Abstract
Background
Crohn’s disease (CD) predisposes patients to intestinal obstruction (IO), a severe complication. This study examined the outcomes and healthcare utilization of patients with CD and IO using data from the National Inpatient Sample (NIS).
Methods
This retrospective analysis of NIS data from 2016-2020 compared hospitalized adult CD patients with and without IO. Outcomes studied include in-hospital mortality, length of stay (LOS), hospitalization charges, and the requirement for intervention, using regression models for adjustment.
Results
Among the 304,149 CD patients, 27,024 had IO. These patients experienced higher in-hospital mortality (3.9% vs. 1.8% for non-IO, adjusted odds ratio [aOR] 1.78, 95% confidence interval [CI] 1.09-2.89; P=0.02), longer mean LOS (7.23 vs. 4.53 days for non-IO, P<0.001), and higher average hospitalization charges ($71,775 vs. $43,717 for non-IO, P<0.001). Additionally, they had higher odds of requiring admission to the intensive care unit (aOR 1.99, 95%CI 1.45-2.73; P<0.001), intubation (aOR 2.53, 95%CI 1.74-3.68; P<0.001), balloon dilation (aOR 1.50, 95%CI 1.132-1.98; P=0.005), or intestinal resection (aOR 2.29, 95%CI 2.11-2.49; P<0.001).
Conclusions
CD patients with IO face considerable challenges, including greater mortality, longer hospital stays, and higher hospitalization costs. The need for intensive care and surgical interventions highlights the urgent need for improved management and treatment strategies to enhance outcomes for these patients.
Keywords: Crohn’s disease, intestinal obstruction, outcomes, in-hospital mortality, predictors
Introduction
Crohn’s disease (CD) is a chronic inflammatory bowel disease that increases the risk of patients developing intestinal obstruction, one of its most challenging complications. The transmural inflammation inherent to CD can lead to the thickening of the intestinal wall, fibrosis, and ultimately to the formation of strictures. These strictures narrow the intestinal lumen, impeding the passage of intestinal contents and in some cases leading to obstruction [1]. Additionally, chronic inflammation may also promote the formation of adhesions and fistulas. As the disease progresses, segments of the intestine may become significantly narrowed or blocked, necessitating medical or surgical intervention [2].
Recent studies have shown an increasing trend in hospitalizations for CD, with intestinal obstruction being one of the leading causes of admission, underscoring the importance of understanding the outcomes and resource utilization in this patient population [3]. Despite advances in medical therapies aimed at reducing inflammation and preventing complications, a significant proportion of patients with CD still face intestinal obstruction due to stricturing, where scar tissue narrows the intestine, and penetrating (fistulizing) disease, which forms abnormal connections that can indirectly cause obstruction by altering the intestinal flow or may progress to inflammation and infection around the fistula, often resulting in additional strictures. Consequently, approximately 70% of CD patients require surgery to manage these complications [4,5].
To address these issues further, this study utilized the National Inpatient Sample (NIS) to analyze the characteristics and outcomes of hospitalized adult patients with CD who develop intestinal obstruction.
Materials and methods
Study design and database description
This was a retrospective analysis of adult patients hospitalized with CD. Data were extracted from the NIS database, covering 2016-2020. The NIS is structured as a stratified probability sample, designed to accurately reflect the landscape of non-federal acute care hospitals across the United States. Specifically, a 20% stratified probability sample of all hospitals is selected for inclusion in the database. Each hospital discharge record in the sample is assigned a weight to ensure national representativeness. This weight is calculated by dividing the total number of discharges from all acute care hospitals in the USA by the number of discharges captured within the 20% sample. This methodological approach allows the findings to be extrapolated to the entire country, providing insights into the epidemiology and outcomes of CD at a national level.
Study patients
The study included patients admitted to the hospital because of exacerbations related to CD, identified through the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes. The analysis differentiated between CD patients with and without intestinal obstruction. Individuals under the age of 18 were excluded from the study. Although Institutional Review Board (IRB) approval was initially pursued, the study was ultimately exempted. This exemption was granted based on the utilization of de-identified, publicly available data, negating the need for traditional IRB oversight.
