Abstract
Objective
Individuals with obesity face unique challenges when visiting healthcare providers, including inadequate equipment. These negative care experiences, often exacerbated by weight stigma, frequently lead to mistrust and reluctance to seek future care. Currently, few instruments exist to ensure that an ambulatory clinic is welcoming to patients with obesity. The following clinical environment checklist was created with an aim to identify weaknesses in accommodating individuals of size.
Methods
A checklist of equipment considered ideal for the care of patients with obesity was developed through a comprehensive review of the literature and feedback from office staff. Eight ambulatory clinics within an urban Midwest setting were assessed, focusing on their accommodations for patients with obesity. Feedback from clinic staff was incorporated to further refine the checklist.
Results
Common equipment deficiencies included extra‐large blood pressure cuffs, wheelchair‐accessible scales, 2XL gowns, and adequate seat dimensions in the waiting area. Healthcare workers reported moral distress for their patients when unable to provide proper care due to these limitations. Newly constructed clinics exhibited better‐equipped facilities for patients with obesity.
Conclusions
Many clinics lack proper equipment to accommodate patients with obesity, resulting in negative care experiences. This clinical environment checklist can identify problem areas and provide solutions to create more welcoming environments, encouraging future care‐seeking behaviors.
Keywords: ambulatory, checklist, environment, obesity
We propose a clinical environment checklist to address the scarcity of instruments for assessing the accommodations of patients with obesity in outpatient clinics. We assessed ambulatory clinics and obtained feedback from clinic staff to formulate the following checklist identifying equipment deficiencies and offering solutions to improve care for patients with obesity.
1. INTRODUCTION
As the number of individuals with obesity increases, so do the health consequences that occur as a result, necessitating more frequent utilization of medical services. Individuals with obesity face unique challenges when visiting healthcare providers, including a lack of appropriate equipment within the healthcare setting and stigmatization, both resulting in decreased routine preventative care, including cancer screenings and vaccinations. 1 , 2 People with obesity frequently encounter care team members who hold negative weight‐based stereotypes or weight bias, which subsequently influence future interactions. 3 Patients who experience stigma from care suffer heightened stress and lowered self‐confidence, consequently leading to decreased adherence to care in the future. 4
Weight bias in healthcare settings has significant emotional and behavioral ramifications for patients with obesity, such as depression, stress, and lower self‐esteem. 5 , 6 Cognitive performance and communication can be impaired by these mental health effects. 7 Moreover, weight stigma not only impairs weight loss programs and treatment outcomes through inconsistent self‐monitoring, increased caloric intake, and reduced energy expenditure but also contributes to weight gain through maladaptive coping mechanisms in response, such as binge eating. 8 , 9 , 10 These implications highlight the importance of addressing weight bias to promote enhanced overall health and well‐being in patients with obesity.
In addition to the harmful impact on mental health, encountering stigma in the clinical setting may cause patients with obesity to be more inclined to delay or fully avoid care in the future. 11 , 12 Despite the best intentions of a physician to provide high‐quality care, past experiences of poor treatment can cause the patient to feel disrespected or upset, resulting in future avoidance of the situation. 4 This includes humiliating encounters such as the inability to fit in a waiting room chair or being weighed in a public space. When patients encounter these problems, the message they receive is that they are abnormal and that the clinic is not intended for them. Clinical environment shortcomings may not be considered by a provider when assessing obesity bias in the office; however, they can have a profound impact within the patient‐provider relationship. Appropriate and accommodating medical equipment may facilitate enhanced confidence in patients with obesity and promote positive interactions with healthcare providers.
