Abstract
Background:
Insufficient knowledge about COVID-19 and low socioeconomic status have been associated with distrustful attitudes towards vaccination against COVID-19.
Objective:
The aim of this study was to explore determinants of COVID-19 vaccine uptake among the general population and health workers.
Methods:
A cross sectional study was conducted in 16 councils which included; Milele, Mpanda, Newala, Simanjiro, Nanyumbu, Muleba, Longido, Ulanga, Igunga, Mbulu, Karatu, Mufindi, Mvomero, Kilolo and Tabora Town. A total of 427 health care workers and 1,907 individuals were sampled from health facilities and households. Structured questionnaires were used to collect the required information.
Results:
Although the majority (93.2%) of health workers were vaccinated, 35.4% perceived their risk of getting COVID-19 infection as high. Self-reported uptake of COVID-19 vaccine was 42.4% among the general population. Significantly low proportion of the general population in Mufindi district council (7.5%) were vaccinated against COVID-19. Health workers' knowledge and perception on COVID-19 vaccination did not vary with socio-demographic factors. Among the general population, those who were separated/divorced (ARR: 0.8: 95% CI; 0.7 to 0.9), those who attained primary level of education (ARR: 0.8: 95% CI; 0.7 to 0.9), self-employed (ARR: 0.8: 95% CI; 0.7 to 0.9) and unemployed (ARR: 0.7: 95% CI; 0.6 to 0.8) were less likely to be vaccinated against COVID-19. Having positive attitude (ARR: 1.2: 95% CI; 1.1 to 1.5) and perception (ARR:1.8: 95% CI; 1.5 to 2.2), and knowledge on COVID-19 prevention (ARR: 3.0: 95% CI; 2.1to 4.4) increased the likelihood COVID-19 vaccine uptake. Prior experience of vaccination against other diseases (ARR:1.2: 95% CI; 1.0 to1.3), having history of chronic diseases (ARR:1.3: 95% CI; 1.2 to 1.4) and a family member who died of COVID-19 (ARR:1.3: 95% CI; 1.1to1.4) were also determinants of COVID-19 vaccine uptake.
Conclusion:
Uptake of COVID-19 vaccine among the general population was significantly low among individuals with primary level of education, self-employed, unemployed, and those who were divorced or separated. Individuals with comprehensive knowledge on COVID-19 vaccination, those with positive attitude and perception on COVID-19 vaccination, having history of chronic diseases, prior vaccination against other diseases, and having a family member who succumbed to COVID-19 increased the likelihood COVID-19 vaccine uptake among the general population. Provision of health education and implementation of socio-behavioural communication change interventions are necessary to equip the general population with appropriate knowledge to transform their negative attitude and perception on COVID-19 vaccination.
BACKGROUND
Coronavirus disease (COVID-19) is an infectious condition caused by the severe acute respiratory syndrome corona virus type 2 (SARS-CoV-2) virus. It poses a higher risk of severe illness in older people and those with underlying medical conditions such as; cardiovascular disease, diabetes, chronic respiratory disease, or cancer. The virus spreads through small liquid particles expelled from the mouth or nose of an infected person when they cough, sneeze, speak, sing or breathe. These particles range from larger respiratory droplets to smaller aerosols.1
For decades, vaccinations have been considered the most effective method for control of rapidly spreading infectious diseases. To achieve the necessary herd immunity to control viral transmission and stop the pandemic, vaccinating more than 70% of the population is crucial and requires strong acceptance and low hesitation levels throughout the population.2 As COVID-19 vaccines are rolled out globally, vaccine hesitancy has stimulated public debates across social media and various multimedia platforms. The level of vaccine hesitancy and contributing factors significantly vary based on individual's location, background, and community.3,4 Being cognisant of factors contributing to vaccine hesitancy may help in developing strategies for delivering vaccine to the most vulnerable populations. Insufficient knowledge, negative attitudes and perceptions about COVID-19 vaccines contribute to vaccine hesitancy which lead to low immunisation coverage in most countries.4,5 Studies conducted around the world have indicated that knowledge, attitude and perception significantly influence uptake of COVID-19 vaccination.6–8 Scepticism towards vaccination is associated with minority ethnicity, lower levels of education, lower income, poor knowledge of COVID-19, and non-compliance with government COVID-19 guidelines.9–13 However, synthesis of data from 5 large scale surveys conducted in 22 countries across Southern, Eastern, Central and Western Africa showed that demographic factors have no clear impact on vaccine acceptance, although variations exist within country regions.14,15
Tanzania welcomed its first shipment of over one million doses of Johnson & Johnson COVID-19 vaccines in July 2021 from the United States as part of the COVAX arrangement. The first phase of the COVID-19 vaccination rollout which began in August 2021, prioritised frontline health workers, elderly (individuals aged 50 years and above) and those with chronic illnesses. Currently, 5 types of vaccines have been approved, received and distributed across the nation. Study conducted by Msuya et al16 highlighted a low vaccine uptake rate (18%) in Tanzania. However, the selection of the study sites was based on vaccine wastage rates might have biased the uptake estimates and undermined the factors which associate with vaccine uptake or hesitancy. Thus, this study employs a multistage random sampling of regions and councils to identify factors associated with varying levels of COVID-19 vaccine uptake among the general population and health workers.
METHODS
Study Design, Site and Population
A cross sectional study was conducted in 16 district and municipal councils in 8 regions to investigate the factors influencing COVID-19 vaccine uptake among the general population and health workers in Tanzania. The district and municipal councils which participated in this study included; Milele, Mpanda, Newala, Simanjiro, Nanyumbu, Muleba, Longido, Ulanga, Igunga, Mbulu, Karatu, Mufindi, Mvomero, Kilolo and Tabora Town.
Sample Size
Assuming that 50% of health workers possess comprehensive knowledge about COVID-19 vaccination, with a confidence level of 95% and a margin of error of 5%, the initial sample size calculated for healthcare providers was 384. Accounting for non-response of 15%, the sample was adjusted to 442. Based on the fact that 52.2% of the Tanzanian population possess good knowledge of COVID-19 vaccines17 and that 48.3% had inadequate knowledge on the causes of COVID-19,18 a decision was made to assume that 50% of the general population have some knowledge on COVID-19 vaccination. Setting the confidence level at 95% and a margin of error at 2.3%, the calculated sample size for the general population was 1,812. Considering a non-response of 10%, the sample was increased to 1,993.