Study variables and outcomes
The primary outcome was in-hospital mortality, as reported in the NIS. The secondary outcomes were: length of stay (LOS), total hospitalization charges and costs, fistulas (abdominal wall, intestinal, sigmoid, abdominorectal, abdominosigmoid, cecosigmoidal, cecal, colon, enterocolic, enterocutaneous, ileorectal or ileosigmoidal, ileum, intestinocolonic, jejunum, pericecal, perineosigmoidal, rectosigmoid [intercommunicating], stercoral), fissures (acute anal, chronic anal fissures, anal fissure, unspecified fissures), megacolon, intestinal abscess, acute kidney injury and need for dialysis, cardiac arrest, hypovolemic shock, vasopressors and need for intubation, septic shock, admission to the intensive care unit (ICU) or parenteral nutrition. The following potential confounders were considered: age in years, sex, race, admission day as weekend or weekday, median income in the patient’s zip code in 4 hierarchical categories, patient comorbidities as measured by the Deyo adaptation of the Charlson comorbidity index for administrative data, hospital location, hospital region, hospital teaching status as teaching or non-teaching, and hospital size (no. of beds).
Statistical analysis
Analyses were performed using STATA, version MP 14.2 (StataCorp, College Station, Texas, United States). We used univariable logistic regression to calculate unadjusted odds ratios (ORs). We used multivariate regression analysis to adjust for confounding factors. A non-parsimonious multivariate logistic regression model was developed to estimate the propensity score. A binomial family and a logit linkage were specified when modeling the propensity score [6]. The double robust method was used to generate treatment weights, and the inverse probability of treatment weighting was used to match cases with controls using generalized linear models [6]. In the second analysis, multivariable regression models were created by including all confounders significantly associated with the outcome in the univariable analysis with a cutoff P-value of 0.2 [7]. Variables that were considered clinically important for the outcome based on the literature review were also included in the model, regardless of whether they were significantly associated with each other in the univariable analysis. A logistic regression model was used for binary outcomes and a linear regression model for continuous outcomes. For other calculations, Fisher’s exact test for proportions and Student’s t-test for continuous variables were used. All P-values were two-sided, with 0.05 as the threshold for statistical significance.
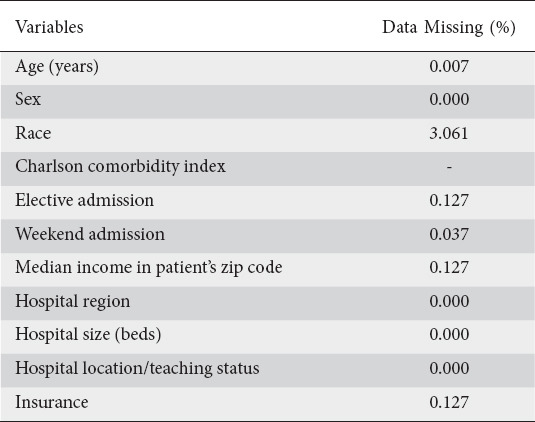
Missing data
There were no missing data for the hospital variables (Table 1). However, there were missing data for some patient characteristic variables. For most variables, the percentage of missing data was minimal (<0.5%), with the exception of race (3.06%). To test whether missing data could lead to bias, we assumed that data were not missing at random and applied the multivariate imputation by chained equations (MICE) method, estimated from sequential multivariable models with fully conditional specifications [8]. A total of 10 imputed data sets were created that included information from all covariates used in the regression models and other covariates in the database with no missing information. The results with and without imputation were similar. Therefore, the results without imputation are reported.
Table 1.
