Abstract
The coexistence of a meningioma and an unruptured intracranial aneurysm was considered a rare phenomenon, accidentally detected by radiological assessment. The relationship between these 2 entities is complex and represents a neurosurgical challenge. We share our experience of a case involving a 36-year-old male patient with no prior medical history who consulted for chronic unilateral left periorbital headaches. The imaging diagnosis revealed 2 lesions, including a partially calcified jugo-olfactory meningioma and an anterior communicating artery aneurysm. He was successfully treated in a single surgical procedure using a left pterional craniotomy for excision of the meningioma followed by clipping of the aneurysm. The patient was discharged home on the fifth postoperative day in good clinical condition. This experience underlines the importance of preoperative imaging assessment, in order to make the right therapeutic decision and avoid unexpected intraoperative disasters.
Keywords: Meningioma, Cerebral aneurysm, Co-Existing, Cerebral angiography
Introduction
The association between intracranial aneurysms and brain tumours is a rare event, usually diagnosed incidentally, and was first reported by Arieti et al. [1,2]. Its incidence varied between 0.7% and 7.7% [1,3,4], but with the increased use of diagnosis imaging the reported incidences are higher in recent literature. This association was found predominantly in women [5]. We describe the case of an anterior communicating artery aneurysm and a jugo-olfactory meningioma, treated simultaneously using the same approach. Treatment guidelines for meningiomas coexisting with aneurysms have not been established and the priority of treatment is controversial.
Case presentation
Patient information: A 36-year-old man was admitted to our department for persistent chronic unilateral left periorbital headache. His medical history was unremarkable apart from cannabis use.
Clinical findings: At the admission, the patient was in good general status, Glasgow Coma Scale was 15/15. His neurological and ophthalmic examination was normal.
Diagnostic assessment
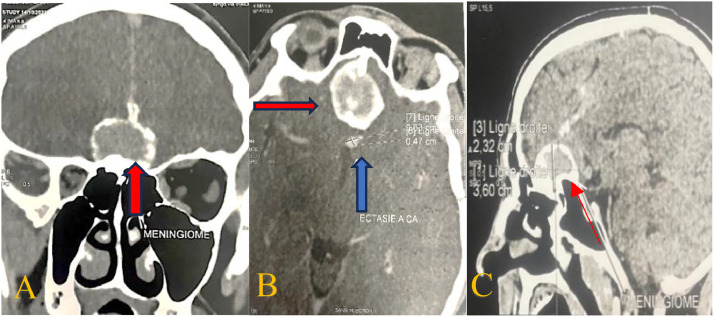
A computed tomography (CT) scan (Fig. 1) revealed a calcified basifrontal meningioma with ectasia of the anterior communicating artery.
Fig. 1.
Preoperative coronal (A), axial (B) and sagittal (C) CT scan showing a basal frontal meningioma (red arrow) associated to aneurysm (blue arrow) (B).
Cerebral magnetic resonance imaging (MRI) revealed a medial fronto-basal extraaxial mass with a calcified wall, centred on the jugo olfactory region, measuring 36 × 30 × 23 mm, with T1 and T2 iso signal, without diffusion restriction, with moderate enhancement after injection. It is relatively well circumscribed, exerting an imprint on the cerebral parenchyma opposite with small bilateral peri-lesional oedema. Adjacent nodular calcification on the anterior side of the brain scythe, measuring 8 × 10 × 10 mm.
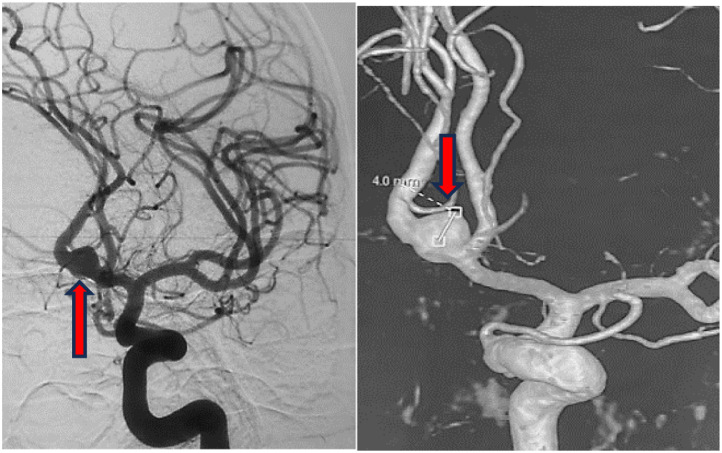
Cerebral angiography (Fig. 2) showed an anterior communicating artery (AComA) aneurysm arising from de Acom itself and filled from a left own in A1 an aplastic right A1, morphologically the aneurysm presents with a large neck of 5mm of diameter with 5mm height.
