Abstract
Background
End-stage renal disease (ESRD) is the final stage of chronic kidney disease. Yet dialysis is not suitable for all ESRD patients. Moreover, while shared decision-making (SDM) is the preferred model for making medical decisions, little is known about SDM between nephrology nurses and ESRD patients in Israel.
Research Objective
Assessing the views, attitudes, practices, and ethical dilemmas of nephrology nurses in Israel regarding SDM with ESRD patients.
Methods
Using the descriptive quantitative approach, questionnaires were completed by 444 nephrology nurses in Israel. In addition to conducting descriptive statistics, t-tests for independent samples, f-tests for analysis of variance, and both tests for independence were also performed.
Ethical Considerations
The research aims, expected advantages and risks have been explained to respondents before completing the questionnaire to secure informed consent. Anonymity and confidentiality were ensured throughout the study. The study was approved by the Research Ethics Committee at the University of Haifa (Approval # 411/21).
Results
About one-third (30%–36.5%) of nurses reported discussing quality of life issues with ESRD patients, asking about their advance directives/power of attorney, exploring cultural/religious beliefs in end-of-life care, and ask about their preferred place of death. Nurses who convey high levels of patient-centered care (68.9%, p<0.0001), have high end-of-life training (76.2%, p<0.0001), and report cooperating with interdisciplinary teams (63.8%, p = 0.0415), also reported higher SDM practices than others. Nurses who refer less patients to palliative care (70%, p<0.0001) reported higher involvement in SDM compared to other nurses.
Conclusions
Nephrology nurses in Israel do not tend to implement the SDM model, despite its potential for improving quality of life for ESRD patients and their families and increasing conservative care options. Policy makers and educators in Israel should develop and implement training programs and support in the workplace, to enhance SDM between nephrology nurses and ESRD patients.
Keywords: nephrology nurses, shared decision-making, end-of-life, End-stage renal disease
Introduction
With end-stage renal disease (ESRD)—the final stage of chronic kidney disease 1 —three main treatment alternatives can be offered: dialysis, transplantation, and hemodialysis. 2 Yet dialysis often entails issues that could negatively impact the outcome, such as psychosocial circumstances, general frailty, comorbid load, and lack of clarity about the goals of this treatment. 3 Moreover, some ESRD patients are not suitable for dialysis, while others become too frail to continue this treatment.4–7 In such cases, conservative treatment or palliative care may be considered better alternatives.3,8
Clinical guidelines address end-of-life (EOL) issues for ESRD patients, such as avoiding futile dialysis, withholding and withdrawing dialysis, and offering palliative care. These guidelines provide nephrology teams with directions for decision-making and dealing with clinical and ethical dilemmas, while informing the patient about the risks and benefits of the treatment options, with an emphasis on the patient's values and preferences.9–11
The term shared decision making (SDM) refers to the process in which both the healthcare professional and the patient play a role in determining with course of treatment to pursue. 12 SDM may be inspired by the patient-centered care (PCC) approach that focuses on the patients and their healthcare providers, rather than on their diseases 13 —while enhancing values such as trust, respecting patients’ preferences, and sharing information with patients. 14 SDM is based on three theoretical models: The first model addresses the clinical practice through the following three stages: choice talk, where the healthcare provider assesses and presents the available treatment or care alternatives; option talk, where the healthcare provider offers adequate information about each option; and decision talk, where the healthcare provider and the patient consider the preferences and reach a shared decision as to the optimal course of treatment.
The second model categorizes SDM into the following three groups: essential SDM elements, such as defining the problem; ideal SDM elements, such as introducing unbiased information; and general SDM qualities, such as holding deliberations and negotiations. Finally, the third theoretical model addresses the following three types of treatment-related decisions: paternalistic decision-making, where the physician has the absolute authority for choosing the implemented course of treatment; shared decision making (SDM), where the physician and the patient jointly choose the implemented treatment; and informed decision-making, where the patient has the exclusive authority to make decisions regarding the treatment that is to be implemented.15–17
In many countries, Israel included, providing PCC is prioritized at the national level. Studies show that PCC leads to better healthcare outcomes, 18 yet little is known about the relationship between PCC and SDM. 19 According to the American Renal Physicians Association, SDM is the preferred model for medical decision-making—especially regarding ESRD patients—EOL patients who may require dialysis. 20 Moreover, little is known about EOL care and SDM among nephrology nurses who care for such patients in Israel.
In Israel, the ethical principle of sanctity of life usually outweighs individual autonomy, as seen in various laws. 21 The Dying Patient Act of 2005, for example, has shifted the normative framework that regulates EOL treatment in Israel from the patient perspective, based on the principle of autonomy, to the physician’s duty approach, based on the principle of sanctity of life. 22 Under this Act, the withholding of life-saving treatment is legally acknowledged for patients whose life expectancy is no greater than 6 months. Patients also have the right to receive palliative care—a service that is publicly funded by the comprehensive healthcare system and provided by the four health maintenance organizations in Israel. 23 (On the other hand, withdrawing or ceasing life-saving treatments is strictly prohibited by Israeli law, as are assisted suicide and euthanasia.) 24
With regards to treatments and expenses incurred by ESRD patients—all such patients are entitled to receive dialytic treatment—an expense that is covered by the national healthcare system. Such services include dialysis treatments, hospitalization, surgical interventions (such as creating and maintaining vascular access), and even partial reimbursement of transportation costs to and from the dialysis centers. 25
Involving nurses in SDM can enhance treatment decisions that are in line with patient's values and preferences, providing they have adequate experience, knowledge of the context and the patient, and intuition, interpretation, and reflection capabilities.26–29 Moreover, nurses can exercise their advisory role in helping patients make their decision, coaching them to express their preferences to the physician, or passing on important information to and from the physicians prior to the patients’ making their final decision.27,30,31
Yet as guidelines in Israel are lacking with regards to SDM, nephrology nurses may simply discuss medical decisions with physicians, based on the patient’s age, comorbidity, and preferences (explicit or implicit)—for example. While nurses can facilitate SDM, acting as a mediator between patients and physicians and providing emotional support for patients and families, the literature is lacking in input regarding nephrology nurses on SDM in EOL. The aim of this study, therefore, is to examine nephrology nurses' views and attitudes on practicing SDM when treating ESRD patients, while exploring conflicts and ethical dilemmas that these nurses face when attempting to execute SDM.
Literature review
Shared medical decision-making
SDM refers to a process whereby both the clinician and the patient take part in reaching healthcare decisions, after discussing the treatment benefits and risks, and while considering the patient's values, preferences, and circumstances. 32 Moreover, it includes prioritizing the patient, improving physical outcomes, and increasing patient safety, while decreasing complications, mortality, clinical errors, and treatment costs. 33 In the context of EOL care, SDM incorporates the patient’s preferences into the EOL consultation, improves patient knowledge and patient-clinician communications, and decreases conflicts. 32
Despite its advantages, SDM is not without challenges. First, medical and nursing students have relatively limited training options on SDM, as do practicing clinicians. Second, they lack accessible, up-to-date, and quality evidence regarding SDM. Third, SDM limits discussions on clinical issues where quality evidence does not exist, has not been synthesized, or has not been researched sufficiently. Moreover, While SDM has become a mandatory requirement in nephrology care in the United States,34,35 and is a health policy priority in Europe, 36 this process has not been adequately implemented in Israel in general, and in nephrology units in particular.