Missing data
Results
Patient characteristics
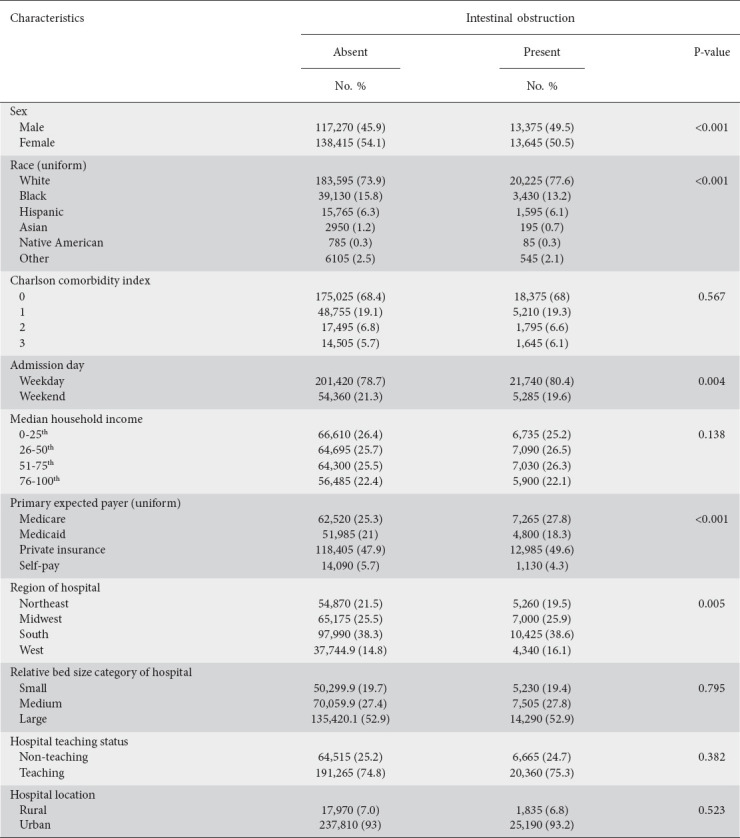
Patient demographics are shown in Fig. 1. The total number of patients in the studied NIS cohort was 174,776,186, of whom 304,149 had a diagnosis of CD. Among patients with CD, 27,024 had intestinal obstruction. Patients with intestinal obstruction were more likely to be White males and insured by Medicaid or private insurance, and less likely to have Medicare, compared to CD patients without intestinal obstruction (Table 2). Among CD patients, intestinal obstruction was more prevalent in the White population. The other characteristics were not statistically different between the 2 patient groups.
Figure 1.
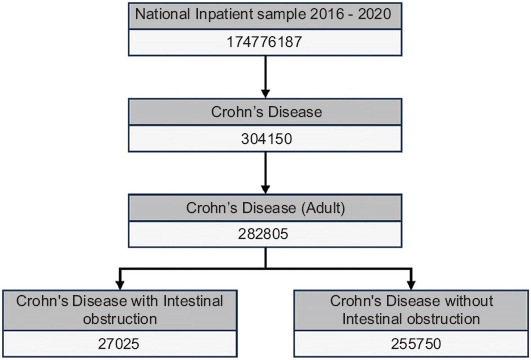
Demographic breakdown of Crohn’s disease patients from National Inpatient Sample discharge data
Table 2.
Patient and hospital characteristics for Crohn’s disease patients with and without intestinal obstruction
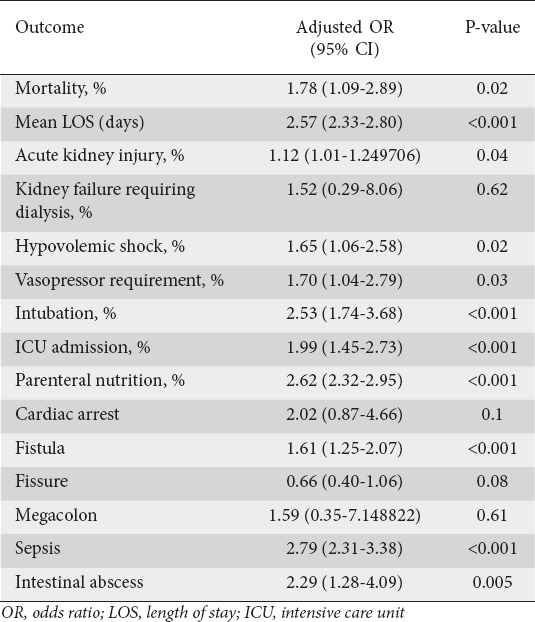
Mortality
The overall inpatient mortality in CD patients was 1.9% (5778). Mortality was 3.9% (1053) in CD patients with intestinal obstruction and 1.8% (4988) in patients without intestinal obstruction (unadjusted). CD patients with intestinal obstruction had a higher risk of in-hospital mortality compared to patients without intestinal obstruction (adjusted odds ratio [aOR] 1.78, 95% confidence interval [CI] 1.09-2.89; P=0.02) (Table 3).