The inadequacy of equipment for patients with obesity in the ambulatory setting is evident across multiple studies. 1 , 2 , 13 Recent findings suggest that less than 20% of primary care offices have height adjustable examination tables and only 11% have a wheelchair accessible weight scale. 13 Primary care physicians are often reluctant to transfer patients with obesity onto standard exam tables, citing safety concerns. Due to difficulties accessing scales accommodating higher weights, providers have no choice but to rely on patient self‐reported weights or refer them to a hospital to obtain a measurement. 1 Undersized gowns, exam tables and blood pressure cuffs are significant barriers to receiving appropriate care for this population, notably delaying their attendance at vital age‐appropriate cancer screening visits. 2 A lack of accessible diagnostic equipment in clinics not only poses physical and emotional hurdles for these patients but also hampers the overall quality of care they receive. There is a continued need to assess and expand accommodations for patients with obesity in ambulatory settings.
Health facilities should aim to be sensitive to the unique needs faced by individuals with obesity by fostering a safe and non‐judgmental atmosphere. By creating a welcoming atmosphere, not only do patients feel more comfortable but their trust in healthcare providers is also bolstered, thereby enhancing the likelihood of adherence to treatment plans. While a few clinical environment checklists exist, such as those from the Canadian Obesity Clinical Guidelines, updates are warranted to address the needs of an increasing population of patients with clinically severe obesity who may not be properly accommodated. 14 Additionally, the following checklist is purposefully concise to allow a quick evaluation of the environment. There remains a pressing need for tools that assist healthcare providers in creating a more inclusive environment for their patients. Here, a clinical environment checklist is proposed with the aim of identifying weaknesses in accommodating patients with obesity.