Fig. 2.
Cerebral angiography shows the anterior communicating artery aneurysm large neck (red arrow).
Therapeutic intervention
The patient underwent a left pterional craniotomy. Optico carotid arachnoid cistern was dissected and left internal carotid artery was identified, A1 segment was progressively dissected and identified for potential temporary clipping.
While progressing towards the anterior communicating artery Complex, the pressure from the frontal lobe pushed by the tumor was preventing optimal brain relaxation, we decided then to resect the meningioma allowing for more space to achieve the Anterior communicating complex. Olfactory groove meningioma was targeted at its base and resected safely using bipolar dissection and suction. It was moderately hemorrhagic and grossly calcified.
Excision was eventually Simpson grade II and anterior communicating artery complex was totally unraveled identifying both A2 segments, left A1 segment and the wide neck aneurysm. Temporary clipping of left A1 allowed for a lesser tension in the aneurysmal sac and a 7 mm Yassargil Clip could be safely applied at the neck. Temporary clip was removed and patency of A2 segments was checked.
Histopathology revealed a transitional and psammomatous meningioma (WHO grade I).
Follow-up and outcome
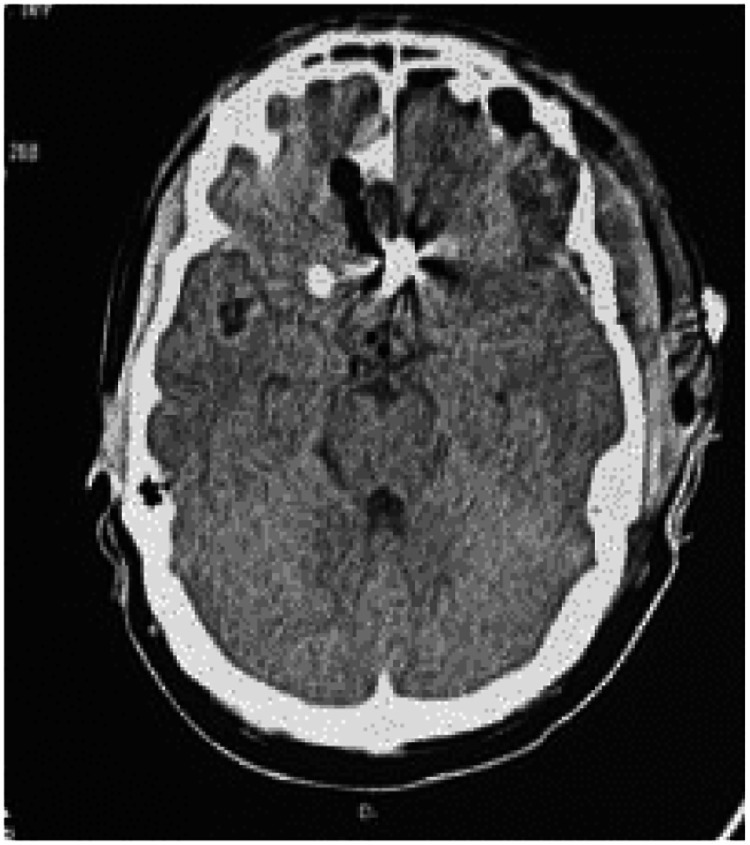
The patient had uneventful course; he was discharged at the fifth postoperative day without neurologic deficit. A postoperative CT scan showed resection of the meningioma and the aneurysm clip applied at the AComA site (Fig. 3).
Fig. 3.
A postoperative CT scan.
Discussion
Cerebral aneurysms have been associated with many tumor types, the meningioma representing the highest rate (29.3%-60%), followed by glioma (27.5%-38%), pituitary adenoma (11%-20.6%), lymphoma, craniopharyngioma, dermoid cyst and squamous cell carcinoma, chordoma and choroid plexus adenoma [2,3,4,6]. Our patient presented with a combination of the anterior communicating artery aneurysm and a jugo-olfactory meningioma.
The coexistence of an aneurysm with a meningioma can be divided into 3 categories: aneurysm related to feeding tumors, aneurysm not related to the feeding tumor and aneurysm enclosed in or close to the meningioma, as in our case [4].
