual and grouped contaminants, offering a novel perspective on the issue.
This study also has some limitations. First, the studies included a variability of exposure time, pollutant detection method, and the instrument used to determine ASD. However, to avoid overestimating the effect, sensitivity analyses were performed that supported the validity of the association with ASD. In addition, the instruments, although diverse, are all approved by the scientific community for the screening or diagnosis of ASD. Second, some meta-analyses had high heterogeneity.
In summary, our systematic review represents an original contribution to the field, distinguished by its meticulous methodology, broad inclusion, and comprehensive analysis of the effects of pollutants on the incidence of autism.
Conclusion and future directions
This systematic review and meta-analysis suggest that children and adolescents exposed to higher contamination levels by pollutants such as nitrogen dioxide, copper, mono-3-carboxy propyl phthalate, mono butyl phthalate, and PCB 138 have a higher risk of developing ASD. Likewise, those exposed to subgroups of environmental pollutants such as carbon monoxide, nitrogen oxides, and metals were associated with ASD. Therefore, it is important to identify the factors that underlie the susceptibility of children and adolescents to contribute effectively to ASD and identify prevention strategies. Future studies should standardize the exposure time to pollutants and the detection methods, allowing for more precise comparisons and better interpretation of the results.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- ASD
Autism Spectrum Disorder
- CDC
Centers for Disease Control and Prevention
- PM
Particulate matter
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PCBs
Polychlorinated biphenyls
- VOC
Volatile organic compounds
- CO
Carbon monoxide
- SOx
Sulfur oxides
- NOx
Nitrogen oxides
- COCHRANE CENTRAL
Cochrane Central Register of Controlled Trials
- CINAHL
Cumulative Index to Nursing and Allied Health Literature
- SciELO
Scientific Electronic Library Online
- EMBASE
Excerpta Medica Database
- PsycINFO
American Psychological Association database
- WoS
Web of Science
- RR
Relative risk
- β
Beta coefficient
- 95% CI
95% confidence intervals
- IVhet
Inverse variance heterogeneity
- ES
Estimate
Authors' contributions
TDC: methodology, formal analysis, investigation, data curation, writing—original draft, writing—revision and editing. MDBD: conceptualization methodology, validation, investigation, writing—review, and editing. EM: investigation, validation and writing – review and editing. FKN: investigation and writing – review and editing. SE: investigation and writing – review and editing. SKM: investigation and writing – review and editing. GZ: investigation and writing – review and editing. AVP: writing – review and editing. JGP: writing – review and editing. ATS: writing – review and editing. WCM: methodology, formal analysis, writing – review and editing. RM: conceptualization, methodology, validation, investigation, data curation, writing—original draft, writing—revision and editing, supervision, project administration. All authors read and approved the final manuscript.
Funding