Nephrology and oncology nurses may face barriers in implementing SDM, such as being introduced late in the SDM process, lack of time, or unsuitable timing of information exchange,31,32,37 as well as additional barriers, such as discrepancies between professionals’ and patients’ perception, professionals’ discomfort in EOL situations, limited consideration of SDM, and difficulties assessing patients’ preferences.14,31,38
Attitudes and barriers in caring for ESRD patients
Nephrology nurses play an important role in dealing with fear of death among dialysis patients and their families. Nurses also play a key role in discussing, delivering, and managing EOL care.39–41 In the United States, an increase can be seen in advance practice nurses and nurse practitioners who have become certified palliative care nurses. Advance practice nurses in nephrology specialize in palliative care, offering treatment and support to EOL patients and their families. In Canada and the United States, nurse practitioners have been found to decrease the use of Emergency Wards and hospitalization, while promoting experiences of positive death in palliative care patients. 41 These nurses also focus on prolonging life and quality of life. 42 In Israel, the role of nurse specialists may include altering palliative care directives, assessing patients’ conditions, conducting emotional conversations with patients, families, and staff members, and supporting patients in EOL and bereavement care. 43
While nurses may hesitate to discuss EOL-related issues with patients, for fear of causing them to lose hope,39,42,44 they often initiate discussions with other team members about dialysis withdrawal and palliative care, after identifying suffering and diminished quality of life in patients. Nurses also offer emotional support to one another, yet find talking about death difficult in general. 45 Specifically, nephrology nurses have been found to have a medium-level avoidance attitude toward dying patients, with depression being prevalent among female nurses and those with more than 20 years’ experience. 46
Nephrology nurses are less confident than physicians in conducting difficult EOL-related conversations, and are less certain as to when to refer patients to palliative care specialists.47,48 On the other hand, some nurses try to impact the patients in their decision-making, if they feel that the patients are not choosing the most optimal or suitable course of treatment. 13 Following the withdrawal of dialysis or the death of a patient, nephrology nurses may suffer from overwhelming grief, following their prolonged relationship with patients and their families. The emotional trauma that they experience is expressed through insomnia, fatigue, difficulty concentrating, social withdrawal, physical pain, and more. The literature also reports nurse's detachment, negatively impacting both their personal and professional lives, and leading to nursing attrition. 44
A study conducted in Israel found that while 96.2% of dialysis nurses agreed that palliative care should be a key component in their patients’ health care, only 61.2% implement this in their units. Moreover, while 93% agreed that pain control should be a component of patient health care, only 67%–77% implement this. In the same study, 64%–70% of the respondents agreed that palliative care should be offered to terminal patients. This spectrum of responses could be attributed to insufficient awareness, nursing protocols, guidance and education, time, and support in the workplace. 49
In a study conducted by the American Nephrology Nurses Association (ANNA) and the National Kidney Foundation s (NKF), nurses were found to have limited knowledge for discussing advance care planning (ACP) with EOL patients and their families; yet those who received related training reported feeling confident in engaging in such conversations. 50 The positive effect of educational programs on nurses' ability to communicate during EOL care was also observed by HSU et al. 51 In line with recommendations that nurses should be provided with additional training on EOL care for patients, including ESRD patients, 46 clinical recommendations in Israel include creating palliative forums for interdisciplinary teams, offering specific training on palliative care, creating palliative care assessment tools and protocols, and promoting communications and support for families.49,52
The Israeli Ministry of Health has also introduced the certification of advanced practice registered nurses who specialize in palliative care, as a significant step toward addressing EOL healthcare needs.52,53 Three additional steps have been introduced by the Ministry, including increasing public awareness regarding palliative care, issuing the Dying Patient Act (2005), and publishing regulations regarding palliative care services. 54
Yet, the provision of palliative care is still inadequate, possibly due to a shortage in healthcare professionals who are trained or skilled in providing palliative care. Significant variance has been seen between palliative care education and training frameworks in Israel. 55 First, less than 20% of participants in such programs are physicians, creating difficulties for nurses to implement their newly acquired knowledge. Moreover, exact data is lacking regarding the scope of healthcare providers who have taken part in workshops or seminars on palliative care and EOL.
Additional barriers for delivering palliative care to patients with kidney disease, as reported by nurses, include differences in cultural and religious practices, nurses’ inexperience, lack of knowledge regarding when and how to approach the topic of palliative care with patients, and lack of collaboration between medical teams and nursing staff. 56 Dialysis nurses may also experience moral distress and be emotionally challenged, especially when patients express a wish to stop dialysis, or when the patients’ medical desires are not in line with those of their families or physicians. In turn, this could lead to poor nursing care, decreased job satisfaction, and feelings of powerlessness.57–60 Additional barriers include poor coordination between nephrology staff and palliative care teams, and clinicians’ perceptions that patients and families are reluctant to discuss palliative care, hospice care, or ACP. Yet many nephrology clinicians (nurses and physicians) report feeling comfortable caring for EOL patients with advanced chronic kidney disease. 61
Nurses' attitudes towards SDM
In EOL care, nurses play an important role in providing patients and their families with emotional support, 31 and are often the first persons to hear patients’ requests regarding treatment, including to withhold or withdraw from dialysis. 55 Nurses perceive themselves as filling an important and complementary role in the physicians’ decision-making process,27,30,31,45 thereby expanding their roles to also serve as educators, supporters, evaluators, and informants.38,62 Within the nephrology nursing practice, ANNA 63 recognizes the importance of palliative care and EOL health care, including professional and ethical responsibilities, referrals to palliative care and EOL programs, and collaborations with interdisciplinary teams. Patients also expect nurses to be involved in such decisions, 30 yet this is often the case. Studies found that in one-third of nephrology units, physicians are the exclusive decision-maker. Moreover, nephrologists rate themselves as most influential in the decision-making process, while nurses rate themselves as third most influential, followed by peers and physicians. 31 In another study, while some nurses perceived themselves as having an impact on patients’ healthcare decisions, others stated that physicians are the sole decision-makers. Moreover, nurses’ behaviors that contribute to SDM were found to include checking the quality of a decision, and complementing and facilitating SDM processes. 30 Other nurses exhibited moral distress when involved in life-prolonging treatment decisions regarding frail or short life-expectancy patients. Moreover, they felt powerless due to being unheard or overruled, and following physicians’ unrealistic expectations. Finally, nurses were found to refuse administering treatment if they were not involved in the decision-making process. 27
The literature emphasizes that in order to include nurses in SDM processes, they must have adequate time, transfer of information between nurses and physicians, knowledge about palliative care, skills in guiding patients at EOL, and clarity about their role in the process. 27 Nurses also state that SDM requires their facilitating of patient-physician communications, 38 clear transfer of information among nurses, and between nurses and healthcare providers, a supportive hospital culture towards nurses’ involvement in SDM, positive nurse-physician and nurse-patient relationships, and knowledge in SDM. 30
Studies show that nurses feel excluded and less involved in the decision-making setting regarding EOL treatment options, such as dialysis withdrawal. They report having a sense of low self-esteem, frustration and job dissatisfaction. 44 While in many countries, including New Zealand, Australia, Canada, the UK, and the US, nurses play an important role in decision-making, 31 SDM has not yet been implemented in nephrology units in Israel,. Yet, some aspects of it were applied in other medical fields, such as mental health, 64 diabetes health care, 65 fertility, 66 and cancer specialty. 67 The current study fills this void. It explores the practice of SDM in nephrology surveys nurses’ views and attitudes pertaining to such practice while providing EOL care to ESRD patients.
Nurses’ decisions to initiate and discuss ACP with patients depend on the mental and physical condition of the patients, and on the formers’ relationship with the latter. Additional barriers include lack of time, knowledge, and experience in discussing ACP issues, as well as difficulty determining the appropriate timing for ACP interventions.50,68 While some nurses report being capable of initiating talks on ACP, others state that this is the physicians’ responsibility to do so. Moreover, as in some cultures ACP may be equated with near death, nurses may delay or refrain from discussing this with patients. 68
Based on this literature review, the aim of this research is twofold: (1) To measure the frequency, extent, characteristics and factors encouraging or inhibiting the use of SDM at EOL care of ESRD patients. (2) To explore the decisional conflicts, ethical dilemmas and sources of decision-making pertaining to EOL care of ESRD patients. The main research question that this research will investigate is the following: To what extent do nephrology nurses pursue an SDM model while managing ethical dilemmas and clinical discretion pertaining to EOL care of ESRD patients in Israel?
