Abstract
Purpose of Review
Platelet-rich plasma (PRP) is an emerging biological intervention for osteoarthritis (OA), yet the outcomes remain uncertain. The purpose of this study was to review current literature regarding the use of PRP for knee and hip OA.
Recent Findings
Recent systematic reviews have found significant clinical improvements in outcomes after the administration of PRP compared to hyaluronic acid (HA) in patients with knee OA. One of these reviews included bone marrow aspirate concentrate (BMAC) as a comparison group and found no significant differences in outcomes between PRP and BMAC. Currently, the literature is lacking on whether leukocyte-rich or leukocyte-poor PRP is superior in patients with knee OA. The literature on PRP for hip OA has not provided consistent results as it has for the knee. Two recent systematic reviews evaluated RCTs for patients undergoing treatment with either PRP or HA for hip OA and found no significant differences in clinical outcomes between groups at final follow-up. Current literature regarding the association between OA grade and PRP efficacy has found varying results.
Summary
The use of PRP injections in the treatment of knee OA appears to be favorable, resulting in clinically comparable or superior outcomes compared to other injection treatments. However, the clinical efficacy of PRP injections in hip OA is far less consistent. Evidence is lacking to suggest that the presence of leukocytes significantly influences clinical outcomes. Further randomized controlled trials on larger cohorts, with longer follow-up, and with comparable formulations are required before recommendations can be made regarding use of PRP for hip OA, the effect of leukocyte concentration, and clinical efficacy based on OA grade.
Keywords: Biologics, Knee osteoarthritis, Hip osteoarthritis, Platelet-rich plasma, PRP
Introduction
Osteoarthritis (OA) is the most common joint disorder in the United States and a leading cause of chronic disability worldwide [1]. OA treatment aims to alleviate pain, enhance function and mobility, improve deformity through surgery, and improve symptoms overall to delay the need for joint replacement. Non-surgical treatment options for knee or hip OA encompass oral nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, and intra-articular injections including hyaluronic acid (HA), corticosteroids (CS), platelet-rich plasma (PRP), and bone marrow aspirate concentrate (BMAC), among others [2].
Advantages of PRP include stimulation of growth factors and inhibition of inflammatory mediators [3]. Similarly, BMAC contains growth factors as well as bone marrow stromal cells involved in chondrogenesis and mediation of anti-inflammatory effects. Hyaluronic acid is known to be useful for lubrication of the joint, cartilage nourishment, and stimulation of production of endogenous HA [4].
PRP is autologous plasma that has been prepared to contain a higher concentration of platelets than in vivo plasma. Upon activation, platelets swiftly release a variety of growth factors, including Transforming Growth Factor (TGF)-β and Insulin-like Growth Factor (IGF)-1, from their α-granules [5]. In conjunction with coagulation factors, cytokines, and other platelet proteins, these growth factors are believed to influence chondrocytes and enhance the chondrocyte cartilaginous matrix as well as diminish the inflammatory effects of certain cytokines involved in the process of OA [6]. Due to its autologous nature, PRP treatment eliminates the risk of immune reactions or blood-transmitted diseases. PRP currently lacks standardized guidelines regarding the optimal number or frequency of injections and the recommended treatment for various stages of gonarthrosis. Furthermore, recent systematic reviews and meta-analyses have explored the impact of PRP on knee and hip OA and have produced conflicting results [3, 7–9]. The purpose of this study was to review current literature regarding the use of PRP for knee and hip OA.
Knee Osteoarthritis
Given the increasing prevalence of knee OA, [4], intra-articular injections including HA, corticosteroids, PRP, and BMAC are gaining popularity as nonoperative options for management of this disease [3]. However, there is uncertainty regarding the superior treatment and current guidelines do not offer clear recommendations. With the growing body of research on this topic, there have been multiple meta-analyses that seek to provide clarity to this subject [3, 4, 8].
