Abstract
Context:
Short implants are acceptable treatment options for atrophic ridges; however, they increase the crown-to-implant (C/I) ratio compared to regular length implants. The study aimed to assess the correlation between the C/I ratio and marginal bone loss (MBL) in single short implants at the posterior of the mandible.
Aims:
The study aimed to assess the correlation between the C/I ratio and MBL in single short implants at the posterior of the mandible.
Settings and Design:
Cross-sectional study.
Materials and Methods:
This cross-sectional study assessed short implants with 6 mm lengths at the posterior of the mandible. The long-cone peri-apical digital radiographs were taken immediately after loading and 24 months later. Age, gender, implant diameter, gingival biotype, and implant brands were the study variables, and the C/I ratio was the predictive factor. The mean MBL at 2 years was considered the study outcome.
Statistical Analysis Used:
The Pearson correlation test was applied to assess the correlation between MBL and C/I.
Results:
Seventy implants (36 Straumann and 34 SGS implants) were studied. A significant difference was observed in the mean MBL between the two implant brands (P < 0.001). Besides, a correlation was found between MBL and the C/I ratio (P = 0.002).
Conclusions:
It seems that the C/I ratio is associated with an MBL increase in single short implants at the posterior of the mandible.
Keywords: Alveolar bone loss, dental implants, mandible, osseointegration, short dental implant
INTRODUCTION
Short implants are acceptable treatment options for atrophic ridges. Short implants have similar survival to implants with 10 mm length or longer.[1,2,3] Short implants reduce the need for bone augmentation and have comparable outcomes to regular implants in the vertically augmented bone.[4] However, short implants increase the crown-to-implant (C/I) ratio compared to regular length implants.[5] It is expected that longer lever arms with higher C/I ratios lead to a non-axial force load and stress to the peri-implant bone.[6]
Despite a high C/I ratio, previous studies reported the promising outcomes of short implants.[7,8] Splinted crowns in two or more short implants are associated with a low marginal bone loss (MBL).[9] A few studies have investigated MBL in single short implants.[6]
This study was designed to investigate the effects of C/I ratio on MBL around a single short implant at the posterior of the mandible. We hypothesized that the high C/I ratio in a short implant is associated with an MBL increase. The study aimed to assess any correlation between C/I and MBL around a single short implant at the posterior of the mandible.
MATERIALS AND METHODS
The cross-sectional study sample was derived from patients referring to the Department of Oral and Maxillofacial Surgery and a private clinic to rehabilitate a partially edentulous area at the posterior of the mandible from September 1, 2017 to December 31, 2021.
Participants
Eligible subjects had an edentulous area at the posterior of the mandible with an insufficient bone height (<9 mm) undergoing short implant restoration. Subjects were excluded from the study if they had a deficient bone width, required horizontal bone augmentation, were smokers, had a systemic disease affecting bone metabolism, consumed any drugs or nasal spray affecting bone regeneration such as corticosteroids, failed to return for follow-up, or refused to enroll in the study. All participants were informed about the study design and objectives, and written informed consent was obtained from them. Finally, 70 patients enrolled in the study.
The Medical Ethics Committee approved the research (IR.SBMU.DRC.REC.1399.030). Also, the study design was consistent with the principles outlined by the World Medical Association’s Declaration of Helsinki on experiments involving human subjects, as revised in 2000.
Variables
The study variables were age, gender, implant diameter, gingival biotype, and implant brands. The C/I ratio was a predictive factor, and the mean MBL at 2 years was considered the study outcome.
Data sources/measurement
Surgical protocol
A crestal incision was made with two short-releasing incisions, and sub-periosteal dissection was done. The implant site was prepared according to the manufacturer’s guidelines. Two implant brands were used, including Straumann SP (Switzerland, Basal) with 4.8 and 4.1 mm diameters and SGS (Budapest, Hungary) with 4 and 4.5 mm diameters. Straumann implants were placed based on a one-stage protocol, and SGS implants were placed based on a two-stage protocol exposed 3 months after insertion.
Prosthetic protocol
All implants were loaded 4 months after insertion. The cemented crown was used. The crown length was measured and documented.