Methodology
Conceptual framework
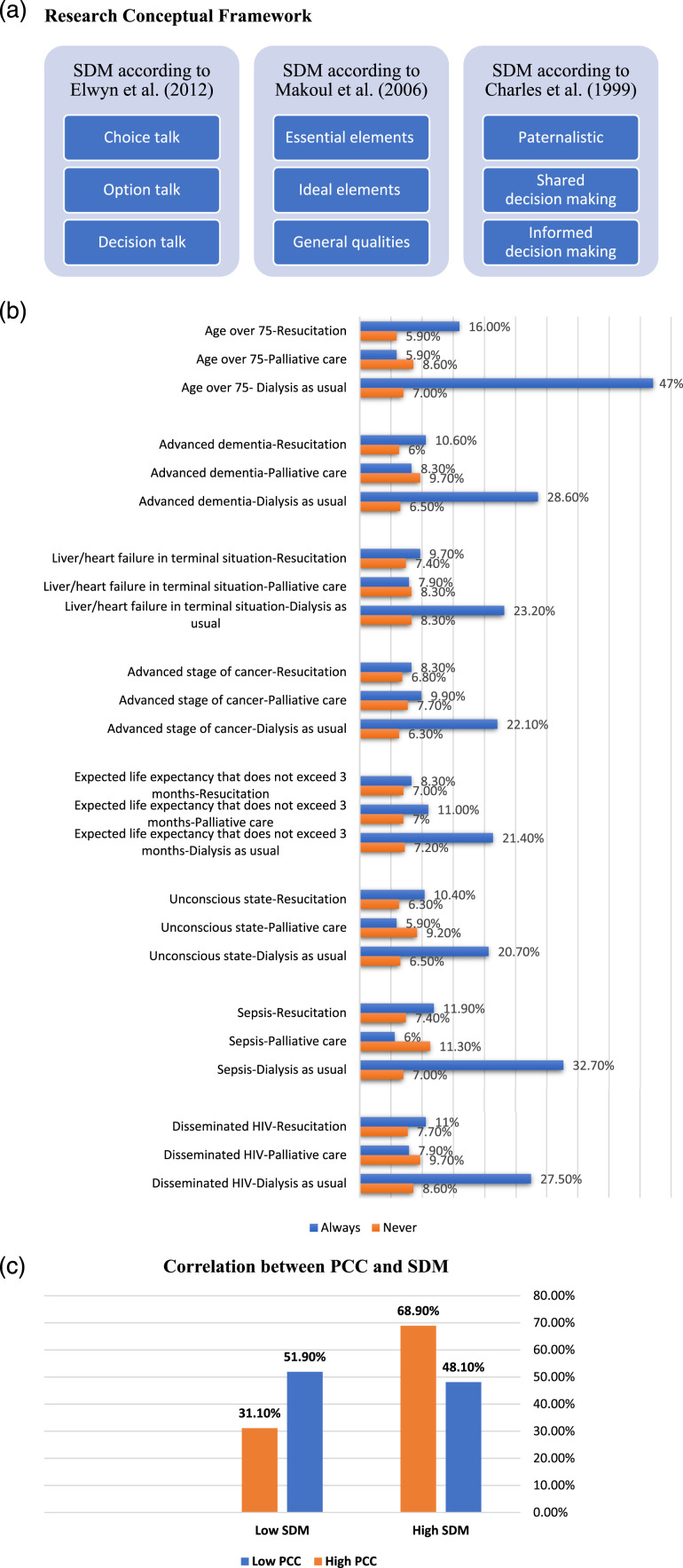
The conceptual framework applied in this study is based on three theoretical SDM models (Figure 1(a)). First, according to Elwyn and his colleagues, 15 SDM in clinical practice includes the following three stages: (1) choice talk, where the healthcare provider assesses and presents the available treatment or care alternatives; (2) option talk, where the healthcare provider offers adequate information about each option; and (3) decision talk, where the healthcare provider and the patient consider the preferences and reach a shared decision as to the optimal course of treatment.
Figure 1.
(a) Research conceptual framework. (b) Dialysis as usual, resuscitation and palliative care in hypothetical conditions in ESRD patients. (c) Correlations between PCC and SDM.
The second model, suggested by Makoul and Clayman, 16 categorizes SDM into three groups: essential SDM elements; ideal SDM elements; and general SDM qualities. First, the nine essential SDM elements include: (a) defining the problem; (b) presenting options; (c) discussing benefits, risks, and costs; (d) exploring patient values and preferences; (e) discussing patient capabilities; (f) exploring physicians’ knowledge and recommendations; (g) checking patients’ understanding; (h) making or deferring decisions; and (i) arranging a follow-up. Next, the four ideal SDM elements include: (a) introducing unbiased information; (b) defining roles; (c) presenting evidence; and (d) reaching a mutual agreement. Finally, the nine general SDM qualities include: (a) conducting deliberations and negotiations; (b) taking a flexible/individualized approach; (c) exchanging information; (d) involving at least two people; (e) finding the middle ground; (f) acting with mutual respect; (g) seeking partnership; (h) enhancing patient education and participation; and (i) deciding on the process and stages.
The third theoretical model, offered by Charles and her colleagues, 17 addresses three types of treatment-related decisions, including: (1) paternalistic decision-making, where physicians have absolute authority for choosing the implemented treatment; (2) SDM, where the physician and the patient jointly choose the implemented treatment; and (3) informed decision-making, where the patient has the exclusive authority to make decisions regarding the treatment that is to be implemented.
Research hypotheses
Palliative care and EOL care are of the utmost importance in nephrology practices. Moreover, nurses are expected to play a central role in providing ESDR patients with PCC, by referring patients to palliative facilities and EOL programs while collaborating with interdisciplinary teams and care providers. 63 Yet nephrology nurses are not always included in SDM processes in a timely and comprehensive manner, 31 despite patients expecting them to be involved in these processes, and despite such collaborations being key to promoting PCC. 26 Indeed, PCC is an important component in SDM, 16 just as SDM is important tool for promoting PCC.31,69 Based on the literature review and conceptual framework presented above, we propose the following hypothesis:
H1
Nephrology nurses who provide PCC and collaborate with interdisciplinary teams and healthcare providers will be more involved in SDM processes than those who do not.
Moreover, nurses tend to lack knowledge of EOL communications regarding ACP, yet studies indicate a range of positive outcomes for nurses’ SDM training programs, including improved attitudes toward collaborative work, enhanced understanding of PCC, and increased intent to engage in SDM.50,51,70 We therefore also propose the following hypothesis:
H2
Nephrology nurses with greater educational training in EOL care will report greater involvement in SDM compared to those with less training.
Research design
Using the descriptive quantitative approach, we examined the views and attitudes of nephrology nurses regarding SDM in ESRD patients. Based on the literature and the theoretical frameworks presented above, we created a cross-sectional questionnaire. It should be noted, however, that this study is part of a larger research project in which we also examined the views and attitudes of nephrology physicians regarding SDM in ESRD patients (article under review).
Research population, sample, and sampling
Our research population included nephrology nurses working in hospitals and community-based dialysis clinics. According to the Israeli Nephrology Nurses Association (INNA) and other current estimations, in December 2021 there were about 1360 nephrology nurses (850 of them are members of this association) working in nephrology wards and dialysis clinics in Israel. Using non-probability and snowball sampling methods, 444 nephrology nurses were recruited to participate in this study, i.e., about 32% of the nephrology nurse population in Israel.
Data collection
First, a pilot study was conducted, with the questionnaire being sent to 10 nurses from nephrology units across Israel. Following the feedback received during the pilot study, the questionnaire was revised and then posted online via the Qualtrics XM software. A link to the survey was posted on eight professional Facebook groups, three WhatsApp groups, and through the mailing list of INNA members. The link was also distributed via snowball sampling and direct calls for participation by the researchers. Printed copies of the survey were also delivered during staff meetings and at two national nephrology conferences.
Data analysis
The data obtained from the questionnaire were analyzed using descriptive and inferential statistics, and a range of analytical methods. For example, to measure differences between respondents from different groups – based on the theoretical categorization of correlations between participants’ EOL training and involvement in SDM – T-tests for independent samples, F-tests for analysis of variance (ANOVA), and both tests for independence were performed. Numerical descriptive measures were also used to describe the most common attitudes among respondents regarding EOL care for ESRD patients and SDM (%). Five primary variables were calculated for testing the research hypotheses: (1) PCC, based on three items from the questionnaire (items 31, 34, 41), each coded on a 1–5 scale. The PCC index equals the mean scores of these items.; (2) Palliative care referral, based on two items (items 82 and 84), each coded on a 1–5 scale. The palliative care referral index equals the mean scores of these items, after reversing the direction of the response scale.; (3) Training, based on two items from the questionnaire (items 12 and 14). Item 12 includes five types of training, for which the sum was calculated to obtain a 1–5 scale. Item 14 was originally a 1–5 Likert-like scale item. The training index equals the means scores of these items after reversing the direction of the response scale.; (4) Cooperation, based on four items (items 32, 46, 47, 48), each coded on a 1–5 scale. The cooperation index is the mean scores of these items.; and (5) Involvement in SDM processes, based on eight items from the questionnaire (items 17, 36, 52, 54, 55, 56, 57, 69). Item 36 includes eight professions, where nurses were coded ‘5’ and all others were coded ‘1’. Item 52 is an open = ended question, where the contents of the responses were coded into a 1–5 scale. Item 69 consists of five types of decision-making, which were coded into a 1–5 scale. Items 17, 54, 55, 56, and 57 were all originally on a 1–5 Likert-like scale. The involvement in SDM processes index was calculated as the means scores of these eight items. The internal consistency of the entire questionnaire was high (Cronbach’s α = 0.86).
