ABSTRACT
COVID-19 vaccination effectively reduces disease severity, hospitalization, and mortality, particularly among individuals with chronic conditions who bear a disproportionate burden of disease complications. Vaccine confidence – belief in its safety, effectiveness, and importance – boosts uptake. However, limited data on vaccine confidence in this population hinders the development of targeted interventions. This study examined COVID-19 vaccine confidence and its impact on uptake among individuals with hypertension or diabetes mellitus in the Kilimanjaro region, Tanzania. A community-based cross-sectional study was conducted in March 2023 among 646 randomly selected adults aged ≥18 years with hypertension or diabetes mellitus in three districts of Kilimanjaro region, northern Tanzania. An interviewer-administered electronic questionnaire assessed confidence and uptake of COVID-19 vaccines in addition to related knowledge and demographic characteristics. Data analysis was done for 646 individuals who consented to participate. Multivariable logistic regression models determined the factors associated with COVID-19 vaccine confidence and its effect on vaccine uptake. The proportion of COVID-19 vaccine confidence among all 646 participants was 70% and was highest for perceived vaccine importance (80%), followed by perceived vaccine effectiveness (77%) and perceived vaccine safety (74%). Good knowledge of COVID-19 vaccines and living in the Mwanga municipal council (MC), a semi-urban district, was independently associated with confidence in the vaccines’ importance, safety, effectiveness, and overall COVID-19 vaccine confidence. Confidence in COVID-19 vaccines increased the odds of vaccine uptake. Targeted interventions to boost vaccine confidence are therefore essential to enhance vaccine uptake in this high-risk population.
KEYWORDS: COVID-19, vaccination, vaccine acceptance, vaccine confidence, vaccine hesitancy, Tanzania
Introduction
COVID-19 was a public health emergency of international concern that has caused over 700 million cases and over 6 million deaths globally.1 People with chronic illnesses are particularly at increased risk of complications from the disease including severe illness, hospitalization, and death.2 For this reason, they were prioritized to receive COVID-19 vaccines. In Tanzania, COVID-19 vaccines were first prioritized among people with chronic illnesses apart from the elderly and healthcare workers, before expanding the eligibility to all adult population aged ≥18 years.3 COVID-19 vaccines prevent severe illness and death from COVID-19 disease.4 Vaccine hesitancy, however, has been a major setback in COVID-19 vaccination acceptance and uptake both in the general population and among people with chronic conditions.5,6
The World Health Organization (WHO) defines vaccine hesitancy as “delay in acceptance or refusal of vaccines despite availability of vaccination services.”7 Vaccine confidence is one of the key drivers of vaccine hesitancy apart from convenience (availability, affordability, and accessibility) and complacency (perceived necessity of vaccines).8 The WHO has also defined vaccine confidence as “trust in the effectiveness and safety of vaccines; the system that delivers them, including the reliability and competence of the health services and health professionals and the motivations of policy-makers who decide on the needed vaccines.”8 Vaccine confidence through the Vaccine Confidence Project (VCP) has been mapped globally across populations using a Vaccine Confidence Index (VCI) before the COVID-19 pandemic.9 The index examines an individual’s perception of vaccine safety, effectiveness, importance, and religious compatibility to assess vaccine confidence.10
Low confidence in COVID-19 vaccine safety, importance, and effectiveness is among the top reasons for COVID-19 vaccine hesitancy and low uptake not only in the general population,5,11–14 but also among people with chronic illnesses.6,15,16 A previous study on COVID-10 vaccine uptake among people with underlying chronic medical conditions in the districts of Columbia found that while some had high confidence in vaccine importance due to their underlying medical condition, others had concerns that the vaccines may aggravate their underlying medical condition.17
Furthermore, available evidence shows that low COVID-19 vaccine confidence from concerns of vaccine safety,5,14,18,19 less confidence in vaccine importance to protect others and themselves,6,18,19 and low trust in the vaccine development and approval,11,19 were strongly associated with low vaccine acceptance among adults in the general population5,11,20 and healthcare workers.18,21 Conversely, high confidence in vaccines’ importance to protect oneself,6,12 and high confidence in vaccine safety and effectiveness14 were strongly associated with high vaccine acceptance and uptake among adults in the general population12,20 and people with underlying chronic medical conditions.6
The first case of COVID-19 in Tanzania was confirmed at Kilimanjaro International Airport in Kilimanjaro region on the 13th of March 2020, 2 months after the WHO declared it as a Public Health Emergency of International Concern (PHEIC).22 This resulted in a panic that was exacerbated by the spread of misinformation not only in the region but also throughout the country. COVID-19 vaccines were first introduced in Tanzania in July 2021 and were prioritized for people with chronic conditions like hypertension and diabetes mellitus due to their increased risk of morbidity and mortality from COVID-19. Currently, more than 13 billion COVID-19 vaccine doses have been administered globally, and more than 39 million doses in Tanzania.23 Despite vaccination strategies such as mass education campaigns and community engagement, COVID-19 vaccination coverage remains low in Tanzania (51%) perhaps due to initial government denial of the vaccines hence causing vaccine hesitancy.24,25
To date, evidence is scarce on drivers of COVID-19 vaccine confidence among people with chronic illnesses including people with hypertension or diabetes mellitus. This study therefore assessed factors associated with COVID-19 vaccine confidence among people with hypertension or diabetes mellitus in the Kilimanjaro region of Tanzania. It also quantified the effect of COVID-19 confidence on COVID-19 vaccine uptake in this population.
