Abstract
Purpose of review
Adolescent wrestlers undergo intense physical combat. While guidelines are effective in keeping the sport safer, concerns specific to the adolescent wrestler may be missed at primary care visits without knowledge of the unique challenges faced by these athletes. The following review highlights important characteristics of the adolescent wrestler which are of interest to primary care providers.
Recent findings
Recommendations for concussion management are evolving to gradual return-to-sport after physician clearance rather than total sport removal. Prolonged skin-to-skin contact also places athletes at greater risk of dermatologic infections, which often require removal from competition, treatment, and/or coverage. Finally, adolescent nutritional literature recommends limiting pre-match weight loss to 3–5% body weight due to noted kidney damage that may result from larger deficits.
Summary
Adolescent wrestlers are more prone to acute injuries than chronic overuse injuries, with most injuries occurring above the trunk. Primary care providers should consider obtaining imaging to rule out severe injuries or referring to specialist providers.
Current guidelines for skin infections require frequent pre-match skin checks and mandatory waiting periods when certain infections are identified. However, the primary care provider is well-equipped for more in-depth skin examination, discussion of skin hygiene, and appropriate treatment of skin infections.
Athletes attempting to meet lower weight classes may put themselves at risk of acute kidney damage, under-fueling, and eating disorders. Current guidelines attempt to mitigate excessive weight changes in the adolescent wrestler during competition season, but primary care providers should emphasize healthier methods of weight fluctuation and look for indicators of physiological or psychological effects.
Keywords: Pediatric, Wrestler, Primary care, Nutrition, Sports injury, Skin infections
Introduction
Wrestling, one of the world’s oldest sports, is a popular activity for adolescent athletes. This sport requires extreme dedication to training and fitness due to difficult maneuvers and stringent weight classes. Takedowns involve dropping an opponent from a standing position to the mat with high intensity, speed, and force, and are often emphasized in wrestling due to the increased scoring opportunity [1, 2]. The array of skilled moves, close proximity of opponents, and fitness requirements also result in the potential for high-impact injuries, communicable diseases/infections, and insufficient nutrition (Fig. 1). The purpose of the following review is to highlight important health consequences that wrestlers may experience which are of interest to primary care providers.
Fig. 1.

Two male wrestlers during a match. Attribution: EveryonephotoStudio/Sutterstock.com
Musculoskeletal
Musculoskeletal (MSK) injuries are a common concern in adolescent wrestlers. Boys wrestling exhibits the second highest rate of acute injuries compared to other boys sports [3]. Adolescent wrestlers are at high risk for acute injuries, particularly above the waist, and are at lower risk for overuse injuries [3]. Injuries in wrestling occur equally in practice and in competition [3–8]. Given the variability of moves in wrestling, the exact mechanism of injury can be hard to identify. Direct blows or forces (42%) and twisting forces (23%) are reported to be the most common mechanisms of injury [6]. These mechanisms occur most commonly in the takedown position (68%) or when an athlete is at a disadvantage [1, 6]. The wrestler defending the takedown is typically at the greatest injury risk due to increased effort in order to protect themselves from the disadvantage [1]. During takedowns and other moves, the most common injuries in pediatric wrestling include muscle strains, joint sprains, concussions, contusions, and abrasions or lacerations.
Head
Concussions, facial traumas, and auricular hematomas are commonly seen in wrestling. Concussions often result from head-to-head or head-to-knee collisions during takedowns but can also result from contact with the mat and floor [1]. Any wrestler with a head injury should also be evaluated for a neck injury [1]. Facial lacerations, nose bleeds, minor abrasions, and dental traumas can occur frequently, especially when an athlete has braces [1]. An auricular hematoma is a collection of blood underneath the perichondrium of the ear that results secondary to trauma [9]. Auricular hematomas most often occurs when wrestlers do not wear appropriate head gear or wear it improperly [1]. Auricular hematomas less than seven days old should be drained as soon as possible, and clinicians should consult with ENT or sports physicians for further guidance and management [10]. When these types of hematomas are not properly drained, left untreated, or reoccur, they can result in what is known as “cauliflower ear” or “wrestler's ear”. Cauliflower ear is the permanent deformity caused by overgrowth in fibrocartilage [11]. When auricular hematomas advance to this point, it is recommended to consult an otolaryngologist or plastic surgeon [12].
Spine/Trunk
Wrestling is the second most frequent sport to suffer cervical spine injuries, defined as any injury to the cervical spinal cord, bones, nerves, or supporting structures of the cervical spine including muscles, ligaments, and tendons [13]. Of the cervical spinal injuries observed in wrestling, cervical strains, cervical cord neuropraxia and lumbosacral spondylolisthesis are the most common, with catastrophic spinal cord injuries occurring very rarely. Though less common of the three, cervical cord neurapraxia is a transient neurological deficit following trauma to the cervical spinal cord due to hyperextensions, hyperflexion, or axial load mechanism which typically resolves in 15 min to 48 h [1, 14, 15]. Lumbosacral spondylolisthesis is a condition where the fifth lumbar vertebra (L5) translates forward over the first sacral vertebra (S1) [16]. This injury often occurs in children and adolescents who participate in a sport that requires repetitive lower back hyperextensions, such as wrestling. Spondylolysis and lumbar strains are additional low back injuries seen in young wrestlers which can occur in extension against resistance, such as lifting an opponent off the mat, and in hyperflexion and twisting, such as during rolling [1, 17]. In the instance of any cervical neck injury, it is important to ensure patients do not have numbness, tingling, or paresthesia which could be indicative of a more severe injury. These symptoms often require immediate stabilization and further imaging often in the emergency room setting [18]. Furthermore, the National Emergency X-Radiography Utilization Study (NEXUS) criteria and the Canadian C-Spine Rules are helpful tools in examining the patient to determine if additional imaging is warranted [19, 20]. In addition to spinal injuries, common rib injuries seen in wrestlers include contusions, costochondral sprains, and rib fractures as a result of direct or indirect trauma [1].
