Abstract
Background/Aim
The aim of this study was to evaluate the Mayo Adhesive Probability (MAP) score as a predictor of split renal function deterioration after robot-assisted partial nephrectomy (RAPN).
Patients and Methods
A total of 30 patients who underwent RAPN were identified retrospectively. The parameters evaluated included patient characteristics, tumor diameter, MAP score, warm ischemic time (WIT), and renal function. Split renal function was evaluated using Tc-99m DTPA renal scintigraphy before and six months after surgery. Univariate and multivariate logistic regression analyses were performed.
Results
Nine patients (30.0%) showed more than 90% preservation of split renal function on the operated side. The MAP score (p=0.015), cT1b tumor (p=0.0002), and WIT (p=0.044) were associated with preservation of split renal function six months after surgery on univariate analysis. The MAP score was the strongest predictor of preservation of split renal function six months after surgery on multivariable analysis (p=0.007). On receiver-operating characteristic (ROC) curve analysis, the MAP score (cutoff value 3.0; p=0.01) was a significant predictor of split renal function six months after surgery.
Conclusion
The MAP score was significantly associated with postoperative split renal function six months after RAPN on the operated kidney side. The MAP score is useful for predicting split renal function after RAPN.
Keywords: Robot-assisted partial nephrectomy (RAPN), renal function, Mayo adhesive probability score
Partial nephrectomy (PN) is the standard treatment for small renal masses (1), and its objectives are to achieve control of the cancer and preserve renal function. The procedure involved in PN has progressed from open to minimally invasive surgery, including laparoscopic partial nephrectomy (LPN) and robot-assisted partial nephrectomy (RAPN) (2).
The Mayo Adhesive Probability (MAP) score is a computed tomography (CT) based scoring system that is useful as a quantitative and qualitative indicator of perinephric fat (PNF) and for predicting surgical time and surgical difficulty prior to partial nephrectomy (PN) (3,4). This scoring system is simple and is calculated based on two indices: perinephric fat thickness and stranding. Perinephric fat thickness is a type of visceral adipose obesity, whereas perinephric stranding may indicate fat inflammation and firmness (3). Recently, it has been reported that thickness and inflammation of perinephric fat may be predictors of decreased renal function in patients with chronic kidney disease (CKD) (5,6).
Thus, we hypothesized that the MAP score is one of the patient-specific metabolic parameters that can predict renal deterioration after PN. The literature on the usefulness of the MAP score as a predictor of postoperative renal function in RAPN is limited and inconclusive. The purpose of this study was to evaluate the MAP score as a predictor of renal function decline after RAPN.
Patients and Methods
Patients. Our Research Ethics Committee approved the study design (approval number H20-09-002) and, because of the retrospective design, the need to obtain informed consent from all eligible patients for their involvement in the study was waived. Between August 2020 and June 2022, 30 patients underwent RAPN for the treatment of renal cell carcinoma at our institution and were analyzed in the present study.
Surgical procedure. All RAPNs in this study were performed by a single expert robotic surgeon (N.H.) using a da Vinci Xi robotic system. The RAPN approach was selected according to the location of the tumor, with a transperitoneal approach for tumors on the anterior side of the kidney and a retroperitoneal approach for tumors on the posterior side of the kidney. The transperitoneal and retroperitoneal approaches were used in 23 and 7 cases, respectively. RAPN procedures were carried out using previously described techniques (7). The assistant placed two additional trocars including the AirSeal iFS (CONMED Japan KK, Tokyo, Japan). The ARIETTA 70 (Hitachi Aloka Medical Ltd., Tokyo, Japan) was used for intraoperative ultrasound to identify tumor distribution and resection margins. After dissecting the gerota fascia from the kidney to expose the tumor, the fat around the tumor was minimally detached. The main renal arteries on the operated side were clamped with a single bulldog clamp, and tumor resection was performed with cold scissors, maintaining a margin of approximately 3 mm. The collecting system closure was completed using 3-0 V-Loc (COVIDIEN Japan, Inc., Tokyo, Japan) as an inner running suture, and additional inner sutures were placed to stop bleeding, followed by renorrhaphy using 3-0 V-Loc.