Recent studies have compared PRP with other treatment modalities. A systematic review of Level I studies compared the efficacy and safety of PRP and HA injections for the treatment of knee OA (Table 1) [8]. A total of 18 studies met inclusion criteria, including 811 patients undergoing PRP injections and 797 patients undergoing HA injections, with a mean follow-up of 11.1 months. The authors found that mean improvement was significantly higher in the PRP group based on various patient-reported outcomes (PROs) including the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), visual analog scale (VAS) for pain, and Subjective International Knee Documentation Committee (IKDC) scores. More than half (51.7%) of the clinical outcomes demonstrated significantly greater improvement with PRP versus HA. Additionally, 81.0% of all PROs reporting on pre- to post-injection scores found significant improvement in PRP patients, compared to only 38.1% of HA patients.
Table 1.
Systematic reviews of randomized controlled trials involving platelet-rich plasma for knee osteoarthritis. *Not a comprehensive list. N refers to the total number of knees that underwent treatment in each study. Age and follow-up are reported as mean, with the “Total” row reported as a weighted mean. BMAC, bone marrow aspirate concentrate; CS, corticosteroid; HA, hyaluronic acid; IKDC, international knee documentation committee; LOE, level of evidence; PLA, placebo; PRP, platelet-rich plasma; VAS, visual analog scale; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index
| Study | LOE | N | Patient Age, years | Follow-Up, months | Outcomes Reported | Outcomes |
|---|---|---|---|---|---|---|
| Belk et al., 2023 [3] | I | 1042 PRP, 226 BMAC, 1128 HA | 57.7 (PRP), 57.0 (BMAC), 59.0 (HA) | 13.5 (PRP), 17.5 (BMAC), 14.4 (HA) | WOMAC, VAS, Subjective IKDC | Higher scores in PRP vs. HA and BMAC vs. HA, no significant differences between PRP and BMAC |
| Qiao et al., 2023 [4] | I | 1046 PRP, 907 HA, 196 PRP + HA, 132 CS, 147 PLA | 59.1 | 6.2 | WOMAC, VAS | PRP and PRP + HA had best scores at 3, 6, and 12 months follow-up |
| Belk et al., 2021 [8] | I | 811 PRP, 797 HA | 57.6 (PRP), 59.3 (HA) | 11.1 | WOMAC, VAS, Subjective IKDC | WOMAC scores significantly better in PRP group, VAS scores significantly lower in PRP group, Subjective IKDC scores significantly higher in PRP group |
| Total | - | 2899 PRP, 226 BMAC, 2832 HA, 196 PRP + HA, 132 CS, 147 PLA | 58.3 | 12.5 | - | - |
A more recent and updated systematic review published in 2023 included 27 Level I studies with a total of 1,042 patients undergoing treatment for knee OA with PRP (mean follow-up 13.5 months), 226 patients with BMAC (mean follow-up 17.5 months), and 1,128 patients with HA (mean follow-up 14.4 months) [3]. The authors concluded that PRP and BMAC had significantly improved outcomes compared to HA based on the WOMAC, VAS, and Subjective IKDC scores, without significant differences between PRP and BMAC.
In a similar meta-analysis published in 2023, Qiao et al. [4] reviewed the use of corticosteroid injections, HA, PRP, and combination therapy (PRP + HA) compared to placebo in the treatment of knee OA [4]. The authors included a total of 35 studies with 3,104 patients, with follow-up ranging from 3 to 12 months. At a 3-month follow-up, PRP and PRP + HA had the best WOMAC scores, and PRP + HA had the best VAS outcomes. PRP, CS, HA, and placebo had similar WOMAC scores at 6 months, and PRP + HA had the best VAS scores. At 12 months, PRP and PRP + HA demonstrated the best WOMAC and VAS scores. Overall, PRP and PRP + HA consistently demonstrated the greatest improvement in function and decreased pain, suggesting PRP may act effectively as a single-agent treatment.
Although much of the current literature shows consistent improvement of knee OA symptoms with PRP injections, many of the reviews have similar limitations. For example, none of them report on knee survivorship i.e. the proportion of knees that were able to delay arthroplasty. Additionally, preparation and administration of the injections differed across studies, as did the PROs assessed.