Radiographic and C/I evaluation
The subjects were radiographed (immediately after loading and 24 months later). A long-cone peri-apical digital radiograph (iRay D3, Dexcowin, South Korea) with 60 kV and 7 mA Dc in 0.20 s was applied. Individual bite blocks attached to the beam-guiding device (XCP, Rinn, Elgin, IL) were used to confirm the radiographs’ reproducibility. EMAGO/advanced 3.43 software (Oral Diagnostic Systems, Amsterdam, Netherlands) was applied to subtract images. The EMAGO program made the automatic gamma correction. The bone level was measured in the mesial and distal surfaces of the implants. MBL was measured at the mesial and distal aspects of implants by comparing the bone level on radiographs taken directly after loading and 24 months later [Figure 1]. If the MBL was different at the mesial and distal of implants, the mean MBL was reported. The bone level was measured from the alveolar crest to the implant collar. If implants had mobility, peri-implant radiolucency, and the presence of pus or infection, they were considered failed implants.
Figure 1.
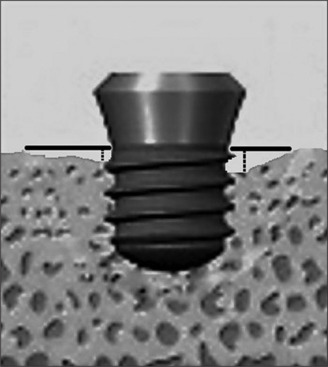
Schematic view of the measurement of marginal bone loss. The bone level was measured from the alveolar crest to the implant collar at the mesial and distal of implants
The C/I ratio was measured immediately after loading. Crown length was calculated as the distance between the occlusal edge of the crown and the level of bone around the implant collar in radiography. The implant length was also considered as the length of implant in the alveolar bone.
Gingival biotype
Thin and thick gingival biotypes (GBs) were categorized according to the transparency of a double-ended periodontal probe (Rolle, Ø 0.5 and 0.75 mm; DBS12 prototype, Deppeler SA, Switzerland). The peri-odontal probe prototype had two unequal thick endings. Transparency was evaluated through the gingival margin while probing the sulcus at the mid-buccal aspect of implants. The gingival biotype was considered thick if the thick probe ending was not evident through the tissue.
Sample size calculation
The sample size was calculated using the formula (r + 1) (Zα/2 + Z 1-β)2 σ2/rd2, where Zα/2 was considered 1.96 (type I error) at a 5% significance level and Z 1-β was 0.84 at 80% power (type II error). According to a similar study, σ (standard deviation) was 0.63 for MBL, and the sample size was 64.[9]
Bias
Two examiners calculated MBL in two sessions.
Statistical analysis
The statistical analyses were performed using SPSS for Windows, version 21 (IBM, USA). MBL and C/I correlation was assessed using the Pearson correlation test. The independent T test was applied to compare MBL between the two implant brands. We considered P values <0.05 statistically significant. The inter-examiner reliability analysis was done using the Kappa test to determine consistency between the two examiners.
RESULTS
Seventy implants (36 Straumann and 34 SGS implants) were studied. The mean age was 50.97 ± 8.96 years. The mean implants’ diameter was 4.25 ± 0.29 mm. The mean MBL was 0.51 ± 0.12 mm. The mean C/I ratio was 1.81 ± 0.21. Variables were compared between the two implant brands [Table 1]. The data analysis showed a significant difference in the mean MBL between the two implant brands (P < 0.001). Besides, the variables were compared between the two gingival biotypes [Table 2]. The results did not demonstrate any difference in the thick and thin gingival biotypes (P > 0.05). The comparison of variables did not show any difference between males and females (P > 0.05) [Table 3]. A correlation was found between MBL and the C/I ratio (P = 0.002) [Table 4]. The inter-rater reliability for the raters was 0.61 (P < 0.001), which indicated a substantial agreement between the examiners. Figure 2 shows a radiographic view of a short implant, immediately after load.
Table 1.
Comparison of study variables between Straumann implants and SGS implants
| Variables | Straumann implants | SGS implants | P |
|---|---|---|---|
| C/I ratio | 1.83±1.9 | 1.79±0.23 | 0.374* |
| Age (years) | 50.06±9.37 | 51.94±8.55 | 0.382* |
| Implant diameter (mm) | 4.31±0.33 | 4.19±0.25 | 0.080* |
| MBL (mm) | 0.43±0.07 | 0.59±0.10 | <0.001* |
| Gender | 17 males, 19 females | 17 males, 17 females | 0.503** |
C/I ratio: Crown/Implant ratio, MBL: Marginal bone loss, *Independent t-test **Chi-square test
Table 2.