Sampling Procedures
In Tanzania, there are 8 Health Sector Zones and 7 Administrative Zones. The study was about health issues, deemed appropriate to use Health Sector Zones. So, in each Health Sector Zone one region was randomly selected, comprising Arusha, Iringa, Kagera, Katavi, Manyara, Morogoro, Mtwara and Tabora. In each selected region, 2 councils were randomly selected.
Stratified by rural-urban classification, 1 ward was randomly selected from each stratum, giving a total of 32 wards. In each ward, four (4) villages/streets were randomly selected, leading to the sampling of 128 villages and streets for the entire study. In each selected village or street, 15 households were selected using simple random sampling techniques. In each selected household, one respondent aged 18 years or above was sampled for the interview. A total of 1,907 individuals were interviewed.
Eight region hospitals and 16 District Hospitals were purposefully sampled in the selected regions and councils respectively. Thirty-two (32) health centres and 64 dispensaries were randomly selected from respective lists of health centres and dispensaries in the councils. This resulted to a total of 120 health facilities participating in this study. Within each participating hospital, 6 health workers were sampled, and in each health centre, 4 health workers were sampled. At the dispensary level, up to 3 health workers were interviewed during each visit. Thus, in total 427 health workers were interviewed.
In the context of this study health workers included doctors, nurses, pharmacists, lobotomy technologists and technicians, health or medical attendants and all other individuals working at the health facilities.
Data Collection
A structured questionnaire was used to collect the required information from the study population. Initially crafted in English, the questionnaire was subsequently translated into Kiswahili. To ensure preservation of the meaning, the questions were back translated into English by an independent person.
Prior to commencing field work, all instruments were pre-tested in the non-survey site. Adjustments were made as necessary based on the findings of the pre-test. Data collection was carried out by trained Research Assistants (RAs) using Open Data Kit (ODK).
Assessment of Knowledge, Attitude and Perception on COVID-19 Vaccination
Knowledge about COVID-19 vaccination was assessed by 9 items (Table 1), each with 2 options, “yes” coded as 1 and “no” coded as 2. Respondents were requested to respond to statements which measured their knowledge on benefits of COVID-19 vaccination, delivery mode, side effects, importance of combining vaccination with other preventive measures and which population is targeted for vaccination. Knowledge score was computed by summing up the score for each item.19 Since there was one false statement, response codes were reversed before calculating the total knowledge score. Using the mean score, the overall knowledge score was dichotomised into comprehensive knowledge and limited knowledge.
TABLE 1:
Questions and Statements Used to Assess Knowledge, Attitude and Perception on COVID-19 Vaccination
| COVID-19 vaccination knowledge (9 items) | Attitude towards COVID-19 vaccination (8 items) | Perception on COVID-19 vaccination (10 items) |
|---|---|---|
| Do you know that COVID-19 Vaccine may protect you from adverse effects of the disease? | I will take the COVID-19 vaccine without any hesitation, if it is available at my neighbourhood | COVID-19 vaccines work |
| Are you aware that COVID-19 Vaccine is available free of charge at the health facilities in your community? | I will also encourage my family/friends/relatives to get vaccinated. | COVID-19 vaccines are safe for use in humans |
| Do you know that administration of COVID-19 vaccine may cause mild side effects? | It is not possible to reduce the incidence of COVID-19 without vaccination | COVID-19 vaccines have passed rigorous quality control for use |
| Can vaccinated person get infected with COVID-19? | The COVID-19 vaccine should be distributed fairly to all of us. | Benefits of COVID-19 vaccine outweighs the risks. |
| vaccine can be given to people who had been infected/sick with COVID-19? | If everyone in the society maintains the preventive measures, the COVID-19 pandemic can be eradicated without vaccination | Safety of COVID-19 vaccine is compromised by shorten time taken to develop and approve it |
| COVID-19 K13. A person who has received COVID-19 vaccine needs to continue following other preventive methods (e.g. distancing, hand washing, use of mask) | It is essential to vaccinate a large proportion of the population in order to defeat COVID-19 pandemic | The Ministry of Health has ensured that available vaccines in Tanzania are safe |
| COVID-19 vaccines can reduce the risk/chance of being infected with COVID-19? | COVID-19 vaccination can cause COVID-19 infections to a person | Fear of serious adverse events prevents me from taking COVID-19 vaccines |
| COVID-19 vaccines prevent severe infection? | COVID-19 vaccine provide a long-term protection against COVID-19 infection | Fear of side effects prevent me from taking COVID-19 vaccines |
| COVID-19 vaccines reduce deaths due to COVID-19? | Do not fully support the government move for vaccinating people against COVID-19 The COVID-19 vaccines is essential for us |
Attitude was assessed by 8 items (Table 1). The assessment focused on the respondent's assertiveness on willingness to be vaccinated or to encourage family member to be vaccinated, effect of COVID-19 on disease prevention, importance of vaccination and adherence to other preventive measures. A 5-point Likert scale was used to measure the extent to which respondent agreed or disagreed with each statement. If respondent strongly agreed with the statement a score of 1 was assigned to the respective statement. A score of 5 was given to the statement which respondent strongly disagree with. Two out of 8 were negative statements and therefore, their codes were reversed prior to computation of the attitude score. The attitude score was constructed by summing up the score for each item, and the mean score was used to dichotomise the overall score into positive and negative attitudes towards COVID-19 vaccination.19
Perception of COVID-19 vaccination focused on the use of the vaccine, trust in the precautionary measures implemented by the Ministry of Health to safeguard Tanzanians' health and concerns over the effectiveness and safety of the vaccine. The assessment of COVID-19 vaccination perception comprised of 10 items (Table 1). A 5-point Likert scale was used to measure the extent to which respondent agreed or disagreed with each statement. If respondent strongly agreed with the statement, a score of 1 was assigned to the respective statement. A score of 5 was given to the statement which respondent strongly disagreed with. The final score was obtained by summing up individual item scores, and the total score was dichotomised into positive and negative attitude using the Mean score as the cut-off point.20
To assess uptake of COVID-19 vaccine, respondents were asked if they have received COVID-19 vaccine. The response options were yes (coded 1) and no (coded 2).
