Abstract
Background
This study aims to assess the knowledge, perceptions, and utilization of point-of-care ultrasound (POCUS) among emergency physicians (EPs) in Saudi Arabia. Point-of-care ultrasound has emerged as a valuable tool in emergency medicine, providing real-time diagnostic information at the bedside. Understanding the current state of POCUS integration and the factors influencing its adoption is crucial for optimizing patient care in emergency settings.
Materials and methods
A cross-sectional study was conducted across various hospitals in Saudi Arabia over six months. The study included 100 EPs, encompassing residents and specialists. Data were collected through an online self-administered questionnaire, exploring demographic factors, POCUS training, equipment availability, and physicians’ perceptions. Statistical analyses were performed using SPSS version 28.0, including descriptive statistics and Chi-square tests.
Results
The study revealed diverse demographic factors, with a majority of physicians working in regional emergency medical centers. While 84.0% of respondents had used an ultrasound device, varying levels of knowledge about POCUS were observed. Regional disparities and differences in training exposure were evident. The majority expressed positive perceptions of POCUS utility, with 67.0% recognizing its usefulness in primary care health centers. However, 31.0% only partially agreed on its daily practice utility, highlighting potential areas for intervention.
Conclusion
This study provides a comprehensive assessment of POCUS awareness, knowledge, and perceptions among EPs in Saudi Arabia. The findings underscore the need for targeted educational initiatives, resource allocation, and regional considerations to enhance POCUS integration. Addressing perceived barriers and regional variations can contribute to the widespread adoption of POCUS, ultimately optimizing patient care in emergency settings.
How to cite this article
Almulhim KN, Alabdulqader RA, Alghamd MK, Alqarni AA, Althikrallah FM, Alarfaj AA. Assessing Point-of-care Ultrasound Knowledge and Utilization among Emergency Physicians in Saudi Arabia: A Cross-sectional Survey. Indian J Crit Care Med 2024;28(8):769–776.
Keywords: Emergency, Health centers, Point-of-care ultrasound, Saudi Arabia
Highlights
This study thoroughly evaluates the awareness, knowledge, and perceptions of point-of-care ultrasound (POCUS) among emergency physicians in Saudi Arabia. The findings emphasize the necessity for focused educational programs, resource allocation, and regional factors to improve POCUS integration. Future research endeavors should focus on addressing barriers to POCUS adoption.
Introduction
Point-of-care ultrasound, which was first utilized by emergency physicians (EPs) in the 1980s, has become more and more popular throughout the world for the diagnosis and treatment of patients who come to the Emergency Department (ED).1 To portray the essential concepts of emergency medicine (EM) in a more cohesive and representative manner, the United States developed the Model of Clinical Practice of Emergency Medicine in 2001. As a crucial diagnostic test, bedside ultrasonography was included in this model. Since the early 2000s, POCUS has reportedly been taught at more than 95% of training hospitals in the United States.2
With the advent of handheld devices of various sizes, healthcare professionals can now perform POCUS at the patient's bedside. These devices are significantly more portable than full-platform systems. EM practitioners have adopted POCUS use broadly, and it has also spread to several other specialties, including critical care (CC), trauma, vascular medicine, obstetrics, and rheumatology. Point-of-care ultrasound has enabled access to reasonably priced technologies in resource-constrained environments around the world. Due to the necessity of immediate triage and assessment, POCUS is now a part of EM procedures.3
Interestingly, the majority of physicians have been reluctant to incorporate this paradigm-shifting technology into their daily practices. This is partly because they are unfamiliar with the tool; POCUS is a relatively new technology, so most frontline physicians have little to no experience with its use; additionally, POCUS is highly operator-dependent; POCUS must be performed by competent practitioners; training is necessary to close gaps in learners’ knowledge and skill; fortunately, recent data suggest that those who are eager to learn POCUS can obtain adequate proficiency with minimal training.4 Learning POCUS will probably be useful for EPs because it is applicable in a wide range of medical settings. However, there is a significant financial commitment needed to incorporate POCUS into standard clinical practice, and there are typically few resources available for medical education. Thus, there needs to be justification for creating a POCUS training curriculum for EPs. A needs assessment is necessary to determine if teaching EPs to use POCUS is necessary and suitable.