Comparison of study variables between thick and thin gingiva biotypes
| Variables | Thick gingiva biotype | Thin gingiva biotype | P |
|---|---|---|---|
| C/I ratio | 1.82±0.22 | 1.79±0.18 | 0.315* |
| Age (years) | 51.20±9.29 | 50.19±8.01 | 0.671* |
| Implant diameter (mm) | 4.26±0.31 | 4.22±0.25 | 0.526* |
| MBL (mm) | 0.51±0.12 | 0.50±0.12 | 0.692* |
| Gender | 29 males, 25 females | 5 males, 11 females | 0.097** |
C/I ratio: Crown/Implant ratio, MBL: Marginal bone loss, *Independent t-test **Fisher’s exact test
Table 3.
Comparison of study variables between male and females
| Variables | Males | Females | Independent T-test |
|---|---|---|---|
| C/I ratio | 1.80±0.22 | 1.82±0.20 | P=0.744 |
| Age (years) | 50.94±8.98 | 51.00±9.07 | P=0.978 |
| Implant diameter (mm) | 4.24±0.29 | 4.27±0.31 | P=0.603 |
| MBL (mm) | 0.52±0.11 | 0.50±0.12 | P=0.692 |
C/I ratio: Crown/Implant ratio, MBL: Marginal bone loss
Table 4.
Correlation between variables and MBL
| Variables | Mean±SD | MBL (mm) | Pearson Correlation test | r |
|---|---|---|---|---|
| C/I ratio | 1.81±0.21 | 0.51±0.12 | P=0.002 | 0.37 |
| Age (years) | 50.97±8.97 | 0.51±0.12 | P=0.998 | 0.171 |
| Implant diameter (mm) | 4.25±30 | 0.51±0.12 | P=0.158 | 0.00 |
C/I ratio: Crown/Implant ratio, MBL: Marginal bone loss
Figure 2.

Radiographic view of a short implant placed at the posterior of mandible, immediately after load
DISCUSSION
Short implants are used widely for prosthetic rehabilitation of patients with inadequate bone heights to avoid risks and complications associated with advanced surgical procedures and achieve acceptable outcomes.[10] The increased C/I ratio is one of the main concerns in applying short implants.
Different studies have investigated the influence of the C/I ratio on marginal bone loss; some showed a positive correlation,[5,11] while others failed to show any correlation.[12,13,14] These controversies remain regarding short implants. Most studies concluded no significant correlation between the C/I ratio and MBL in short implants.[8,15,16,17,18,19,20] These studies used a heterogeneous sample of dental implants with different lengths and types.
Our study demonstrated a significant correlation between MBL and the C/I ratio, which is consistent with the results of Di Fiore et al.[21] They showed that a higher C/I ratio (≥2) was associated with greater MBL in short dental implants placed in the posterior mandible. Also, the study of Hingsammer et al.[22] showed a correlation between the C/I ratio and MBL in 76 homogeneous implants with a length of 6.5 mm and a diameter of 4.0 mm. They suggested that the C/I ratio should not exceed 1.7 to avoid increased early marginal bone loss.
One of the aspects that should be considered when interpreting the differences between studies is the splinting of restorations. Splinting the restoration can result in a better distribution of occlusal loads and reduced stress, which may cause lower marginal bone loss.[23,24] In some studies, the authors used both simple and splinted crowns,[5,8,19,20,23] but only one of them specified the number of short and standard implants that have been used.[8] The systematic review conducted by Pellizzer et al.[6] showed that MBL increased as the C/I ratio increased in single crowns, consistent with our study results.
Besides the increased C/I ratio, another aspect that may contribute to the increased marginal bone loss in our study is that all implants were loaded with cemented type crowns. A recent systematic review revealed increased biological complications with cemented crowns,[25] which are associated with excess cement.[26,27]
This study was conducted on short implants at the posterior of the mandible to ensure a homogeneous sample. Also, the long follow-up was one of the other strengths of this study. The limitations of our study were the small sample size and MBL measurement errors. Two examiners interpreted the radiographs to reduce these errors.
Within the limitations of our study, analytical measurements showed that the increased C/I ratio could increase MBL in single short dental implants at the posterior of the mandible. More studies with larger sample sizes and longer follow-ups are required for more definite conclusions in applying single short implants.