Finally, to measure PCC, we referred to the following five sub-variables: (1) scope of the physician’s role in the patient’s decision-making process and outcomes; (2) responsibility regarding medical decisions; (3) patient’s understanding of ceasing dialysis; (4) discussing dialysis with the patient prior to treatment; and (5) patient’s understanding of palliative care and hospice.
Ethical considerations
At the onset of the questionnaire, before question #1, a short description was presented regarding the research aims, expected advantages, risks, and duration needed for completing the questionnaire—serving as informed consent granted by the respondent. The researchers' contact details were also clearly stated. Anonymity and confidentiality were ensured throughout the study. The complete research study was approved by the Research Ethics Committee at the researchers' affiliated academic institution (Approval # 411/21).
Results
Respondents' characteristics
Of the 444 completed questionnaires, 223 were completed in the printed version, while 221 were completed digitally online. The research sample included 63.2% females and 36.8% males, with a mean age of 45 years (SD = ±10.2). The majority of respondents were born in Israel (67.2%) and married (73.9%). Moreover, 53.1% were Jewish and 46.9% Arabs. In connection to religion, 53.1% were Jewish, 36% Muslims, 13.9% Christians and 1.9% Agonistics. Table 1 describes the research sample.
Table 1.
Participant characteristics.
| Variables | |
|---|---|
| Gender | Females = 63.2%; males = 36.8% |
| Age | Range: 23–72 years (M = 45; SD±10.2) |
| Country of birth | Israel = 67.2%; Russia = 17.7%; Ukraine = 3.3%; other = 11.8% |
| Marital status | Married = 73.9%; single = 14.8%; divorced = 6.5%; in a relationship = 2.9%; widowed = 1.9% |
| Nationality | Jewish = 53.1%; Arabs = 46.9% |
| Religion | Jewish = 53.1%; Christian = 13.9%; Muslim = 36%; Agonistic = 1.9%; Druze = 0.5% |
| Level of religiosity | Jewish Ultra-orthodox = 2.3%; religious = 20.8%; traditional = 38.6%; secular = 38.3% |
| Specialization a | Registered nurse = 100%; nephrology nurse = 78.6%; nephrology nurse and advanced palliative care = 10.8% |
| Work experience | Range: 0.5–43 years (M = 14; SD±9.9) |
| Type of workplace | Public hospital = 50%; government hospital = 24.8%; private dialysis clinic in the community = 18.2%; private hospital = 8.1% |
| Geographical region of workplace | South = 12.4%; Center = 28.2%; Sharon = 9.2%; North = 38.3%; Jerusalem and surrounding area = 11.7% |
aNurses could have more than one specialization.
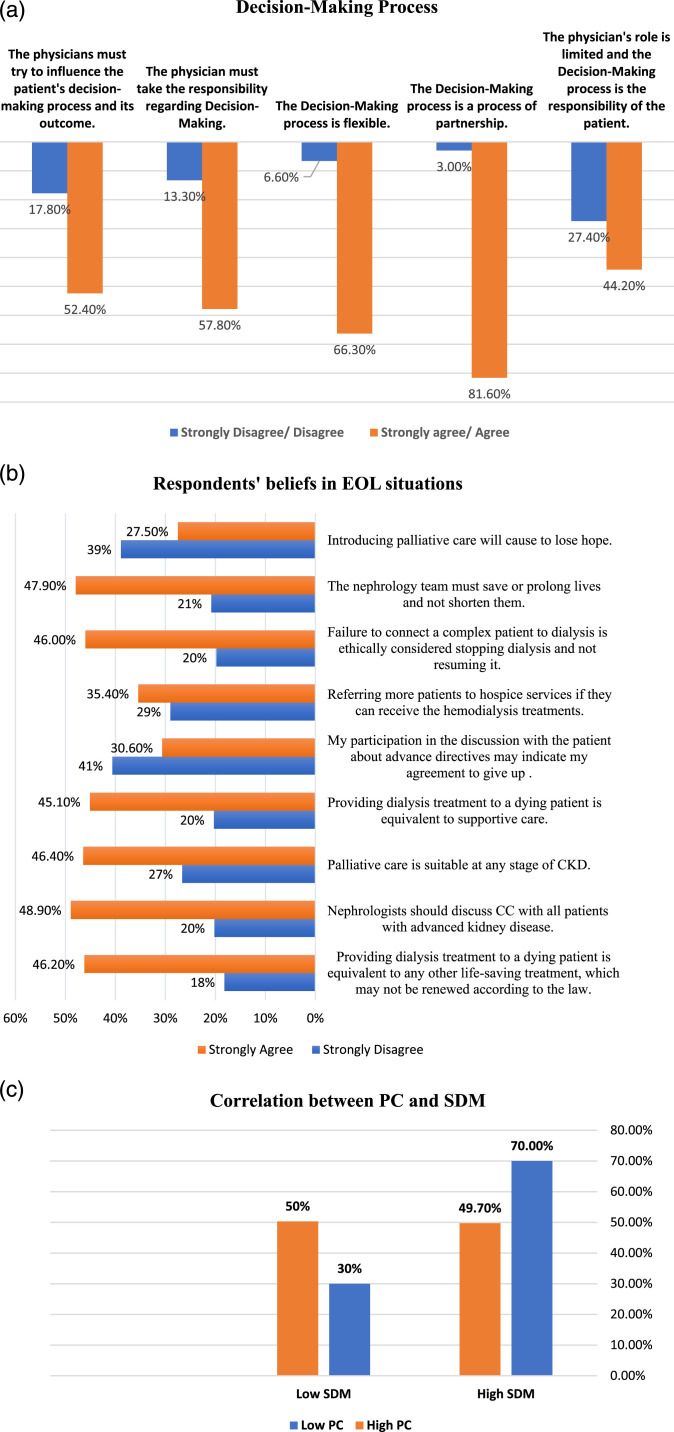
Nurses’ attitudes toward SDM
The findings show that while nephrology nurses strongly agree or agree that clinical decision-making is a process of partnership (81.6%), and one that is flexible (66.3%), they also believe that the physicians must take responsibility regarding the medical decision (57.8%). Moreover, while half the respondents strongly agree or agree that the physicians must try to influence the patient's decision-making and its outcomes (52.4%), almost half (44.2%) perceive that the physician's role is limited and as such, the decision-making responsibility is the patients’ (Figure 2(a)).
Figure 2.
(a) The decision-making process. (b) Respondents' beliefs regarding EOL situations. (c) Correlations between palliative care and SDM.
A small percentage of respondents report that it is the physician who makes the final decision—either after consulting with nurses (10.4%) or without doing so (5.4%). Decision-making regarding care for ESRD patients is claimed to be most impacted by professional considerations (90%), followed by specific emotional consequences of the specific case (59%). Potential legal liability, religious beliefs, self-esteem within the department, workload, and the number of patients under the respondents’ responsibility were found to play a lesser role (about 36%–50% each).
