Abstract
Background
Recent studies have questioned the validity of targeting the thoracic medial branch via anesthetic blocks or radiofrequency neurotomy for the diagnosis or treatment of pain from the thoracic zygapophysial joints.
Purpose
To define the origin and course of the articular branches to the thoracic zygapophysial joints at all levels.
Design
Cadaveric dissection.
Setting
The Gross Anatomy Laboratory at the University of New England College of Osteopathic Medicine.
Subjects
One cadaveric thoracic spine.
Methods
Gross and stereoscopic dissection of the bilateral dorsal rami T1–T12 was performed on one embalmed cadaver. The medial and lateral branches were traced from their cutaneous distribution to the origin at the dorsal ramus. The articular branches were identified using stereoscopic dissection by tracing their origin from the dorsal ramus or medial branch to the capsule of the zygapophysial joint. The images were recorded using digital photography.
Results
Twenty-two of the twenty-four articular branches were identified in a single cadaveric specimen. Articular branches at T7 on the right side and T9 on the left side were not identified. 5 of the 22 (18%) articular branches were observed to arise from the proximal segment of the medial branch of the dorsal ramus. Of the remainder, 17 of the 22 (78%) articular branches were observed to arise from the dorsal primary ramus itself. At levels T1-9, the articular branch coursed inferiorly along the lamina to reach the joint capsule. At levels T10-T12, the articular branch traversed the intervertebral foramen to reach the facet joint. The T12 medial branch on the left was seen to travel inferior to innervate the L1/L2 zygapophysial joint.
Conclusion
The source of the innervation for the thoracic zygapophysial is variable and can arise from the dorsal ramus itself or from the proximal segment of the medial branch. Unlike the cervical and lumbar medial branches, which innervate two joints each, in this case, the thoracic dorsal rami appear to innervate only the zygapophysial joint at the level of the nerve exit. It should be noted that the findings may be limited in their generalizability due to the reliance on a single cadaver study.
1. Introduction
Provocative intra-articular injections performed by Dreyfuss et al. [1] provided preliminary confirmation that the thoracic zygapophysial joints could generate pain in a reproducible local and referred pattern.
Based on controlled diagnostic blocks, thoracic zygapophysial joints have been implicated in an estimated 34%–48% of patients with chronic mid-back and upper-back pain. Thoracic medial branch blocks and radiofrequency ablation (RFA) have therefore emerged as attractive diagnostic and therapeutic options, respectively, for pain postulated to derive from the thoracic zygapophysial joint [2,3].
Targeting the medial branch is a standard treatment for addressing cervical and lumbar zygapophysial joint-related pain. These techniques are based on the rationale that interrupting nociceptive signaling in the medial branches of the dorsal rami, which innervate the zygapophysial joint in question, may have diagnostic and prognostic (as in medial branch block) as well as therapeutic utility (as in radiofrequency neurotomy). Successful medial branch blocks and subsequent radiofrequency ablation, however, require precise anatomic localization of the target sensory nerve. Face validity of thoracic medial branch blocks was based on an early cadaveric study with India ink. Therapeutic targets for medial branch neurotomy in the thoracic spine were subsequently guided by dissections conducted by Chua and Bogduk. The study demonstrated that the medial branches exhibited a consistent course at the upper (T1-T4) and lower (T9-10) thoracic levels, crossing the superolateral aspect of the transverse process [4]. The relationship with osseous landmarks at these levels lent credence to fluoroscopic-based techniques. Notably, however, the study observed that the medial branches at the mid-thoracic levels (T5-T8) assumed a course through soft tissue in the middle of the intertransverse space without consistent relationship to fluoroscopically observable landmarks.
Recent studies, however, have called into question the fundamental basis of thoracic medial branch blocks and medial branch neurotomy [5,6]. This experimental study was conducted to further clarify the anatomic origin and course of articular branches that innervate the thoracic zygapophysial joints, with the aim of providing guidance for future procedures.
