Abstract
Background
Percutaneous rhizotomy is a group of techniques used to treat trigeminal neuralgia. Radiofrequency thermocoagulation (RF) and Chemical Rhizotomy (CR) using glycerol are among the most frequently used methods. We have recently refined Ethanol Rhizotomy (ER) under Digital Subtraction Angiography (DSA) guidance.
Objective
A descriptive, retrospective study was conducted to compare our refined ER and RF ablation in patients with trigeminal neuralgia in terms of long-term pain relief and side effects.
Method
Between 2012 and 2014, 33 patients with typical trigeminal neuralgia were enrolled, 10 of whom received RF and 23 received ER under (DSA) guidance with ethanol injected while in the supine position. The pain relief, duration of pain-free period, need for repeat injection, and recurrence of pain were recorded together with procedure-related complications within 7 years after the procedures.
Results
After a single intervention or, in some cases, a maximum of two repeated interventions, all 33 patients experienced complete pain relief. Nevertheless, following a single procedure, the success rate was 95.6% (22/23) in the ER group and 60% (6/10) in the RF group. Notably, complete numbness was the most significant side effect, with a higher incidence in the ER group (30.4%) compared to the RF group (0%) (p = 0.02). The recurrence rate was statistically different (p = 0.01) between the two groups, with 4.4% and 40% recorded in the ER and RF groups, respectively.
Conclusion
We demonstrated the usefulness of our refined ER procedure as a safe, cost-effective, and efficient second-line treatment for TN.
Keywords: Trigeminal neuralgia, Rhizotomy, Rhizolysis, Ethanol, Radiofrequency
1. Introduction
Trigeminal neuralgia (TN), also called tic douloureux [1], is a chronic pain condition that specifically affects the 5th cranial nerve. The condition is characterized by extreme, sporadic, sudden burning or shock-like facial pain that lasts a few seconds to several minutes per episode. This condition is described as one of the most painful conditions humans can experience [2] with an estimated annual incidence of new cases standing at 12 per 100,000 individuals [3].
The first line of treatment for TN typically involves pharmaceutical interventions with analgesic and/or anti-epileptic medications. However, the diminishing efficacy of these drugs and the emergence of drug-related side effects over time necessitate alternative pain relief procedures for approximately half of the patients [4]. Patients who fail the first line of medical treatment may benefit from percutaneous intervention, including balloon compression (BC), chemical rhizotomy (CR), and radiofrequency thermocoagulation (RF) [5].
The initial application of RF for treating TN encountered challenges primarily related to electrode design and procedural complications. It was not until 1974, when Sweet and Wepsic [6] introduced an improved electrode design and described their method for selectively ablating trigeminal rootlets, that this technique garnered widespread acceptance as an effective approach for TN management.
The discovery of chemical rhizotomy as a method to reduce trigeminal pain was serendipitously in 1981 when Hakanson [7] and colleagues were attempting to inject glycerol mixed with tantalum into the trigeminal cave to prepare the target for the radiation in the TN treatment. Ethanol had been used even earlier [8], in 1910, when Harris pioneered the injection of ethanol into the trigeminal cave, and subsequently, in 1914, Hartel described a method to access the foramen ovale [9]. However, conventional ethanol rhizotomy (ER) was found to be less effective than glycerol rhizotomy (GR) for TN treatment, making GR a preferred method. Leveraging the cost-effectiveness and ready availability of ethanol, we have further improved the ethanol rhizotomy procedure for TN treatment, yielding promising outcomes. In this study, we retrospectively analyzed a single-center experience of 33 patients with typical TN, 10 of whom had RF and 23 had ER under Digital Subtraction Angiography (DSA) guidance and compared the pain relief and durability outcomes between the two procedures.
2. Methods
2.1. Patient selection
This study received Ethics Committee approval with document number 22/HMUIRD, and consent was obtained from all the participants.