Data Analysis
The collected independent variables included; social demographic characteristics, knowledge, perception and attitude towards COVID-19 vaccination. Uptake of COVID-19 vaccine was the dependent variable assessed. The collected quantitative data was processed in Statistical Software for Data Science (STATA) version 18.21
Data analysis involved describing the demographic characteristics of the participants and summarising categorical variables using percentages, along with mean and standard deviation for normally distributed data. Chi-squared analysis was used to compare proportions of individuals with knowledge, positive attitude and perception on COVID-19 vaccination against their counterpart groups.
For variable measured using the Likert scale, response options were re-categorised into agree or disagree. Scores for knowledge, attitude and perception towards COVID-19 vaccination were constructed, and then categorised into high and low knowledge, as well as positive and negative attitude and perception.
Principle Components Analysis (PCA) was performed to establish factor scores or domain variable for KAP, which were subsequently used in logistic regression analysis to explore the effects of KAP on COVID-19 vaccines uptake. Finally, logistic regression analysis was performed to identify factors which influencing the uptake of COVID-19 vaccines in Tanzania.
Ethical Considerations
This study was approved by the National Health Research Ethics Committee of Tanzania (Certificate reference number NIMR/HQ/R.8a/Vol.IX/3981). Study participants provided written informed consent before being enrolled for the study.
RESULTS
Demographics of Studied General Population and Health Workers
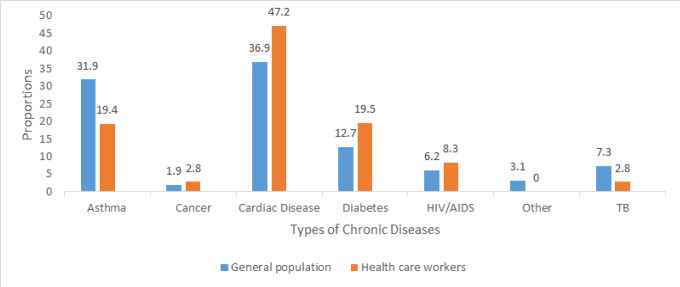
The response rate for the general population and Healthcare Workers (HWs) was 95.7% and 96.6% respectively. For both groups (general population and HWs), majority of respondents were aged between 18 and 49 years, married and residing in urbans (Table 2). Of the interviewed individuals 13.6% of the general population and 8.4% of HWs had history of chronic illnesses. Notably, a significantly high proportion of HWs (47.2%) and the general population (36.9%) had a history of cardiac disease (Figure 1).
TABLE 2:
Socio-demographics of Respondents
| Variables | General Population (N = 1907) n (%) | Health Workers (N = 427) n (%) |
|---|---|---|
| Age group (Years) | ||
| 18–29 | 512 (26.7) | 125 (29.3) |
| 30–39 | 574 (29.9) | 189 (44.3) |
| 40–49 | 421 (21.9) | 66 (15.5) |
| 50–59 | 250 (13.0) | 44 (10.3) |
| 60+ | 163 (8.5) | 3 (0.7) |
| Sex | ||
| Female | 1,034 (54.2) | 242 (56.7) |
| Male | 873 (45.8) | 185 (43.3) |
| Marital status | ||
| Cohabiting | 80 (4.2) | 4 (0.9) |
| Divorced/separated | 107 (5.6) | 8 (1.9) |
| Married | 1,300 (68.2) | 290 (67.9) |
| Single | 420 (22.0) | 125 (29.3) |
| Level of education | ||
| College/University | 116 (6.1) | - |
| No formal education | 191 (10.0) | - |
| Primary education | 1,177 (61.7) | - |
| Secondary Education | 423 (22.2) | - |
| Employment status | NA | |
| Government sector | 79 (4.1) | 422 |
| Housewife | 324 (17.0) | |
| Private Sector | 110 (5.8) | |
| Self employed | 1,035 (54.3) | |
| Student | 38 (2.0) | |
| Unemployed | 321 (16.8) | |
| Place of residence | ||
| Rural | 715 (37.5) | 146 (34.2) |
| Urban | 1,192 (62.5) | 281 (65.8) |
FIGURE 1:
Proportion of Respondents with Chronic Diseases
Given the nature of their job, almost all HWs (99.1%) believed that COVID-19 is present in Tanzania. Additionally, nearly two thirds reported administering COVID-19 vaccine to clients, but only 50% had received training on COVID-19 vaccine, and 35.4% believed that they were at high risk of contracting a COVID-19 infection (Table 3).
TABLE 3:
Family Member COVID-19 Experience and Mortality and Vaccine Uptake
| Variables | General Population (N = 1907) n (%) | Health Workers (N = 427) n (%) |
|---|---|---|
| Family member infected with COVID-19 | 132 (6.9) | 7 (18.1) |
| Family member died from COVID-19 | 24 (18.2) | 25 (32.5) |
| Received COVID-19 vaccine | 809 (42.4) | 394 (92.3) |
| Ready for vaccine booster dose | 732 (90.5) | 367 (93.1) |
| Ever received other vaccine | 1,517 (79.5) | 417 (97.7) |
| Agreed COVID-19 is present | 1725 (90.5) | 423 (99.1) |
Corona Virus Infection and COVID-19 Vaccine Uptake
A significantly higher percentage of HWs (18%) than the general population (6.9%) acknowledged to have had family members infected with COVID-19. Among those with infected family members, 32.5% of HWs and 18.2% of general population affirmed that the infected members had passed away (Table 3).
Majority of the general population (79.5%) and HWs (97.7%) reported having been vaccinated against other diseases and were ready for booster doses. However, compared to the general population (42.4%) a significantly high proportion of HWs (92.3%) claimed to have been vaccinated against COVID-19 (Table 3). Notably, 92.7% of HWs who believed that COVID-19 is present in the country were vaccinated against the disease, whereas only 50% of those who did not believe in the presence of the disease is in Tanzania received the vaccine.