Perioperative data. The following parameters were collected: age, sex, body mass index, tumor side, tumor size, clinical stage, RENAL nephrometry score (RNS), the MAP score, pre- and postoperative total renal function, pre- and postoperative split renal function, operative time, WIT, estimated blood loss (EBL), clinical T stage, histopathological types of the tumor, and perioperative complications. Perioperative complications were evaluated using the Clavien-Dindo classification.
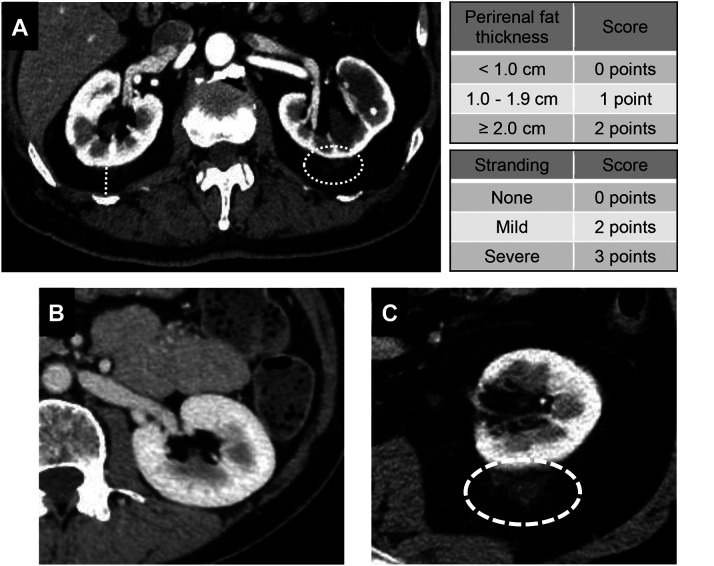
The MAP score. The MAP score is calculated based on two indices: perinephric fat thickness and perinephric stranding. Perinephric fat thickness is measured by the distance between the renal capsule and the body wall at the level of the renal vein (<1 cm:0 points, 1.1-1.9 cm:1 point, >2.0 cm:2 points). The perinephric stranding score is measured at the same level (no stranding:0 points, mild stranding:1 point, severe stranding:2 points). The two scores are summed and scored from 0 to 5 points (Figure 1).
Figure 1.
Method for determining perinephric fat measurements and grading of perinephric stranding. A) The distance between the renal capsule and the body wall at the level of the renal vein is measured (white dotted line). Stranding is evaluated at the perinephric fat of the operated side (white dotted circle). B) Patients with a Mayo adhesive probability (MAP) score of 0. Perinephric fat is thin with no stranding. C) Patients with a MAP score of 5. Perinephric fat is thick and shows severe stranding with inflammation.
An independent reviewer assessed the preoperative CT for each patient as described by Davidiuk et al. (3). In previous studies, with MAP scores <2, it was considered easier to detach perinephric fat and less difficult to perform surgery (8), therefore, patients were classified into three groups by their MAP scores: easy case group, MAP score 0-1; intermediate case group, MAP score 2-3; and difficult case group, MAP score 4-5.
Perioperative renal function. The serum creatinine (sCr) concentration and estimated glomerular filtration rate (eGFR) were used to assess preoperative and postoperative total renal function. Split renal function was analyzed using renal scintigraphy with technetium-99m diethylene-triamine-pentaacetate (Tc-99m DTPA) immediately before and six months after surgery, and the change in GFR on the operated side was calculated. According to a previous study, preservation of renal function was defined as maintenance of postoperative GFR on the operated side ≥90% (8).
The primary objective was to determine whether the MAP score could predict the preservation of postoperative split renal function on the operated side kidney. The secondary objective was to determine the cutoff value of the MAP score to predict postoperative split renal function on the operated side ≥90% after RAPN.