We conducted a retrospective descriptive study involving 33 patients diagnosed with typical trigeminal neuralgia between 2012 and 2014, who underwent either radiofrequency (RF) treatment (n = 10) or newly developed ethanol rhizotomy (ER) (n = 23) and were followed up for a minimum of six years.
The typical trigeminal neuralgia is characterized by sudden, electric shock-like pain on one side of the face, lasting for a few seconds to minutes, with pain-free periods between episodes. The pain often comes from triggers such as wind, face washing, teeth brushing, eating, or talking. All patients had received the treatment with anticonvulsant medicaments until the pain became intolerable, at this point, intervention was considered. Patients having indications for percutaneous intervention are divided into two groups by the patient's decision after receiving a full explanation about the advantages and inconveniences of each method: RF or ER.
2.2. Radiofrequency thermocoagulation (RF) procedure
RF procedure was standardized and performed under fluoroscopy guidance with the NeuroTherm generator version NT1100. The patient was placed supine with a neck roll to ensure the extension. The submental fluoroscopy view was shown to visualize the foramen ovale. No medicament was required. We explained to the patients that they may experience sudden pain upon needle insertion into the foramen ovale. The patient was also asked to describe the territories affected during stimulation. A 21gauge RF needles with a 5 mm active tip length was employed with the Neurotherm RF cannula (RF-SE-10-CE). The insertion point was 1.5 cm laterally from the mouth corner, and the trajectory of Hartel was followed to 0.5 cm below the middle point of the lower eyelid and 1 cm in front of the tragus [10]. The insertion of the needle to the foramen ovale was felt by the doctor or by the triggering pain of the patient. The needle tip's position through the foramen ovale was verified by fluoroscopy in submental and lateral views. The needle was advanced until its tip reached the midpoint between the superior and inferior borders of the petrous bone. The obturator was then removed, and the electrode was inserted inside the needle. The sensory test was done with frequency at 50Hz, 1.0 ms, and voltage gradually increasing from 0. If the patient showed no sensory change at 5 volts, or the territory did not correspond to the painful zone, the needle advanced 5 mm, and the sensory test was done again in a new position. The ideal needle position was confirmed if the patient felt the sensory change at lower than 1 volt in the habitual painful territory. The electrode was removed to inject 0.2 ml of a local anesthetic agent through that needle, and then the electrode was re-inserted. The burning phase was done automatically with a target of 80 °C for 90 s. Patients can be discharged the same day or observed in the hospital for one night. If the pain persisted the next day, the procedure would be repeated using the same protocol, and the pain relief would be recorded as the final result of the intervention the next day.
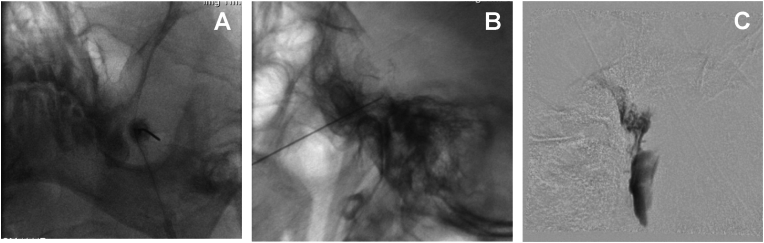
2.3. Ethanol rhizotomy (ER) procedure
Patient setting and needle insertion were similar to those in RF. A spinal 25 Gauge needle (Spinocan) was used. After inserting the needle through the foramen ovale, a sequence of subtraction angiography was performed with a frame rate of 1f/s to verify that the needle tip was in the Meckel's cave without vascular leakage. The high-quality subtraction images allowed visualization of Meckel's cave, the Gasserian ganglion, and the trigeminal canal. Different patterns may arise, indicating that the needle tip is not within Meckel's cave. The needle should be repositioned until achieving opacification of Meckel's cave on DSA. 0.2 ml of local anesthetic agent (Lidocaine 2%) was injected. One minute later, a clinical examination was done on the DSA table to confirm the achievement of numbness on the ipsilateral half-face. Then, 0.3 ml of absolute ethanol was slowly injected. The needle was removed after the injection. The patient was maintained in a supine position for a minimum of 10 min following the injection of ethanol. Pain relief was evaluated 3 h after intervention. Clinical assessment of masseter weakness was conducted by placing thumbs above the mandibular corners and instructing patients to chatter. The patient was discharged the same day or the next day after being examined by the treating doctor and an experienced ophthalmologist.