Shoulder
Shoulders are amongst the most common regions to be injured in the sport of wrestling [6]. Shoulder injuries include rotator cuff muscle strains, acromioclavicular (AC) joint separations, shoulder subluxations or dislocations, and shoulder contusions [6]. In addition, ruptures of the pectoralis major, injuries to the suprascapular nerve and suprascapular tendon, avulsion fractures to the scapula and lesser tuberosity, and clavicle fractures may be sustained [1, 21]. Wrestlers will often present in pain and with immobilization of their arm and shoulder. Radiographs can rule out dislocation or fracture (Fig. 2). In the case of a dislocation, the shoulder should be relocated as soon as possible to limit muscular spasms and neurovascular injury [22]. Athletes with a history of shoulder dislocations may be candidates for orthopedic referral.
Fig. 2.
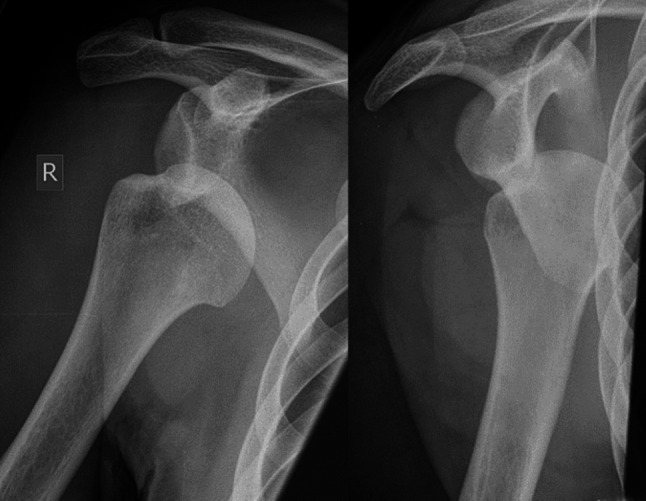
Dislocated right shoulder visible on a radiograph. Notice the displacement of the humeral head relative to the glenoid. Attribution: Hellerhoff, CC BY-SA 4.0 < https://creativecommons.org/licenses/by-sa/4.0 > , via Wikimedia Commons. Feburary 1, 2017.
Available at: https://commons.wikimedia.org/wiki/File:X-Ray_of_Dislocated_Shoulder.jpg. Accessed May 28, 2024
Elbow
Sprains are the most common elbow injury in wrestling and result from hyperextension and abduction of the joint. Sprains of this mechanism affect the ulnar collateral ligament and the anterior capsule of the elbow. The general mechanism of injury that can result in a sprain or elbow dislocation is when the wrestler encounters the playing surface followed by contact with another player [23]. Standard clinical practice for elbow dislocations involves radiographs which can assess for elbow reduction and also rule out fractures that can be associated with dislocations. Orthopedic consultation can aid in reduction and continued management after a dislocation event [24]. The skeletally immature population appears to be more susceptible to elbow dislocation with an associated avulsion fracture [1] (Fig. 3). Various types of avulsion fractures about the elbow include medial epicondyle and olecranon avulsions [1, 24]. Opinion varies on conservative verses surgical management for different avulsion fracture injuries. These should be stabilized and referred over to an orthopedic or sports medicine provider for further treatment [24, 25].
Fig. 3.

Epicondyle avulsion on a right elbow visible on a radiograph
Hand/Wrist
While hand and wrist injuries are less frequently reported in wrestlers, fractures, contusions, and ligament sprains do occur [1, 25]. Common sprains include metacarpophalangeal sprains, proximal interphalangeal sprains, and thumb metacarpophalangeal ulnar collateral ligament sprains [1]. Hand injuries are most likely to occur as the result of player-to-player contact followed by player-to-mat contact [25].
Lower Extremity
Lower extremity injuries in adolescent wrestlers are consistently less common than upper extremity injuries [6, 26, 27]. Knee injuries are the most frequently sustained lower extremity injuries [6, 27, 28]. Yard et al. (2007) noted that 15.4% of high school wrestling injuries occurred in the knee, with the knee as the site of 7% of all strains and sprains. Similarly, Pasque & Hewett (2000) found that 17% of total injuries in high school wrestlers were of the knee, including contusions, meniscus tears, ligament tears, prepatellar bursitis, and patellar tendonitis. They also noted that 44% of season-ending injuries occurred in the knee, with meniscus tears as a particularly common cause [6]. Ankle injuries were also common lower extremity injuries, with ankle sprains reported to comprise 7.6% of all injuries and 38% of all joint sprains in high school wrestlers [6, 27]. Any concern for meniscus injuries or significant ligamentous injuries (i.e. ACL) should be referred to an orthopedic or sports medicine specialist for advanced imaging and further management.
Prevention of injury
Given the full-body involvement of wrestling, injuries can affect any region of the body. Strategies to help limit or prevent injuries should be considered. Strategies such as implementing controlled drill simulations and training scenarios for high-risk maneuvers and encouraging coaches to emphasize proper wrestling technique may assist in injury prevention [2, 23]. Moreover, encouraging referees to strictly enforce penalties for slamming and dangerous holds helps reduce acute contact injuries [2]. Primary care physicians may emphasize sufficient warming up and stretching before matches, the use of proper technique, and participation in conditioning programs as general injury-prevention strategies for the adolescent wrestler [29]. While minor injuries are considered part of the sport for many adolescent wrestlers, any concern for more severe injuries – such as concussions, nerve injury, recurrent joint instability, and ligament tears – may benefit from referral to a specialist.