Hip Osteoarthritis
Osteoarthritis of the hip is a similarly debilitating condition, causing decreased mobility and quality of life [10]. Compared to knee OA, fewer studies have assessed clinical outcomes following intra-articular PRP injections for hip OA.
In 2021, a randomized pilot study comparing leukocyte-poor PRP versus low-molecular weight HA in 33 hips found significant improvement in the WOMAC score and hip internal rotation at 6 months in the PRP group [11]. Additionally, a significantly higher proportion of patients in the HA group failed nonoperative management and underwent hip arthroplasty during the follow-up period compared to patients in the PRP group. While hip survivorship was similar between the 2 groups at 1 year following injection therapy, the PRP group demonstrated more successful survivorship at 2 years.
A subsequent systematic review and meta-analysis of level I and II randomized controlled trials (RCTs) included 6 studies with 211 patients undergoing PRP injections (mean follow-up 12.2 months) and 197 patients undergoing HA injections (mean follow-up 11.9 months) (Table 2) [7]. No significant differences were found between groups with regard to the WOMAC, VAS, or Harris Hip Score (HHS), and this remained the result even when the study with the highest risk of bias was excluded. An additional subanalysis was performed including only patients treated with leukocyte-poor PRP, and still no significant differences in WOMAC scores were found between groups at final follow-up.
Table 2.
Systematic reviews of randomized controlled trials involving platelet-rich plasma for hip osteoarthritis. *Not a comprehensive list. N refers to the total number of hips that underwent treatment with PRP or HA in each study. Age and follow-up are reported as mean, with the “Total” row reported as weighted mean. HA, hyaluronic acid; HHS, Harris Hip Score, LOE, level of evidence; PRP, platelet-rich plasma; VAS, visual analog scale; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index
| Study | LOE | N (PRP, HA) | Patient Age (PRP, HA), years | Follow-Up (PRP, HA), months | Outcomes Reported | Outcomes |
|---|---|---|---|---|---|---|
| Belk et al., 2022 [7] | II | 211, 197 | 60.0, 62.3 | 12.2, 11.9 | WOMAC, VAS, HHS, hip survivorship | No significant difference between groups at final follow-up |
| Sambe et al., 2023 [12] | II | 246, 232 | 61.0, 63.2 | 12.2, 11.9 | WOMAC, VAS, HHS | No significant difference between groups at final follow-up |
| Total | - | 457, 429 | 60.5, 62.8 | 12.2, 11.9 | - | - |
An updated meta-analysis of RCTs published in 2023 included 7 trials and 478 participants with follow-up ranging between 1 and 12 months [12]. The authors found no statistically significant differences in WOMAC scores between groups at 1–2 months or 12 months, but at 6 months the PRP group had a significant improvement in WOMAC score compared to the HA group. This 6 month mark was again significant using the VAS pain assessment, with the PRP group having a significantly lower VAS score compared to the HA group. Using the HHS for functional assessment, there were no significant differences between groups at any time point.
Future research is needed in the study of PRP injections for hip OA. Although there have been a few systematic reviews published on this topic, they have inconsistent results compared to similar studies on knee OA. They often have small samples sizes and inconsistent control groups (placebo vs. HA vs. CS), with a follow-up duration of 24 months or less. There is high heterogeneity between studies, including PRP composition, dosing, injection intervals, and PROs. Only one study included in these reviews has reported on hip survivorship, which is a great indicator of injection efficacy. More multi-center RCTs with longer follow-up are needed before definitive conclusions can be made regarding PRP for hip OA.
Leukocyte-Rich vs. Leukocyte-Poor PRP for Osteoarthritis
The popularity of PRP injections comes with debate regarding the ideal composition. Usage of both leukocyte-rich (LR-PRP) and leukocyte-poor PRP (LP-PRP) has been described in the literature, but there is a paucity of data regarding the ideal leukocyte concentration for the treatment of OA. Higher concentrations of white blood cells has been shown to cause expression of multiple inflammatory markers with potential for more painful side effects, favoring the use of LP-PRP [13]. In contrast, other studies have shown that the actions of neutrophils can promote anti-inflammatory factors [14]. However, research comparing the effects of different concentrations is still lacking.