During the study period, only two operators carried out both of these techniques. The protocol has been established and standardized to ensure the quality of procedures and their reproducibility. Those procedures were standardized and performed by one of two experienced doctors.
2.4. Follow-up and data collection
Outpatient records and telephone interviews were used to assess the outcomes of RF and ER interventions in the patient cohort. The pain relief was evaluated right after the procedure and at 24 h after. If the pain persisted with the same or increased intensity after 24 h, we repeated the additional intervention. This repeated procedure was documented, and the pain relief evaluated 24 h after the first intervention was considered the initial outcome.
A structured report, featuring a set of simple basic questions, was employed to document pain characteristics. This structured reporting system enabled us to gather data as if conducting a prospective study. In the event that any data was omitted in the medical report, we obtained detailed information through telephone inquiries.
The clinical exam post-intervention recorded the pain relief, numbness territories, masseter weakness, and corneal reflex and included consultation by an experienced ophthalmologist. The patients were asked to see the doctor two weeks after treatment and to call back if the pain recurred. A telephone interview was done at 6 years post-intervention to collect recurrence and numbness duration data.
2.5. Statistical analysis
The data collected from 33 patients was analyzed using RStudio version 1.4.1106. The χ2 test or Fisher's exact test was used for the comparison of efficacy as well as the complications of the two protocols. The recurrent cases were noted when the patients returned for pain consultation or by the periodic telephone survey. Kaplan Meier curves were plotted for the time to recurrence of TN requiring further treatment after the intervention.
3. Results
From June 2012 to September 2014, 33 patients with TN underwent either RF or ER. All patients had a long treatment history, ultimately leading to the failure of the conservative method, prompting the consideration of an intervention. Patients had suffered from TN for a median duration of 6 years and followed up at least 6 years.
3.1. Baseline characteristics of patients
Baseline demographics and clinical characteristics of the TN patients are described in Table 1. The mean age was 68 ± 16 in the RF group and 64 ± 10 in the ER group, with no statistically significant difference (p = 0.353). The most affected single trigeminal division was V2, while V1 was the least affected, accounting for only 6% of cases. In most cases (45.5%), patients had at least two divisions affected. There were no significant differences between the RF and ER groups in terms of the painful division subgroups, as determined by χ2 or Fisher's exact test (p = 0.22) in cases where at least two branches were affected. Among the patients, ten underwent RF treatment, while 23 received ER. All patients presented with typical TN and met the criteria for intervention. However, it's worth noting that only ten patients opted for RF due to its higher cost compared to ER.
Table 1.
Demographics data and clinical characteristics of patients treated with RF or ER.