Table 3.
Primary and secondary outcomes
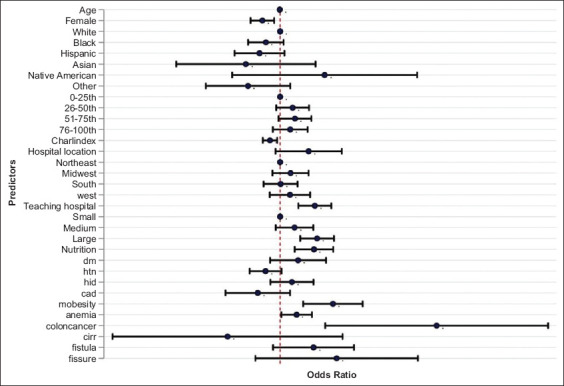
Independent predictors of mortality
The strength of the association of mortality from intestinal obstruction in CD patients with multiple variables was tested individually using univariate regression analysis. Multiple patient, hospital, and treatment-level variables were tested. The final model is presented in Fig. 2. The variables found to be independent predictors of increased mortality from intestinal obstruction in patients with CD were anemia, malnourishment, and the Charlson comorbidity index, which quantifies the burden of comorbid conditions by assigning scores based on the presence and severity of various medical conditions.
Figure 2.
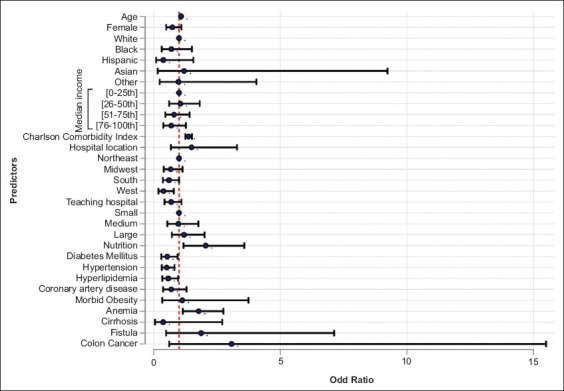
Predictors of mortality in Crohn’s disease patients with intestinal obstruction
Morbidity
The overall rate of fistulas was 0.8% and 0.1% among patients with and without intestinal obstruction, respectively, and this difference was significant after adjusting for confounders (aOR 1.61, 95%CI 1.25-2.07; P<0.001). Similarly, the rate of intestinal abscess formation differed significantly between the 2 subgroups (aOR 2.29, 95%CI 1.28-4.08; P<0.001). The rate of megacolon and intestinal fissures did not differ between the 2 groups (Table 3).
Treatment setting and length of stay
The overall mean LOS was 4.79 days for patients hospitalized with CD, 4.53 days for patients without intestinal obstruction, and 7.23 days for patients with intestinal obstruction. After adjusting for confounders, patients with intestinal obstruction had a comparative mean LOS that was significantly higher by 2.56 days (P<0.001).
The odds of requiring an ICU stay were twice as high for CD patients with intestinal obstruction compared with patients without intestinal obstruction (aOR 1.99, 95%CI 1.45-2.73; P<0.001). Similarly, CD patients had higher odds of requiring intubation and vasopressor therapy (aOR 2.53, 95%CI 1.74-3.68; P<0.001) and (aOR 1.70, 95%CI 1.04-2.79; P=0.03) respectively (Table 3). Malnourishment was identified as an independent predictor for ICU admission (aOR 5.93, 95%CI 3.29-10.70; P<0.001), and the need for intubation (aOR 1.52, 95%CI 1.20-1.94; P<0.001) in CD patients with intestinal obstruction (Figs. 3 and 4 respectively).
Figure 3.
