Abstract
Granulomatosis with polyangiitis (GPA) is a rare autoimmune disease with multi-system involvement. It involves the upper respiratory tract, lungs and kidneys. A 36-year-old female patient presented to a tertiary care referral hospital in Central India in 2023 with complaints of low-grade fever, dry cough and loss of appetite initially followed by dyspnoea, purpuric skin lesions, right lower limb swelling with pain and redness. Her chest radiograph revealed right upper lobe cavitary lesion with consolidation in the right lower lobe. Mycobacterium tuberculosis was detected in sputum and broncho alveolar lavage via cartridge based nucleic acid amplification assay. Later, computed tomography pulmonary angiography revealed bilateral pulmonary artery thromboembolism. Furthermore, her cytoplasmic-antineutrophil cytoplasmic antibody test was positive, serum creatinine was rising, urine microscopy had red cell casts and lower limb venous doppler revealed deep venous thrombosis. Histopathological examination of the skin lesion revealed vasculitis. Based on these findings, the patient was diagnosed with GPA. The patient improved with pulse steroids, cyclophosphamide, anticoagulants and anti-tuberculous therapy.
Keywords: Granulomatosis with Polyangiitis, Pulmonary Tuberculosis, Deep Venous Thrombosis, Vasculitis, c-ANCA, Case Report, India
Granulomatosis with polyangiitis (GPA) formerly known as Wegner’s granulomatosis is a systemic vasculitis involving small vessels predominantly.1 In countries with high prevalence of tuberculosis (TB), the diagnosis can be challenging as the presentation of GPA is heterogenous and can mimic TB due to its clinico-radiological overlap.2 In addition, immunosuppressive therapy, which is the main-stay of treatment for GPA can also lead to an increased risk of infections such as TB. We present an extremely rare case of GPA who, at presentation, had pulmonary tuberculosis as well as pulmonary thromboembolism. Whether there was an increased predisposition of one disease because of the other or an extremely rare coincidence of all 3 diseases occurring together remains debatable.
Case Report
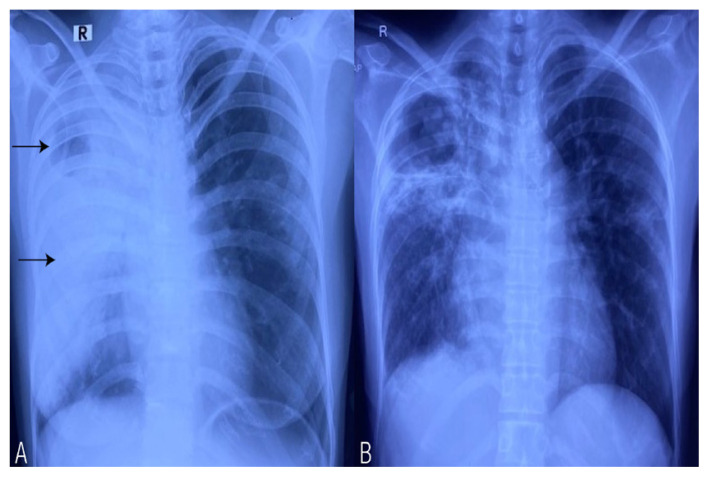
A 36-year-old female patient, a house-wife without any obvious risk factors and co-morbidities, presented to a tertiary care referral hospital in Central India in 2023 with complaints of low-grade fever, dry cough and loss of appetite for 1 month. On evaluation by a general practitioner, she was suspected as having pulmonary TB as her chest radiograph showed a cavity in the right upper lobe along with consolidation in right upper and lower lobes [Figure 1A]. This was then confirmed by sputum examination for acid fast bacillus (AFB) by cartridge based nucleic acid amplification test (CBNAAT), which was positive. She was hence started on anti-tuberculous therapy (ATT). However, there was not much improvement clinically even after 1 month of starting ATT and she developed shortness of breath, purpuric skin lesions, epistaxis and also accompanying right lower limb swelling with pain and redness. On initial examination her blood pressure was 138/88 mmHg, oxygen saturation was 88% at room air and pulse rate was 92 beats/minute. Her haemogram test and serum electrolytes were normal but urine routine and microscopy showed red cell casts, blood urea nitrogen was 16.07 mmol/L, plasma creatine was 167.2 μmol/L (which gradually increased to 387.2 μmol/L) and elevated D-dimer levels (2.3 FEU/L). Urine and blood cultures were found to be normal.
