SUMMARY
OBJECTIVE:
Sudden cardiac death or arrest describes an unexpected cardiac cause-related death or arrest that occurs rapidly out of the hospital or in the emergency room. This study aimed to reveal the relationship between coronary angiographic findings and cardiac death secondary to acute ST-elevation myocardial infarction.
MATERIALS AND METHODS:
Patients presenting with acute ST-elevation myocardial infarction complicated with cardiac arrest were included in the study. The severity of coronary artery disease, coronary chronic total occlusion, coronary collateral circulation, and blood flow in the infarct-related artery were recorded. Patients were divided into two groups, namely, deaths secondary to cardiac arrest and survivors of cardiac arrest.
RESULTS:
A total of 161 cardiac deaths and 42 survivors of cardiac arrest were included. The most frequent (46.3%) location of the culprit lesion was on the proximal left anterior descending artery. The left-dominant coronary circulation was 59.1%. There was a difference in the SYNTAX score (16.3±3.8 vs. 13.6±1.9; p=0.03) and the presence of chronic total occlusion (19.2 vs. 0%; p=0.02) between survivors and cardiac deaths. A high SYNTAX score (OR: 0.38, 95%CI: 0.27–0.53, p<0.01) was determined as an independent predictor of death secondary to cardiac arrest.
CONCLUSION:
The chronic total occlusion presence and SYNTAX score may predict death after cardiac arrest secondary to ST-elevation myocardial infarction.
KEYWORDS: Sudden cardiac death, Survivors, Sudden cardiac arrest, Myocardial infarction
INTRODUCTION
Sudden cardiac death/sudden cardiac arrest refers to an unexpected death or arrest from a cardiovascular cause that occurs rapidly out of the hospital or in the emergency room 1 . The presumption based on epidemiologic studies is that the most common cardiac pathology underlying all sudden cardiac deaths is attributable to coronary heart disease 2 . Ventricular tachycardia and ventricular fibrillation are the most frequent in the first hours of an infarction 3 . Ventricular tachycardia or ventricular fibrillation accounts for the majority of episodes. However, bradyarrhythmia is responsible for some cases of sudden cardiac death/sudden cardiac arrest 4 . The largest experience with acute ST-elevation myocardial infarction (MI) comes from the GUSTO-1 trial of 40,895 patients who were treated with thrombolytic therapy 5 . The overall incidence of ventricular tachycardia or ventricular fibrillation was 10.2%. Approximately 80–85% of these arrhythmias occurred in the first 48 h. These data do not include patients with SCD who do not survive until hospitalization. It has been estimated that more than 50% of deaths due to acute myocardial infarcts occur out of the hospital, and most episodes occur within 1 h of symptom onset 6 .
The aim of this study was to identify the coronary anatomy of patients with acute ST-elevation MIs complicated by sudden cardiac death or sudden cardiac arrest. More specifically, we studied the differences between sudden cardiac death and survivors of sudden cardiac arrest.
METHODS
Patients presented with acute anterior and inferior myocardial infarction between January 2013 and March 2024 were examined. Patients with out-of-hospital cardiac arrest or in-hospital cardiac arrest were included in the study. Coronary angiography and primary angioplasty were performed as treatment immediately after the patient arrived at the hospital. Right and left coronary angiograms were obtained in multiple projections. None of the patients received fibrinolytics. Two experienced cardiologists who were blinded to angiographic data interpreted all coronary angiographies recorded upon admission. The principal angiographic and clinical data were entered into a database. The reduction in luminal diameter was visually estimated to be due to graded coronary stenoses.
The lesion was considered the culprit if it was a fresh occlusion at angiography. Epicardial blood flow in the infarct-related artery was graded according to the thrombolysis in myocardial infarction (TIMI) group definitions 7 . The occlusion was classified as acute if angiography showed a thrombus at the location of the occlusion or if a guide wire was able to pass through the occlusion easily. If there was no acute occlusion, the lesion with the most severe reduction was assigned as the culprit if lesion localization corresponded with the location of ST segment elevations.
The coronary arteries were divided into proximal, mid, and distal segments. The severity of coronary artery disease was scored using the SYNTAX score I 8 . Coronary chronic total occlusion was defined as an occluded coronary artery with TIMI 0 flow for at least 3 months. The Rentrop-Cohen method was used to categorize coronary collateral circulation 9 .
Patients with known heart failure and coronary artery disease (coronary angioplasty and previous MI), left bundle branch block, Brugada syndrome, QT prolongation, congenital short QT syndrome, Wolff-Parkinson-White syndrome, familial polymorphic VT, and sudden unexplained death were not included in the study.
