Abstract
Background
Fluoroscopy guided interventions are widely used procedures in the treatment of musculoskeletal conditions. Understanding the movement of the needle is part of a resident's initial training when performing these procedures. Needle navigation training is largely gained with fluoroscopy.
Objective
The purpose of this study is to determine whether the use of ultrasound training can lead to a decrease in time to reach a target under fluoroscopy.
Methods
32 medical students or residents. Exposure of one group of trainees to a practice session of needle navigation using ultrasound. The control group did not participate in ultrasound training. Time to reach the target during a fluoroscopy guided needle navigation test was measured in both groups.
Results
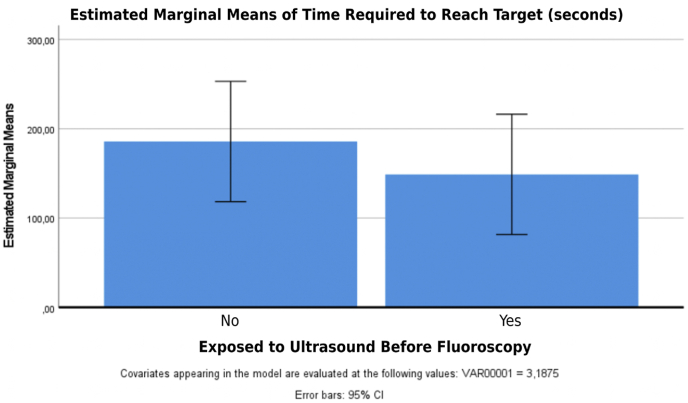
The mean time to reach the target under fluoroscopy of the students unexposed to an ultrasound training (group 1 control group) was 183 s (standard deviation = 160 s), while that after ultrasound training (group 2 experimental group) was 150,81 s (standard deviation = 96 s) (p = 0,483)
Conclusion
Fluoroscopy needle navigation training was not improved by a 1-h group practice session with in-plane ultrasound needle navigation practice. Further studies need to be done with exposure for residents to a group practice session longer than 1-h
Keywords: Ultrasound, Injection, Fluoroscopy, Education, Medical teaching, Resident education
1. Introduction
Fluoroscopy guided interventions are widely used procedures in the treatment of musculoskeletal conditions, especially painful spinal pathologies. Fluoroscopically guided interventions expose patients as well as the health care team to ionizing radiation. The physician is responsible for the dose of radiation produced during a procedure and the exposure time depends on his technique. Several studies have already demonstrated that formal training prior to the use of fluoroscopy reduces radiation time [1] by reducing unnecessary steps and reducing procedure time.
Understanding the movement of the needle is part of a resident's initial training when performing these procedures. Fluoroscopy allows the physician to observe the needle trajectory in real time and allows them to triangulate the needle tip position with orthogonal and complementary views. The needle is in the most axial view possible (parallel to x-ray beam) on initial needle driving and the use of serial images or briefly continuous images allows for a live view of the needle as it progresses towards the target. The majority of the initial needle navigation is performed in a pin-point or hub-view under fluoroscopic guidance and achieving this and maintaining this during needle advancement is a crucial initial step in learning fluoroscopy guided procedures.
Proper utilization of a spinal needle in fluoroscopy can be divided into two steps: the initial positioning of the needle coaxially parallel to x-ray beam (initial hub-view) followed by subsequent needle driving or advancement stage to reach the target.
A normal spinal needle has a bevel that impacts the needle's trajectory when advancing through soft tissues. The needle has a natural tendency to bend slightly away from the bevel [2]. In addition, the effect of the bevel can be accentuated in certain clinical situations to circumvent anatomical structures and this therefore generates a greater displacement outside the axis of the needle. This concept must be understood by residents in order to plan the three-dimensional movements of their needles. Acquiring the skill to control a curved needle is a fundamental competency for these procedures.
Currently, the skill of needle navigation is largely gained by practicing with fluoroscopy with the direct supervision of a staff physician, directly on patients unless expensive phantom models are readily available. This requires use of a fluoroscopy machine and room, a radiology technician, lead protective equipment and exposure to radiation. However, it is interesting to wonder if part of the learning of needle navigation could be completed under ultrasound. Ultrasound has the advantage of no radiation and increases the confidence of the resident practicing under fluoroscopy. Equally important, patients would be less subject to technical errors of a novice resident and benefit from a more comfortable, shorter intervention.