2. Methods
For this study, one adult male (67 years) embalmed cadaver was obtained through the University of New England Willed Donor Program. The cadaver had no known previous thoracic surgery, but fluoroscopic imaging did reveal two lumbar vertebrae (L2, L4) with a prior vertebroplasty procedure.
Bilateral dissection was performed on the cadaver using loupes (Zeiss Loupes: EM ProS 4.0x/450) and stereo-microscopic (Nikon SMZ 745 Stereo Microscope) visualization. The dissection was completed with the cadaver in the prone position. The skin was removed carefully to preserve all medial and lateral dorsal thoracic cutaneous nerves and the fascia was dissected away to reveal the trapezius and latissimus dorsi musculature. The superficial back muscles (trapezius, latissimus dorsi and rhomboids), intermediate back muscles (serratus posterior superior and inferior) were reflected to reveal the thin layer of thoracolumbar fascia encasing the erector spinae muscles.
The thoracolumbar fascia was removed, and the longissimus muscle was reflected from superior to inferior, removing the attachments of the muscle to reveal all lateral branches of the dorsal rami. Medially, the spinalis and semispinalis muscles were removed to reveal the medial branch of the dorsal rami and its branches lying in the fascial plane superficial to the thoracic multifidus. The thoracic multifidus and rotatores muscles were then removed carefully, in some cases fiber by fiber, to reveal the medial branch exiting the intervertebral foramen along with the associated transforaminal ligaments. In most cases, these transforaminal ligaments were delicately reflected to reveal the articular branch of the dorsal rami.
3. Results
For each level (T1-T12), the course of the medial branch was dissected from distal to proximal (Fig. 1a). In this specimen, the medial branch exited the intervertebral foramen into the intertransverse space anterior to the lamina, between the rotatores muscle and the multifidus thoracis muscle. At the T1-T9 segments, as the medial branch reached the lateral edge of the multifidus thoracis muscle, it curved inferomedially near the superolateral edge of the transverse process. At the T10-T12 segments, the medial branch passed directly over the transverse process in a small groove. The medial branch then continued, at all levels, passing between the multifidus thoracis muscle and the semispinalis thoracis muscle. In this plane, the medial branch gave off multiple nerves entering the musculature, and great care was exercised in tracing these branches deep to the zygapophysial joint, with the aim of identifying evidence of the previously described innervation pattern.
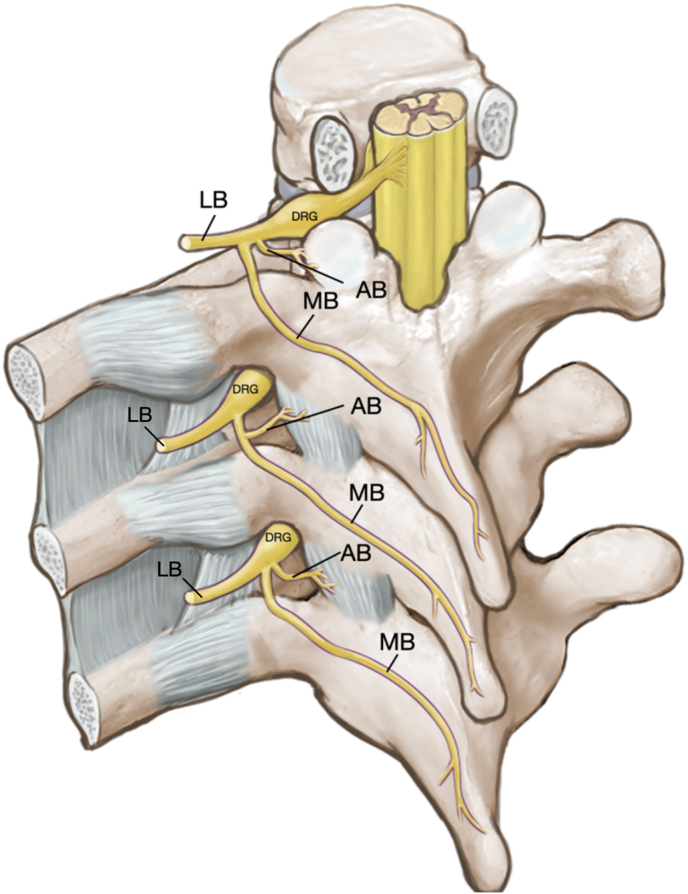
Fig. 1a.