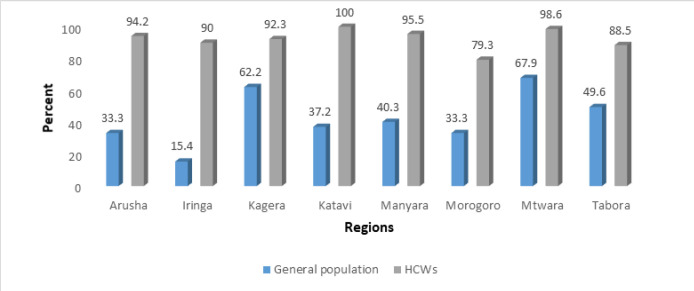
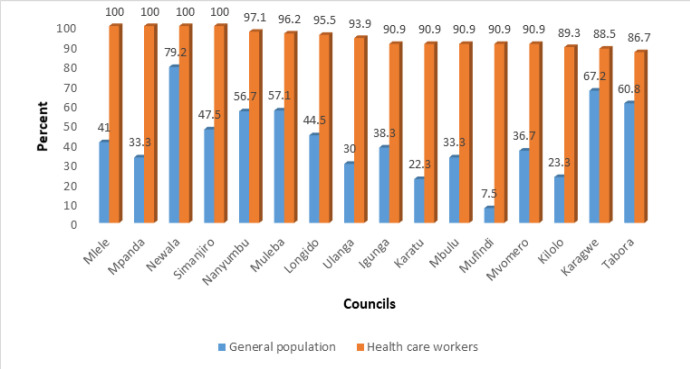
There is regional and district variation in the uptake of the COVID-19 vaccine, particularly among the general population. HWs in Morogoro demonstrated a lower uptake of COVID-19 vaccine compared to other regions (Figure 2). Self-reported uptake of COVID-19 vaccine was below 42% in half of the studied district councils, with only 7.5% of the general population in Mufundi reporting to have been vaccinated against COVID-19. Newala, Karagwe and Tabora district councils seemed to have good COVID-19 vaccine coverage compared to other studied district councils (Figure 3).
FIGURE 2:
Uptake of COVID-19 Vaccine among Health Workers and General Population by Region
FIGURE 3:
Uptake of COVID-19 Vaccine among Health Workers and General Population by Council
Knowledge on COVID-19 Vaccination
In general, HWs exhibited good knowledge regarding COVID-19 vaccine benefits and its side effects. The majority (94.6%) of HWs were aware that the administration of the COVID-19 vaccine may cause mild size effects.
In contrast, 54.9% of the general population possessed this knowledge. Additionally, slightly over half of the general population (53.4%) was unaware that a person who had received COVID-19 vaccine could still get infected with COVID-19 (Table 4). There was a significantly lower proportion of the general population (78.4%) compared to HWs (99.5%), who agreed that it is crucial to continue with other preventive methods even after receiving COVID-19 vaccine.
TABLE 4:
Health Workers' and General Population's Knowledge on COVID-19 Vaccination
| Knowledge Statement | General Population (N = 1907) | Health Workers (N = 427) |
|---|---|---|
| Administration of COVID-19 vaccine may cause mild side effects | 1,133 (59.4) | 404 (94.6) |
| Vaccinated person get infected with COVID-19 | 1,018 (53.4) | 390 (91.3) |
| COVID-19 vaccine administration to people infected with COVID-19 | 1,040 (54.5) | 371 (86.9) |
| Continuing with other preventive methods after receiving COVID-19 vaccine | 1,496 (78.4) | 425 (99.5) |
| COVID-19 vaccines reduce the risk of being infected | 1,387 (72.7) | 326 (76.3) |
| COVID-19 vaccines reduce deaths due to COVID-19 | 1,427 (74.8) | 422 (98.8) |
| COVID-19 vaccines prevent severe infections | 1371 (71.9) | 420 (98.4) |
Attitude Towards COVID-19 Vaccines
More than half of HWs (56.4%) and 41.1% of the general population believed that it is not possible to reduce the incidence of COVID-19 without vaccination. Furthermore, majority of both HWs and the general population agreed that COVID-19 vaccines should be fairly distributed to all. However, it is important to note that 57.9% of the general population and 83% of HWs believed that if everyone in the society adheres to and maintains preventive measures, the COVID-19 pandemic can be eradicated without vaccination. Whereas 71% of the general population felt that it is essential to vaccinate a large proportion of the population in order to defeat the COVID-19 pandemic, less than half of the HWs (48.9%) shared this belief. Interestingly, a substantial proportion of respondents believed that vaccine can cause COVID-19 infection to a person (Table 5).
TABLE 5:
Health Workers and General Population with Positive Attitude Towards COVID-19 Vaccination
| Statement | General Population n (%) | Health Workers n (%) |
|---|---|---|
| It is not possible to reduce the incidence of COVID-19 without vaccination | 783 (41.1) | 241 (56.4) |
| The COVID-19 vaccine should be distributed fairly to all of us. | 1392 (73.0) | 354 (82.9) |
| If everyone in the society maintains the preventive measures, the COVID-19 pandemic can be eradicated without vaccination | 1105 (57.9) | 354 (82.9) |
| It is essential to vaccinate a large proportion of the population in order to defeat COVID-19 pandemic | 1368 (71.7) | 209 (48.9) |
| COVID-19 vaccination can cause COVID-19 infections to a person | 501 (26.3) | 147 (34.4) |
| COVID-19 vaccine provide a long-term protection against COVID-19 infection | 1121 (58.8) | 341 (79.9) |
Perception on COVID-19 Vaccination
HWs perceived COVID-19 vaccine as effective (98.6%) and safe for use (97.4%). On the other hand, the general population was doubtful. Slightly above 50% and 48.6% of the general population believed that the vaccine is effective and safe respectively. Furthermore, only 52.1% of the general population thought that the benefits of COVID-19 vaccine outweigh the risks. Compared with the HWs (15%), significantly high proportion of the general population (34.3%) hesitate to take up CIVID-19 vaccine because of its side effects. Only 56% of the general population was willing to recommend or encourage a friend or relative to take up COVID-19 vaccine (Table 6).