CONCLUSION
It seems that the C/I ratio is associated with an MBL increase in a single short implant at the posterior of the mandible.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rossi F, Lang NP, Ricci E, Ferraioli L, Baldi N, Botticelli D. Long-term follow-up of single crowns supported by short, moderately rough implants—A prospective 10-year cohort study. Clin Oral Implants Res. 2018;29:1212–9. doi: 10.1111/clr.13386. [DOI] [PubMed] [Google Scholar]
- 2.Ajayi YO, Nwachukwu N, Akinboboye BO. Treatment outcome of short dental implants. J West Afr Coll Surg. 2017;7:52–71. [PMC free article] [PubMed] [Google Scholar]
- 3.Caramês J, Pinto AC, Caramês G, Francisco H, Fialho J, Marques D. Survival rate of 1008 short dental implants with 21 months of average follow-up: A retrospective study. J Clin Med. 2020;9:3943. doi: 10.3390/jcm9123943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Terheyden H, Meijer GJ, Raghoebar GM. Vertical bone augmentation and regular implants versus short implants in the vertically deficient posterior mandible: A systematic review and meta-analysis of randomized studies. Int J Oral Maxillofac Surg. 2021;50:1249–58. doi: 10.1016/j.ijom.2021.01.005. [DOI] [PubMed] [Google Scholar]
- 5.Malchiodi L, Cucchi A, Ghensi P, Consonni D, Nocini PF. Influence of crown-implant ratio on implant success rates and crestal bone levels: A 36-month follow-up prospective study. Clin Oral Implants Res. 2014;25:240–51. doi: 10.1111/clr.12105. [DOI] [PubMed] [Google Scholar]
- 6.Pellizzer EP, Marcela de Luna Gomes J, Araújo Lemos CA, Minatel L, Justino de Oliveira Limírio JP, Dantas de Moraes SL. The influence of crown-to-implant ratio in single crowns on clinical outcomes: A systematic review and meta-analysis. J Prosthet Dent. 2021;126:497–502. doi: 10.1016/j.prosdent.2020.06.010. [DOI] [PubMed] [Google Scholar]
- 7.Tang Y, Yu H, Wang J, Gao M, Qiu L. Influence of crown-to-implant ratio and different prosthetic designs on the clinical conditions of short implants in posterior regions: A 4-year retrospective clinical and radiographic study. Clin Implant Dent Relat Res. 2020;22:119–27. doi: 10.1111/cid.12881. [DOI] [PubMed] [Google Scholar]
- 8.Guarnieri R, Di Nardo D, Gaimari G, Miccoli G, Testarelli L. Short vs. standard laser-microgrooved implants supporting single and splinted crowns: A prospective study with 3 years follow-up. J Prosthodont. 2019;28:e771–9. doi: 10.1111/jopr.12959. [DOI] [PubMed] [Google Scholar]
- 9.Tabrizi R, Arabion H, Aliabadi E, Hasanzadeh F. Does increasing the number of short implants reduce marginal bone loss in the posterior mandible? A prospective study. Br J Oral Maxillofac Surg. 2016;54:731–5. doi: 10.1016/j.bjoms.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 10.Rameh S, Menhall A, Younes R. Key factors influencing short implant success. Oral Maxillofac Surg. 2020;24:263–75. doi: 10.1007/s10006-020-00841-y. [DOI] [PubMed] [Google Scholar]
- 11.Naert I, Duyck J, Hosny M, Jacobs R, Quirynen M, van Steenberghe D. Evaluation of factors influencing the marginal bone stability around implants in the treatment of partial edentulism. Clin Implant Dent Relat Res. 2001;3:30–8. doi: 10.1111/j.1708-8208.2001.tb00126.x. [DOI] [PubMed] [Google Scholar]
- 12.Urdaneta RA, Rodriguez S, McNeil DC, Weed M, Chuang SK. The effect of increased crown-to-implant ratio on single-tooth locking-taper implants. Int J Oral Maxillofac Implants. 2010;25:729–43. [PubMed] [Google Scholar]
- 13.Okada S, Koretake K, Miyamoto Y, Oue H, Akagawa Y. Increased crown-to-implant ratio may not be a risk factor for dental implant failure under appropriate plaque control. PLoS One. 2013;8:e63992. doi: 10.1371/journal.pone.0063992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blanes RJ. To what extent does the crown-implant ratio affect the survival and complications of implant-supported reconstructions? A systematic review. Clin Oral Implants Res. 2009;20(Suppl 4):67–72. doi: 10.1111/j.1600-0501.2009.01762.x. [DOI] [PubMed] [Google Scholar]