Statistical analysis. To compare patient characteristics between the preserved split renal function (GFR ≥90%) and the non-preserved split renal function (GFR <90%) groups, differences between groups were evaluated using the Wilcoxon rank-sum test for continuous variables, with significance at p<0.05. Continuous data are presented as median and interquartile range (IQR) or mean and standard deviation (SD) values. Associations of patient and tumor characteristics with the preservation of split renal function on the operated side (GFR ≥90%) were evaluated using logistic regression models, in which odds ratios and 95% confidence intervals (CIs) were estimated. The change in GFR on the operated side was compared among the three groups (easy case group, intermediate case group, and difficult case group) using analysis of variance (ANOVA). Receiver-operating characteristic (ROC) curve analysis was also performed to determine the value of the MAP score determining the risk of GFR reduction on the operated side. All analyses were performed using JMP version 11.0 software (SAS, Cary, NC, USA).
Results
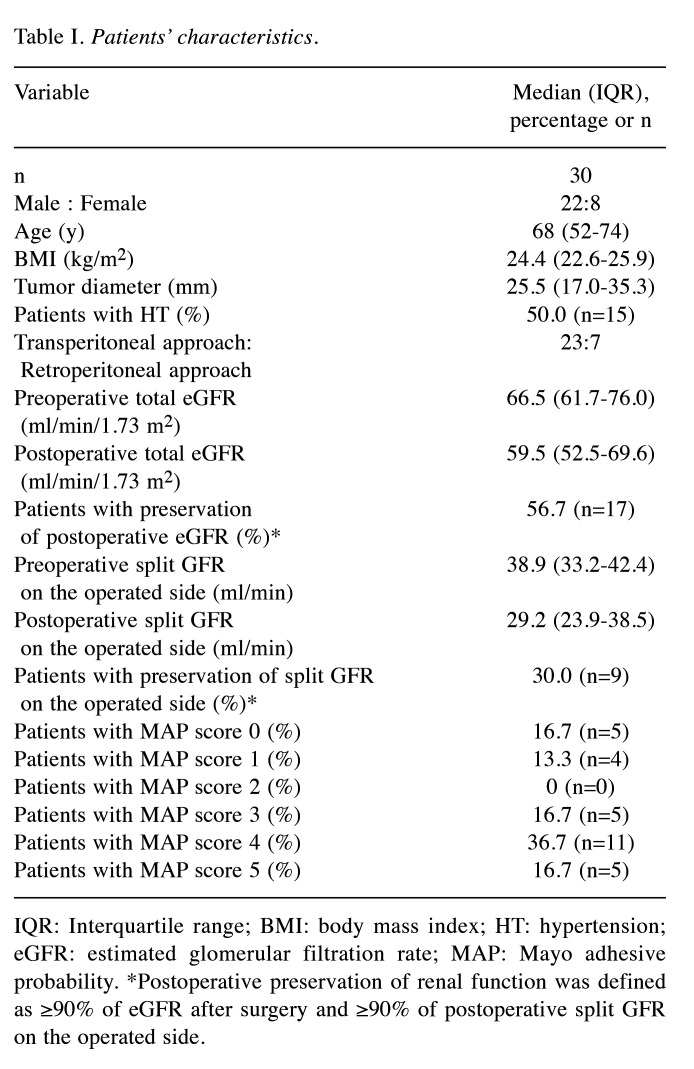
Patients’ characteristics. The baseline clinical features and perioperative results for the 30 participants in the study are presented in Table I. The median age was 68 [interquartile range (IQR)=52-74] years, the median BMI was 24.4 (IQR=22.6-25.9) kg/m2, and most patients were men (73.3%). The percentage of patients with hypertension (HT) was 50.0%. Overall, 83.3% (n=25) of the tumors were renal cell carcinomas (RCCs) with no positive resection margins. The median preoperative and postoperative total eGFRs were 66.5 (IQR=61.7-76.0) and 59.5 (IQR=52.5-69.6) ml/min/1.73 m2, respectively, and the percentage of patients who maintained postoperative total eGFR ≥90% was 56.7% (n=17). The median preoperative and postoperative split GFRs on the operated side were 38.9 (IQR=14.4-48.9) and 29.2 (IQR=23.9-38.5) ml/min/1.73 m2, respectively, and the percentage of patients who maintained split GFR on the operated side ≥90% was 30% (n=9). The number of patients in each MAP score group was as follows: easy case group (MAP score: 0-1), 9; intermediate case group (MAP score: 2-3), 5; and difficult case group (MAP score: 4-5), 16. The mean perinephric fat thickness points were 1.17±0.67 (0 points:5, 1 point: 15, 2 points: 10), and the mean stranding points were 1.73±1.19 (0 points: 9, 2 points: 11, 3 points: 10). The most common RNS value was 9, and two of the participants had highly complex tumors (≥10 points).