Research has already demonstrated that simulated learning of deliberate ultrasound needle insertion improved ultrasound guided injection [[3], [4], [5]]. Other studies also demonstrated that needle navigation training under fluoroscopic simulation translates into practical improvement of real life needle navigation in fluoroscopy guided procedures [6,7]. No known studies have evaluated the potential for ultrasound needle navigation practice to translate into an improvement in performance in fluoroscopic needle navigation.
Clinical experience shows that a reduction in the time required for the same technique to reach a target in fluoroscopy correlates with better patient comfort. Our team has identified four major advantages of ultrasound over fluoroscopy in the context of residency training. First, it does not require a technologist and can be operated entirely by one person, reducing the resources needed to learn needle navigation. Second, it offers a real-time image of the needle, specifically a curved needle, with optimal visualization parallel to the needle. Third, it does not produce radiation. Finally, the ultrasound machine is more accessible in most academic centers. If the hypothesis is confirmed, this training can be reproduced with minimal resources to help residents acquire better needle navigations under fluoroscopy and understand the mechanics of a curved spinal needle as it progresses through tissue. That would be a solution for simple and profitable learning
The purpose of this study is to determine whether the use of ultrasound training can lead to a decrease in time to reach a target under fluoroscopy. If this study is successful, it could be reproduced in a “boot camp” format given by senior residents to junior residents in order to improve their needle handling technique. Therefore, any resident interested in learning fluoroscopy could benefit from practice under ultrasound. This could imply that exposure to ultrasound during residency would be relevant for a resident seeking subspecialization in needle manipulation under fluoroscopy.
2. Methods
Data and survey collection for this project was performed with ethical committee review approval from the Centre hospitalier de l’Université de Montréal (CHUM). Written consent was obtained from all residents and medical student trainees who participated in this study.