Rio Grande do Sul Research Support Foundation (FAPERGS), the National Research Council of Brazil (CNPq), the Coordination for the Improvement of Higher Education Personnel (CAPES—Financial Code 001) and Ministry of Science, Technology and Innovation of Colombia grant No. 751–2018.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zeidan J, Fombonne E, Scorah J, Ibrahim A, Durkin MS, Saxena S, et al. Global prevalence of autism: A systematic review update. Autism Res. 2022;15(5):778–90. 10.1002/aur.2696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maenner MJ, Warren Z, Williams AR, Amoakohene E, Bakian AV, Bilder DA, et al. Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2020. MMWR Surveill Summ. 2023;72(2):1–14. 10.15585/mmwr.ss7202a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lavelle TA, Weinstein MC, Newhouse JP, Munir K, Kuhlthau KA, Prosser LA. Economic burden of childhood autism spectrum disorders. Pediatrics. 2014;133(3):e520–9. [DOI] [PMC free article] [PubMed]
- 4.Chowdhury A, Naz A, Maiti SK. Bioaccumulation of potentially toxic elements in three mangrove species and human health risk due to their ethnobotanical uses. Environ Sci Pollut Res. 2021;28(25):33042–59. 10.1007/s11356-021-12566-w [DOI] [PubMed] [Google Scholar]
- 5.Saghazadeh A, Rezaei N. Systematic review and meta-analysis links autism and toxic metals and highlights the impact of country development status: Higher blood and erythrocyte levels for mercury and lead, and higher hair antimony, cadmium, lead, and mercury. Prog Neuro-Psychopharmacology Biol Psychiatry. 2017;79:340–68. 10.1016/j.pnpbp.2017.07.011 [DOI] [PubMed] [Google Scholar]
- 6.Baj J, Flieger W, Flieger M, Forma A, Sitarz E, Skórzyńska-Dziduszko K, et al. Autism spectrum disorder: Trace elements imbalances and the pathogenesis and severity of autistic symptoms. Neurosci Biobehav Rev. 2021;129:117–32. 10.1016/j.neubiorev.2021.07.029 [DOI] [PubMed] [Google Scholar]
- 7.Blanc N, Liao J, Gilliland F, Zhang J (Jim), Berhane K, Huang G, et al. A systematic review of evidence for maternal preconception exposure to outdoor air pollution on Children’s health. Environ Pollut. 2023;318:120850. [DOI] [PMC free article] [PubMed]
- 8.Dutheil F, Comptour A, Morlon R, Mermillod M, Pereira B, Baker JS, et al. Autism spectrum disorder and air pollution: A systematic review and meta-analysis. Environ Pollut. 2021;278:116856. 10.1016/j.envpol.2021.116856 [DOI] [PubMed] [Google Scholar]
- 9.Miani A, Imbriani G, De Filippis G, De Giorgi D, Peccarisi L, Colangelo M, et al. Autism Spectrum Disorder and Prenatal or Early Life Exposure to Pesticides: A Short Review. Int J Environ Res Public Health. 2021;18(20):10991. 10.3390/ijerph182010991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flores-Pajot M-C, Ofner M, Do MT, Lavigne E, Villeneuve PJ. Childhood autism spectrum disorders and exposure to nitrogen dioxide, and particulate matter air pollution: A review and meta-analysis. Environ Res. 2016;151:763–76. 10.1016/j.envres.2016.07.030 [DOI] [PubMed] [Google Scholar]
- 11.Bertoletti ACC, Peres KK, Faccioli LS, Vacci MC, Mata IR da, Kuyven CJ, et al. Early exposure to agricultural pesticides and the occurrence of autism spectrum disorder: a systematic review. Rev Paul Pediatr. 2022;41:e2021360. [DOI] [PMC free article] [PubMed]
- 12.Fu P, Guo X, Cheung FMH, Yung KKL. The association between PM2.5 exposure and neurological disorders: A systematic review and meta-analysis. Sci Total Environ. 2019;655:1240–8. [DOI] [PubMed]
- 13.Amnuaylojaroen T, Parasin N, Saokaew S. Exploring the association between early-life air pollution exposure and autism spectrum disorders in children: A systematic review and meta-analysis. Reprod Toxicol. 2024;125:108582. 10.1016/j.reprotox.2024.108582 [DOI] [PubMed] [Google Scholar]
- 14.Wang M, Hossain F, Sulaiman R, Ren X. Exposure to Inorganic Arsenic and Lead and Autism Spectrum Disorder in Children: A Systematic Review and Meta-Analysis. Chem Res Toxicol. 2019;32(10):1904–19. 10.1021/acs.chemrestox.9b00134 [DOI] [PubMed] [Google Scholar]
- 15.Chun H, Leung C, Wen SW, McDonald J, Shin HH. Maternal exposure to air pollution and risk of autism in children: A systematic review and meta-analysis. Environ Pollut. 2020;256: 113307. 10.1016/j.envpol.2019.113307 [DOI] [PubMed] [Google Scholar]