Figure 1.
A: Chest radiograph showing a cavity in the right upper lobe (upper arrow) along with consolidation in right upper and lower lobes (lower arrow). B: Follow-up chest radiograph showing significant resolution of the consolidation.
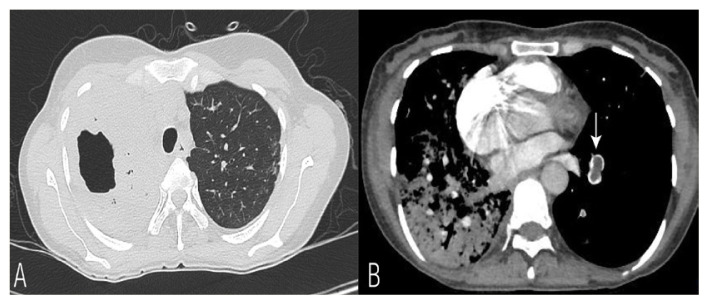
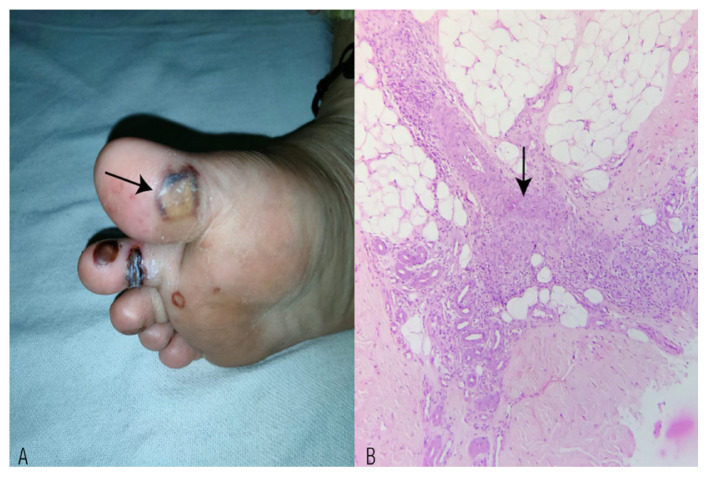
Arterial and venous colour doppler of bilateral limbs revealed long segment hypoechoic thrombus in right saphenous and popliteal vein with no arterial thrombus. 2-dimensional echocardiography showed dilated right atrium, right ventricle internal diameter (RVID = 3.23 cm) with peak systolic right ventricular pressure of 56 mmHg, mild tricuspid regurgitation with normal right ventricle and left ventricle systolic function. On further evaluation, computed tomography pulmonary angiography (CTPA) was done. Parenchymal window showed dense consolidation in right hemithorax with a cavity in right upper lobe and angiogram images revealed hypodense thrombus in the lumen of segmental arteries of right lower lobe and left lower lobar artery suggestive of pulmonary thromboembolism [Figure 2]. Autoimmune work-up revealed negative antinuclear antibodies (ANA) profile whilst cytoplasmic-antineutrophil cytoplasmic antibody (c-ANCA) was strongly positive (>200 RU/mL, biological reference: <20, done via immunofluorescence). Perinuclear-ANCA, C4 and C3 were all negative. Punch biopsy from the purpuric skin lesions showed vasculitis consistent with GPA [Figure 3]. Flexible bronchoscopy revealed no obvious endobronchial growth as such, but bronchoalveolar lavage (BAL) for AFB and CBNAAT was positive for mycobacterium TB. Diagnosis of GPA was made based on serology, involvement of respiratory tract, haematuria and skin biopsy.