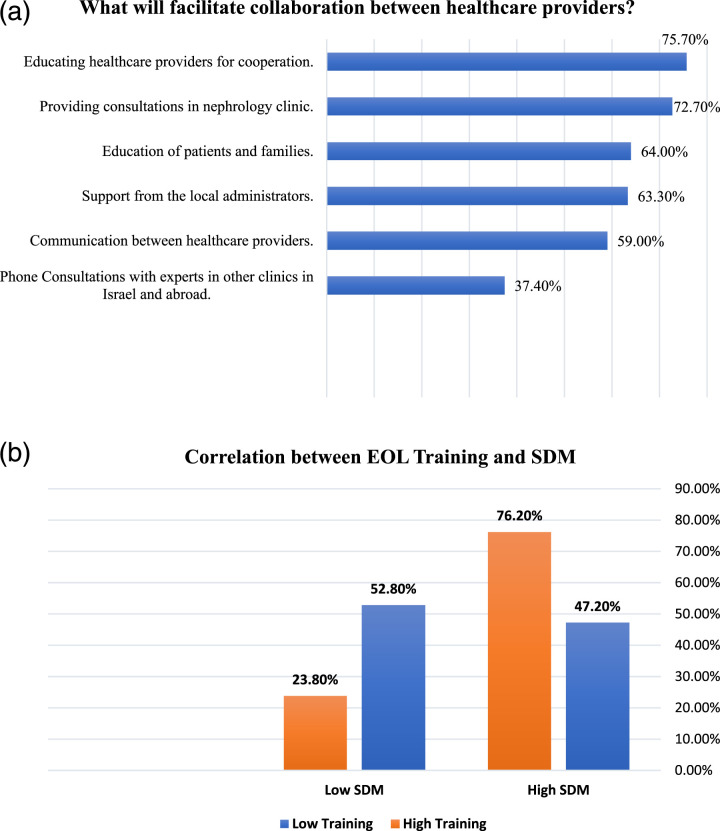
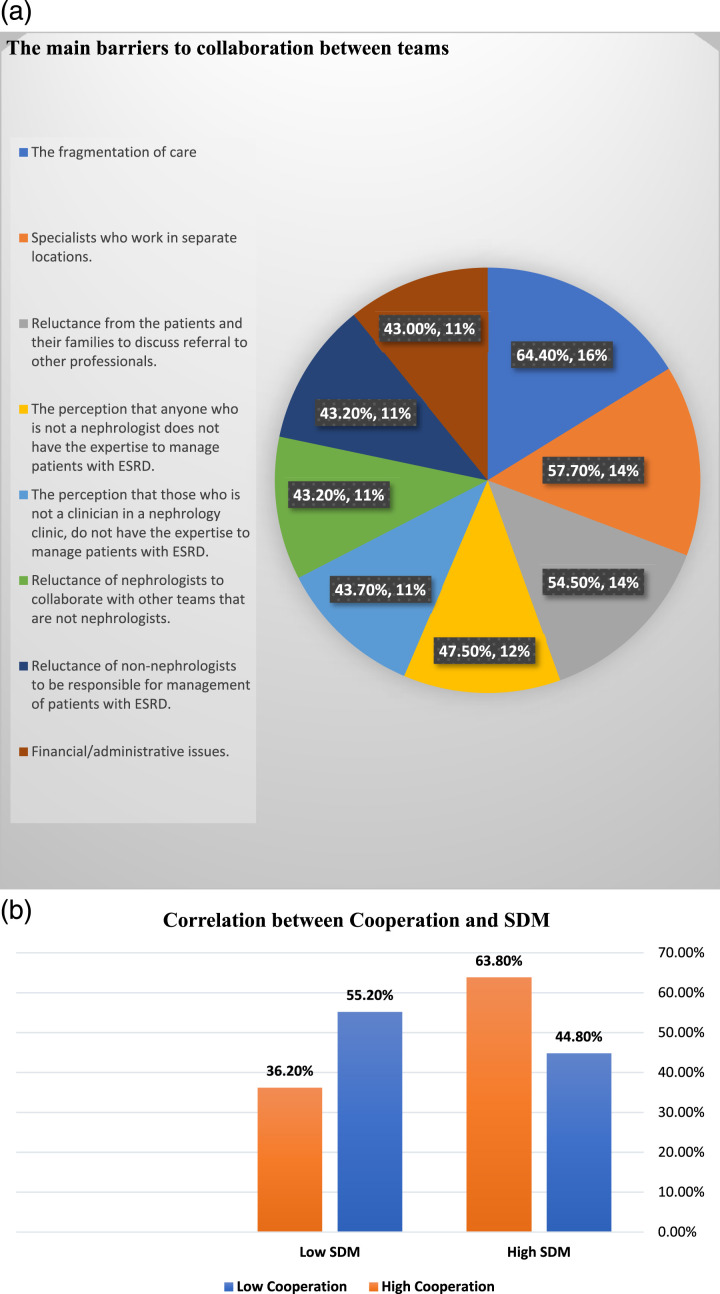
The study also reveals that nurses believe that physicians tend to make decision together with other healthcare professionals, including nurses (71%), other physicians on the ward (66%), social workers (61%), palliative care consultants and physicians outside the ward (41%), the hospital’s Ethics Committee (28%), and religious authorities from the patient's surroundings (26%). Moreover, nurses strongly agree that collaborations between teams improve patient care efficiency (51.2%) and job satisfaction (47.1%), while reducing workloads (33.8%). Respondents also perceive an additional range of factors as facilitating team collaborations (Figure 3(a)).
Figure 3.
(a) Facilitating collaborations between healthcare providers. (b) Correlations between training and SDM.
Barriers to team collaborations (Figure 4(a)), on the other hand, include fragmentation of care (64.4%), specialists working from different locations (57.7%), and patients and families’ reluctance to discuss referral to other professionals (54.4%).
Figure 4.
(a) Main barriers in collaboration between teams. (b) Correlations between cooperation and SDM.
With regards to physician-patient communications, about 36% of respondents believe that it is important to discuss all available treatment options with ESRD patients. Interestingly, almost 12% of respondents believe that patients with ESRD tend to avoid discussing their prognosis, 60.8% claim that patients do not fully understand the consequences of stopping dialysis, and 15% state that ESRD patients are more prone to depression and anxiety, which limits their decision-making abilities regarding EOL care.
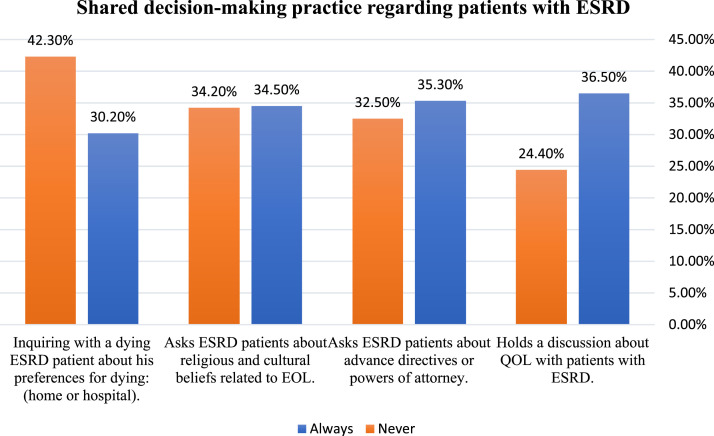
SDM practices
Regarding SDM practices, Jewish Ultra-orthodox Jewish or religious respondents reported the highest levels of progressive involvement in SDM (70.7%) compared to traditional or secular respondents who report lower levels (64.8% and 56.1%, respectively) [χ2 (2) = 6.10, p = 0.0473]. About one-third of the respondents believe that they regularly conduct discussions about quality of life with ESRD patients (36.5%), ask them about their advance directives/power of attorney (35.3%), inquire about religious and cultural beliefs related to EOL (34.5%), and inquire about their patient's preferred place of dying (30.2%) (Figure 5(a)).
Figure 5.
SDM practices regarding ESRD patients.
Nurses’ attitudes toward EOL training and care of ESRD patients
The findings show that about 40% of the nephrology nurses in this study report that they meet patients with ESRD who are aged 75 and older between 10–20 times a month or more, 19.5% encounter patients with end-stage liver/heart failure, and 18% care for patients with advanced stages of dementia and sepsis within these frequency rates. A smaller portion (14.5%–16%) of nephrology nurses care for patients with other co-morbidities.
About 26% of respondents reported having received no specific training for providing EOL care. Almost half the respondents reported having received training on EOL symptom and care management (45%), legal issues relating to EOL and palliative care (43%), and advance directives (33%). the EOL training was conducted via workshops (46.8%), professional conferences (40%), while on the job (40%), or in academic institutions (30%). Differences were seen in the respondents’ levels of EOL training based on their religious affiliation, whereby Christian respondents reported the highest levels of advanced training (67.8%), followed by Jewish (52.7%) and Muslim or (46.5%) Druze respondents [χ2 (3) = 10.19, p = 0.0170]. No such significant differences were found based on the respondents' religiosity levels.
About two-thirds of respondents reported that they feel comfortable conversing with ESRD patients and their families regarding prognoses, quality of life, and treatment options (62.3%). About half the respondents feel confident in managing palliative care for patients who stop receiving dialysis (54.1%) and in assisting them in formulating and executing advance directives/power of attorney (52.2%), and report having received sufficient training in managing and evaluating EOL symptoms among ESRD patients (49.3%).
When examining the respondents’ perceptions as to how nephrologists would act in hypothetical EOL situations (Figure 1(b)), the findings indicate that few nurses (20.7%–23.2%) believe that nephrologists would offer dialysis to patients with liver/heart failure in a terminal state, to patients with a life expectancy of up to 3 months, or to patients in advanced stages of cancer. Moreover, very few nurses (8.6%) believe that nephrologists would offer dialysis to patients with disseminated human immunodeficiency virus (HIV). Nurses also believe that palliative care is mainly offered mostly when the patient’s life expectancy is up to 3 months (11%) or in advanced stages of cancer (9.9%). Such treatment will mostly not be offered when the patient has sepsis (11.3%), disseminated HIV (10%) or advanced dementia. Finally, very few nurses believe that nephrologists will always resuscitate ESRD patients with a life expectancy of up to 3 months or in advanced stages of cancer (8.3%) and will resuscitate patients over the age of 75 (16%).