Methodology
Study design, setting, and population
We conducted a community-based cross-sectional study in March 2023 in three districts; Moshi Municipal Council (MC), Moshi District Council (DC), and Mwanga Municipal Council (MC) of Kilimanjaro region, northern Tanzania. We included adults aged ≥18 years who had either hypertension or diabetes mellitus. Participant’s diabetes and/or hypertensive status was self-reported and further validated using their clinic cards and current use of diabetes or anti-hypertensive medications. Kilimanjaro region was purposefully selected because it was the first region to have reported an imported COVID-19 case early in the pandemic, hence massively impacted.22 The three districts were randomly selected with consideration of urban and rural representation. Wards were further randomly selected from each district taking into consideration their population weight. Participating villages/streets were then randomly selected from each ward. Hamlets were then randomly selected from each village. A list of households with people who met the inclusion criteria was provided by a community health worker from each hamlet. The sample size was estimated using a single proportion formula N=[(Zα/2)2 × p(1-p)]/ε2 where the proportion of COVID-19 vaccine hesitancy among people with diabetes was 26% from a previous study.26 Taking a standard normal value of 1.96 corresponding to a 95% confidence level, a standard error of 3.5%, and assuming a non-response rate of 10%, we obtained a minimum sample size of 663 individuals.
Variables
Confidence in COVID-19 vaccine safety, effectiveness, importance, and overall COVID-19 vaccine confidence were the primary dependent variables. We adopted the Vaccine Confidence Index (VCI) that was developed in 2015 by the Vaccine Confidence Project. It uses standardized methodology to map individual’s perception on vaccine importance, safety, effectiveness, and compatibility with people’s beliefs; all of which entails vaccine confidence.9 Participants were asked to rate their responses to three questions regarding their perception of COVID-19 vaccine importance, safety, and effectiveness. Responses to the three questions ‘COVID-19 vaccines are important,’ ‘COVID-19 vaccines are safe,’ and ‘COVID-19 vaccines are effective’ were coded in a Likert scale from ‘Strongly agree,’ ‘Agree,’ ‘I don’t know,’ ‘Disagree,’ and ‘Strongly disagree.’ A response of ‘Strongly agree’ and ‘Agree’ to either of the questions was regarded as having confidence in either and no confidence if otherwise. The confidence variables in COVID-19 vaccine importance, safety, and effectiveness were further used to derive the overall COVID-19 vaccine confidence. Participants were considered to have overall COVID-19 vaccine confidence if they had confidence in COVID-19 vaccine importance, safety, and effectiveness (all three components) and no overall COVID-19 vaccine confidence if otherwise. COVID-19 uptake (secondary dependent variable) was examined based on its association with confidence in vaccine safety, effectiveness, importance, and overall COVID-19 vaccine confidence. Details on how COVID-19 vaccine uptake was derived have been published elsewhere20 and this was further validated using records from vaccination cards.
The independent variables included COVID-19 vaccine knowledge and participant demographic characteristics including; age in years and categories (<50, 50–59, 60–69, 70 and above), sex (male and female), district of residence (Moshi MC, Moshi DC, Mwanga MC), bank account ownership, marital status, level of education, and health insurance ownership. Bank account ownership was used as a proxy for socioeconomic status. Details on how COVID-19 vaccine knowledge was derived have been published elsewhere.20 Participants were also asked about their history of COVID-19 infection.
Data management and analysis
Data management and analysis were done using STATA version 18. Categorical variables were summarized using absolute numbers and percentages, while measures of central tendencies and their respective measures of dispersion summarized continuous variables. Independent variables were cross-tabulated against COVID-19 importance, safety, effectiveness, and overall COVID-19 vaccine confidence and vaccine uptake and the Chi-squared test was used to assess their association for which a p-value of less than 0.05 was considered statistically significant. Multivariable logistic regression was used to estimate odds ratios and their 95% confidence intervals (CI) using a manual stepwise regression approach (at an alpha level of 0.1) for the factors associated with COVID-19 importance, safety, effectiveness, and overall COVID-19 vaccine confidence and their effect on COVID-19 vaccine uptake. Age and sex were specified a priori as confounders for the effect of perceived confidence in COVID-19 vaccines and the effect on COVID-19 vaccine uptake. For this analysis, none of the potential confounders apart from COVID-19 vaccine knowledge produced at least a 10% change in the odds ratio, and therefore all models were adjusted for age, sex, and COVID-19 vaccine knowledge.
Results
Participant characteristics
Data were analyzed for 646 participants. More than three-quarters of all participants (78.3%) were females and about a third (30.2%) were aged >70 years with the median (interquartile range, IQR) being 62 (54, 72) years. About three-quarters, (73.2%) attained primary education level. Fewer than half of the participants (42.6%) had good knowledge of COVID-19 vaccines and just over half (52.2%) had taken the COVID-19 vaccines (Table 1). About two-thirds (62%) of participants had taken the Johnson & Johnson vaccine, followed by Sinopharm (16.1%) and a lower proportion of participants had taken Pfizer, Moderna, AstraZeneca, Sinovac (data not shown in the table).
Table 1.