Figure 2.
A: Parenchymal window of computed tomography (CT)thorax showing dense consolidation in right hemithorax with a cavity in right upper lobe. B: CT pulmonary angiogram image revealing hypodense thrombus in the arterial branch of left lower lobe (vertical arrow) highly suggestive of pulmonary thromboembolism.
Figure 3.
A: Photograph showing haemorrhagic vesicles with perilesional purpura and erythema over the sole region (arrow). B: Haematoxylin and eosin stain of subcutaneous tissue at ×100 magnification showing medium-sized vessels infiltrated by histiocytes in aggregates, lymphocytes and a few neutrophils. The vessel wall shows focal fibrinoid necrosis (arrow).
Since GPA with deep venous thrombosis and pulmonary TBwere diagnosed almost simultaneously, a combined treatment for GPA, TB and deep venous thrombosis was promptly started at the same time, to avoid further worsening of patient’s clinical condition. The patient was treated with pulse methylprednisolone 1 g for 3 days followed by gradual tapering of steroids along with cyclophosphamide. Anti-TB treatment was started along with systemic anticoagulation (initially started with heparin and gradually switched to rivaroxaban). The patient improved significantly over the subsequent weeks and is under regular follow-up [Figure 1B].
Patient consent was obtained for the publication of this case.
Discussion
The diagnosis of GPA is based on a combination of various clinical manifestations of a systemic disease suggestive of vasculitis; positive ANCA serology and histological evidence of necrotising vasculitis, necrotising glomerulonephritis or granulomatous inflammation from a relevant organ biopsy, such as the skin, lung or kidney.2 The diagnosis of concomitant GPA and TB is challenging because firstly clinical features of TB and GPA are overlapping, secondly despite considerable specificity of c-ANCA in GPA, c-ANCA levels have occasionally been reported to be raised in patients with TB.3 Both these aetiologies coexisted in the current patient as on one hand, AFB was detected twice in sputum as well as BAL, and on the other hand, a positive c-ANCA, vasculitis on skin histopathology and dramatic response of lung consolidation to steroids confirmed the presence of GPA.4
Both TB and ANCA associated vasculitis can lead to a hypercoagulable state and lead to an increased incidence of venous thromboembolic (VTE) diseases.5 Patients appear to be particularly at risk especially during active periods of inflammation.6 Occasional detection of ANCA in TB may also suggest triggering of an autoimmune reaction with mycobacterium TB as the inciting antigen. Although one can debate these manifestations being bracketed under one broad spectrum of TB, the authors would prefer to label GPA as an independent occurrence because of the combined presence of c-ANCA, vasculitis on skin biopsy, response to steroids and lack of drug induced lupus/ANA.
The Wegener’s Clinical Occurrence of Thrombosis study recruited 180 patients during active periods of disease. The reported incidence of VTE was 7.0 per 100 person-years (95% confidence interval: 4.0–11.4).7 In a case report published in Iran, a 28-year-old male was diagnosed with both TB and GPA and was hence started on both immunosuppressants and ATT; the patient eventually developed cerebral venous thrombosis which was treated with anticoagulation medication. In another case published by Khilani et al., a patient was initially started with ATT based on clinico-radiological features but eventually turned out to be Wegners following detection of vasculitis and c-ANCA.4 The current patient was also found to have both TB and GPA, but with deep venous thrombosis at the time of presentation which is a very rare entity.8
The complexity of the possible inter-relationships between the disease entities enables more than one hypothesis to be possible; it is virtually impossible to determine which one leads to the other. But the simultaneous detection of 3 entities, which can otherwise exist independently also, makes this case worthwhile and intriguing.
Co-existing diagnosis of these 3 entities is a challenge to manage. This is because immunosuppressants such as steroids and cyclophosphamide is the gold standard treatment in Wegners, while these may increase the severity of TB. However, treatment of Wegners is warranted to reduce mortality and morbidity in due course. At the same time, Wegners leads to progressive renal disease which leads to change in the ATT regimen as per the renal parameters.