TABLE 6:
Health Workers and General Population with Positive Perception on COVID-19 Vaccination
| Perception statements | General Population N (%) | Health Workers N (%) |
|---|---|---|
| COVID-19 vaccines work | 984 (51.6) | 421 (98.6) |
| COVID-19 vaccines are safe for use in humans | 927 (48.6) | 415 (97.2) |
| Routine vaccines are safer than COVID-19 vaccine | 734 (38.5) | 183 (41.9) |
| COVID-19 vaccines have passed rigorous quality control for use | 850 (44.60) | 379 (88.76) |
| Benefits of COVID-19 vaccine outweighs the risks | 994 (52.1) | 415 (97.2) |
| Shortcuts which are taken to develop and approve vaccines during a pandemic emergency compromise their safety | 436 (22.9) | 108 (25.3) |
| I trust that the Ministry of Health has ensured that the vaccines made available in Tanzania are safe | 1,037 (54.4) | 414 (97.0) |
| My concerns about related to side effects (minor/short term effects) prevent me from taking COVID-19 vaccine | 654 (34.3) | 64 (15.0) |
| The government is pushing you into a vaccination decision you do not fully support | 792 (41.5) | 30 (7.0) |
| The COVID-19 vaccines is essential for us | 1,097 (57.5) | 420 (98.4) |
| I will take the COVID-19 vaccine without any hesitation, if it is available at my neighbourhood | 1,020 (53.5) | 403 (94.4) |
| I will also encourage my family/friends/relatives to get vaccinated. | 1,068 (56.0) | 424 (99.3) |
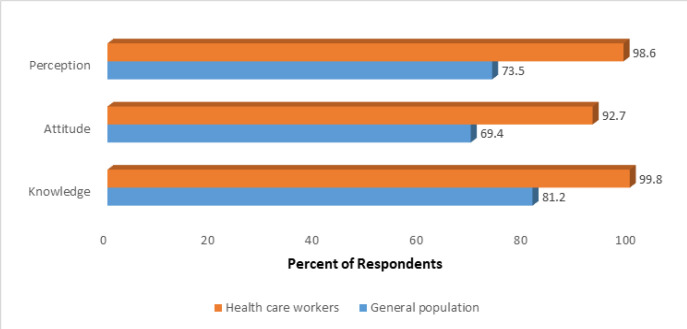
In generally, HWs exhibited a positive attitude and perception towards COVID-19 vaccine, and demonstrated greater knowledge compared to the general population (Figure 4). However, HWs' knowledge and perception regarding COVID-19 vaccine did not vary with socio-demographic factors. The attitude of HWs towards COVID-19 vaccination, however, varied with region and vaccination status against COVID-19. In Morogoro (81%) and Mtwara (88%), a lower proportion of HWs exhibited a positive attitude towards COVID-19 vaccination, compared to other regions (over 90%). HWs who received the COVID-19 vaccine (93.9%) were more likely to have positive attitude towards COVID-19 vaccination than those who did not vaccinate (78.8%). Among the general population, factors such as; age, marital status, education, region, COVID-19 vaccination status, employment status, family members' COVID-19 status, vaccination against other diseases status, belief in the presence of COVID-19 in the country and perceived risk played a role. Individuals aged 60+ years, those cohabiting, divorced/separated, with no formal education, unemployed, without family member affected by COVID-19, not vaccinated against COVID-19 or other diseases, not believing that COVID-19 is present in the country, and those with perceived low risk of being infected with COVID-19 were more likely to have limited knowledge, negative attitude and perception towards COVID-19 vaccination. Whereas non-HWs respondents from Arusha, Manyara, Mtwara were less likely to have positive attitude and perception towards COVID-19 vaccination, those in Tabora were more likely to have limited knowledge on COVID-19 vaccination (Table 7).
FIGURE 4:
Percent of Health Workers and General Population with Adequate Knowledge, and Positive Attitude and Perception on COVID-19 Vaccination
TABLE 7:
Knowledge, Attitude and Perception on COVID-19 Vaccine Among General Population by Sociodemographics
| Variables | Adequate knowledge | Positive attitude | Positive perception |
|---|---|---|---|
| Age | |||
| 18–29 | 421 (82.2) | 348 (67.9) | 384 (75.0) |
| 30–39 | 470 (81.9) | 409 (71.2) | 442 (77.0) |
| 40–49 | 353 (83.8) | 306 (72.7) | 313 (74.3) |
| 50–59 | 207 (82.8) | 177 (70.8) | 172 (68.80) |
| 60+ | 97 (64.7)** | 84 (56.0)** | 90 (60.0)** |
| Marital status | |||
| Cohabiting | 53 (66.2)** | 44 (55.0)** | 53 (66.25)** |
| Divorced/separated | 72 (67.3)** | 65 (60.7)** | 71 (66.36)** |
| Married | 1081 (83.1) | 917 (70.5) | 962 (74.0) |
| Single | 342 (81.4) | 298 (70.9) | 315 (75.0) |
| Vaccinated against COVID-19 | |||
| No | 772 (70.3)** | 614 (55.9)** | 739 (67.3)** |
| Yes | 776 (95.9) | 710 (87.8) | 662 (81.8) |
| Level of education | |||
| College/University | 112 (96.55) | 102 (87.9) | 85 (73.28) |
| No formal education | 100 (52.36)** | 73 (38.22)** | 107 (56.02)** |
| Primary education | 937 (79.61) | 798 (67.80) | 867 (73.66) |
| Secondary Education | 399 (94.33) | 351 (82.98) | 342 (80.85) |
| Employment status | |||
| Government sector | 76 (96.20) | 70 (88.6) | 57 (72.15) |
| Housewife | 229 (70.68)** | 189 (58.3)** | 223 (68.83)** |
| Private Sector | 103 (93.64) | 91 (82.7) | 81 (73.64) |
| Self employed | 872 (84.25) | 731 (70.6) | 779 (75.27) |
| Student | 36 (94.7) | 31 (81.6) | 32 (84.2) |
| Unemployed | 232 (72.3)** | 212 (66.0)** | 229 (71.3) |
| Family member been infected with COVID-19 | |||
| Do not Know | - | 26 (33.3)** | 38 (48.7) |
| No | 1421 (80.1)** | 1181 (69.6)** | 1268 (74.7) |
| Yes | 127 (96.2) | 117 (88.6) | 95 (71.9) |