Statistical analysis
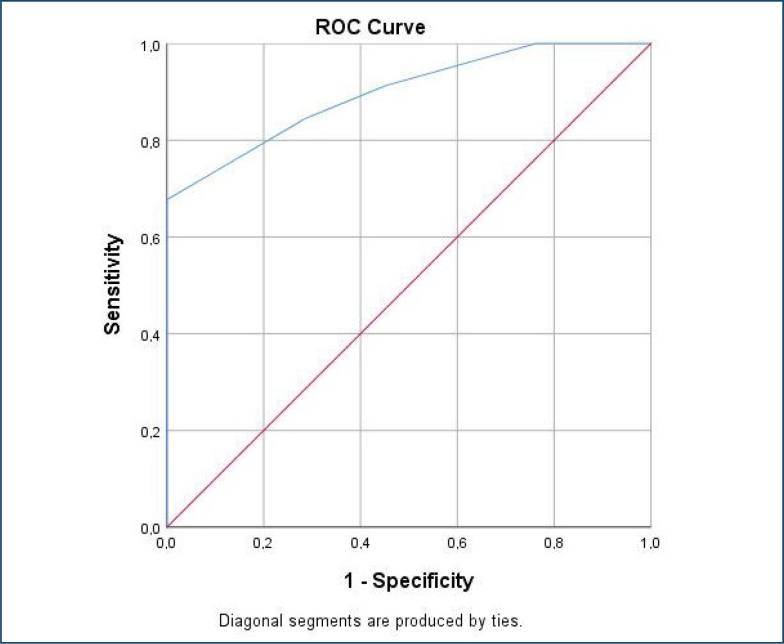
Descriptive statistics for baseline parameters of continuous variables with a normal distribution were presented as mean±standard deviation. Qualitative variables were presented as numbers and percentages. The significance of differences in the means of continuous variables was evaluated using the Student's t-test. Categorical variables were compared using the chi-square test or Fisher's exact test as appropriate. Univariate logistic regression analysis was used to determine the independent predictor of mortality after cardiac arrest. The sensitivity and specificity of the SYNTAX score 1 to predict death were analyzed by receiver operating characteristics (ROC) analysis. A p-value below 0.05 was considered statistically significant. All tests were performed using the SPSS 22.0 (SPSS Inc., Chicago, IL) software version.
RESULTS
A total of 302 sudden cardiac arrests were examined. After exclusion criteria, 203 arrests associated with ST-elevation MI were included in the study. A total of 161 deaths occurred within 1 h after the angiogram. Notably, 42 patients were included in the survivors group. Demographic data on deaths and survivors are summarized in Table 1. The time from symptom onset to collapse in patients with ventricular fibrillation and out-of-hospital cardiac arrest secondary to acute coronary syndrome is unknown. The median time between collapse and angiogram was 22.5±11.2 min after in-hospital cardiac arrest. Anterior localization was statistically more frequent in all cardiac arrests secondary to acute coronary events (68.5 vs. 31.5%; p=0.05).
Table 1. Baseline characteristics of the study patients.
| Variables | Deaths secondary to cardiac arrest (n=161) | Survivors of cardiac arrest (n=42) | All cardiac arrests (n=203) |
p-value | |
|---|---|---|---|---|---|
| Age | 71.5±11 | 73.5±8 | 71.9±10.5 | 0.27 | |
| Male | 78 (48.4) | 12 (28.6) | 90 (44.3) | 0.021 | |
| Smoking | 90 (55.9) | 20 (47.6) | 110 (54.2) | 0.603 | |
| Hypertension | 29 (18) | 7 (16.6) | 36 (17.7) | 0.940 | |
| Alcohol intake | 87 (54.0) | 19 (45.2) | 106 (52.2) | 0.459 | |
| Obesity | 103 (64) | 23 (56.1) | 126 (62) | 0.295 | |
| LVEF (%) | 34.9±10.3 | 38.2±7.7 | 35.6±9.9 | 0.086 | |
| ST-segment elevation | |||||
| Anterior | 109 (67.7) | 30 (71.4) | 139 (68.5) | 0.643 | |
| Non-anterior | 52 (32.3) | 12 (28.6) | 64 (31.5) | 0.643 | |
| Complaints at first arrival | |||||
| Chest pain | 17 (10.6) | 33 (78.6) | 50 (24.6) | <0.01 | |
| Cardiac arrest* | 144 (89.4) | 9 (21.4) | 153 (75.4) | <0.01 | |
LVEF: left ventricular ejection fraction.