Table I. Patients’ characteristics.
IQR: Interquartile range; BMI: body mass index; HT: hypertension; eGFR: estimated glomerular filtration rate; MAP: Mayo adhesive probability. *Postoperative preservation of renal function was defined as ≥90% of eGFR after surgery and ≥90% of postoperative split GFR on the operated side.
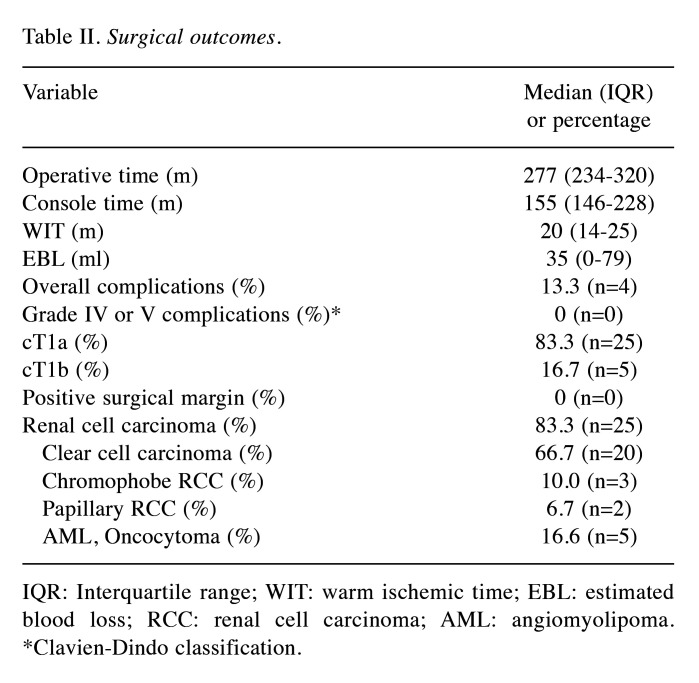
Surgical outcomes. The median operative time was 277 (IQR=234-320) min, console time was 155 (IQR=146-228) min, WIT was 20 (IQR=14-25) min, and EBL was 35 (IQR=0-79) ml. RAPN was not converted to other surgical procedures. According to the Clavien-Dindo classification, overall complications were observed in 4 (13.3%) RAPN patients. These included two cases of drug-induced liver dysfunction, one case of fever, and one case of urinary retention. No grade IV or V complications of the Clavien-Dindo classification were observed during the entire postoperative course. All postoperative complications were evaluated within 30 days after surgery. On histopathological evaluation, 83.3% (n=25) were renal cell carcinoma cases, and 16.7% (n=5) were angiomyolipoma or oncocytoma. Tumors were classified as cT1a in 25 patients and cT1b in 5 patients according to the 2010 TNM classification (Table II) (9).
Table II. Surgical outcomes.
