Abstract
Angiosarcomas are rare, accounting for only 1–2% of sarcomas in the head and neck region. We present an extremely rare case of primary non-radiation-induced angiosarcoma of the parotid with epithelioid morphology which required a tertiary center second opinion for its histological characteristics. We discuss the presentation, imaging, diagnosis, characteristics, and pathway of this case. As parotid lumps are common, a surgical sieve is required to rule out other possible conditions. Early correct diagnosis is crucial in conditions such as angiosarcomas due to their quick metastatic potential.
Keywords (3-10 MESH): Angiosarcoma, diagnosis, differential, head and neck neoplasms, maxillofacial abnormalities, parotid gland
INTRODUCTION
Angiosarcoma is defined by the World Health Organization classification of tumors (2005)[1] as “a malignant neoplasm of vascular phenotype whose constituent tumour cells have endothelial features.” Angiosarcomas are rare, accounting for only 1–2% of sarcomas in the head and neck region.[2] Unfortunately, 20–30% of patients with angiosarcoma present to the clinician with metastasis.[3] Angiosarcomas with epithelioid histological morphology are particularly rare and elderly men have a higher predilection to this malignancy. We present a case where an angiosarcoma of the parotid was misdiagnosed for temporomandibular joint (TMJ) dysfunction by the dentist.
CASE REPORT
A 92-year-old male patient was referred to our maxillofacial unit for a painful and clicking TMJ. As he was referred under the routine pathway, he was seen five–six weeks after referral complaining of a dislocated right jaw. Medically, he had a history of non-muscle invasive G3 pT1 bladder cancer treated with Bacillus Calmette-Guerin treatment in 2010, chronic kidney disease stage 4, coronary artery disease with a percutaneous coronary intervention to the left anterior descending artery in 2012, and took aspirin, simvastatin, amlodipine, doxazosin. He had no allergies. Clinically, there was a 3-cm diameter ill-defined firm but not tethered swelling over the right parotid region [Figure 1]. There was no facial nerve involvement.
Figure 1.

3cm ill-defined swelling of the right parotid
After an orthopantomogram(OPG) showed no abnormality in the right condylar region [Figure 2], a head and neck non-contrast magnetic resonance imaging (MRI) was requested which showed low signal focal lesions on T1 and high signal on T2 SPIR (fat suppression) sequences, with the largest in the inferior pole of the right parotid gland measuring 3.3 × 2.8 × 2.5cm and multiple significant lymph nodes in the neck bilaterally involving levels II–V. The findings suggested a lymphoproliferative process. A subsequent urgent core biopsy of the parotid showed necrotic fibrous tissue containing numerous vascular channels lined by enlarged endothelial cells. Atypical mitoses were seen and no native parotid tissue was identified. A tertiary center referral for a second opinion was required which further described a mitotically active tumor composed of polygonal cells with immunohistochemistry positive for CD31, CD34, and ERG with a high proliferation index (Ki-67). An angiosarcoma with epithelioid morphology was diagnosed. At his results appointment, he had right-sided House-Brackmann 3 facial weakness.
Figure 2.

Orthopantomogram(OPG) showing no obvious abnormality in the right condylar region and no obvious dental pathology on the right side
Head and neck MRI with contrast and computerized tomography (CT) thorax [Figure 3] were requested for staging and his case was presented to the Head and Neck Multidisciplinary Team. This new MRI [Figure 4] showed multiple predominantly superficial heterogenous ill-defined bilateral parotid masses with some deep involvement of the right parotid with the right side measuring 4 × 3.3 cm and extending to parapharyngeal fat with multiple bilateral lymph nodes and some soft tissue attenuation in the lung apices. There was no bony involvement. The CT chest showed multiple well-defined thin-walled cavities with adjacent ground glass changes. The tumor was staged as T2N2cM1. The patient was put on supportive care with the option of palliative radiotherapy. The patient deceased four months after referral by the dentist.
Figure 3.
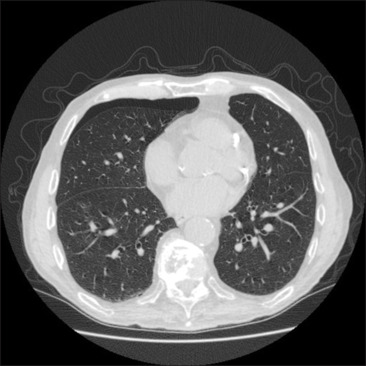
CT chest—multiple well-defined thin-walled cavities with adjacent ground glass changes
Figure 4.
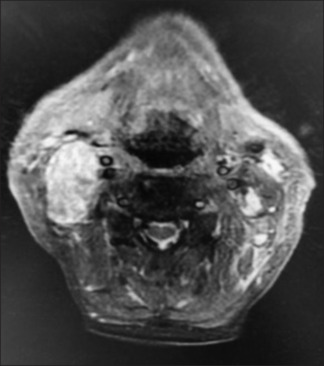
MRI head and neck showing right parotid mass
DISCUSSION
Angiosarcomas are rare and usually present as a painless mass. Some risk factors have been proposed such as trauma, ionizing radiation, and chronic lymphoedema,[4] and these should be queried when ascertaining a history. Most angiosarcomas arise post-irradiation due to the ionizing effects on the endothelial cells.[5] They have early metastatic potential, the most common site being the lungs.[6] Cervical lymph nodes should be palpated. Due to the proximity of the facial nerve to the parotid, a facial nerve examination should also be performed.