Skin Infections
Skin infections pose a unique hazard in adolescent wrestling with nearly 74% of all high school athletic-based skin infections occurring amongst wrestlers [30]. Moreover, one in five wrestlers are temporarily removed from practice or competition each year due to skin infections [31]. The prevalence of skin infections amongst athletes in combat sports such as wrestling has given rise to a unique naming system for these infections coined gladiatorum infections [32]. While vectors of these pathogens can be quite varied, direct skin-skin contact with other athletes is suggested to be the primary mechanism and is further exacerbated by the high proportion of exposed skin on the face, neck, and extremities [33]. However, while not the primary vector, these pathogens can also survive on wrestling mats, gymnasium floors, equipment, and many other surfaces to which wrestlers are frequently exposed, making infection control particularly challenging and of concern for clinicians caring for these athletes [34].
As a first step, providers should recommend showers and/or handwashing after practice, frequent uniform washing, and adherence to guidelines by pertinent regulatory organizations to minimize pathogen transmission.
The National Collegiate Athletic Association (NCAA) and National Federation of State High School Associations (NFHS) have established regulations that restrict sport participation due to cutaneous infection. Naturally, it is prudent for clinicians seeing this patient population to be aware of these guidelines and how they may affect their patients’ athletic participation. While often generalizable, individual states and municipalities may adhere entirely or partially to these guidelines and variations to these protocols exist at the local and state level. In general, guidelines are based on factors such as time since last lesion formation, total hours of pharmacotherapy, and hardening of lesion surfaces.
Knowledge of common skin infections – whether bacterial, fungal, or viral in nature – is essential for clinicians caring for adolescent wrestlers. Prompt identification accompanied by aggressive treatment is not only imperative to get the wrestler back to activity, it is important for community health and to prevent long term complications associated with latent infections in individuals [35].
Herpes gladiatorum
Herpes gladiatorum predominantly results from herpes simplex virus (HSV) type 1 infection, as shown in Fig. 4, and will typically yield symptoms within eight days of exposure with roughly 70% of infections presenting on the face, called herpes labialis. [35]. Patients with herpes labialis often report localizable facial pain accompanied by pharyngitis and a high fever as precursors to the vesicular outbreak. Regional lymphadenopathy presenting with these infections is of note to differentiate them from other skin infections such as folliculitis and cellulitis [35]. HSV has historically been poorly diagnosed by clinicians at initial presentation with some studies reporting as little as 10% accuracy [36]. Physicians may begin treatment for HSV if suspected on exam before confirmatory polymerase chain reaction (PCR) testing is performed.
Fig. 4.

Herpes gladiatorum located on the lateral aspect of the neck. Attribution: No machine-readable author provided. Gentgeen assumed (based on copyright claims)., CC BY-SA 3.0 < http://creativecommons.org/licenses/by-sa/3.0/ > , via Wikimedia Commons. May 6, 2006.
Available at: https://commons.wikimedia.org/wiki/File:Herpes_zoster_neck.png. Accessed May 29, 2024
Primary infection symptoms will often resolve within 14 days without intervention, however three times daily acyclovir or valacyclovir for 5–10 days can aid recovery and, importantly, limit transmission [31, 37]. Once the primary outbreak has passed, HSV will frequently lie dormant in the trigeminal ganglia, and the patient will be at risk for infection resurgence [38]. Prophylactic use of valacyclovir has been indicated for wrestlers > 12 years old with prior HSV infections to resist reactivation [37, 39]. Effective prophylactic regimens consist of once daily valacyclovir or twice daily acyclovir or famciclovir [37].
Tinea gladiatorum (ringworm)
The dermatophyte Trichophyton tonsurans has historically been the causative agent of this condition yielding the vast majority (92%) of infections [40]. Infections are generally in the trunk (tinea corporis) however can be dispersed across several areas including the feet (tinea pedis), head (tinea capitis), and groin (tinea cruris). Clinical presentation is a slightly raised, erythematous, annular lesion with a leading edge and central clearing (Fig. 5). Clinical caution must be taken to differentiate this from impetigo or common skin abrasions wrestlers experience from mat surfaces or equipment.
Fig. 5.

Erythematous tinea gladiatorum annular lesion. Attribution: Corina G., Public domain, via Wikimedia Commons. October 6, 2012.
Available at: https://commons.wikimedia.org/wiki/File:Tinea_corporis.png. Accessed May 29, 2024
A variety of antifungal topical therapeutics have been indicated as the primary treatment for tinea in adults and adolescents consisting of terbinafine, itraconazole, ketoconazole, clotrimazole, and miconazole applied 1–2 times daily for a period of 2–4 weeks [31, 41]. However, systemic treatment such as griseofulvin and terbinafine are prescribed in children with weight-based dosage when there is widespread involvement or areas difficult to treat with topical therapeutics [31].
Cellulitis and Methicillin-Resistant Staphylococcus Aureus (MRSA)
Cellulitis typically stems from Streptococci or Staphylococci infection resulting in diffuse patches of erythematous skin with subcutaneous edema [37]. However, while MRSA based infections are also Staphylococci based, they can be difficult to treat given their resistance and a challenge to differentiate from other skin infections as they often present as non-specific purulent lesions mimicking many other bacteria.
Typical cellulitis can be managed successfully through cephalexin or azithromycin 2–4 × daily for 5–10 days [38]. Particularly with MRSA treatment, local resistance trends should be considered with antibiotic selection. Topical mupirocin 2% ointment applied three times daily can treat smaller and localized infections. Oral regimens in children and adults often consist of clindamycin or trimethoprim/sulfamethoxazole. Newer antibiotics such as linezolid can be taken orally in the setting of antibiotic resistance or allergy. (38) Bacterial cultures are recommended for skin infections when antibiotics are prescribed to confirm pathogen type and resistance [37].