2. METHODS
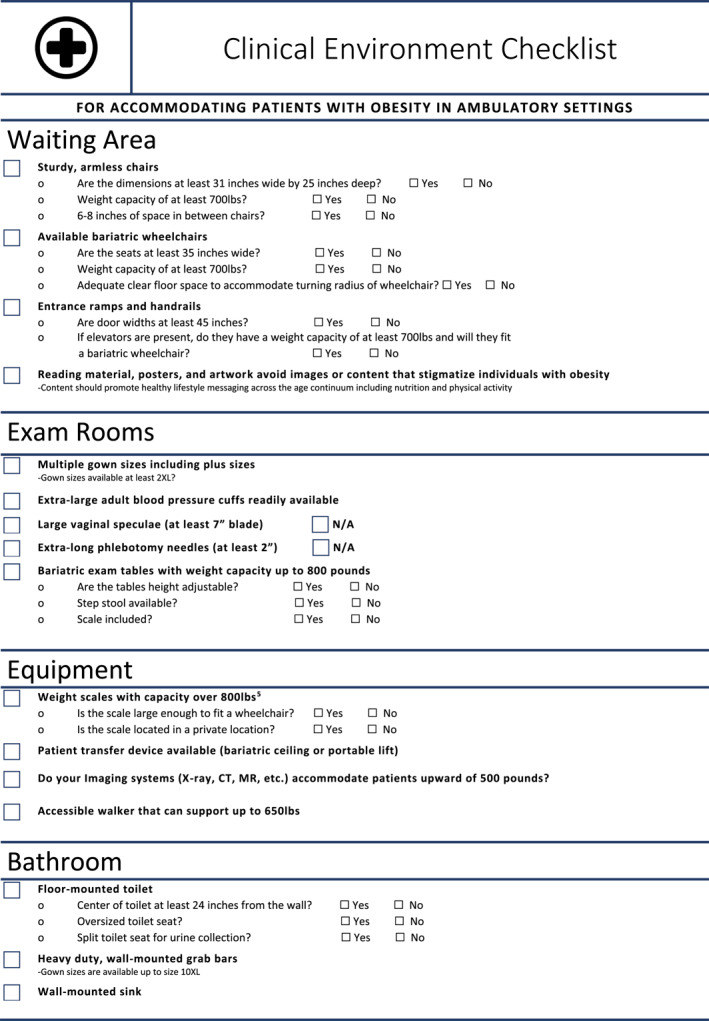
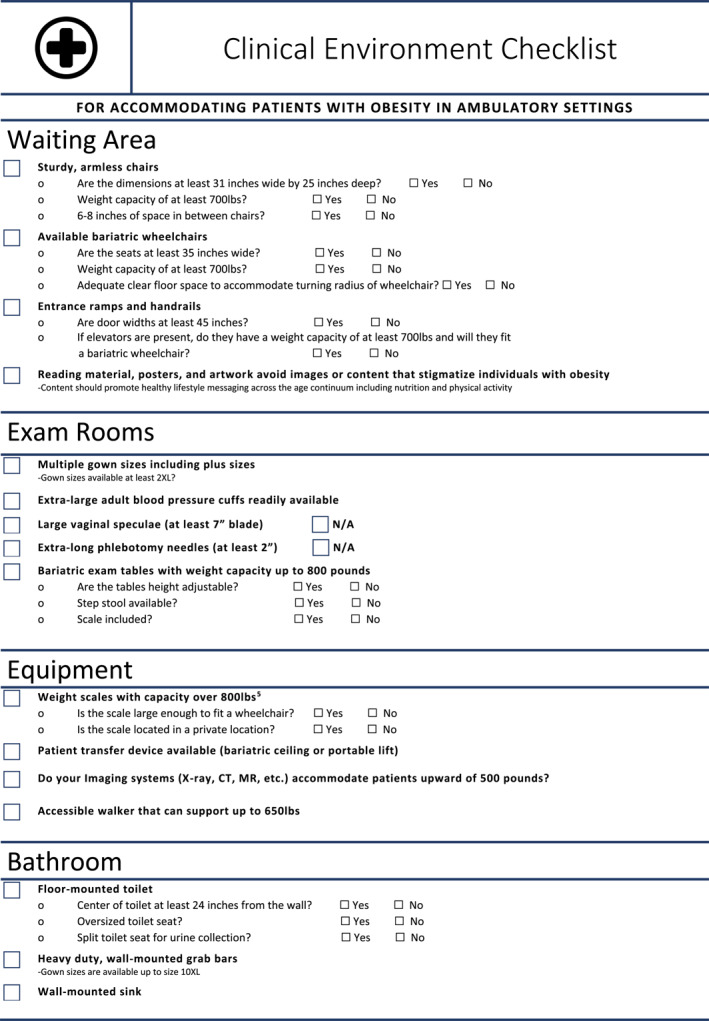
A comprehensive checklist focusing on equipment, furniture, and design tailored for the care of patients with obesity was first developed. This checklist was guided by architectural statements, recommendations from government organizations, and scientific research. 15 , 16 , 17 The checklist was piloted in several ambulatory settings for feedback. Ambulatory settings were defined as healthcare environments where patients receive care on an outpatient basis without overnight stays. Feedback was obtained from front‐office staff, medical assistants, and registered nurses on the relevance of the checklist and the most pressing problems they encountered during visits with this population. This information was incorporated to further refine and consolidate the checklist, ensuring that no important factors were overlooked. Notably, federal guidelines and rules do not fully address standards for equipment accessibility for people with obesity, instead noting that there is “insufficient data to determine specific criteria at this time.” 1 , 18 Continuing to update recommendations for clinic facilities and proper equipment is a critical tool to improve care and optimize outcomes in this rising patient population. This checklist serves as a helpful resource for those setting up a clinic or evaluating their current clinical environment, verifying that they have the necessary equipment to provide quality care and create a comfortable environment for patients with obesity (Table 1).
TABLE 1.
Clinical environment checklist for accommodating individuals of size.
|
3. RESULTS
The clinical environment checklist was implemented across eight ambulatory clinics in a large Midwest city. These included specialty clinics (Obstetrics and Gynecology, Bariatric Surgery, Cardiology, Urology, Ophthalmology, and Neurology) and a primary care facility (Table 2). This variety of clinical settings provided a wide‐ranging assessment of accommodations available for patients with obesity across different medical specialties.
TABLE 2.