| Overall | ER | RF | p | test | |
|---|---|---|---|---|---|
| n | 33 | 23 | 10 | ||
| Age (mean (SD)) | 65.39 (12.46) | 64.04 (10.28) | 68.50 (16.69) | 0.353 | |
| Sex (%) | |||||
| Male | 22 (66.7) | 17 (73.9) | 5 (50.0) | 0.349 | |
| Female | 11 (33.3) | 6 (26.1) | 5 (50.0) | ||
| Pain Suffering time (median [IQR]) | 6.00 [5.00, 10.00] | 6.00 [5.00, 10.00] | 5.00 [2.50, 8.75] | 0.226 | nonnorm |
| Pain Side (%) | |||||
| Right | 20 (60.6) | 14 (60.9) | 6 (60.0) | 1 | |
| Left | 13 (39.4) | 9 (39.1) | 4 (40.0) | ||
| Pain Division (%) | |||||
| 2,3 Divisions | 15 (45.5) | 11 (47.8) | 4 (40.0) | 0.22 | |
| V1 (ophthalmic) | 2 (6.1) | 1 (4.3) | 1 (10.0) | ||
| V2 (maxillary) | 9 (27.3) | 8 (34.8) | 1 (10.0) | ||
| V3 (mandibular) | 7 (21.2) | 3 (13.0) | 4 (40.0) | ||
3.2. Initial pain relief
Pain relief was assessed the day following the intervention. In cases where the pain persisted with the same or increased intensity, a subsequent intervention was administered with the same protocol, and the result was validated the following day. Ultimately, all patients achieved pain relief. Complete pain relief was observed in 95.7% (20/23) of patients in the ER group compared with 60% (6/10) of patients in the RF group (Table 2). Four patients (40%) in the RF group required a second intervention, whereas this rate was significantly lower (4.3%) in the ER group (p = 0.005). In the RF group, four patients experienced burning hyperalgesia 3 h post-intervention, coinciding with the dissipation of local anesthesia (Table 2).
Table 2.
Pain post 1st intervention.
| ER | RF | p | |
|---|---|---|---|
| n | 23 | 10 | |
| Complete pain relief | 22 (95.7) | 6 (60.0) | 0.005 |
| Unchanged Pain | 1 (4.3) | 0 (0.0) | |
| Pain Increased required intervention | 0 (0.0) | 4 (40.0) |
3.3. Complications
The most frequent complication observed in this study was numbness, categorized as complete or partial (Table 3). In the ER group, complete and partial numbness was reported in 30.4% and 69.6% of patients, respectively. None of the patients in the RF group experienced complete numbness, while partial numbness was observed in 80% of the patients. Statistical analysis showed a significant difference between the two groups (p = 0.02).
Table 3.
Complications.
| ER | RF | p | |
|---|---|---|---|
| Total number | 23 | 10 | |
| Sensory loose | |||
| Complete numbness | 7 (30.4) | 0 (0.0) | 0.021 |
| Partial numbness | 16 (69.6) | 8 (80.0) | |
| Normal sensory | 0 (0.0) | 2 (20.0) | |
| Dysanesthesia | |||
| No dysanesthesia | 19 (82.6) | 5 (50.0) | 0.132 |
| Dysanesthesia | 4 (17.4) | 5 (50.0) | |
| Corneal reflex | |||
| Normal corneal reflex | 12 (52.2) | 10 (100.0) | 0.028 |
| Partial corneal reflex loose | 9 (39.1) | 0 (0.0) | |
| Complete corneal reflex loose | 2 (8.7) | 0 (0.0) | |
| Herpes simplex | |||
| 1 division | 3 (13.0) | 3 (30.0) | |
| 2 + 3 division | 1 (4.3) | 1 (10.0) | |
| No Herpes | 19 (82.6) | 6 (60.0) | |
| Masseter weakness | |||
| Normal | 1 (4.3) | 1 (10.0) | 1 |
| Weakness | 22 (95.7) | 9 (90.0) | |
| Pain recurrence | |||
| No recurrence after 7 years | 19 (82.6) | 6 (60.0) | 0.342 |
| Recurrence | 4 (17.4) | 4 (40.0) | |
| Time to recurrence (years) | 3.00 (1.87) | 2.25 (0.96) | 0.493 |
Among the subset of patients who reported numbness, 60% experienced numbness in only one division, and 40% had numbness in two divisions in the RF group. In the ER group, 25% and 75% of the patients experienced numbness in one and at least two divisions, respectively (Table 4).
Table 4.
Numbness division affected.
| Division |
ER |
RF |
|---|---|---|
| 4 | 5 | |
| V1 | 0 (0.0) | 0 (0.0) |
| V2 | 1 (25.0) | 2 (40.0) |
| V3 | 0 (0.0) | 1 (20.0) |
| V1+V2 | 0 (0.0) | 0 (0.0) |
| V1+V3 | 0 (0.0) | 1 (20.0) |
| V2+V3 | 1 (25.0) | 1 (20.0) |
| V1+V2+V3 | 2 (50.0) | 0 (0.0) |
The study identified complete or partial loss of corneal reflex in 47.8% (11/23) of the patients in the ER group. This complication was absent in the RF group, making a significant difference between the two groups with p = 0.028.