The primary aim of this study is to investigate the current status, education, perceptions, and barriers to using POCUS in emergency medical centers in Saudi Arabia through a national survey.
Materials and Methods
Study Design
The study employed a cross-sectional design and was conducted over six months in various hospitals in Saudi Arabia.
Population and Samples of Study
The targeted study population comprised EPs, including residents, specialists, and consultants. All EPs were included in the inclusion criteria, while other specialists were excluded from the sample, as were those who didn't want to participate in this questionnaire. The final sample size consisted of 100 EPs.
Study Tool
Previous studies describing applications of POCUS were reviewed.2, 4 Based on this, the researchers built their questionnaire. Based on this, the researchers built their questionnaire. The questionnaire consisted of 24 questions, which were divided into four sections. The first section included the participants’ demographic factors in this survey, and the second section included questions through which we understand the perception of physicians considering POCUS in emergencies. The third section included a set of questions to identify the degree of physicians’ familiarity with and interest in the technique of focused evaluation using ultrasound imaging in trauma POCUS courses. The fourth section included questions to determine the relationship between the level of knowledge and demographic factors.
After that, it was presented to a group of consultants and specialists to ensure the integrity of its paragraphs, and what was necessary was deleted and modified. The researchers presented it to an exploratory group outside the scope of the study to ensure its validity. The questionnaire was distributed online on social media, such as LinkedIn, private WhatsApp groups, private Telegram groups, and X platform for EM practitioners.
Data Collection
Data were collected through an online, self-administered questionnaire, ensuring anonymity by excluding personally identifiable information. The questionnaire aimed to gather information without posing any risk or harm to the participants. The potential benefits of the study included enhancing patient management decisions, ultimately leading to improved patient outcomes.
Statistical Analysis
For data analysis, Google Forms facilitated the collection and review of data, maintaining subject confidentiality and participant information. Microsoft Office Excel (2023) was employed for data storage, with subsequent analysis conducted using SPSS.
Descriptive statistics, such as mean, median, standard deviation, and frequencies, were utilized for quantitative variables visually presented in figures. Qualitative data underwent analysis through the Chi-square test, with a significance level set at p < 0.05 for all statistical tests conducted. To address ethical concerns, participants provided informed consent, ensuring their willingness to partake in the research.
Results
Table 1 presents the demographic characteristics of the 100 participating EPs. Most respondents worked in regional emergency medical centers and were from Riyadh Province. Also, Table 1 represents the ability of respondents to use ultrasound devices.
Table 1.
Demographic factors of the participants (N = 100)
| Items | Demographic characteristics | Count | Column N % |
|---|---|---|---|
| What is the type of emergency medical facility you work for? | Regional Emergency Medical Center | 55 | 55.0% |
| Local Emergency Medical Center | 45 | 45.0% | |
| Where is the emergency medical facility where you work? | Al Baha Province | 9 | 9.0% |
| Eastern Province | 20 | 20.0% | |
| Jizan Province | 4 | 4.0% | |
| Riyadh Province | 29 | 29.0% | |
| Madinah Province | 12 | 12.0% | |
| Al-Jawf Province | 1 | 1.0% | |
| Makkah Province | 6 | 6.0% | |
| Northern Borders Province | 3 | 3.0% | |
| Tabuk Province | 2 | 2.0% | |
| Aseer Province | 4 | 4.0% | |