In the literature, several hypotheses have been put forward to explain this collision, including hemodynamic factors, hormonal factors and a genetic factor. The hemodynamic factors are linked to an increase in directional blood flow due to a greater blood supply around slow-growing meningiomas, which could cause haemodynamic stress on the cerebral arteries leading to degeneration of the arterial wall and the formation of aneurysms, hormonal factors, such as the influence of IGF-1 on arterial walls (dilation of arteries, atherosclerosis), a genetic factor, notably in Klippel-Treaunay syndrome, which leads to an association between meningioma and aneurysm, but with insufficient evidence, and direct tumor invasion and neovascularization directed towards the tumor [1,6].
In general, the symptoms of a brain tumor progress gradually or rapidly depending on the degree of aggressiveness, whereas vascular problems usually present suddenly. Patients with meningiomas associated with symptomatic unruptured intracranial aneurysm must be diagnosed and treated rapidly, hence the importance of carefully evaluating the neuroimaging available (CT scan, MRI and cerebral arteriography) for each neurosurgical case, taking into account the clinical presentation of that case.
The choice of treatment is difficult because no guidelines or recommendations have been established for treating cases with both lesions. The consensus is that lesions presenting symptoms should be treated as a priority [4]. However, the proximal spatial relationship between the meningioma and the aneurysm remains the most important factor in deciding the treatment strategy. If the tumor is primary and proximal to the aneurysm, simultaneous resection and clipping have been proposed as the best treatment option [7]. As in our patient, first the meningioma was resected to reduce the mass effect, followed by clipping of the aneurysm.
Conclusion
The coexistence of an aneurysm and a meningioma can be difficult to manage and represents a challenge for any neurosurgeon. Although rare, it must be taken into account in the preoperative radiological assessment of patients (brain CT and MRI), as well as preoperative angiography in cases of doubt to avoid intraoperative ruptures.
As there is no consensus on the optimal treatment for this type of collision, an individualized therapeutic strategy must be adapted according to the clinical presentation and the anatomical relationship between the 2 lesions, in particular the size of the meningioma, their location and the difficulty of clipping the aneurysm.
Patient consent
Informed consent was obtained from the patient to publish her case.
Ethics approval and consent to participate
Informed consent was obtained from the patient prior to the submission of this article. Also, this article respects both the Consensus-based Clinical Case Reporting Guideline and the Recommendations for the Conducting, Reporting, Editing, and Publication of Scholarly Work in Medical Journals.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Salma Abbas, Email: Dr.s.abbas48@gmail.com.
Mahjouba Boutarbouch, Email: mahjouba.boutarbouch@gmail.com.
References
- 1.Algburi HA, Sharma M, Ismail M, Albulaihed SA, Al-Gertani MR, Majeed SN, et al. The coexistence of anterior communicating artery aneurysm and meningioma: A literature review and illustrative case. Surg Neurol Int. 2022;13:569. doi: 10.25259/SNI_1039_2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Papadimitriou K, Rocca A, Dunet V, Daniel RT. Feeding artery aneurysms associated with large meningiomas: case report and review of the literature. Heliyon. 2020;6(5):e04071. doi: 10.1016/j.heliyon.2020.e04071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lara-Olivas J A, Sangrador-Deitos MV, Villalobos-Díaz R, Marian-Magaña R, Gomez-Amador JL. A rare case of a right infratentorial meningioma and a left giant posterior communicating thrombosed aneurysm. Surg Neurol Int. 2023;14:317. doi: 10.25259/SNI_473_2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanaka S, Kobayashi M, Hinose T, Oikawa N, Kinoshita M, Yoshikawa A, et al. Intraoperative rupture of intracerebral aneurysm immediately after meningioma resection: a case report. BMC Neurol. 2022;22:135. doi: 10.1186/s12883-022-02664-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fischer P.B.R, Palkovic S, Holling M, Niederstadt T, Jeibmann A, Wassmann H. Coexistence of cerebral aneurysm and meningioma—pure accident? Clin Neurol Neurosurg. 2009;111(Issue 8):647–654. doi: 10.1016/j.clineuro.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 6.Onyia C, Ojo O, Arekhandia B. Tumeur cérébrale sellaire coexistant avec un anévrisme communicant postérieur gauche provoquant un ptosis: enseignements tirés (à propos d'un cas) Pan Afr Med J. 2023;44:60. doi: 10.11604/pamj.2023.44.60.38596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waqas M, Hadi Y B, Ujjan B, Javed G. Clinoidal meningioma associated with an internal carotid artery aneurysm. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2014-206707. [DOI] [PMC free article] [PubMed] [Google Scholar]