The objective was to expose one group of trainees to a practice session of needle navigation using ultrasound (group 2 experimental) and no ultrasound training to the control group (group 1). Both groups were then exposed to a fluoroscopy guided needle navigation test.
-
●
Material
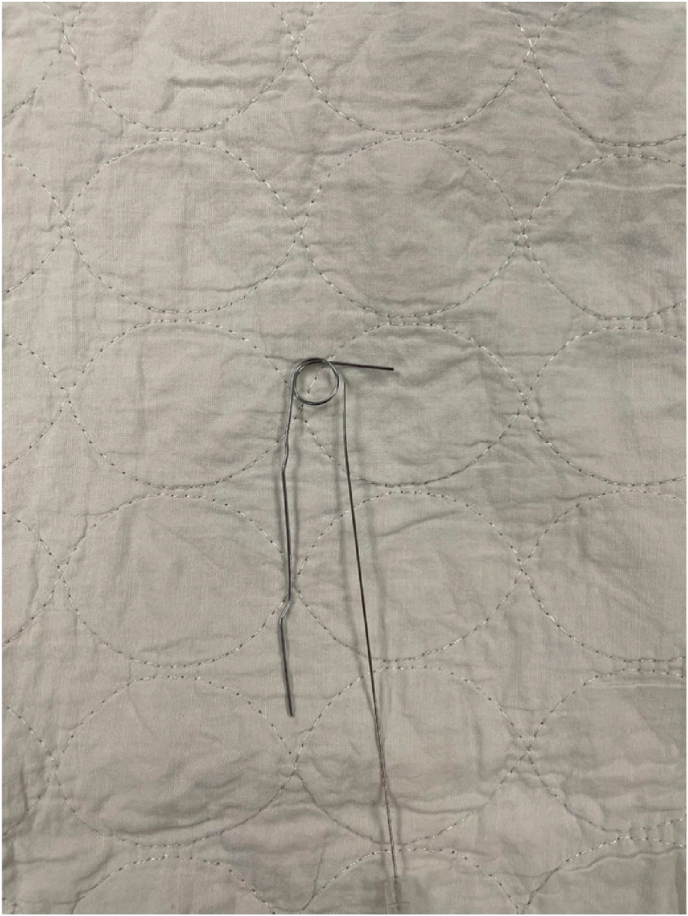
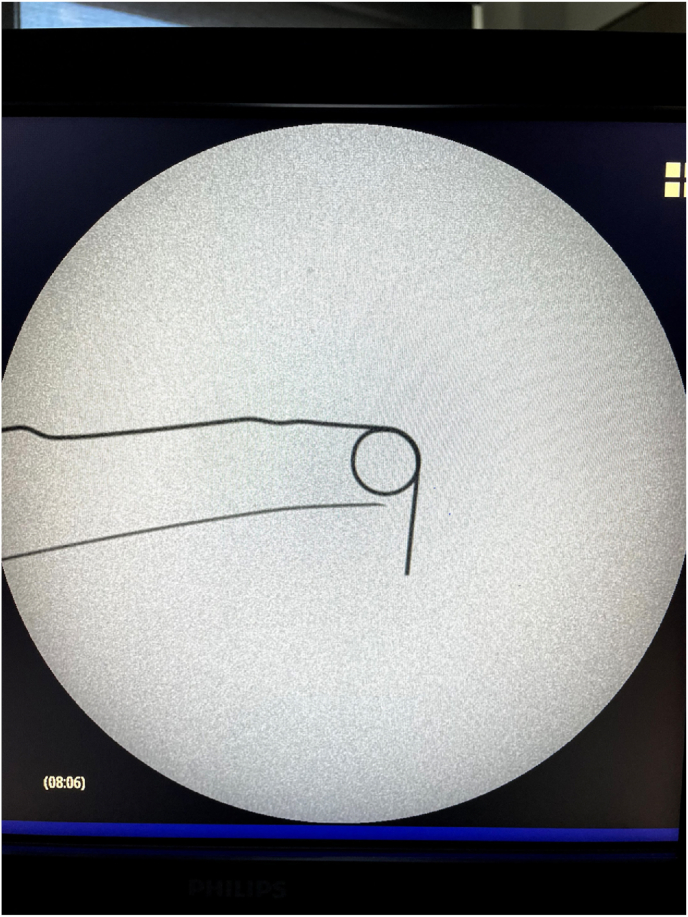
A 1 cm in diameter target was inserted on a pig's femur. The target rested on the bone at a depth of 15 cm from the surface of the pig's skin. The fluoroscopy beam was placed perpendicular to the target and the target was centered on the image shown on the screen. Each participant had their own spine needle bent at approximately five degrees towards the bevel as commonly seen in a clinical context (See Fig. 1, Fig. 2, Fig. 3, Fig. 4).
Fig. 1.
An image of a spinal needle next to the metal coil representing the target before it is inserted over the bone.
Fig. 2.
An image of a spinal needle next to the metal coil representing the target before it is inserted over the bone, as it will be viewed on fluoroscopy imaging.
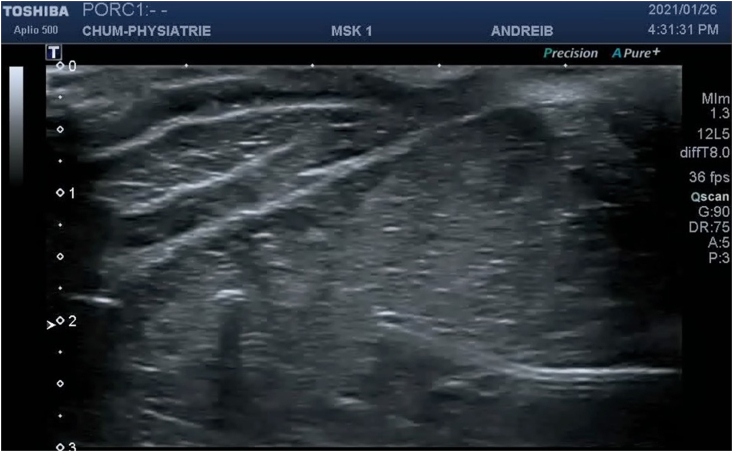
Fig. 3.
An image of the pig's muscle, fluoroscopic beam and captor next to the guiding screen as it was used with the participants.
Fig. 4.
An image of the ultrasound visualisation of a curved needle advancing through muscle tissue as it was used in this experiment.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.inpm.2022.100169
The following is/are the supplementary data related to this article:
-
●
Study participants
All Quebec medical resident physicians and medical students who have not significantly been exposed to ultrasound or fluoroscopy training represent our sample for population. We excluded any student or resident who had already had significant prior training with needle manipulation under ultrasound or fluoroscopy. A training was considered significant if there were more than 30 total prior injections done by the participants. Prior to any measure of data, each participant was asked to complete a survey assessing their prior use of needle guided procedures, age, year of medical training and comfort with a needle. The results of the survey were compared between the two groups to confirm proper randomization of the groups. The 32 participants were randomly separated into two groups, Group 1 and 2.