| Najran Province | 4 | 4.0% | |
| Ha'il Province | 2 | 2.0% | |
| Qassim Province | 4 | 4.0% | |
| Please choose your position. | 1st year of resident | 5 | 5.0% |
| 2nd year of resident | 12 | 12.0% | |
| 3rd year of resident | 14 | 14.0% | |
| 4th year of resident | 13 | 13.0% | |
| General Physician | 15 | 15.0% | |
| Specialist | 41 | 41.0% | |
| Please select the number of years of service from your specialist. | 1–5 years | 36 | 36.0% |
| 6–10 years | 42 | 42.0% | |
| 11–15 years | 9 | 9.0% | |
| 16–20 years | 13 | 13.0% | |
| How many ultrasound machines do your emergency medical centers own? (including hand-held machine) | 1 | 47 | 47.0% |
| 2 | 21 | 21.0% | |
| 3 | 11 | 11.0% | |
| 4 | 1 | 1.0% | |
| 5 and more | 20 | 20.0% | |
| Have you ever used an ultrasound device? | No | 16 | 16.0% |
| Yes | 84 | 84.0% | |
| What is your degree of knowledge about POCUS/emergency ultrasound, performed by non-radiologists emergency physicians? | 1 (I was not aware at all of its existence) | 4 | 4.0% |
| 2 | 18 | 18.0% | |
| 3 | 26 | 26.0% | |
| 4 | 37 | 37.0% | |
| 5 (I am fully aware of its existence) | 15 | 15.0% | |
| What level of knowledge do you have about POCUS/emergency ultrasound? | Elementary knowledge | 14 | 14.0% |
| Basic knowledge to perform a diagnostic study | 23 | 23.0% | |
| Sufficient knowledge to perform diagnostic studies on a routine basis | 51 | 51.0% | |
| I have complete training and I can work as a trainer in ultrasound | 12 | 12.0% | |
| To what extent has the hospital contributed to your training in POCUS/emergency ultrasound? | In no way | 21 | 21.0% |
| It has been mentioned superficially | 25 | 25.0% | |
| It has been addressed as a topic or as part of a specific topic | 15 | 15.0% | |
| It has been taught in depth and we have even carried out POCUS/emergency ultrasound during my degree | 20 | 20.0% | |
| It has been taught specifically and there have been workshops | 19 | 19.0% |
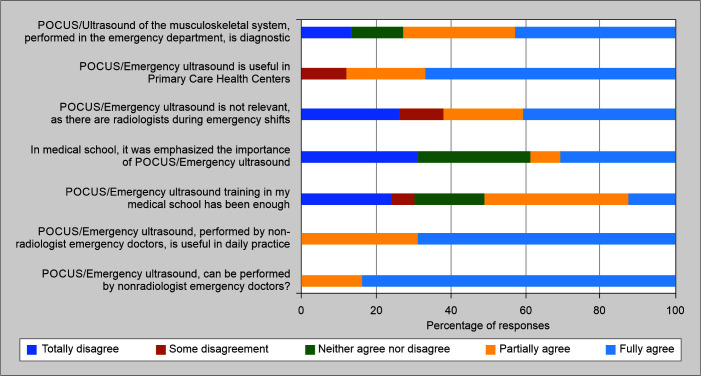
Table 2 and Figure 1 delve into the physicians’ perceptions of POCUS. Notably, 84.0% fully agreed that non-radiologist emergency doctors can perform POCUS. However, opinions were more divided regarding the utility of POCUS in daily practice, with 69.0% partially agreeing. A significant portion (41.0%) disagreed with the idea that POCUS is not relevant due to the presence of radiologists during emergency shifts. Conversely, 67.0% agreed that POCUS is useful in primary care health centers.
Table 2.
The perception of the physicians considering POCUS/emergency ultrasound
| Items | Totally disagree | Some disagreement | Neither agree nor disagree | Partially agree | Fully agree |
|---|---|---|---|---|---|
| POCUS/emergency ultrasound, can be performed by non-radiologist emergency doctors? | |||||
| Count | 0 | 0 | 0 | 16 | 84 |
| Row N % | 0.0% | 0.0% | 0.0% | 16.0% | 84.0% |
| POCUS/emergency ultrasound, performed by non-radiologist emergency doctors, is useful in daily practice. | |||||
| Count | 0 | 0 | 0 | 31 | 69 |
| Row N % | 0.0% | 0.0% | 0.0% | 31.0% | 69.0% |
| POCUS/emergency ultrasound training in my medical school has been enough. | |||||
| Count | 24 | 6 | 19 | 38 | 13 |
| Row N % | 24.0% | 6.0% | 19.0% | 38.0% | 13.0% |
| In medical school, it was emphasized the importance of POCUS/emergency ultrasound. | |||||
| Count | 31 | 0 | 30 | 8 | 31 |
| Row N % | 31.0% | 0.0% | 30.0% | 8.0% | 31.0% |
| POCUS/emergency ultrasound is not relevant, as there are radiologists during emergency shifts. | |||||
| Count | 26 | 12 | 21 | 0 | 41 |
| Row N % | 26.0% | 12.0% | 21.0% | 0.0% | 41.0% |
| POCUS/emergency ultrasound is useful in primary care health centers. | |||||
| Count | 0 | 12 | 0 | 21 | 67 |
| Row N % | 0.0% | 12.0% | 0.0% | 21.0% | 67.0% |
| POCUS/emergency ultrasound of the musculoskeletal system, performed in the emergency department, is diagnostic | |||||
| Count | 13 | 0 | 14 | 30 | 43 |
| Row N % | 13.0% | 0.0% | 14.0% | 30.0% | 43.0% |
Fig. 1.