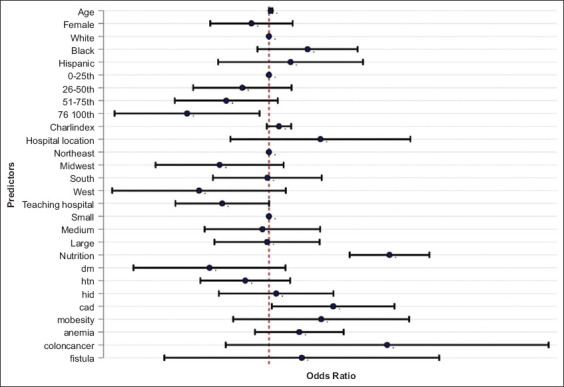
Predictors of Intensive Care Unit Admission in Crohn’s disease patients with Intestinal obstruction
Figure 4.
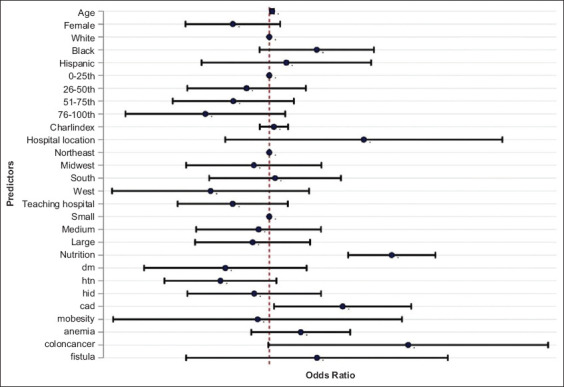
Predictors of intubation in Crohn’s disease patients with intestinal obstruction
Resource utilization
The total cost of hospitalization and parenteral nutrition was used as a marker for resource utilization. Mean hospitalization charges per patient were $46,395.97 (95%CI 45,434.07-47,357.87) for the entire study population, $71,775 (95%CI $68,665-74,886) for patients with intestinal obstruction, and $43,717.018 (95%CI $42,813-44,621) for patients without bowel obstruction (unadjusted). After adjusting for confounders, total hospitalization charges for patients with bowel obstruction were significantly higher by $27,293 (P<0.001). Patients with bowel obstruction had higher odds of requiring parenteral nutrition (aOR 2.61, 95%CI 2.32-2.94; P<0.001) (Table 3).
Treatment modalities
Balloon dilation and Intestinal resection
Among CD patients with intestinal obstruction, the total number of interventions was 29,780, with balloon dilation and intestinal resection being 2,070 (7%) and 27,710 (93%), respectively. The likelihood of requiring surgical or endoscopic intervention among CD patients with intestinal obstruction was 19.69%, compared to 9.56% for those without obstruction (aOR 2.24, 95%CI 2.07-2.44; P<0.001).
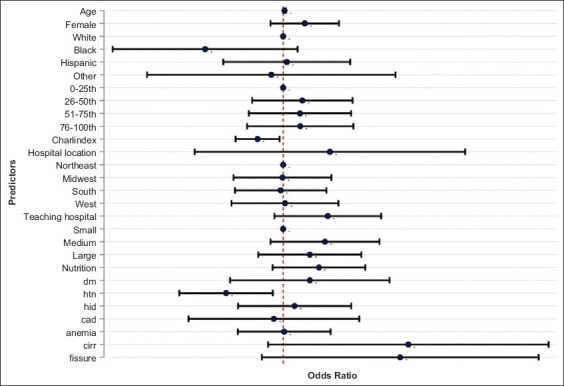
After adjusting for confounding factors, patients with intestinal obstruction were 1.5 times more likely to undergo balloon dilation compared to those without obstruction (aOR 1.50, 95%CI 1.132-1.98; P=0.005). No significant predictors for increased risk of balloon dilation were identified (Fig. 5). Furthermore, intestinal resection was more than twice as likely in patients with intestinal obstruction compared to those without (aOR 2.29, 95%CI 2.11-2.49; P=0.005). Independent predictors of increased risk for intestinal resection included malnutrition (aOR 1.52, 95%CI 1.20-1.95; P=0.001), colon cancer (aOR 7.12, 95%CI 1.76-28.83; P=0.006), and morbid obesity (aOR 1.93, 95%CI 1.34-2.82; P=0.001). The procedure was also more frequently performed in large teaching hospitals (aOR 1.58, 95%CI 1.28-1.96; P=0.005) and in males (aOR 2.29, 95%CI 2.11-2.49; P=0.001). Fig. 6 provides detailed predictors for the increased risk of intestinal resection.