Background characteristics of individuals with diabetes mellitus and hypertension in Kilimanjaro region, Tanzania (N = 646).
| Variables | Frequency | Percent |
|---|---|---|
| Age (years) | ||
| Median (IQR) | 62 (54-72) | |
| <50 | 100 | 15.5 |
| 50-59 | 181 | 28.0 |
| 60-69 | 170 | 26.3 |
| 70+ | 195 | 30.2 |
| Sex | ||
| Male | 140 | 21.7 |
| Female | 506 | 78.3 |
| Education | ||
| None | 81 | 12.5 |
| Primary education | 473 | 73.2 |
| Secondary or above | 92 | 14.2 |
| District | ||
| Moshi MC | 217 | 33.6 |
| Moshi DC | 174 | 26.9 |
| Mwanga MC | 255 | 39.5 |
| Marital status1 | ||
| In union | 364 | 56.4 |
| Not in union | 282 | 43.7 |
| Religion | ||
| Muslim | 317 | 49.1 |
| Christian | 320 | 49.5 |
| Others | 9 | 1.4 |
| Health insurance | ||
| No | 435 | 67.3 |
| Yes | 211 | 32.7 |
| Bank account | ||
| No | 537 | 83.1 |
| Yes | 109 | 16.9 |
| Ever being infected with COVID-19 | ||
| No | 612 | 94.7 |
| Yes | 34 | 5.3 |
| COVID-19 risk perception | ||
| Not at risk | 394 | 61.0 |
| At risk | 252 | 39.0 |
| COVID-19 vaccine knowledge2 | ||
| Poor knowledge | 371 | 57.4 |
| Good knowledge | 275 | 42.6 |
| COVID-19 vaccine uptake2 | ||
| No | 307 | 47.5 |
| Yes | 339 | 52.5 |
1In union meant married/cohabiting and not in union included being single/separated/divorced/widow/widower.
2Details on how COVID-19 vaccine knowledge and uptake were measured have been published elsewhere.20
COVID-19 vaccine confidence
Seventy percent of the participants had overall COVID-19 vaccine confidence, i.e., combined perceived confidence in COVID-19 vaccines’ safety, effectiveness, and importance. Of the 646 individuals, 80% had confidence in vaccine importance, 77% had confidence in vaccine effectiveness, and 74% had confidence in vaccine safety (Figure 1).
Figure 1.
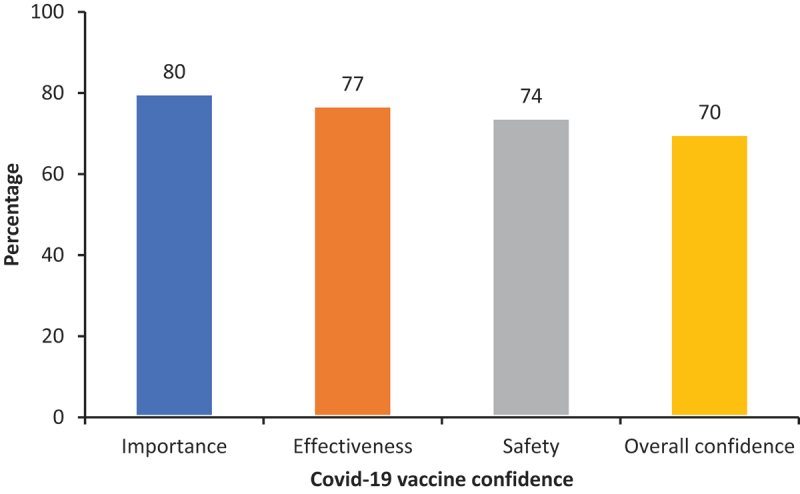
COVID-19 vaccine confidence among individuals with hypertension or diabetes mellitus in Kilimanjaro region, Tanzania.
Table 2 summarizes the association between participants’ characteristics and the overall COVID-19 vaccine confidence using Chi-square test. There was a significant difference in the proportion of participants who had overall COVID-19 vaccine confidence across categories of COVID-19 vaccine knowledge, COVID-19 risk perception, marital status, education, district, and owning a bank account. A higher proportion of participants who had overall COVID-19 vaccine confidence had good COVID-19 knowledge (90.6%) vs to those with poor knowledge (55.3%), perceived themselves as at risk of getting COVID-19 (74.6%) vs to their counterparts (67.5%), were in union, i.e., married or cohabiting (74.2%) than those who were not in union (separated, divorced, widows and widowers) (65.3%), had attained secondary education and above (82.6%) than those in primary education (71.7%) and no education (48.2%) and owned a bank account (82.6%) than those who do not (67.8%) (Table 2). The distribution of participants’ characteristics across other components of confidence, i.e., perceived importance, safety, and effectiveness are given in the Supplementary file.
Table 2.
COVID-19 vaccine confidence among by participants’ characteristics among individuals with hypertension or diabetes mellitus in Kilimanjaro region, Tanzania (N = 646).