The perception of the physicians considering POCUS/emergency ultrasound
Table 3 assesses the physicians’ familiarity with the Focused Assessment with Sonography in Trauma (FAST) technique and their interest in POCUS courses. A majority (53.0%) claimed full mastery of the FAST technique, and an overwhelming 66.0% expressed full interest in participating in POCUS courses. Additionally, all respondents (100.0%) believed that POCUS could be beneficial for their training and specialty in the future.
Table 3.
Degree of familiarity with FAST technique and interest in participating in courses of POCUS
| Items | Count | Column N % |
|---|---|---|
| How familiar are you with the “FAST” technique in POCUS/emergency ultrasound? | ||
| 1 (I have no idea at all) | 1 | 1.0% |
| 3.00 | 14 | 14.0% |
| 4.00 | 32 | 32.0% |
| 5.00 (I am fully master FAST technique | 53 | 53.0% |
| Would you be interested in participating in courses, or working with POCUS/emergency ultrasound? | ||
| 1.00 (I am not interested) | 0 | 0.0% |
| 2.00 | 15 | 15.0% |
| 3.00 | 10 | 10.0% |
| 4.00 | 9 | 9.0% |
| 5.00 (I am fully interested) | 66 | 66.0% |
| Do you think that POCUS/emergency ultrasound could help in your training and could be useful for your specialty in the future? | ||
| No | 0 | 0.0% |
| Yes | 100 | 100.0% |
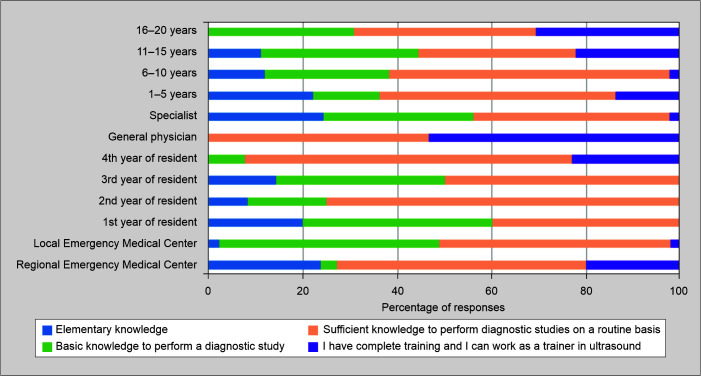
Table 4 and Figure 2 investigate the association between the level of knowledge about POCUS and demographic factors. The type of emergency medical facility showed a significant association with knowledge levels (p < 0.001), as did the position (p < 0.001), number of years of service (p = 0.078), ownership of ultrasound machines (p = 0.002), and previous use of ultrasound devices (p = 0.008). These findings suggest that these demographic factors may influence the level of knowledge about POCUS among EPs.
Table 4.