The most common imaging used to identify angiosarcomas are MRIs or CT scans though a definite diagnosis of an angiosarcoma requires a biopsy.[7] Epithelioid cells in the biopsy can make carcinoma a possible differential, therefore immunochemical stains—ERG, CD34, CD31, factor VIII, and vimentin are recommended.[2] Erythroblast transformation specific related gene (ERG) is expressed by angiosarcomas and other endothelial-derived malignancies but no other carcinomas other than prostatic adenocarcinoma.[8] CD31 is a protein, which is usually found on endothelial cells. As malignant endothelial cells retain CD31, testing for CD31 can demonstrate angiosarcomas. The CD34 marker is not specific for vascular differentiation and can stain for other sarcomas and meningiomas.[8] As angiosarcomas are rarely aspirated and difficult to diagnose with fine needle aspiration,[9] a core biopsy was ordered in this case. Core biopsy provides histological structure compared to fine needle aspiration which shows cells. Early and correct diagnosis is important as the 5-year survival rate is about 15 percent.[6]
The median survival of patients who have no treatment is 7 months.[4] Treatment involves surgery+/-radiotherapy+/-chemotherapy. In a longitudinal study of 28 patients treated for head and neck angiosarcoma with a median follow-up of 32 months, 67% of surgically treated patients with adjuvant radiotherapy +/-chemotherapy were disease-free compared to 8% of patients who were surgically treated only.[10] Common chemotherapy drugs include doxorubicine or paclitaxel. Prognosis is poor and there is a high rate of recurrence and incomplete excision[7] likely due the anatomical location and skip lesions. Satellite lesions are possible[6] and surgical margins should be two–five cm.[4] This is often difficult in the head and neck due to vital structures. Deep margins are also an important consideration. In the retrospective study of 14 patients surgically treated for angiosarcoma by Choi et al. (2015)[6], of all the risk factors, only deep margins were significantly associated with recurrence.
As parotid lumps are common, it is always important to have a surgical sieve. Early correct diagnosis is crucial in conditions such as angiosarcomas. Differential diagnoses of parotid lumps include pleomorphic adenoma, Warthin’s tumor, adenoid cystic carcinoma, lymph node metastasis from the scalp or face, mucoepidermoid carcinoma, lymphoma, infection, sialocele. Other reported differential diagnoses of angiosarcomas in the parotid region include haemangiomas, Kaposi sarcomas, and pyogenic granulomas.[10]
We present a rare case of primary non-radiation-induced angiosarcoma of the parotid with epithelioid morphology which was highly aggressive and needed a second opinion for its histological characteristics. We discuss the presentation, imaging, diagnosis, characteristics, and pathway of this case.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initial s will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
*This case was presented as an oral presentation at the fourth Edition International Conference on Dentistry and Oral Health on September 2021 (online due to COVID-19).
REFERENCES
- 1.El-Naggar AK, Chan CJK, Grandis RJ, Takata T, Slootweg PJ. Lyon, France: International Agency for Research on Cancer (IARC); 2017. WHO classification of head and neck tumours. [Google Scholar]
- 2.Ducharne-Asuaje E, Dorion D, Lamarre L, Coindre JM, Geha S. Primary high-grade poorly differentiated angiosarcoma of an intra-parotid lymph node. Head Neck Pathol. 2016;10:225–8. doi: 10.1007/s12105-015-0631-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Florou V, Wilky BA. Current and future directions for angiosarcoma therapy. Curr Treat Options Oncol. 2018;19:14. doi: 10.1007/s11864-018-0531-3. [DOI] [PubMed] [Google Scholar]
- 4.Issara K, Boughaleb Z, Tawfiq N, Bouchbika Z, Benchakroun N, Jouhadi H, et al. Un cas d’angiosarcome de l’oreille externe. Pan Afr Med J. 2016;24:117. doi: 10.11604/pamj.2016.24.177.9834. doi: 10.11604/pamj.2016.24.177.9834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Damiani S, Salfi NC, Collina G, Neri F. Angiosarcoma of the parotid gland arising in congenital nonirradiated hemangioma. A case with adverse outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endodo. 2004;97:665–6. doi: 10.1016/j.tripleo.2004.03.021. [DOI] [PubMed] [Google Scholar]
- 6.Choi JH, Ahn KC, Chang H, Minn KW, Jin US, Kim BJ. Surgical treatment and prognosis of angiosarcoma of the scalp: A retrospective analysis of 14 patients in a single institution. BioMed Res Int. 2015;2015:321896. doi: 10.1155/2015/321896. doi: 10.1155/2015/321896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buraïma F, Kouassi YM, Coulibaly AS, Touré A, Tanon-anoh M, Kouassi B. A case of middle-ear angiosarcoma. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128:87–9. doi: 10.1016/j.anorl.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 8.Sullivan HC, Edgar MA, Cohen C, Kovach CK, HooKim K, Reid MD. The utility of ERG, CD31 and CD34 in the cytological diagnosis of angiosarcoma: An analysis of 25 cases. J Clin Pathol. 2015;68:44–50. doi: 10.1136/jclinpath-2014-202629. [DOI] [PubMed] [Google Scholar]
- 9.Geller RL, Hookim K, Sullivan HC, Stuart LN, Edgar MA, Reid MD. Cytologic features of angiosarcoma: A review of 26 cases diagnosed on FNA. Cancer Cytopathol. 2016;124:659–68. doi: 10.1002/cncy.21726. [DOI] [PubMed] [Google Scholar]
- 10.Gru AA, Becker N, Pfeifer JD. Angiosarcoma of the parotid gland with at (12; 22) translocation creating a EWSR1–ATF1 fusion: A diagnostic dilemma. J Clin Pathol. 2013;66:452–4. doi: 10.1136/jclinpath-2012-201433. [DOI] [PubMed] [Google Scholar]