Schematic of anatomic dissection from current study showing the two configurations of the articular branch (AB) arising from the dorsal ramus on the upper and lower levels and arising from the proximal part of the medial branch (MB) on the second level (Fig. 1a). DRG – dorsal root ganglion; LB – lateral branch.
In this dissection, the conventional innervation (dual level innervation with articular branches arising from the distal medial branches after they crossed the superolateral transverse process, as described by Chua and Bogduk as shown in Fig. 1b) was not observed at any of the levels. However, an intricate arcading of nerves was noted to exist between the medial branches. As the medial branch reached the midline at the upper segments (T1-T6), it exited through the erector spinae and superficial musculature to become cutaneous. At the lower thoracic segments (T7-T12), the medial branch entered the musculature exclusively and did not give rise to any cutaneous nerves.
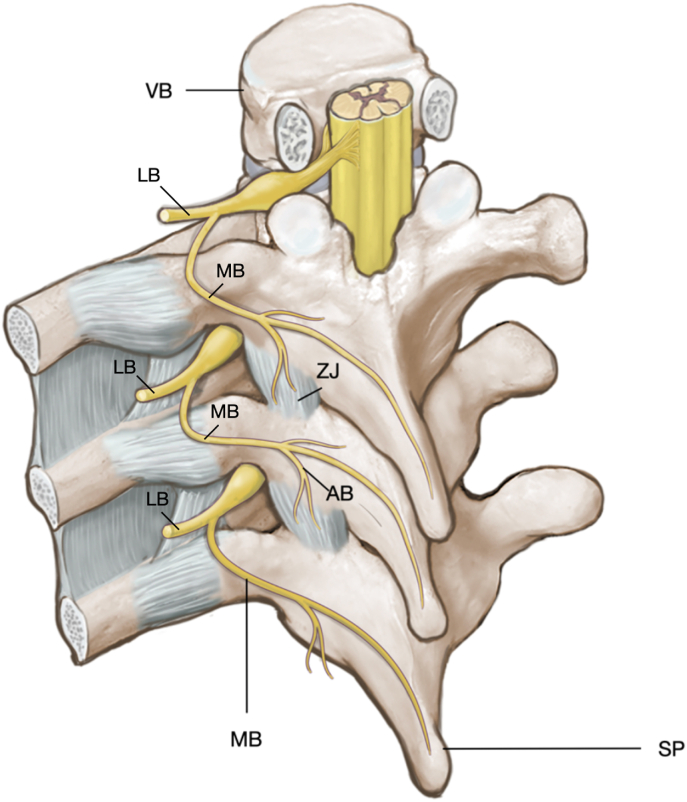
Fig. 1b.
Schematic of anatomic discussion showing the articular branch (AB) arising from the distal part of the medial branch (MB) providing innervation to the zygapophysial joint (ZJ); from Chua WH, Bogduk N. The surgical anatomy of thoracic facet denervation. Acta Neurochir (Wien). 1995; 136 (3–4):140–144. https://doi.org/10.1007/BF01410616. Reproduced with permission (Fig. 1b). LB – lateral branch of the dorsal ramus; VB – vertebral body; SP – spinous process.
The articular branches innervating the zygapophysial joints were identified on 22 of the 24 dorsal rami dissected. At the upper thoracic segments (T1-3), each articular branch was seen arising from the very proximal segment of the medial branch in 5 of the 6 (83.3%) levels dissected (Fig. 2a). One branch, T3 on the left side, arose from the dorsal ramus itself. These articular branches then descended inferiorly along the lamina, deep to the laminotransverse ligament to enter the capsule of the zygapophysial joint.