In 2016, a meta-analysis of 6 RCTs and 3 prospective comparative studies, with a total of 1,055 patients, compared the clinical outcomes and rates of adverse reactions between LP-PRP, LR-PRP, HA, and placebo for the treatment of knee OA [13]. The authors found that LP-PRP significantly improved WOMAC scores when compared to HA or placebo (normal saline and/or local anesthetic), but no significant difference was observed with LR-PRP. Also, there was no difference in IKDC scores between any treatment groups. Overall, PRP injections had a higher incidence of adverse reactions compared to HA, but the incidence was not affected by leukocyte concentration. These adverse reactions occurred in 17/1,055 patients (1.6%) and mainly consisted of local swelling and pain, with one study reporting syncope, dizziness, headache, gastritis, and tachycardia.
Another meta-analysis published in 2021 studied differences between LR-PRP and LP-PRP for the treatment of knee OA [14]. However, of the 32 identified studies, the level of evidence ranged from I-IV, and only 1 directly compared LP-PRP and LR-PRP. Overall, 1,162 knees underwent LP-PRP injections and 628 underwent LR-PRP injections. The authors found that both LR-PRP and LP-PRP resulted in similar improvements in pain and function over 12 months of follow-up. However, there was evidence for LR-PRP causing an increased incidence of adverse reactions compared to LP-PRP.
In 2022, Abbas et al. [15] published a network meta-analysis encompassing 20 RCTs and 3 prospective comparative studies, including 2,260 patients with knee OA who received injections of either LR-PRP or LP-PRP [15]. Patients were monitored for a mean of 9.9 months. The authors found no significant differences between groups regarding PROs or adverse reactions. Also in 2022, Di Martino et al. [16] published a RCT including 90 patients undergoing LR-PRP injections and 85 undergoing LP-PRP injections for knee OA [16]. The authors found no statistically significant differences between groups regarding both clinical outcomes or adverse events at a final follow-up of 12 months.
At this time, there is no clear superiority of LR-PRP or LP-PRP in the treatment of OA. This is a field with great opportunity to better explore PRP composition and injection characteristics, and the subsequent effects on human joints. Further research is needed directly comparing the use of LR-PRP vs. LP-PRP.
Grade of Osteoarthritis
Another important question regarding use of PRP is its efficacy for different grades of OA. The Kellgren-Lawrence (K-L) classification is commonly used as a tool for radiographic diagnosis of OA, and can be used to guide clinical decision-making [17]. Typically used for knee OA, the classification assigns a grade of 0–4, with Grade 0 representing no evidence of OA and Grade 4 signifying severe OA with marked joint space narrowing. Current literature regarding the association between OA grade and PRP efficacy has found varying results.
A recent meta-analysis of 31 RCTs reviewed the use of PRP in various stages of knee OA, including 2,705 patients followed for a range of 3 months to 2 years [18]. The included studies were divided by K-L classification: stage 1–2 (5 studies), stage 1–3 (20 studies), and stage 1–4 (6 studies). The main finding of this study was that PRP therapy improved pain and function irrespective of knee OA stage, compared to control group injections (HA, CS, prolotherapy, ozone, peptide, BMAC, saline).
Single retrospective studies have been inconclusive on the topic of PRP efficacy based on OA grade. A recent retrospective analysis of 431 patients found PRP therapy resulted in statistically significant improvements in WOMAC and VAS pain scores at 3 and 12 months, regardless of OA grade [19]. Two other retrospective analyses found that while PRP therapy resulted in clinically favorable outcomes, higher degree of OA severity resulted in significantly decreased injection efficacy [20, 21]. However, these retrospective studies may carry less weight than the previously described systematic reviews of level I studies.
Further research is necessary regarding PRP therapy in varying stages of OA. The lack of data on this topic may be a reflection of the overall need for ongoing research regarding the efficacy of PRP compared to other therapies, as well as the significance of leukocyte concentration. Future studies should consider incorporating sub-analyses based on OA grade to continue characterizing the use of PRP therapy in different patient groups.