The association between level of knowledge and demographic factors
| What level of knowledge do you have about POCUS/emergency ultrasound? | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Elementary knowledge | Basic knowledge to perform a diagnostic study | Sufficient knowledge to perform diagnostic studies on a routine basis | I have complete training and I can work as a trainer in ultrasound | p-value | |||||
| Count | Row N % | Count | Row N % | Count | Row N % | Count | Row N % | ||
| What is the type of emergency medical facility you work for? | |||||||||
| Regional Emergency Medical Center | 13 | 23.6% | 2 | 3.6% | 29 | 52.7% | 11 | 20.0% | 0.000* |
| Local Emergency Medical Center | 1 | 2.2% | 21 | 46.7% | 22 | 48.9% | 1 | 2.2% | |
| Please choose your position | |||||||||
| 1st year of resident | 1 | 20.0% | 2 | 40.0% | 2 | 40.0% | 0 | 0.0% | 0.000* |
| 2nd year of resident | 1 | 8.3% | 2 | 16.7% | 9 | 75.0% | 0 | 0.0% | |
| 3rd year of resident | 2 | 14.3% | 5 | 35.7% | 7 | 50.0% | 0 | 0.0% | |
| 4th year of resident | 0 | 0.0% | 1 | 7.7% | 9 | 69.2% | 3 | 23.1% | |
| General physician | 0 | 0.0% | 0 | 0.0% | 7 | 46.7% | 8 | 53.3% | |
| Specialist | 10 | 24.4% | 13 | 31.7% | 17 | 41.5% | 1 | 2.4% | |
| Please select the number of years of service from your specialist. | |||||||||
| 1–5 years | 8 | 22.2% | 5 | 13.9% | 18 | 50.0% | 5 | 13.9% | 0.078 |
| 6–10 years | 5 | 11.9% | 11 | 26.2% | 25 | 59.5% | 1 | 2.4% | |
| 11–15 years | 1 | 11.1% | 3 | 33.3% | 3 | 33.3% | 2 | 22.2% | |
| 16–20 years | 0 | 0.0% | 4 | 30.8% | 5 | 38.5% | 4 | 30.8% | |
| How many ultrasound machines do your Emergency Medical Centers own? (including hand-held machine) | |||||||||
| 1 | 9 | 19.1% | 15 | 31.9% | 21 | 44.7% | 2 | 4.3% | 0.002* |
| 2 | 2 | 9.5% | 2 | 9.5% | 8 | 38.1% | 9 | 42.9% | |
| 3 | 0 | 0.0% | 3 | 27.3% | 8 | 72.7% | 0 | 0.0% | |
| 4 | 0 | 0.0% | 0 | 0.0% | 1 | 100.0% | 0 | 0.0% | |
| 5 and more | 3 | 15.0% | 3 | 15.0% | 13 | 65.0% | 1 | 5.0% | |
| Have you ever used an ultrasound device? | |||||||||
| No | 1 | 6.3% | 9 | 56.3% | 5 | 31.3% | 1 | 6.3% | 0.008* |
| Yes | 13 | 15.5% | 14 | 16.7% | 46 | 54.8% | 11 | 13.1% | |
Fig. 2.
Association between level of knowledge and demographic factors
Discussion
The results of the current study demonstrate a varied level of knowledge among EPs regarding POCUS, with a substantial portion reporting sufficient knowledge to perform diagnostic studies routinely. This finding aligns with the global recognition of POCUS as a valuable tool in EM.5 POCUS aids in rapid and accurate diagnosis, facilitating timely and effective patient management, particularly in critical and time-sensitive situations.6–8 The majority of respondents expressed positive perceptions regarding the utility of POCUS in daily practice and its relevance in primary care health centers, underlining its potential impact on diverse healthcare settings.
The majority of EPs (84.0%) in this study fully agreed that non-radiologists, specifically emergency doctors, can effectively perform POCUS. This positive perception aligns with the growing global acknowledgment of the role of non-radiologists in utilizing ultrasound at the bedside.9,10 The accessibility and immediacy of POCUS make it a valuable tool for EPs to obtain real-time diagnostic information, contributing to more prompt decision-making and improved patient outcomes.11,12 While most respondents acknowledged POCUS's potential, the data also show that 31.0% only partially agreed that POCUS is useful in daily practice. In a previous study conducted among medical interns, the authors found that 75% of the participants believed that POCUS was an essential skill, and only 25% would use it in their daily work.4 This discrepancy in opinion suggests a need for further exploration into the factors influencing physicians’ perceptions. Potential reasons could include variations in training, exposure to POCUS applications, or specific challenges encountered in daily practice. Understanding these factors can inform targeted interventions to enhance the perceived utility of POCUS among EPs.