| Received vaccine against other diseases | |||
| I do not know | - | ||
| No | 254 (65.1)** | 194 (49.7)** | 247 (63.3)* |
| Yes | 1294 (85.3) | 1130 (74.5) | 1154 (76.1) |
| Region | |||
| Arusha | 187 (77.9) | 135 (56.2)** | 133 (55.4)** |
| Iringa | 203 (84.6) | 178 (74.2) | 197 (82.1) |
| Kagera | 238 (100.0) | 233 (97.9) | 216 (90.8) |
| Katavi | 152 (65.8) | 162 (70.1) | 179 (77.5) |
| Manyara | 191 (80.2) | 141 (59.2)** | 157 (65.9)** |
| Morogoro | 196 (81.7) | 175 (72.9) | 202 (84.2) |
| Mtwara | 195 (81.2) | 133 (55.4)** | 178 (74.2) |
| Tabora | 186 (77.5)** | 167 (69.6) | 139 (57.9)** |
| COVID-19 is present in our country | |||
| No | 67 (36.8)** | 52 (28.6)** | 86 (47.25)** |
| Yes | 1481 (85.9) | 1272 (73.7) | 1315 (76.23) |
| Risk of getting COVID-19 infection | |||
| Low risk | 639 (77.5)** | 530 (64.3)** | 586 (71.12)** |
| High risk | 909 (83.9) | 974 (73.3) | 815 (75.25) |
P<0.001
Respondents from the general population who were separated/divorced (ARR= 0.8; 95% CI 0.7 to 0.9), had a primary level of education (ARR=0.8; 95% CI 0.7 to 0.9), were self-employed (ARR= 0.8; 95% CI 0.7 to 0.9) and unemployed (ARR= 0.7; 95% CI 0.6 to 0.8) were less likely to report being vaccinated with COVID-19 vaccine. Conversely, those with positive attitude (ARR=1.2; 95% CI 1.1 to 1.5), positive perception (ARR=1.8; 95% CI 1.5 to 2.2), and high knowledge (ARR= 3.0; 95% CI 2.1to 4.4)) on COVID-19 vaccination were more likely to be vaccinated than their counterparts. Respondents with history of chronic diseases (ARR=1.3; 95% CI1.2 to 1.4) and those who had received vaccine against other diseases (ARR=1.2; 95% CI1.0 to1.3) were also likely to be vaccinated. Additionally, respondents from general population who reported that their family members died of COVID-19 were more likely to be vaccinated against the disease (ARR=1.3; 95% CI 1.1to1.4) (Table 8).
TABLE 8:
Determinants of General Population's Uptake of COVID-19 Vaccine
| Variables | CRR (95% CI) | ARR (95% CI) |
|---|---|---|
| Marital status | ||
| Married | Ref | Ref |
| Cohabiting | 0.6 (0.4 – 0.9) | 0.8 (0.6 – 1.1) |
| Single | 1.0 (0.8 – 1.2) | 1.1 (0.9 – 1.3) |
| Divorced/separated | 0.6 (0.5 – 0.8) | 0.8 (0.7 – 0.9) |
| Level of education | ||
| College/University | Ref | Ref |
| No formal education | 0.6 (0.5 – 0.7) | 0.9 (0.7 – 1.1) |
| Primary education | 0.6 (0.5 – 0.7) | 0.8 (0.7 – 0.9) |
| Secondary Education | 0.8 (0.6 – 0.9) | 0.9 (0.8 – 1.1) |
| Employment status | ||
| Private Sector | Ref | Ref |
| Government sector | 1.4 (0.9 – 1.4) | 1.1 (0.9 – 1.3) |
| Housewife | 0.6 (0.5 – 0.8) | 0.9 (0.8 – 1.1) |
| Self employed | 0.6 (0.5 – 0.7) | 0.8 (0.7 – 0.9) |
| Student | 0.5 (0.4 – 0.6) | 0.7 (0.4 – 1.1) |
| Unemployed | 0.5 (0.4 – 0.6) | 0.7 (0.6 – 0.8) |
| History of chronic disease | ||
| No | Ref | Ref |
| Yes | 1.6 (1.4 – 1.8) | 1.3 (1.2 – 1.4) |
| Received vaccine for other diseases | ||
| No | Ref | Ref |
| Yes | 1.6 (1.3 – 1.8) | 1.2 (1.0 – 1.3) |
| Family members died from COVID-19 | ||
| No | Ref | Ref |
| Yes | 1.7 (1.5 – 1.9) | 1.3 (1.1 – 1.4) |
| COVID-19 vaccine knowledge | ||
| Low | Ref | Ref |
| High | 5.4 (3.9 – 7.6) | 3.0 (2.1 – 4.4) |
| Perception on COVID-19 vaccine | ||
| Negative | Ref | Ref |
| Positive | 1.6 (1.4 – 1.9) | 1.8 (1.5 – 2.2) |
| Attitude towards COVID-19 vaccine | ||
| Negative | Ref | Ref |
| Positive | 3.2 (2.6 – 3.8) | 1.2 (1.1 – 1.5) |
DISCUSSION
Vaccination against COVID-19 stands as a crucial and lifesaving preventive measure against the COVID-19 pandemic.16–19 Vaccinating at least 70% or more of the population is imperative for establishing herd immunity, reducing disease severity and mortality, and ultimately halting the epidemic.17,20,21 Despite the importance of vaccination, Tanzania's coverage of COVID-19 vaccination remains significantly low.
The 42% uptake of COVID-19 vaccine reported by the current study is higher than 18% reported by the study conducted in 6 regions of the Tanzanian mainland and 2 in Zanzibar between December 2021 and April 2022.16 The disparity may be attributed to the timing of the Msuya et al16 study, conducted during a period of heightened vaccine hesitancy among the general community members in Tanzania. Additionally, regions which participating in that study were selected based on the vaccine wastage rates, with regions experiencing high vaccine wastage demonstrating lower COVID-19 vaccine uptake. The current study was implemented between July and August, 2022 after the country had expanded its COVID-19 vaccination awareness campaigns and other outreach activities. Furthermore, and the National Vaccine Development Plan (NVDP) underwent revision to ensure that rural populations' access to vaccinations and enhance the capacity of health workers and facilities for vaccine delivery. Nevertheless, the reported COVID-19 vaccination coverage of 42% in this study falls below the global target of 70% and country target of 60%.