Though immunosuppressive therapy is relatively contraindicated in patients with active TB, untreated GPA might be life-threatening. Moreover, combined treatments for both vasculitis and TB shows positive patient response, according to published case reports.9,10
Conclusion
To the best of the authors’ knowledge, this is the first case report presenting a coexisting diagnosis of GPA, pulmonary TB, deep venous thrombosis and pulmonary thromboembolism. Therefore, clinicians should be aware of potential multiple differential diagnoses when considering diagnosis and treatment.
Footnotes
AUTHORS’ CONTRIBUTION: STP and AK conceptualised the work. AK, KK and AG managed the patient. STP collected the data. KK performed the literature search. STP, AK and KK drafted the initial manuscript. AK and AG edited and finalised the manuscript. All authors approved the final version of the manuscript.
References
- 1.Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65:1–11. doi: 10.1002/art.37715. [DOI] [PubMed] [Google Scholar]
- 2.Robson JC, Grayson PC, Ponte C, Suppiah R, Craven A, Judge A, et al. 2022 American College of Rheumatology/European Alliance of Associations for Rheumatology classification criteria for granulomatosis with polyangiitis. Arthritis Rheumatol. 2022;74:393–9. doi: 10.1002/art.41986. [DOI] [PubMed] [Google Scholar]
- 3.Flores-Suárez LF, Cabiedes J, Villa AR, van der Woude FJ, Alcocer-Varela J. Prevalence of antineutrophil cytoplasmic autoantibodies in patients with tuberculosis. Rheumatology (Oxford) 2003;42:223–9. doi: 10.1093/rheumatology/keg066. [DOI] [PubMed] [Google Scholar]
- 4.Khilani GC, Banga A, Sharma SC, Gupta SD. Wegener’s granulomatosis: An isolated lung mass responding to antituberculosis therapy and atypical course. J Assoc Physicians India. 2003;51:731–3. [PubMed] [Google Scholar]
- 5.Kager LM, Blok DC, Lede IO, Rahman W, Afroz R, Bresser P, et al. Pulmonary tuberculosis induces a systemic hypercoagulable state. J Infect. 2015;70:324–34. doi: 10.1016/j.jinf.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 6.Stassen PM, Derks RP, Kallenberg CG, Stegeman CA. Venous thromboembolism in ANCA-associated vasculitis--incidence and risk factors. Rheumatology (Oxford) 2008;47:530–4. doi: 10.1093/rheumatology/ken035. [DOI] [PubMed] [Google Scholar]
- 7.Merkel PA, Lo GH, Holbrook JT, Tibbs AK, Allen NB, Davis JC, Jr, et al. Brief communication: high incidence of venous thrombotic events among patients with Wegener granulomatosis: the Wegener’s Clinical Occurrence of Thrombosis (WeCLOT) Study. Ann Intern Med. 2005;142:620–6. doi: 10.7326/0003-4819-142-8-200505030-00011. [DOI] [PubMed] [Google Scholar]
- 8.Rostami Z, Cegolon L, Jafari NJ, Gholami N, Mousavi SV, Allahyari F, et al. A rare case of coexistence of Wegener’s granulomatosis and pulmonary tuberculosis with subsequent development of thrombosis of the cerebral veins. BMC Infect Dis. 2021;21:948. doi: 10.1186/s12879-021-06583-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oxley Oxland J, Ensor J, Freercks R. Tuberculosis and pauci-immune crescentic glomerulonephritis. BMJ Case Rep 2018; 2018:bcr201722. 1948 doi: 10.1136/bcr-2017-221948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sopeña B, Sobrado J, Javier Pérez A, Oliver J, Courel M, Palomares L, et al. Rapidly progressive glomerulonephritis and pulmonary tuberculosis. Nephron. 1991;57:251–2. doi: 10.1159/000186268. [DOI] [PubMed] [Google Scholar]