Molluscum contagiosum (MC) gladiatorum
Molluscum contagiosum is a poxvirus disease presenting most frequently in children less than fourteen years old [42]. Clinical exam reveals white, pearl-like, domed papules on the skin which typically resolve without pharmacologic intervention within one year [32] (Fig. 6). Moreover, a study from Basdag et al. found no significant difference in resolution of MC at 18 months between a control and treatment group [43]. Therefore, clinical focus should be on prevention of transmission with mechanical interventions such as curettage or cryotherapy being indicated for persistent lesions if the patient is amenable. Lesions should be covered thoroughly post-treatment before return to play is initiated and remain covered during play until fully healed [44].
Fig. 6.

Molluscum contagiosum papules located on the right lateral aspect of the trunk. Attribution: Dave Bray, MD, Walter Reed Army Medical Center, Public domain, via Wikimedia Commons. January 13, 2011.
Available at: https://commons.wikimedia.org/wiki/File:Molluscum_on_child.jpg. Accessed May 29, 2024
Folliculitis
Folliculitis results from bacterial infiltration of hair follicles frequently from Staphylococcus Aureus (Fig. 7). Infections present as erythematous skin patches or pustules often surrounding friction points between skin and equipment or mats [37]. Infections frequently resolve uneventfully without intervention however topical antibiotics such as mupirocin 2% creams can be applied if infections fail to improve [37].
Fig. 7.

Folliculitis infection with visible erythema and pustules surrounding hair follicles. Attribution: Da pacem Domine, CC0, via Wikimedia Commons. July 2, 2017.
Available at: https://commons.wikimedia.org/wiki/File:Folliculitis2.jpg. Accessed May 29, 2024
Verruca vulgaris (warts)
Verruca vulgaris most commonly presents on the hands and feet as raised, hyperkeratotic, scale-like lesions resulting from human papilloma virus infection of cutaneous tissue [31] (Fig. 8). Therapeutics such as tretinoin, cantharidin, podophyllin, or curettage are effective treatment options [31, 37]. These often painless lesions are not considered to be highly contagious and therefore, do not restrict wrestlers from participation. The NFHS does require lesions to be covered if prone to bleeding [45].
Fig. 8.

Verruca vulgaris (warts) located on the dorsal aspect of the second left digit. Credit: Mohamed boujil, CC BY-SA 4.0 < https://creativecommons.org/licenses/by-sa/4.0 > , via Wikimedia Commons. June 2, 2018.
Available at: https://commons.wikimedia.org/wiki/File:Verrue.jpg. Accessed May 28, 2024
Impetigo
Typical infections of impetigo result from Streptococci or Staphylococci species. These infections present as clusters of crusted, brown or honey-colored lesions precipitating from pustule lysis (Fig. 9). Ecthyma, resulting from beta-hemolytic Streptococci, is also on the differential, presenting as a ring of erythematous tissue encircling a yellow-crusted ulcer.
Fig. 9.

Impetigo infection located on the forearm. Attribution: Evanherk at Dutch Wikipedia, CC BY-SA 3.0 < http://creativecommons.org/licenses/by-sa/3.0/ > , via Wikimedia Commons. March 1, 2004.
Available at https://commons.wikimedia.org/wiki/File:Impetigo_elbow.jpg. Accessed May 28, 2024
Treatment for impetigo in adults and children is often dicloxacillin, cephalexin, clindamycin, or erythromycin taken three to four times daily or topical mupirocin 2% ointment applied three times daily. Ecthyma treatment mirrors that of impetigo, however only oral therapeutics are indicated. While uncommon, this condition can lead to kidney dysfunction in the form of glomerulonephritis if left untreated [38].
Clinicians should counsel patients on the importance of good hygiene habits including routine showering directly after practice, sanitizing equipment frequently, and visually evaluating skin before wrestling involvement to minimize risk of infection or disease transmission [35]. Given the prevalence of skin infections in adolescent wrestling, efforts to implement more advanced infection control mechanisms have been indicated and further case control studies will be necessary to elucidate best practices on this sparsely studied topic [27]. A summary table of discussed skin infections and recommended treatment has been provided (Table 1).
Table 1.
Clinical Presentation and Treatment for Adolescent Wrestler Skin Infections
| Infection | Clinical Presentation | Treatment | Return-to-Play |
|---|---|---|---|
| Herpes gladiatorum |
• Localized pain, primarily on the face • Fever • Pharyngitis • Lymphadenopathy |
• PCR testing for verification • 3 × daily acyclovir or valacyclovir for 5–10 days, though often resolves without intervention |
• Primary outbreak: Minimum 10 days if primary infection. 14 days if accompanying systemic symptoms • All lesions are healed with scabs and no new vesicle formation • Recurrent outbreak: Minimum 120 h once antiviral therapy is initiated |
| Tinea gladiatorum (ringworm) |
• Slightly raised, erythematous, annular lesion with a leading edge and central clearing • Primarily on trunk, feet, head, or groin |
• Antifungal topical therapeutics such as terbinafine, itraconazole, ketoconazole, clotrimazole, and miconazole applied 1–2 times daily for a period of 2–4 weeks • Griseofulvin or terbinafine are prescribed for a systemic treatment in children with weight-based dosage when topical therapeutics are unsuccessful |
• 3 days after starting treatment if lesion on body • 14 days after starting treatment if scalp involvement |
| Cellulitis |
• Diffuse patches of erythematous skin with subcutaneous edema • Test for MRSA |
• Cephalexin or azithromycin 2–4 × daily for 5–10 days • Topical mupirocin 2% ointment applied 3 × daily for smaller infections |
• 72 h after treatment and no further drainage. Once return, cover area with dressing until complete resolution |
| Molluscum contagiosum (MC) gladiatorum | • White, pearl-like, domed papules | • Full coverage of lesions, prevent transmission | • Participation permitted after immediate treatment with covering dressing |
| Folliculitis |
• Erythematous skin patches or pustules • Often surrounding friction points |
• Topical antibiotics (mupirocin 2%) for persistent infections | • 72 h after treatment and no further drainage. Once return, cover area with dressing until complete resolution |
| Verruca vulgaris (warts) |
• Raised, hyperkeratotic, scale-like lesions • Often on hands and feet |