Patients with ventricular fibrillation out-of-hospital cardiac arrest secondary to acute coronary syndrome.
Bold indicates significant values (p<0.05).
Angiographic data are summarized in Table 2. The infarct-related artery in all cardiac arrests was LAD, RCA, or CX in 63.1, 29.6, and 7.4%, respectively. The most frequent (46.3%) location of the culprit lesion was in the proximal LAD, followed by the proximal RCA (25.1%). Considering coronary dominance in all cardiac arrest cases, 59.1% left-dominant, 21.2% right-dominant, and 19.7% co-dominants were detected. Flow in the infarct artery was absent or severely decreased in 74.9% of all cardiac arrests. Rentrop grade 2–3 collaterals to the infarct-related coronary artery were present in 21.2% of the patients. There were no differences between the two groups concerning the location of the culprit along the coronary arteries, the presence or absence of collaterals to the infarct artery, and coronary dominancy. Left ventricular ejection fraction (LVEF) was 34.9±10.3% in deaths and 38.2±7.7% in survivors (p=0.086).
Table 2. Coronary angiography results of the patients.
| Variables | Deaths secondary to cardiac arrest (n=161) | Survivors of cardiac arrest (n=42) | All cardiac arrests (n=203) | p-value | |
|---|---|---|---|---|---|
| Location of culprit lesion on LAD | 103 (64) | 25 (59.5) | 128 (63.1) | 0.877 | |
| Location of culprit lesion on RCA | 46 (28.6) | 14 (33.3) | 60 (29.6) | 0.877 | |
| Location of culprit lesion on CX | 12 (7.5) | 3 (7.1) | 15 (7.4) | 0.877 | |
| Coronary dominancy | |||||
| Left | 94 (58.4) | 26 (61.9) | 120 (59.1) | 0.475 | |
| Right | 37 (23) | 6 (14.3) | 43 (21.2) | ||
| Codominancy | 30 (18.6) | 10 (23.8) | 40 (19.7) | ||
| Chronic total occlusion other than IRA | 31 (19.2) | 0 | 31 (15.2) | 0.033 | |
| LAD | 24 (14.9) | 0 | 24 (11.8) | ||
| RCA | 7 (4.3) | 0 | 7 (3.4) | ||
| CX | 6 (3.7) | 0 | 6 (2.9) | ||
| SYNTAX score | 16.7±3.5 | 12.1±1.7 | 15.8±3.7 | 0.031 | |
| TIMI-flow grade | |||||
| 0–1 | 125 (77.6) | 27 (64.3) | 152 (74.9) | 0.084 | |
| 2–3 | 36 (22.4) | 15 (35.7) | 51 (25.1) | ||
| Collaterals to IRA* | |||||
| 0–1 | 129 (80.1) | 31 (73.8) | 160 (78.8) | 0.372 | |
| 2–3 | 32 (19.9) | 11 (26.2) | 43 (21.2) | ||
CX: circumflex artery; LAD: left anterior descending artery; IRA: infarct-related artery; RCA: right coronary artery; SYNTAX: SYNergy between PCI with TAXUS and Cardiac Surgery; TIMI: thrombolysis in myocardial infarction.
Six patients had two chronic occlusions.
Bold indicates significant values (p<0.05).
Between survivors and deaths, there was a difference in the SYNTAX score and the presence of chronic total occlusion. Of all cardiac arrests, 31 (15.2%) had chronic occlusions in a non-infarct related coronary artery. All of the patients with chronic occlusion died within 1 h after coronary angiography, secondary to acute coronary events. On the contrary, in the survivor group, chronic total occlusion was not found (19.2 vs. 0%; p=0.02). It was found that the SYNTAX score was higher in the death group (16.3±3.8 vs. 13.6±1.9; p=0.03). The receiver operating characteristic (ROC) curve was used to test the accuracy of the SYNTAX score in the prediction of deaths secondary to acute coronary events. The optimal SYNTAX score cut-off value of 13.5 provided the highest sensitivity (84.5%) and specificity (71.4%) for predicting death. The area under the curve for the SYNTAX score was 0.898 (p<0.01) (Figure 1). A high SYNTAX score (OR: 0.38, 95%CI: 0.27–0.53, p<0.01) was determined as an independent predictor of mortality after cardiac arrest.
Figure 1. Determination of SYNTAX score cut-off value for predicting death.
The mortality rate in patients with out-of-hospital VF was 89.4%. The mortality rate was found to be 10.6% in patients who presented with a complaint of chest pain (in-hospital cardiac arrest).