Discussion
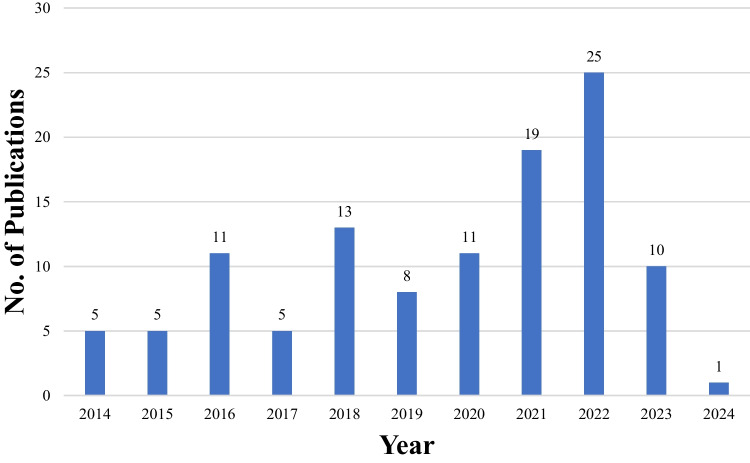
A review of studies over the past 5 years on patients with primary knee OA (Table 3) demonstrates repeated significant improvement of PROs using PRP compared with HA; however, updated RCTs comparing these treatment options are needed, as 2 of the 5 studies reported no significant differences between groups. A review of key primary hip OA studies over the past 5 years (Table 3) demonstrates a lack of significant improvement of PROs using PRP compared with HA; only one study showed significant improvement, specifically with regard to the HHS. Overall, there is a need for additional primary studies in the use of PRP for both hip and knee OA, as demonstrated in Fig. 1.
Table 3.
Level I primary studies on platelet-rich plasma for knee and hip osteoarthritis over the past 5 years. *Not a comprehensive list. N refers to the total number of knees/hips that underwent treatment in each study. BMAC, bone marrow aspirate concentrate; HA, hyaluronic acid; HHS, Harris Hip Score; IKDC, International Knee Documentation Committee; LOE, level of evidence; KOOS, Knee Injury and Osteoarthritis Outcome Score; n.s., not significant; PRP, platelet-rich plasma; VAS, visual analog scale; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index
| Knee Studies | LOE | N | Outcomes Reported | Outcomes |
| Huang et al., 2019 [22] | I |
40 PRP, 40 HA |
WOMAC | PRP group significantly improved compared to HA group |
| VAS | No significant difference between groups | |||
| Raeissadat et al., 2021 [23] | I |
52 PRP, 49 HA |
WOMAC | PRP group significantly improved compared to HA group |
| VAS | PRP group significantly improved compared to HA group | |||
| Sdeek et al., 2021 [24] | I |
95 PRP, 94 HA |
WOMAC, VAS, IKDC | No significant difference between groups for WOMAC, VAS, IKDC |
| Dulic et al., 2021 [25] | I |
34 PRP, 111 BMAC, 30 HA |
WOMAC | Both PRP and BMAC groups significantly improved compared to HA, but no difference between BMAC and PRP groups |
| IKDC | BMAC significantly improved compared to HA, but no significant difference between PRP and HA | |||
| KOOS | No significant differences between groups | |||
| Di Martino et al., 2019 [26] | I | 85 PRP, 82 HA | VAS, IKDC | No significant differences between groups for VAS or IKDC |
| Hip Studies | LOE | N | Outcomes Reported | Outcomes |
| Kraeutler et al., 2021 [11] | I | 18 PRP, 13 HA | WOMAC | No significant differences between groups |
| Villanova-López et al., 2020 [27] | I | 38 PRP, 36 HA | WOMAC, VAS, HHS | No significant differences between groups for WOMAC or VAS. PRP group reported significantly better HHS compared with HA group |
Fig. 1.