• Tretinoin, cantharidin, podophyllin, or curettage if desired | • No restrictions |
| Impetigo | • Clusters of crusted, brown or honey-colored lesions precipitating from pustule lysis |
• Dicloxacillin, cephalexin, clindamycin, or erythromycin 3–4 × daily • Or topical mupirocin 2% ointment 3 × daily |
• 72 h after treatment and no further drainage. Once return, cover area with dressing until complete resolution |
Note: Return-to-Play guidelines based on National Federation of State High School Associations (NFHS). PCR = Polymerase Chain Reaction
Nutrition and Weight Concerns
Wrestling competitions often involve multiple middle or high schools and are separated according to weight classes to equalize the opportunity for athletes of all sizes. Regulations tend to be regional, but most school districts adhere to guidelines set forth by the NFHS, which aim to reduce harmful weight cycling in wrestling. Traditionally, wrestlers are encouraged to compete in the lowest weight class possible. To meet the qualifications for lower weight classes, wrestlers reduce their body weight by drastic means before weigh-ins – termed Rapid Weight Loss (RWL). After weigh-ins but before their match, athletes may then replenish lost nutrients through Rapid Weight Gain (RWG). Due to the effects of cyclic RWL and RWG on the adolescent wrestler’s available energy and strength, current research challenges the traditional goal of competing at the lowest weight class possible [46, 47]. Coaches and parents are most involved in this cyclic weight management process, but their lack of professional nutrition knowledge may prove detrimental for wrestlers [48]. Primary care providers should be sure to educate wrestlers and parents on the dangers of RWL and RWG and suggest more sustainable methods of making weight.
During RWL, wrestlers use methods such as restricting food or fluid intake, taking diuretics or emetics, using sweat suits or steam rooms, or consistent spitting to reduce their total fluid weight [49]. Prior studies have found that through these methods, total body weight loss greater than 5% may lead to increased creatinine, blood urea nitrogen, and urine specific gravity – all indicators of dehydration and acute kidney damage [50, 51]. Weight loss from under 5% within a 24-h period has not been definitively linked to the same critical issues, but it is not recommended for adolescent competitors [52]. In addition to acute kidney damage, adolescent wrestlers may suffer hormone resistance and relative energy deficiency in sport [53]. Potential long-term effects of relative energy deficiency in sport include decreased bone health, altered hormone production, and mood changes[54]. Coupled with clear short-term detriments, there is indication that minimizing this practice is beneficial for the health of adolescent athletes [46].
The period of RWG is much shorter than RWL – sometimes only an hour between weigh-ins and match start. Reaching recommended nutrition thresholds, including an adolescent athlete diet with 50% carbohydrates and water intake hours in advance is exceedingly difficult or even impossible during RWG [55]. For example, muscle glycogen may be unable to reach pre-RWL levels even after a carbohydrate-rich meal [56]. Protein, calcium, and iron are often deficient in adolescents at baseline, further increasing risk for MSK injury during a nutrient deficit [57]. Though RWG remains a lesser concern than RWL for sports providers, the physiological stress of RWG may also be detrimental to adolescent wrestlers, especially for females who tend to gain more weight during RWG [58, 59]. Primary care providers should encourage healthy, limited weight loss and weight gain for the best success of adolescent wrestlers.
The cyclic process of weight management affects not only physical aspects of an athlete but also psychological. Eating disorders are more common among athletes than non-athletes, especially in those who participate in weight class sports [60]. Specifically, bulimia is common among wrestlers due to their need to consistently and rapidly lose weight [61]. Though traditional nutrition concerns target females, adolescent wrestler males may actually display more unhealthy eating habits [62]. RWL has also been associated with other negative outcomes, such as poor mood states [63]. Despite underlying nutrition risks, wrestlers tend to be confident in their body image [64]. Adolescent wrestlers, therefore, should primarily be screened for unhealthy habits regarding their weight rather than unhealthy perceptions of their body image. Wrestlers who demonstrate an exceptionally risky pattern of weight management or those who appear unwilling to accept the risks of RWL and RWG may be candidates for referral to a sport psychologist or sport dietician. If disordered eating is suspected, referral to specialists in this area may be warranted.
In order to combat the cyclic weight gain and loss process due to its physiological and psychological detriments, the National Federation of State High School Associations (NFHS) has provided a list of guidelines for adolescent wrestlers which include weigh in procedures and match procedures. While not a rulebook, many schools do adopt these guidelines as rules. Since the 2006–2007 season, a stringent weight management program was released by NFHS. These statements require that wrestlers are eligible for their pre-season weigh-in only if they have a urine specific gravity of 1.025 or less (indicating good hydration) and if they have a body fat of at least 7% in males and 12% in females. Using their pre-season weight, athletes are then restricted from losing more than 1.5% of their weight per week. According to these guidelines, an athlete may continue to move to lower weight classes throughout the season, but the minimum weight class for each week is fixed at the beginning of the season in order to reduce the practice of RWL. To combat RWG, NFHS also allows a maximum of two pounds gained during a multiple-day competition from pre-match weigh-in on day one to pre-match weigh-in on any subsequent day. Athletes are prohibited from gaining greater than one pound between any two consecutive days of competition. While the above guidelines offer useful information to parents, coaches, and wrestlers, it is essential for primary care providers to monitor nutritional habits as certain athletes may be more impacted by cyclical weight management.