Compliance with clinical environment checklist items in eight ambulatory clinics.
| Checklist item | Met recommendations N (%) | Did not meet recommendations N (%) | Not assessed/not applicable N (%) |
|---|---|---|---|
| Waiting area | |||
| Sturdy, armless chairs | 7 (87.5%) | 1 (12.5%) | 0 (0%) |
| Chairs at least 31 × 25” | 6 (75%) | 2 (25%) | 0 (0%) |
| Chair capacity 700 pounds (lb) | 2 (25%) | 2 (25%) | 4 (50%) |
| 6–8″ between chairs | 4 (50%) | 4 (50%) | 0 (0%) |
| Bariatric wheelchairs available | 5 (62.5%) | 3 (37.5%) | 0 (0%) |
| Wheelchair seats 35″ wide | 5 (62.5%) | 3 (37.5%) | 0 (0%) |
| Wheelchair capacity 700 lb | 5 (62.5%) | 3 (37.5%) | 0 (0%) |
| Sufficient floor space for wheelchair | 6 (75%) | 2 (25%) | 0 (0%) |
| Ramps and handrails | 3 (37.5%) | 4 (50%) | 1 (12.5%) |
| Door widths 45″ | 5 (62.5%) | 3 (37.5%) | 0 (0%) |
| Elevator weight capacity | 5 (62.5%) | 0 (0%) | 3 (37.5%) |
| Reading materials | 8 (100%) | 0 (0%) | 0 (0%) |
| Exam rooms | |||
| Plus‐sized gowns | 6 (75%) | 1 (12.5%) | 1 (12.5%) |
| Extra large cuffs | 7 (87.5%) | 1 (12.5%) | 0 (0%) |
| Large vaginal speculae | 4 (50%) | 0 (0%) | 4 (50%) |
| Phlebotomy needles 2″ | 1 (12.5%) | 4 (50%) | 3 (37.5%) |
| Bariatric exam table | 3 (37.5%) | 4 (50%) | 1 (12.5%) |
| Height adjustable exam table | 5 (62.5%) | 2 (25%) | 1 (12.5%) |
| Step stool | 5 (62.5%) | 0 (0%) | 3 (37.5%) |
| Exam table with scale included | 1 (12.5%) | 6 (75%) | 1 (12.5%) |
| Equipment | |||
| Scale capacity 800 lb | 6 (75%) | 1 (12.5%) | 1 (12.5%) |
| Scale fits a wheelchair | 5 (62.5%) | 2 (25%) | 1 (12.5%) |
| Scale in private location | 3 (37.5%) | 4 (50%) | 1 (12.5%) |
| Bariatric lift available | 3 (37.5%) | 4 (50%) | 1 (12.5%) |
| Imaging accommodates 500 lb | 6 (75%) | 1 (12.5%) | 1 (12.5%) |
| Walker supports 650 lb | 3 (37.5%) | 3 (37.5%) | 2 (25%) |
| Bathroom | |||
| Floor‐mounted toilet | 6 (75%) | 1 (12.5%) | 1 (12.5%) |
| Toilet 24″ from wall | 2 (25%) | 5 (62.5%) | 1 (12.5%) |
| Oversized seat | 3 (37.5%) | 4 (50%) | 1 (12.5%) |
| Split toilet seat | 7 (87.5%) | 0 (0%) | 1 (12.5%) |
| Wall‐mounted grab bars | 7 (87.5%) | 0 (0%) | 1 (12.5%) |
| Wall‐mounted sink | 7 (87.5%) | 0 (0%) | 1 (12.5%) |
Following implementation and feedback, several refinements were made to the clinical environment checklist to enhance its clarity and applicability across diverse clinical settings. For instance, the checklist now includes a specific item for door widths, ensuring accessibility for patients using larger mobility aids. In response to staff feedback highlighting the variability in equipment needs across specialties, we added “not applicable” options for items such as vaginal speculae and extra‐long phlebotomy needles. Additionally, based on consistent feedback from multiple sites, the checklist now explicitly asks whether the scale is large enough to accommodate a wheelchair, addressing a major concern raised by staff. These modifications and additions have improved the checklist's utility as an assessment tool to provide comfortable and dignified care to patients across the weight spectrum.