-
●
Study protocol
Both groups were shown a PowerPoint presentation explaining theoretical concepts required for proper needle driving at the beginning of the study. The PowerPoint presentation explained the theoretical concepts required for proper needle driving in both ultrasound and fluoroscopy needle injections. All study participants were then randomly assigned to either the control or experimental group.
The control group (group 1) were randomly selected from the participants and did not participate in a 1 h, hands-on, ultrasound training. This group attempted to attain the target under fluoroscopy without the prior practical training under ultrasound. The control group's lack of ultrasound training prior to the fluoroscopic procedure is meant to simulate the current curriculum of physiatry residents.
The experimental group (group 2) had a 1 h group training, supervised by senior physiatry residents and staff physiatrist with a fellowship in spinal interventions. The training was dedicated to the deliberate practice of needle manipulation. During this session, a live demonstration using ultrasound was used to show advancement of a curved spinal needle through a pig leg. All possible movements were demonstrated, including advancement, retraction, change of needle bevel direction and needle redirection. Participants were then given the opportunity, while being supervised, to manipulate the same curved needle that will be used during the fluoroscopy procedure. They were able to appreciate under live ultrasound, while manipulating the curved needle, the directional change in trajectory of the needle due to the curvature and how to adjust it. Each participant had equivalent hands-on training as a rotation system was implemented for everyone to have an equal amount of practice opportunities. The supervisor spent about 5 min for his initial demonstration, the remainder of the time was spent by the participants for hands-on practice. Each participant spent a minimum of 30 min practicing as we utilized all the four available machines in the clinic.
During the assessment phase of needle navigation using fluoroscopy, participants had only one instruction: “the needle tip must hit the target of the pig's leg within the circle (as demonstrated above)". No more teaching than the previous theoretical session was given to either group. Any improvement perceived during the fluoroscopy session should therefore be secondary to practice under ultrasound.
-
●
Evaluation
Grading the performance of the procedure was made by measuring the time to reach the target in fluoroscopy on the pig leg. The stopwatch was started as soon as the needle touched the skin of the pig and was stopped as soon as the radiopaque target was reached. Confirmation that the target has been reached was verified by the head physician supervising the session. The time to reach the target is directly correlated with the total radiation. No hints or help was given to the participant during the fluoroscopy needle navigation prior to or during the measurement.
-
●
Statistical analysis
It was determined that with a sample of 20 participants and a standard deviation of 10 s, it is possible to detect a difference of 16.4 s between the two groups with a power of 80% and an alpha of 1.25%. Prior to meeting with our statistician, we conducted a pilot trial time-to-target test with a senior staff, a senior resident and a junior resident. Each person did 3 runs of a similar test used in the study, and their times were averaged. This was the sample data used to determine likely variation in our study sample as well to determine the 16.4 s threshold.
The paired sample t-test was used in the comparison of results before and after training, and p < 0.05 was considered to be significant. In total, 32 medical students participated. The average age of the students was 23.09 (standard deviation = 2.68), and 62.5% (n = 20) of the students were female.
3. Results
There was no participant drop out. Our study did not demonstrate any statistically significant difference in the mean time required to reach the target for both groups. The mean time to reach the target under fluoroscopy of the students unexposed to an ultrasound training (group 1 control group) was 183.94 s (standard deviation = 159.84 s), while that after ultrasound training (group 2 experimental group) was 150.81 s (standard deviation = 95.80 s) (p = 0.483; Table 1). Further evaluation between the subgroups (age, sex, level of training) also did not demonstrate any statistically significant difference.
Table 1.