IQR: Interquartile range; WIT: warm ischemic time; EBL: estimated blood loss; RCC: renal cell carcinoma; AML: angiomyolipoma. *Clavien-Dindo classification
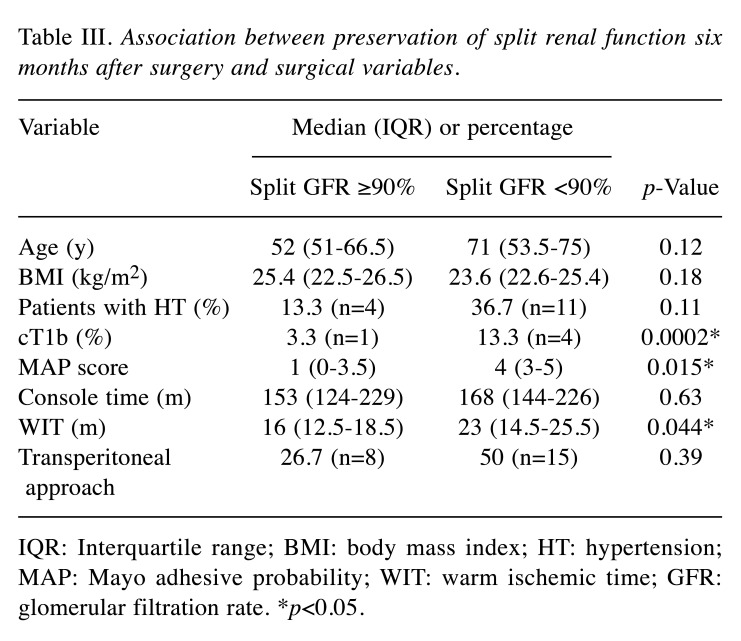
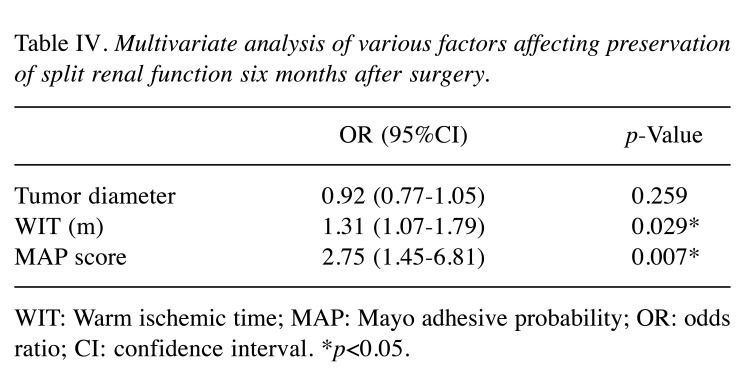
Preservation of split renal function. In 43.3% (n=13) of patients, eGFR, as the indicator of total renal function, at six months after RAPN was less than 90% of the preoperative eGFR, whereas, in 70.0% (n=21) of patients, the split GFR on the operated side was less than 90% of the preoperative split GFR at six months after RAPN. The changes in GFR on the operated side for the three groups stratified by the MAP score are shown in Figure 2. The mean changes in GFR on the operated side were -4.09±5.85 ml/min for the easy case group (MAP score 0-1), -5.15±4.53 ml/min for the intermediate case group (MAP score 2-3), and -9.91±4.58 ml/min for the difficult case group (MAP score 4-5). On univariable analysis, the MAP score (p=0.015), cT1b tumor (p=0.0002), and WIT (p=0.044) were associated with preservation of split renal function six months after surgery (Table III). On multivariable analysis, tumor diameter, MAP score, and WIT were identified as independent variables. The MAP score (p=0.007) and WIT (p=0.029) were significant independent predictors of split renal function after surgery (Table IV). On ROC curve analysis, the MAP score (cutoff value 3.0; p=0.01) significantly predicted split renal function on the operated side six months after surgery (Figure 3).
Figure 2.
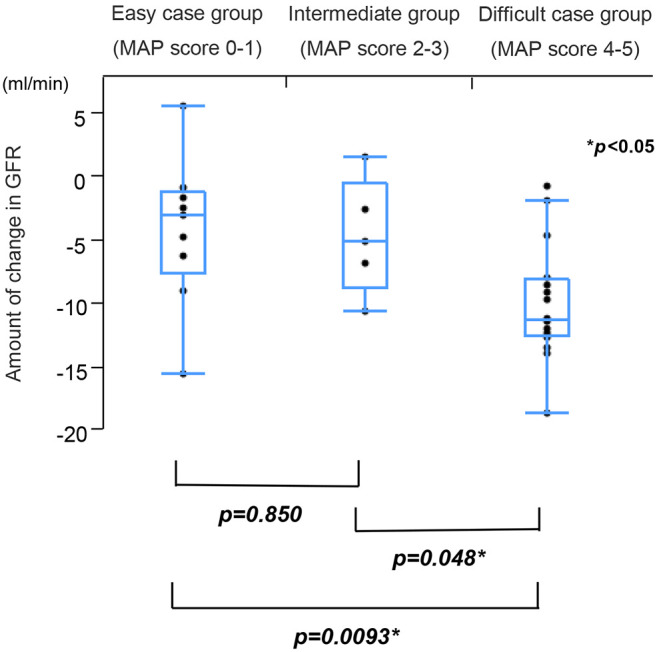
Comparison of the amount of change in the GFR on the operated side among the three groups on analysis of variance. Easy case group: Mayo adhesive probability (MAP) score 0-1, intermediate case group: MAP score 2-3, difficult case group: MAP score 4-5.