Finally, we also examined the respondents' attitudes towards EOL care for patients with ESRD. In Israel, although the law forbids stopping life-support or life-saving treatments after they have been started, yet in certain circumstances dialysis treatments can be stopped. 69 As seen in Figure 2(b), about 50% of respondents strongly agree or agree that providing dialysis to dying patients is equivalent to any other life-saving treatment. Overall, between 30%–50% of respondents agree that nephrologists should discuss conservative care options and advance directives with these patients, and refer them to palliative care. Finally, the respondents' religiosity level is correlated with their attitudes towards palliative care, whereby the more religious the respondents, the less in favor they are of palliative care (χ2 (2) = 16.74, p = 0.0002).
The relationship between SDM styles and treatment decisions
The first hypothesis, whereby nurses who provide PCC and collaborate with interdisciplinary teams will be more involved in SDM than others, was confirmed. As seen in Figure 1(c), a significant positive correlation was seen between PCC and involvement in SDM [χ2(1) = 16.97; p<.0001]. Moreover, as seen in Figure 4(b), a significant positive correlation was also seen between collaboration and involvement in SDM [χ2(1) = 4.16, p = 0.0415], whereby nurses who reported high levels of PCC and who collaborate with interdisciplinary teams, also reported high SDM involvement.
The second hypotheses, whereby nurses with greater training in EOL care will report greater involvement in SDM compared to others, was partially confirmed. As seen in Figure 2(c), a significant negative correlation was seen between palliative care and involvement in SDM [χ2(1) = 16.61; p<.0001], whereby nurses who refer more patients to palliative care report lower levels of involvement in SDM processes. However, as seen in Figure 3(b), a significant positive correlation was seen between EOL training and involvement in SDM [χ2(1) = 38.99; p<0.0001).
Discussion
The aim of this study was to investigate the degree to which the SDM model is implemented by nephrology nurses in Israel when providing EOL care for ESRD patients. The findings indicate that about one-third of respondents always discuss quality of life with ESRD patients, inquire about their preferred place of dying and religious and cultural beliefs, and ask about their advance directives/power of attorney; yet one-third of respondents never do so. One-quarter of respondents never discuss quality of life with their patients and almost half never inquire into their preferred place of dying. Yet nephrology nurses are expected to have a professional and ethical responsibility to provide PCC and referrals to palliative care and EOL programs,50–52,63,70 and are considered a key source for managing and delivering such care. 41 The findings of this study highlight that nurses are not always as involved in SDM process as they would like to be and as it is suggested in the literature that they should be, and they rate themselves as having a low place in terms of their impact on the decision-making process—a finding that is in line with previous studies.31,71 Moreover, as with previous studies, our findings indicate that some nurses believe that the physician has the exclusive decision-making responsibility. 30
In the current study, a gap was also seen between what respondents declare and what they actually do in relation to SDM practices and EOL care. In Canada and the United States, the role of the nephrology nurse is to promote positive experiences of dying among palliative care patients, 41 assist patients in EOL decision-making, and initiate discussions about death and dying.39,43 As seen in previous studies, respondents also address their lack of time and knowledge regarding palliative care, 27 and may refrain from initiating EOL conversations due to lack of familiarity with the patients’ cultural/religious beliefs, lack of formal policies, and feelings of discomfort. 72 Finally, some nurses believe that palliative care is not within the scope of their practice.50,68
The findings of this study also reveal that about two-thirds of respondents strongly agree that physicians should be responsible for the decision-making; half also believe that physicians should attempt to influence the patient in the decision-making process. On the other hand, more than 80% strongly agree that decision-making should be a process of partnership, and almost half believe that the physician's role is limited. These contrasting data represent the complexity of medical decisions in general, and in EOL nephrology care in particular. The literature indicates that nurses support patients in constructing the most suitable treatment, and facilitate SDM by enhancing patient-physician communications and preparing patients for relevant conversations.50,68
As mentioned, a significant correlation was seen among respondents between PCC and involvement in SDM—a finding that highlights the importance of implementing a PCC approach among healthcare professionals, in order to fully achieve SDM, 14 as well as the importance of SDM as a means for promoting PCC.31,69 Our findings also correspond with patients' expectations that nurses should be involved in such decisions, thereby promoting PCC. 30 According to the literature, in order to transition to a PCC approach of SDM, nephrology nurses should focus on asking the right questions, while building an effective patient-physician partnership, as a means for enhancing patients’ autonomy. 73
A positive correlation was also found between EOL training and involvement in SDM, in line with previous studies, 74 whereby such training improves nurses' attitudes toward SDM processes 51 and toward collaborative work, while deepening their understanding of PCC and their intent to engage in SDM. 70
Finally, only about one-third of nephrology nurses in Israel were found to have received training on advance directives, and only one-quarter had undergone training on legal issues relating to EOL, palliative care, and symptom management in EOL care. A recent study found that nephrology nurses who received training related to ACP reported feeling comfortable and confident engaging in EOL discussions with patients. 50 Moreover, up to 50% of respondents agree that nephrologists should discuss conservative care options or advance directives with patients, and should refer them to palliative care when needed. We also found that nurses perceive themselves as less confident than physicians in conducting difficult EOL conversations, having less clarity about when to refer patients to palliative care specialists, and having less psychological support when caring for EOL patients.47,48
Limitations
Despite the important contribution of this study to the literature, several research limitations should be addressed. First, the study focuses specifically on the attitudes of nephrology nurses in Israel regarding SDM in EOL health care. As such, generalization of the findings to additional nursing populations should be made with caution. However, the large sample included in this study indicates that these findings are likely to also be representative of nurses from additional fields. Moreover, the non-probability and snowball sampling applied in this study limits the equal chance of potential participants being included in the sample; this sampling method could also have potential sampling bias (since respondents select other participants for the sample), as well as a potential margin of error. It may be that we did not reach all nurses in nephrology care, as not all nurses have access to the Internet and social media. Yet despite these limitations, the variety of sources for recruiting respondents (including via the INNA) ensures that the study provides a coherent and rich snapshot of the research phenomenon. Finally, as the questionnaire was relatively long, participants may have dropped out prior to answering all questions. Yet the number of completed questionnaires was adequately substantial for reaching important results and conclusions.
Conclusions
Nephrology nurses in Israel do not tend to implement SDM models in EOL health care. Moreover, few nurses discuss quality of life with EOL patients, ask about their advance directives/power of attorney, or inquire about their related cultural or religious beliefs at EOL, or inquire about the patient’s preferred place of dying. The nurses in this study reported that the nephrology staff tend to make decisions about dialysis withholding/withdrawal and about referrals to palliative care without including the EOL patient or family. Improved SDM and collaborations within interdisciplinary teams and between teams and their patients could improve care quality and offered treatment options, including offering palliative care. As such, nephrology programs should develop and conduct training programs on PC and SDM for medical and nursing students and professionals, especially in EOL care.
Appendix 1.
Questionnaire Description
The questionnaire included 89 items, comprised mostly of closed-ended questions, items that were rated on a 1–5 Likert-like scale, and some open-ended questions. Some items, that had been previously validated and published in the literature, were translated into Hebrew, discussed, and revised by the researchers of this article. The questionnaire was comprised of four sections: (1) eleven background questions, such as marital status, workplace, experience, and age; (2) seven questions were adapted from Metzger and her colleagues, 61 regarding the respondents’ training in EOL care and decision-making, including two closed-ended questions assessing. For example, questions regarding their nursing training (items 12, 13), or providing patients with assistance in preparing advance directives or appointing power of attorney (items 14–18), which the respondents were asked to rate on a 1–5 Likert-like scale, such as 1 = strongly disagree, 5 = strongly agree; (3) based on the conceptual framework of this research15–17,75, 39 items examined the respondents' attitudes and practices regarding SDM, and were rated on a 1–5 Likert-like scale, such as 1 = strongly disagree, 5 = strongly agree. Some questions assessed whether the respondents define the problem for the patient during the decision-making process, or whether they offer the patient freedom of choice regarding the proposed treatment. Other questions assessed who the physician tends to involve when making decisions regarding ESRD patients, using close-ended multiple choices questions; and (4) finally, 32 items addressed EOL care for ESRD patients, and nurses’ attitudes toward such care, based on Lunney et al.’s (2002) 76 categorization of EOL care. Some items addressed issues such as the role of palliative care and the complexity of care in ESRD patients, while others, adapted from Hong et al., (2021), 77 aimed at assessing how nurses think physicians would act in certain hypothetical situations, such as referring the ESRD patient to dialysis or palliative care. High overall consistency was seen for the questionnaire (Cronbach’s α = 0.86).