The emphasis on POCUS during medical school is a critical aspect of physician training. The data indicate that 30.0% of respondents felt that POCUS was superficially mentioned during their medical education, while 15.0% reported that it was taught in-depth and included practical application during their degree. The same was reported in different studies, which showed that the curricular design and delivery across undergraduate medical education programs in the United States remain variable without widely adopted national standards and guidelines.13 This finding underscores the need for standardized and comprehensive POCUS training in medical curricula to ensure that EPs are adequately prepared for the practical application of ultrasound in their professional practice.14 A notable finding is a disagreement among 41.0% of respondents who felt that POCUS is not relevant in emergency shifts where radiologists are present. This perception may indicate a lack of understanding of the complementary role of POCUS, even in the presence of radiologists. POCUS can provide rapid assessments that guide immediate interventions, especially in time-sensitive situations, and can be a valuable adjunct to traditional imaging modalities.15
Concerning the utility of POCUS in primary care health centers, a substantial 67.0% fully agreed with its usefulness. This finding suggests that EPs recognize the potential of POCUS beyond the emergency department, extending its benefits to primary care settings. This aligns with the evolving role of POCUS in various healthcare domains.16 In assessing the diagnostic capabilities of musculoskeletal ultrasound in the emergency department, 43.0% fully agreed that it is diagnostic. This finding highlights the potential of POCUS in musculoskeletal assessments, aiding in the rapid diagnosis of injuries or conditions, which is crucial in the emergency setting.17–21
Training and education play a pivotal role in shaping physicians’ attitudes and competence in utilizing POCUS. The association between the type of emergency medical facility and physicians’ knowledge levels suggests that physicians working in regional emergency medical centers may have more exposure to training opportunities, resources, and collaborative practices that contribute to a higher level of POCUS knowledge. This finding emphasizes the need for targeted educational interventions, workshops, and continuous training programs to bridge the knowledge gap among EPs, especially those working in local emergency medical centers.
The study's outcomes also underscore the positive correlation between the ownership of ultrasound machines and physicians’ knowledge levels. Facilities with more ultrasound machines, including handheld devices, could potentially offer a more conducive environment for physicians to gain hands-on experience and confidence in utilizing POCUS. Increased investment in ultrasound equipment, along with strategic placement and accessibility, may enhance overall POCUS integration in emergency settings.22
Regional variations in POCUS awareness, as reflected in the distribution of respondents across different provinces, suggest potential disparities in the implementation of POCUS training programs or awareness campaigns. Riyadh Province, with the highest representation, may have more extensive educational resources and collaborations, contributing to a higher level of knowledge among its EPs. Recognizing these regional differences is crucial for tailoring interventions and allocating resources effectively, ensuring equitable access to POCUS education across diverse geographical areas.
Despite the positive attitudes toward POCUS expressed by the majority of respondents, a notable proportion had not used an ultrasound device. This raises questions about the barriers preventing some physicians from incorporating POCUS into their practice. Identifying and addressing these barriers, which may include limited access to training opportunities, equipment, or time constraints, is essential for promoting wider adoption of POCUS among EPs and ICU.2,23–26
The study's limitations should be acknowledged. Though adequate for initial exploration, the sample size may not fully capture the diversity of EPs across all regions of Saudi Arabia. Additionally, while ensuring anonymity, the self-administered questionnaire relies on participants’ self-reporting and may introduce response bias. Future research could employ qualitative methods, such as interviews or focus groups, to delve deeper into physicians’ experiences and perceptions regarding POCUS.
Conclusion
This study sheds light on the current landscape of POCUS awareness, knowledge, and perceptions among EPs in Saudi Arabia. The findings underscore the importance of targeted educational initiatives, resource allocation, and regional considerations in promoting the effective integration of POCUS into emergency medical practice. Future research endeavors should focus on addressing barriers to POCUS adoption, exploring the long-term impact of POCUS training, and evaluating the effectiveness of different educational strategies in enhancing POCUS proficiency among EPs. Ultimately, a concerted effort from healthcare institutions, policymakers, and educators is required to harness the full potential of POCUS and optimize patient care in emergency settings.