Figure 5.
Predictors of balloon dilation in Crohn’s disease patients with intestinal obstruction
Figure 6.
Predictors of intestinal resection in Crohn’s disease patients with intestinal obstruction
Discussion
Our study included 304,149 patients diagnosed with CD, of whom 27,024 experienced intestinal obstruction. This subgroup had a significantly higher in-hospital mortality rate (3.9%) compared to patients without obstruction (1.8%). They also faced longer hospital stays and higher resource utilization, with patients experiencing obstruction having higher average hospital costs.
The prevalence of intestinal obstruction in CD, as observed in our study, is consistent with findings reported by Aniwan et al [3] and Torres et al [4], who noted an increasing trend in hospitalizations for CD, with a significant portion of these cases requiring surgical intervention because of stricturing or penetrating disease. This phenomenon underscores the transmural nature of CD, which inherently predisposes patients to develop strictures that can lead to obstruction [9,10]. Our analysis also highlights that white males, particularly those insured by Medicaid or private insurance, are more frequently diagnosed with intestinal obstruction. This observation suggests that demographic and socioeconomic factors may be at play, potentially influencing the progression of the disease and/or access to healthcare services [11,12].
Our findings also reveal that intestinal obstruction in CD is associated with significant increases in in-hospital mortality, ICU admissions, and the need for parenteral nutrition, reinforcing the severity of this complication. Previous reports have highlighted the progression towards complications requiring surgical intervention in up to 70% of CD patients over their disease course [13-15]. This is mirrored in our findings, where the necessity for interventions such as balloon dilation and intestinal resection was significantly more common in patients with intestinal obstruction, underscoring the critical role of timely and aggressive management strategies to mitigate complications and improve outcomes [16,17].
Our study showed no significant difference in the occurrence of fissures and fistulas between CD patients with and without intestinal obstruction. This contrasts with previous assumptions that structural complications in CD are closely linked with penetrating ones [18]. Our observations align with recent studies advocating for personalized care in CD, challenging the conventional correlation between structural and penetrating complications [19,20].
Our study had some limitations. First, the retrospective design of our study meant that the exposure was not fully randomized. We relied on multivariate regression models to account for confounding factors [21,22]. We also controlled for the different characteristics at the patient and hospital level, which further reduces the likelihood of confounding. Second, an administrative database was analyzed to obtain the data. The lack of detailed clinical information in such databases limits the ability to identify specific causes of mortality. Using ICD-10 codes instead of clinical parameters may lead to misclassification of diagnoses. ICD-10-CM codes were used to derive the data, which are more specific than ICD-9-CM and have shown high sensitivity and specificity in the study of gastrointestinal disorders [23].
Our study also had several strengths. We used the NIS, which includes data on patients with diverse hospital-level characteristics from more than 45 states. This results in superior external validity and generalizability; therefore, we believe the results obtained should reflect the patient population admitted to hospitals in the USA [24]. In addition, the NIS eliminates the common limitation of single-center studies by allowing a large sample size, as it is the largest publicly available, all-payer database that includes an inpatient population. Propensity matching is a powerful tool in analyzing administrative databases and helps control for confounding by indication [25]. It uses a wide range of empirically derived covariates that are surrogates for unmeasured confounding variables while comparing cases with controls [26,27]. Using nationally representative data in our study eliminated the biases associated with single- or multicenter studies. Similarly, the differentiated variables in the database provided the opportunity to account for elements such as estimated household income, hospitalizations, costs, and hospital factors, which is usually not possible in single-center studies. The findings of this study have important clinical implications, suggesting a potential paradigm shift in the management of CD, with early surgical intervention before complications like intestinal obstruction occur. Early identification and aggressive treatment strategies could potentially improve patient outcomes and quality of life [28].