| Variable | Participants (n) | Overall COVID-19 vaccine confidence (%) | P value |
|---|---|---|---|
| Age (years) | .004 | ||
| <50 | 100 | 72 (72.0) | |
| 50-59 | 181 | 137 (75.7) | |
| 60-69 | 170 | 127 (74.7) | |
| 70+ | 195 | 118 (60.5) | |
| Sex | .59 | ||
| Male | 140 | 101 (72.1) | |
| Female | 506 | 353 (69.8) | |
| Education | <.001 | ||
| None | 81 | 39 (48.2) | |
| Primary Education | 473 | 339 (71.7) | |
| Secondary and above | 92 | 76 (82.6) | |
| District | .03 | ||
| Moshi MC | 217 | 145 (66.8) | |
| Moshi DC | 174 | 115 (66.1) | |
| Mwanga MC | 255 | 194 (76.1) | |
| Marital status1 | .01 | ||
| In union | 364 | 270 (74.2) | |
| Not in union | 282 | 184 (65.3) | |
| Have bank account | .002 | ||
| No | 537 | 364 (67.8) | |
| Yes | 109 | 90 (82.6) | |
| Religion | .44 | ||
| Muslim | 317 | 224 (70.7) | |
| Christian | 320 | 222 (69.4) | |
| Others | 9 | 8 (88.9) | |
| Covid-19 risk perception | .05 | ||
| Not at risk | 394 | 266 (67.5) | |
| At risk | 252 | 188 (74.6) | |
| Ever infected with COVID-19 disease | .23 | ||
| No | 612 | 427 (69.8) | |
| Yes | 34 | 27 (79.4) | |
| COVID-19 vaccine knowledge2 | <.001 | ||
| Poor knowledge | 371 | 205 (55.3) | |
| Good Knowledge | 275 | 249 (90.6) |
1In union is being married or cohabiting. Not in union includes being single/divorced/separated/widow/widower.
2Details on how COVID-19 vaccine knowledge was measured have been published elsewhere.20
Factors associated with COVID-19 vaccine confidence
In the multivariable analysis, the district of residence and knowledge of COVID-19 vaccines significantly predicted confidence in vaccines’ importance, safety, effectiveness, and overall COVID-19 vaccine confidence. Compared to participants living in the Moshi municipality (an urban district in the region), participants living in Mwanga MC (semi-urban district) had significantly higher odds of having confidence in vaccines’ importance (OR 2.13, 95% CI 1.26–3.59), safety (OR 1.67, 95% CI 1.04–2.67), effectiveness (OR 1.94, 95% CI 1.18–3.18) and overall COVID-19 vaccine confidence (OR 2.01, 95% CI 1.27–3.19). Good knowledge of COVID-19 vaccines was strongly associated with higher odds of confidence in vaccines’ importance (OR 11.41, 95% CI 5.75–22.65), safety (OR 6.76, 95% CI 4.09–11.16), effectiveness (OR 8.30, 95% CI 4.71–14.63) and overall COVID-19 vaccine confidence (OR 7.23, 95% CI 4.53–11.69). Having a bank account was significantly associated with higher odds of having confidence in vaccines’ safety (OR 2.20, 95% CI 1.07–4.51) but no evidence of association with having confidence in vaccines’ importance, safety, and overall COVID-19 vaccine confidence (Table 3).
Table 3.
Adjusted odds ratios and 95% confidence intervals for predictors of COVID-19 confidence in effectiveness, safety, importance, and overall confidence among the study population (N = 646).
| Variable | Importance | Safety | Effectiveness | Overall |
|---|---|---|---|---|
| Age | ||||
| <50 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| 50-59 | 1.09 (0.53-2.25) | 1.21 (0.64-2.30) | 1.23 (0.63-2.40) | 1.15 (0.62-2.14) |
| 60-69 | 1.41 (0.68-2.92) | 1.57 (0.82-3.02) | 1.76 (0.88-3.50) | 1.48 (0.80-2.78) |
| 70+ | 0.78 (0.39-1.57) | 0.98 (0.52-1.85) | 0.89 (0.46-1.70) | 0.97 (0.52-1.80) |
| Sex | ||||
| Male | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Female | 1.17 (0.65-2.10) | 1.28 (0.75-2.17) | 1.26 (0.72-2.18) | 1.30 (0.78-2.17) |
| Education | ||||
| None | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Primary education | 1.49 (0.83-2.69) | 1.45 (0.83-2.54) | 2.09 (1.18-3.70) | 1.60 (0.92-2.80) |
| Secondary and above | 1.51 (0.58-3.98) | 1.88 (0.76-4.64) | 2.77 (1.10-6.97) | 2.23 (0.93-5.30) |
| District | ||||
| Moshi MC | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Moshi DC | 1.30 (0.74-2.28) | 1.07 (0.63-1.80) | 1.25 (0.72-2.15) | 1.16 (0.70-1.93) |
| Mwanga MC | 2.13 (1.26-3.59) | 1.67 (1.04-2.67) | 1.94 (1.18-3.18) | 2.01 (1.27-3.19) |
| Marital status1 | ||||
| In union | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Not in union | 0.87 (0.54-1.38) | 0.78 (0.51-1.19) | 0.80 (0.51-1.25) | 0.80 (0.53-1.21) |
| Religion | ||||
| Muslim | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Christian | 0.96 (0.62-1.50) | 1.03 (0.69-1.55) | 0.99 (0.65-1.52) | 1.03 (0.70-1.53) |
| Others | 1.57 (0.17-14.29) | - | 1.81 (0.20-16.16) | 2.95 (0.33-26.11) |
| Bank account | ||||
| No | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Yes | 1.35 (0.63-2.90) | 2.20 (1.07-4.51) | 1.07 (0.54-2.14) | 1.61 (0.84-3.08) |
| Covid-19 disease risk perception | ||||
| Not at risk | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| At risk | 1.36 (0.85-2.16) | 1.03 (0.68-1.57) | 1.41 (0.91-2.19) | 1.13 (0.76-1.69) |
| Ever infected with Covid-19 | ||||
| No | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Yes | 1.42 (0.37-5.41) | 1.00 (0.34-2.99) | 0.92 (0.30-2.79) | 0.83 (0.31-2.22) |
| Covid-19 vaccine knowledge2 | ||||
| Poor knowledge | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Good knowledge | 11.41 (5.75-22.65) | 6.76 (4.09-11.16) | 8.30 (4.71-14.63) | 7.23 (4.53-11.69) |
1In union is being married or cohabiting. Not in union includes being single/divorced/separated/widow/widower.