Ethical Approval
The study adhered to ethical standards, obtaining clearance from the ethical committee of the medical college at King Faisal University. The Research Ethics Committee at King Faisal University grants its ethical approval to the protocol. No. KFU-REC-2023-DEC-ETHICS1795.
Orcid
Khalid Nabeel Almulhim https://orcid.org/0000-0001-8564-8620
Razan Anwar Alabdulqader https://orcid.org/0000-0002-4794-0185
Mohammed Khalid Alghamd https://orcid.org/0009-0006-8983-2365
Alwaleed A Alqarni https://orcid.org/0009-0001-3228-4648
Farah M Althikrallah https://orcid.org/0009-0001-0046-3481
Ahmed A Alarfaj https://orcid.org/0000-0003-3062-2241
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Alzayedi AS, Azizalrahman AA, AlMadi HA, Althekair AM, Blaivas M, Karakitsos D. Use and education of point‐of‐care ultrasound in pediatric emergency medicine in Saudi Arabia. J Ultrasound Med. 2017;36(11):2219–2225. doi: 10.1002/jum.14254. [DOI] [PubMed] [Google Scholar]
- 2.Yoo J, Kang SY, Jo IJ, Kim T, Lee G, Park JE, et al. The use of point-of-care ultrasound in Emergency Medical Centers in Korea: A national cross-sectional survey. J Korean Med Sci. 2021;36(21):1–12. doi: 10.3346/jkms.2021.36.e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee L, DeCara JM. Point-of-care ultrasound. Curr Cardiol Rep. 2020;22(11):149. doi: 10.1007/s11886-020-01394-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jarwan W, Alshamrani AA, Alghamdi A, Mahmood N, Kharal YM, Rajendram R, et al. Point-of-care ultrasound training: An assessment of interns’ needs and barriers to training. Cureus. 2020;12(10) doi: 10.7759/cureus.11209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hashim A, Tahir MJ, Ullah I, Asghar MS, Siddiqi H, Yousaf Z. The utility of point of care ultrasonography (POCUS) Ann Med Surg. 2021;71:102982. doi: 10.1016/j.amsu.2021.102982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Verras C, Ventoulis I, Bezati S, Matsiras D, Parissis J, Polyzogopoulou E. Point of care ultrasonography for the septic patient in the emergency department: A literature review. J Clin Med. 2023;12(3):1105. doi: 10.3390/jcm12031105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koratala A, Reisinger N. POCUS for nephrologists: Basic principles and a general approach. Kidney360. 2021;2(10):1660–1668. doi: 10.34067/KID.0002482021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Umuhire OF, Henry MB, Levine AC, Cattermole GN, Henwood P. Impact of ultrasound on management for dyspnea presentations in a Rwandan emergency department. Ultrasound J. 2019;11(1):18. doi: 10.1186/s13089-019-0133-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sidhu PS, Ewertsen C, Piskunowicz M, Secil M, Ricci P, Fischer T, et al. Diversity of current ultrasound practice within and outside radiology departments with a vision for 20 years into the future: A position paper of the ESR ultrasound subcommittee. Insights Imaging. 2023;14(1):202. doi: 10.1186/s13244-023-01548-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sippel S, Muruganandan K, Levine A, Shah S. Review article: Use of ultrasound in the developing world. Int J Emerg Med. 2011;4(1):72. doi: 10.1186/1865-1380-4-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi W, Cho YS, Ha YR, Oh JH, Lee H, Kang BS, et al. Role of point-of-care ultrasound in critical care and emergency medicine: Update and future perspective. Clin Exp Emerg Med. 2023;10(4):363–381. doi: 10.15441/ceem.23.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ali N, Chhotani AA, Iqbal SP, Soomar SM, Raheem A, Waheed S. Point of care ultrasonographic life support in emergency (PULSE)-a quasi-experimental study. Int J Emerg Med. 2023;16(1):49. doi: 10.1186/s12245-023-00525-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tarique U, Tang B, Singh M, Kulasegaram KM, Ailon J. Ultrasound curricula in undergraduate medical education: A scoping review. J Ultrasound Med. 2018;37(1):69–82. doi: 10.1002/jum.14333. [DOI] [PubMed] [Google Scholar]