Randomized controlled trials published over past 10 years on use of platelet-rich plasma for treatment of knee or hip osteoarthritis
The management of knee and hip OA is a pressing concern in medicine due to its widespread impact on patients’ quality of life. Recent studies highlight a lack of standardization in the literature, particularly regarding treatment guidelines, outcome measures, and terminology [28, 29]. This inconsistency creates confusion among clinicians and may result in suboptimal care for patients. Furthermore, variations in terminology and classification systems for OA further complicate matters, hindering progress in understanding the condition’s pathophysiology and treatment [30]. Various medical organizations and expert panels offer differing perspectives on the optimal approaches to managing OA, leading to confusion among clinicians and potentially suboptimal care for patients [28]. Additionally, there is a lack of consensus on outcome measures and evaluation criteria used in clinical trials and research studies evaluating OA management strategies [31]. Addressing these challenges necessitates collaborative efforts within the medical community to establish clear and consistent standards.
Conclusions
The use of PRP injections in the treatment of knee OA appears to be favorable, resulting in clinically comparable or superior outcomes compared to other injection treatments. However, the clinical efficacy of PRP injections in hip OA is far less consistent. Evidence is lacking to suggest that the presence of leukocytes significantly influences clinical outcomes. Further randomized controlled trials on larger cohorts, with longer follow-up, and with comparable formulations are required before recommendations can be made regarding use of PRP for hip OA, the effect of leukocyte concentration, and clinical efficacy based on OA grade.
Author contributions
G.T. and J.D. wrote the main manuscript text and prepared Tables 1 and 2. M.K. provided guidance and supervision and edited throughout the process.
Funding
No funding was received.
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Grace Tanguilig, Jaydeep Dhillon, and Matthew Kraeutler declare that they have no conflict of interest.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian J Intern Med. 2011;2(2):205–12. [PMC free article] [PubMed] [Google Scholar]
- 2.Siddiq MAB, Clegg D, Jansen TL, Rasker JJ. Emerging and new treatment options for knee osteoarthritis. Curr Rheumatol Rev. 2022;18(1):20–32. 10.2174/1573397117666211116111738 [DOI] [PubMed] [Google Scholar]
- 3.Belk JW, Lim JJ, Keeter C, McCulloch PC, Houck DA, McCarty EC, Frank RM, Kraeutler MJ. Patients with knee osteoarthritis who receive platelet-rich plasma or bone marrow aspirate concentrate injections have better outcomes than patients who receive hyaluronic acid: systematic review and meta-analysis. Arthroscopy. 2023;39(7):1714–34. 10.1016/j.arthro.2023.03.001 [DOI] [PubMed] [Google Scholar]
- 4.Qiao X, Yan L, Feng Y, Li X, Zhang K, Lv Z, Xu C, Zhao S, Liu F, Yang X, Tian Z. Efficacy and safety of corticosteroids, hyaluronic acid, and PRP and combination therapy for knee osteoarthritis: a systematic review and network meta-analysis. BMC Musculoskelet Disord. 2023;24(1):926. 10.1186/s12891-023-06925-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Le ADK, Enweze L, DeBaun MR, Dragoo JL. Platelet-rich plasma. Clin Sports Med. 2019;38(1):17–44. 10.1016/j.csm.2018.08.001 [DOI] [PubMed] [Google Scholar]