4. DISCUSSION
The instrument was trialed in several clinic environments, encompassing a wide array of specialty care settings. The outcomes revealed mixed adherence to the checklist items, with some clinics meeting most or all the requirements, while others displayed larger gaps in care. Many ambulatory clinics lacked accessible equipment, with the most common deficiencies being extra‐large blood pressure cuffs, wheelchair accessible weight scales, 2XL gowns, and adequate seat dimensions in the waiting area. Waiting areas rarely had armless chairs or chair dimensions for an individual with a higher body weight to comfortably await their appointment. The absence of a patient lift or transfer device was observed in nearly all clinics. As a result, physicians may be required to examine patients while they remain seated in a chair or wheelchair, negatively impacting the care they provide. Unlike recent findings demonstrating that only approximately 20% of clinics are equipped with height‐adjustable examination tables, all of the clinics evaluated possessed this equipment. 13 On average, the exam tables had a maximum weight capacity of 500 pounds (227 kg), while some were able to accommodate individuals up to 650 pounds (295 kg). Patients with obesity at these clinics were likely to experience challenges with diagnostic equipment such as CT or X‐ray; however, most clinics were situated near hospitals, which enabled direct referrals for patients requiring this equipment. It should be noted that the assessment was conducted solely in an urban setting, and obtaining imaging may prove more difficult in rural areas. Unsurprisingly, the more recently constructed clinics exhibited better‐equipped facilities to cater to the needs of patients with obesity, suggesting the importance of modern clinic design in accommodating this patient population effectively.
Qualitative feedback received from office staff, including nurses and medical assistants, aligns with past research highlighting equipment inadequacies. 1 , 2 , 13 Specifically, staff consistently reported insufficiently sized blood pressure cuffs and scales that were not wheelchair accessible. Consistent with past studies, multiple clinics reported difficulty weighing patients, hindering accurate weight measurements. This has significant implications for evaluating risk factors, monitoring weight loss progress, and determining eligibility for bariatric surgery. Several healthcare workers expressed distress stemming from the impact of these deficiencies on patient care. Through first‐hand accounts from medical personnel, a better understanding of the most pressing issues was obtained, helping to further optimize the checklist.
5. CONCLUSION
There continues to be a gap in the literature concerning accommodations for patients with obesity in the ambulatory setting. This checklist serves as a resource for clinic administrators, staff, and providers to evaluate their current clinical environment or plan for future equipment. A quantitative study utilizing this checklist would be useful to examine accommodations more thoroughly across various ambulatory healthcare settings. Limitations of this preliminary study include the small sample size of clinics assessed, the geographic confinement to one region, and the lack of qualitative data from subjective patient experiences. Incorporating the perspectives of individuals living with obesity is essential for the continued development of this clinical checklist. Moreover, only limited validity evidence is provided for this instrument; future studies might aim to collect relationships to other variables, internal structure, and consequence evidence. Future research should include collecting patient feedback on the checklist to identify the most distressing deficiencies and further elucidate approaches to mitigate stigma in the ambulatory setting. Continued development and testing of interventions to enhance clinic environments based on the checklist could demonstrate an impact on patient engagement and outcomes. Additional research focused on improving the clinical environment is warranted to ensure that facilities provide accessible, respectful, and compassionate care to patients with obesity.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ACKNOWLEDGMENTS
This publication is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award (T99HP39199). The contents are those of the author(s) and do not necessarily represent the official views of or an endorsement by HRSA, HHS or the U.S. Government.