Conclusion
The primary care provider’s care regarding adolescent wrestlers primarily revolve around potential MSK injuries, skin infections, and nutritional deficits. Adolescent wrestlers are often injured due to acute trauma rather than overuse, and most injuries occur above the waist. Still, providers should examine for signs of unidentified fractures, concussions, or other MSK issues while emphasizing the benefit of proper warm-ups. Skin conditions are prevalent given the prolonged skin-to-skin nature of the sport and are usually identified pre-match; however, primary care providers may counsel patients on good hygiene and conduct further examination at regular visits. Nutrition concerns may also be apparent in the adolescent wrestler due to weight cycling associated with “making weight.” Providers should assess for underlying issues which point to insufficient nutrition, suggest healthier alternatives to meeting a wrestler’s weight goals, and emphasize the importance of regaining nutrients safely after weight loss.
Author contributions
C.S, J.M, V.C, N.H, wrote the main manuscript text. C.S and J.J prepared Figs. 1–9. C.S and J.M prepared Table 1. All authors reviewed the manuscript.
Funding
No funding was received.
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hewett TE, Pasque C, Heyl R, Wroble R. Wrestling injuries. Med Sport Sci. 2005;48:152–78. 10.1159/000084288 [DOI] [PubMed] [Google Scholar]
- 2.Boden BP, Lin W, Young M, Mueller FO. Catastrophic injuries in wrestlers. Am J Sports Med. 2002;30(6):791–5. 10.1177/03635465020300060601 [DOI] [PubMed] [Google Scholar]
- 3.Ritzer EE, Yang J, Kistamgari S, Collins CL, Smith GA. An epidemiologic comparison of acute and overuse injuries in high school sports. Inj Epidemiol. 2021;8(1):51. 10.1186/s40621-021-00344-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robinson TW, Corlette J, Collins CL, Comstock RD. Shoulder injuries among US high school athletes, 2005/2006-2011/2012. Pediatrics. 2014;133(2):272–9. 10.1542/peds.2013-2279 [DOI] [PubMed] [Google Scholar]
- 5.Bonza JE, Fields SK, Yard EE, Dawn CR. Shoulder injuries among United States high school athletes during the 2005–2006 and 2006–2007 school years. J Athl Train. 2009;44(1):76–83. 10.4085/1062-6050-44.1.76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pasque CB, Hewett TE. A prospective study of high school wrestling injuries. Am J Sports Med. 2000;28(4):509–15. 10.1177/03635465000280041101 [DOI] [PubMed] [Google Scholar]
- 7.Rechel JA, Yard EE, Comstock RD. An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2008;43(2):197–204. 10.4085/1062-6050-43.2.197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garrick JG, Requa RK. Injuries in high school sports. Pediatrics. 1978;61(3):465–9. 10.1542/peds.61.3.465 [DOI] [PubMed] [Google Scholar]
- 9.Krogmann RJ, Jamal Z, King KC. Auricular Hematoma. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC. [PubMed]
- 10.Malloy K. Assessment and management of auricular hematoma and cauliflower ear.: UpToDate; 2022 [updated June 8, 2022. Available from: https://www.uptodate.com/contents/assessment-and-management-of-auricular-hematoma-and-cauliflower-ear#H3540829.
- 11.Patel BC, Skidmore K, Hutchison J, Hatcher JD. Cauliflower Ear. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC.; 2024. [PubMed]
- 12.Kalambe Ghate S, Kalambe A, Maldhure S. Auricular haematoma an avoidable cosmetic deformity: A chance or negligence. Am J Otolaryngol. 2022;43(1):103232. 10.1016/j.amjoto.2021.103232 [DOI] [PubMed] [Google Scholar]
- 13.Meron A, McMullen C, Laker SR, Currie D, Comstock RD. Epidemiology of Cervical Spine Injuries in High School Athletes Over a Ten-Year Period. Pm r. 2018;10(4):365–72. 10.1016/j.pmrj.2017.09.003 [DOI] [PubMed] [Google Scholar]
- 14.Qureshi SA, Hecht AC. Burner Syndrome and Cervical Cord Neuropraxia. Seminars in Spine Surgery. 2010;22(4):193–7. 10.1053/j.semss.2010.06.005 [DOI] [Google Scholar]
- 15.Clark AJ, Auguste KI, Sun PP. Cervical spinal stenosis and sports-related cervical cord neurapraxia. Neurosurgical Focus FOC. 2011;31(5):E7. 10.3171/2011.7.FOCUS11173 [DOI] [PubMed]
- 16.Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC.; 2024. [PubMed]
- 17.Maffulli N, Longo UG, Gougoulias N, Caine D, Denaro V. Sport injuries: a review of outcomes. Br Med Bull. 2011;97:47–80. 10.1093/bmb/ldq026 [DOI] [PubMed] [Google Scholar]
- 18.Halloran L. Wrestling injuries. Orthop Nurs. 2008;27(3):189–92; quiz 93–4. 10.1097/01.NOR.0000320548.20611.16 [DOI] [PubMed]
- 19.Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94–9. 10.1056/NEJM200007133430203 [DOI] [PubMed]
- 20.Bandiera G, Stiell IG, Wells GA, Clement C, De Maio V, Vandemheen KL, et al. The Canadian C-spine rule performs better than unstructured physician judgment. Ann Emerg Med. 2003;42(3):395–402. 10.1016/S0196-0644(03)00422-0 [DOI] [PubMed] [Google Scholar]
- 21.Twomey-Kozak J, Whitlock KG, O’Donnell JA, Klifto CS, Anakwenze O. Epidemiology of Sports-Related Clavicle Fractures in the United States: Injuries From 2015 to 2019. Orthop J Sports Med. 2022;10(10):23259671221126550. 10.1177/23259671221126553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Youm T, Takemoto R, Park BK. Acute management of shoulder dislocations. J Am Acad Orthop Surg. 2014;22(12):761–71. 10.5435/JAAOS-22-12-761 [DOI] [PubMed] [Google Scholar]