In conclusion, our study underscores the severe burden of intestinal obstruction in patients with CD, not only in terms of clinical outcomes but also regarding healthcare resource utilization. It calls for a multidisciplinary approach to management that includes early identification, aggressive medical therapy, and, when necessary, surgical intervention to prevent complications. Our findings support the need for ongoing research into more effective treatments to mitigate the risk of obstruction in CD and improve patient care and outcomes.
Summary Box
What is already known:
Crohn’s disease (CD) is a chronic inflammatory condition that increases the risk of developing intestinal obstruction (IO)
IO is a severe complication of CD, leading to significant morbidity and often requiring medical or surgical intervention
Hospitalizations for CD are increasing, with IO being one of the leading causes of admission
Approximately 70% of CD patients will require surgery to manage complications such as stricturing or penetrating disease
What the new findings are:
CD patients with IO have significantly higher in-hospital mortality rates compared to those without IO
Patients with IO experience longer hospital stays and incur higher hospitalization charges
The need for intensive care and surgical interventions, such as intensive care unit admission, intubation, balloon dilation, and intestinal resection, is significantly higher in CD patients with IO
Independent predictors of increased mortality in CD patients with IO include anemia, malnourishment, and higher Charlson comorbidity index score
Biography
Rochester General Hospital, Rochester, NY; Saint Louis University, MO; Vanderbilt University Medical Center, Nashville, Tennessee; Center for Advanced Therapeutic Endoscopy, Centura Health, Denver, Colorado, USA
Footnotes
Conflict of Interest: DGA: Consultant, Boston Scientific. All other authors: No conflict of interest
References
- 1.Ford MM. Crohn's disease obstructions. Clin Colon Rectal Surg. 2021;34:227–232. doi: 10.1055/s-0041-1729926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldstone RN, Steinhagen RM. Abdominal emergencies in inflammatory bowel disease. Surg Clin North Am. 2019;99:1141–1150. doi: 10.1016/j.suc.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Aniwan S, Park SH, Loftus EV., Jr Epidemiology, natural history, and risk stratification of Crohn's disease. Gastroenterol Clin North Am. 2017;46:463–480. doi: 10.1016/j.gtc.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 4.Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn's disease. Lancet. 2017;389:1741–1755. doi: 10.1016/S0140-6736(16)31711-1. [DOI] [PubMed] [Google Scholar]
- 5.Rieder F, Fiocchi C, Rogler G. Mechanisms, management, and treatment of fibrosis in patients with inflammatory bowel diseases. Gastroenterology. 2017;152:340–350. doi: 10.1053/j.gastro.2016.09.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dugoff EH, Schuler M, Stuart EA. Generalizing observational study results:applying propensity score methods to complex surveys. Health Serv Res. 2014;49:284–303. doi: 10.1111/1475-6773.12090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vittinghoff E, Glidden DV, Shiboski SC, et al. Regression methods in biostatistics:linear, logistic, survival, and repeated measures models. 1st edition. Boston, MA: Springer; 2012. [Google Scholar]
- 8.White IR, Royston P, Wood AM. Multiple imputation using chained equations:Issues and guidance for practice. Stat Med. 2011;30:377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 9.Golovics PA, Mandel MD, Lovasz BD, Lakatos PL. Inflammatory bowel disease course in Crohn's disease:is the natural history changing? World J Gastroenterol. 2014;20:3198–3207. doi: 10.3748/wjg.v20.i12.3198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berg DF, Bahadursingh AM, Kaminski DL, Longo WE. Acute surgical emergencies in inflammatory bowel disease. Am J Surg. 2002;184:45–51. doi: 10.1016/s0002-9610(02)00879-6. [DOI] [PubMed] [Google Scholar]
- 11.Burbage SC, Krupsky KL, Cambron-Mellott MJ, et al. Racial and ethnic disparities health-related outcomes in Crohn's disease:results from the National Health and Wellness Survey. Crohns Colitis 360. 2024;6:otae021. doi: 10.1093/crocol/otae021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barnes EL, Nowell WB, Venkatachalam S, Dobes A, Kappelman MD. Racial and ethnic distribution of inflammatory bowel disease in the United States. Inflamm Bowel Dis. 2022;28:983–987. doi: 10.1093/ibd/izab219. [DOI] [PubMed] [Google Scholar]
- 13.Cho CW, You MW, Oh CH, Lee CK, Moon SK. Long-term disease course of Crohn's Disease:changes in disease location, phenotype, activities, and predictive factors. Gut Liver. 2022;16:157–170. doi: 10.5009/gnl210118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sacchetti F, Caprino P, Potenza AE, Pastena D, Presacco S, Sofo L. Early and late outcomes of a series of 255 patients with Crohn's disease who underwent resection:10 years of experience at a single referral center. Updates Surg. 2022;74:1657–1664. doi: 10.1007/s13304-022-01322-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prevention CfDCa. International classification of diseases, (ICD-10-CM/PCS) transition - background 2015. [[Accessed 16 July 2024]]. Available from: https://archive.cdc.gov/www_cdc_gov/nchs/icd/icd10cm_pcs_background.htm .
