Abstract
Introduction
Complex regional pain syndrome (CRPS) is characterized by chronic pain disproportional to any inciting event, and is associated with poor quality of life, and large clinical, healthcare, and societal costs. A CRPS diagnosis is challenging due to the lack of biomarkers and objective laboratory and radiographic tests. CRPS is currently diagnosed according to the IASP clinical diagnostic criteria, and it is not a radiological diagnosis. We report a case of acrometastasis to the hand that was initially thought to be CRPS. The purpose of this publication is to reinforce the importance of CRPS to be a diagnosis of exclusion.
Case presentation
A woman in her 70s presented to a primary care facility with moderate pain in the dorsum of her right wrist and hand that began approximately two weeks prior without trauma. The initial reading of the white blood cell scan and three-phase bone scan (TPBS) were suggested to be compatible with CRPS; however, a pain medicine specialist did not confirm the diagnosis. The patient was later diagnosed with acrometastasis as a result of a bone biopsy demonstrating metastatic lung adenocarcinoma.
Conclusion
CRPS shares clinical indications with various inflammatory diseases. Imaging techniques cannot be solely utilized to diagnose CRPS due to nonuniform findings and not only low but varying sensitivity and specificity. The WBC scan, laboratory results, and the three-phase bone scan did not properly demonstrate CRPS. Our case demonstrates the importance of excluding all conditions with similar presentations prior to determining a CRPS diagnosis and understanding the importance of interpreting a TPBS.
Keywords: Complex regional pain syndrome, Acrometastasis, Three phase bone scan
1. Introduction
Complex regional pain syndrome (CRPS) is a rare condition characterized by chronic pain disproportional to any inciting event, and is associated with poor quality of life, and substantial clinical, healthcare, and societal costs. The severity, symptoms, and potential causes of CRPS vary widely [1]. Complex regional pain syndrome is commonly diagnosed using the International Association for the Study of Pain (IASP) clinical diagnostic criteria, formerly known as the Budapest Consensus Criteria which evaluates sensory, motor, sudomotor, vasomotor, and trophic abnormalities [[1], [2], [3]]. A diagnosis of CRPS type I occurs in patients without known nerve injury/trauma; whereas, CRPS type II occurs in patients with known nerve injury/trauma. A CRPS diagnosis is challenging due to the lack of biomarkers, and objective laboratory and radiographic tests. A CRPS misdiagnosis may lead to extensive medical costs, delay of appropriate treatment options, and exposure to nonindicated treatments.
A potential misdiagnosis is acrometastasis, a bone metastasis distal to the elbow or knee, which is characterized as painful, swollen, and reddened lesions that affect soft tissue and results in reduced range of motion (ROM) [4]. Acrometastasis is extremely rare and represents 0.1% of all bone metastases [4,5]. In ∼10% of acrometastasis cases, it occurs as the first manifestation of previously undiagnosed cancer [6]. Lung cancer is the most common cancer associated with acrometastasis (40–50% of cases) followed by gastrointestinal and urinary tract cancers, respectively [4,5]. The low incidence of this disease in the hand is likely due to the reduction in red marrow, which metastases demonstrate tropism towards [7]. Patients with hand acrometastasis present with generalized symptoms such as swelling, tenderness, loss of function, and erythema which commonly occur with other ailments such as infections, cellulitis, osteomyelitis, sarcoidosis, and other inflammatory diseases. In the hand, the finger/phalanx (68%) is the most common metastatic tumor location followed by the carpal (14%) and metacarpal (14%) sites [4]. The median reported interval from primary tumor diagnosis to acrometastasis is 24 months [4].
We report a case of acrometastasis to the hand that was initially referred to a pain clinic due to concern for CRPS. Upon referral to a pain medicine physician, CRPS was excluded and a diagnosis of metastatic adenocarcinoma consistent with origin from a lung primary was made. The purpose of this publication is to reinforce the importance of CRPS to be a diagnosis of exclusion and to demonstrate the proper three-phase bone scan (TPBS) interpretation. The patient consented and provided authorization to the publication of this case report.