2Details on how COVID-19 vaccine knowledge was measured have been published elsewhere.20
Effect of COVID-19 vaccine confidence on COVID-19 vaccine uptake
In both crude and adjusted logistic regression models, confidence in vaccines’ importance, safety, effectiveness, and overall COVID-19 vaccine confidence was strongly associated with higher odds of COVID-19 vaccine uptake compared to not having COVID-19 vaccine confidence. After adjusting for age, sex, and knowledge of COVID-19 vaccines, having confidence in vaccines’ importance (OR 6.35, 95% CI 3.82–10.55, p < .001), safety (OR 7.36, 95% CI 4.67–11.61, p < .001), effectiveness (OR 7.15, 95% CI 4.42–11.55, p < .001) and overall COVID-19 vaccine confidence (OR 6.88, 95% CI 4.46–10.61, p < .001) was strongly associated with higher odds of COVID-19 vaccine uptake (Table 4).
Table 4.
Effect of COVID-19 vaccine confidence on vaccine uptake among individuals with hypertension and diabetes mellitus in Kilimanjaro region, Tanzania (N = 646).
| Variable | 1COR (95% CI) | P value | 2AOR(95% CI) | P value |
|---|---|---|---|---|
| Importance | <0.001 | <.001 | ||
| No | 1.00 (ref) | 1.00 (ref) | ||
| Yes | 7.25 (4.46-11.76) | 6.35 (3.82-10.55) | ||
| Safety | <0.001 | <.001 | ||
| No | 1.00 (ref) | 1.00 (ref) | ||
| Yes | 8.00 (5.20-12.33) | 7.36 (4.67-11.61) | ||
| Effectiveness | <0.001 | <.001 | ||
| No | 1.00 (ref) | 1.00 (ref) | ||
| Yes | 7.83 (4.97-12.33) | 7.15 (4.42-11.55) | ||
| Overall confidence | <0.001 | <.001 | ||
| No | 1.00 (ref) | 1.00 (ref) | ||
| Yes | 7.64 (5.11-11.42) | 6.88 (4.46-10.61) |
OR, Odds Ratio. 1Crude odds ratio. 2Adjusted odds ratio. The odds ratio was derived from the logistic regression model and in the multivariable analyses were adjusted for age, sex, and COVID-19 vaccine knowledge.
Discussion
We investigated factors associated with confidence in COVID-19 vaccines’ safety effectiveness, importance, and overall COVID-19 confidence and the effect of confidence on COVID-19 vaccine uptake among people with hypertension or diabetes mellitus in the Kilimanjaro region of Tanzania. This study revealed that overall, the proportion of participants with overall COVID-19 vaccine confidence was 70% and was highest for perceived vaccine importance (80%), followed by perceived vaccine effectiveness (77%) and perceived vaccine safety (74%). High confidence in COVID-19 vaccines in this population (70%) may be due to their high-risk profile. Since people with underlying medical conditions are at an increased risk of complications of COVID-19 including death and hence prioritized to receive the vaccines, they may have been more likely to seek information regarding COVID-19 vaccines from trustful sources like healthcare workers. This therefore may explain the high confidence levels in this group compared to the general population among adult community members in Tanzania.14
Nevertheless, we observed low COVID-19 vaccine uptake of just above half of the participants. This is contrary to what we expected because of the high-risk nature of our study population together with the initial prioritization of COVID-19 vaccination among people with underlying chronic conditions. A possible explanation for our observed findings could be due to myths that were spreading about potential safety concerns of COVID-19 vaccines in the initial phases of the COVID-19 vaccine rollout. Additionally, this could have been compounded by the initial government denial of the existence of COVID-19 disease before the COVID-19 vaccine rollout in Tanzania, leading to low confidence in the vaccines and therefore explaining this low uptake.25 A qualitative study among general community members in Tanzania further revealed that conflicting information from the government leaders who discouraged people from getting vaccinated and encouraged traditional medicine instead was reported as one of the barriers to COVID-19 vaccine uptake among unvaccinated participants.27 These may have stemmed lasting concerns on the safety of the vaccines resulting in hesitancy that can lead to low vaccine uptake.
We also explored factors associated with COVID-19 vaccine confidence. The study found that good knowledge of COVID-19 vaccines was strongly associated with having confidence in vaccines’ safety, effectiveness, importance, and overall COVID-19 vaccine confidence. Sources of information that people trust influence what they know about vaccines and this subsequently affects their knowledge and hence confidence in vaccines.28 Social media has been a major means of spreading rumors, misinformation, and disinformation about COVID-19 vaccines. Having social media as the trusted source of information has been associated with COVID-19 vaccine confidence as opposed to having healthcare bodies and government sources as the source of information.28 These findings are consistent with the results we obtained from our previous study among general community members in Tanzania.20 This suggests that having the right information regarding vaccines can influence one’s knowledge and perception of vaccines and therefore confidence. For this, education campaigns have been one of the key interventions to address public confidence in COVID-19 vaccines and therefore increase uptake in Tanzania.29 Targeted interventions to educate people with chronic illnesses are highly needed to increase vaccine confidence in this population.