- 6.Cook CS, Smith PA. Clinical update: Why PRP should be your first choice for injection therapy in treating osteoarthritis of the knee. Curr Rev Musculoskelet Med. 2018;11(4):583–92. 10.1007/s12178-018-9524-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belk JW, Houck DA, Littlefield CP, Kraeutler MJ, Potyk AG, Mei-Dan O, Dragoo JL, Frank RM, McCarty EC. Platelet-rich plasma versus hyaluronic acid for hip osteoarthritis yields similarly beneficial short-term clinical outcomes: a systematic review and meta-analysis of level i and ii randomized controlled trials. Arthroscopy. 2022;38(6):2035–46. 10.1016/j.arthro.2021.11.005 [DOI] [PubMed] [Google Scholar]
- 8.Belk JW, Kraeutler MJ, Houck DA, Goodrich JA, Dragoo JL, McCarty EC. Platelet-rich plasma versus hyaluronic acid for knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Am J Sports Med. 2021;49(1):249–60. 10.1177/0363546520909397 [DOI] [PubMed] [Google Scholar]
- 9.Medina-Porqueres I, Ortega-Castillo M, Muriel-Garcia A. Effectiveness of platelet-rich plasma in the management of hip osteoarthritis: a systematic review and meta-analysis. Clin Rheumatol. 2021;40(1):53–64. 10.1007/s10067-020-05241-x [DOI] [PubMed] [Google Scholar]
- 10.Xiong Y, Gong C, Peng X, Liu X, Su X, Tao X, Li Y, Wen Y, Li W. Efficacy and safety of platelet-rich plasma injections for the treatment of osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Front Med (Lausanne). 2023;10:1204144. 10.3389/fmed.2023.1204144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kraeutler MJ, Houck DA, Garabekyan T, Miller SL, Dragoo JL, Mei-Dan O. Comparing intra-articular injections of leukocyte-poor platelet-rich plasma versus low-molecular weight hyaluronic acid for the treatment of symptomatic osteoarthritis of the hip: a double-blind, randomized pilot study. Orthop J Sports Med. 2021;9(1):2325967120969210. 10.1177/2325967120969210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sambe HG, Yasir M, Man RK, Gogikar A, Nanda A, Janga LSN, Hamid P. Comparing intra-articular platelet-rich plasma with hyaluronic acid for the treatment of hip osteoarthritis: a systematic review and meta-analysis. Cureus. 2023;15(10):e47919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Riboh JC, Saltzman BM, Yanke AB, Fortier L, Cole BJ. Effect of leukocyte concentration on the efficacy of platelet-rich plasma in the treatment of knee osteoarthritis. Am J Sports Med. 2016;44(3):792–800. 10.1177/0363546515580787 [DOI] [PubMed] [Google Scholar]
- 14.Kim JH, Park YB, Ha CW, Roh YJ, Park JG. Adverse reactions and clinical outcomes for leukocyte-poor versus leukocyte-rich platelet-rich plasma in knee osteoarthritis: a systematic review and meta-analysis. Orthop J Sports Med. 2021;9(6):23259671211011948. 10.1177/23259671211011948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abbas A, Du JT, Dhotar HS. The effect of leukocyte concentration on platelet-rich plasma injections for knee osteoarthritis: a network meta-analysis. J Bone Joint Surg Am. 2022;104(6):559–70. 10.2106/JBJS.20.02258 [DOI] [PubMed] [Google Scholar]
- 16.Di Martino A, Boffa A, Andriolo L, Romandini I, Altamura SA, Cenacchi A, Roverini V, Zaffagnini S, Filardo G. Leukocyte-rich versus leukocyte-poor platelet-rich plasma for the treatment of knee osteoarthritis: a double-blind randomized trial. Am J Sports Med. 2022;50(3):609–17. 10.1177/03635465211064303 [DOI] [PubMed] [Google Scholar]
- 17.Kohn MD, Sassoon AA, Fernando ND. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin Orthop Relat Res. 2016;474(8):1886–93. 10.1007/s11999-016-4732-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vilchez-Cavazos F, Blázquez-Saldaña J, Gamboa-Alonso AA, Peña-Martínez VM, Acosta-Olivo CA, Sánchez-García A, Simental-Mendía M. The use of platelet-rich plasma in studies with early knee osteoarthritis versus advanced stages of the disease: a systematic review and meta-analysis of 31 randomized clinical trials. Arch Orthop Trauma Surg. 2023;143(3):1393–408. 10.1007/s00402-021-04304-1 [DOI] [PubMed] [Google Scholar]