2. Case report
A woman in her 70s presented to a primary care facility with moderate pain in the dorsum of her right wrist with tenderness over her third and fourth carpometacarpal joints that began approximately two weeks prior without known trauma. Past medical history included: hypertension, chronic obstructive pulmonary disease, gastroesophageal reflux disease, asthma, methicillin-resistant Staphylococcus aureus of the right knee, and bilateral carpal tunnel syndrome. The patient stopped smoking tobacco cigarettes twenty-two years prior. A hand x-ray demonstrated no evidence of an acute osseous fracture with bony demineralization and interphalangeal and first carpometacarpal joint space narrowing. The radiologist recommended a three-phase bone scan and an MRI of right hand to exclude an occult fracture. The patient was referred to an orthopedic hand surgeon. Two weeks later, the patient visited an orthopedic hand surgeon and demonstrated inflammation over the extensor digitorum communis (EDC) and tenderness over her third and fourth carpometacarpal joints of her right hand. The patient was diagnosed with extensor tenosynovitis by the orthopedic hand surgeon. A wrist cock-up brace, and a corticosteroid injection targeting the EDC was administered. Six weeks later the patient returned to the orthopedic office, noting short-term relief but eventual return of symptoms. Edema was noted on the right hand. The orthopedic hand surgeon ordered tests and imaging which included: magnetic resonance imaging (MRI), three-phase bone scan (TPBS), whole-body white blood cell (WBC) scan, erythrocyte sedimentation rate (ESR), complete blood count (CBC), and C-reactive protein (CRP).
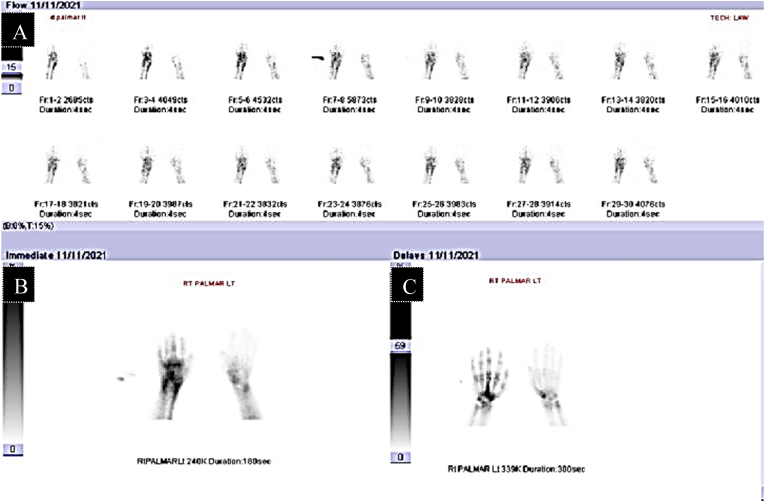
The MRI radiology reading was consistent with a differential diagnosis of osteomyelitis, soft tissue cellulitis, and tenosynovitis (Fig. 1A). A week later, a TPBS was performed after an IV injection of technetium (Tc) 99 m methylene diphosphonate. All three phases (angiographic immediate blood pool and delayed) were abnormal (i.e., increased uptake) at the right wrist and proximal and midshaft third metacarpal (Fig. 2). Specifically, the angiographic (flow) phase demonstrated asymmetric hyperemia about the right wrist and proximal metacarpals. The immediate blood pool phase demonstrated extensive abnormal soft-tissue tracer accumulation about the right wrist and proximal metacarpals. The three-hour delayed images demonstrated moderate periarticular tracer accumulation about the right wrist and metacarpal joints with intense tracer accumulation of the proximal and midshaft of the right third metacarpal. The radiology reading suggested these findings were compatible with CRPS.
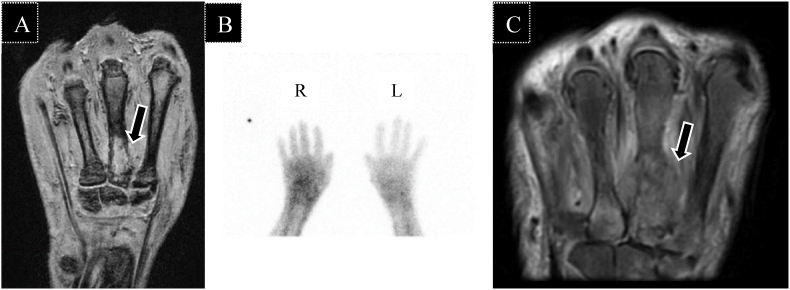
Fig. 1.
Magnetic resonance imaging and white blood cell scan showing perpetuation of acrometastasis to the hand. (A) Coronal T2 magnetic resonance image of right hand two weeks post initial orthopedic patient visit: arrow depicts marrow signal alteration at the 3rd and 4th metacarpal bones with cortical destruction and extensive soft tissue edema of the surrounding muscles and increased peritendinous fluid around the flexor and extensor tendons. (B) White blood cell scan of both hands taken one week after first MRI: asymmetric uptake of white blood cells in the right hand at the level of the metacarpals relative to the left. (C) Coronal T2 fat saturation magnetic resonance image of right hand taken 4 weeks after first MRI: arrow depicts marrow and fusiform soft tissue abnormality centered along the proximal half of the third metacarpal spanning three cm longitudinally.