Motor function was also affected in both groups. Masseter weakness was detected in 95.7% of patients in the ER group and 90% in the RF group, with no significant difference observed (p = 1).
3.4. Recurrence of pain
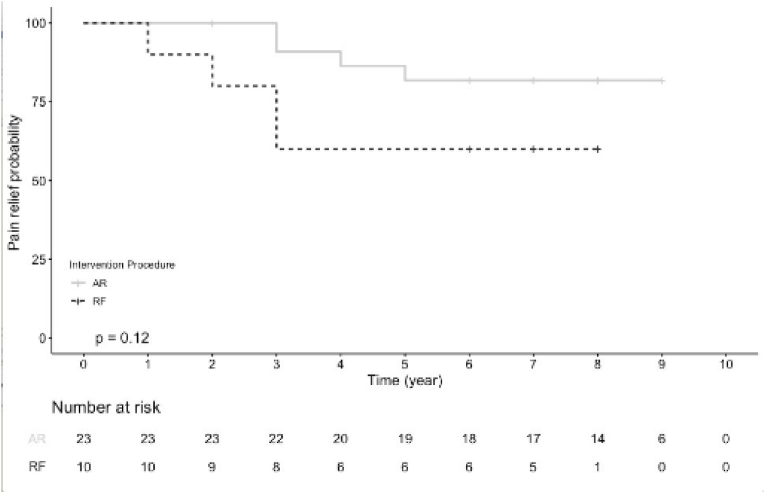
The recurrence rates after the first injection for the ER and RF groups were compared using Kaplan-Meier analysis (Fig. 1). The follow-up duration was extended for a minimum of six years, with the overall complications presented in Table 3. The recurrence rates for the ER and RF groups were 17.4% and 40%, respectively; however, this disparity was statistically insignificant (p = 0.342). Although the ER curve appeared to be positioned above the RF curve, the statistical analysis revealed no significant difference (p = 0.12) (log-rank test). It's worth noting that the number of recurrent cases remained limited, preventing the determination of a median time to recurrence (see Fig. 2).
Fig. 1.
Pain recurrence.
Fig. 2.
Needle inserted through the foramen ovale. A: Submental view. B: Lateral view. C: Meckel's cave and trigeminal canal on DSA.
4. Discussion
In this retrospective study of a single-center cohort of 33 TN patients who failed the first line of medical treatment. In our hospital, these patients are presented with three treatment options, one of them being Microvascular Decompression (MVD), typically conducted by neurosurgeons. Surgeons often regard MVD as a high-risk procedure, leading them to recommend percutaneous intervention, consequently, this study cohort exhibited a mean age of 65, with the oldest patient being 92. This aspect also underscores the advantages of percutaneous intervention over surgery, even in the face of significant advancements in surgical techniques today.
Percutaneous chemodenervation, employing glycerol, phenol, or alcohol, has been described as a potential procedure for managing TN. Glycerol is currently the preferred chemodenervating agent due to its high efficacy. Most previous studies have found that glycerol rhizotomy (GR) achieves initial pain relief in 70 to greater than 90% of patients with TN [11]. While ethanol may not directly penetrate the Gasserian ganglion, it effectively envelops the ganglion within Meckel's cave and the trigeminal root canal. Consequently, the effectiveness of ethanol may not result from nerve structure destruction but rather from alterations in the surrounding structures of the ganglion and trigeminal nerve [10,12]. Similarly reported by surgeons, when there was no visible vascular conflict during surgery, only rubbing the nerve could alleviate trigeminal pain [12]. In our protocol, all injections were administered with the patient in the supine position. This positioning ensures that Meckel's cave and the trigeminal canal are oriented upwards, with Meckel's cave situated at the highest point. Ethanol, being less dense than cerebrospinal fluid, naturally flows to cover the upper portions of these adjoining structures that contain cerebrospinal fluid. Our unique protocol includes the gradual injection of ethanol into Meckel's cave while the patient is in a supine position, a distinctive approach that, to the best of our knowledge, has not been previously documented in the literature for percutaneous interventions in the treatment of trigeminal neuralgia.