Those living in Mwanga MC had higher odds of confidence in the vaccines’ safety, importance, effectiveness, and overall COVID-19 vaccines than those living in Moshi MC. Door-to-door campaigns that were intensively conducted in Mwanga MC by community health workers may have explained the higher odds of vaccine confidence in these areas than in Moshi MC. Additionally, Moshi MC is located in an urban area while Mwanga MC is in a semi-urban area. Since people living in urban areas have relatively more access to sources of information like social media where rumors and myths about the vaccines spread which influence confidence in the vaccines, this may have explained the higher confidence we observed in this semi-urban district as compared to the urban district.
Confidence in vaccines is strongly linked with vaccination decisions including acceptance, uptake, hesitancy, and refusal. Our study found that confidence in COVID-19 vaccine safety, effectiveness, importance, and overall COVID-19 vaccine confidence is strongly associated with higher odds of uptake of COVID-19 vaccines. Safety concerns, fear of side effects, doubts over vaccine effectiveness, and fear of aggravation of underlying medical conditions by vaccines are reasons for unwillingness to vaccinate and non-receipts of COVID-19 vaccines among people with chronic illnesses.30–32 Nonetheless, confidence in the COVID-19 vaccines’ importance, safety, and effectiveness was associated with higher odds of uptake of COVID-19 vaccines among people with chronic illnesses in Ethiopia.30 Similar findings have been reported among general community members in Tanzania,20 in an international survey from low- and middle-income countries in Africa and Asia,12 and a global multi-country survey.5 Vaccine confidence, apart from convenience and complacency, has been conceptualized by the WHO’s Strategic Advisory Group of Experts in Immunization as one of the key drivers for vaccination decisions.8 Tanzania’s COVID-19 vaccination coverage was substantially low after the initial rollout of COVID-19 vaccines from June 2021 perhaps due to the initial refusal of COVID-19 vaccines from the government officials.25 Raising vaccine confidence was a strategy that Tanzania received from the WHO and its collaborative partners in January 2022 to increase vaccine demand and uptake.33 This included awareness campaigns to increase awareness of vaccine importance and hence, vaccination which was done door-to-door. This strategy yielded a substantial rise in vaccine coverage from less than 10% in January 2021 to more than 50% in April 2023 in the target population.33 This therefore implies that strategies to increase vaccine confidence such as education and social behavior change interventions can have a substantial impact on vaccine uptake and therefore coverage. This is particularly critical to mitigate the increased risk of morbidity and mortality from COVID-19 disease that people with underlying medical conditions like hypertension or diabetes mellitus bear.
Value that this study adds
This is the first study to elucidate factors associated with COVID-19 vaccine confidence and the effect it has on COVID-19 vaccine uptake among people with chronic illnesses in Tanzania. Our study also quantified the effect that vaccine confidence had on COVID-19 vaccine uptake. Our findings imply that improving public confidence in COVID-19 vaccines’ importance, safety, and effectiveness among people with chronic illnesses can lessen vaccine hesitancy and improve vaccination rates and therefore curb the disproportionate increased risk of morbidity and mortality that this population bears. These findings could also enhance interventions targeted to improve vaccination rates in the current and future pandemics.
Strengths and limitations
The response rate of participants to this study was 97% and hence selection bias due to non-response is unlikely. However, selection bias may have been introduced since data were collected during the working hours of the day and hence more likely to have missed the working group of eligible participants. Furthermore, not all participants’ vaccine uptake self-reports were validated using records from vaccination cards leading to possible misclassification of vaccination uptake. Nevertheless, the proportion of those whose vaccination status was not validated by vaccination cards was less than 10% hence the possible misclassification is unlikely to have impacted our estimates. Lastly, our study was conducted among individuals with chronic illnesses, i.e., either hypertension or diabetes, hence our findings cannot be generalized to a wide range of populations.
Conclusions
Seventy percent of the participants had confidence in COVID-19 vaccine safety, importance, effectiveness, and overall COVID-19 vaccine confidence. Having good knowledge of COVID-19 vaccines and living in Mwanga MC increased the odds of COVID-19 vaccine confidence. We also found COVID-19 vaccine confidence was strongly associated with higher odds of vaccine uptake. These findings highlight the need for designing interventions such as education on the safety, effectiveness, and importance of COVID-19 vaccines for people with chronic illnesses. A particular focus should be in urban areas to curb misinformation, increase vaccine confidence, and eventually uptake, without leaving the rural and disadvantaged residents behind.
Supplementary Material
Acknowledgments
We would like to extend our sincere gratitude to all study participants, a team of data collectors from the Kilimanjaro Christian Medical University College, the Institute of Public Health, the ethical committee team, and local authorities for making this study possible.
Biography
Monica Mtei is a Tutorial Assistant at Kilimanjaro Christian Medical University College (KCMUCo), Department of Epidemiology and Biostatistics, Moshi Tanzania and a PhD candicate at the London School of Hygiene and Tropical Medicine; DMB is an Assistant Lecturer at KCMUCo, Department of Epidemiology and Biostatistics, Moshi Tanzania; CA is an Assistant Lecturer at KCMUCo, department of Epidemiology and Biostatistics, Moshi Tanzania; JSB is a Tutorial Assistant at KCMUCo, Department of Community Health, Moshi Tanzania; LJS is an Assistant lecturer at KCMUCo, Department of Epidemiology and Biostatistics, Moshi Tanzania; AF is a Research Administrator at Kilimanjaro Christian Medical Centre, Joint Malaria Program, Moshi Tanzania; IBM is a Lecturer at KCMUCo, Department of Epidemiology and Biostatistics and a Research Fellow at Lund University, Department of Translational Medicine, Malmo Sweden; JN is a Lecturer at KCMUCo, Department of Epidemiology and Biostatistics, Moshi Tanzania; JMG is an assistant lecturer at KCMUCo, Department of Epidemiology and Biostatistics and Community Health Department, Moshi Tanzania; SEM is a Professor in Maternal and Child Health at KCMUCo, Community Health Department and Department of Epidemiology and Biostatistics, Moshi Tanzania.