- 16.Wang L, Tang S, Wu S, Yao L, Su D, Wang Y. Maternal Exposure to Pesticides and Risk of Autism Spectrum Disorders in Offspring: A Meta-analysis. J Autism Dev Disord. 2022;52(4):1640–51. 10.1007/s10803-021-05063-z [DOI] [PubMed] [Google Scholar]
- 17.Xu Y, Yang X, Chen D, Xu Y, Lan L, Zhao S, et al. Maternal exposure to pesticides and autism or attention-deficit/hyperactivity disorders in offspring: A meta-analysis. Chemosphere. 2023;313:137459. 10.1016/j.chemosphere.2022.137459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu H, Ding L, Qu G, Guo X, Liang M, Ma S, et al. Particulate matter exposure during pregnancy and infancy and risks of autism spectrum disorder in children: A systematic review and meta-analysis. Sci Total Environ. 2023;855:158830. 10.1016/j.scitotenv.2022.158830 [DOI] [PubMed] [Google Scholar]
- 19.Balalian AA, Stingone JA, Kahn LG, Herbstman JB, Graeve RI, Stellman SD, et al. Perinatal exposure to polychlorinated biphenyls (PCBs) and child neurodevelopment: A comprehensive systematic review of outcomes and methodological approaches. Environ Res. 2024;252:118912. 10.1016/j.envres.2024.118912 [DOI] [PubMed] [Google Scholar]
- 20.Morales-Suárez-Varela M, Peraita-Costa I, Llopis- GA. Systematic review of the association between particulate matter exposure and autism spectrum disorders. Environ Res. 2017;153:150–60. 10.1016/j.envres.2016.11.022 [DOI] [PubMed] [Google Scholar]
- 21.Yao H, Fu Y, Weng X, Zeng Z, Tan Y, Wu X, et al. The Association between Prenatal Per- and Polyfluoroalkyl Substances Exposure and Neurobehavioral Problems in Offspring: A Meta-Analysis. Int J Environ Res Public Health. 2023;20(3):1668. 10.3390/ijerph20031668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stojsavljević A, Lakićević N, Pavlović S. Does Lead Have a Connection to Autism? A Systematic Review and Meta-Analysis. Toxics. 2023;11(9):753. 10.3390/toxics11090753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yu X, Rahman MM, Wang Z, Carter SA, Schwartz J, Chen Z, et al. Evidence of susceptibility to autism risks associated with early life ambient air pollution: A systematic review. Environ Res. 2022;208:112590. 10.1016/j.envres.2021.112590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin L-Z, Zhan X-L, Jin C-Y, Liang J-H, Jing J, Dong G-H. The epidemiological evidence linking exposure to ambient particulate matter with neurodevelopmental disorders: A systematic review and meta-analysis. Environ Res. 2022;209:112876. 10.1016/j.envres.2022.112876 [DOI] [PubMed] [Google Scholar]
- 25.Lam J, Sutton P, Kalkbrenner A, Windham G, Halladay A, Koustas E, et al. A Systematic Review and Meta-Analysis of Multiple Airborne Pollutants and Autism Spectrum Disorder. Kesavachandran CN, editor. PLoS One. 2016;11(9):e0161851. [DOI] [PMC free article] [PubMed]
- 26.Burns JS, Williams PL, Sergeyev O, Korrick SA, Rudnev S, Plaku-Alakbarova B, et al. Associations of Peri-pubertal Serum Dioxins and Polychlorinated Biphenyls with Growth and Body Composition among Russian Boys in a Longitudinal Cohort. Int J Hyg Environ Health. 2020;223(1):228. 10.1016/j.ijheh.2019.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rossignol DA, Genuis SJ, Frye RE. Environmental toxicants and autism spectrum disorders: a systematic review. Transl Psychiatry. 2014;4(2):e360–e360. 10.1038/tp.2014.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed]
- 29.United States Environmental Protection Agency. Criteria Air Pollutants | US EPA [Internet]. 2022
- 30.Agency for Toxic Substances and Disease Registry. Chemical Classifications. 2012;1–3.
- 31.Barendregt JJ, Doi SA. MetaXL User Guide. 2015;1–52.