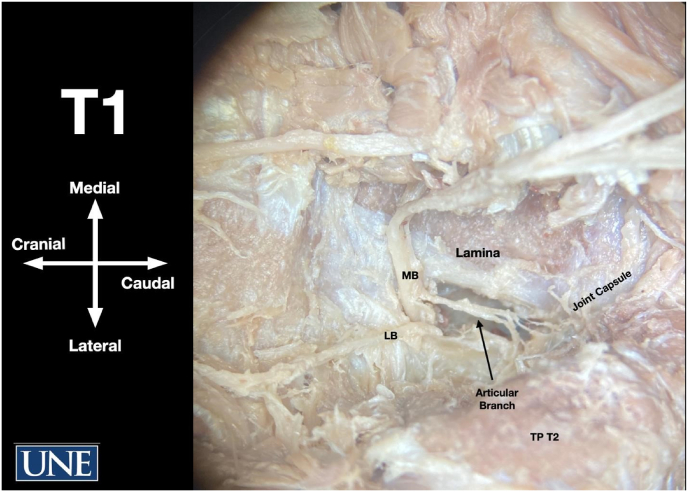
Fig. 2a.
Image of the T1 dorsal ramus showing the articular branch arising from the medial branch, descending along the lamina, and entering the joint capsule. MB medial branch, LB lateral branch TP transverse process (Fig. 2a).
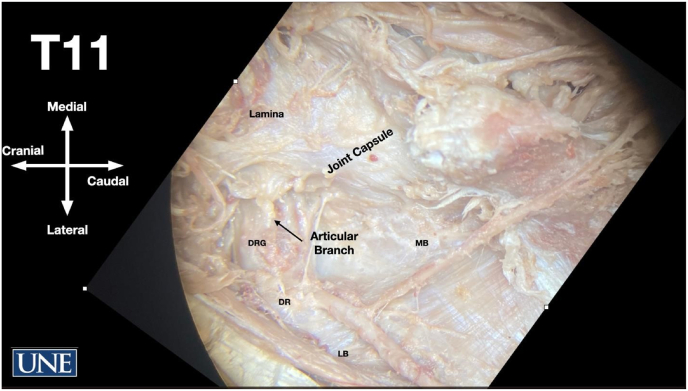
At the middle thoracic segments, T4-9 (note that T7 on the right and T9 on the left were not visualized in this dissection), all the identified articular branches arose from the dorsal ramus itself before its division into medial and lateral branches as shown in Fig. 2b. The articular nerve followed a similar pathway to those in the upper thoracic levels, descending along the lamina into the zygapophysial joint space. At the lower thoracic segments (T10-12), the articular branch was once again seen to arise from the dorsal ramus, but this time it did so more proximal and very close to the dorsal root ganglion. At these levels, the articular branch took a more transverse path, directly into the joint space, as illustrated in Fig. 2c. On the left side, the T12 medial branch was seen descending and coursing directly over the T12/L1 zygapophysial joint, with small nerves entering the joint space. During the dissection, small nerve branches were identified that appeared to be ascending toward the lamina above. However, upon further examination, these branches were traced to the surrounding local vasculature, and none of them were observed to extend far enough to reach the joint above.
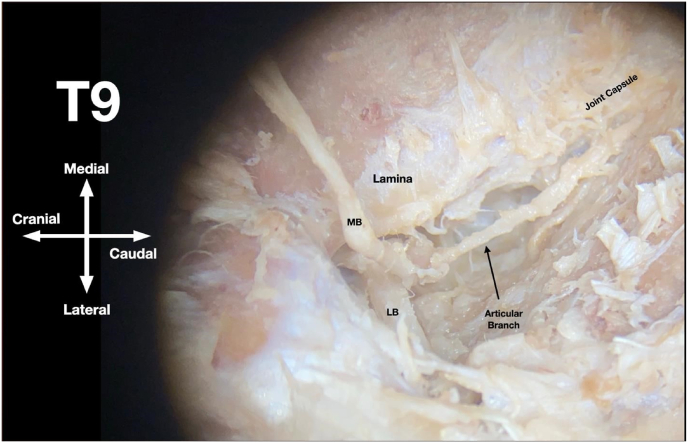
Fig. 2b.