Fig. 2.
Three-phase bone scan depicting right hand abnormalities in all three phases. (A) Angiographic phase: significant asymmetric hyperemia about the right wrist and proximal metacarpals. (B) Immediate blood pool phase: extensive abnormal soft tissue tracer accumulation about the right wrist and proximal metacarpals (C) Three hour delayed images: moderate periarticular accumulation about the right wrist and metacarpal phalangeal joints with intense tracer accumulation in the proximal and mid shaft of the right third metacarpal.
A WBC scan was conducted. Delayed images of the hand were obtained following injection of technetium 99 M Certec labeled WBC's depicting asymmetric uptake of the right hand at the level of the metacarpals relative to the left (Fig. 1B). The WBC scan reading stated that these findings can be seen in CRPS. The lab work demonstrated an elevated CRP (2.01 mg/dL) and, ESR (49 mm/hr.), and normal WBC count (7.2 K/cumm). Due to the interpretation of the WBC scan and TPBS, the patient was recommended to a pain medicine specialist for a diagnosis of CRPS.
Two weeks later, a pain medicine specialist concluded the patient did not demonstrate CRPS according to the IASP criteria. Although the patient demonstrated temperature asymmetry and edema, she lacked continuing pain disproportionate to any inciting event and no other diagnosis that better explained her signs and symptoms. The patient's inflammatory markers were elevated, and the previous MRI had concern for infection. A new MRI was ordered to further assist with determining a definitive diagnosis. The new MRI was suggestive of malignancy on the proximal half of the third metacarpal although indolent infection was a possible alternative (Fig. 1C). The following day, a right hand third and fourth metacarpal soft tissue and bone incisional biopsy led to a diagnosis of metastatic adenocarcinoma consistent with origin from a lung primary. The patient's wrist and hand were placed into a splint. A week later, an anatomic and clinical pathology specialist diagnosed the patient with metastatic adenocarcinoma consistent with origin from a lung primary. The diagnosis was further confirmed by computed tomography scan with contrast and positron emission tomography (PET) scan of the chest that both depicted a large mass (6.6 x 5.6 x 6 cm) within the right upper lobe with spiculated margins extending towards the right lung apex and perihilar region. One week later, an MRI of the brain with and without contrast found two enhancing metastatic lesions in the left temporal lobe measuring up to 2.4 cm with vasogenic edema and mass effect causing minimal left-to-right midline shaft. The patient met with a radiation oncologist and proceeded to receive treatment for metastatic non-small cell lung cancer.
3. Discussion
Overdiagnosis of CRPS may occur, because CRPS shares signs and symptoms with various diseases such as acrometastasis as shown in Table 1. Many signs and symptoms of CRPS can also be caused by other diseases [8]. In our case report, correct diagnosis was vital as the mean life expectancy after diagnosis of acrometastasis is six months [4]. Approximately, one in nine (11%) cases of acrometastasis to the hand are treated initially as inflammatory conditions [5]. To our knowledge, existing published literature contains one case in which a malignant tumor (i.e., synovial sarcoma) was initially recognized as CRPS [9]. In addition, previous case reports describe the misdiagnosis of CRPS in individuals with a benign vascular tumors (i.e., glomus tumor) in the upper and lower extremities [10,11].
Table 1.
Clinical indications of complex regional pain syndrome and acrometastasis to the handa.
| Possible Clinical Indications | Complex Regional Pain Syndrome | Acrometastasis to the Hand | Patient-reported Symptoms |
|---|---|---|---|
| Intense Pain | X | X | X |
| Hyperalgesia | X | ||
| Allodynia | X | ||
| Temperature asymmetry | X | X | X |
| Skin color changes | X | X | X |
| Skin color asymmetry | X | X | X |
| Edema | X | X | X |
| Sweating changes | X | ||
| Sweating asymmetry | X | ||
| Decreased range of motion | X | X | X |
| Motor dysfunction | X | X | X |
| Trophic changes | X |
X denotes that the clinical indication maybe present in the respective condition.
Not all patients will display every clinical indication at presentation.