MM is a medical doctor and a tutorial assistant at the Institute of Public Health, Department of Epidemiology and Biostatistics at Kilimanjaro Christian Medical University College.
Funding Statement
The author (s) reported that there is no funding associated with the work featured in this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data will be made available upon request.
Statement of ethical approval
This study was approved by the Kilimanjaro Christian Medical University College Ethical Review Board (REC.2609). Informed consent was obtained from all participants before interviewing the participants. Consent was given verbally and was voluntary i.e., participants had the right to withdraw their participation from any time during the interview. All interviews were conducted face-to-face and an interview lasted for an average of 20–30minutes. Privacy and confidentiality was ensured before commencing the interviews.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2024.2396213
References
- 1.World Health Organization . WHO coronavirus (COVID-19) dashboard | WHO coronavirus (COVID-19) dashboard with vaccination data [Internet]. 2023. [accessed 2023 Oct 5]. https://covid19.who.int/?mapFilter=vaccinations.
- 2.CDC - Centers for Disease Control and Prevention . COVID-19 and people with certain medical conditions [Internet]. 2023. [accessed 2023 Oct 5]. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html.
- 3.World Health Organization . COVID-19 Vaccines Advice [Internet]. 2023. [accessed 2023 Oct 5]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines/advice.
- 4.CDC - Centers for Disease Control and Prevention . Benefits of getting a COVID-19 vaccine [Internet]. 2023. [accessed 2023 Oct 5]. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/vaccine-benefits.html.
- 5.de Figueiredo A, Simas C, Larson HJ.. COVID-19 vaccine acceptance and its socio-demographic and emotional determinants: a multi-country cross-sectional study. Vaccine. 2023. Jan 9;41(2):354–8. doi: 10.1016/j.vaccine.2022.10.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Hanawi MK, Ahmad K, Haque R, Keramat SA. Willingness to receive COVID-19 vaccination among adults with chronic diseases in the Kingdom of Saudi Arabia. J Infect Public Health. 2021;14(10):1489–1496. doi: 10.1016/j.jiph.2021.08.002. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization (WHO) . Summary WHO SAGE conclusions and recommendations on vaccine hesitancy-guide-to-tailoring-immunization-programmes-TIP.Pdf. 2015. [accessed 2023 Oct 5].
- 8.MacDonald NE, Eskola J, Liang X, Chaudhuri M, Dube E, Gellin B. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 9.Project VC. About the vaccine confidence project – the vaccine confidence project. [accessed 2023 Oct 5]. https://www.vaccineconfidence.org/who-we-are/about/.
- 10.Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Cook AR, Jones NS. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine [Internet]. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soares P, Moniz M, Gama A, Laires PA, Pedro AR, Dias S, Dias S, Leite A, Nunes C. Factors associated with COVID-19 vaccine hesitancy. Vaccines (Basel). 2021;9(3):300–314. doi: 10.3390/vaccines9030300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bono SA, Faria E, Villela DM, Siau CS, Chen WS, Pengpid S, Sessou P, Ditekemena JD, Amodan BO, Hosseinipour MC, et al. Factors affecting COVID-19 vaccine acceptance: an international survey among low- and middle-income countries. Vaccines (Basel). 2021;9(5):515–519. doi: 10.3390/vaccines9050515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yupari-Azabache IL, Luis Díaz-Ortega J, Bardales-Aguirre LB, Barros-Sevillano S, Paredes-Díaz SE, Yupari IL. Factors associated with the acceptance of COVID-19 vaccines in citizens of Northern Peru: cross-sectional study. Risk Manag Healthc Policy. 2022. doi: 10.2147/RMHP.S374385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mtei M, Mboya IB, Mgongo M, Manongi R, Amour C, Bilakwate JS, Nyaki AY, Ngocho J, Jonas N, Farah A, et al. Confidence in COVID-19 vaccine effectiveness and safety and its effect on vaccine uptake in Tanzania: a community-based cross-sectional study. Hum Vaccin Immunother. 2023;19(1). doi: 10.1080/21645515.2023.2191576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jiang N, Gu P, Sun, Han H, Liu W, Sun X, Song N, Jiang X. Acceptance of COVID-19 vaccines in patients with chronic diseases: a cross-sectional study. J Clin Nurs. 2022;31(21–22):3286–3300. doi: 10.1111/jocn.16284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bulusu A, Segarra C, Khayat L. Analysis of COVID-19 vaccine uptake among people with underlying chronic conditions in 2022: a cross-sectional study. SSM-Popul Health [Internet]. 2023. [accessed 2023 Oct 6];22:101422. doi: 10.1016/j.ssmph.2023.101422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bulusu A, Segarra C, Khayat L. Analysis of COVID-19 vaccine uptake among people with underlying chronic conditions in 2022: a cross-sectional study. SSM-Popul Health. 