Table III. Association between preservation of split renal function six months after surgery and surgical variables.
IQR: Interquartile range; BMI: body mass index; HT: hypertension; MAP: Mayo adhesive probability; WIT: warm ischemic time; GFR: glomerular filtration rate. *p<0.05.
Table IV. Multivariate analysis of various factors affecting preservation of split renal function six months after surgery.
WIT: Warm ischemic time; MAP: Mayo adhesive probability; OR: odds ratio; CI: confidence interval. *p<0.05.
Figure 3.
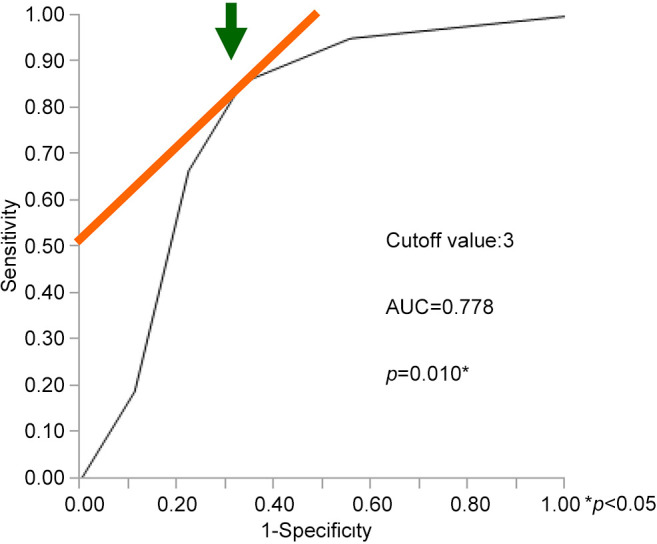
Receiver-operating characteristic analysis for the Mayo adhesive probability (MAP) score as a predictor of deterioration of operated side renal function after RAPN. A MAP score cutoff value of 3.0 (arrow) offers optimal accuracy (area under the ROC curve 0.778).-
Discussion
To date, RAPN has been reported to result in significantly better preservation of renal function than LPN (10). However, previous reports have mainly identified tumor factors, such as WIT, tumor diameter, residual renal volume, and renal hilar tumor as factors affecting postoperative renal function (8,11,12). Though these are of course important factors in preserving renal function, in practice, the thickness and firmness of PNF may compromise feasibility and surgical outcomes. In the present study, whether the MAP score could predict renal function deterioration after RAPN was evaluated. The MAP score is a simple system to score PNF status, and the results showed that the MAP score was significantly associated with deterioration of GFR on the operated renal side at six months postoperatively.
In recent years, several studies have shown that increased PNF is associated with the progression and development of CKD (5,6,13). The presence of excess PNF was related to a 2.3-fold increased risk of CKD, after adjustments for BMI and the presence of excess visceral adipose tissue (14). Metabolic syndrome and CKD share common risk factors, which include obesity, hypertension, hyperglycemia, and high cholesterol, and the combined presence of these risk factors may increase the burden on the kidneys and increase the risk of CKD. Therefore, since the MAP score suggests visceral fat and fat inflammation, the present study showed that perinephric fat status, a factor other than tumor, was an indicator of deterioration in postoperative split renal function on the operated side.