Image of the T9 dorsal ramus showing the articular branch arising from the dorsal ramus, descending along the lamina, and entering the joint capsule. MB medial branch, LB lateral branch TP transverse process (Fig. 2b).
Fig. 2c.
Image of the T11 dorsal ramus showing the articular branch arising from the dorsal ramus just distal to the dorsal root ganglion and traversing the intervertebral foramen entering the joint capsule. MB medial branch, LB lateral branch TP transverse process, DRG dorsal root ganglion, DR dorsal ramus (Fig. 2c).
To summarize, in this cadaveric dissection, innervation to the zygapophysial joints was identified in 22 of the 24 dorsal rami dissected. At the upper thoracic segments (T1-3), the articular branch arose from the very proximal part of the medial branch of the dorsal ramus. At the middle thoracic segments (T4-9), the articular branch derived from the dorsal rami itself before their division into the medial and lateral branches. And at the lower thoracic segments (T10-12), the articular branch was again observed to arise from the dorsal ramus, situated even more proximally than at the middle thoracic segments and near the dorsal root ganglion.
4. Discussion
This detailed anatomic study aimed to update our current understanding of the anatomic course of the medial branch of the dorsal ramus, as well as to identify the origin and course of the articular nerves that innervate the zygapophysial joints of the thoracic vertebrae. This knowledge is essential for guiding procedures, including thoracic medial branch blocks and radiofrequency neurotomy. Notably, previous anatomical investigations have failed to establish a consensus regarding both the course of the medial branch and the origin and course of the articular branches (see Table 1).
Table 1.
Summary of findings of previous studies.
| Study | Number of Cadavers | Demographics (Gender, Mean Age) | Thoracic Levels or Nerves Dissected | Findings |
|---|---|---|---|---|
| Chua and Bogduk (1995) | 4 | 2 male, 2 female Age: 68.5 |
84 medial branches | Origin (Medial Branch): |
| ||||
| Course (Medial Branch): | ||||
| ||||
| Origin (Articular Branch): | ||||
| ||||
| ||||
| Course (Articular Branch): | ||||
| ||||
| ||||
| Archetypical course of medial branches consistently exhibited by nerves at the upper thoracic levels (T1-T4) and lower levels (T9-T10) | ||||
| Ishizuka et al. (2012) | 10 | 8 male, 2 female Age: 72 | 120 pairs of thoracic spinal nerves | Origin (Medial Branch): |
| ||||
| Course (Medial Branch): | ||||
| ||||
| ||||
| Origin (Articular Branch): | ||||
| ||||
| Course (Articular Branch): | ||||
| ||||
| Joshi et al. (2019) | 10 | 5 male, 5 female Age: 68.6 | Dorsal rami of T4-T8 48 inferior articular branches, 51 superior articular branches | Origin (Medial Branch): |
| ||||
| Course (Medial Branch): | ||||
| Dorsal ramus divided into medial and lateral branches | ||||
| Origin (Articular Branch): | ||||
| ||||
| ||||
| Course (Articular Branch): | ||||
| ||||
| Koutp et al. (2022) | 20 | 13 male, 7 female Age: 78.8 |
T10-T12 120 pairs of thoracic spinal nerves |
Origin (Medial Branch): |
| ||||
| Course (Medial Branch): | ||||
| ||||
| ||||
| ||||
| Origin (Articular Branch): | ||||
| ||||
| Course (Articular Branch): | ||||
| ||||
| Koutp et al. (2022) | 20 | 10 male, 10 female Age: 84.45 |
T1-T9 462 medial branches; 118 articular branches |
Origin (Medial Branch): |
| ||||
| Course (Medial Branch): | ||||
| ||||
| Origin (Articular Branch): | ||||
| ||||
| Course (Articular Branch): | ||||
| ||||
| Current study | 1 | 1 male Age: 67 | T1-T12 | Origin (Medial Branch): |
| ||||
| Course (Medial Branch) | ||||
| ||||
| Origin (Articular Branch): | ||||
| ||||
| ||||
| ||||
| Course (Articular Branch): | ||||
| ||||
|