- 16.Cushing K, Higgins PDR. Management of Crohn disease:a review. JAMA. 2021;325:69–80. doi: 10.1001/jama.2020.18936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang W, Tang Y, Nong L, Sun Y. Risk factors for postoperative intra-abdominal septic complications after surgery in Crohn's disease:a meta-analysis of observational studies. J Crohns Colitis. 2015;9:293–301. doi: 10.1093/ecco-jcc/jju028. [DOI] [PubMed] [Google Scholar]
- 18.Hsu YC, Wu TC, Lo YC, Wang LS. Gastrointestinal complications and extraintestinal manifestations of inflammatory bowel disease in Taiwan:A population-based study. J Chin Med Assoc. 2017;80:56–62. doi: 10.1016/j.jcma.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 19.Clinton JW, Cross RK. Personalized treatment for Crohn's disease:current approaches and future directions. Clin Exp Gastroenterol. 2023;16:249–276. doi: 10.2147/CEG.S360248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borg-Bartolo SP, Boyapati RK, Satsangi J, et al. Precision medicine in inflammatory bowel disease:concept, progress and challenges. F1000Res. 2020;9 doi: 10.12688/f1000research.20928.1. F1000 Faculty Rev-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Memtsoudis SG. Limitations associated with the analysis of data from administrative databases. Anesthesiology. 2009;111:449. doi: 10.1097/ALN.0b013e3181adf739. [DOI] [PubMed] [Google Scholar]
- 22.Mori M, Brown KJ, Geirsson A. Understanding limitations of the National Inpatient Sample to facilitate its proper use. JAMA Surg. 2019;154:881–882. doi: 10.1001/jamasurg.2019.1172. [DOI] [PubMed] [Google Scholar]
- 23.Kalaria R, Desai D, Abraham P, et al. Temporal change in phenotypic behaviour in patients with Crohn's disease:do Indian patients behave differently from Western and other Asian patients? J Crohns Colitis. 2016;10:255–261. doi: 10.1093/ecco-jcc/jjv202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.HCUP National Inpatient Sample (NIS) Overview of the National (Nationwide) Inpatient Sample (NIS). Accessed February 14, 2020. [[Accessed 16 July 2024]]. Available from: https://www.hcup-us.ahrq.gov/nisoverview.jsp .
- 25.Seeger JD, Williams PL, Walker AM. An application of propensity score matching using claims data. Pharmacoepidemiol Drug Saf. 2005;14:465–476. doi: 10.1002/pds.1062. [DOI] [PubMed] [Google Scholar]
- 26.Austin PC, Wu CF, Lee DS, Tu JV. Comparing the high-dimensional propensity score for use with administrative data with propensity scores derived from high-quality clinical data. Statist Methods Med Res. 2020;29:568–588. doi: 10.1177/0962280219842362. [DOI] [PubMed] [Google Scholar]
- 27.Yu R, Silber JH, Rosenbaum PR. Rejoinder:matching methods for observational studies derived from large administrative databases. Statist Sci. 2020;35:371–374. [Google Scholar]
- 28.Xia K, Gao RY, Wu XC, Yin L, Chen CQ. Timing of individualized surgical intervention in Crohn's disease. World J Gastrointest Surg. 2022;14:1320–1328. doi: 10.4240/wjgs.v14.i12.1320. [DOI] [PMC free article] [PubMed] [Google Scholar]