- 32.Doi SAR, Barendregt JJ, Khan S, Thalib L, Williams GM. Advances in the meta-analysis of heterogeneous clinical trials I: The inverse variance heterogeneity model. Contemp Clin Trials. 2015;45(Pt A):130–8. 10.1016/j.cct.2015.05.009 [DOI] [PubMed] [Google Scholar]
- 33.Alampi JD, Lanphear BP, Braun JM, Chen A, Takaro TK, Muckle G, et al. Association between Gestational Exposure to Toxicants and Autistic Behaviors Using Bayesian Quantile Regression. Am J Epidemiol. 2021;190(9):1803–13. 10.1093/aje/kwab065 [DOI] [PubMed] [Google Scholar]
- 34.Barkoski JM, Philippat C, Tancredi D, Schmidt RJ, Ozonoff S, Barr DB, et al. In utero pyrethroid pesticide exposure in relation to autism spectrum disorder (ASD) and other neurodevelopmental outcomes at 3 years in the MARBLES longitudinal cohort. Environ Res. 2021;194:110495. 10.1016/j.envres.2020.110495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bernardo BA, Lanphear BP, Venners SA, Arbuckle TE, Braun JM, Muckle G, et al. Assessing the relation between plasma PCB concentrations and elevated autistic behaviours using bayesian predictive odds ratios. Int J Environ Res Public Health. 2019;16(3):1–17. 10.3390/ijerph16030457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Braun JM, Kalkbrenner AE, Just AC, Yolton K, Calafat AM, Sjödin A, et al. Gestational Exposure to Endocrine-Disrupting Chemicals and Reciprocal Social, Repetitive, and Stereotypic Behaviors in 4- and 5-Year-Old Children: The HOME Study. Environ Health Perspect. 2014;122(5):513–20. 10.1289/ehp.1307261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carter SA, Rahman MM, Lin JC, Shu YH, Chow T, Yu X, et al. In utero exposure to near-roadway air pollution and autism spectrum disorder in children. Environ Int. 2022;158:106898. 10.1016/j.envint.2021.106898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gong T, Almqvist C, Bölte S, Lichtenstein P, Anckarsäter H, Lind T, et al. Exposure to air pollution from traffic and neurodevelopmental disorders in swedish twins. Twin Res Hum Genet. 2014;17(6):553–62. 10.1017/thg.2014.58 [DOI] [PubMed] [Google Scholar]
- 39.Granillo L, Sethi S, Keil KP, Lin Y, Ozonoff S, Iosif A-M, et al. Polychlorinated biphenyls influence on autism spectrum disorder risk in the MARBLES cohort. Environ Res. 2019;171(1):177–84. 10.1016/j.envres.2018.12.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guxens M, Ghassabian A, Gong T, Garcia-Esteban R, Porta D, Giorgis-Allemand L, et al. Air pollution exposure during pregnancy and childhood autistic traits in four European population-based cohort studies: The ESCAPE project. Environ Health Perspect. 2016;124(1):133–40. 10.1289/ehp.1408483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haggerty DK, Strakovsky RS, Talge NM, Carignan CC, Glazier-Essalmi AN, Ingersoll BR, et al. Prenatal phthalate exposures and autism spectrum disorder symptoms in low-risk children. Neurotoxicol Teratol. 2021;83:106947. 10.1016/j.ntt.2021.106947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hansen JB, Bilenberg N, Timmermann CAG, Jensen RC, Frederiksen H, Andersson AM, et al. Prenatal exposure to bisphenol A and autistic- and ADHD-related symptoms in children aged 2 and5 years from the Odense Child Cohort. Environ Heal A Glob Access Sci Source. 2021;20(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jo H, Eckel SP, Chen JC, Cockburn M, Martinez MP, Chow T, et al. Gestational diabetes mellitus, prenatal air pollution exposure, and autism spectrum disorder. Environ Int. 2019;133:105110. 10.1016/j.envint.2019.105110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Joyce EE, Chavarro JE, Rando J, Song AY, Croen LA, Fallin MD, et al. Prenatal exposure to pesticide residues in the diet in association with child autism-related traits: Results from the EARLI study. Autism Res. 2022;15(5):957–70. 10.1002/aur.2698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jung CR, Lin YT, Hwang BF. Air Pollution and Newly Diagnostic Autism Spectrum Disorders: A Population-Based Cohort Study in Taiwan. PLoS One. 2013;8(9). [DOI] [PMC free article] [PubMed]