Hata et al. reported that in laparoscopic partial nephrectomy, the MAP score was a significant predictor of worsening split renal function at three months postoperatively, with a cutoff value of 1.5 (15). However, there have been no studies of relatively long-term postoperative split-renal function in RAPN. The present study showed that the MAP score was a significant discriminative tool for predicting split renal function on the operated side six months after RAPN with a cutoff value of 3.0 (p=0.01). This score was higher than that reported for LPN, indicating that RAPN is more useful in patients with thicker and stiffer PNF. In the present study, the previously reported tumor size was not significantly associated with preserving postoperative split renal function on multivariate analysis. However, the MAP score was the most relevant. This may be due to the fact that RAPN has made resection of the tumor easier, even for relatively large tumors. However, it may be due to the patient’s metabolic factors that affect postoperative split renal function. These results suggest that RAPN may be more advantageous than LPN in preserving split renal function, especially in difficult cases with high MAP scores.
The present study is the first to demonstrate the utility of the MAP score for predicting split renal function after RAPN. There were, however, some limitations. First, this was a retrospective study, and second, it was a study of a relatively small number of patients at a single institution. A future study with a larger sample size at multiple institutions is needed.
Conclusion
An increased MAP score was significantly associated with deterioration of postoperative split renal function six months after surgery on the operated kidney side. The MAP score is useful for predicting postoperative split renal function after RAPN. In addition, the present results suggest that RAPN may be able to better preserve split renal function on the operated kidney side even in complex cases as evaluated by the MAP score than LPN.
Conflicts of Interest
The Authors declare that they have no conflicts of interest in relation to this study.
Authors’ Contributions
Hiroshi Matsuzaki: conception of the study and writing of the manuscript, Kazuna Tsubouchi: data and statistical analysis, Yu Okabe, Takeshi Miyazaki, Naotaka Gunge, Kosuke Tominaga, Yuichiro Fukuhara, Fumihiro Yamazaki, Masahiro Tachibana, Chizuru Nakagawa, Nobuyuki Nakamura: data collection, Nobuhiro Haga: editing of the manuscript.
References
- 1.Ljungberg B, Bensalah K, Canfield S, Dabestani S, Hofmann F, Hora M, Kuczyk MA, Lam T, Marconi L, Merseburger AS, Mulders P, Powles T, Staehler M, Volpe A, Bex A. EAU Guidelines on Renal Cell Carcinoma: 2014 update. Eur Urol. 2015;67(5):913–924. doi: 10.1016/j.eururo.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 2.Pierorazio PM, Patel HD, Feng T, Yohannan J, Hyams ES, Allaf ME. Robotic-assisted versus traditional laparoscopic partial nephrectomy: comparison of outcomes and evaluation of learning curve. Urology. 2011;78(4):813–819. doi: 10.1016/j.urology.2011.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davidiuk AJ, Parker AS, Thomas CS, Leibovich BC, Castle EP, Heckman MG, Custer K, Thiel DD. Mayo adhesive probability score: an accurate image-based scoring system to predict adherent perinephric fat in partial nephrectomy. Eur Urol. 2014;66(6):1165–1171. doi: 10.1016/j.eururo.2014.08.054. [DOI] [PubMed] [Google Scholar]
- 4.Bier S, Aufderklamm S, Todenhöfer T, Kruck S, Schuster K, Rausch S, Othman A, Notohamiprodjo M, Nikolaou K, Schwentner C, Stenzl A, Bier G, Bedke J. Prediction of postoperative risks in laparoscopic partial nephrectomy using RENAL, Mayo adhesive probability and renal pelvic score. Anticancer Res. 2017;37(3):1369–1373. doi: 10.21873/anticanres.11457. [DOI] [PubMed] [Google Scholar]