- 15.Adánez MH, Brezavšček M, Vach K, Fonseca M, Att W. Clinical and radiographic evaluation of short implants placed in the posterior mandible: A 1-year pilot split-mouth study. J Oral Implantol. 2018;44:250–9. doi: 10.1563/aaid-joi-D-18-00037. [DOI] [PubMed] [Google Scholar]
- 16.Sahrmann P, Naenni N, Jung RE, Held U, Truninger T, Hämmerle CH, et al. Success of 6-mm implants with single-tooth restorations: A 3-year randomized controlled clinical trial. J Dent Res. 2016;95:623–8. doi: 10.1177/0022034516633432. [DOI] [PubMed] [Google Scholar]
- 17.Hadzik J, Krawiec M, Sławecki K, Kunert-Keil C, Dominiak M, Gedrange T. The Influence of the crown-implant ratio on the crestal bone level and implant secondary stability: 36-month clinical study. Biomed Res Int. 2018;2018:4246874. doi: 10.1155/2018/4246874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghariani L, Segaan L, Rayyan MM, Galli S, Jimbo R, Ibrahim A. Does crown/implant ratio influence the survival and marginal bone level of short single implants in the mandibular molar? A preliminary investigation consisting of 12 patients. J Oral Rehabil. 2016;43:127–35. doi: 10.1111/joor.12342. [DOI] [PubMed] [Google Scholar]
- 19.Malchiodi L, Caricasulo R, Cucchi A, Vinci R, Agliardi E, Gherlone E. Evaluation of ultrashort and longer implants with microrough surfaces: Results of a 24- to 36-month prospective study. Int J Oral Maxillofac Implants. 2017;32:171–9. doi: 10.11607/jomi.4648. [DOI] [PubMed] [Google Scholar]
- 20.Mangano F, Frezzato I, Frezzato A, Veronesi G, Mortellaro C, Mangano C. The effect of Crown-to-Implant ratio on the clinical performance of extra-short locking-taper implants. J Craniofac Surg. 2016;27:675–81. doi: 10.1097/SCS.0000000000002562. [DOI] [PubMed] [Google Scholar]
- 21.Di Fiore A, Vigolo P, Sivolella S, Cavallin F, Katsoulis J, Monaco C, et al. Influence of Crown-to-Implant Ratio on long-term marginal bone loss around short implants. Int J Oral Maxillofac Implants. 2019;34:992–8. doi: 10.11607/jomi.7161. [DOI] [PubMed] [Google Scholar]
- 22.Hingsammer L, Watzek G, Pommer B. The influence of crown-to-implant ratio on marginal bone levels around splinted short dental implants: A radiological and clincial short term analysis. Clin Implant Dent Relat Res. 2017;19:1090–8. doi: 10.1111/cid.12546. [DOI] [PubMed] [Google Scholar]
- 23.Blanes RJ, Bernard JP, Blanes ZM, Belser UC. A 10-year prospective study of ITI dental implants placed in the posterior region. I: Clinical and radiographic results. Clin Oral Implants Res. 2007;18:699–706. doi: 10.1111/j.1600-0501.2006.01306.x. [DOI] [PubMed] [Google Scholar]
- 24.Nissan J, Gross O, Ghelfan O, Priel I, Gross M, Chaushu G. The effect of splinting implant-supported restorations on stress distribution of different crown-implant ratios and crown height spaces. J Oral Maxillofac Surg. 2011;69:2990–4. doi: 10.1016/j.joms.2011.06.210. [DOI] [PubMed] [Google Scholar]
- 25.Sailer I, Mühlemann S, Zwahlen M, Hämmerle CH, Schneider D. Cemented and screw-retained implant reconstructions: A systematic review of the survival and complication rates. Clin Oral Implants Res. 2012;23(Suppl 6):163–201. doi: 10.1111/j.1600-0501.2012.02538.x. [DOI] [PubMed] [Google Scholar]
- 26.Bornstein MM, Schmid B, Belser UC, Lussi A, Buser D. Early loading of non-submerged titanium implants with a sandblasted and acid-etched surface. 5-year results of a prospective study in partially edentulous patients. Clin Oral Implants Res. 2005;16:631–8. doi: 10.1111/j.1600-0501.2005.01209.x. [DOI] [PubMed] [Google Scholar]
- 27.Abboud M, Koeck B, Stark H, Wahl G, Paillon R. Immediate loading of single-tooth implants in the posterior region. Int J Oral Maxillofac Implants. 2005;20:61–8. [PubMed] [Google Scholar]