DISCUSSION
According to our study results, the presence of chronic total occlusion and a higher SYNTAX score may be predictive of mortality after cardiac arrest secondary to ST-elevation MI. Additionally, the mortality rate in out-of-hospital VF was found to be higher than in-hospital cardiac arrest. Our finding is the increased risk of mortality with acute occlusion in the proximal LAD when compared with acute occlusion of the RCA or CX. The size of the infarct is correlated with early VF in large studies of patients hospitalized for AMI. Proximal LAD occlusion, which is associated with a large amount of myocardium, has a larger region at risk of necrosis 10 . However, it defies previous theories that acute RCA occlusions, which typically supply the conduction system, are more likely to result in potentially fatal arrhythmias 11 . Previous studies found associations between early VF and IRAs inconsistent, but some either included few or no patients with out-of-hospital VF or had no angiographic data. Other studies did not specifically address out-of-hospital VF secondary to ST-elevation MI and possibly included a heterogeneous group of patients with cardiac arrest 12 . In addition, a hypothesis, generated by previous studies, is that vagal tone in patients with acute occlusion of RCA protects against early VF during AMI. The cause of the vagotonia appears to be stimulation of cardiac vagal afferent receptors common in the inferoposterior of the left ventricle 13 .
One of our study findings is the presence of an association between mortality and the extent of coronary artery disease. The SYNTAX score was significantly higher in deaths secondary to acute coronary events. Our results conflict with autopsy data from patients who experienced an out-of-hospital cardiac arrest, where the degree of CAD was not substantially different from that of patients who had stable angina or a prior infarction 14 . This discrepancy could be explained by the different autopsy methods used to characterize the degree of CAD. According to Kyriakidis et al., there is a correlation between the Gensini score, which measures the extent of CAD, and in-hospital primary VF 15 .
Coronary dominance is defined based on the vascular supply of the posterior interventricular septum. When the interventricular septum is supplied by the posterior descending branch of the left circumflex artery, it is a left-dominant circulation. Left-dominant circulation is reported to be present in 2–10.1% of the general population 16 . However, we found the left dominance rate to be 59.1%. Several studies have attempted to determine the effect of coronary dominance on mortality as an outcome in patients with acute coronary syndrome. Observational data suggest that left-dominant circulation may be a risk factor for adverse outcomes 17 . Considering that our study population was sudden cardiac death or sudden cardiac arrest survivors, unlike the general population, and the left dominance was detected as more common, it can be thought that our study results support the previous studies.
In our study, mortality was found to be 89.4% in patients with cardiac arrest at the first admission to the hospital. Factors such as the time to reach the patient, the time to arrive at the hospital, and resuscitation experience determine mortality. Mortality among patients who collapse in an unmonitored setting correlates with the duration of the arrest 18 .
Limitations
The study was somewhat limited by the small number of patients. Victims in whom resuscitation was unsuccessful may have had a different coronary anatomy from those who were successfully revived. Lack of knowledge about preexisting LVEF is one of the study limitations. These data are only accessible through prospective study designs, which are highly difficult to perform. Some risk factors that may be different between the two groups (sleep apnea syndrome, regular physical activity, depression, anxiety, psychological stress, and caffeine intake) were not recorded.
CONCLUSION
According to our data obtained by acute angiography, LAD proximal lesions were the most common location in sudden cardiac arrest and sudden cardiac death secondary to ST-elevation MI. The presence of a chronic occlusion in a non-infarct-related artery or a higher SYNTAX score is possibly an additional independent determinant of mortality after a cardiac arrest.
Footnotes
Funding: none.