2023;22:101422. doi: 10.1016/j.ssmph.2023.101422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oliver K, Raut A, Pierre S, Silvera L, Boulos A, Gale A, Baum A, Chory A, Davis NJ, D’Souza D, et al. Factors associated with COVID-19 vaccine receipt at two integrated healthcare systems in New York City: a cross-sectional study of healthcare workers. BMJ Open. 2022;12(1):e053641. doi: 10.1136/bmjopen-2021-053641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aseneh JB, Agbor VN, Kadia BM, Okolie EA, Ofomata CJ, Etombi CL, Ekaney DS, Joko Fru YW. Factors associated with COVID-19 vaccine hesitancy among healthcare workers in Cameroon and Nigeria: a web-based cross-sectional study. Int Health. 2023; 1–13. doi: 10.1093/inthealth/ihad013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mtei M, Mboya IB, Mgongo M, Manongi R, Amour C, Bilakwate JS, Nyaki AY, Ngocho J, Jonas N, Farah A, et al. Confidence in COVID-19 vaccine effectiveness and safety and its effect on vaccine uptake in Tanzania: a community-based cross-sectional study. Hum Vaccin Immunother [Internet]. 2023. [accessed 2023 Sep 21];19(1). doi: 10.1080/21645515.2023.2191576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown Aseneh J, Agbor N, Momo Kadia B, Okolie EA, Janefrances Ofomata C, Linonge Etombi C, Ekaney DS, Joko Fru YW. Factors associated with COVID-19 vaccine hesitancy among healthcare workers in Cameroon and Nigeria: a web-based cross-sectional study. Int Health [Internet]. 2023. [accessed 2023 Oct 4]. 15(6):1–13. doi: 10.1093/inthealth/ihad013AdvanceAccesspublication02023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tarimo CS, Wu J. The first confirmed case of COVID-19 in Tanzania: recommendations based on lesson learned from China. Trop Med Health. 2020. Apr 26;48(1). doi: 10.1186/s41182-020-00214-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization (WHO) . WHO coronavirus (COVID-19) dashboard | WHO coronavirus (COVID-19) dashboard with vaccination data [internet]. 2023. [accessed 2023 Oct 6]. https://covid19.who.int/?mapFilter=vaccinations/.
- 24.World Health Organization T. WHO (World Health Organization) . From below 10 to 51 percent - Tanzania increases COVID-19 vaccination coverage. [accessed 2023 Nov 11]. https://www.afro.who.int/countries/united-republic-of-tanzania/news/below-10-51-percent-tanzania-increases-covid-19-vaccination-coverage.
- 25.Makoni M. Tanzania refuses COVID-19 vaccines. Lancet [Internet]. 2021;397(10274):566. doi: 10.1016/S0140-6736(21)00362-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Osuagwu UL, Langsi R, Ovenseri-Ogbomo G, Mashige KP, Abu EK, Envuladu EA, Goson PC, Ekpenyong BN, Oloruntoba R, Miner CA, et al. Analysis of perception, reasons, and motivations for COVID-19 vaccination in people with diabetes across sub-saharan Africa: a mixed-method approach. Int J Environ Res Public Health. 2022. Jul 1;19(13):7875. doi: 10.3390/ijerph19137875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mgongo MB, Manongi RN, Mboya IB, Ngocho JS, Amour C, Mtei M, Bilakwate JS, Nyaki AY, George JM, Leyaro BJ, et al. A qualitative study on barriers to COVID-19 vaccine uptake among community members in Tanzania. Vaccines (Basel). 2023. Aug 1;11(8):1366. doi: 10.3390/vaccines11081366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.CDC Africa . COVID-19 perception survey final report 20.02.2021. 2021. [accessed 2023 Sep 18].
- 29.GAVI Vaccine Alliance. GAVI Vaccine Alliance . How Tanzania leapfrogged into the lead on COVID-19 vaccination | Gavi, the vaccine alliance. 2023. [accessed 2023 Oct 13]. https://www.gavi.org/vaccineswork/how-tanzania-leapfrogged-lead-covid-19-vaccination.
- 30.Dagnew Baye N, Agegnehu Teshome A, Agimas Ayenew A, Tilahun Mulu A, Chekol Abebe E, Tilahun Muche Z. Attitude and level of COVID-19 vaccination and its determinants among patients with chronic disease visiting Debre Tabor Comprehensive Specialized Hospital, Northwest Ethiopia: a cross-sectional study. PLOS ONE. 2022. Dec 1;17(12 December):e0278914. doi: 10.1371/journal.pone.0278914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choi T, Chan B, Grech L, Kwok A, Webber K, Wong J, Nguyen M, Bain N, Day D, McCartney A, et al. Factors influencing COVID-19 vaccine hesitancy among patients with serious chronic illnesses during the initial Australian vaccine rollout: a multi-centre qualitative analysis using the health belief model. Vaccines (Basel). 2023. Feb 1;11(2):239. doi: 10.3390/vaccines11020239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ojewale LY, Mukumbang FC. COVID-19 vaccine hesitancy among Nigerians living with non-communicable diseases: a qualitative study. BMJ Open. 2023;13(2):e065901. doi: 10.1136/bmjopen-2022-065901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization UR of T . From below 10 to 51 percent - Tanzania increases COVID-19 vaccination coverage | WHO | regional office for Africa [Internet]. 2023. [accessed 2023 Oct 5]. https://www.afro.who.int/countries/united-republic-of-tanzania/news/below-10-51-percent-tanzania-increases-covid-19-vaccination-coverage/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available upon request.