Unexpectedly, our study noted pain relief in only 6 patients (60%) in the RF group, which contrasts with previous studies reporting success rates ranging from 80% to 100% [13]. The lower success rate observed in the RF group might be attributed to the fact that these patients had already failed first-line treatments and the relatively small sample size of our cohort.
Taken together, pain relief was attained through both RF and ER in our study, albeit possibly through distinct mechanisms [12]. RF ablates nerve structures through localized heating, thereby reducing pain [12]. However, our results reinforce the usefulness of ER as a cost-effective and efficient second-line treatment of TN.
Several studies have recorded a broad spectrum of recurrence rates after GR and RF procedures. For instance, between 34% and 83% of the patients may experience pain recurrence within 5 years after the GR procedure [13]. In this study, we observed pain recurrence within 7 years in only 17.4% of the patients following ER. We noted a recurrence rate of 40% within 7 years in the RF group, which is relatively high in comparison to previous studies [11]. While ER exhibited lower pain recurrence rates in our study, suggesting potentially superior long-term pain management outcomes, this observation wasn't statistically significant. More extensive studies with larger sample sizes are necessary to evaluate the pain recurrence rates.
During RF, precise placement of the needle's probe into the corresponding branch is challenging, especially for the first division, as revealed by the sensory test. Although the initial aim was to target only a specific area of ganglion nerve tissues, heat induced by radiofrequency ablation might affect various branches of the Gasserian ganglion, leading to diverse side effects encompassing sensory and motor functions (Table 4). Continuous refinement of electrodes did not produce better outcomes as expected [9]. Meanwhile, during ER, the divisional difference is not a critical factor as ethanol envelopes the entire ganglion and trigeminal root.
Notably, in the RF group, four patients experienced intense pain post-procedure after a delay of 3 h. They required additional intervention, which could be attributed to the irritating effects of RF on the non-ablated part of the trigeminal ganglion. Noorani also described a case of anesthesia dolorosa following RF [5].
Both ER and RF procedures are safe, although we observed several common complications, including numbness, dysaesthesia, masseter weakness, reduced corneal reflex, Herpes simplex. Numbness was more frequently observed in the ER group than in the RF group, and this difference was statistically significant. It's important to note that numbness induced by ethanol could be recovered, but we do not have sufficient data to illustrate the recovery of this sensory function. Most authors have reported sensory restoration after rhizotomy, emphasizing the importance of protecting nerve structures when choosing treatment methods. On the other hand, a reduction in corneal reflex appeared to be more pronounced in the ER group. This could be attributed to the vulnerability of small nerve fibers, which are more easily damaged by ethanol compared to BC and RF methods [5].
Collectively, we demonstrated that our refined ER procedure is not only safe and efficient but also cost-effective for the treatment of TN. This is especially crucial since cost considerations are of utmost importance for many patients, particularly in developing countries.
Limitations: This study, being retrospective, may have inherent biases, especially with a limited sample size. The variation in the size of these two groups could influence the analysis, which is regarded as a drawback of this retrospective study design.
5. Conclusion
With the correct technique, ER offers distinct advantages in the treatment of trigeminal neuralgia and also sheds light on the pathology's mechanism and potential treatment approaches. RF is another effective treatment method, albeit at a higher cost. However, the presence of certain complications associated with these methods highlights the need for further improvements in treating this condition to enhance patients' quality of life.
Declaration of competing interest
All the authors have read and concur with the current version of the manuscript. The material submitted for publication has not been previously reported and is not under consideration for publication elsewhere. The authors declare no conflicting financial interest.