- 14.Ramgobin D, Gupta V, Mittal R, Su L, Patel MA, Shaheen N. POCUS in internal medicine curriculum: Quest for the holy grail of modern medicine. J Community Hosp Intern Med Perspect. 2022;12(5):36–42. doi: 10.55729/2000-9666.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chelikam N, Vyas A, Desai R, Khan N, Raol K, Kavarthapu A, et al. Past and present of point-of-care ultrasound (PoCUS): A narrative review. Cureus. 2023;15(2):1–21. doi: 10.7759/cureus.50155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Osterwalder J, Polyzogopoulou E, Hoffmann B. Point-of-care ultrasound—history, current and evolving clinical concepts in emergency medicine. Medicina (B Aires) 2023;59(12):2179. doi: 10.3390/medicina59122179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adhikari S, Marx J, Crum T. Point-of-care ultrasound diagnosis of acute Achilles tendon rupture in the ED. Am J Emerg Med. 2012;30(4):634.e3–634.e4. doi: 10.1016/j.ajem.2011.01.029. [DOI] [PubMed] [Google Scholar]
- 18.Lee WJ, Tsai WS, Wu RH. Focused ultrasound for traumatic ankle pain in the emergency department. J Emerg Med. 2013;44(2):476–477. doi: 10.1016/j.jemermed.2012.02.047. [DOI] [PubMed] [Google Scholar]
- 19.Odom M, Haas N, Phillips K. Bedside ultrasound diagnosis of complete Achilles Tendon tear in a 25-year-old man with calf injury. J Emerg Med. 2018;54(5):694–696. doi: 10.1016/j.jemermed.2018.01.028. [DOI] [PubMed] [Google Scholar]
- 20.Stickles S, Friedman L, Demarest M, Raio C. Achilles tendon rupture. West J Emerg Med. 2015;16(1):161–162. doi: 10.5811/westjem.2014.10.24127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Habibullah N, Dayo J, Soomar SM, Ali N. Use of point-of-care ultrasound in a low-resource setting to diagnose Achilles tendon rupture and avulsion fracture of the calcaneal bone. Int J Emerg Med. 2023;16(1):66. doi: 10.1186/s12245-023-00544-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shaddock L, Smith T. Potential for use of portable ultrasound devices in rural and remote settings in Australia and other developed countries: A systematic review. J Multidiscip Healthc. 2022;15:605–625. doi: 10.2147/JMDH.S359084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pouryahya P, McR Meyer AD, Koo MPM. Prevalence and utility of point‐of‐care ultrasound in the emergency department: A prospective observational study. Australas J Ultrasound Med. 2019;22(4):273–278. doi: 10.1002/ajum.12172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tadesse AZ, Abicho TB, Alemu DM, Aspler A. Point of care ultrasound (POCUS) utilization and barriers by senior emergency medicine and critical care residents at Two Teaching Referral Hospitals, Addis Ababa, Ethiopia. Cirocchi R, ed. Emerg Med Int. 2023;2023:1–6. doi: 10.1155/2023/7584670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhattacharjee S, Prasanna M, Maitra S, Ray BR. Lung ultrasound findings in a patient with lymphangitic carcinomatosis. Indian J Crit Care Med. 2024;28(1):82–83. doi: 10.5005/jp-journals-10071-24597. DOI: 10.5005%2Fjp-journals-10071-24597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rajbanshi LK, Bajracharya A, Devkota D. Author Reply: Lung ultrasound score-does it really predict extubation failure? Indian J Crit Care Med. 2023;27(11):857. doi: 10.5005/jp-journals-10071-24559. DOI: 10.5005%2Fjp-journals-10071-24559. [DOI] [PMC free article] [PubMed] [Google Scholar]