- 46.Kim JI, Lee J, Lee KS, Lee YA, Shin CH, Hong YC, et al. Association of phthalate exposure with autistic traits in children. Environ Int. 2021;157:106775. 10.1016/j.envint.2021.106775 [DOI] [PubMed] [Google Scholar]
- 47.Lizé M, Monfort C, Rouget F, Limon G, Durand G, Tillaut H, et al. Prenatal exposure to organophosphate pesticides and autism spectrum disorders in 11-year-old children in the French PELAGIE cohort. Environ Res. 2022;212:113348. 10.1016/j.envres.2022.113348 [DOI] [PubMed] [Google Scholar]
- 48.Nowack N, Wittsiepe J, Kasper-Sonnenberg M, Wilhelm M, Schölmerich A. Influence of low-level prenatal exposure to PCDD/Fs and PCBs on empathizing, systemizing and autistic traits: Results from the duisburg birth cohort study. PLoS ONE. 2015;10(6):1–20. 10.1371/journal.pone.0129906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oudin A, Frondelius K, Haglund N, Källén K, Forsberg B, Gustafsson P, et al. Prenatal exposure to air pollution as a potential risk factor for autism and ADHD. Environ Int. 2019;133:105149. 10.1016/j.envint.2019.105149 [DOI] [PubMed] [Google Scholar]
- 50.Oulhote Y, Lanphear B, Braun JM, Webster GM, Arbuckle TE, Etzel T, et al. Gestational exposures to phthalates and folic acid, and autistic traits in Canadian children. Environ Health Perspect. 2020;128(2):1–12. 10.1289/EHP5621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pagalan L, Bickford C, Weikum W, Lanphear B, Brauer M, Lanphear N, et al. Association of Prenatal Exposure to Air Pollution with Autism Spectrum Disorder. JAMA Pediatr. 2019;173(1):86–92. 10.1001/jamapediatrics.2018.3101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pham C, Symeonides C, O’Hely M, Sly PD, Knibbs LD, Thomson S, et al. Early life environmental factors associated with autism spectrum disorder symptoms in children at age 2 years: A birth cohort study. Autism. 2022;26(7):1864–81. 10.1177/13623613211068223 [DOI] [PubMed] [Google Scholar]
- 53.Philippat C, Barkoski J, Tancredi DJ, Elms B, Barr DB, Ozonoff S, et al. Prenatal exposure to organophosphate pesticides and risk of autism spectrum disorders and other non-typical development at 3 years in a high-risk cohort. Int J Hyg Environ Health. 2018;221(3):548–55. 10.1016/j.ijheh.2018.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rahman MM, Shu YH, Chow T, Lurmann FW, Yu X, Martinez MP, et al. Prenatal Exposure to Air Pollution and Autism Spectrum Disorder: Sensitive Windows of Exposure and Sex Differences. Environ Health Perspect. 2022;130(1):1–9. 10.1289/EHP9509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rahman MM, Carter SA, Lin JC, Chow T, Yu X, Martinez MP, et al. Prenatal exposure to tailpipe and non-tailpipe tracers of particulate matter pollution and autism spectrum disorders. Environ Int. 2023;171:107736. 10.1016/j.envint.2023.107736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sagiv SK, Harris MH, Gunier RB, Kogut KR, Harley KG, Deardorff J, et al. Erratum: “Prenatal Organophosphate Pesticide Exposure and Traits Related to Autism Spectrum Disorders in a Population Living in Proximity to Agriculture.” Environ Health Perspect. 2018;126(7):079001. 10.1289/EHP4002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.van den Dries MA, Guxens M, Pronk A, Spaan S, El Marroun H, Jusko TA, et al. Organophosphate pesticide metabolite concentrations in urine during pregnancy and offspring attention-deficit hyperactivity disorder and autistic traits. Environ Int. 2019;131:105002. 10.1016/j.envint.2019.105002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Von Ehrenstein OS, Aralis H, Cockburn M, Ritz B. In utero exposure to toxic air pollutants and risk of childhood autism. Epidemiology. 2014;25(6):851–8. 10.1097/EDE.0000000000000150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang SY, Cheng YY, Guo HR, Tseng YC. Air pollution during pregnancy and childhood autism spectrum disorder in Taiwan. Int J Environ Res Public Health. 2021;18(18). [DOI] [PMC free article] [PubMed]
- 60.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ WV. Cochrane Handbook for Systematic Reviews of Interventions version 6.3. Cochrane. 2022.