Various imaging techniques and laboratory tests are utilized as adjuncts to help diagnose CRPS and exclude other conditions [8,12]. However, there currently is no single measurement or interpretation that establishes a diagnosis of CRPS [1,13]. The CBC, ESR, and CRP laboratory tests are commonly utilized in the investigation of CRPS cases; however, they are predominantly used to exclude infection or rheumatologic diseases [8]. Imaging techniques such as MRI cannot be solely utilized to diagnose CRPS due to nonuniform findings, and a low sensitivity and specificity [8]. Nonspecific MRI findings at times seen include periarticular marrow edema, soft tissue swelling and joint effusions [13]. Although associated with variable predictive capabilities, the TPBS has been suggested as helpful radiographic technique to help exclude a diagnosis of CRPS based on increased sensitivity and higher negative predictive value in comparison to MRI and plain film radiography [12,14]. A TPBS is a multi-step imaging procedure that exploits the pharmacology of methyldiphosphonate to yield information about perfusion status, soft tissue edema and inflammation, and degree of osteoblastic activity in the relevant joint or extremity [15]. A TBPS of CRPS manifests as asymmetric uptake, and increased bone metabolism and turnover and these activities may be seen in all three phases [13,15]. Some have suggested that the delayed phase changes are the most consistent in CRPS [16]. However, bone changes are not currently part of the IASP criteria and the value of a three-phase bone scan to support a diagnosis of CRPS has been questioned [1,17,18]. TPBS findings may also change whether in acute CRPS versus chronic CRPS. Furthermore, tests like the x-rays, TPBS, and MRI have demonstrated wide ranges for specificity, sensitivity, positive predictive value, and negative predictive value [14]. In conclusion, it must be remembered that the standard for CRPS diagnosis is the IASP clinical diagnostic criteria and that it is not a radiological diagnosis.
The patient did have official readings from the TPBS and WBC scan concerning for CRPS which resulted in the referral. However, upon presentation the patient demonstrated other abnormalities that required further examination. First, the patient had elevated inflammatory markers which would not be suggestive of CRPS. Furthermore, the initial MRI was concerning for osteomyelitis or tenosynovitis. Although the bone scan did demonstrate increased periarticular uptake (Fig. 2A), when specifically looking at the delayed phase image the abnormality only existed in the third metacarpal (Fig. 2C). In CRPS, the delayed phase image demonstrates prominent periarticular activity and has the highest sensitivity of all phases [16,19]. For CRPS, one would expect the whole hand to display increased periarticular activity not just the third metacarpal. A CRPS diagnosis was unlikely; therefore, tumor or infection were the most likely diagnoses at the time. The WBC scan was not suggestive of osteomyelitis as no focal WBC uptake was seen in the third metacarpal. The TBPS directly led to a false diagnosis, and TPBS are neither fully sensitive nor specific to diagnose CRPS. TPBS are not a part of the IASP criteria, and therefore, should be used only to support or not support a diagnosis, but not to form the diagnosis of CRPS. Physicians who have received a radiological diagnosis of CRPS should still evaluate patients according to IASP clinical diagnostic criteria. Our case demonstrates the importance of excluding all conditions with similar presentations prior to determining a CRPS diagnosis. Additionally, physicians need to understand the interpretation of a TPBS.
Funding
The authors have no sources of funding to declare for this manuscript.
Authorship statement
David Provenzano MD, and Hunter Leech, were involved with study inception, data collection, and manuscript preparation. Leonard DeRiggi, MD was involved with data collection and manuscript preparation.
Previous presentations
American Society of Regional Anesthesia and Pain Medicine 21st Annual Meeting. Orlando, Florida. November 2022.
Declaration of competing interest
Dr. Provenzano has consulted for Avanos, Boston Scientific, Medtronic, Nevro, and SI Bone. Pain Diagnostics and Interventional Care received research support from Avanos, Medtronic, Nevro, Stimgenics, and Abbott. HXL and LAD have no conflicts to report.