References
- 1.Shankar Kikkeri N., Nagalli S. StatPearls. Treasure Island (FL) StatPearls Publishing; 2023. Trigeminal neuralgia. [Google Scholar]
- 2.Trigeminal neuralgia – causes, symptoms and treatments. https://www.aans.org/ available from:
- 3.National institute of neurological disorders and stroke. https://www.ninds.nih.gov/health-information/disorders/trigeminal-neuralgia Trigeminal Neuralgia.
- 4.Missios S., Mohammadi A.M., Barnett G.H. Percutaneous treatments for trigeminal neuralgia. Neurosurg Clin. 2014 Oct;25(4):751–762. doi: 10.1016/j.nec.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 5.Noorani I., Lodge A., Vajramani G., Sparrow O. Comparing percutaneous treatments of trigeminal neuralgia: 19 Years of experience in a single centre. Stereotact Funct Neurosurg. 2016 Apr 13;94(2):75–85. doi: 10.1159/000445077. [DOI] [PubMed] [Google Scholar]
- 6.Sweet W.H., Wepsic J.G. Controlled thermocoagulation of trigeminal ganglion and rootlets for differential destruction of pain fibers: Part 1: trigeminal neuralgia. J Neurosurg. 1974 Feb 1;40(2):143–156. doi: 10.3171/jns.1974.40.2.0143. [DOI] [PubMed] [Google Scholar]
- 7.Håkanson S. Trigeminal neuralgia treated by the injection of glycerol into the trigeminal cistern. Neurosurgery. 1981 Dec;9(6):638–646. doi: 10.1227/00006123-198112000-00005. https://doi:10.1227/00006123-198112000-00005 [DOI] [PubMed] [Google Scholar]
- 8.Wang J.Y., Bender M.T., Bettegowda C. Percutaneous procedures for the treatment of trigeminal neuralgia. Neurosurg Clin. 2016 Jul;27(3):277–295. doi: 10.1016/j.nec.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 9.Skirving D.J., Dan N.G. A 20-year review of percutaneous balloon compression of the trigeminal ganglion. J Neurosurg. 2001 Jun;94(6):913–917. doi: 10.3171/jns.2001.94.6.0913. [DOI] [PubMed] [Google Scholar]
- 10.Alvernia J.E., Sindou M.P., Dang N.D., Maley J.H., Mertens P. Percutaneous approach to the foramen ovale: an anatomical study of the extracranial trajectory with the incorrect trajectories to be avoided. Acta Neurochir. 2010 Jun;152(6):1043–1053. doi: 10.1007/s00701-010-0604-y. [DOI] [PubMed] [Google Scholar]
- 11.Texakalidis P., Xenos D., Tora M.S., Wetzel J.S., Boulis N.M. Comparative safety and efficacy of percutaneous approaches for the treatment of trigeminal neuralgia: a systematic review and meta-analysis. Clin Neurol Neurosurg. 2019 Jul;182:112–122. doi: 10.1016/j.clineuro.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 12.Moraci A., Buonaiuto C., Punzo A., Parlato C., Amalfi R. Trigeminal neuralgia treated by percutaneous thermocoagulation. Comparative analysis of percutaneous thermocoagulation and other surgical procedures. Neurochirurgia. 1992 Mar;35(2):48–53. doi: 10.1055/s-2008-1052245. https://doi:10.1055/s-2008-1052245 [DOI] [PubMed] [Google Scholar]
- 13.Udupi B.P., Chouhan R.S., Dash H.H., Bithal P.K., Prabhakar H. Comparative evaluation of percutaneous retrogasserian glycerol rhizolysis and radiofrequency thermocoagulation techniques in the management of trigeminal neuralgia. Neurosurgery. 2012 Feb;70(2):407–412. doi: 10.1227/NEU.0b013e318233a85f. https://doi:10.1227/NEU.0b013e318233a85f discussion 412-413. [DOI] [PubMed] [Google Scholar]