- 23.Dizdarevic I, Low S, Currie DW, Comstock RD, Hammoud S, Atanda A Jr. Epidemiology of Elbow Dislocations in High School Athletes. Am J Sports Med. 2016;44(1):202–8. 10.1177/0363546515610527 [DOI] [PubMed] [Google Scholar]
- 24.Barton D, DeSilva G. An Update on Simple Elbow Dislocations: A Protocol for Early Return to Sport in High School Wrestlers. Curr Sports Med Rep. 2021;20(5):266–70. 10.1249/JSR.0000000000000845 [DOI] [PubMed] [Google Scholar]
- 25.Johnson BK, Brou L, Fields SK, Erkenbeck AN, Comstock RD. Hand and Wrist Injuries Among US High School Athletes: 2005/06–2015/16. Pediatrics. 2017;140(6). 10.1542/peds.2017-1255 [DOI] [PubMed]
- 26.Myers RJ, Linakis SW, Mello MJ, Linakis JG. Competitive Wrestling-related Injuries in School Aged Athletes in U.S. Emergency Departments. West J Emerg Med. 2010;11(5):442–9. [PMC free article] [PubMed]
- 27.Yard EE, Collins CL, Dick RW, Comstock RD. An epidemiologic comparison of high school and college wrestling injuries. Am J Sports Med. 2008;36(1):57–64. 10.1177/0363546507307507 [DOI] [PubMed] [Google Scholar]
- 28.Clifton DR, Onate JA, Hertel J, Pierpoint LA, Currie DW, Wasserman EB, et al. The First Decade of Web-Based Sports Injury Surveillance: Descriptive Epidemiology of Injuries in US High School Boys’ Basketball (2005–2006 Through 2013–2014) and National Collegiate Athletic Association Men’s Basketball (2004–2005 Through 2013–2014). J Athl Train. 2018;53(11):1025–36. 10.4085/1062-6050-148-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Safety Tips: Wrestling Rady Children's Hospital-Sand Diego [Available from: https://www.rchsd.org/health-article/safety-tips-wrestling/.
- 30.Ashack KA, Burton KA, Johnson TR, Currie DW, Comstock RD, Dellavalle RP. Skin infections among US high school athletes: A national survey. J Am Acad Dermatol. 2016;74(4):679–84 e1. 10.1016/j.jaad.2015.10.042 [DOI] [PubMed]
- 31.Peterson AR, Nash E, Anderson BJ. Infectious Disease in Contact Sports. Sports Health. 2019;11(1):47–58. 10.1177/1941738118789954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thompson AJ, Matinpour K, Hardin J, Hsu S. Molluscum gladiatorum. Dermatol Online J. 2014;20(6). 10.5070/D3206022855 [PubMed]
- 33.Turbeville SD, Cowan LD, Greenfield RA. Infectious disease outbreaks in competitive sports: a review of the literature. Am J Sports Med. 2006;34(11):1860–5. 10.1177/0363546505285385 [DOI] [PubMed] [Google Scholar]
- 34.Caputo R, De Boulle K, Del Rosso J, Nowicki R. Prevalence of superficial fungal infections among sports-active individuals: results from the Achilles survey, a review of the literature. J Eur Acad Dermatol Venereol. 2001;15(4):312–6. [PubMed] [Google Scholar]
- 35.Anderson BJ. Managing herpes gladiatorum outbreaks in competitive wrestling: the 2007 Minnesota experience. Curr Sports Med Rep. 2008;7(6):323–7. 10.1249/JSR.0b013e31818eebde [DOI] [PubMed] [Google Scholar]
- 36.Dworkin MS, Shoemaker PC, Spitters C, Cent A, Hobson AC, Vieira J, et al. Endemic spread of herpes simplex virus type 1 among adolescent wrestlers and their coaches. Pediatr Infect Dis J. 1999;18(12):1108–9. 10.1097/00006454-199912000-00020 [DOI] [PubMed] [Google Scholar]
- 37.Wilson EK, Deweber K, Berry JW, Wilckens JH. Cutaneous infections in wrestlers. Sports Health. 2013;5(5):423–37. 10.1177/1941738113481179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pecci M, Comeau D, Chawla V. Skin conditions in the athlete. Am J Sports Med. 2009;37(2):406–18. 10.1177/0363546508325663 [DOI] [PubMed] [Google Scholar]
- 39.Anderson BJ, McGuire DP, Reed M, Foster M, Ortiz D. Prophylactic Valacyclovir to Prevent Outbreaks of Primary Herpes Gladiatorum at a 28-Day Wrestling Camp: A 10-Year Review. Clin J Sport Med. 2016;26(4):272–8. 10.1097/JSM.0000000000000255 [DOI] [PubMed] [Google Scholar]
- 40.Kermani F, Moosazadeh M, Hosseini SA, Bandalizadeh Z, Barzegari S, Shokohi T. Tinea Gladiatorum and Dermatophyte Contamination Among Wrestlers and in Wrestling Halls: A Systematic Review and Meta-analysis. Curr Microbiol. 2020;77(4):602–11. 10.1007/s00284-019-01816-3 [DOI] [PubMed] [Google Scholar]
- 41.Zalewski A, Goldust M, Szepietowski JC. Tinea Gladiatorum: Epidemiology, Clinical Aspects, and Management. J Clin Med. 2022;11(14). 10.3390/jcm11144066 [DOI] [PMC free article] [PubMed]
- 42.Olsen JR, Gallacher J, Piguet V, Francis NA. Epidemiology of molluscum contagiosum in children: a systematic review. Fam Pract. 2014;31(2):130–6. 10.1093/fampra/cmt075 [DOI] [PubMed] [Google Scholar]
- 43.Basdag H, Rainer BM, Cohen BA. Molluscum contagiosum: to treat or not to treat? Experience with 170 children in an outpatient clinic setting in the northeastern United States. Pediatr Dermatol. 2015;32(3):353–7. 10.1111/pde.12504 [DOI] [PubMed] [Google Scholar]
- 44.Pujalte GGA, Costa LMC, Clapp AD, Presutti RJ, Sluzevich JC. More Than Skin Deep: Dermatologic Conditions in Athletes. Sports Health. 2023;15(1):74–85. 10.1177/19417381211065026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sports-Related Skin Infections Position Statement and Guidelines, (2022).