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Minerva Center for Interdisciplinary Studies of the End of Life.
Correction (October 2023): This article has been updated with minor textual corrections since its original publication.
ORCID iDs
Wassiem Abu Hatoum https://orcid.org/0000-0002-4649-7994
Daniel Sperling https://orcid.org/0000-0002-4371-7736
References
- 1.Zhou Y, Yang J. Chronic kidney disease: overview. Chronic kidney disease. Singapore: Springer, 2020, pp. 3–12. [Google Scholar]
- 2.Friedman EA. Introduction and options in therapy. Present and Future Therapies for End-Stage Renal Disease. New Jersey: World Scientific Publishing Company, 2022, pp. 1–8. [Google Scholar]
- 3.Misra M. ESRD in the Elderly: The Scope of the Problem. Dialysis in older adults: a clinical handbook. New York: Springer, 2015, pp. 1–8. [Google Scholar]
- 4.Bagasha P, Leng M, Katabira E, et al. Health-related quality of life, palliative care needs and 12-month survival among patients with end stage renal disease in Uganda: protocol for a mixed methods longitudinal study. BMC Nephrol 2020; 21(1): 531–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buur LE, Finderup J, Søndergaard H, et al. Shared decision-making and planning end-of-life care for patients with end-stage kidney disease: a protocol for developing and testing a complex intervention. Pilot Feasibility Stud 2022; 8(1): 226–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gunda S, Thomas M, Smith S. National survey of palliative care in end-stage renal disease in the UK. Nephrol Dial Transplant 2005; 20(2): 392–395. [DOI] [PubMed] [Google Scholar]
- 7.Okamoto I, Tonkin-Crine S, Rayner H, et al. Conservative care for esrd in the united kingdom: a national survey. Clin J Am Soc Nephrol 2015; 10(1): 120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martin DE, Harris DCH, Jha V, et al. Ethical challenges in nephrology: a call for action. Nat Rev Nephrol 2020; 16(10): 603–613. [DOI] [PubMed] [Google Scholar]
- 9.Holley JL, Davison SN, Moss AH. Nephrologists’ changing practices in reported end-of-life decision-making. Clin J Am Soc Nephrol 2007; 2(1): 107–111. [DOI] [PubMed] [Google Scholar]
- 10.Moss AH. Shared decision-making in dialysis: the new RPA/ASN guideline on appropriate initiation and withdrawal of treatment. Am J Kidney Dis 2001; 37(5): 1081–1091. [DOI] [PubMed] [Google Scholar]
- 11.National Kidney Foundation . 2006 updates clinical practice guidelines. USA: American Journal of Kidney Diseases, 2006. [Google Scholar]
- 12.Blount A. Getting from “Delivering Care to Patients” to “Partnership with Patients”. Patient-centered primary care. USA: Springer International Publisher, 2019, pp. 59–62. [Google Scholar]
- 13.Noble H, Brazil K, Burns A, et al. Clinician views of patient decisional conflict when deciding between dialysis and conservative management: qualitative findings from the Palliative Care in chronic kidney disease (PACKS) study. Palliat Med 2017; 31(10): 921–931. [DOI] [PubMed] [Google Scholar]
- 14.Karnieli-Miller O, Artom TR, Neufeld-Kroszynski G. Time to rise to the challenge of truly implementing patient-centered care and shared decision-making in Israel : the educational and policy mission. The Journal of Evidence, Education and Quality in Healthcare 2022; 171: 68–73. [DOI] [PubMed] [Google Scholar]
- 15.Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med 2012; 27(10): 1361–1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns 2006; 60(3): 301–312. [DOI] [PubMed] [Google Scholar]
- 17.Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med 1999; 49(5): 651–661. [DOI] [PubMed] [Google Scholar]
- 18.Topaz M, Bar-Bachar O, Admi H, et al. Patient-centered care via health information technology: a qualitative study with experts from Israel and the U.S. Inform Health Soc Care 2020; 45(3): 217–228. [DOI] [PubMed] [Google Scholar]
- 19.Moumjid N, Durand M-A, Carretier J, et al. Implementation of shared decision-making and patient-centered carein France: towards a wider uptake in 2022. Z Evid Fortbild Qual Gesundhwes 2022; 171:42–48. [DOI] [PubMed] [Google Scholar]
- 20.Galla JH. Clinical practice guideline on shared decision-making in the appropriate initiation of and withdrawal from dialysis. J Am Soc Nephrol 2000; 11(7): 1340–1342. [DOI] [PubMed] [Google Scholar]
- 21.Schweda M, Schicktanz S, Raz A, et al. Beyond cultural stereotyping: views on end-of-life decision making among religious and secular persons in the USA, Germany, and Israel. BMC Med Ethics 2017; 18(1): 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shalev C. End-of-life care in israel—the dying patient law, 2005. Isr Law Rev 2009; 42(2): 279–305. [Google Scholar]
- 23.Muscat NA, Figueras J, Kluge Het al. Health systems in action Israel. Israel: World Health Organization, 2022, pp. 8–9. [Google Scholar]
- 24.Dopelt K, Cohen D, Amar-krispel E, et al. Facing death : attitudes toward physician-assisted end of life among physicians working at a tertiary-care-hospital in Israel. Int J Environ Res Publ Health 2021; 18(12): 6396–63911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Assady S, Boner G, Davidovits M, et al. Nephrology in Israel. In: Nephrology worldwide. Springer, 2021, pp. 329–343. [Google Scholar]
- 26.Ahn D, Williams S, Stankus N, et al. Advance care planning among African American patients on haemodialysis and their end-of-life care preferences. J Ren Care 2021; 47(4): 265–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arends SAM, Thodé M, De Veer AJE, et al. Nurses’ perspective on their involvement in decision-making about life-prolonging treatments: a quantitative survey study. J Adv Nurs 2022; 78(9): 2884–2893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nibbelink CW, Brewer BB. Decision-making in nursing practice: an integrative literature review. J Clin Nurs 2018; 27(5–6): 917–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weiner S. End-of-life care discussions: a survey of dialysis patients and professionals. J Pain Symptom Manag 2010; 39(2): 395–396. [Google Scholar]
- 30.Bos-van den Hoek DW, Thodé M, Jongerden IP, et al. The role of hospital nurses in shared decision-making about life-prolonging treatment: a qualitative interview study. J Adv Nurs 2021; 77(1): 296–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stoye A, Zimmer JM, Girndt M, et al. The role of different nephrology experts in informed shared decision-making for renal replacement therapy. J Ren Care 2022; 48(3): 177–184. [DOI] [PubMed] [Google Scholar]
- 32.Hoffmann TC, Légaré F, Simmons MB, et al. Shared decision making: what do clinicians need to know and why should they bother? Med J Aust 2014; 201(1): 35–39. [DOI] [PubMed] [Google Scholar]
- 33.Hanum C, Findyartini A. Interprofessional shared decision-making: a literature review. Jurnal Pendidikan Kedokteran Indonesia The Indonesian Journal of Medical Education 2020. 9(1): 81–94. [Google Scholar]
- 34.Schell JO, Cohen RA. A communication framework for dialysis decision-making for frail elderly patients. Clin J Am Soc Nephrol 2014; 9(11): 2014–2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moss AH. Revised dialysis clinical practice guideline promotes more informed decision-making. Clin J Am Soc Nephrol 2010; 5(12): 2380–2383. [DOI] [PubMed] [Google Scholar]
- 36.Engels N, De Graav G, Van Der Nat P, et al. Shared decision-making in advanced kidney disease: a scoping review protocol. BMJ Open 2020; 10(2): e034142–e034146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fung E, Slesnick N, Kurella Tamura M, et al. A survey of views and practice patterns of dialysis medical directors toward end-of-life decision making for patients with end-stage renal disease. Palliat Med 2016; 30(7): 653–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McCarter SP, Tariman JD, Spawn N, et al. Barriers and promoters to participation in the era of shared treatment decision-making. West J Nurs Res 2016; 38(10): 1282–1297. [DOI] [PubMed] [Google Scholar]
- 39.Haras MS. Planning for a good death: a neglected but essential part of ESRD care. Nephrol Nurs J 2008; 35(5): 451–458. [PubMed] [Google Scholar]