References
- 1.Harden R.N., McCabe C.S., Goebel A., et al. Complex regional pain syndrome: practical diagnostic and treatment guidelines, 5th edition. Pain Med. 2022;23(Suppl 1):S1–s53. doi: 10.1093/pm/pnac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harden R.N., Bruehl S., Stanton-Hicks M., Wilson P.R. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007;8(4):326–331. doi: 10.1111/j.1526-4637.2006.00169.x. [DOI] [PubMed] [Google Scholar]
- 3.Goebel A., Birklein F., Brunner F., et al. The Valencia consensus-based adaptation of the IASP complex regional pain syndrome diagnostic criteria. Pain. 2021;162(9):2346–2348. doi: 10.1097/j.pain.0000000000002245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Umana G.E., Scalia G., Palmisciano P., et al. Acrometastases to the hand: a systematic review. Medicina. 2021;57(9) doi: 10.3390/medicina57090950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sahoo T.K., Das S.K., Majumdar S.K., Senapati S.N., Parida D.K. Digital acrometastasis as initial presentation in carcinoma of lung A case report and review of literature. J Clin Diagn Res : J Clin Diagn Res. 2016;10(6):Xd01–xd02. doi: 10.7860/JCDR/2016/16063.7951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Apollonatou V., Loukides S., Papaioannou A.I., Papiris S. Acrometastasis due to lung adenocarcinoma. Advances in respiratory medicine. 2018;86(2):97–100. doi: 10.5603/ARM.2018.0013. [DOI] [PubMed] [Google Scholar]
- 7.Flynn C.J., Danjoux C., Wong J., et al. Two cases of acrometastasis to the hands and review of the literature. Curr Oncol. 2008;15(5):51–58. doi: 10.3747/co.v15i5.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Eijs F., Stanton-Hicks M., Van Zundert J., et al. Evidence-based interventional pain medicine according to clinical diagnoses. 16. Complex regional pain syndrome. Pain Pract. 2011;11(1):70–87. doi: 10.1111/j.1533-2500.2010.00388.x. [DOI] [PubMed] [Google Scholar]
- 9.Kennedy R., Hester J., Simon D.W. Malignancy as a possible complication of complex regional pain syndrome: a case report. Pain Med. 2010;11(1):101–105. doi: 10.1111/j.1526-4637.2009.00753.x. [DOI] [PubMed] [Google Scholar]
- 10.Nazemi A.K., Grossi J., Tavernier F.B., Boyce B.F., Komatsu D.E., Khan F.A. Glomus tumor of the lower extremity previously misdiagnosed as complex regional pain syndrome in close proximity to a myxofibrosarcoma: a case report. Journal of the American Academy of Orthopaedic Surgeons Global research & reviews. 2022;6(7) doi: 10.5435/JAAOSGlobal-D-21-00311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Macharia C., Nthumba P.M. Glomus tumor presenting as complex regional pain syndrome of the left upper limb: a case report. J Med Case Rep. 2015;9:293. doi: 10.1186/s13256-015-0793-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee E., Worsley D.F. Role of radionuclide imaging in the orthopedic patient. Orthop Clin N Am. 2006;37(3):485–501. doi: 10.1016/j.ocl.2006.04.003. [viii] [DOI] [PubMed] [Google Scholar]
- 13.Intenzo C.M., Kim S.M., Capuzzi D.M. The role of nuclear medicine in the evaluation of complex regional pain syndrome type I. Clin Nucl Med. 2005;30(6):400–407. doi: 10.1097/01.rlu.0000162605.14734.11. [DOI] [PubMed] [Google Scholar]
- 14.Cappello Z.J., Kasdan M.L., Louis D.S. Meta-analysis of imaging techniques for the diagnosis of complex regional pain syndrome type I. J Hand Surg. 2012;37(2):288–296. doi: 10.1016/j.jhsa.2011.10.035. [DOI] [PubMed] [Google Scholar]
- 15.Howard B.A., Roy L., Kaye A.D., Pyati S. Utility of radionuclide bone scintigraphy in complex regional pain syndrome. Curr Pain Headache Rep. 2018;22(1):7. doi: 10.1007/s11916-018-0659-7. [DOI] [PubMed] [Google Scholar]
- 16.O'Donoghue J.P., Powe J.E., Mattar A.G., Hurwitz G.A., Laurin N.R. Three-phase bone scintigraphy. Asymmetric patterns in the upper extremities of asymptomatic normals and reflex sympathetic dystrophy patients. Clin Nucl Med. 1993;18(10):829–836. doi: 10.1097/00003072-199310000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Bruehl S. Complex regional pain syndrome. BMJ. 2015;351:h2730. doi: 10.1136/bmj.h2730. [DOI] [PubMed] [Google Scholar]
- 18.Lee G.W., Weeks P.M. The role of bone scintigraphy in diagnosing reflex sympathetic dystrophy. J Hand Surg Am. 1995;20(3):458–463. doi: 10.1016/S0363-5023(05)80107-8. [DOI] [PubMed] [Google Scholar]
- 19.Sampath S., Mittal B.R., Arun S., Sood A., Bhattacharya A., Sharma A. Usefulness of asymmetry score on quantitative three-phase bone scintigraphy in the evaluation of complex regional pain syndrome. Indian J Nucl Med : IJNM : the official journal of the Society of Nuclear Medicine, India. 2013;28(1):11–16. doi: 10.4103/0972-3919.116798. [DOI] [PMC free article] [PubMed] [Google Scholar]