- 61.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135. 10.1186/1471-2288-14-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.National Institutes of Health. Study quality assessment tools. 2014. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- 63.Xu K, Li Z, Qiao J, Wang S, Xie P, Zong Z, et al. Persistent organic pollutants exposure and risk of autism spectrum disorders: A systematic review and meta-analysis. Environ Pollut. 2023;336:122439. 10.1016/j.envpol.2023.122439 [DOI] [PubMed] [Google Scholar]
- 64.Ding M, Shi S, Qie S, Li J, Xi X. Association between heavy metals exposure (cadmium, lead, arsenic, mercury) and child autistic disorder: a systematic review and meta-analysis. Front Pediatr. 2023;11:1169733. [DOI] [PMC free article] [PubMed]
- 65.Amadi CN, Orish CN, Frazzoli C, Orisakwe OE. Association of autism with toxic metals: A systematic review of case-control studies. Pharmacol Biochem Behav. 2022;212:173313. 10.1016/j.pbb.2021.173313 [DOI] [PubMed] [Google Scholar]
- 66.Jafari Mohammadabadi H, Rahmatian A, Sayehmiri F, Rafiei M. The Relationship Between the Level of Copper, Lead, Mercury and Autism Disorders: A Meta-Analysis. Pediatr Heal Med Ther. 2020;11:369–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jeddi MZ, Janani L, Memari AH, Akhondzadeh S, Yunesian M. The role of phthalate esters in autism development: A systematic review. Environ Res. 2016;151:493–504. 10.1016/j.envres.2016.08.021 [DOI] [PubMed] [Google Scholar]
- 68.Radke EG, Braun JM, Nachman RM, Cooper GS. Phthalate exposure and neurodevelopment: A systematic review and meta-analysis of human epidemiological evidence. Environ Int. 2020;137:105408. 10.1016/j.envint.2019.105408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Volk HE, Hertz-Picciotto I, Delwiche L, Lurmann F, McConnell R. Residential Proximity to Freeways and Autism in the CHARGE Study. Environ Health Perspect. 2011;119(6):873–7. 10.1289/ehp.1002835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Grandjean P, Landrigan PJ. Neurobehavioural effects of developmental toxicity. Lancet Neurol. 2014;13(3):330–8. 10.1016/S1474-4422(13)70278-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shelton JF, Hertz-Picciotto I, Pessah IN. Tipping the Balance of Autism Risk: Potential Mechanisms Linking Pesticides and Autism. Environ Health Perspect. 2012;120(7):944–51. 10.1289/ehp.1104553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Neven KY, Saenen ND, Tarantini L, Janssen BG, Lefebvre W, Vanpoucke C, et al. Placental promoter methylation of DNA repair genes and prenatal exposure to particulate air pollution: an ENVIR ON AGE cohort study. Lancet Planet Heal. 2018;2(4):e174–83. 10.1016/S2542-5196(18)30049-4 [DOI] [PubMed] [Google Scholar]
- 73.Alfano R, Bijnens E, Langie SAS, Nawrot TS, Reimann B, Vanbrabant K, et al. Epigenome-wide analysis of maternal exposure to green space during gestation and cord blood DNA methylation in the ENVIRONAGE cohort. Environ Res. 2023;216:114828. 10.1016/j.envres.2022.114828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Li Y, Xie T, Cardoso Melo RD, de Vries M, Lakerveld J, Zijlema W, et al. Longitudinal effects of environmental noise and air pollution exposure on autism spectrum disorder and attention-deficit/hyperactivity disorder during adolescence and early adulthood: The TRAILS study. Environ Res. 2023;227:115704. 10.1016/j.envres.2023.115704 [DOI] [PubMed] [Google Scholar]
- 75.Zhuang H, Liang Z, Ma G, Qureshi A, Ran X, Feng C, et al. Autism spectrum disorder: pathogenesis, biomarker, and intervention therapy. MedComm. 2024;5(3):e497. [DOI] [PMC free article] [PubMed]
- 76.Cosemans C, Madhloum N, Sleurs H, Alfano R, Verheyen L, Wang C, et al. Prenatal particulate matter exposure is linked with neurobehavioural development in early life. Environ Res. 2024;252:118879. 10.1016/j.envres.2024.118879 [DOI] [PubMed] [Google Scholar]
- 77.Hertz-Picciotto I, Schmidt RJ, Krakowiak P. Understanding environmental contributions to autism: Causal concepts and the state of science. Autism Res. 2018;11(4):554–86. 10.1002/aur.1938 [DOI] [PubMed] [Google Scholar]
- 78.Costa LG, Cole TB, Dao K, Chang Y-C, Garrick JM. Developmental impact of air pollution on brain function. Neurochem Int. 2019;131:104580. 10.1016/j.neuint.2019.104580 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
No datasets were generated or analysed during the current study.