- 5.Sun X, Han F, Miao W, Hou N, Cao Z, Zhang G. Sonographic evaluation of para- and perirenal fat thickness is an independent predictor of early kidney damage in obese patients. Int Urol Nephrol. 2013;45(6):1589–1595. doi: 10.1007/s11255-013-0404-4. [DOI] [PubMed] [Google Scholar]
- 6.D’Marco L, Salazar J, Cortez M, Salazar M, Wettel M, Lima-Martínez M, Rojas E, Roque W, Bermúdez V. Perirenal fat thickness is associated with metabolic risk factors in patients with chronic kidney disease. Kidney Res Clin Pract. 2019;38(3):365–372. doi: 10.23876/j.krcp.18.0155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kondo T, Takagi T, Morita S, Omae K, Hashimoto Y, Kobayashi H, Iizuka J, Yoshida K, Fukuda N, Tanabe K. Early unclamping might reduce the risk of renal artery pseudoaneurysm after robot-assisted laparoscopic partial nephrectomy. Int J Urol. 2015;22(12):1096–1102. doi: 10.1111/iju.12902. [DOI] [PubMed] [Google Scholar]
- 8.Ohba K, Matsuo T, Mitsunari K, Nakamura Y, Nakanishi H, Mochizuki Y, Miyata Y. Preservation of split renal function after laparoscopic and robot-assisted partial nephrectomy. Anticancer Res. 2022;42(6):3055–3060. doi: 10.21873/anticanres.15792. [DOI] [PubMed] [Google Scholar]
- 9.Kim SP, Alt AL, Weight CJ, Costello BA, Cheville JC, Lohse C, Allmer C, Leibovich BC. Independent validation of the 2010 American Joint Committee on Cancer TNM classification for renal cell carcinoma: results from a large, single institution cohort. J Urol. 2011;185(6):2035–2039. doi: 10.1016/j.juro.2011.02.059. [DOI] [PubMed] [Google Scholar]
- 10.Tachibana H, Takagi T, Kondo T, Ishida H, Tanabe K. Robot-assisted laparoscopic partial nephrectomy versus laparoscopic partial nephrectomy: A propensity score-matched comparative analysis of surgical outcomes and preserved renal parenchymal volume. Int J of Urology. 2018;25(4):359–364. doi: 10.1111/iju.13529. [DOI] [PubMed] [Google Scholar]
- 11.Hinata N, Shiroki R, Tanabe K, Eto M, Takenaka A, Kawakita M, Hara I, Hongo F, Ibuki N, Nasu Y, Teishima J, Kawai N, Kawauchi A, Kondo T, Kawamorita N, Oyama C, Horie S, Shimbo M, Kato M, Kanayama H, Koito Y, Fujisawa M, Japanese Society of Endourology Robot-assisted partial nephrectomy versus standard laparoscopic partial nephrectomy for renal hilar tumor: A prospective multi-institutional study. Int J of Urology. 2021;28(4):382–389. doi: 10.1111/iju.14469. [DOI] [PubMed] [Google Scholar]
- 12.Yu YD, Nguyen NH, Ryu HY, Hong SK, Byun SS, Lee S. Predictors of renal function after open and robot-assisted partial nephrectomy: A propensity score-matched study. Int J Urol. 2019;26(3):377–384. doi: 10.1111/iju.13879. [DOI] [PubMed] [Google Scholar]
- 13.Geraci G, Zammuto MM, Mattina A, Zanoli L, Geraci C, Granata A, Nardi E, Fatuzzo PM, Cottone S, Mulè G. Para-perirenal distribution of body fat is associated with reduced glomerular filtration rate regardless of other indices of adiposity in hypertensive patients. J Clin Hypertens (Greenwich) 2018;20(10):1438–1446. doi: 10.1111/jch.13366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foster MC, Hwang SJ, Porter SA, Massaro JM, Hoffmann U, Fox CS. Fatty kidney, hypertension, and chronic kidney disease: the Framingham Heart Study. Hypertension. 2011;58(5):784–790. doi: 10.1161/HYPERTENSIONAHA.111.175315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hata J, Matsuoka Y, Onagi A, Honda-Takinami R, Matsuoka K, Sato Y, Akaihata H, Ogawa S, Kataoka M, Hosoi T, Kojima Y. Usefulness of the mayo adhesive probability score as a predictive factor for renal function deterioration after partial nephrectomy: a retrospective case–control study. Int Urol Nephrol. 2021;53(11):2281–2288. doi: 10.1007/s11255-021-02986-5. [DOI] [PubMed] [Google Scholar]