- 40.Ho TM, Barbero E, Hidalgo C, et al. Spanish nephrology nurses’ views and attitudes towards caring for dying patients. J Ren Care 2010; 36(1): 2–8. [DOI] [PubMed] [Google Scholar]
- 41.Montoya V. Advanced practice nurses and end-of-life care for patients with progressive chronic kidney disease and end stage renal disease. Nephrol Nurs J 2017; 44(3): 256–259. [PubMed] [Google Scholar]
- 42.Rosemeyer AK. The nurse’s role in end-of-life decision making for people on hemodialysis. Nephrol Nurs J 2008; 35(5): 513–514. [PubMed] [Google Scholar]
- 43.Csorba S. The role of a nurse specialist in palliative care: an israeli experience. Asia Pac J Oncol Nurs 2017; 4(2): 112–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fouché N, Bidii D, De Swardt C. An exploration of nephrology nurses’ experiences of caring for dying patients with end Stage Kidney Disease (ESKD) following withdrawal of dialysis – A South African perspective. International Journal of Africa Nursing Sciences 2022; 17(5): 100460. [Google Scholar]
- 45.Axelsson L, Benzein E, Lindberg J, et al. End-of-life and palliative care of patients on maintenance hemodialysis treatment: a focus group study. BMC Palliat Care 2019; 18(1): 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dönmez Ç, Yılmaz M, Helvacı İ. Opinions of nephrology nurses about death concept. Progress in Health Sciences 2015; 5(1): 63–68. [Google Scholar]
- 47.Ducharlet K, Philip J, Kiburg K, et al. Renal supportive care, palliative care and end-of-life care: Perceptions of similarities, differences and challenges across Australia and New Zealand. Nephrology 2021; 26(1): 15–22. [DOI] [PubMed] [Google Scholar]
- 48.Cheung KL, Schell JO, Rubin A, et al. Communication skills training for nurses and social workers: an initiative to promote interdisciplinary advance care planning and palliative care in patients on dialysis. Nephrol Nurs J 2021; 48(6): 547–552. [PMC free article] [PubMed] [Google Scholar]
- 49.Madar H, Gilad G, Elenhoren E, et al. Dialysis nurses for palliative care. J Ren Care 2007; 33(1): 35–38. [DOI] [PubMed] [Google Scholar]
- 50.Payongayong JV, Thomas-Hawkins C, Jarrín OF, et al. Effects of end-of-life communication knowledge, attitudes, and perceived behavioral control on end -of-life communication behaviors among nephrology nurse practitioners. Nephrol Nurs J 2022; 49(3): 213–225. [PubMed] [Google Scholar]
- 51.Hsu HC, Lin MH. The impact of an educational program on nurses’ shared decision making attitudes: a randomized controlled trial. Appl Nurs Res 2022; 65(1): 151587. [DOI] [PubMed] [Google Scholar]
- 52.Collett D, Feder S, Aaron E, et al. Palliative care advanced practice nursing in Israel: bridging creation and implementation. Int Nurs Rev 2020; 67(3): 136–144. [DOI] [PubMed] [Google Scholar]
- 53.Scheinberg-Andrews C, Ganz FD. Israeli nurses' palliative care knowledge, attitudes, behaviors, and practices. Oncol Nurs Forum 2020; 47(2): 213–221. [DOI] [PubMed] [Google Scholar]
- 54.Ami SB, Yaffe A. Palliative care in Israel: the nursing perspective. Journal of Palliative Medecine 2015; S5(1): 1–4. [Google Scholar]
- 55.Bentur N. Education programs and in-service training in palliative care in Israel-current Situation. 2017; RR-762-17: Myers-JDC-Brookdale Institute. (Hebrew).
- 56.de Barbieri I, Strini V, Noble H, et al. Nurse-perceived facilitators and barriers to palliative care in patients with kidney disease: a European Delphi survey. J Ren Care 2022; 48(1): 49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bublitz L, Fowler K, Fulkco D, et al. Narrative survey of renal nurses - An enquiry of challenging clinical situations with adults on haemodialysis approaching end of life. Renal Society of Australasia Journal 2017; 13(2): 65–70. [Google Scholar]
- 58.Maffoni M, Argentero P, Giorgi I, et al. Healthcare professionals’ moral distress in adult palliative care: a systematic review. BMJ Support Palliat Care 2019; 9(3): 245–254. [DOI] [PubMed] [Google Scholar]
- 59.Mullen SL. Experiences of nurses who provide advance care planning in the dialysis setting. {Doctoral dissertation}. Ann Arbor (US): Walden University, 2022. [Google Scholar]
- 60.Rego F, Sommovigo V, Setti I, et al. How supportive ethical relationships are negatively related to palliative care professionals negative affectivity and moral distress: a portuguese sample. Int J Environ Res Publ Health 2022; 19(7): 3863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Metzger M, Yoder J, Fitzgibbon K, et al. Nephrology and palliative care collaboration in the care of patients with advanced kidney disease: results of a clinician survey. Kidney Med 2021; 3(3): 368–377.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tariman JD, Szubski KL. The evolving role of the nurse during the cancer treatment decision-making process: a literature review. Clin J Oncol Nurs 2015; 19(5): 548–556. [DOI] [PubMed] [Google Scholar]
- 63.American Nephrology Nurses Association . Position statement nephrology nurse’s role in palliative and end-of-life care. Nephrol Nurs J 2018; 45(6): 549–613. [Google Scholar]
- 64.Zisman-Ilani Y, Roe D, Elwyn G, et al. Shared Decision Making for Psychiatric Rehabilitation Services Before Discharge from Psychiatric Hospitals. Health Commun 2019; 34(6): 631–637. [DOI] [PubMed] [Google Scholar]
- 65.Karnieli-Miller O, Karnieli E, Kroszynski GN. Enhancing patient centered care through understanding barriers and promotors to implementing shared decision process in diabetes. Israel: The Israel National Institute For Health Policy Research, 2020. [Google Scholar]
- 66.Medina-Artom TR, Adashi EY. Patient-centered care in Israeli IVF units: divergent perceptions of patients and providers. Isr J Health Pol Res 2020. 9(1): 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lipovetski O, Cojocaru D. Achieving patient-centered care with shared decision-making among colorectal cancer patients in Israel. Revista Cercetare si Interventie Socialia 2020; 70: 250–264. [Google Scholar]
- 68.Chen JO, Lin CC. Exploring the Barriers Faced by Nephrology Nurses in Initiating Patients With Chronic Kidney Disease Into Advance Care Planning Using Focus-Group Interviews. J Nurs Res 2021; 29(6): e179. [DOI] [PubMed] [Google Scholar]
- 69.Amir N, McCarthy HJ, Tong A. A working partnership: a review of shared decision-making in nephrology. Nephrology 2021; 26(11): 851–857. [DOI] [PubMed] [Google Scholar]
- 70.Hsiao CY, Wu JC, Lin PC, et al. Effectiveness of interprofessional shared decision-making training: a mixed-method study. Patient Educ Couns 2022; 105(11): 3287–3297. [DOI] [PubMed] [Google Scholar]
- 71.Sugizaki CSA, Rodrigues HCN, Ivo JFM, et al. The relationship between grip strength with health-related quality of life and mortality in hemodialysis patients. 2022; 47(21):21–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Luckett T, Spencer L, Morton RL, et al. Advance care planning in chronic kidney disease: a survey of current practice in Australia. Nephrology 2017; 22(2): 139–149. [DOI] [PubMed] [Google Scholar]
- 73.Verberne WR, Stiggelbout AM, Bos WJW, et al. Asking the right questions: towards a person-centered conception of shared decision-making regarding treatment of advanced chronic kidney disease in older patients. BMC Med Ethics 2022; 23(1): 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lenzen SA, Daniëls R, van Bokhoven MA, et al. What makes it so difficult for nurses to coach patients in shared decision making? A process evaluation. Int J Nurs Stud 2018; 80(1): 1–11. [DOI] [PubMed] [Google Scholar]
- 75.Elwyn G, Lloyd A, May C, et al. Collaborative deliberation: a model for patient care. Patient Educ Couns 2014; 97(2): 158–164. [DOI] [PubMed] [Google Scholar]
- 76.Lunney JR, Lynn J, Hogan C. Profiles of older medicare decedents. J Am Geriatr Soc 2002; 50(6): 1108–1112. [DOI] [PubMed] [Google Scholar]
- 77.Hong YA, Chung S, Park WY, et al. Nephrologists’ perspectives on decision making about life-sustaining treatment and palliative care at end of life: a questionnaire survey in Korea. J Palliat Med 2021; 24(4): 527–535. [DOI] [PubMed] [Google Scholar]