Study participant's demographic data.
| Group |
P value | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | Total | ||||
| Gender | Female | N | 10 | 10 | 20 | 1.000 |
| % | 62.5% | 62.5% | 62.5% | |||
| Male | N | 6 | 6 | 12 | ||
| % | 37.5% | 37.5% | 37.5% | |||
| Which year of medicine are you in? | 1 | N | 4 | 3 | 7 | 0.002 |
| % | 25.0% | 18.8% | 21.9% | |||
| 2 | N | 0 | 4 | 4 | ||
| % | 0.0% | 25.0% | 12.5% | |||
| 3 | N | 8 | 0 | 8 | ||
| % | 50.0% | 0.0% | 25.0% | |||
| 4 | N | 2 | 5 | 7 | ||
| % | 12.5% | 31.3% | 21.9% | |||
| PGY-1 | N | 0 | 2 | 2 | ||
| % | 0.0% | 12.5% | 6.3% | |||
| PGY-2 | N | 1 | 2 | 3 | ||
| % | 6.3% | 12.5% | 9.4% | |||
| PGY-3 | N | 1 | 0 | 1 | ||
| % | 6.3% | 0.0% | 3.1% | |||
| How many needle infiltrations have you done? | 0 | N | 9 | 8 | 17 | 0.481 |
| % | 56.3% | 50.0% | 53.1% | |||
| 1–5 | N | 7 | 5 | 12 | ||
| % | 43.8% | 31.3% | 37.5% | |||
| 10–15 | N | 0 | 1 | 1 | ||
| % | 0.0% | 6.3% | 3.1% | |||
| 5–10 | N | 0 | 2 | 2 | ||
| % | 0.0% | 12.5% | 6.3% | |||
| Age | N | 16 | 16 | 32 | ||
| Mean | 22.38 | 23.81 | 23.09 | 0.131 | ||
| Standard Deviation | 1.96 | 3.15 | 2.68 | |||
| Minimum | 19.00 | 19.00 | 19.00 | |||
| Maximum | 26.00 | 30.00 | 30.00 | |||
| On a scale of 1–5, how comfortable are you with a needle, if 1 is very uncomfortable and 5 is extremely comfortable. | N | 16 | 16 | 32 | ||
| Mean | 2.94 | 3.06 | 3.00 | 0.716 | ||
| Standard Deviation | 1.06 | .93 | .98 | |||
| Minimum | 1.00 | 1.00 | 1.00 | |||
| Maximum | 5.00 | 5.00 | 5.00 | |||
| Time to get to target (seconds) | N | 16 | 16 | 32 | ||
| Mean | 183.94 | 150.81 | 167.38 | 0.483 | ||
| Standard Deviation | 159.84 | 95.80 | 130.71 | |||
| Minimum | 47.00 | 30.00 | 30.00 | |||
| Maximum | 531.00 | 327.00 | 531.00 | |||
4. Discussion
The results of this study show that medical students and residents desiring to learn fluoroscopy needle navigation should not expect improvement in performance in fluoroscopy needle navigation from ultrasound based training alone. We believe that the main reason why the needle navigation time to reach target under fluoroscopy was not greatly reduced by a practice on ultrasound was due to the way the needle was viewed on the screen. Although the needle navigation itself might be better understood by trainees first exposed to an in-plane ultrasound practice session, this does not translate into a better performance on obtaining initial pin-point view or hub-view required for navigation towards the target under fluoroscopy guidance. As described in the introduction, there are 2 phases to proper needle utilization under fluoroscopy, the initial positioning for hub-view then the advancement or driving phase of the needle. Anecdotal observation from the supervising staff physician was that once initial hub-view was obtained, subsequent needle driving was faster in group 2, but this is purely observation. An alternative could have been for the supervisor to set up the initial hub-view and then measure the time to target to more truly reflect needle navigation of the curved needle.
Some participants felt they would be more at ease navigating the needle under fluoroscopy had they tried the ultrasound first.
The great variability in time to reach the target is probably explained by the comfort manipulating the needle in general, not just understanding the way the needle navigates through the muscle. It was clear for the physician measuring the time to reach the target under fluoroscopy that for every participant that the majority of the time required to reach the target was spent on aligning the needle in order to obtain a hub-view of the needle. Once the needle was properly aligned, each participant advanced the needle to varying degrees of comfort towards the target. Having not planned to measure the 2 steps of needle advancement separately was a limitation of this study and may have contributed to under-evaluating the effect of the ultrasound session to help with the needle navigation phase. In very novice participants as it was chosen for this study to properly represent novice trainees in their residency, the comfort level with a needle and the proper alignment for needle a pin point view under fluoroscopy were much more significantly affecting the time required to reach the target. Although improvement in performance was shown in previous studies comparing the needle navigation within one visualization modality; either ultrasound or fluoroscopy, we did not demonstrate any statistically significant improvement when jumping from one modality to the other, herein ultrasound to fluoroscopy. We believe that this transposition of skills from one modality to the other was probably not translating into a significant change because the practice round was not long enough. It is likely that repeated ultrasound practice does improve the needle navigation in fluoroscopy as well, but not after 1 h of practice.