Boland W, Li WS, Dilly CK. Accommodating patients with obesity in ambulatory care: a clinical environment checklist. Obes Sci Pract. 2024;e70006. 10.1002/osp4.70006
REFERENCES
- 1. Agaronnik ND, Lagu T, DeJong C, et al. Accommodating patients with obesity and mobility difficulties: observations from physicians. Disabil Health J. 2021;14(1):100951. 10.1016/j.dhjo.2020.100951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for White and African‐American obese women. Int J Obes. 2006;30(1):147‐155. 10.1038/sj.ijo.0803105 [DOI] [PubMed] [Google Scholar]
- 3. Rubino F, Puhl RM, Cummings DE, et al. Joint international consensus statement for ending stigma of obesity. Nat Med. 2020;26(4):485‐497. 10.1038/s41591-020-0803-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319‐326. 10.1111/obr.12266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hemmingsson E. A new model of the role of psychological and emotional distress in promoting obesity: conceptual review with implications for treatment and prevention. Obes Rev. 2014;15(9):769‐779. 10.1111/obr.12197 [DOI] [PubMed] [Google Scholar]
- 6. Hilbert A, Braehler E, Haeuser W, Zenger M. Weight bias internalization, core self‐evaluation, and health in overweight and obese persons. Obesity. 2014;22(1):79‐85. 10.1002/oby.20561 [DOI] [PubMed] [Google Scholar]
- 7. Schmader T, Johns M, Forbes C. An integrated process model of stereotype threat effects on performance. Psychol Rev. 2008;115(2):336‐356. 10.1037/0033-295x.115.2.336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Carels RA, Young KM, Wott CB, et al. Weight bias and weight loss treatment outcomes in treatment‐seeking adults. Ann Behav Med. 2009;37(3):350‐355. 10.1007/s12160-009-9109-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ashmore JA, Friedman KE, Reichmann SK, Musante GJ. Weight‐based stigmatization, psychological distress, and binge eating behavior among obese treatment‐seeking adults. Eat Behav. 2008;9(2):203‐209. 10.1016/j.eatbeh.2007.09.006 [DOI] [PubMed] [Google Scholar]
- 10. Puhl RM, Himmelstein MS, Pearl RL. Weight stigma as a psychosocial contributor to obesity. Am Psychol. 2020;75(2):274‐289. 10.1037/amp0000538 [DOI] [PubMed] [Google Scholar]
- 11. Drury CA, Louis M. Exploring the association between body weight, stigma of obesity, and health care avoidance. J Am Acad Nurse Pract. 2002;14(12):554‐561. [DOI] [PubMed] [Google Scholar]
- 12. Alberga AS, Edache IY, Forhan M, Russell‐Mayhew S. Weight bias and health care utilization: a scoping review. Prim Health Care Res Dev. 2019;20:e116. 10.1017/s1463423619000227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mudrick NR, Swager LC, Breslin ML. Presence of accessible equipment and interior elements in primary care offices. Health Equity. 2019;3(1):275‐279. 10.1089/heq.2019.0006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Forhan MGC, Hung P. Enabling participation in activities of daily living for people living with obesity. In: Canadian Adult Obesity Clinical Practice Guidelines [Internet]; 2020. obesitycanada.ca/guidelines. https://obesitycanada.ca/guidelines/participation [Google Scholar]
- 15. Bariatric Safe Patient Handling and Mobility Guidebook: A Resource Guide for Care of Persons of Size. : VHA Center for Engineering & Occupational Safety and Health (CEOSH); 2015. [Google Scholar]
- 16. Wignall D. Design as a critical tool in bariatric patient care. J Diabetes Sci Technol. 2008;2(2):263‐267. 10.1177/193229680800200216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Andrade SD. Planning and Design Guidelines for Bariatric Healthcare Facilities. The American Institute of Architects; 2006. [Google Scholar]
- 18. Architectural, Transportation Barriers Compliance B . Standards for accessible medical diagnostic equipment. Final rule. Fed Regist. 2017;82(5):2810‐2848. [PubMed] [Google Scholar]