- 19.Prost D, Bardot T, Baud A, Calvo A, Aumont S, Collado H, Borne J, Rajon O, Ponsot A, Malaterre A, Dahak Y, Magalon G, Sabatier F, Magalon J. Long term improvement of knee osteoarthritis after injection of single high/very high volume of very pure PRP: A retrospective analysis of patients optimally managed in dedicated centers. Regen Ther. 2024;25:203–12. 10.1016/j.reth.2023.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saita Y, Kobayashi Y, Nishio H, Wakayama T, Fukusato S, Uchino S, Momoi Y, Ikeda H, Kaneko K. Predictors of effectiveness of platelet-rich plasma therapy for knee osteoarthritis: a retrospective cohort study. J Clin Med. 2021;10(19):4514. 10.3390/jcm10194514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sánchez M, Jorquera C, Sánchez P, Beitia M, García-Cano B, Guadilla J, Delgado D. Platelet-rich plasma injections delay the need for knee arthroplasty: a retrospective study and survival analysis. Int Orthop. 2021;45(2):401–10. 10.1007/s00264-020-04669-9 [DOI] [PubMed] [Google Scholar]
- 22.Huang Y, Liu X, Xu X, Liu J. Intra-articular injections of platelet-rich plasma, hyaluronic acid or corticosteroids for knee osteoarthritis : A prospective randomized controlled study. Orthopade. 2019;48(3):239–47. 10.1007/s00132-018-03659-5 [DOI] [PubMed] [Google Scholar]
- 23.Raeissadat SA, Ghazi Hosseini P, Bahrami MH, et al. The comparison effects of intra-articular injection of Platelet Rich Plasma (PRP), Plasma Rich in Growth Factor (PRGF), Hyaluronic Acid (HA), and ozone in knee osteoarthritis; a one year randomized clinical trial. BMC Musculoskelet Disord. 2021;22(1):134. 10.1186/s12891-021-04017-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sdeek M, Sabry D, El-Sdeek H, Darweash A. Intra-articular injection of Platelet rich plasma versus Hyaluronic acid for moderate knee osteoarthritis. A prospective, double-blind randomized controlled trial on 189 patients with follow-up for three years. Acta Orthop Belg. 2021;87(4):729–34. 10.52628/87.4.18 [DOI] [PubMed] [Google Scholar]
- 25.Dulic O, Rasovic P, Lalic I, et al. Bone marrow aspirate concentrate versus platelet rich plasma or hyaluronic acid for the treatment of knee osteoarthritis. Medicina (Kaunas). 2021;57(11):1193. 10.3390/medicina57111193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Di Martino A, Di Matteo B, Papio T, et al. Platelet-rich plasma versus hyaluronic acid injections for the treatment of knee osteoarthritis: results at 5 years of a double-blind, randomized controlled trial. Am J Sports Med. 2019;47(2):347–54. 10.1177/0363546518814532 [DOI] [PubMed] [Google Scholar]
- 27.Villanova-López MM, Núñez-Núñez M, Fernández-Prieto D, et al. Randomized, double-blind, controlled trial, phase III, to evaluate the use of platelet-rich plasma versus hyaluronic acid in hip coxarthrosis. Rev Esp Cir Ortop Traumatol (Engl Ed). 2020;64(2):134–42 (English, Spanish). [DOI] [PubMed] [Google Scholar]
- 28.Saltzman BM, Frank RM, Davey A, et al. Lack of standardization among clinical trials of injection therapies for knee osteoarthritis: a systematic review. Phys Sportsmed. 2020;48(3):266–89. 10.1080/00913847.2020.1726716 [DOI] [PubMed] [Google Scholar]
- 29.Schiphof D, de Klerk BM, Koes BW, Bierma-Zeinstra S. Good reliability, questionable validity of 25 different classification criteria of knee osteoarthritis: a systematic appraisal. J Clin Epidemiol. 2008;61(12):1205-1215.e2. 10.1016/j.jclinepi.2008.04.003 [DOI] [PubMed] [Google Scholar]
- 30.Schiphof D, Boers M, Bierma-Zeinstra SM. Differences in descriptions of Kellgren and Lawrence grades of knee osteoarthritis. Ann Rheum Dis. 2008;67(7):1034–6. 10.1136/ard.2007.079020 [DOI] [PubMed] [Google Scholar]
- 31.Bellamy N. Outcome measurement in osteoarthritis clinical trials. J Rheumatol Suppl. 1995;43:49–51. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.