Originally described by Chua and Bogduk, the medial branch was reported to consistently follow a specific course: it originated from the dorsal ramus and stayed in the intertransverse space where it continued laterally to the superolateral border of the transverse process. From here, the medial branch passed inferomedially between the multifidus and semispinalis muscle before emerging through the spinalis and superficial back muscles to become cutaneous [4]. It's worth noting that at mid-thoracic levels (T5-T8), the medial branch was observed to enter the posterior compartment of the back instead of contacting the transverse process, thereby limiting the utility of osseous landmarks. This pattern was similarly described by Ishizuka et al. and Koupt et al. [5,7,8] This study reaffirms this observed course of the medial branch and additionally identifies an arcading of the distal medial branches.
The origin and course of the articular branches was also originally described by Chua and Bogduk. These authors delineated two types of articular branches: an ascending branch originating from the medial branch as it passed caudally to the zygapophysial joint, and a descending branch that also arose from medial branch but passed through the multifidus muscle after the medial branch curved over the superolateral edge of the transverse process [4]. Other studies, however, did not consistently corroborate these findings. The validity of targeting thoracic medial branches was initially challenged in a study by Ishizuka et al. who noted that the medial branches were present at the lateral bifurcation of the posterior ramus but did not send branches to the zygapophysial joint in any specimen. Instead, the articular branches of the thoracic zygapophysial joints seemed to originate from an “articular type descending branch,” which was the first branch of the posterior ramus [5]. Additional data from gross and stereoscopic dissection of T4-T8 dorsal rami conducted by Joshi et al. found that only 11% of specimens had articular branches emanating from the thoracic medial branch [6]. The “descending branch” described by Ishizuka was thought to potentially correspond to the articular branches seen in this study. Notably, in 88% of specimens, the articular branches appeared to originate from the posterior ramus and necessitated a partial lateral laminectomy for full exposure due to their proximity to the intervertebral foramen. The dissections of Joshi et al. also described ascending branches, but these branches were not tracked to confirm their entry into the zygapophysial joint. These branches were also seen in our dissection, but they are likely to be vascular nerves and do not appear to extend to the joint above.
Subsequently, Koupt et al. conducted a dissection of 20 spines, focusing at the T1-T9 segments, and demonstrated that the articular branches originated from the medial branch and entered the joint capsule only at the adjacent level [8]. In a second study by Koupt, also involving 20 spines, two distinct topographical courses of the medial branch at the T10-T12 segment. In 70% of cases, the medial branch originated from the dorsal ramus about 5 mm from the lateral margin of the intervertebral foramen, resembling the descriptions of Chua and Bogduk. In the remaining 30%, however, the medial branch passed parallel but superior to the previously described course, with no contact to the superolateral transverse process. Two fine articular branches arising from the medial branch with an ascending and descending pattern was seen often at segments T11 and T12 [7]. Koupt et al. were unable to definitively exclude the possibility of a singular articular branch arising from the dorsal branch, as described by Ishizuka et al. [7] The present study identified a single articular branch originating from the proximal medial branch at the upper thoracic segments T1-3, a single articular branch originating from the dorsal ramus at the segments T4-11, and ascending and descending articular branches in the T12 segment, mirroring the pattern in the lumbar spine.