We believe the curriculum to train a physiatry, anesthesia or radiology resident for fluoroscopy injection should prioritize simulation with a fluoroscope. The expected benefits of prior ultrasound practice sessions before fluoroscopy practice sessions was not conclusive to a better performance under fluoroscopy needle navigation with our outcome measure.
Further studies on the subject need to be done to demonstrate the most adequate way of facilitating needle navigation acquisition. A study evaluating whether the time to reach a target under fluoroscopy is improved if the needle was already placed in a pinpoint view at a specific distance from the target would be interesting. This would reduce time required by the participants to reach the target. Also, this study assessed the learning after only an hour long group ultrasound practice session. A longer, individual ultrasound session should also be compared to evaluate if there is any significant difference. The hour-long session was chosen because it reflects an easily reproducible “boot camp” class currently being taught in the curriculum of many physiatry programs.
5. Limitation of this study
There are sources of bias in this study. Participants were obviously not blinded to their group allocation. There was a significant source of bias when taking measurements under fluoroscopy. Participants are aware of their prior exposure. A participant knew that they would be exposed to ultrasound training prior to their fluoroscopy session and this may impact the performance in fluoroscopy. We hoped to give participants as little information as possible as to which of the two techniques is the independent factor.
The physician who led the teaching session under ultrasound was unblinded to the group they were supervising.
The physicians assessing the fluoroscopy needle navigation were however blinded to the group allocation. The ultrasound session can familiarize the participants with the materials (needle and pig's foot). We attempted to diminish the improvement attributable to the knowledge behind the manipulation by giving a theoretical session to both groups. We believe that some of the improvement in time to target may be attributable to familiarization with the materials, but this difference also reflects the current reality of a resident who has had no prior ultrasound training.
6. Conclusion
Fluoroscopy needle navigation training was not improved by a 1-h group practice session with in-plane ultrasound needle navigation practice.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Meisinger Q.C., Stahl C.M., Andre M.P., Kinney T.B., Newton I.G. Radiation protection for the fluoroscopy operator and staff. AJR Am J Roentgenol. 2016 Oct;207(4):745–754. doi: 10.2214/AJR.16.16556. Epub 2016 Jul 19. PMID: 27440524. [DOI] [PubMed] [Google Scholar]
- 2.Kallem V., Cowan N.J. IEEE int conf robot autom. 2007 apr 10. 2007. Image-guided control of flexible bevel-tip needles; pp. 3015–3020. PMID: 21359170; PMCID: PMC3043465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barthet M., Gasmi M., Boustiere C., et al. EUS training in a live pig model: does it improve echo endoscope hands-on and trainee competence? Endoscopy. 2007;39(6):535–539. doi: 10.1055/s-2007-966336. [DOI] [PubMed] [Google Scholar]
- 4.Fritscher-ravens A., Cuming T., Dhar S., et al. Endoscopic ultrasound-guided fine needle aspiration training: evaluation of a new porcine lymphadenopathy model for in vivo hands-on teaching and training, and review of the literature. Endoscopy. 2013;45(2):114–120. doi: 10.1055/s-0032-1325931. [DOI] [PubMed] [Google Scholar]
- 5.Kim S.C., Hauser S., Staniek A., Weber S. Learning curve of medical students in ultrasound-guided simulated nerve block. J Anesth. 2014;28(1):76–80. doi: 10.1007/s00540-013-1680-y. [DOI] [PubMed] [Google Scholar]
- 6.Yang H., Schaffer K., Liu L., Mahesh M., Yousem D.M. Benchmarking lumbar puncture fluoroscopy time during fellowship training. AJNR Am J Neuroradiol. 2017;38(3):656–658. doi: 10.3174/ajnr.A5031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Charnoff J., Naqvi U., Weaver M., Price C. Resident education of ultrasound guided procedures: a homemade practice model pilot study. Am J Phys Med Rehabil. 2019;98(10):e116–e118. doi: 10.1097/PHM.0000000000001259. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.