REFERENCES
- 1.Andersen LW, Holmberg MJ, Berg KM, Donnino MW, Granfeldt A. In-hospital cardiac arrest: a review. JAMA. 2019;321(12):1200–1210. doi: 10.1001/jama.2019.1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Razavi AC, Whelton SP, Blumenthal RS, Sperling LS, Blaha MJ, Dzaye O. Coronary artery calcium and sudden cardiac death: current evidence and future directions. Curr Opin Cardiol. 2023;38(6):509–514. doi: 10.1097/HCO.0000000000001081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khederlou H, Azimi Pirsaraei SV, Rabbani E, Motedayen M. Correlations between cardiovascular risk factors and ventricular arrhythmias following primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction. J Tehran Heart Cent. 2023;18(2):122–128. doi: 10.18502/jthc.v18i2.13322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strasburger JF, Eckstein G, Butler M, Noffke P, Wacker-Gussmann A. Fetal arrhythmia diagnosis and pharmacologic management. J Clin Pharmacol. 2022;62(Suppl 1):S53–S66. doi: 10.1002/jcph.2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strasburger JF, Eckstein G, Butler M, Noffke P, Wacker-Gussmann A. Fetal arrhythmia diagnosis and pharmacologic management. J Clin Pharmacol. 2022;62(Suppl 1):S53–S66. doi: 10.1002/jcph.2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krahn AD, Tfelt-Hansen J, Tadros R, Steinberg C, Semsarian C, Han HC. Latent causes of sudden cardiac arrest. JACC Clin Electrophysiol. 2022;8(6):806–821. doi: 10.1016/j.jacep.2021.12.014. [DOI] [PubMed] [Google Scholar]
- 7.Sabatine MS, Braunwald E. Thrombolysis in myocardial infarction (TIMI) study group: JACC focus seminar 2/8. J Am Coll Cardiol. 2021;77(22):2822–2845. doi: 10.1016/j.jacc.2021.01.060. [DOI] [PubMed] [Google Scholar]
- 8.Serruys PW, Revaiah PC, Ninomiya K, Masuda S, Kotoku N, Kageyama S, et al. 10 years of SYNTAX: closing an era of clinical research after identifying new outcome determinants. JACC Asia. 2023;3(3):409–430. doi: 10.1016/j.jacasi.2023.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Freund A, Stiermaier T, Waha-Thiele S, Eitel I, Schock S, Lurz P, et al. Coronary collaterals in patients with ST-elevation myocardial infarction presenting late after symptom onset. Clin Res Cardiol. 2020;109(10):1307–1315. doi: 10.1007/s00392-020-01625-w. [DOI] [PubMed] [Google Scholar]
- 10.Brener SJ, Witzenbichler B, Maehara A, Dizon J, Fahy M, El-Omar M, et al. Infarct size and mortality in patients with proximal versus mid left anterior descending artery occlusion: the intracoronary abciximab and aspiration thrombectomy in patients with large anterior myocardial infarction (INFUSE-AMI) trial. Am Heart J. 2013;166(1):64–70. doi: 10.1016/j.ahj.2013.03.029. [DOI] [PubMed] [Google Scholar]
- 11.Loughlin MJ, Diego JM. Right ventricle injury in RCA occlusion: exploration using precordial bipolar leads and surrogate vectorcardiograms. J Electrocardiol. 2023;79:89–96. doi: 10.1016/j.jelectrocard.2023.03.012. [DOI] [PubMed] [Google Scholar]
- 12.Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–1487. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 13.Mark AL. The Bezold-Jarisch reflex revisited: clinical implications of inhibitory reflexes originating in the heart. J Am Coll Cardiol. 1983;1(1):90–102. doi: 10.1016/s0735-1097(83)80014-x. [DOI] [PubMed] [Google Scholar]
- 14.Davies MJ. Anatomic features in victims of sudden coronary death. Coronary artery pathology. Circulation. 1992;85(1 Suppl):I19–I24. [PubMed] [Google Scholar]
- 15.Kyriakidis M, Petropoulakis P, Antonopoulos A, Barbetseas J, Georgiakodis F, Aspiotis N, et al. Early ventricular fibrillation in patients with acute myocardial infarction: correlation with coronary angiographic findings. Eur Heart J. 1993;14(3):364–368. doi: 10.1093/eurheartj/14.3.364. [DOI] [PubMed] [Google Scholar]
- 16.Ihdayhid AR, Goeller M, Dey D, Nerlekar N, Yap G, Thakur U, et al. Comparison of coronary atherosclerotic plaque burden and composition as assessed on coronary computed tomography angiography in east asian and european-origin caucasians. Am J Cardiol. 2019;124(7):1012–1019. doi: 10.1016/j.amjcard.2019.06.020. [DOI] [PubMed] [Google Scholar]
- 17.Veltman CE, Hoeven BL, Hoogslag GE, Boden H, Kharbanda RK, Graaf MA, et al. Influence of coronary vessel dominance on short- and long-term outcome in patients after ST-segment elevation myocardial infarction. Eur Heart J. 2015;36(17):1023–1030. doi: 10.1093/eurheartj/ehu236. [DOI] [PubMed] [Google Scholar]
- 18.McGuigan PJ, Edwards J, Blackwood B, Dark P, Doidge JC, Harrison DA, et al. The association between time of in hospital cardiac arrest and mortality; a retrospective analysis of two UK databases. Resuscitation. 2023;186:109750–109750. doi: 10.1016/j.resuscitation.2023.109750. [DOI] [PubMed] [Google Scholar]