These findings raise concerns about the validity of targeting the thoracic medial branches for thoracic zygapophysial pain, primarily due to the proximal origin of the articular branch at all thoracic levels. Our findings align with similar conclusions drawn from the work of Ishizuka et al. and Joshi et al. [5,6] Targeting the articular branch directly may not be safe or practical due to the proximity to the dorsal root ganglion and ventral ramus. Additionally, the proximity to the intervertebral foramen may compromise the diagnostic and prognostic value of thoracic medial branch blocks, as they have the potential for foraminal spread [6]. A potential approach, which may warrant future investigation, would involve targeting the articular branch at the articular margin itself.
The limitations of this study include the sample size of a single cadaver, which may limit the ability to extrapolate the findings at a population level. Articular branches at T7 right and T9 left were not identified in the dissection. Additionally, the absence of direct histological confirmation for the articular branches under investigation underscores the need for further validation of the identified structures to ensure the accuracy of the reported findings.
5. Conclusion
The clinical implications of our detailed anatomic study challenge the fundamental concept of targeting the thoracic medial branch nerves for anesthetizing the thoracic zygapophysial joints. In our dissection, the articular branch was observed to originate from the very proximal part of the medial branch (T1-3) or directly from the dorsal ramus itself (T4-12). This observation indicates that the previously advocated targeting of the medial branch would not effectively disrupt nociceptive signaling from the thoracic zygapophysial joints. Directly targeting the proximal articular branches as an alternative approach may carry the risk of injuring critical structures, including the dorsal root ganglion and ventral ramus. Consequently, a potential avenue for future investigation involves targeting the articular branch at the articular margin as a management strategy for thoracic zygapophysial joint pain.
The authors would like to thank Paul J. Mast OMS-2, Hunter T. Scott OMS-2 and James R. Withers OMS-3 for their assistance with the dissections. The authors would also like to thank Oran Suta for his assistance with graphics arts and illustrations.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Dreyfuss P., Tibiletti C., Dreyer S.J. Thoracic zygapophysial joint pain patterns: a study in normal volunteers. Spine. 1994;19(7):807–811. doi: 10.1097/00007632-199404000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Manchikanti L., Singh V., Pampati V., Beyer C.D., Damron K.S. Evaluation of the prevalence of facet joint pain in chronic thoracic pain. Pain Physician. 2002;5(4):354–359. [PubMed] [Google Scholar]
- 3.Atluri S., Datta S., Falco F.J.E., Lee M. Systematic review of diagnostic utility and therapeutic effectiveness of thoracic facet joint interventions. Pain Physician. 2008;11(5):611–629. [PubMed] [Google Scholar]
- 4.Chua W.H., Bogduk N. The surgical anatomy of thoracic facet denervation. Acta Neurochir. 1995;136(3–4):140–144. doi: 10.1007/BF01410616. [DOI] [PubMed] [Google Scholar]
- 5.Ishizuka K., Sakai H., Tsuzuki N., Nagashima M. Topographic anatomy of the posterior ramus of thoracic spinal nerve and surrounding structures. Spine. 2012;37(14):E817–E822. doi: 10.1097/BRS.0b013e31824b65ea. [DOI] [PubMed] [Google Scholar]
- 6.Joshi A., Amrhein T.J., Holmes M.A., Talsma J., Shonyo M., Taylor A.B. The source and the course of the articular branches to the T4-T8 zygapophysial joints. Pain Med. 2019;20(12):2371–2376. doi: 10.1093/pm/pnz116. [DOI] [PubMed] [Google Scholar]
- 7.Koutp A., Petritsch J., Skias C., et al. Anatomical topographical investigation of the medial branch of the dorsal thoracic branch of the spinal nerve in the segments T10—T12. Pain Med. 2022;23(11):1863–1868. doi: 10.1093/pm/pnac073. [DOI] [PubMed] [Google Scholar]
- 8.Koutp A., Sadoghi P., Petritsch J., Skias C., et al. Anatomical-topographical investigation of the branches of the dorsal ramus of thoracic spinal nerves. Pain Med. 2022;23(11):1869–1874. doi: 10.1093/pm/pnac072. [DOI] [PubMed] [Google Scholar]