- 46.Roemmich JN, Sinning WE. Weight loss and wrestling training: effects on nutrition, growth, maturation, body composition, and strength. J Appl Physiol (1985). 1997;82(6):1751–9. [DOI] [PubMed]
- 47.Kiningham R, Monseau A. Caring for Wrestlers. Curr Sports Med Rep. 2015;14(5):404–12. 10.1249/JSR.0000000000000193 [DOI] [PubMed] [Google Scholar]
- 48.Knox C. Review and Commentary of the Nutritional Recommendations, Weight Management Regulations, Weight Management Practices, and the Potential of Disordered Eating Patterns in High School Age Wrestlers. The Sport Journal 2017
- 49.Khalili-Borna D, Honsik K. Wrestling and sports medicine. Curr Sports Med Rep. 2005;4(3):144–9. 10.1097/01.CSMR.0000306197.51994.16 [DOI] [PubMed] [Google Scholar]
- 50.Lakicevic N, Paoli A, Roklicer R, Trivic T, Korovljev D, Ostojic SM, et al. Effects of Rapid Weight Loss on Kidney Function in Combat Sport Athletes. Medicina (Kaunas). 2021;57(6). 10.3390/medicina57060551 [DOI] [PMC free article] [PubMed]
- 51.Trivic T, Roklicer R, Zenic N, Modric T, Milovancev A, Lukic-Sarkanovic M, et al. Rapid weight loss can increase the risk of acute kidney injury in wrestlers. BMJ Open Sport Exerc Med. 2023;9(2):e001617. 10.1136/bmjsem-2023-001617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Martínez-Aranda LM, Sanz-Matesanz M, Orozco-Durán G, González-Fernández FT, Rodríguez-García L, Guadalupe-Grau A. Effects of Different Rapid Weight Loss Strategies and Percentages on Performance-Related Parameters in Combat Sports: An Updated Systematic Review. Int J Environ Res Public Health. 2023;20(6) 10.3390/ijerph20065158 [DOI] [PMC free article] [PubMed]
- 53.Sams D, Geiselman J. Effects of Relative Energy Deficiency in Sport (RED-S) on the Growth and Development of Adolescent Wrestlers: A Clinical Review. Nutr Perspect: J Counc Nutr. 2021;44(2):5–7. [Google Scholar]
- 54.Gould RJ, Ridout AJ, Newton JL. Relative Energy Deficiency in Sport (RED-S) in Adolescents - A Practical Review. Int J Sports Med. 2023;44(4):236–46. 10.1055/a-1947-3174 [DOI] [PubMed] [Google Scholar]
- 55.Smith JW, Holmes ME, McAllister MJ. Nutritional Considerations for Performance in Young Athletes. J Sports Med (Hindawi Publ Corp). 2015;2015:734649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kondo E, Shiose K, Osawa T, Motonaga K, Kamei A, Nakajima K, et al. Effects of an overnight high-carbohydrate meal on muscle glycogen after rapid weight loss in male collegiate wrestlers. BMC Sports Sci Med Rehabil. 2021;13(1):96. 10.1186/s13102-021-00325-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Petrie HJ, Stover EA, Horswill CA. Nutritional concerns for the child and adolescent competitor. Nutrition. 2004;20(7–8):620–31. 10.1016/j.nut.2004.04.002 [DOI] [PubMed] [Google Scholar]
- 58.Viveiros L, Moreira A, Zourdos MC, Aoki MS, Capitani CD. Pattern of Weight Loss of Young Female and Male Wrestlers. J Strength Cond Res. 2015;29(11):3149–55. 10.1519/JSC.0000000000000968 [DOI] [PubMed] [Google Scholar]
- 59.Matthews JJ, Stanhope EN, Godwin MS, Holmes MEJ, Artioli GG. The Magnitude of Rapid Weight Loss and Rapid Weight Gain in Combat Sport Athletes Preparing for Competition: A Systematic Review. Int J Sport Nutr Exerc Metab. 2019;29(4):441–52. 10.1123/ijsnem.2018-0165 [DOI] [PubMed] [Google Scholar]
- 60.Kontele I, Vassilakou T. Nutritional Risks among Adolescent Athletes with Disordered Eating. Children (Basel). 2021;8(8). 10.3390/children8080715 [DOI] [PMC free article] [PubMed]
- 61.Lakin JA, Steen SN, Oppliger RA. Eating behaviors, weight loss methods, and nutrition practices among high school wrestlers. J Community Health Nurs. 1990;7(4):223–34. 10.1207/s15327655jchn0704_5 [DOI] [PubMed] [Google Scholar]
- 62.Aksu A, Altun S, İmamoğlu O, Karacabey K. Investigation of Eating Behaviors in Young Wrestlers. Postmodern Openings. 2020;11:163–74. 10.18662/po/11.2/168 [DOI] [Google Scholar]
- 63.Hrvoje K, Baić M, Slacanac K. Mood Aspects of Rapid Weight Loss in Adolescent Wrestlers. Kinesiology. 2016;48. 10.26582/k.48.2.7
- 64.Satterfield NA, Stutts LA. Pinning down the problems and influences: Disordered eating and body satisfaction in male wrestlers. Psychol Sport Exerc. 2021;54:101884. 10.1016/j.psychsport.2021.101884 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.