The heightened knowledge, and more favourable attitudes and perceptions on COVID-19 vaccination reported in this study may be the results of concerted efforts by the government and other stakeholders to raise community awareness about the importance of accepting the vaccine, in order to curtail the spread of the virus. Prior to these government intervention, people's perception towards COVID-19 vaccines was poor.22
Generally, HWs showed a higher likelihood of being vaccinated against COVID-19 compared to the general population, a trend possibly cushioned by their comprehensive knowledge, positive attitude and perception regarding COVID-19 vaccination. This may have offset the differences in uptake of COVID-19 vaccination among HWs belonging to various social, demographics and economic groups.
Numerous studies have reported low uptake of COVID-19 vaccine among specific groups including young individuals, females, those with low perceived risk of infection, low education level, low socio-economic status, and those holding negative attitude towards vaccines.16,17,21,24–31 Our study demonstrated that respondents from the general population who were separated/divorced, had reached primary level of education, self-employed or unemployed were less likely to report being vaccinated with COVID-19 vaccine.
Consistent with other studies,16,17,21, 24-31 our study confirms the role of social-demographic characteristics, knowledge, attitude and perception in shaping COVID-19 vaccination behaviour. Specifically, general population respondents with better knowledge, positive attitude and perception about COVID-19 vaccination were more likely to be vaccinated than their counterparts.
Contrary to Ahmed et al, who reported no significant difference in vaccine acceptance between medical professionals and the general population,32 our study revealed that almost all HWs had comprehensive knowledge, and positive attitude and perception on COVID-19 vaccination which may have increased their likelihood of being vaccinated compared to the general population.
Furthermore, while other studies showed that personal loss due to COVID-19 could deter vaccine acceptance,32 our study demonstrated an opposite trend. Individuals who had family member infected with or who died from COVID-19 were more likely to have received the vaccine, potentially motivated by the fear of personal infection or loss.
CONCLUSION
Uptake of COVID-19 vaccine among the general population was significantly low among individuals with primary level education, those who were self-employed, unemployed, and those who were divorced or separated. Individuals with comprehensive knowledge about COVID-19 vaccination, those with positive attitude and perception towards COVID-19 vaccination, having history of chronic diseases, prior vaccination against other diseases, and having a family member who succumbed to COVID-19 increased the likelihood of COVID-19 vaccine uptake among the general population. Provision of health education and implementation of socio-behavioural communication change interventions are necessary to equip the general population with the appropriate knowledge to transform their negative attitude and perception on COVID-19 vaccination. Moreover, refreshers training courses should be provided to health workers as a substantial proportion exhibited limited knowledge about COVID-19 vaccination.
Acknowledgments:
Ministry of Health and National Institute for Medical Research
Funding Statement
Funding: Ministry of Health through Global Fund.
Footnotes
Peer Reviewed
Competing Interests: None declared.
REFERENCES
- 1.https://www.who.int/health-topics/coronavirus#tab=tab_1 Accessed on 1st of February 2024
- 2.Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470–7. 10.3201/eid2607.200282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vasudevan, L. et al. (2020) ‘Parental concerns and uptake of childhood vaccines in rural Tanzania – a mixed methods study’. BMC Public Health, pp. 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thapar R, Kumar N, Surendran P, Shahdiya A, Mahendran Vet al. Vaccine hesitancy among mothers of under-five children in Coastal South India: a facility-based cross-sectional study. F1000Res. 2021. Sep 16; 10:186. Doi: 10.12688/f1000research.28293.2. PMCID: PMC8477350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Quinn, S. C. et al. (2021) ‘Willingness of Black and White Adults to Accept Vaccines in Development: An Exploratory Study Using National Survey Data’, American Journal of Health Promotion, 35(4), pp. 571–579. Doi: 10.1177/0890117120979918. [DOI] [PubMed] [Google Scholar]
- 6.Ciardi, F. et al. (2021) ‘Knowledge, attitudes and perceptions of covid-19 vaccination among healthcare workers of an inner-city hospital in New York’, Vaccines, 9(5), pp. 1–16. Doi: 10.3390/vaccines9050516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Zalfawi, S. M. et al. (2021) ‘Public knowledge, attitude, and perception towards COVID-19 vaccination in Saudi Arabia’, International Journal of Environmental Research and Public Health, 18(19). Doi: 10.3390/ijerph181910081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paul, E., Steptoe, A. and Fancourt, D.. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications', The Lancet Regional Health - Europe. Elsevier Ltd, 1. Doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed]
- 9.Islam, M. S. et al. Knowledge, attitudes and perceptions towards COVID-19 vaccinations: a cross-sectional community survey in Bangladesh. BMC Public Health. BMC Public Health, 21(1), pp. 1–11. Doi: 10.1186/s12889-021-11880-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mohamed NA, Solehan HM, Mohd Rani MD, Ithnin M, Che Isahak CI. Knowledge, acceptance and perception on COVID-19 vaccine among Malaysians: A web-based survey. PLoS One. 2021. Aug 13;16(8): e0256110. Doi: 10.1371/journal.pone.0256110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rivera-Lozada O, Galvez CA, Castro-Alzate E, Bonilla-Asalde CA. Factors associated with knowledge, attitudes and preventive practices towards COVID-19 in health care professionals in Lima, Peru. F1000Res. 2021. Jul 16; 10:582. Doi: 10.12688/f1000research.53689.3. PMID: 34804498; PMCID: PMC8567687. [DOI] [PMC free article] [PubMed]
- 12.Lau LL, Hung N, Go DJ, Ferma J, Choi M, Dodd W, Wei X. Knowledge, attitudes and practices of COVID-19 among income-poor households in the Philippines: A cross-sectional study. J Glob Health. 2020. Jun;10(1):011007. Doi: 10.7189/jogh.10.011007. PMID: 32566169; PMCID: PMC7294392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tulloch, O., Roldan de Jong, T. and Bardosh, K. (2021) Data Synthesis: COVID-19 Vaccine Perceptions in Africa: Social and Behavioural Science Data, March 2020-March 2021, Brighton: Social Science in Humanitarian Action (SSHAP) DOI: 10.19088/SSHAP.2028 [DOI]
- 14.Ekpenyong, B. N. et al. Knowledge, Attitudes, and Perceptions of COVID-19 Among Healthcare and Non-Healthcare Workers in Sub-Saharan Africa: A Web-Based Survey. Health security, 19(4), pp. 393–404. Doi: 10.1089/hs.2020.0208. [DOI] [PubMed] [Google Scholar]
- 15.Wong MCS, Wong ELY, Huang J, Cheung AWLet al. Acceptance of the COVID-19 vaccine based on the health belief model: a population-based survey in Hong Kong. Vaccine. 2021;39(7):1148–56. 10.1016/j.vaccine.2020.12.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Msuya SE, Manongi RN, Jonas N, Mtei M, Amour C, Mgongo MB, Bilakwate JSet al. COVID-19 Vaccine Uptake and Associated Factors in Sub-Saharan Africa: Evidence from a Community-Based Survey in Tanzania. Vaccines. 2023; 11(2):465. 10.3390/vaccines11020465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chilongola Jaffu O., Rwegoshola Kevin M., Balingumu Omary H., Semvua Hadija S., Kwigizile Edith T.. COVID-19 Knowledge, Attitudes, Practices, and vaccination hesitancy in Moshi, Kilimanjaro Region, Northern Tanzania. Tanzania Journal of Health Research 2020; 23 (1). 10.4314/thrb.v23i1.3 [DOI] [Google Scholar]
- 18.Mgongo Melina Bernard, Manongi Rachel N., Mboya Innocent B., Ngocho James S., Amour Caroline, Mtei Monica, Bilakwate Julieth S., Nyaki Ahmed Yusuph, George Johnston M., Leyaro Beatrice J., Farah Amina, Kengia James T., Tinuga Florian, Bakari Abdalla H., Kirakoya Fatimata B., Araya Awet, Kapologwe Ntuli A. & Msuya Sia E.. (2023) A Qualitative Study on Barriers to COVID-19 Vaccine Uptake among Community Members in Tanzania. Vaccines 11:8, pages 1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abdelhafz Ahmed Samir, Mohammed Zeinab, Ibrahim Maha Emad, Ziady Hany H., Alorabi Mohamed, Ayyad Mohamed, Sultan Eman A.. Knowledge, Perceptions, and Attitude of Egyptians Towards the Novel Coronavirus Disease (COVID-19). Journal of Community Health (2020) 45:881–890 10.1007/s10900-020-00827-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weitkunat R, Pottgieβer C, Meyer N, et al. Perceived Risk of Bovine Spongiform Encephalopathy and Dietary Behavior. Journal of Health Psychology. 2003;8(3):373–381. Doi: 10.1177/13591053030083007 [DOI] [PubMed] [Google Scholar]
- 21.StataCorp. 2023. Stata Statistical Software: Release 18. College Station, TX: StataCorp LLC. [Google Scholar]
- 22.Ackah, B.B.B.; Woo, M.; Stallwood, L.; Fazal, Z.A.; Okpani, A.; Ukah, U.V.; Adu, P.A.. COVID-19 vaccine hesitancy in Africa: A scoping review. Glob. Health Res. Policy 2022, 7, 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ayeni, G.O.; Idris, I.O.; Adebisi, Y.A.. Addressing the social issues around vaccination could be the pivotal strategy to achieve the 2022 COVID-19 vaccination coverage target. Ann. Med. Surg. 2022, 80, 104299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang, Y.; Wu, G.; Chen, S.; Ju, X.; Yimaer, W.; Zhang, W.; Lin, S.; Hao, Y.; Gu, J.; Li, J. A. review on COVID-19 transmission, epidemiological features, prevention and vaccination. Med. Rev. 2022, 2, 23–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ogunleye, O.O.; Godman, B.; Fadare, J.O.; Mudenda, S.; Adeoti, A.O.; Yinka-Ogunleye, A.F.; Ogundele, S.O.; Oyawole, M.R.; Schönfeldt, M.; Rashed, W.M.; et al. Coronavirus Disease 2019 (COVID-19) Pandemic across Africa: Current Status of Vaccinations and Implications for the Future. Vaccines 2022, 10, 1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lawal, L.; Bello, M.A.; Murwira, T.; Avoka, C.; Ma'Aruf, S.Y.; Omonhinmin, I.H.; Maluleke, P.; Tsagkaris, C.; Onyeaka, H.. Low coverage of COVID-19 vaccines in Africa: Current evidence and the way forward. Hum. Vaccines Immunother. 2022, 18, 2034457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kabakama, S.; Konje, E.T.; Dinga, J.N.; Kishamawe, C.; Morhason-Bello, I.; Hayombe, P.; Adeyemi, O.; Chimuka, E.; Lumu, I.; Amuasi, J.; et al. Commentary on COVID-19 Vaccine Hesitancy in sub-Saharan Africa. Trop. Med. Infect. Dis. 2022, 7, 130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hamisi, N.M., Dai, B. & Ibrahim, M.. Global Health Security amid COVID-19: Tanzanian government's response to the COVID-19 Pandemic. BMC Public Health 23, 205 (2023). 10.1186/s12889-023-14991-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davis, T.P.; Yimam, A.K.; Kalam, A.; Tolossa, A.D.; Kanwagi, R.; Bauler, S.; Kulathungam, L.; Larson, H.. Behavioural Determinants of COVID-19-Vaccine Acceptance in Rural Areas of Six Lower- and Middle-Income Countries. Vaccines 2022, 10, 214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Rabin, K.; Ratzan, S.C.; Leigh, J.P.; Hu, J.; El-Mohandes, A.. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat. Commun. 2022, 13, 3801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ahiakpa, J.K.; Cosmas, N.T.; Anyiam, F.E.; Enalume, K.O.; Lawan, I.; Gabriel, I.B.; Oforka, C.L.; Dahir, H.G.; Fausat, S.T.; Nwobodo, M.A.; et al. COVID-19 vaccines uptake: Public knowledge, awareness, perception and acceptance among adult Africans. PLoS ONE 2022, 17, e0268230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ahmed MH, Siraj SS, Klein J, Ali FY, Kanfe SG. Knowledge and attitude towards second COVID-19 vaccine dose among health professionals working at public health facilities in a low income country. Infect Drug Resist. 2021. Aug 12; 14:3125–3134. Doi: 10.2147/IDR.S327954. PMID: 34408455; PMCID: PMC8366936 [DOI] [PMC free article] [PubMed] [Google Scholar]